Professional Documents
Culture Documents
Suture Materials in Dentistry
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Suture Materials in Dentistry
Copyright:
Available Formats
Volume 5, Issue 4, April – 2020 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165
Suture Materials in Dentistry
Dr. Vamsee Krishna N1,5*, Dr. Jasmitha C2, Dr. Madhuri Nadhamuni3,5, Dr. Dattaprasad S4,5
1
Associate Professor, Department of Conservative Dentistry & Endodontics.
2
Under graduate, CKS Theja Institute of Dental Sciences & Research, Tirupati,
Andhra Pradesh, India.
3
Senior Lecturer, Department of Orthodontics & Dentofacial Orthopaedics.
4
Professor & Head, Department of Conservative Dentistry & Endodontics.
5
CKS Theja Institute of Dental Sciences & Research, Tirupati, Andhra Pradesh, India.
*Corresponding author:
Dr. Vamsee Krishna. N, M.D.S,
Associate Professor, Department of Conservative Dentistry & Endodontics,
CKS Theja Institute of Dental Sciences & Research, Tirupati, Andhra Pradesh, India.
Abstract:- Soft tissue appearance after periradicular clinicians in understanding the availability of different
surgery plays a major role in the aesthetics. The suture suture materials, alternatives to sutures and their role in
material used also influence the wound closure, soft tissue healing of periapical surgery.
hemostasis and healing of wound along with the surgical
and suturing technique used. It is essential for The Ideal properties of Suture are [4]:
professional to be aware of the properties of the suture It can be utilized in any operation.
material and its interaction with the surrounding It can be handled easily and comfortably.
tissues. This article gives an overview regarding current Minimal tissue reaction.
and new advances in Suture materials and alternatives High breaking strength.
to sutures in dentistry. High knot security.
It does not cut, tear or shrink the tissue.
Keywords:- Periradicular Surgery; Soft Tissue Healing; It is non-allergenic, non-carcinogenic
Sutures.
It is absorbed predictably with no tissue reaction
I. INTRODUCTION
Sutures can be classified according to several
parameters like source material (natural or synthetic),
An endodontically-treated tooth with
structure (Monofilament or Multifilament), degradation
persistent periapical lesion is managed by apical surgery.
(absorbable or non-absorbable), tissue reaction (Reactive or
The primary goal of apical surgery is elimination of
Not reactive), and coating (Coated or Uncoated). The
bacteria and its by-products from the periapical region with
decision of using which type of suture material depends of
subsequent healing of existent apical periodontitis. The
a series of factors. They are the time needed for the wound
prognosis of apical surgery is based on the systemic
to heal, the issue of temporary or permanent need of the
condition of the patient, tooth condition, and soft tissue
suture to ensure mechanical support, the condition of the
handling during surgery [1].
wound and tissue response to the material [5]. Sizes of the
suture are given by a number representing their diameter.
Oral wound healing varies with general wound
They range from 1-0 to 12-0, the higher the first number
healing in two ways. Primarily, wound in the oral cavity
(Ex: ‘12’ in ‘12-0’), the finer is the suture material. The
cannot be immobilized due to the functional movements of
selected size of suture material should match the tissue into
oral tissues. Secondly, oral cavity is colonized by different
which it is implanted [6].
bacteria which causes wound infection [2]. Endodontic
microsurgery alone may not accelerate healing, but through
Types of Suture materials [6]:
accurate preoperative treatment planning, proper flap
Natural absorbable monofilament sutures: Catgut,
design and soft tissue handling during procedure, perfect
Collagen
tissue adaptation of edges, suturing technique, and choosing
proper suture material. Depending on the type of suture Synthetic absorbable monofilament sutures:
material used, wound healing differs based on their tissue Polydioxanone (PDS), Polyglyconate (Maxon),
response, bacterial colonization, and physical properties Polyglecaprone (Monocril)
[3]. Synthetic absorbable monofilament/multifilament
sutures: Polyglycolic acid, Polyglactin 910
Literature review was performed by searching in the Natural non-absorbable multifilament sutures: Linen,
databases Pubmed, Web of Science and Scopus on the Silk, Cotton
topic, using the following keywords: sutures materials, Synthetic non-absorbable monofilament/multifilament
absorbable sutures, non-absorbable sutures and sutures: Polyester (Dacron, Mersilene), Polyamide
biocompatible materials. The present review helps the (Nylon), Stainless steel
IJISRT20APR777 www.ijisrt.com 981
Volume 5, Issue 4, April – 2020 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165
Synthetic non-absorbable monofilament sutures: absorbable suture, mass loss and strength loss profiles
Polypropylene (Surgilene, Prolene), Polybutester should be matched. Presently, there is no such absorbable
(Novafil), Polyethylene (Polytetrafluoroethylene) suture with ideal degradation properties.
Suture material selection should be considered during As the oral cavity contains different microorganisms,
treatment planning of oral surgery. Absorbable natural the sutures get contaminated when they come in contact
yarns (catgut) are responsible for the most intense with oral tissues. To reduce the complications like stitch
inflammatory reaction among all suture, besides presenting abscesses, the sutures should be opened just before suturing
a time very short and unpredictable absorption. The tensile [10]. bacterial adherence to sutures and inflammatory
strength is retained for less than 60 days in case of reactions of oral tissues are more common with braided silk
absorbable sutures whereas it is retained for more than 60 and cotton when compared with nylon,
days in case of non-absorbable sutures. The emergence of Polytetrafluoroethylene, polyester and polyglecaprone
the synthetic absorbable was very promising for several [11,12]. In a histological study of human gingival tissue,
reasons [5]: presence of neutrophils is more near silk sutures.
inflammatory reactions significantly less than natural Fibroblasts & new capillaries formation occurred at a slow
absorbable rate near silk sutures compared to tissues away from the
keep much of the resistance until the absorption process silk sutures indicating the delayed healing and severe tissue
begins reactions associated with silk sutures [13].
available with different times of absorption - short,
medium and long, giving opportunity to the clinician The coating on braided suture reduces friction that
choose the suitable material for each case. occurs during sliding and helps in stitching [10]. Knot tie-
down is better with monofilament or coated multifilament
In general, the monofilaments are appointed as more suture than rough uncoated multifilament suture. Coated
advantageous, because the multifilamentary provide sutures have high bending stiffness that is attributable to the
conditions for the development of infection, since bacterial loss of mobility of suture under bending force. The stiffness
colonies are formed in spaces between filaments [5]. also increases with increase in suture size and its chemical
Multifilament sutures have large surface area in contact constituent [9].
with tissues and inflammatory cells can penetrate into the
interstitial space within the suture causing more tissue Clinical disadvantages of suturing:
reaction. Braided suture trap plaque and soak up bacteria causing
infection and delaying healing. This is called "wick
Monofilament suture show less knot tie-down effect."
resistance, lower tissue drag and easily forms a stable knot Breakdown products of absorbable suture materials
due to its lower bending stiffness. Polytetrafluoroethylene cause inflammatory reactions in the tissues.
is the biocompatible monofilament suture that shows Length of the surgery increases with suturing which can
minimal memory, low surface friction, resistance to in vivo be increase the postoperative pain.
degradation and superior handling characteristics. But
chemical inertness and low static coefficient of friction Recent Advances and Emerging Trends:
makes the knot less secure [7]. Absorbable sutures are used as a vehicle to deliver of
a variety of biochemicals like antibiotics, growth factors
Suture characteristics are divided into Biological and etc., to improve wound healing. Recent advances in suture
Mechanical/Physical aspects [8]. materials are Absorbable staples, Tissue adhesives,
Biological Characteristics include Biodegradation, Surgical zippers, Drug eluting sutures, Antibacterial
Sterility, & Tissue tolerability. sutures, Stem cell seeded sutures, Smart sutures, Electronic
Physical Characteristics include Resistance to traction sutures [14].
strength, Capillarity, Flexibility, Plasticity, Elasticity, &
Manoeuvrability. Surgical Staples
Knot efficiency is the mechanical property of suture which Humer Hultl in 1908 developed surgical staples. As
depends on the extrinsic and intrinsic factors of a suture the surgical staples are made of inert steel, they can be left
material [9]. in the tissues for weeks. Specially designed extractors are
Extrinsic factors: Suture size, Throws in a knot, knot type used for the removal of staples. Surgical staples are
and tension applied. recently modified as absorbable staples (Lactomer).
Intrinsic factors: physical structure, surface treatment and Advantages are less time for suturing, rapid wound closure
coefficient of friction of sutures. & can be used in contaminated wounds [14].
Mass loss & strength loss profiles and Tissue Adhesives
biocompatibility of degradation products play a major role Naturally or artificially derived tissue adhesives are
in biodegradation and absorption of sutures. Degradation currently used for local hemostasis & wound closure. When
occurs by hydrolysis and phagocytosis and the rate of the adhesive is applied to a clean and dry wound, it rapidly
degradation is depending on the temperature and pH of the polymerizes and forms a firm bond approximating the
surrounding tissues of the suture [7]. For an ideal wound edges.
IJISRT20APR777 www.ijisrt.com 982
Volume 5, Issue 4, April – 2020 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165
Ideal properties of tissue adhesives [15]: Surgical Zipper
It should have adhesive property that bonds glue with This non-invasive suture material is used for skin
adjacent tissue. closures which need to be opened for inspection. This
It should have cohesive property that bonds the glue zipper can’t be used in wet conditions, high tension areas
molecules with one another. and in wounds with more than 20 degrees curvature [17].
It should have biodegradable property.
It should be biocompatible with minimal cytotoxicity. Antibacterial sutures:
It should be hydrophilic so that at body temperature it These antibacterial sutures reduce the postoperative
readily spreads on wet wound surfaces. infections and complications. Diacetyl chitin based sutures
It should be flexible and strong with the elastic modulus are absorbable and used in cases of epithelial and
same as that of tissue being glued. connective tissues with short term wound healing. The
bacterial attachment over the sutures can be prevented by
It should generate minimal heat during polymerization.
oxidative plasma treatment though controlled etching
resulting in a cost-effective antibacterial sutures without
Gingival bandage tape: Miller suggested sutureless
gingival grafting where a bandage tape is applied to the compromising the desirable features [18,19,20].
attached gingiva on both sides of the graft. As the
moisture prevents adhesion of tape to gingiva, complete Drug-eluting sutures
Different anti-microbial, pain management & anti-
hemostasis is necessary. Otherwise wound edges do not
inflammatory drugs, cytokines and extracellular matrix
effectively evert and gets loosened. Advantages with the
gingival bandage tape are they have greater tensile proteins are made available at the wound site by these drug
strength, good biocompatibility with lesser tissue eluting sutures. Coating the suture surface with
reaction and give good aesthetic results than sutured Tetracycline, levofloxacin, etc., by dip method or by
wounds or stapled wounds [14]. electrospinning method is done without compromising their
mechanical properties for the drug-eluting braided
multifilament silk sutures [21,22].
Autologous fibrin glue: It is Fibrin Fibronectin Sealing
System (FFSS)". This biologic adhesive contains
Stem cells seeded sutures
fibrinogen, fibronectin, factor XIII, thrombin, calcium
chloride and aprotinin. These are good hemostatic To increase the cell count and accelerate healing at the
wound site, stem cells seeded sutures are preferred. The
agents that are completely biodegradable with poor
stem cells are transplanted into the soft tissues using this
adhesive properties. [14,15].
type of sutures, but the main problem is their physical
properties are been compromised. Adipose derived stem
Cyanoacrylate: The usage of cyanoacrylate to repair
wounds or as hemostatic agents is extended recently to cell seeded sutures showed equally distributed viable cells
with increased metabolic activity at the wound healing area.
dental procedures. Exothermic heat produced during
Also the mesenchymal stem cells seeded sutures showed
polymerisation is avoided by applying drop by drop of
rapid wound healing by depositing collagen at the healing
cyanoacrylate and protecting the surrounding tissues
site [18,23].
[14,15,16].
Collagen- and Protein-based Sealants: An air and fluid Smart sutures
Shape memory polymers are used for developing the
tight seal is formed with these collagen and protein-
smart sutures which helps in self-tightening of knots in
based sealant when collagen crosslinks with
glutaraldehyde. deep wounds. These are available in a pre-stretched
condition made by cooling the filaments below their critical
As Protein-based adhesives are derived from bovine temperature. The sutures are loosely adapted at controlled
serum albumin, the foreign protein present causes stress to the wounds and on stimulating them above the
hypersensitization. Glutaraldehyde in collagen based critical temperature using external source, they regain their
original shape with defined tension across the tissues and
adhesives is a neurotoxin. These sealants show strong
forms a self-tightening knot [18,24].
inflammatory response and degradation is also very slow.
[15].
Electronic sutures
An ultrathin electronic suture of 1mm wide and 3mm
Polyurethane Adhesives: Polyurethane adhesives are
formed by the reaction of polyether-or polyester- thickness was developed with flexible silicon sensors
polyols with polyfunctional isocyanates. These impregnated on silk strips or polymers. These sutures are
adhesives form a strong bond with the surface by used for checking the wound condition by measuring the
reacting with hydroxyls and amines found in tissue. pH & bacterial count at the site. They improve wound
healing by accurately monitoring the oxygen, temperature
This resorbable adhesive is more biocompatible and
and enzymes at healing sites [18].
improves tissue healing [15].
IJISRT20APR777 www.ijisrt.com 983
Volume 5, Issue 4, April – 2020 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165
II. CONCLUSION [12]. F. Javed, M. Al-Askar, K. Almas, G.E. Romanos, and
K. Al-Hezaimi, “Tissue reactions to various suture
By following the basic rules, a good soft tissue materials used in oral surgical interventions,” ISRN
healing can occur after dental surgery. Esthetics play a Dentistry, vol. 2012, article id 762095.
major role along with minimizing postoperative infections [13]. R.S. Abi Rached, B.E. de Toledo, T. Okamoto, E.
& complications after oral surgery. To reach this goal, Marcantonio Junior, J.E. Sampaio, S.R. Orrico, et al.,
proper treatment planning considering the tissue condition “Reaction of the human gingival tissue to different
of wound, hemostasis & reapproximating the wound edges suture materials used in periodontal surgery,” Braz.
without tension by choosing correct suture material is Dent. J., vol. 2, no. 2, pp. 103-113, 1992.
necessary. With the advancement in suture technology [14]. H.R. Sajna, and A. Ramesh, “Wound closure-
clinician can reach the ultimate goal of pink esthetics in Alternatives to sutures,” J. Cont. Med. A. Dent., vol.
modern dentistry. 5, no. 2, pp. 17-20, 2017.
[15]. M.J. Buckley, and E.J. Beckman, “Adhesive use in
REFERENCES oral and maxillofacial surgery,” Oral Maxillofac.
Surg. Clin. North Am., vol. 22, no. 1, pp. 195-199,
[1]. W.C. Liao, Y.L. Lee, Y.L. Tsai, H.J. Lin, M.C. 2010.
Chang, S.F. Chang, et al., “Outcome assessment of [16]. A. Habib, A. Mehanna, and A. Medra,
apical surgery: A study of 234 teeth,” J. Formos. Med. “Cyanoacrylate: A handy tissue glue in maxillofacial
Assoc., vol. 118, no. 6, pp. 1055-1061, 2019. surgery: our experience in Alexandria,” Egypt. J.
[2]. M. Dragovic, M. Pejovic, J. Stepic, S. Colic, B. Maxillofac. Oral Surg., vol. 12, no. 3, pp. 243-247,
Dozic, S. Dragovic, et al., “Comparison of four 2013.
different suture materials in respect to oral wound [17]. D. Chen, J. Song, Y. Zhao, X. Zheng, and A. Yu,
healing, microbial colonization, tissue reaction and “Systematic review and meta-analysis of surgical
clinical features-randomized clinical study,” Clin. zipper technique versus intracutaneous sutures for the
Oral Investig., vol. 24, no.4, pp. 1527-1541, 2020. closing of surgical incision,” PLoS One, vol. 11, no. 9,
[3]. P. Velvart, and C.I. Peters, “Soft tissue management pii. e0162471, 2016.
in endodontic surgery,” J. Endod., vol.31, no. 1, pp. 4- [18]. C. Dennis, S. Sethu, S. Nayak, L. Mohan, Y.Y. Morsi,
16, 2005. and G. Manivasagam, “Suture materials-Current and
[4]. M.H. Kudur, S.B. Pai, H. Sripathi, and S. Prabhu. emerging trends,” J. Biomed. Mater. Res. A., vol. 104,
“Sutures and suturing techniques in skin closure,” no. 6, pp. 1544-1559, 2016.
Indian J. Dermatol. Venereol. Leprol., vol. 75, no. 4, [19]. P. Roy, P. Klita, P. Golmei, I. Hazarika, H.
pp. 425-434, 2009. Lalhlenmawia, and R.S. Dutta, “A need of a novel
[5]. I.A. Filho, I.A. Neto, M.H. Wanderley Costa Dantas, antimicrobial suture for surgical site infection,”
T.B.M. Sampaio, and A.C.M. Rego, “Surgical Research & Reviews: Journal of Microbiology and
Sutures: The necessary update of current knowledge,” Virology, vol. 6, no. 3, pp. 1-4, 2016.
J. Gastroenterol. Pancreatol. Liver Disord., vol. 6, no. [20]. M.G. Onesti, S. Carella, and N. Scuderi,
1, pp. 1-5, 2018. “Effectiveness of antimicrobial-coated sutures for the
[6]. K.P. Chellamani, D. Veerasubramanian, and R.S.V. prevention of surgical site infection: A review of the
Balaji, “Surgical sutures: An overview,” J. Acad. literature,” Eur. Rev. Med. Pharmacol. Sci., vol. 22,
Indus. Res., vol. 1, no. 12, pp. 778-782, 2013. no. 17, pp. 5729-5739, 2018.
[7]. D. Abellan, J. Nart, A. Pascual, R.E Cohen, and J.D. [21]. A. Arora, G. Aggarwal, J. Chander, P. Maman, and
Sanz-Moliner, “Physical and mechanical evaluation of M. Nagpal, “Drug eluting sutures: A recent update,” J.
five suture materials on three knot configurations: An Appl. Pharm. Sci., vol. 9, no. 7, pp. 111-123, 2019.
invitro study,” Polymers (Basel), vol. 8, no. 4, pii: [22]. M. Champeau, J.M. Thomassin, T. Tassaing, and C.
E147, 2016. Jerome, “Current manufacturing processes of drug-
[8]. F. Minozzi, P. Bollero, V. Unfer, A. Dolci, and M. eluting sutures,” Expert Opin. Drug Deliv., vol. 14,
Galli, “The sutures in dentistry,” Eur. Rev. Med. no. 11, pp. 1293-1303, 2017.
Pharmacol. Sci., vol. 13, no. 3, pp. 217-226, 2009. [23]. A.K. Reckhenrich, B.M. Kirsch, E.A. Wahl, T.L.
[9]. C.C. Chu, “Types and properties of surgical sutures. Schenck, F. Rezaeian, Y. Harder, et al., “Surgical
Biotextiles as medical implants,” pp. 231–273, 2013. sutures filled with adipose-derived stem cells promote
[10]. G. Zhang, T. Ren, X. Zeng, and E. Van Der Heide, wound healing”. PLoS One, vol. 9, no. 3, pii. e91169,
“Influence of surgical suture properties on the 2014.
tribological interactions with artificial skin by a [24]. R. Duarah, Y.P. Singh, P. Gupta, B.B. Mandal, and N.
capstan experiment approach,” Friction, vol. 5, no. 1, Karak. “Smart self-tightening surgical suture from a
pp. 87-98, 2017. tough bio-based hyperbranched polyurethane/reduced
[11]. N. Yilmaz, S. Inal, M. Muglali, T. Guvenc, and B. carbon dot nanocomposite,” Biomedical Materials,
Bas, “Effects of polyglecaprone 25, silk and catgut vol. 13, no. 4, pii. 045004, 2018.
suture materials on oral mucosa wound healing in
diabetic rats: An evaluation of nitric oxide dynamics,”
Med. Oral Patol. Oral Cir. Bucal., vol.15, no. 3, pp.
e526-e530, 2010.
IJISRT20APR777 www.ijisrt.com 984
You might also like
- ISSN 2347-5579: Use of Porous Polyethylene Implants For Orbital Reconstruction-A ReviewDocument3 pagesISSN 2347-5579: Use of Porous Polyethylene Implants For Orbital Reconstruction-A ReviewVISHAKHANo ratings yet
- Micro-Implants For Orthodontic Anchorage: A Review: July 2013Document6 pagesMicro-Implants For Orthodontic Anchorage: A Review: July 2013Vijay ChinthaNo ratings yet
- From Conventional To Unconventional - The Denture JourneyDocument4 pagesFrom Conventional To Unconventional - The Denture JourneySSR-IIJLS JournalNo ratings yet
- Evaluation of Gingival Fiber Retention Technique oDocument7 pagesEvaluation of Gingival Fiber Retention Technique oAbdur RehmanNo ratings yet
- Clinical Evaluation of Caries Removal Efficacy of Polymer Burs Running Title Efficacy of Polymer BursDocument8 pagesClinical Evaluation of Caries Removal Efficacy of Polymer Burs Running Title Efficacy of Polymer BursInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Biologic width significance for implant dentistryDocument8 pagesBiologic width significance for implant dentistryaakanksha bhardwajNo ratings yet
- Obturating Materials in Pediatric Dentistry a ReviDocument9 pagesObturating Materials in Pediatric Dentistry a Revikathuriayug5No ratings yet
- 2015 @dentallib Anil Kishen Nanotechnology PDFDocument206 pages2015 @dentallib Anil Kishen Nanotechnology PDFAnik BanerjeeNo ratings yet
- Biologic Width and ImplantsDocument8 pagesBiologic Width and ImplantsShruti Maroo - RathiNo ratings yet
- Smart MaterialsDocument4 pagesSmart MaterialsRisana RahoofNo ratings yet
- Effect of retraction materials on gingival healthDocument5 pagesEffect of retraction materials on gingival healthAastha DuaNo ratings yet
- ANUPAMATISSUEREVIEW2014Document7 pagesANUPAMATISSUEREVIEW2014liana rahmayaniNo ratings yet
- Journal of Dentistry and Oral BiologyDocument4 pagesJournal of Dentistry and Oral BiologyzaheerbdsNo ratings yet
- Socket Preservation Following Extraction A Review ArticleDocument4 pagesSocket Preservation Following Extraction A Review ArticleInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Peri-Implantitis: A Curse To ImplantsDocument11 pagesPeri-Implantitis: A Curse To ImplantsIJRASETPublicationsNo ratings yet
- JDVARKLADAKISSUTURESDocument6 pagesJDVARKLADAKISSUTURESKazi Zihadul AlamNo ratings yet
- Provisional Restorations in Fixed ProsthodonticsDocument4 pagesProvisional Restorations in Fixed ProsthodonticsPhoebe David100% (1)
- Brandt 2012Document23 pagesBrandt 2012EmilioPatlanNo ratings yet
- Restoring One Maxillary Fractured Incisor With A Porcelain Veneer A Case ReportDocument5 pagesRestoring One Maxillary Fractured Incisor With A Porcelain Veneer A Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Eview: Retentive Aids in Maxillofacial Prosthodontics - A ReviewDocument5 pagesEview: Retentive Aids in Maxillofacial Prosthodontics - A ReviewjoephinNo ratings yet
- Review of retentive aids in maxillofacial prosthesesDocument4 pagesReview of retentive aids in maxillofacial prosthesesmaha mohNo ratings yet
- Comparative Evaluation of Biofilm Adhesion To Different Types of Archwire and Microbiological Colonization During Orthodontic TreatmentDocument8 pagesComparative Evaluation of Biofilm Adhesion To Different Types of Archwire and Microbiological Colonization During Orthodontic TreatmentSorabh JainNo ratings yet
- A Review On Prosthetic Rehabilitation of Maxillofacial Region 2014Document5 pagesA Review On Prosthetic Rehabilitation of Maxillofacial Region 2014Zachary DuongNo ratings yet
- A Comparative Study of N-Butyl Cyanoacrylate and Conventional Silk Sutures in The Closure of Intra Oral Incisions After Modified CorticotomyPeizocisionDocument10 pagesA Comparative Study of N-Butyl Cyanoacrylate and Conventional Silk Sutures in The Closure of Intra Oral Incisions After Modified CorticotomyPeizocisionInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Modern Endodontic Principles Part 5: Obturation: Dental Update March 2016Document11 pagesModern Endodontic Principles Part 5: Obturation: Dental Update March 2016Julius M SiahaanNo ratings yet
- Medicina 59 00355Document12 pagesMedicina 59 00355Anuj BhardwajNo ratings yet
- Oktawati 2020Document3 pagesOktawati 2020Mariatun ZahronasutionNo ratings yet
- Flexible Denture Base Material A Viable AlternativDocument5 pagesFlexible Denture Base Material A Viable AlternativRaluca ChisciucNo ratings yet
- Peri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentFrom EverandPeri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentNo ratings yet
- Retentive Aids in Maxillofacial ProsthesisDocument109 pagesRetentive Aids in Maxillofacial ProsthesisEnu KambojNo ratings yet
- Review Article: Nanomaterials in Periodontal Tissue EngineeringDocument6 pagesReview Article: Nanomaterials in Periodontal Tissue EngineeringChaudhari SonaliNo ratings yet
- Reviez Literatura Adhesivos DnetalesDocument9 pagesReviez Literatura Adhesivos DnetalespaulinaNo ratings yet
- To Determine The Impact of Two Different Intra-Orifice Barrier Materials On Resistance of Fracture of Endodontically Treated TeethDocument8 pagesTo Determine The Impact of Two Different Intra-Orifice Barrier Materials On Resistance of Fracture of Endodontically Treated TeethInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Evaluation of The Fracture Resistance and Modulus of Elasticity of Commercially Available Core MaDocument4 pagesEvaluation of The Fracture Resistance and Modulus of Elasticity of Commercially Available Core MaSatya AsatyaNo ratings yet
- Smart Materials Smart ThinkDocument4 pagesSmart Materials Smart ThinkAthenaeum Scientific PublishersNo ratings yet
- Dentalife Ian 2018 DR BindermanDocument6 pagesDentalife Ian 2018 DR Bindermangabrielbalan568No ratings yet
- Shrestha - Kishen - 2016 - Antibacterial Nanoparticles in EndodonticsDocument10 pagesShrestha - Kishen - 2016 - Antibacterial Nanoparticles in EndodonticsdrchanyccNo ratings yet
- Endo Don TicDocument8 pagesEndo Don TicArmareality Armareality100% (1)
- Ijdos 2377 8075 08 6049Document6 pagesIjdos 2377 8075 08 6049ARAVINDAN GEETHA KRRISHNANNo ratings yet
- 28 Tripty RahangdaleDocument16 pages28 Tripty RahangdaleDrShweta SainiNo ratings yet
- Tanpa Judul PDFDocument7 pagesTanpa Judul PDFnadyashintakasihNo ratings yet
- Critical Evaluation of Suture Materials and Suturing Techniques in Implant Dentistry PDFDocument10 pagesCritical Evaluation of Suture Materials and Suturing Techniques in Implant Dentistry PDFria mayantiNo ratings yet
- Dennis Et Al-2016-Journal of Biomedical Materials Research Part ADocument16 pagesDennis Et Al-2016-Journal of Biomedical Materials Research Part Asiti nur fatimahNo ratings yet
- The Orthodontic Mini-Implants Failures Based On Patient Outcomes: Systematic ReviewDocument13 pagesThe Orthodontic Mini-Implants Failures Based On Patient Outcomes: Systematic ReviewKristin HalimNo ratings yet
- Knowledge and Awareness Among Dental Students About Choice of Complete Denture Occlusion in Edentulous PatientDocument7 pagesKnowledge and Awareness Among Dental Students About Choice of Complete Denture Occlusion in Edentulous PatientInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Management of Anterior Teeth Fracture With Preservation of Fractured Fragment-Two Case ReportsDocument9 pagesManagement of Anterior Teeth Fracture With Preservation of Fractured Fragment-Two Case ReportsMonica MarcilliaNo ratings yet
- Periodontal Considerations Determining The Design and Location of Margins in Restorative DentistryDocument9 pagesPeriodontal Considerations Determining The Design and Location of Margins in Restorative DentistryAnonymous AyxIccS4aXNo ratings yet
- Endo MidtermsDocument55 pagesEndo MidtermsPaul Jullean E. MakalintalNo ratings yet
- HealTalk1May June 2018Document5 pagesHealTalk1May June 2018Syarifina PutriNo ratings yet
- RetenedoresDocument5 pagesRetenedoresYayis LondoñoNo ratings yet
- A Case Report On Combination of Vista With Connective Tissue Graft As A Predictable Surgical Approach in Management of Multiple Gingival RecessionDocument5 pagesA Case Report On Combination of Vista With Connective Tissue Graft As A Predictable Surgical Approach in Management of Multiple Gingival RecessionInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- A Technique For Relining Transitional Removable Denture - A Case ReportDocument4 pagesA Technique For Relining Transitional Removable Denture - A Case ReportEduard Gabriel GavrilăNo ratings yet
- Microbial Contamination of Removable Dental Prosthesis at Different Interval of Usage An in Vitro StudyDocument6 pagesMicrobial Contamination of Removable Dental Prosthesis at Different Interval of Usage An in Vitro Studyhafidh akbarNo ratings yet
- Anodized Dental Implant Surface: Systematic ReviewDocument24 pagesAnodized Dental Implant Surface: Systematic ReviewRik ChatterjeeNo ratings yet
- Management of Peri-Implantitis: A Systematic Review, 2010-2015Document9 pagesManagement of Peri-Implantitis: A Systematic Review, 2010-2015Angela RamirezNo ratings yet
- Simplified Protocol For Relining Provisional Prosthesis On Natural Abutments A Technical Note. The International Journal Fabio Galli. 2018. TIJPRDDocument4 pagesSimplified Protocol For Relining Provisional Prosthesis On Natural Abutments A Technical Note. The International Journal Fabio Galli. 2018. TIJPRDValeria CrespoNo ratings yet
- InstrumentationDocument12 pagesInstrumentationMaiush JbNo ratings yet
- Bio DentineDocument238 pagesBio DentineMandreri100% (1)
- The Peri-Implant Zone - A Review of LiteratureDocument7 pagesThe Peri-Implant Zone - A Review of LiteratureJuanOso Gutierrez ArayaNo ratings yet
- An Analysis on Mental Health Issues among IndividualsDocument6 pagesAn Analysis on Mental Health Issues among IndividualsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Insights into Nipah Virus: A Review of Epidemiology, Pathogenesis, and Therapeutic AdvancesDocument8 pagesInsights into Nipah Virus: A Review of Epidemiology, Pathogenesis, and Therapeutic AdvancesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Compact and Wearable Ventilator System for Enhanced Patient CareDocument4 pagesCompact and Wearable Ventilator System for Enhanced Patient CareInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Smart Cities: Boosting Economic Growth through Innovation and EfficiencyDocument19 pagesSmart Cities: Boosting Economic Growth through Innovation and EfficiencyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Implications of Adnexal Invasions in Primary Extramammary Paget’s Disease: A Systematic ReviewDocument6 pagesImplications of Adnexal Invasions in Primary Extramammary Paget’s Disease: A Systematic ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Parkinson’s Detection Using Voice Features and Spiral DrawingsDocument5 pagesParkinson’s Detection Using Voice Features and Spiral DrawingsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- The Relationship between Teacher Reflective Practice and Students Engagement in the Public Elementary SchoolDocument31 pagesThe Relationship between Teacher Reflective Practice and Students Engagement in the Public Elementary SchoolInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Harnessing Open Innovation for Translating Global Languages into Indian LanuagesDocument7 pagesHarnessing Open Innovation for Translating Global Languages into Indian LanuagesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Air Quality Index Prediction using Bi-LSTMDocument8 pagesAir Quality Index Prediction using Bi-LSTMInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Investigating Factors Influencing Employee Absenteeism: A Case Study of Secondary Schools in MuscatDocument16 pagesInvestigating Factors Influencing Employee Absenteeism: A Case Study of Secondary Schools in MuscatInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Advancing Healthcare Predictions: Harnessing Machine Learning for Accurate Health Index PrognosisDocument8 pagesAdvancing Healthcare Predictions: Harnessing Machine Learning for Accurate Health Index PrognosisInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Exploring the Molecular Docking Interactions between the Polyherbal Formulation Ibadhychooranam and Human Aldose Reductase Enzyme as a Novel Approach for Investigating its Potential Efficacy in Management of CataractDocument7 pagesExploring the Molecular Docking Interactions between the Polyherbal Formulation Ibadhychooranam and Human Aldose Reductase Enzyme as a Novel Approach for Investigating its Potential Efficacy in Management of CataractInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Dense Wavelength Division Multiplexing (DWDM) in IT Networks: A Leap Beyond Synchronous Digital Hierarchy (SDH)Document2 pagesDense Wavelength Division Multiplexing (DWDM) in IT Networks: A Leap Beyond Synchronous Digital Hierarchy (SDH)International Journal of Innovative Science and Research TechnologyNo ratings yet
- The Making of Object Recognition Eyeglasses for the Visually Impaired using Image AIDocument6 pagesThe Making of Object Recognition Eyeglasses for the Visually Impaired using Image AIInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- The Utilization of Date Palm (Phoenix dactylifera) Leaf Fiber as a Main Component in Making an Improvised Water FilterDocument11 pagesThe Utilization of Date Palm (Phoenix dactylifera) Leaf Fiber as a Main Component in Making an Improvised Water FilterInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- The Impact of Digital Marketing Dimensions on Customer SatisfactionDocument6 pagesThe Impact of Digital Marketing Dimensions on Customer SatisfactionInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- A Survey of the Plastic Waste used in Paving BlocksDocument4 pagesA Survey of the Plastic Waste used in Paving BlocksInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Diabetic Retinopathy Stage Detection Using CNN and Inception V3Document9 pagesDiabetic Retinopathy Stage Detection Using CNN and Inception V3International Journal of Innovative Science and Research TechnologyNo ratings yet
- Formulation and Evaluation of Poly Herbal Body ScrubDocument6 pagesFormulation and Evaluation of Poly Herbal Body ScrubInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Comparatively Design and Analyze Elevated Rectangular Water Reservoir with and without Bracing for Different Stagging HeightDocument4 pagesComparatively Design and Analyze Elevated Rectangular Water Reservoir with and without Bracing for Different Stagging HeightInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Terracing as an Old-Style Scheme of Soil Water Preservation in Djingliya-Mandara Mountains- CameroonDocument14 pagesTerracing as an Old-Style Scheme of Soil Water Preservation in Djingliya-Mandara Mountains- CameroonInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Explorning the Role of Machine Learning in Enhancing Cloud SecurityDocument5 pagesExplorning the Role of Machine Learning in Enhancing Cloud SecurityInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Auto Encoder Driven Hybrid Pipelines for Image Deblurring using NAFNETDocument6 pagesAuto Encoder Driven Hybrid Pipelines for Image Deblurring using NAFNETInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Cyberbullying: Legal and Ethical Implications, Challenges and Opportunities for Policy DevelopmentDocument7 pagesCyberbullying: Legal and Ethical Implications, Challenges and Opportunities for Policy DevelopmentInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- A Review: Pink Eye Outbreak in IndiaDocument3 pagesA Review: Pink Eye Outbreak in IndiaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Design, Development and Evaluation of Methi-Shikakai Herbal ShampooDocument8 pagesDesign, Development and Evaluation of Methi-Shikakai Herbal ShampooInternational Journal of Innovative Science and Research Technology100% (3)
- Electro-Optics Properties of Intact Cocoa Beans based on Near Infrared TechnologyDocument7 pagesElectro-Optics Properties of Intact Cocoa Beans based on Near Infrared TechnologyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Hepatic Portovenous Gas in a Young MaleDocument2 pagesHepatic Portovenous Gas in a Young MaleInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Navigating Digitalization: AHP Insights for SMEs' Strategic TransformationDocument11 pagesNavigating Digitalization: AHP Insights for SMEs' Strategic TransformationInternational Journal of Innovative Science and Research Technology100% (1)
- Automatic Power Factor ControllerDocument4 pagesAutomatic Power Factor ControllerInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Hospital departments, medical terms, and anatomyDocument18 pagesHospital departments, medical terms, and anatomyThanh ToànNo ratings yet
- Artigo - Thought Disorder Schizophrenia - EnglishDocument11 pagesArtigo - Thought Disorder Schizophrenia - EnglishFrancisco ReigNo ratings yet
- Turkey's Growing Healthcare Sector Driven by Private ProvidersDocument69 pagesTurkey's Growing Healthcare Sector Driven by Private ProviderssbulenterisNo ratings yet
- Tibia and Fibula Fracture PhysiotherapyDocument31 pagesTibia and Fibula Fracture Physiotherapyunknown unknown100% (1)
- Nursing Care of The Older Adult in Wellness: Geriatric Nursing AssessmentDocument36 pagesNursing Care of The Older Adult in Wellness: Geriatric Nursing AssessmentRuby Corazon Ediza100% (6)
- Observing Gender SensitivityDocument54 pagesObserving Gender SensitivityOrlando NajeraNo ratings yet
- Semi-Detailed Lesson Plan in T.L.E FoodsDocument3 pagesSemi-Detailed Lesson Plan in T.L.E Foodsgracelyn riveraNo ratings yet
- Declaration of James Sheldon2318Document7 pagesDeclaration of James Sheldon2318James Sheldon Jr.No ratings yet
- Sub-Adventitial Divestment Technique For Resecting Artery-Involved Pancreatic Cancer: A Retrospective Cohort StudyDocument11 pagesSub-Adventitial Divestment Technique For Resecting Artery-Involved Pancreatic Cancer: A Retrospective Cohort StudyMatias Jurado ChaconNo ratings yet
- Rare Homeopathic Remedies for Specific ConditionsDocument8 pagesRare Homeopathic Remedies for Specific ConditionsIndhumathiNo ratings yet
- Case Study Attendance Score DisputeDocument3 pagesCase Study Attendance Score DisputeSyed Aamir Ahmed0% (2)
- Abbott PIMA CD4 BR NewDocument2 pagesAbbott PIMA CD4 BR NewangelinaNo ratings yet
- Safety and Influence of A Novel Powder Form of Coconut Inflorescence Sap On Glycemic Index and LipidDocument1 pageSafety and Influence of A Novel Powder Form of Coconut Inflorescence Sap On Glycemic Index and LipidPriscila CerqueiraNo ratings yet
- Runner Ru4rxDocument45 pagesRunner Ru4rxfcdypmsbssNo ratings yet
- Board and Reviewer Assignments for Convened IRB ReviewDocument5 pagesBoard and Reviewer Assignments for Convened IRB ReviewMuhammad Zaryab KhanNo ratings yet
- Immediate Dentures ExplainedDocument64 pagesImmediate Dentures ExplainedDHANASRI MOTAPARTHYNo ratings yet
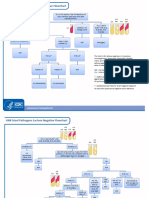
- GNR Stool Pathogens Lactose Negative FlowchartDocument2 pagesGNR Stool Pathogens Lactose Negative FlowchartKeithNo ratings yet
- Module 2Document43 pagesModule 2jbg060595No ratings yet
- National Leprosy Control ProgramDocument35 pagesNational Leprosy Control ProgramJL CalvinNo ratings yet
- P.E 1 - Module - First Quarter - Health Behavior and Risk FactorsDocument30 pagesP.E 1 - Module - First Quarter - Health Behavior and Risk Factorsjohn charles garaldeNo ratings yet
- The Movie "PK" AnalysisDocument2 pagesThe Movie "PK" AnalysisKerstmis “Scale” NataliaNo ratings yet
- DSP 15-12-23Document36 pagesDSP 15-12-23Fu'ad ParkhaniNo ratings yet
- UPSC Prelims 2021 Geography Revision: High Probable Topics Part 2Document86 pagesUPSC Prelims 2021 Geography Revision: High Probable Topics Part 2PreethiNo ratings yet
- Effects of A Capacitive-Resistive Electric Transfer Therapy OnDocument8 pagesEffects of A Capacitive-Resistive Electric Transfer Therapy OnAnna Lygia LunardiNo ratings yet
- Psychology Learning Objectives, Contents, Activities and EvaluationDocument12 pagesPsychology Learning Objectives, Contents, Activities and EvaluationSAYMABANUNo ratings yet
- Grade 8 BowDocument7 pagesGrade 8 BowJorely Barbero MundaNo ratings yet
- Physical Education and Health 2 - Grade 11 NotesDocument6 pagesPhysical Education and Health 2 - Grade 11 NotesPedro HampaslupaNo ratings yet
- Lecture PATHFT2Document7 pagesLecture PATHFT2Gniese Stephanie Gallema AlsayNo ratings yet
- Glucosamine PDFDocument6 pagesGlucosamine PDFChrist FarandyNo ratings yet
- Meaning and Definition of Management DevelopmentDocument7 pagesMeaning and Definition of Management DevelopmentRiteshTirkey100% (2)