Professional Documents
Culture Documents
Articles: Background
Uploaded by
Bianca AlinaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Articles: Background
Uploaded by
Bianca AlinaCopyright:
Available Formats
Articles
Brexanolone injection in post-partum depression:
two multicentre, double-blind, randomised,
placebo-controlled, phase 3 trials
Samantha Meltzer-Brody, Helen Colquhoun, Robert Riesenberg, C Neill Epperson, Kristina M Deligiannidis, David R Rubinow, Haihong Li,
Abdul J Sankoh, Christine Clemson, Amy Schacterle, Jeffrey Jonas, Stephen Kanes
Summary
Background Post-partum depression is associated with substantial morbidity, and improved pharmacological treatment Published Online
options are urgently needed. We assessed brexanolone injection (formerly SAGE-547 injection), a positive allosteric August 31, 2018
http://dx.doi.org/10.1016/
modulator of γ-aminobutyric-acid type A (GABAA) receptors, for the treatment of moderate to severe post-partum S0140-6736(18)31551-4
depression.
Department of Psychiatry,
University of North Carolina
Methods We did two double-blind, randomised, placebo-controlled, phase 3 trials, at 30 clinical research centres and School of Medicine, Chapel Hill,
specialised psychiatric units in the USA. Eligible women were aged 18–45 years, 6 months post partum or less at NC, USA (S Meltzer-Brody MD,
Prof D R Rubinow MD); Sage
screening, with post-partum depression and a qualifying 17-item Hamilton Rating Scale for Depression (HAM-D) Therapeutics, Cambridge, MA,
score (≥26 for study 1; 20–25 for study 2). Women with renal failure requiring dialysis, anaemia, known allergy to USA (H Colquhoun MD, H Li PhD,
allopregnanolone or to progesterone, or medical history of schizophrenia, bipolar disorder, or schizoaffective A J Sankoh PhD, C Clemson PhD,
disorder were excluded. Patients were randomly assigned (1:1:1) to receive a single intravenous injection of either A Schacterle PhD, J Jonas MD,
S Kanes MD); Atlanta Center for
brexanolone 90 µg/kg per h (BRX90), brexanolone 60 µg/kg per h (BRX60), or matching placebo for 60 h in study 1, Medical Research, Atlanta, GA,
or (1:1) BRX90 or matching placebo for 60 h in study 2. Patients, the study team, site staff, and the principal USA (R Riesenberg MD);
investigator were masked to treatment allocation. The primary efficacy endpoint was the change from baseline in the Department of Psychiatry,
17-item HAM-D total score at 60 h, assessed in all patients who started infusion of study drug or placebo, had a valid Perelman School of Medicine,
University of Pennsylvania,
HAM-D baseline assessment, and had at least one post-baseline HAM-D assessment. The safety population included Philadelphia, PA, USA
all randomised patients who started infusion of study drug or placebo. Patients were followed up until day 30. The (Prof C N Epperson MD);
trials have been completed and are registered with ClinicalTrials.gov, numbers NCT02942004 (study 1) and Feinstein Institute for Medical
NCT02942017 (study 2). Research, Northwell Health,
Manhasset, NY, USA
(K M Deligiannidis MD); and
Findings Participants were enrolled between Aug 1, 2016, and Oct 19, 2017, in study 1, and between July 25, 2016, and Department of Psychiatry,
Oct 11, 2017, in study 2. We screened 375 women simultaneously across both studies, of whom 138 were randomly Zucker Hillside Hospital,
assigned to receive either BRX90 (n=45), BRX60 (n=47), or placebo (n=46) in study 1, and 108 were randomly assigned to Glen Oaks, NY, USA
(K M Deligiannidis)
receive BRX90 (n=54) or placebo (n=54) in study 2. In study 1, at 60 h, the least-squares (LS) mean reduction in HAM-D
Correspondence to:
total score from baseline was 19·5 points (SE 1·2) in the BRX60 group and 17·7 points (1·2) in the BRX90 group Dr Samantha Meltzer-Brody,
compared with 14·0 points (1·1) in the placebo group (difference –5·5 [95% CI –8·8 to –2·2], p=0·0013 for the BRX60 Department of Psychiatry,
group; –3·7 [95% CI –6·9 to –0·5], p=0·0252 for the BRX90 group). In study 2, at 60 h, the LS mean reduction in University of North Carolina
HAM-D total score from baseline was 14·6 points (SE 0·8) in the BRX90 group compared with 12·1 points (SE 0·8) for School of Medicine Chapel Hill,
NC 27514, USA
the placebo group (difference –2·5 [95% CI –4·5 to –0·5], p=0·0160). In study 1, 19 patients in the BRX60 group and samantha_meltzer-brody@
22 patients in the BRX90 group had adverse events compared with 22 patients in the placebo group. In study 2, 25 patients med.unc.edu
in the BRX90 group had adverse events compared with 24 patients in the placebo group. The most common treatment-
emergent adverse events in the brexanolone groups were headache (n=7 BRX60 group and n=6 BRX90 group vs n=7
placebo group for study 1; n=9 BRX90 group vs n=6 placebo group for study 2), dizziness (n=6 BRX60 group and n=6
BRX90 group vs n=1 placebo group for study 1; n=5 BRX90 group vs n=4 placebo group for study 2), and somnolence
(n=7 BRX60 group and n=2 BRX90 group vs n=3 placebo group for study 1; n=4 BRX90 group vs n=2 placebo group for
study 2). In study 1, one patient in the BRX60 group had two serious adverse events (suicidal ideation and intentional
overdose attempt during follow-up). In study 2, one patient in the BRX90 group had two serious adverse events (altered
state of consciousness and syncope), which were considered to be treatment related.
Interpretation Administration of brexanolone injection for post-partum depression resulted in significant and clinically
meaningful reductions in HAM-D total score at 60 h compared with placebo, with rapid onset of action and durable
treatment response during the study period. Our results suggest that brexanolone injection is a novel therapeutic drug
for post-partum depression that has the potential to improve treatment options for women with this disorder.
Funding Sage Therapeutics, Inc.
Copyright © 2018 Sage Therapeutics, Inc.
www.thelancet.com Published online August 31, 2018 http://dx.doi.org/10.1016/S0140-6736(18)31551-4 1
Articles
Research in context
Evidence before this study allosteric modulator mechanism in post-partum depression or
The relevance of γ-aminobutyric acid (GABA) signalling in major depressive disorder.
post-partum depression has been established by numerous
Added value of this study
studies in animals and humans. Plasma concentrations of the
The two studies presented are the first phase 3 clinical trials to
neuroactive steroid allopregnanolone, a positive allosteric
investigate the efficacy of brexanolone injection in post-partum
modulator of GABA type A (GABAA) receptors, increase during
depression and the second and third study of a trio of
pregnancy and decrease substantially after childbirth in both
placebo-controlled post-partum depression studies done
rodents and humans, and fluctuations in allopregnanolone
according to one umbrella protocol. If the use of brexanolone
have profound effects on anxiety and depression in animal
injection is approved by regulatory authorities, this drug could
models. Additionally, GABAergic signalling might be regulated
be the first pharmacological therapy specifically indicated for
by compensatory post-partum changes in GABAA receptor
post-partum depression. In contrast to brexanolone injection,
levels and composition. Deletion of the GABAA receptor δ
currently available pharmacological treatments for depression,
subunit gene in mice results in maternal depression phenotypes
such as selective serotonin-reuptake inhibitors (SSRIs), have
restricted to the post-partum period that can be reversed by
limited links to existing hypotheses regarding the cause of
administration of the GABAA agonist
post-partum depression. The onset of efficacy for SSRIs ranges
4,5,6,7-tetrahydroisoxazolo[5,4-c]pyridin-3-ol. Furthermore,
from at least 1–2 weeks to months, and remission rates in post-
mice deficient in the potassium-chloride cotransporter (KCC2),
partum depression remain low. The current trials, and previous
which is required for functional GABA signalling, also
studies of brexanolone injection, suggest the potential to
demonstrate these maternal depression phenotypes and lack
develop a post-partum depression medication with the
the ability to suppress stress-induced activation of the
possibility of a rapid onset that could alleviate the substantial
hypothalamic-pituitary-adrenal axis, an additional pathway
impact of post-partum depression on the mother, her infant,
implicated in the development of post-partum depression.
and family.
Previous phase 1 and 2 clinical studies of brexanolone injection,
a proprietary formulation of allopregnanolone, have Implications of all the available data
demonstrated promising treatment effects in measures of Preclinical studies with allopregnanolone and clinical studies of
mood symptoms in post-partum depression. These data brexanolone injection, including the current phase 3 studies,
supported further exploration of the association between suggest that positive allosteric modulation of GABAA receptors
positive allosteric modulation of GABAA receptors and is a viable therapeutic approach that might provide additional
post-partum depression. treatment options for women with untreated post-partum
We searched PubMed from database inception to Feb 13, 2018, depression. Additional treatment options for post-partum
without language restrictions, for publications using the search depression might have important implications across two
terms “allopregnanolone,” “neuroactive steroid,” “GABAA generations since studies suggest that untreated post-partum
positive allosteric modulator,” “postpartum depression,” depression impacts the mother and her child. Our trials support
“depression,” and “major depressive disorder”. With the current and future regulatory applications for brexanolone
exception of our two previous studies of brexanolone injection injection and the continued study of GABAA receptor positive
in post-partum depression, our search retrieved no clinical trials allosteric modulators for the treatment of post-partum
investigating the neuroactive steroid or GABAA positive depression.
Introduction maternal morbidity and child morbidity associated
Post-partum depression is the most common com- with impaired mother–infant attachment, and infant
plication of childbirth and can result in considerable malnutrition during the first year of life.1,10–12
suffering for mothers, children, and families.1,2 Post- The underlying mechanisms of impaired mother–infant
partum depression is estimated to affect 10–20% of attachment are likely due to multiple aspects of disrupted
women who give birth worldwide, and occurs in low- parenting, sometimes termed lack of sensitivity, observed
income, middle-income, and high-income countries.1–4 in mothers with post-partum depression, including poor
Approximately 40–80% of cases of post-partum depression responsiveness, poor recognition of infant cues, dis
are considered moderate to severe.1,3,5,6 In the USA, the engagement and withdrawal, and intrusiveness.13,14 The
estimated prevalence of post-partum depression in new degree of parental sensitivity is associated with a child’s
mothers varies by state from 8–20%, with an overall mean emotional regulation during infancy, and studies15 suggest
prevalence of 11·5%.2 The public health impact of post- that infants of mothers with untreated post-partum
partum depression is substantial; in the UK, the estimated depression might demonstrate an increased risk of
cost per case is £74 000.7 This economic burden is difficulty with emotional regulation in early life and social
multifactorial, but contributing factors include maternal behaviour as a consequence of disrupted parenting. This
death from suicide,8,9 loss of work days due to depression, increased risk can continue through adolescence and can
2 www.thelancet.com Published online August 31, 2018 http://dx.doi.org/10.1016/S0140-6736(18)31551-4
Articles
be associated with poorer outcomes, including decreased integrated data analyses with our previous phase 2 trial,37
academic performance and increased risk of depression.16–18 which was completed before the initiation of study 1 and 2.
Antidepressant treatment of post-partum depression with Patients were recruited to clinical research centres
a 12 week course of therapy has been associated with and specialised psychiatric units through self-referrals,
improvements in the quality of mother–infant interaction physician referrals, and radio-based, television-based, and
and infant play.19 Increased understanding of the broad web-based methods. Pre-screening was done through
impact of post-partum depression has led to an treatment site patient database searches or phone
international consensus on the importance of screening interviews to confirm patients met high-level entry
and early treatment of post-partum depression.15,20–22 criteria (ie, ≤6 months post partum, feeling depressed or
The stigma associated with maternal psychiatric anxious, aged 18 years or older). The principal investigator
illness often prevents mothers from seeking treatment at each site was responsible for recruitment and
for post-partum depression, and substantial disparities enrolment of patients. The trials were deemed complete
in education, country, race, and ethnicity might restrict when pre-determined enrolment targets were achieved.
access to effective treatment.23–25 Many women treated Both trials enrolled ambulatory female participants
for post-partum depression with currently available aged 18–45 years, who provided a signed informed
therapies, such as selective serotonin-reuptake inhibitors consent form before any procedures were done, were in
(SSRIs), do not achieve adequate response or full good physical health with no clinically significant findings
remission of symptoms, and the ability of SSRIs to as determined by the principal investigator on physical
prevent post-partum depression is also unclear.26–28 To examination, 12-lead electrocardiogram (ECG), or clinical
date, no pharmacological therapies have been developed laboratory tests, had agreed to adhere to study require
specifically for post-partum depression. Thus, improved ments, and had stopped lactating at the time of screening
pharmacological treatment options are urgently needed. or had temporarily ceased breastfeeding while receiving
The hypothalamic-pituitary-adrenal (HPA) axis, peri the study drug until 4 days after the end of infusion.
natal hormonal fluctuations, and γ-aminobutyric acid Eligible participants also had to have a negative pregnancy
(GABA) signalling have been implicated in the patho test before initiation of study drug, had a major depressive
physiology of post-partum depression, and previous episode with onset no earlier than the third trimester and
studies29–32 have identified associations between these no later than 4 weeks after delivery, as determined by
potential mechanisms. In mouse models of GABA dys the Structured Clinical Interview for Diagnostic and
function, mice were found to have post-partum de Statistical Manual of Mental Disorders (DSM)-IV Axis I
pression-like maternal behaviours and defects in HPA Disorders (SCID-I),38 had a qualifying HAM-D total score
axis regulation, indicating an association between GABA (≥26 for study 1; 20–25 for study 2) before infusion,39 were
and HPA regulation.29 Additionally, plasma concentra 6 months post partum or less at screening, were willing
tions of allopregnanolone, a potent positive allosteric to delay the start of new pharmacotherapeutic drug
modulator of synaptic and extrasynaptic GABA type A regimens from study drug infusion until completion of
(GABAA) receptors, which is an endogenous progesterone 72 h assessments, and agreed to use an approved form
meta bolite, decrease considerably following childbirth, of birth control during the study and for 30 days there
indicating an association between perinatal hormonal after. Women with onset of post-partum depression in
fluctuations and GABA regulation.33–36 the peri-partum period were included on the basis of
A soluble, proprietary, β-cyclodextrin-based, intra previous literature demonstrating post-partum depression
venous formulation of allopregnanolone—brexanolone development in this time period.6,40,41 Participants taking
injection (formerly SAGE-547 injection)—had rapid prescribed psychotropic medication at baseline had to be
and durable antidepressant effects during the study at a stable dose 14 days before screening until completion
period in our previous double-blind, randomised, of the 72 h assessments. Concomitant psychotropic
phase 2 clinical trial.37 Here, we report the results of two medications are listed in the appendix. See Online for appendix
large phase 3, double-blind, randomised, placebo- Individuals were excluded if they had renal failure
controlled trials of brexanolone injection in women requiring dialysis, fulminant hepatic failure, anaemia
with moderate to severe post-partum depression. (baseline haemoglobin <10 g/dL), known allergy to
Additionally, integrated results from all three, placebo- allopregnanolone or to progesterone, active psychosis
controlled trials of brexanolone injection in post- (determined by investigator), medical history of schizo
partum depression are presented. phrenia, bipolar disorder, or schizoaffective disorder, had
attempted suicide during the current episode of post-
Methods partum depression, or a history of alcohol or drug abuse
Study design and participants in the previous 12 months (by self-report or drug
We did two multicentre, randomised, double-blind, screening). Individuals were also excluded if they had
placebo-controlled phase 3 trials at 30 clinical research been exposed to another investigational medication up to
centres and specialised psychiatric units in the USA 30 days before screening, had previously participated in
under an umbrella protocol that facilitated subsequent this study or other studies of brexanolone injection,
www.thelancet.com Published online August 31, 2018 http://dx.doi.org/10.1016/S0140-6736(18)31551-4 3
Articles
or had electro-convulsive therapy up to 14 days before Statistics and Consulting and 4G Clinical until database
screening or had therapy planned within 7 days after lock, to maintain blinding of study personnel throughout
infusion. the studies. In the event of a medical emergency, the
Relevant institutional review boards or independent principal investigator was required to contact the medical
ethics committee approved both studies, and all patients monitor to initiate the unmasking process; no such
provided written informed consent. unmasking events occurred.
Randomisation and masking Procedures
Eligible patients were randomly assigned (1:1:1) to Brexanolone injection is a sterile solution of 5 mg/mL
receive brexanolone injection 90 µg/kg per h (BRX90), allopregnanolone in 250 mg/mL sulfobutylether-β-cyclo-
brexanolone injection 60 µg/kg per h (BRX60), or dextrin, which is buffered with citrate and diluted with
matching placebo infusion in study 1, or (1:1) BRX90 or sterile water to render it isotonic for intravenous use.37
matching placebo infusion in study 2, according to a For the BRX90 groups, each patient received a single
computer-generated randomisation. The first random continuous infusion of study drug for 60 h according to
isation schedule for each study was generated by Applied the following schedule: 30 µg/kg per h (0–4 h); 60 µg/kg
Statistics and Consulting (Spruce Pine, NC, USA), and per h (4–24 h); 90 µg/kg per h (24–52 h); 60 µg/kg per h
subsequent schedules were generated by Sage (52–56 h); 30 µg/kg per h (56–60 h). Patients in the
Therapeutics, Inc (Cambridge, MA, USA). The second BRX60 group received study drug according to the same
and third randomisation schedules were produced to dosing schedule, but were administered 60 µg/kg per h
accommodate regulatory authority requests for increased at 24–52 h. The dose and infusion rates were based
sample sizes and stratification of randomisation based on on pharmacokinetic modelling and previous studies.37,42
antidepressant use, and were implemented using Prancer Changes to infusion rates were made on the basis of
interactive response technology system (4G Clinical, pre-determined protocol rules and tolerability. Patients
Wellesley, MA, USA): the second list was unstratified and were treated in a medically-supervised setting for 72 h,
the third list was stratified by antidepressant use. Overall, consisting of 60 h of study drug infusion and an
less than 25% of the randomly assigned participants in additional 12 h for completion of assessments. Patients
the two studies were randomised manually using the were followed up until day 30, with clinical and safety
first randomisation list. The remaining participants were assessments done at days 7 and 30.
randomly assigned using interactive response technology
based on the second and third lists. All participants in Outcomes
study 1 were randomly assigned using a block size of 6. In The primary efficacy outcome measure in both
study 2, the first randomisation list used a block size of studies 1 and 2 was the change from baseline in mean
2 and subsequent lists had a block size of 4. MedSource 17-item Hamilton Rating Scale for Depression (HAM-D)39
(Houston, TX, USA) provided masked randomisation total score at 60 h post-infusion. Blinded on-site raters
code lists to the site pharmacists for treatment assignment were trained on the use of the HAM-D scale by MedAvante
for the first randomisation list in each study. The Prancer (Hamilton, NJ, USA) to enable consistent scoring. The
interactive response technology system dispensed treat on-site investigators made the final decision on the
ment assignments for subsequent randomisation lists. HAM-D scores throughout the study. An additional
The site pharmacist who prepared the study drug quality control measure was introduced during the
(brexanolone injection or matching placebo) was not study (for approximately 50% of patients enrolled in
masked to treatment assignment. The site pharmacist studies 1 and 2) to have the HAM-D interviews recorded
provided masked study drug to the study team with only and scored by an independent, blinded, central reviewer
the rate of infusion noted to maintain study blind. at MedAvante (who was not an employee of the study
Patients, the study team (including medical monitors), sponsor) to ensure that each site was following the
site staff (with the exception of the pharmacists), and the HAM-D rater guidelines and to provide an opportunity
principal investigator were masked to treatment alloca for intervention, such as retraining the site raters, if
tion, and infusion bags for all treatment groups were needed. The on-site rater could decide to accept or reject
identical in appearance. Two placebo infusion rates were the central rater score if the two scores were different.
used in study 1 and one placebo infusion rate in study 2, Additional information on rating is described in the
which matched the active dose groups, thereby fully appendix.
maintaining the blind. Secondary efficacy outcome measures were mean
The shared study database for studies 1 and 2 was locked HAM-D total score and least-squares (LS) mean change
when the final visit of the last randomised and infused from baseline during the inpatient stay at 0, 2, 4, 8,
patient was completed, data entry into the database for all 12, 24, 36, 48, 60, and 72 h after infusion and follow-up
patients was completed, and the database for all patients days 7 and 30; Clinical Global Impression-Improvement
was deemed clean, without any outstanding queries (CGI-I) response, defined as a rating of 1 (very
(Nov 3, 2017). Randomisation lists were held by Applied much improved) or 2 (much improved);43 change from
4 www.thelancet.com Published online August 31, 2018 http://dx.doi.org/10.1016/S0140-6736(18)31551-4
Articles
baseline in score on the Montgomery-Åsberg Depression repeated measures. The model included study, pooled
Rating Scale;44 change from baseline in HAM-D subscale study site, treatment, baseline antidepressant use, visit
(including Bech 6,45 Core,46 Anxiety,47 and Maier48) score timepoint, and treatment-by-visit timepoint interaction
and individual item scores; and change from baseline in terms as fixed effects, and baseline HAM-D total score as
scores on the Edinburgh Postnatal Depression Scale,49 a covariate. For safety analyses, a conservative approach
Patient Health Questionnaire 9,50 and the Generalized was used, including treatment-emergent adverse events
Anxiety Disorder 7-item questionnaire.51 observed in any group receiving brexanolone injection.
Safety and tolerability were investigated by recording All statistical analyses were done using SAS (version 9.3).
adverse events, vital signs, clinical laboratory assessments, The completed trials are registered with ClinicalTrials.gov,
ECG parameters, and Columbia Suicide Severity Rating numbers NCT02942004 (study 1) and NCT02942017
Scale scores.52 (study 2).
Statistical analysis Role of the funding source
On the assumption of a two-sided t test at an α level of The study funder was involved in the study design, data
0·05 for study 1, a sample size of 120 patients (40 patients analysis, interpretation, and writing of the report. All
per group) would provide 90% power to detect a mean authors had full access to all the data, and the corres
treatment difference of 9·0 between the brexanolone and ponding author had final responsibility for the decision
placebo groups, with an assumed SD of 12 points. On the to submit for publication.
assumption of a two-sided t test at an α level of 0·05 for
study 2, a sample size of 100 patients (50 patients per Results
group) would provide 90% power to detect a mean Study 1 was done between Aug 1, 2016, and Oct, 19, 2017,
treatment difference of 8·0 between the brexanolone and and study 2 between July 25, 2016, and Oct 11, 2017.
placebo groups, with an assumed SD of 12 points. Across both studies, we screened 375 women simul
The primary efficacy endpoint was analysed in the taneously, of whom 138 were randomly assigned to
modified intention-to-treat population, which included receive either BRX90 (n=45), BRX60 (n=47), or placebo
all patients who started infusion of study drug or placebo, (n=46) in study 1, and 108 were randomly assigned
had a valid HAM-D baseline assessment, and had at to receive BRX90 (n=54) or placebo (n=54) in study 2
least one post-baseline HAM-D assessment. The safety (figure 1). 25 (18%) of 138 patients discontinued study 1,
population included all randomised patients who started and eight (7%) of 108 patients discontinued study 2. The
infusion of study drug or placebo. most common reasons for discontinuation were patients
For both studies, LS mean HAM-D total score and the did not receive the infusion, were lost to follow-up,
change in LS mean HAM-D total score from baseline or withdrew consent (appendix). In both studies, the
were analysed using a mixed effects model for repeated number of patients in the safety and efficacy analysis
measures, as prespecified in the protocol and statistical populations were the same. Three (2%) of 122 patients in
analysis plan. The linear model included centre (pooled), study 1, and three (3%) of 104 patients in the study 2 had
treatment, baseline antidepressant use, baseline HAM-D missing data for the primary efficacy outcome at 60 h. All
total score, assessment timepoint, and timepoint-by- patients in both studies had at least one safety assessment.
treatment as explanatory variables, which were treated as Demographics and baseline characteristics were gen
fixed effects. Least square means, 95% CIs, and p values erally well balanced across treatment groups within
were calculated using model-based point estimates and each study (table 1). In study 1, the mean age was
reported for each timepoint. A generalised estimating 27·8 years (SD 6·0) in the BRX90 group, 27·3 years
equation method for repeated binary responses was used (6·1) in the BRX60 group, and 27·0 years (6·0) in the
to analyse categorical variables, such as response and placebo group. In study 2, the mean age was 28·4 years
remission. (SD 6·1) in the BRX90 group and 27·4 years (5·9) in the
We did a separate, pre-planned analysis of the placebo group. Of 246 patients included in both studies,
integrated datasets from our previous 2017 trial,37 and most patients were white (153 [62%]); 86 (35%) were
studies 1 and 2, using the same statistical methods as black or African-American and 43 (17%) were Hispanic
previously described, to assess the safety and efficacy of or Latino. The onset of post-partum depression was
brexanolone in the largest possible placebo-controlled similar across all groups. Across all cohorts in both
post-partum depression patient population. The studies, a higher proportion of patients had onset of
integrated analysis was preplanned in conjunction with post-partum depression within 4 weeks of delivery than
regulatory authorities for the efficacy and safety analyses. the third trimester (range 67–78%). Across both studies,
For efficacy analyses, all placebo groups and all BRX90 53 (22%) of 246 patients were taking antidepressants at
groups were integrated. Efficacy data for the single baseline. The use of psychotropic medication is shown
BRX60 group was not included in this integrated in the appendix.
analysis. Similar to the individual studies, the primary At the end of the 60 h infusion, in study 1, the LS mean
endpoint was analysed using a mixed effects model for reduction in HAM-D total score was 19·5 points (SE 1·2)
www.thelancet.com Published online August 31, 2018 http://dx.doi.org/10.1016/S0140-6736(18)31551-4 5
Articles
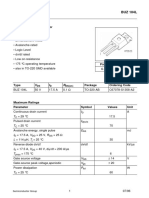
Study 1 Study 2
375 women assessed 375 women assessed
for eligibility* for eligibility*
129 ineligible* 129 ineligible*
138 randomly 108 randomly
assigned assigned
46 assigned to 47 assigned to 45 assigned to 54 assigned to 54 assigned to
placebo BRX60 BRX90 placebo BRX90
3 did not receive 9 did not receive 4 did not receive 1 did not receive 3 did not receive
infusion infusion infusion infusion infusion
2 screening 3 positive drug 2 withdrew 1 withdrew 2 withdrew
critera not screen consent consent consent
confirmed 2 withdrew 1 positive drug 1 screening critera
1 withdrew consent screen not confirmed
consent 2 screening 1 randomised in
criteria error
not confirmed
1 infant illness
1 did not present
43 received placebo 38 received BRX60 41 received BRX90 53 received placebo 51 received BRX90
1 discontinued 3 discontinued 5 discontinued 1 discontinued 3 discontinued
treatment treatment treatment treatment treatment
1 lost to follow-up 2 withdrew 3 withdrew 1 lost to follow-up 1 lost to follow-up
consent consent 1 withdrew
1 lost to follow-up 2 lost to follow-up consent
1 adverse event
42 completed the 35 completed the 36 completed the 52 completed the 48 completed the
study study study study study
43 included in mITT 38 included in mITT 41 included in mITT 53 included in mITT 51 included in mITT
efficacy efficacy efficacy efficacy efficacy
population population population population population
43 included in safety 38 included in safety 41 included in safety 53 included in safety 51 included in safety
population population population population population
Figure 1: Trial profiles for studies 1 and 2
mITT=modified intention-to-treat. BRX60=brexanolone injection 60 µg/kg per h. BRX90=brexanolone injection 90 µg/kg per h. *Screening for studies 1 and
2 was done simultaneously because of protocol similarities, thus the same 375 women were screened for both studies. In study 1, data for the 60 h (primary
outcome) were available for 43 patients in the placebo group, 37 patients in the BRX60 group, and 39 patients in the BRX90 group. Data was obtained from
42 patients in the placebo group, 35 patients in the BRX60 group, and 36 patients in the BRX90 group at day 30. In study 2, data for the 60 h (primary outcome)
were available for 52 patients in the placebo group and 49 patients in the BRX90 group. Data was obtained from 52 patients in the placebo group and 48 patients
in the BRX90 at day 30.
in the BRX60 group and 17·7 points (1·2) in the BRX90 with 12·1 points (0·8) in the placebo group (–2·5 [95% CI
group compared with 14·0 points (1·1) in the placebo –4·5 to –0·5], p=0·0160; table 2).
group (table 2). The mean difference between the placebo In study 1, HAM-D total scores were significantly
group and both brexanolone injection groups was reduced in the BRX60 group compared with the placebo
statistically significant (–5·5 [95% CI –8·8 to –2·2], group at 24 h and all timepoints thereafter in the BRX60
p=0·0013 for BRX60; –3·7 [–6·9 to –0·5], p=0·0252 for group. In study 2, HAM-D total scores were significantly
BRX90; table 2). At the end of the 60 h infusion, in study 2, reduced in the BRX90 group compared with the placebo
the mean reduction in HAM-D total score from baseline group at 48 h and until day 7 (table 2). HAM-D total
was 14·6 points (SE 0·8) in the BRX90 group compared score did not return to baseline by day 30 in any of the
6 www.thelancet.com Published online August 31, 2018 http://dx.doi.org/10.1016/S0140-6736(18)31551-4
Articles
Study 1 Study 2
Placebo (n=46) BRX60 (n=47) BRX90 (n=45) Placebo (n=54) BRX90 (n=54)
Characteristics
Age, years 27·0 (6·0) 27·3 (6·1) 27·8 (6·0) 27·4 (5·9) 28·4 (6·1)
Ethnicity
Hispanic or Latino 8 (17%) 3 (6%) 7 (16%) 14 (26%) 11 (20%)
Not Hispanic or Latino 38 (83%) 44 (94%) 38 (84%) 40 (74%) 43 (80%)
Race
Black or African-American 17 (37%) 15 (32%) 12 (27%) 19 (35%) 23 (43%)
White 28 (61%) 31 (66%) 29 (64%) 34 (63%) 31 (57%)
Other 1 (2%) 1 (2%) 4 (9%) 1 (2%) 0
Height, cm 165·3 (7·9) 163·9 (6·2) 164·3 (6·6) 162·5 (8·3) 164·3 (6·0)
Weight, kg 82·2 (23·3) 83·8 (20·7) 80·7 (20·6) 86·5 (24·3) 86·7 (24·3)
Body-mass index, kg/m² 30·1 (8·2) 31·2 (7·5) 29·8 (7·0) 32·6 (8·1) 32·0 (8·3)
Personal history of psychiatric disorders
Depression (non-PPD) 20 (43%) 19 (40%) 21 (47%) 18 (33%) 13 (24%)
Anxiety 15 (33%) 20 (43%) 21 (47%) 19 (35%) 17 (31%)
Premenstrual dysphoric disorder 0 1 (2%) 3 (7%) 1 (2%) 2 (4%)
Substance abuse 0 0 1 (2%) 0 1 (2%)
Other 3 (7%) 5 (11%) 2 (4%) 3 (6%) 2 (4%)
Previous PPD episodes 16 (35%) 17 (36%) 12 (27%) 21 (39%) 19 (35%)
Family history of PPD
Yes 9 (20%) 13 (28%) 16 (36%) 13 (24%) 17 (31%)
No 37 (80%) 34 (72%) 29 (64%) 41 (76%) 37 (69%)
Onset of PPD
Third trimester 14 (30%) 11 (23%) 10 (22%) 12 (22%) 12 (22%)
Within 4 weeks of delivery 31 (67%) 35 (74%) 35 (78%) 42 (78%) 42 (78%)
Antidepressant use
Baseline antidepressant use 12 (26%) 12 (26%) 10 (22%) 10 (19%) 9 (17%)
Previous antidepressant use 14 (30%) 15 (32%) 13 (29%) 10 (19%) 12 (22%)
Concomitant antidepressant use 14 (30%) 14 (30%) 13 (29%) 15 (28%) 12 (22%)
Other measures*
HAM-D 28·6 (2·5) 29·1 (2·7) 28·4 (2·5) 22·7 (1·6) 22·6 (1·6)
EPDS 21·7 (3·0) 21·7 (3·4) 20·0 (3·9) 18·7 (4·1) 18·9 (3·9)
Data are n (%) or mean (SD). Weight, height, and body-mass index data were obtained at screening. Medical histories were coded according to the Medical Dictionary for
Regulatory Activity version 19.1 or later. BRX60=brexanolone injection 60 µg/kg per h. BRX90=brexanolone injection 90 µg/kg per h. PPD=post-partum depression.
HAM-D=Hamilton Rating Scale for Depression. EPDS=Edinburgh Postnatal Depression Scale. *Assessed before infusion on day 1.
Table 1: Baseline demographics and characteristics
brexanolone groups (figure 2). In study 1, the LS mean significant difference identified in HAM-D total scores
reduction in HAM-D total score in both BRX60 and between the BRX90 and placebo groups at day 30 (table 2).
BRX90 groups at day 30 was similar to that observed at the In study 1 and 2, the LS mean change in HAM-D total
end of the 60 h infusion (19·5 points [SE 1·4] at day 30 vs score from baseline was similar for patients in the brex
19·5 points [1·2] at 60 h for BRX60; 17·6 points [1·4] at anolone injection groups with and without concomitant
day 30 vs 17·7 points [1·2] at 60 h for BRX90), and the antidepressant treatment, and the proportion of patients
reduction in HAM-D total scores from baseline at who received rescue antidepressant treatment during the
day 30 was significantly higher in the BRX60 group follow-up period was low (appendix).
(p=0·0044) and BRX90 group (p=0·0481) than the placebo HAM-D total scores were further examined for re
group (table 2). In study 2, the LS mean reduction in mission (HAM-D total score ≤7) and response (reduction
HAM-D total score observed in the BRX90 group at day 30 in HAM-D total score ≥50%; appendix). In study 1,
(14·7 points [SE 1·0]) was of similar magnitude to that between 24 h and 72 h and at day 30, the proportions of
observed at the end of the 60 h infusion (14·6 points [0·8]). patients achieving HAM-D remission were higher for
In study 2, a marked improvement in the HAM-D total both the BRX60 and BRX90 groups compared with
score was found in the placebo group after day 7, with no placebo, with statistical significance achieved for the
www.thelancet.com Published online August 31, 2018 http://dx.doi.org/10.1016/S0140-6736(18)31551-4 7
Articles
BRX60 group at multiple timepoints, including at the
p value*
end of the 60 h infusion (19 [51%] of 37 patients in the
0·0389
0·0991
0·0160
0·3280
0·3947
0·4216
0·0022
0·6710
0·0255
0·2522
0·1431
BRX60 group vs seven [16%] of 43 patients in the placebo
group; odds ratio [OR] 6·0 [95% CI 2·1 to 17·8],
The change from baseline in the total LS mean HAM-D score was analysed using a mixed effects model for repeated measures. p values were calculated by two-sided t test. HAM-D=Hamilton Rating Scale for Depression. LS=least squares.
p=0·0011). In study 2, the proportion of patients
–6·1 to -0·4
–4·5 to -0·5
–4·7 to -0·1
–5·7 to -1·3
–3·8 to 0·6
–2·6 to 1·0
–2·1 to 0·9
–2·9 to 1·0
–3·1 to 0·8
–4·1 to 0·4
–2·0 to 3·1
achieving HAM-D remission was higher for the BRX90
95% CI
group than the placebo at all timepoints between 8 h and
day 7 (appendix), reaching statistical significance at
difference*
multiple timepoints, including at the end of the 60 h
–0·8 (0·9)
–0·6 (0·7)
–1·0 (1·0)
–2·4 (1·2)
–3·2 (1·4)
–2·5 (1·0)
–1·6 (1·1)
–1·9 (1·1)
–1·1 (1·0)
0·5 (1·3)
–3·5 (1·1)
LS means
infusion (30 [61%] of 49 patients in the BRX90 group vs
(SE)
20 [38%] of 52 patients in the placebo group; OR 3·4
BRX90 (n=51)
[95% CI 1·5 to 7·9], p=0·0033). The proportion of
change from
baseline (SE)
–4·6 (0·6)
–14·6 (0·8)
–11·4 (0·8)
–13·0 (0·9)
–12·3 (0·8)
–15·3 (0·8)
–9·1 (0·8)
–8·4 (0·7)
–7·3 (0·7)
–14·7 (1·0)
–14·0 (1·1)
patients who achieved a HAM-D response was similar
LS mean
for both brexanolone injection groups in study 1 between
24 h and day 30, with statistical significance achieved
for both the BRX90 and BRX60 groups across multiple
change from
baseline (SE)
–9·8 (0·8)
–10·6 (0·9)
–11·8 (0·8)
–4·0 (0·6)
–8·0 (0·8)
–10·5 (0·8)
–15·2 (0·9)
–6·6 (0·7)
–12·1 (0·8)
–7·4 (0·7)
–10·7 (1·0)
timepoints. The proportion of patients achieving a
LS mean
Study 2
Placebo
(n=53)
HAM-D response in study 2 was also higher in the
BRX90 group compared with placebo between 24 h and
day 7, reaching statistical significance at all timepoints
p value*
0·7968
0·3906
0·6097
0·0481
0·1440
0·3799
0·1389
0·8677
0·7801
0·0252
0·0511
between 48 h and day 7.
HAM-D data were supported by CGI-I response data
(appendix). In study 1, the proportion of patients with
–6·9 to –0·5
–5·9 to 0·8
–7·6 to 0·0
–2·6 to 2·0
–5·5 to 0·8
–2·9 to 2·2
–6·7 to 0·0
–2·0 to 3·5
–5·2 to 2·0
–4·5 to 1·8
–1·7 to 2·0
available response data at 60 h who achieved a CGI-I
95% CI
response was significantly higher in the BRX60 group
(31 [84%] of 37 patients; OR 4·0 [95% CI 1·3 to 11·7],
p=0·0131) and BRX90 group (32 [82%] of 39 patients,
change from difference*(SE)
OR 4·0 [1·4 to 11·6], p=0·0095) than the placebo group
0·2 (0·9)
–1·6 (1·8)
–3·8 (1·9)
–1·4 (1·6)
–2·3 (1·6)
–0·4 (1·3)
–3·7 (1·6)
0·7 (1·4)
–0·3 (1·2)
–2·5 (1·7)
–3·3 (1·7)
LS means
(24 [56%] of 43 patients). The proportion of patients
achieving a CGI-I response was significantly higher in the
BRX60=brexanolone injection 60 µg/kg per h. BRX90=brexanolone injection 90 µg/kg per h. *Compared with placebo.
BRX90 group than the placebo group at 72 h and day 30,
BRX90 (n=41)
baseline (SE)
–7·2 (0·9)
–17·6 (1·4)
–4·9 (0·7)
–13·9 (1·2)
–16·9 (1·2)
–14·9 (1·3)
–8·5 (1·0)
–13·0 (1·2)
–9·1 (1·0)
–17·2 (1·2)
–17·7 (1·2)
and significantly higher in the BRX60 group than the
LS mean
placebo group at 36, 48, 60, and 72 h, and at days 7 and 30.
In study 2, the proportion of patients with available
response data at 60 h who achieved a CGI-I response was
significantly higher in the BRX90 group than the placebo
p value*
0·0046
0·0094
0·0044
0·0288
0·3840
0·0020
0·9591
0·0827
0·0013
0·1292
0·0110
group (39 [79·6%] of 49 patients in the BRX90 group
vs 29 [55·8%] of 52 patients in the placebo group;
OR 5·0 [95% CI 2·0 to 12·5], p=0·0005). These significant
–8·8 to –2·2
–7·7 to –0·4
–8·5 to –1·6
–9·5 to –1·8
–8·3 to –1·9
–7·9 to –1·1
–7·5 to –1·1
–1·8 to 1·9
–4·7 to 0·6
–4·5 to 0·3
–4·1 to 1·6
increases in CGI-I response occurred as early as 36 h and
95% CI
were sustained at day 7. The HAM-D and CGI-I results
are also consistent with additional secondary efficacy out
comes that were directionally supportive (appendix).
difference*
–5·6 (1·9)
–5·5 (1·6)
–4·3 (1·6)
–1·3 (1·4)
–2·0 (1·3)
–5·1 (1·6)
–4·1 (1·8)
–5·0 (1·7)
0·1 (1·0)
–4·5 (1·7)
–2·1 (1·2)
Brexanolone injection was generally well tolerated in
LS means
both studies (table 3; appendix). The most common
(SE)
treatment-emergent adverse events were headache
BRX60 (n=38)
(seven patients in the BRX60 group and six patients in
change from
baseline (SE)
–9·0 (0·9)
–17·4 (1·4)
–5·0 (0·7)
–19·5 (1·4)
–10·2 (1·0)
–15·0 (1·2)
–18·0 (1·3)
–11·0 (1·1)
–19·5 (1·2)
–17·7 (1·2)
–19·7 (1·3)
the BRX90 group vs seven patients in the placebo group
LS mean
for study 1; nine patients in the BRX90 group vs
Table 2: LS mean HAM-D scores
six patients in the placebo group for study 2), dizziness
Placebo (n=43)
(six patients in the BRX60 and BRX90 groups vs
change from
baseline (SE)
–6·9 (0·8)
–8·1 (0·9)
–9·8 (1·0)
–5·0 (0·7)
–13·6 (1·2)
–13·8 (1·3)
–12·6 (1·1)
–14·0 (1·1)
–13·3 (1·3)
–14·7 (1·2)
–10·7 (1·1)
one patient in the placebo group for study 1; five patients
LS mean
Study 1
in the BRX90 group vs four patients in the placebo group
for study 2), and somnolence (seven patients in the
BRX60 group and two patients in the BRX90 group vs
30 days
7 days
48 h
60 h
36 h
24 h
72 h
12 h
three patients in the placebo group for study 1;
8h
4h
2h
four patients in the BRX90 group vs two patients in the
8 www.thelancet.com Published online August 31, 2018 http://dx.doi.org/10.1016/S0140-6736(18)31551-4
Articles
placebo group for study 2), with dizziness and
A Study 1
somnolence occurring more frequently in patients 0 BRX60 (n=38)
receiving brexanolone injection than placebo. These
Change from baseline in mean HAM-D total score (%)
BRX90 (n=41)
Placebo (n=43)
sedation-related events were generally mild, short-lived,
and self-limiting. In study 1, one (3%) of 38 patients in –20
the BRX60 group had two serious adverse events
(suicidal ideation and intentional overdose attempt –40
during follow-up). This patient had three previous
suicide attempts before the study, and the event was not *
–60 * *
considered drug related by the principal investigator. *
**
One (3%) of 38 patients in the BRX60 group had ** *
two severe adverse events (somnolence and loss of con –80
sciousness) during treatment, completing treatment
following interruption of dosing and rapid resolution of End of infusion (60 h)
–100
the adverse events. In study 2, one (2%) of 51 patients in
the BRX90 group had two serious adverse events (altered B Study 2
state of consciousness and syncope), which were mod 0 BRX90 (n=51)
Change from baseline in mean HAM-D total score (%)
erate in intensity and considered to be treatment related. Placebo (n=53)
Two (4%) of 51 patients in the BRX90 group had severe
–20
adverse events (fatigue [n=1] and presyncope [n=1]).
Overall, of the 130 patients who received brexanolone
across studies 1 and 2, five (4%) patients had excessive –40
sedation considered to be due to brexanolone injection;
in all cases, the patients alerted staff and infusion was
–60 *
stopped immediately. All patients who lost consciousness *
*
regained consciousness within 15 min of infusion *
cessation, and all excessive sedation events were –80
completely resolved within 90 min. No respiratory or
haemo-dynamic compromise was associated with these End of infusion (60 h)
–100
cases of excessive sedation. No clinically significant 0 3 6 9 12 15 18 21 24 27 30
differences in laboratory parameters, vital signs, or Time (days)
ECGs were observed between the brexanolone injection
Figure 2: Percentage change from baseline in mean HAM-D total score in
groups and placebo groups. study 1 (A) and 2 (B)
Our previous 2017 phase 2 trial of the BRX90 dose37 was p values were calculated by two-sided t test. BRX60=brexanolone injection
done using the same umbrella protocol as studies 1 and 2, 60 µg/kg per h. BRX90=brexanolone injection 90 µg/kg per h. *p<0·05 vs placebo.
facilitating analysis of integrated comparative efficacy of
BRX90 versus placebo groups across all three trials analyses also showed greater LS mean differences in
(appendix). Patients in the BRX60 group in study 1 were HAM-D score in the BRX90 group compared with the
not included in this integrated analysis. Similar to the placebo group from baseline in all subgroups examined
individual studies, the integrated BRX90 analysis showed for race, age, ethnicity, body-mass index, personal history
a rapid decrease in HAM-D scores (ie, depressive symp of post-partum depression, family history of major
toms) in the BRX90 group compared with the placebo depressive disorder, duration between delivery and index
groups, which was sustained until day 30 (figure 3). At the treatment, time of symptom onset, and HAM-D severity
end of the 60 h infusion, the LS mean reduction in (appendix). The proportion of patients who required
HAM-D total score from baseline was significantly larger rescue medication was low (13 [13%] of 102 patients in
in the BRX90 group than the placebo group (LS mean the BRX90 cohort vs 13 [12%] of 107 patients in the
difference –4·1 [95% CI –6·0 to –2·3], p<0·0001; placebo cohorts; appendix).
appendix), which was also observed at 24 h (–3·0 [95% CI Of the patients with available data, a higher proportion
–4·8 to –1·2], p=0·0012) and was sustained at day 30 of patients in the BRX90 cohort achieved remission than
(–2·6 [95% CI –4·7 to –0·4], p=0·0213). did patients in the placebo cohort between 24 h
In the integrated analysis, the LS mean difference in (26 [26%] of 101 patients in the BRX90 cohort vs 16 [15%] of
HAM-D total score was higher in the BRX90 subgroups 106 patients in the placebo cohort; OR 2·5 [95% CI
(with and without concomitant antidepressant treatment) 1·2 to 5·1], p=0·0142) and day 7 (43 [43%] of 100 patients
than the placebo group at 60 h (–4·3 [95% CI –6·5 to –2·2], in the BRX90 cohorts vs 30 [28%] of 106 patients in the
p<0·0001 for patients without antidepressant treatment; placebo cohorts; OR 2·4 [95% CI 1·2 to 4·5], p=0·0087),
–4·5 [95% CI –8·4 to –0·5], p=0·0282 for patients with and a higher proportion of patients in the BRX90 group
antidepressant treatment; appendix). At 60 h, subgroup had HAM-D response than patients in the placebo group
www.thelancet.com Published online August 31, 2018 http://dx.doi.org/10.1016/S0140-6736(18)31551-4 9
Articles
HAM-D items were consistent with the changes in overall
Study 1 Study 2
HAM-D total scores observed (appendix). These HAM-D
Placebo BRX60 BRX90 Placebo BRX90 results were further supported by the analysis of CGI-I
(n=43) (n=38) (n=41) (n=53) (n=51)
response in the integrated study population: of the
Overall patients who had available data, the proportion of patients
Any adverse event 22 (51%) 19 (50%) 22 (54%) 24 (45%) 25 (49%) who achieved a CGI-I response was significantly higher
Severe adverse event 0 1 (3%) 0 1 (2%) 2 (4%) than placebo at both 24 h (52 [51%] of 101 patients in the
Serious adverse event 0 1 (3%) 0 0 1 (2%) BRX90 group vs 44 [42%] of 106 patients in the placebo
Adverse event leading 1 (2%) 1 (3%) 0 0 2 (4%) group, OR 2·1 [95% CI 1·1 to 3·7], p=0·0177) and day
to discontinuation of
study treatment
30 (73 [78%] of 94 patients vs 66 [63%] of 105, OR 2·8
[1·4 to 5·5], p=0·0028; appendix).
Deaths 0 0 0 0 0
To examine safety and tolerability of brexanolone in the
Adverse events in three or more patients
largest possible study population available, we used a
Headache 7 (16%) 7 (18%) 6 (15%) 6 (11%) 9 (18%)
more conservative approach, including safety assess
Dizziness 1 (2%) 6 (16%) 6 (15%) 4 (8%) 5 (10%)
ments from the BRX60 study 1 group (brexanolone-ALL
Somnolence 3 (7%) 7 (18%) 2 (5%) 2 (4%) 4 (8%)
group; n=140). Across all placebo-controlled post-partum
Infusion site pain 1 (2%) 1 (3%) 4 (10%) 2 (4%) 5 (10%)
depression studies, two (1%) of 140 patients in the
Nausea 3 (7%) 1 (3%) 0 2 (4%) 5 (10%)
brexanolone-ALL group had two serious adverse events
Dry mouth 0 4 (11%) 0 1 (2%) 2 (4%)
each, compared with no patients in the placebo group,
Fatigue 0 1 (3%) 1 (2%) 2 (4%) 3 (6%)
and three (2%) of 140 patients in the brexanolone-ALL
Data are n (%). Treatment-emergent adverse events were defined as an adverse event with onset after the start of group had at least one severe adverse event compared
study drug, or any worsening of a pre-existing medical condition or adverse event with onset after the start of study with two (2%) of 107 patients in the placebo group. The
drug. Treatment-emergent adverse events were coded according to the Medical Dictionary for Regulatory Activities
proportion of patients who had at least one adverse event
version 19.1 or later. BRX60=brexanolone injection 60 µg/kg per h. BRX90=brexanolone injection 90 µg/kg per h.
was similar between groups (54 [50%] of 107 patients in
Table 3: Treatment-emergent adverse events the placebo cohorts; 70 [50%] of 140 patients in the
brexanolone-ALL group). The most common adverse
0 BRX90 (n=102) events in the brexanolone-ALL group were head
ache (n=22), dizziness (n=19), and somnolence (n=15;
Change from baseline in mean HAM-D total score (%)
Placebo (n=107)
appendix). No deaths or unexpected adverse events were
–20 reported.
–40 Discussion
* Women with post-partum depression have an increased
* * risk of morbidity and mortality, and thus additional
–60 ** * treatment options are urgently needed.53 The present
phase 3, double-blind, randomised, placebo-controlled
–80 trials of brexanolone injection in women with moderate
to severe post-partum depression HAM-D score ≥20),
End of infusion (60 h) confirm and extend the findings of our smaller
–100
0 3 6 9 12 15 18 21 24 27 30 phase 2 study,37 which showed that brexanolone injection
Time (days) reduced depressive symptoms compared with placebo.
The HAM-D is considered the gold standard assessment
Figure 3: Percentage change from baseline in mean HAM-D total score in the in clinical trials of major depression,54 including
integrated BRX90 study population
p values were calculated by two-sided t test. BRX90=brexanolone injection
pharmacotherapy trials in post-partum depression.55–57
90 µg/kg. *p<0·05 vs placebo. Consequently, as post-partum depression is considered
a subtype of major depression in the DSM-5 and the
between 24 h (51 [50%] of 101 patients in the BRX90 International Classification of Diseases, the HAM-D
cohort vs 43 [41%] of 106 patients in the placebo group; was considered the most appropriate primary endpoint.58
OR 2·1, 95% CI 1·1 to 3·8, p=0·0183) and day Across all three studies, brexanolone injection was
30 (66 [70%] of 94 patients in the BRX90 group vs associated with rapid onset of action (within 60 h) and
65 [62%] of 105 patients in the placebo group; OR 1·9, durable responses that were sustained for up to 30 days
95% CI 1·0 to 3·6, p=0·0408; appendix). Of the 70 patients after infusion. Of the patients who had a response at
in the BRX90 group who had a response at 60 h and had 60 h, 94% did not relapse at day 30.
available data at day 30, 66 (94%) did not relapse at day 30 Although this trial was not designed to investigate the
(appendix). effects of brexanolone on children and families of
In the integrated study population, the changes from patients, the potential impact of a treatment with rapid
baseline in all calculated HAM-D subscales and individual onset of action should not be underestimated. Netsi and
10 www.thelancet.com Published online August 31, 2018 http://dx.doi.org/10.1016/S0140-6736(18)31551-4
Articles
colleagues,15 examined the adverse effects of post-partum across our three placebo-controlled trials of brexanolone
depression on child development in a large observational injection in post-partum depression; however, despite
study of women and their offspring and found that the robust placebo response in studies 1 and 2, the
children of women with persistent and severe post- primary endpoint was met, with clinically meaningful
partum depression showed increased risk for behavioural and statistically significant treatment differences ob
problems by age 3·5 years, and lower mathematics served between the brexanolone injection groups and
grades and depression during adolescence. Furthermore, placebo groups. Furthermore, integrated analyses of
women with persistent post-partum depression were efficacy in the placebo-controlled study population
more likely to experience depressive symptoms lasting at revealed that the variability of the estimates was reduced
least 11 years after childbirth, prolonging the impact due to increased sample size, and additional timepoints
on both mother and child.15 Additional studies59,60 have and secondary endpoints showed statistically signifi
revealed an association with infanticide and decreased cant improvements for BRX90 relative to placebo.
use of preventive paediatric health care. Brexanolone injection has only been assessed in the
Thus, we believe the results from these two phase 3 studies context of post-partum depression, thus it is unclear
have the potential to change the treatment approach whether positive allosteric modulation of GABA might
for post-partum depression. After the 60 h infusion, be generally applicable in major depressive disorder
patients in the BRX90 groups had sig nificantly larger outside of the perinatal period, although studies of a
reductions from baseline in LS mean HAM-D total scores candidate have been announced by the study sponsor.
than patients in the placebo groups, regardless of initial The tolerability profile in these phase 3 trials is
HAM-D total score stratification. In study 1, a similar effect consistent with the GABAergic effect of brexanolone
was observed for patients in the BRX60 group. Therefore, injection. Consistent with the primary pharmacology of
our data indicate that substantial relief of post-partum brexanolone injection, which is a GABA positive allosteric
depress ive symptoms can be provided within less modulator, somnolence, dizziness, and sedation occurred
than 3 days of treatment. in approximately 30% of patients. The overall incidence
The majority of patients in all three studies did not of adverse events in the drug and placebo groups were
receive antidepressants during the study, indicating that similar. The most common adverse events in studies 1 and
brexanolone injection is a primary, rather than adjunctive, 2 and across all placebo-controlled brexanolone injection
therapy in post-partum depression. When the reduct studies were headache, dizziness, and somnolence. The
ion in depressive symptoms was examined accord incidence of dizziness and somnolence was higher in the
ing to antidepressant medication use, no differences brexanolone injection groups than the placebo groups,
were observed. Additionally, consistent with the HAM-D but these events were typically mild in severity and did
subscale and individual item analyses showing an not lead to discontinuation of treatment.
improvement in core symptoms of depression, brex One limitation of these data is that the patient pop
anolone injection had antidepressant effects. The broad ulation in these trials is representative of moderate to
antidepressant response observed in HAM-D individual severe post-partum depression patients in the USA,37
items also shows that the effect of brexanolone injection and thus the generalisability of these data to a wider
was not driven solely by improvements in sleep. The population has yet to be determined. Trial participants had
treatment effect persisted for the duration of study moderate to severe symptoms according to the HAM-D,
(until day 30) in the BRX90 and BRX60 treatment groups, but few would qualify or require an inpatient care. All
as assessed by HAM-D total scores, HAM-D remission, patients were administered brexanolone in jection in a
HAM-D response, and CGI-I response. Although mean supervised setting. The majority of patients were treated
differences in HAM-D total score from baseline were not at research centres, with some treated in other settings,
statistically significant at all timepoints after the acute such as psychiatry inpatient units. Additionally, the
60 h treatment, overall variability in depression response HAM-D results could have been affected by respondent
in patients between completion of dosing and day 30 was fatigue due to frequent administration. Although these
negligible. This maintenance of response is consistent trials assessed women for a 30-day follow-up period, the
with phase 2 data.37 effects of brexanolone injection treatment after this time
Previous studies61,62 of depression (predominantly in period are unknown, which is an important limitation of
major depressive disorder) have demonstrated highly these trials. Data on the effectiveness of current
variable responses to placebo, and large placebo effects antidepressant therapy in post-partum depression are
might contribute to the inability of some studies to show scarce, so the long-term efficacy of brexanolone injection
significant treatment effects.61,63 Higher levels of super compared with currently available oral antidepressants
vision and frequent assessment of patients in addition remains unclear.
to expectancy of outcome in clinical trial participants are These findings confirm the results of our previously
hypothesised to contribute to this variability. These reported phase 2 data and provide strong evidence for the
hypotheses can be applied to the current studies, in efficacy and safety of brexanolone injection in women with
which we observed a similar variable placebo response moderate to severe post-partum depression. The presumed
www.thelancet.com Published online August 31, 2018 http://dx.doi.org/10.1016/S0140-6736(18)31551-4 11
Articles
mechanism of action of brexanolone injection (ie, positive 13 Field T. Postpartum depression effects on early interactions,
allosteric modulation of GABAA receptors) is a novel parenting, and safety practices: a review. Infant Behav Dev 2010;
33: 1–6.
approach in the development of a therapeutic drug for 14 Murray L, Halligan SL, Cooper P. Effects of postnatal depression on
post-partum depression that has the potential to improve mother-infant interactions, and child development. In: Bremner JG,
treatment options for women with post-partum depression. Wachs TD, eds. Handbook of infant development, 2nd edn. Malden:
Wiley-Blackwell, 2010: 192–220.
Contributors 15 Netsi E, Pearson RM, Murray L, Cooper P, Craske MG, Stein A.
All authors contributed to the design of the study and writing of the Association of persistent and severe postnatal depression with child
manuscript. SM-B, SK, and HC designed the study. SM-B and SK wrote outcomes. JAMA Psychiatry 2018; 75: 247–53.
the first draft. CNE, KMD, RR, and DRR were investigators in the study. 16 Muzik M, Morelen D, Hruschak J, Rosenblum KL, Bocknek E,
HL and AJS did statistical analysis. Beeghly M. Psychopathology and parenting: an examination of
perceived and observed parenting in mothers with depression and
Declaration of interests PTSD. J Affect Disord 2017; 207: 242–50.
SM-B reports personal fees from MedScape and grants from Sage
17 Pearson RM, Evans J, Kounali D, et al. Maternal depression during
Therapeutics, Inc, awarded to the University of North Carolina (Chapel pregnancy and the postnatal period: risks and possible mechanisms
Hill, NC, USA) during the conduct of the study, and grants from Janssen for offspring depression at age 18 years. JAMA Psychiatry 2013;
outside the submitted work. HC, HL, AJS, CC, AS, are JJ are employees of 70: 1312–19.
Sage Therapeutics, Inc, and own stock or stock options in the company. 18 Stein A, Pearson RM, Goodman SH, et al. Effects of perinatal
CNE reports personal fees from Asarina Pharma, personal fees for mental disorders on the fetus and child. Lancet 2014; 384: 1800–19.
consultancy and grants from Sage Therapeutics, Inc. KMD received a 19 Goodman SH, Broth MR, Hall CM, Stowe ZN. Treatment of
grant from Sage Therapeutics, Inc, awarded to her institution. DRR postpartum depression in mothers: Secondary benefits to the
reports personal fees and has stock options in Sage Therapeutics, Inc. infants. Infant Ment Health J 2008; 29: 492–513.
SK is an employee of Sage Therapeutics, Inc., owns stocks in the 20 NICE. Antenatal and postnatal mental health: clinical management
company, and has a patent pending (SAGE-547 for Neuropsychiatric and service guidance. 2014. https://www.nice.org.uk/guidance/
Conditions). RR declares no competing interests. cg192 (accessed Aug 15, 2018).
21 O’Connor E, Rossom RC, Henninger M, Groom HC, Burda BU.
Acknowledgments
Primary care screening for and treatment of depression in pregnant
We thank members of the Sage Therapeutics, Inc, Clinical Operations and postpartum women: evidence report and systematic review for
team, including Julie Donovan, Corey Leonardi, and Mollie Baird, for the the US Preventive Services Task Force. JAMA 2016; 315: 388–406.
planning, management, and execution of the clinical trial. This study 22 Siu AL, Force USPST, Bibbins-Domingo K, et al. Screening for
was supported by Sage Therapeutics, Inc. The authors thank depression in adults: US Preventive Services Task Force
Jeffrey R Skaar and Sloka Iyengar at Boston Strategic Partners Recommendation Statement. JAMA 2016; 315: 380–87.
(supported by Sage Therapeutics, Inc), and Paul Miller at Sage 23 Byatt N, Biebel K, Friedman L, Debordes-Jackson G, Ziedonis D,
Therapeutics, Inc, for editorial support. Pbert L. Patient’s views on depression care in obstetric settings:
References how do they compare to the views of perinatal health care
1 Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, professionals? Gen Hosp Psychiatry 2013; 35: 598–604.
Swinson T. Perinatal depression: a systematic review of prevalence 24 Meltzer-Brody S. Treating perinatal depression: risks and stigma.
and incidence. Obstet Gynecol 2005; 106: 1071–83. Obstet Gynecol 2014; 124: 653–54.
2 Ko JY, Rockhill KM, Tong VT, Morrow B, Farr SL. Trends in 25 Di Florio A, Putnam K, Altemus M, et al. The impact of education,
postpartum depressive symptoms-27 States, 2004, 2008, and 2012. country, race and ethnicity on the self-report of postpartum
MMWR Morb Mortal Wkly Rep 2017; 66: 153–58. depression using the Edinburgh Postnatal Depression Scale.
3 Howard LM, Molyneaux E, Dennis CL, Rochat T, Stein A, Psychol Med 2017; 47: 787–99.
Milgrom J. Non-psychotic mental disorders in the perinatal period. 26 Molyneaux E, Howard LM, McGeown HR, Karia AM, Trevillion K.
Lancet 2014; 384: 1775–88. Antidepressant treatment for postnatal depression.
4 Earls MF. Incorporating recognition and management of perinatal Cochrane Database Syst Rev 2014; 9: CD002018.
and postpartum depression into pediatric practice. Pediatrics 2010; 27 Molyneaux E, Telesia LA, Henshaw C, Boath E, Bradley E,
126: 1032–39. Howard LM. Antidepressants for preventing postnatal depression.
5 Fellmeth G, Fazel M, Plugge E. Migration and perinatal mental Cochrane Database Syst Rev 2018; 4: CD004363.
health in women from low- and middle-income countries: 28 Cox EQ, Sowa NA, Meltzer-Brody SE, Gaynes BN. The perinatal
a systematic review and meta-analysis. BJOG 2017; 124: 742–52. depression treatment cascade: baby steps toward improving
6 Postpartum Depression: Action Towards Causes and Treatment outcomes. J Clin Psychiatry 2016; 77: 1189–200.
(PACT) Consotrium. Heterogeneity of postpartum depression: 29 Melón LC, Hooper A, Yang X, Moss SJ, Maguire J. Inability to
a latent class analysis. Lancet Psychiatry 2015; 2: 59–67. suppress the stress-induced activation of the HPA axis during the
7 Bauer A, Parsonage M, Knapp M, Lemmi V, Adelaja B. The costs of peripartum period engenders deficits in postpartum behaviors in
perinatal mental health problems. London: London School of mice. Psychoneuroendocrinology 2017; 90: 182–93.
Economics, 2014. https://www.nwcscnsenate.nhs.uk/files/3914/7030/ 30 Maguire J, Mody I. GABA(A)R plasticity during pregnancy:
1256/Costs_of_perinatal_mh.pdf (accessed Aug 15, 2018). relevance to postpartum depression. Neuron 2008; 59: 207–13.
8 Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide 31 Mody I, Maguire J. The reciprocal regulation of stress hormones
mortality in mental disorders: a meta-review. World Psychiatry 2014; and GABA(A) receptors. Front Cell Neurosci 2011; 6: 4.
13: 153–60. 32 Meltzer-Brody S, Howard LM, Bergink V, et al. Postpartum
9 Johannsen BM, Larsen JT, Laursen TM, Bergink V, Meltzer-Brody S, psychiatric disorders. Nat Rev Dis Primers 2018; 4: 18022.
Munk-Olsen T. All-cause mortality in women with severe 33 Majewska MD, Harrison NL, Schwartz RD, Barker JL, Paul SM.
postpartum psychiatric disorders. Am J Psychiatry 2016; 173: 635–42. Steroid hormone metabolites are barbiturate-like modulators of the
10 Parsons CE, Young KS, Rochat TJ, Kringelbach ML, Stein A. Postnatal GABA receptor. Science 1986; 232: 1004–07.
depression and its effects on child development: a review of evidence 34 Osborne LM, Gispen F, Sanyal A, Yenokyan G, Meilman S, Payne JL.
from low- and middle-income countries. Br Med Bull 2012; 101: 57–79. Lower allopregnanolone during pregnancy predicts postpartum
11 Szegda K, Markenson G, Bertone-Johnson ER, Chasan-Taber L. depression: an exploratory study. Psychoneuroendocrinology 2017;
Depression during pregnancy: a risk factor for adverse neonatal 79: 116–21.
outcomes? A critical review of the literature. 35 Paul SM, Purdy RH. Neuroactive steroids. FASEB J 1992; 6: 2311–22.
J Matern Fetal Neonatal Med 2014; 27: 960–67. 36 Luisi S, Petraglia F, Benedetto C, et al. Serum allopregnanolone
12 Accortt EE, Cheadle AC, Dunkel Schetter C. Prenatal depression levels in pregnant women: changes during pregnancy, at delivery,
and adverse birth outcomes: an updated systematic review. and in hypertensive patients. J Clin Endocrinol Metab 2000;
Matern Child Health J 2015; 19: 1306–37. 85: 2429–33.
12 www.thelancet.com Published online August 31, 2018 http://dx.doi.org/10.1016/S0140-6736(18)31551-4
Articles
37 Kanes S, Colquhoun H, Gunduz-Bruce H, et al. Brexanolone 51 Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for
(SAGE-547 injection) in post-partum depression: a randomised assessing generalized anxiety disorder: the GAD-7. Arch Intern Med
controlled trial. Lancet 2017; 390: 480–89. 2006; 166: 1092–97.
38 First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical 52 Posner K, Brown GK, Stanley B, et al. The Columbia-Suicide
interview for DSM-IV axis I disorders, clinician version (SCID-CV). severity rating scale: initial validity and internal consistency
Washington, DC: American Psychiatric Press, 1996. findings from three multisite studies with adolescents and adults.
39 Hamilton M. A rating scale for depression. Am J Psychiatry 2011; 168: 1266–77.
J Neurol Neurosurg Psychiatry 1960; 23: 56–62. 53 Alexander JL. Quest for timely detection and treatment of women
40 Milgrom J, Gemmill AW, Bilszta JL, et al. Antenatal risk factors for with depression. J Manag Care Pharm 2007; 13 (suppl 9A): S3–11.
postnatal depression: a large prospective study. J Affect Disord 2008; 54 Khan A, Khan SR, Shankles EB, Polissar NL. Relative sensitivity of
108: 147–57. the Montgomery-Asberg Depression rating scale, the Hamilton
41 Serati M, Redaelli M, Buoli M, Altamura AC. Perinatal major Depression rating scale and the Clinical Global Impressions rating
depression biomarkers: a systematic review. J Affect Disord 2016; scale in antidepressant clinical trials. Int Clin Psychopharmacol 2002;
193: 391–404. 17: 281–85.
42 Kanes SJ, Colquhoun H, Doherty J, et al. Open-label, 55 Hantsoo L, Ward-O’Brien D, Czarkowski KA, Gueorguieva R,
proof-of-concept study of brexanolone in the treatment of severe Price LH, Epperson CN. A randomized, placebo-controlled,
postpartum depression. Hum Psychopharmacol 2017; 32: e2576. double-blind trial of sertraline for postpartum depression.
43 Guy W. ECDEU assessment manual for psychopharmacology. Psychopharmacology 2014; 231: 939–48.
Rockville, MD: US Department of Health, Education, and Welfare, 56 Kim DR, Epperson CN, Weiss AR, Wisner KL. Pharmacotherapy of
Public Health Service, Alcohol, Drug Abuse, and Mental Health postpartum depression: an update. Expert Opin Pharmacother 2014;
Administration, National Institute of Mental Health, 15: 1223–34.
Psychopharmacology Research Branch, Division of Extramural 57 Wisner KL, Hanusa BH, Perel JM, et al. Postpartum depression:
Research Programs, 1976. a randomized trial of sertraline versus nortriptyline.
44 Montgomery SA, Asberg M. A new depression scale designed to be J Clin Psychopharmacol 2006; 26: 353–60.
sensitive to change. Br J Psychiatry 1979; 134: 382–89. 58 American Psychiatric Association. Diagnostic and statistical manual
45 Bech P, Allerup P, Gram LF, et al. The Hamilton depression scale. of mental disorders: DSM-5, 5th edn. Washington, DC: American
Evaluation of objectivity using logistic models. Psychiatric Association, 2013.
Acta Psychiatr Scand 1981; 63: 290–99. 59 Flynn HA, Davis M, Marcus SM, Cunningham R, Blow FC.
46 Gibbons RD, Clark DC, Kupfer DJ. Exactly what does the Rates of maternal depression in pediatric emergency department
Hamilton depression rating scale measure? J Psychiatr Res 1993; and relationship to child service utilization.
27: 259–73. Gen Hosp Psychiatry 2004; 26: 316–22.
47 Pancheri P, Picardi A, Pasquini M, Gaetano P, Biondi M. 60 Kauppi A, Kumpulainen K, Vanamo T, Merikanto J, Karkola K.
Psychopathological dimensions of depression: a factor study of the Maternal depression and filicide-case study of ten mothers.
17-item Hamilton depression rating scale in unipolar depressed Arch Womens Ment Health 2008; 11: 201–06.
outpatients. J Affect Disord 2002; 68: 41–47. 61 Walsh BT, Seidman SN, Sysko R, Gould M. Placebo response in
48 Maier W, Philipp M. Improving the assessment of severity of studies of major depression: variable, substantial, and growing.
depressive states: a reduction of the Hamilton Depression Scale. JAMA 2002; 287: 1840–47.
Pharmacopsychiatry 1985; 18: 114–15. 62 Khan A, Fahl Mar K, Faucett J, Khan Schilling S, Brown WA.
49 Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Has the rising placebo response impacted antidepressant clinical
Development of the 10-item Edinburgh Postnatal Depression Scale. trial outcome? Data from the US Food and Drug Administration
Br J Psychiatry 1987; 150: 782–86. 1987–2013. World Psychiatry 2017; 16: 181–92.
50 Spitzer RL, Kroenke K, Williams JB. Validation and utility of a 63 Undurraga J, Baldessarini RJ. Randomized, placebo-controlled
self-report version of PRIME-MD: the PHQ primary care study. trials of antidepressants for acute major depression: thirty-year
Primary Care Evaluation of Mental Disorders. Patient Health meta-analytic review. Neuropsychopharmacology 2012; 37: 851–64.
Questionnaire. JAMA 1999; 282: 1737–44.
www.thelancet.com Published online August 31, 2018 http://dx.doi.org/10.1016/S0140-6736(18)31551-4 13
You might also like
- The Massachusetts General Hospital Guide to Depression: New Treatment Insights and OptionsFrom EverandThe Massachusetts General Hospital Guide to Depression: New Treatment Insights and OptionsBenjamin G. ShaperoNo ratings yet
- Cuma Abstraknya Aja: TTG Risperidone: Stroke Therapy TreatmentsDocument6 pagesCuma Abstraknya Aja: TTG Risperidone: Stroke Therapy TreatmentsChandz ChanDra ErryandariNo ratings yet
- Treatment–Refractory Schizophrenia: A Clinical ConundrumFrom EverandTreatment–Refractory Schizophrenia: A Clinical ConundrumPeter F. BuckleyNo ratings yet
- CorrespondenceDocument3 pagesCorrespondenceklysmanu93No ratings yet
- Single-Dose Synthetic Psilocybin With Psychotherapy For Treatment-Resistant Bipolar Type II Major Depressive EpisodesDocument8 pagesSingle-Dose Synthetic Psilocybin With Psychotherapy For Treatment-Resistant Bipolar Type II Major Depressive EpisodesPepa PIGNo ratings yet
- Clozapine and Haloperidol in ModeratelyDocument8 pagesClozapine and Haloperidol in Moderatelyrinaldiapt08No ratings yet
- Effects of Risperidone and Olanzapine Dose Reduction On Cognitive Function in Stable Patients With SchizophreniaDocument6 pagesEffects of Risperidone and Olanzapine Dose Reduction On Cognitive Function in Stable Patients With Schizophreniawen zhangNo ratings yet
- AsenapineTransdermalPatchVsPlaceboPosterAbstract CITROME BiolPsych2019Document1 pageAsenapineTransdermalPatchVsPlaceboPosterAbstract CITROME BiolPsych2019Leslie CitromeNo ratings yet
- Low-Dose Quetiapine in Schizophrenia: Meta-Analysis High-: The Psychiatrist OnlineDocument5 pagesLow-Dose Quetiapine in Schizophrenia: Meta-Analysis High-: The Psychiatrist OnlineMichael CoxNo ratings yet
- A Placebo-Controlled Trial of Phenelzine, Cognitive Behavioral Group Therapy, and Their Combination For Social Anxiety DisorderDocument10 pagesA Placebo-Controlled Trial of Phenelzine, Cognitive Behavioral Group Therapy, and Their Combination For Social Anxiety DisorderEmaa AmooraNo ratings yet
- Appi Ajp 2014 13121625Document9 pagesAppi Ajp 2014 13121625Orion OriNo ratings yet
- Trial of Psilocybin Versus Escitalopram For Depression: Original ArticleDocument10 pagesTrial of Psilocybin Versus Escitalopram For Depression: Original ArticleCristina Duran GarcíaNo ratings yet
- Ajp 156 5 702Document8 pagesAjp 156 5 7029 PsychologyNo ratings yet
- Muscarinic Cholinergic Receptor Agonist and Peripheral Antagonist For Schizophrenia (2021)Document10 pagesMuscarinic Cholinergic Receptor Agonist and Peripheral Antagonist For Schizophrenia (2021)ShadeLRKNo ratings yet
- Prevention of Postpartum Depression: A Pilot Randomized Clinical TrialDocument3 pagesPrevention of Postpartum Depression: A Pilot Randomized Clinical Trialportgas aceNo ratings yet
- Reduction of PTSD Symptoms With Pre-Reactivation Propranolol Therapy: A Randomized Controlled TrialDocument7 pagesReduction of PTSD Symptoms With Pre-Reactivation Propranolol Therapy: A Randomized Controlled TrialKateNo ratings yet
- Paroxetine Personality 2Document9 pagesParoxetine Personality 2PrissTinkNo ratings yet
- A Selective Summary of Psychopharmacology Research Published in First Half of 2017Document3 pagesA Selective Summary of Psychopharmacology Research Published in First Half of 2017gion.nandNo ratings yet
- Clonazepam 2 PDFDocument8 pagesClonazepam 2 PDFKatterine RebolledoNo ratings yet
- Pitman 2002 Biological-PsychiatryDocument4 pagesPitman 2002 Biological-PsychiatryQwerty QwertyNo ratings yet
- Efecto de Dextrometorfano - Bupropion en Ttno Depresivo MayorDocument10 pagesEfecto de Dextrometorfano - Bupropion en Ttno Depresivo MayorLina MariaNo ratings yet
- Randomized, Placebo-Controlled Trial Pregabalin For The Treatment of Postherpetic Neuralgia: ADocument12 pagesRandomized, Placebo-Controlled Trial Pregabalin For The Treatment of Postherpetic Neuralgia: AadityaNo ratings yet
- PANDA SertralineDocument12 pagesPANDA SertralinenomansnNo ratings yet
- Kane1988 PDFDocument8 pagesKane1988 PDFRavi KumarNo ratings yet
- Serum Interleukin-6 Is A Predictive Biomarker For Ketamine's Antidepressant Effect in Treatment-Resistant Patients With Major DepressionDocument3 pagesSerum Interleukin-6 Is A Predictive Biomarker For Ketamine's Antidepressant Effect in Treatment-Resistant Patients With Major DepressionAlex AlexNo ratings yet
- Rajiv P. Sharma Et Al - CSF Neurotensin Concentrations and Antipsychotic Treatment in Schizophrenia and Schizoaffective DisorderDocument3 pagesRajiv P. Sharma Et Al - CSF Neurotensin Concentrations and Antipsychotic Treatment in Schizophrenia and Schizoaffective DisorderLonkesNo ratings yet
- Changes in Brain Function (Quantitative EEG Cordance) During Placebo Lead-In and Treatment Outcomes in Clinical Trials For Major DepressionDocument7 pagesChanges in Brain Function (Quantitative EEG Cordance) During Placebo Lead-In and Treatment Outcomes in Clinical Trials For Major DepressiondebdotnetNo ratings yet
- PIIS2215036618300968Document13 pagesPIIS2215036618300968zuhrul_baladNo ratings yet
- Escitalopram in Post Traumatic Stress DisorderDocument11 pagesEscitalopram in Post Traumatic Stress DisorderVivekNo ratings yet
- Britishjournalofpsychiatry BRITISHJOURNALOFPSYCHIATRY (2001), 179,514 518 (2 0 0 1), 1 7 9, 5 1 4 5 1 8Document6 pagesBritishjournalofpsychiatry BRITISHJOURNALOFPSYCHIATRY (2001), 179,514 518 (2 0 0 1), 1 7 9, 5 1 4 5 1 8Imam FirdausNo ratings yet
- A Double-Blind, Placebo-Controlled Study of Quetiapine and Paroxetine As Monotherapy in Adults With Bipolar Depression (EMBOLDEN II)Document12 pagesA Double-Blind, Placebo-Controlled Study of Quetiapine and Paroxetine As Monotherapy in Adults With Bipolar Depression (EMBOLDEN II)HugoMattosNo ratings yet
- Short-Term and Long-Term Evaluation of Selective Serotonin Reuptake Inhibitors in The Treatment of Panic Disorder: Fluoxetine Vs CitalopramDocument6 pagesShort-Term and Long-Term Evaluation of Selective Serotonin Reuptake Inhibitors in The Treatment of Panic Disorder: Fluoxetine Vs CitalopramBakhita MaryamNo ratings yet
- Clozapine: SchizophrenicDocument8 pagesClozapine: SchizophrenicVictoria FellowsNo ratings yet
- Artigo InglesDocument11 pagesArtigo InglesEllen AndradeNo ratings yet
- Quetiapine As An AdjunctiveDocument5 pagesQuetiapine As An AdjunctivemoniaNo ratings yet
- Pharmacotherapy Relapse Prevention in Body Dysmorphic Disorder: A Double-Blind, Placebo-Controlled TrialDocument9 pagesPharmacotherapy Relapse Prevention in Body Dysmorphic Disorder: A Double-Blind, Placebo-Controlled Trialyeremias setyawanNo ratings yet
- Clozapine in Treatment of Schizophrenia: V. Burtea P. Ifteni A Teodorescu L. RogozeaDocument6 pagesClozapine in Treatment of Schizophrenia: V. Burtea P. Ifteni A Teodorescu L. RogozeaReza Badruun Syahrul HakimNo ratings yet
- Lap Chak 2003Document6 pagesLap Chak 2003Zahra NisaNo ratings yet
- Reprodutibilidade Da Eficácia Do Escitalopram em Pacientes Com Depressão Maior Anteriormente Remitidos Com EscitalopramDocument2 pagesReprodutibilidade Da Eficácia Do Escitalopram em Pacientes Com Depressão Maior Anteriormente Remitidos Com EscitalopramIratanFernandesNo ratings yet
- TCC Con Fase de Continuación para DepresiónDocument15 pagesTCC Con Fase de Continuación para DepresiónGuillermo Van LooNo ratings yet
- Bevilaqua-Grossi Et Al 2016 Arch Phys Med RehabilDocument9 pagesBevilaqua-Grossi Et Al 2016 Arch Phys Med Rehabilcris.endo.ceNo ratings yet
- Assessing The Effectiveness of Pharmacotherapy ForDocument1 pageAssessing The Effectiveness of Pharmacotherapy ForArthur AlvesNo ratings yet
- The Role of Psychedelics in Palliative Care Reconsidered: A Case For PsilocybinDocument3 pagesThe Role of Psychedelics in Palliative Care Reconsidered: A Case For PsilocybinJosé Carlos Solís SuárezNo ratings yet
- JURNAL ASLI FarmakoterapiDocument4 pagesJURNAL ASLI FarmakoterapiWulandiraNo ratings yet
- New England Journal Medicine: The ofDocument12 pagesNew England Journal Medicine: The ofwardahNo ratings yet
- Hongos Contra La MigrañaDocument10 pagesHongos Contra La MigrañaRamón Vargas CortezNo ratings yet
- A Randomized, Double-Blind, Placebo-Controlled Study of Citalopram in Adolescents With Major Depressive Disorder - Von Knorring 2006Document5 pagesA Randomized, Double-Blind, Placebo-Controlled Study of Citalopram in Adolescents With Major Depressive Disorder - Von Knorring 2006Julio JuarezNo ratings yet
- Effect of Duloxetine On Pain Function and Quality of Life Among Patients With Chemotherapy-Induced Painful Peripheral NeuropathyDocument9 pagesEffect of Duloxetine On Pain Function and Quality of Life Among Patients With Chemotherapy-Induced Painful Peripheral NeuropathypokNo ratings yet
- Aripiprazol - Augmentare in Depresia RezistentaDocument9 pagesAripiprazol - Augmentare in Depresia RezistentaRobert MovileanuNo ratings yet
- Freudenreich 2002Document8 pagesFreudenreich 2002citra kurnia pratiwiNo ratings yet
- ZiprasidoneHaloperidolAgitationlPostHocAbstractICOSR CITROME SchizBull2005Document2 pagesZiprasidoneHaloperidolAgitationlPostHocAbstractICOSR CITROME SchizBull2005Leslie CitromeNo ratings yet
- CurryDocument8 pagesCurryuricomasNo ratings yet
- What Does The PANSS Mean?Document8 pagesWhat Does The PANSS Mean?Farin MauliaNo ratings yet
- Tohen 2003Document9 pagesTohen 2003Francisco VillalonNo ratings yet
- Cannabis and ShizoDocument2 pagesCannabis and ShizoFarah MuthiaNo ratings yet
- Journal of Affective DisordersDocument8 pagesJournal of Affective DisordersDeni SetyawanNo ratings yet
- Paper 2Document5 pagesPaper 2fernanda cornejoNo ratings yet
- Comparative Efficacy and Tolerability of 32 Oral Antipsychotics For The Acute Treatment of Adults With Multi-Episode Schizophrenia PDFDocument13 pagesComparative Efficacy and Tolerability of 32 Oral Antipsychotics For The Acute Treatment of Adults With Multi-Episode Schizophrenia PDFfrancesca_valdiviaNo ratings yet
- Nejmoa 2300184Document11 pagesNejmoa 2300184Hector RivasNo ratings yet
- Effect of Music Therapy Derived From The Five Elements in Traditional Chinese Medicine On Post-Stroke DepressionDocument6 pagesEffect of Music Therapy Derived From The Five Elements in Traditional Chinese Medicine On Post-Stroke DepressionwindapuspitasalimNo ratings yet
- PDAC - DSaRM 11022018 FDABackgrounderDocument33 pagesPDAC - DSaRM 11022018 FDABackgrounderBianca AlinaNo ratings yet
- Wondering How To Offer Brexanolone For Postpartum Depression - Here's How We're Piloting It - Consult QDDocument3 pagesWondering How To Offer Brexanolone For Postpartum Depression - Here's How We're Piloting It - Consult QDBianca AlinaNo ratings yet
- Brexanolone Infusion Rapidly Relieves Postpartum Depression - Psychiatry & Behavioral Health Learning NetworkDocument3 pagesBrexanolone Infusion Rapidly Relieves Postpartum Depression - Psychiatry & Behavioral Health Learning NetworkBianca AlinaNo ratings yet
- Neurobiology of Stress 12 (2020) 100212Document8 pagesNeurobiology of Stress 12 (2020) 100212Bianca AlinaNo ratings yet
- Articles: BackgroundDocument13 pagesArticles: BackgroundBianca AlinaNo ratings yet
- Read MeDocument1 pageRead Meanon_637749750No ratings yet
- Psychiatry Research: Review ArticleDocument7 pagesPsychiatry Research: Review ArticleBianca AlinaNo ratings yet
- Allopregnanolone Derivatives with Increased SolubilityDocument7 pagesAllopregnanolone Derivatives with Increased SolubilityBianca AlinaNo ratings yet
- ConfigureDocument1 pageConfigureBianca AlinaNo ratings yet
- Install Program - Easy 3 Step GuideDocument1 pageInstall Program - Easy 3 Step GuideBianca AlinaNo ratings yet
- Adobe Photoshop CC Legal NoticesDocument25 pagesAdobe Photoshop CC Legal NoticesRichard BirchNo ratings yet
- SerialsDocument1 pageSerialsBianca AlinaNo ratings yet
- Installation InstructionsDocument1 pageInstallation InstructionsBianca AlinaNo ratings yet
- Change LogDocument8 pagesChange LogNguyễn Võ Ngọc ThạchNo ratings yet
- Cubic Spline Tutorial v3Document6 pagesCubic Spline Tutorial v3Praveen SrivastavaNo ratings yet
- Nitobond SBR (Latex)Document4 pagesNitobond SBR (Latex)Samarakoon Banda100% (1)
- 1.1 Enterprise AssessmentDocument1 page1.1 Enterprise AssessmentGermanRobertoFongNo ratings yet
- FacebookH Cking 1 3 (SFILEDocument10 pagesFacebookH Cking 1 3 (SFILEFitra AkbarNo ratings yet
- Download Zinc Surfaces A Guide To Alloys Finishes Fabrication And Maintenance In Architecture And Art 1St Edition L William Zahner all chapterDocument68 pagesDownload Zinc Surfaces A Guide To Alloys Finishes Fabrication And Maintenance In Architecture And Art 1St Edition L William Zahner all chapterdevin.brown498100% (7)
- A Primer On Financial Time Series AnalysisDocument93 pagesA Primer On Financial Time Series AnalysisKM AgritechNo ratings yet
- NABARD Dairy Farming Project - PDF - Agriculture - Loans PDFDocument7 pagesNABARD Dairy Farming Project - PDF - Agriculture - Loans PDFshiba prasad panjaNo ratings yet
- 01 A Brief Introduction To Cloud ComputingDocument25 pages01 A Brief Introduction To Cloud ComputingfirasibraheemNo ratings yet
- DataSheet IMA18-10BE1ZC0K 6041793 enDocument8 pagesDataSheet IMA18-10BE1ZC0K 6041793 enRuben Hernandez TrejoNo ratings yet
- Tutorial Task 3 - A C P I WK 2Document8 pagesTutorial Task 3 - A C P I WK 2BM70621 Alya Zahirah Binti AziziNo ratings yet
- Sunera Best Practices For Remediating SoDsDocument7 pagesSunera Best Practices For Remediating SoDssura anil reddyNo ratings yet
- Spare Parts List: WarningDocument5 pagesSpare Parts List: WarningÃbdøū Èqúípmeńť MédîcàlNo ratings yet
- CD 1 - Screening & DiagnosisDocument27 pagesCD 1 - Screening & DiagnosiskhairulfatinNo ratings yet
- Inventario de Autoestima de Coopersmith PDFDocument10 pagesInventario de Autoestima de Coopersmith PDFNancy BerduzcoNo ratings yet
- ForwardMails PDFDocument7 pagesForwardMails PDFJesús Ramón Romero EusebioNo ratings yet
- Ncm110nif Midterm Laboratory NotesDocument12 pagesNcm110nif Midterm Laboratory NotesMicah jay MalvasNo ratings yet
- Summarised Maths Notes (Neilab Osman)Document37 pagesSummarised Maths Notes (Neilab Osman)dubravko_akmacicNo ratings yet
- Cheat Codes SkyrimDocument13 pagesCheat Codes SkyrimDerry RahmaNo ratings yet
- Little ThingsDocument3 pagesLittle ThingszwartwerkerijNo ratings yet
- PathFit 1 (Lessons)Document10 pagesPathFit 1 (Lessons)Patawaran, Myka R.No ratings yet
- Power System Analysis and Design, SI EditionDocument5 pagesPower System Analysis and Design, SI EditionAkimeNo ratings yet
- FMAI - Ch04 - Stock MarketDocument105 pagesFMAI - Ch04 - Stock Marketngoc duongNo ratings yet
- AP Standard Data All PDFDocument963 pagesAP Standard Data All PDFSiva Kumar100% (1)
- 2008-14-03Document6 pages2008-14-03RAMON CALDERONNo ratings yet
- CAFA Open House HighlightsDocument1 pageCAFA Open House HighlightsDaniel LaiNo ratings yet
- Quantification Skills in The Construction IndustryDocument34 pagesQuantification Skills in The Construction IndustryBRGRNo ratings yet
- AlternatorDocument3 pagesAlternatorVatsal PatelNo ratings yet
- LINDA ALOYSIUS Unit 6 Seminar Information 2015-16 - Seminar 4 Readings PDFDocument2 pagesLINDA ALOYSIUS Unit 6 Seminar Information 2015-16 - Seminar 4 Readings PDFBence MagyarlakiNo ratings yet
- DSC analysis of hair denaturationDocument2 pagesDSC analysis of hair denaturationDiosel Rezia PrazaNo ratings yet
- Sipmos Power Transistor: BUZ 104LDocument10 pagesSipmos Power Transistor: BUZ 104LAlexsander MeloNo ratings yet
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- My Grandmother's Hands: Racialized Trauma and the Pathway to Mending Our Hearts and BodiesFrom EverandMy Grandmother's Hands: Racialized Trauma and the Pathway to Mending Our Hearts and BodiesRating: 5 out of 5 stars5/5 (70)
- An Autobiography of Trauma: A Healing JourneyFrom EverandAn Autobiography of Trauma: A Healing JourneyRating: 5 out of 5 stars5/5 (2)
- BORDERLINE PERSONALITY DISORDER: Help Yourself and Help Others. Articulate Guide to BPD. Tools and Techniques to Control Emotions, Anger, and Mood Swings. Save All Your Relationships and Yourself. NEW VERSIONFrom EverandBORDERLINE PERSONALITY DISORDER: Help Yourself and Help Others. Articulate Guide to BPD. Tools and Techniques to Control Emotions, Anger, and Mood Swings. Save All Your Relationships and Yourself. NEW VERSIONRating: 4.5 out of 5 stars4.5/5 (24)
- The Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a TimeFrom EverandThe Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a TimeRating: 4.5 out of 5 stars4.5/5 (140)
- Rewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and WorryFrom EverandRewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and WorryRating: 4.5 out of 5 stars4.5/5 (157)
- Rapid Weight Loss Hypnosis: How to Lose Weight with Self-Hypnosis, Positive Affirmations, Guided Meditations, and Hypnotherapy to Stop Emotional Eating, Food Addiction, Binge Eating and MoreFrom EverandRapid Weight Loss Hypnosis: How to Lose Weight with Self-Hypnosis, Positive Affirmations, Guided Meditations, and Hypnotherapy to Stop Emotional Eating, Food Addiction, Binge Eating and MoreRating: 5 out of 5 stars5/5 (17)
- Feel the Fear… and Do It Anyway: Dynamic Techniques for Turning Fear, Indecision, and Anger into Power, Action, and LoveFrom EverandFeel the Fear… and Do It Anyway: Dynamic Techniques for Turning Fear, Indecision, and Anger into Power, Action, and LoveRating: 4 out of 5 stars4/5 (249)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisFrom EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (9)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsFrom EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsRating: 4.5 out of 5 stars4.5/5 (38)
- Summary: No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems Model by Richard C. Schwartz PhD & Alanis Morissette: Key Takeaways, Summary & AnalysisFrom EverandSummary: No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems Model by Richard C. Schwartz PhD & Alanis Morissette: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (5)
- The Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control & Becoming WholeFrom EverandThe Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control & Becoming WholeRating: 4.5 out of 5 stars4.5/5 (49)
- Binaural Beats: Activation of pineal gland – Stress reduction – Meditation – Brainwave entrainment – Deep relaxationFrom EverandBinaural Beats: Activation of pineal gland – Stress reduction – Meditation – Brainwave entrainment – Deep relaxationRating: 5 out of 5 stars5/5 (9)
- Embrace Your Weird: Face Your Fears and Unleash CreativityFrom EverandEmbrace Your Weird: Face Your Fears and Unleash CreativityRating: 4.5 out of 5 stars4.5/5 (124)
- Summary of The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk MDFrom EverandSummary of The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk MDRating: 4.5 out of 5 stars4.5/5 (167)
- The Autoimmune Cure: Healing the Trauma and Other Triggers That Have Turned Your Body Against YouFrom EverandThe Autoimmune Cure: Healing the Trauma and Other Triggers That Have Turned Your Body Against YouNo ratings yet
- Winning the War in Your Mind: Change Your Thinking, Change Your LifeFrom EverandWinning the War in Your Mind: Change Your Thinking, Change Your LifeRating: 5 out of 5 stars5/5 (558)
- Somatic Therapy Workbook: A Step-by-Step Guide to Experiencing Greater Mind-Body ConnectionFrom EverandSomatic Therapy Workbook: A Step-by-Step Guide to Experiencing Greater Mind-Body ConnectionNo ratings yet
- Don't Panic: Taking Control of Anxiety AttacksFrom EverandDon't Panic: Taking Control of Anxiety AttacksRating: 4 out of 5 stars4/5 (12)
- Heal the Body, Heal the Mind: A Somatic Approach to Moving Beyond TraumaFrom EverandHeal the Body, Heal the Mind: A Somatic Approach to Moving Beyond TraumaRating: 4.5 out of 5 stars4.5/5 (56)
- Overcoming Unwanted Intrusive Thoughts: A CBT-Based Guide to Getting Over Frightening, Obsessive, or Disturbing ThoughtsFrom EverandOvercoming Unwanted Intrusive Thoughts: A CBT-Based Guide to Getting Over Frightening, Obsessive, or Disturbing ThoughtsRating: 4.5 out of 5 stars4.5/5 (48)
- Vagus Nerve: A Complete Self Help Guide to Stimulate and Activate Vagal Tone — A Self Healing Exercises to Reduce Chronic Illness, PTSD, Anxiety, Inflammation, Depression, Trauma, and AngerFrom EverandVagus Nerve: A Complete Self Help Guide to Stimulate and Activate Vagal Tone — A Self Healing Exercises to Reduce Chronic Illness, PTSD, Anxiety, Inflammation, Depression, Trauma, and AngerRating: 4.5 out of 5 stars4.5/5 (16)
- The Anatomy of Loneliness: How to Find Your Way Back to ConnectionFrom EverandThe Anatomy of Loneliness: How to Find Your Way Back to ConnectionRating: 4.5 out of 5 stars4.5/5 (162)
- The Secrets of Vagus Nerve Stimulation: 18 Proven, Science-Backed Exercises and Methods to Activate Your Vagal Tone and Heal from Inflammation, Chronic Stress, Anxiety, Epilepsy, and Depression.From EverandThe Secrets of Vagus Nerve Stimulation: 18 Proven, Science-Backed Exercises and Methods to Activate Your Vagal Tone and Heal from Inflammation, Chronic Stress, Anxiety, Epilepsy, and Depression.Rating: 5 out of 5 stars5/5 (14)
- Triggers: How We Can Stop Reacting and Start HealingFrom EverandTriggers: How We Can Stop Reacting and Start HealingRating: 5 out of 5 stars5/5 (58)