Professional Documents
Culture Documents
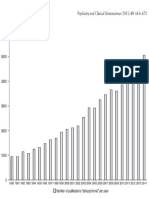
Appi Ps 201800073
Uploaded by
Doc HadiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Appi Ps 201800073
Uploaded by
Doc HadiCopyright:
Available Formats
OPEN FORUM
Treatment Implications of Situational Variability in
Cognitive and Negative Symptoms of Schizophrenia
Jasmine Mote, Ph.D., Paul M. Grant, Ph.D., Steven M. Silverstein, Ph.D.
Cognitive impairments and negative symptoms in schizo- evidence for the situational variability of cognitive impairments
phrenia are associated with poorer outcomes and are typically and negative symptoms in schizophrenia and highlights psy-
resistant to pharmacological interventions. However, these chosocial treatments that capitalize on this variability. The
features can vary dramatically in their level of expression, and authors’ goals are to stimulate development and implementa-
they can improve as a function of external context (by providing tion of interventions and to show practitioners how they can
performance-contingent incentives and a more stimulating achieve more positive outcomes in their clinical work with what
environment) and internal context (by challenging defeatist is often seen as a hard-to-treat population.
performance beliefs and by reducing stress and improving
physical health). This Open Forum briefly reviews some of this Psychiatric Services 2018; 69:1095–1097; doi: 10.1176/appi.ps.201800073
A stereotypical clinical picture of a person living with individuals with schizophrenia optimize their effectiveness
chronic schizophrenia is someone with cognitive impair- in their multiple roles. The evidence for situational vari-
ments and negative symptomatology. A case example from ability of these impairments offers hope for both practi-
our work would be an inpatient who exhibits multiple tioners and consumers of mental health services that these
neurocognitive impairments (on testing), exhibits restricted difficulties may be more malleable than previously thought.
affect, paces up and down the ward talking to himself, and In this Open Forum, we discuss four contexts that appear to
appears uninterested in interacting with others. However, influence the severity of cognitive impairments and negative
how do we understand the transformation that occurs symptoms among persons with schizophrenia and highlight
when this same person volunteers to grill food during a unit treatment implications for each.
summertime picnic, engages in conversations with others
while cooking, shows a range of affect, and plays Frisbee
Performance-Contingent Rewards
after lunch? Or what about a young man who scores within
the severely impaired range on a variety of standardized Performance-contingent rewards include financial, social, and
cognitive assessments but is a virtuoso video gamer who other types (for example, food) of reinforcement. Although
writes his own music, drives his car in an urban area, and they may seem trivial, these rewards, particularly social rein-
does well in college-level art courses? Would we still con- forcement, have been shown to improve positive affect,
sider him “severely cognitively impaired?” self-efficacy, hope, and trust among persons with a variety
Research, both old and new, indicates vast situational of psychiatric conditions. Specific to schizophrenia, financial
variability in the expression of cognitive and negative and social reinforcement have been shown to improve cog-
symptoms among individuals with schizophrenia. Cognitive nitive performance (including executive functioning), reduce
impairments (for example, difficulties in executive func- the expression of negative symptoms such as self-neglect and
tioning, working memory, and attention) and negative inactivity, and improve social functioning (1–3).
symptoms (for example, blunted affect, amotivation, aso- One intervention that uses performance-contingent re-
ciality, anhedonia, and alogia) are often correlated with one wards to improve cognition and social functioning among
another, associated with poorer outcomes, and resistant to persons with schizophrenia is the combination of attention
pharmacological interventions—and thus often perceived shaping with skills training (4). In this intervention, partic-
as intractable. Because of the relationship of cognition and ipants are given tangible rewards (money or food) and so-
negative symptoms with functional outcomes, it is para- cial reinforcement (praise and encouragement) when they
mount to understand the contexts that may improve such complete small, individualized attention goals (for exam-
symptoms and then use that information to continue to ple, focusing on the person speaking for three consecutive
develop, investigate, and implement treatments that help minutes) during a group skills training session (for example,
Psychiatric Services 69:10, October 2018 ps.psychiatryonline.org 1095
SITUATIONAL VARIABILITY IN COGNITIVE AND NEGATIVE SYMPTOMS
social skills training). As participants continue to meet their thought, “If I fail partly, it is as bad as being a complete
attentiveness goals in subsequent group sessions, the criteria failure.” These beliefs appear to moderate the relationship
for earning a reward are increased (for example, reinforce- between negative symptoms and functioning and to mediate
ment is given for five consecutive minutes of attention). the relationship between negative symptoms and cognitive
Integration of attention shaping and skills training has been impairment among persons with schizophrenia (7). This
shown to improve attentiveness (in and outside of study finding suggests that people with schizophrenia may not
groups) and skills acquisition, compared with the effects of believe they can succeed at certain behaviors (social engage-
skills training alone. Social reinforcers can generate treat- ment and cognitive task performance), which in turn reduces
ment effects that are comparable to those of tangible rein- their motivation to persist in challenging tasks, including
forcers (for example, money) (3). Thus, mental health neuropsychological tests (7).
practitioners already have a powerful tool that, when used Cognitive-behavioral therapy is considered the bench-
systematically and in conjunction with extinction tech- mark for treating many mental health conditions and in-
niques targeting inattentive and disruptive behaviors, can volves therapists helping consumers change their thoughts
be expected to produce strong and generalizable gains, re- in order to help them change their feelings and behaviors.
gardless of an agency’s budget. Thus, it is an ideal therapeutic orientation from which to
address defeatist performance beliefs. Recovery-oriented
cognitive therapy is one approach that promotes the devel-
Enriched Versus Deprived Environments
opment of positive beliefs about the self in people with
An enriched environment may include a number of factors, schizophrenia. It does so via systematic engagement of the
such as an increased opportunity for social interactions, in- individual in personally meaningful activities in order to
creased autonomy, or access to evidence-based psychosocial lead to a cycle of success, improved functioning, and reduced
rehabilitation services. Multiple studies have shown cogni- negative symptoms (8). Such results suggest that explicitly
tive improvements when the external environment of a targeting defeatist performance beliefs of persons with
person with schizophrenia changes for the better (for ex- schizophrenia can reduce negative symptoms and may re-
ample, when the person transitions from homelessness to duce cognitive impairments observed on standardized tests.
living in an independent apartment) or becomes more
structured, even in the absence of targeted cognitive inter-
Stress and Physical Health
ventions (2). Furthermore, in psychiatric institutions, factors
such as a more stimulating social environment (for example, Stress and an elevated physiological arousal level are asso-
number of positive statements made to patients) and phys- ciated with illness onset and relapse among persons with
ical environment (for example, number of personal posses- schizophrenia. These individuals are at higher risk of co-
sions allowed in the patient’s room) are correlated with occurring general medical conditions that are associated
fewer negative symptoms and longer community tenure af- with stress, including hypertension, cardiovascular disease,
ter hospital discharge (5,6). and increased blood glucose levels. Stress and hypertension
The treatment implications of these data are clear: greater have both been associated with poorer cognitive perfor-
attention to the socioaffective contexts in which persons with mance in schizophrenia (9,10). The presence of diabetes,
schizophrenia live and are treated can lead to clinically sig- which has a profile of cognitive impairment virtually iden-
nificant improvements in multiple domains of functioning. tical to that found in schizophrenia, is also associated with
This is not news. For example, the deinstitutionalization poorer cognitive functioning among persons with schizo-
movement in the United States was partly inspired by public phrenia, with greater impairment related to greater diabetic
outcry over the deplorable conditions of state psychiatric severity (11). In addition, there is some evidence that changes
facilities. However, the movement inadvertently led to an in- in the level of cortisol, a hormone whose release is often
crease in homelessness and imprisonment rates of people associated with stress, are correlated with negative symp-
with serious mental illness because of a lack of improvements toms among persons with schizophrenia (12).
in community-based care. The more recent promotion of Individuals with schizophrenia benefit from the same
recovery-focused care across the United States is one step in psychosocial treatments that reduce stress and improve
promoting enriching and personally meaningful environments physical health of those without schizophrenia: treatments
after deinstitutionalization. However, the potential for envi- that focus on exercise, mindfulness, and improving positive
ronmental contexts and staff behavior to affect the outcomes of emotion. Recent evidence has shown that exercise enhances
persons with schizophrenia has not been fulfilled and is typi- outcomes as an adjunct to cognitive remediation—the gold
cally not addressed in research and health care policy domains. standard treatment for cognitive impairments—among persons
with schizophrenia (13). Treatments that combine mindfulness
with cognitive enhancement training are also showing prom-
Defeatist Performance Beliefs
ise (14). Furthermore, improving positive emotions and mind-
Defeatist performance beliefs are the overgeneralized neg- fulness skills has been shown to promote resiliency, enhance
ative thoughts about one’s abilities, such as endorsing the cognitive resources, regulate stress responses, and improve
1096 ps.psychiatryonline.org Psychiatric Services 69:10, October 2018
MOTE ET AL.
other physical health outcomes of individuals with and without Development Service, U.S. Department of Veterans Affairs (VA). The
schizophrenia. Positive emotion and mindfulness interventions contents do not necessarily represent the views of the VA or the U.S.
government.
have also been shown to improve negative symptoms among
Dr. Silverstein reports receipt of consultant fees from Boehringer-
those with schizophrenia (15).
Ingelheim and receipt of research funds from diaMentis, Inc. The other
authors report no financial relationships with commercial interests.
Discussion
Received February 13, 2018; revision received April 24, 2018; accepted
This Open Forum discussion only scratches the surface of May 31, 2018; published online August 20, 2018.
contexts that have been shown to influence the degree of
expression of cognitive impairments and negative symp- REFERENCES
toms among persons with schizophrenia. Other important 1. Park S, Gibson C, McMichael T: Socioaffective factors modulate
working memory in schizophrenia patients. Neuroscience 139:
contexts should be considered in regard to their relation-
373-384, 2006
ship to cognitive impairments and negative symptoms, in- 2. Silverstein SM, Wilkniss SM: The future of cognitive rehabilitation
cluding (but not limited to) culture, gender, affect and of schizophrenia. Schizophrenia Bulletin 30:679–692, 2004
mood states, trauma history, psychological factors (for 3. Silverstein SM, Hatashita-Wong M, Wilkniss S, et al: Behavioral
example, internalized stigma), sleep disorders (for exam- rehabilitation of the “treatment-refractory” schizophrenia patient:
conceptual foundations, interventions, and outcome data. Psycho-
ple, apnea), the detrimental effects of anticholinergic load
logical Services 3:145–169, 2006
of medications on cognition, poor visual acuity, and the 4. Silverstein SM, Roché MW, Khan Z, et al: Enhancing and pro-
many complicated interactions that these internal and ex- moting recovery in attentionally impaired people diagnosed with
ternal factors have on one another. Furthermore, although schizophrenia: results from a randomized controlled trial of at-
not the focus of this Open Forum, positive symptoms, tention shaping in a partial hospital program. American Journal of
Psychiatric Rehabilitation 17:272–305, 2014
disorganized behavior, and aggressive behavior have also
5. Oshima I, Mino Y, Inomata Y: Institutionalisation and schizo-
been shown to be modifiable by context, and thus the phrenia in Japan: social environments and negative symptoms: na-
comprehensive approach we espouse should be relevant to tionwide survey of in-patients. British Journal of Psychiatry 183:
other aspects of schizophrenia that are associated with a 50–56, 2003
reduced level of functioning (3,16). 6. Coleman JC, Paul GL: Relationship between staffing ratios and
effectiveness of inpatient psychiatric units. Psychiatric Services 52:
What remains clear is that the features of schizophrenia
1374–1379, 2001
that are consistently found to be most related to functional 7. Beck AT, Himelstein R, Bredemeier K, et al: What accounts for
outcomes under typical conditions can vary significantly as a poor functioning in people with schizophrenia? A re-evaluation
function of multiple factors. Moreover, each of the factors of the contributions of neurocognitive vs attitudinal and moti-
we discussed is modifiable, and it has already been shown vational factors. Psychological Medicine (Epub ahead of print,
Mar 4, 2018)
that specific modifications have clinical benefit. Rather than
8. Grant PM, Bredemeier K, Beck AT: Six-month follow-up of
training practitioners to view cognitive impairments and recovery-oriented cognitive therapy for low-functioning individu-
negative symptoms as stable, core aspects of a mental dis- als with schizophrenia. Psychiatric Services 68:997–1002, 2017
ease, programs should train practitioners to use their clinical 9. Krkovic K, Moritz S, Lincoln TM: Neurocognitive deficits or stress
skills to promote internal and external changes associated overload: why do individuals with schizophrenia show poor per-
formance in neurocognitive tests? Schizophrenia Research 183:
with reductions in these symptoms. By systematically pro-
151–156, 2017
viding behavior-specific incentives (social or otherwise), 10. Morra LF, Strauss GP: Severity of hypertension predicts the gen-
improving living and treatment environments, increasing eralized neurocognitive deficit in schizophrenia. Schizophrenia
opportunities for personally meaningful activities, providing Research 176:527–528, 2016
hope for recovery, allowing for experiences to build the 11. Dickinson D, Gold JM, Dickerson FB, et al: Evidence of exacer-
bated cognitive deficits in schizophrenia patients with comorbid
confidence that a person can succeed despite beliefs to the
diabetes. Psychosomatics 49:123–131, 2008
contrary, and improving resilience to stress, clinicians can 12. Bradley AJ, Dinan TG: A systematic review of hypothalamic-
help individuals with schizophrenia combat the most debili- pituitary-adrenal axis function in schizophrenia: implications for
tating aspects of their disorder. mortality. Journal of Psychopharmacology 24(suppl):91–118, 2010
13. Campos C, Rocha NBF, Lattari E, et al: Exercise induced neuro-
plasticity to enhance therapeutic outcomes of cognitive remediation in
AUTHOR AND ARTICLE INFORMATION
schizophrenia: analyzing the role of brain derived neurotrophic factor.
Dr. Mote is with the Social and Community Reintegration Research CNS and Neurological Disorders Drug Targets 16:638–651, 2017
Program, Edith Nourse Rogers Memorial Veterans Hospital, Bedford, 14. Tabak NT, Granholm E: Mindful cognitive enhancement training
Massachusetts. Dr. Grant is with the Department of Psychiatry, Perel- for psychosis: a pilot study. Schizophrenia Research 157:312–313, 2014
man School of Medicine, University of Pennsylvania, Philadelphia. Dr. 15. Garland EL, Fredrickson B, Kring AM, et al: Upward spirals of
Silverstein is with the Division of Schizophrenia Research, Rutgers Uni- positive emotions counter downward spirals of negativity: insights
versity Behavioral Health Care, and the Department of Psychiatry, from the broaden-and-build theory and affective neuroscience on
Rutgers–Robert Wood Johnson Medical School, Piscataway, New Jersey. the treatment of emotion dysfunctions and deficits in psychopa-
Send correspondence to Dr. Mote (e-mail: jasmine.mote@gmail.com). thology. Clinical Psychology Review 30:849–864, 2010
This work was supported in part by award D1873-F to Dr. Mote from 16. Zarlock SP: Social expectations, language, and schizophrenia. Journal
the Research Enhancement Award Program, Rehabilitation Research and of Humanistic Psychology 6:68–74, 1966
Psychiatric Services 69:10, October 2018 ps.psychiatryonline.org 1097
You might also like
- Gale Researcher Guide for: Overview of Behavioral and Mental Disorders in PsychologyFrom EverandGale Researcher Guide for: Overview of Behavioral and Mental Disorders in PsychologyNo ratings yet
- Discover Recovery: A Comprehensive Addiction Recovery WorkbookFrom EverandDiscover Recovery: A Comprehensive Addiction Recovery WorkbookNo ratings yet
- Spiritual Assessment in Social Work and Mental Health PracticeFrom EverandSpiritual Assessment in Social Work and Mental Health PracticeNo ratings yet
- Recent Advances in Social Skills Training For SchizophreniaDocument12 pagesRecent Advances in Social Skills Training For SchizophreniavinodksahuNo ratings yet
- Psychosocial Approaches in Schizophrenia: Presenter: Dr.D.Archanaa Chairperson: Ms - NeethiDocument61 pagesPsychosocial Approaches in Schizophrenia: Presenter: Dr.D.Archanaa Chairperson: Ms - NeethidarchanaavigneshNo ratings yet
- Hunger: Mentalization-based Treatments for Eating DisordersFrom EverandHunger: Mentalization-based Treatments for Eating DisordersRating: 1 out of 5 stars1/5 (1)
- PDR ReportDocument11 pagesPDR ReportAndreasNo ratings yet
- Fuel Minds: Unleash Your Potential with Mind and Body WellnessFrom EverandFuel Minds: Unleash Your Potential with Mind and Body WellnessNo ratings yet
- Building Bridges: A Guide to Emotional Regulation and EnhancementFrom EverandBuilding Bridges: A Guide to Emotional Regulation and EnhancementNo ratings yet
- Esquizo ITP 2011Document4 pagesEsquizo ITP 2011DrMartens AGNo ratings yet
- The Effect of Meditation and Relaxation on Individuals Diagnosed with Long-Term SchizophreniaFrom EverandThe Effect of Meditation and Relaxation on Individuals Diagnosed with Long-Term SchizophreniaNo ratings yet
- ROLE of AssingmentDocument7 pagesROLE of AssingmentMaleeha AyubNo ratings yet
- Cognitive Impairment in DepressionDocument4 pagesCognitive Impairment in DepressionYosieAgniUtamiNo ratings yet
- Mental Health, Intellectual and Developmental Disabilities and the Ageing ProcessFrom EverandMental Health, Intellectual and Developmental Disabilities and the Ageing ProcessNo ratings yet
- Recent Advances in Social Skills Training For SchizophreniaDocument12 pagesRecent Advances in Social Skills Training For SchizophreniaPriya RaguramanNo ratings yet
- Prediction of Disability in Schizophrenia: Symptoms, Cognition, and Self-AssessmentDocument20 pagesPrediction of Disability in Schizophrenia: Symptoms, Cognition, and Self-AssessmentEmanu PompilioNo ratings yet
- The Influence of Art and Music On Cognitive Function and Mental Health Well Being pr1Document7 pagesThe Influence of Art and Music On Cognitive Function and Mental Health Well Being pr1Patricia CayabyabNo ratings yet
- Pathways to Recovery: Preventing Relapse in First Episode Psychosis: Strategies for Relapse Prevention and Mental Health Resilience in First Episode PsychosisFrom EverandPathways to Recovery: Preventing Relapse in First Episode Psychosis: Strategies for Relapse Prevention and Mental Health Resilience in First Episode PsychosisNo ratings yet
- Impact of Stigma On The Clients' Participation in Mental Health ServicesDocument19 pagesImpact of Stigma On The Clients' Participation in Mental Health ServicesJoshua C. Gandi100% (1)
- Schizophrenia and Behavior ModificationDocument8 pagesSchizophrenia and Behavior ModificationMelanie HallNo ratings yet
- Tijmann, JDocument43 pagesTijmann, JNabil Sangga BuanaNo ratings yet
- DEFININGDocument9 pagesDEFININGrushnaNo ratings yet
- Nutritional and Herbal Therapies for Children and Adolescents: A Handbook for Mental Health CliniciansFrom EverandNutritional and Herbal Therapies for Children and Adolescents: A Handbook for Mental Health CliniciansNo ratings yet
- Food Counselling. How To Motivate People To Change Eating HabitsFrom EverandFood Counselling. How To Motivate People To Change Eating HabitsNo ratings yet
- EMOTIONAL SELF-REGULATION AND ARTISTIC THERAPIESFrom EverandEMOTIONAL SELF-REGULATION AND ARTISTIC THERAPIESRating: 5 out of 5 stars5/5 (1)
- PSY120Document4 pagesPSY120Racheal MukiriNo ratings yet
- Quality of Life in Caregivers of Patients With Schizophrenia A Literature ReviewDocument6 pagesQuality of Life in Caregivers of Patients With Schizophrenia A Literature Reviewgw0q12dxNo ratings yet
- An Integrative Paradigm for Mental Health Care: Ideas and Methods Shaping the FutureFrom EverandAn Integrative Paradigm for Mental Health Care: Ideas and Methods Shaping the FutureNo ratings yet
- Psychological Perspectives Poverty Full - 0Document46 pagesPsychological Perspectives Poverty Full - 0Parthiban S. GopalNo ratings yet
- Recovery Oriented Cognitive TherapyDocument30 pagesRecovery Oriented Cognitive TherapyhibaNo ratings yet
- Psychosocial Interventions CompleteDocument14 pagesPsychosocial Interventions CompleteDwane PaulsonNo ratings yet
- Mental Health Group Therapy Activities for Adults: A Complete Guide to Group Therapy activities for Mental Health and WellbeingFrom EverandMental Health Group Therapy Activities for Adults: A Complete Guide to Group Therapy activities for Mental Health and WellbeingNo ratings yet
- Schizophrenia ResearchDocument10 pagesSchizophrenia ResearchMason FNo ratings yet
- Week 2 Recovery Model of Mental Illness - A Complementary Approach To Psychiatric CareDocument5 pagesWeek 2 Recovery Model of Mental Illness - A Complementary Approach To Psychiatric CareNg WinnieNo ratings yet
- Nutritional Counselling. How To Motivate People To Correct Their Eating HabitsFrom EverandNutritional Counselling. How To Motivate People To Correct Their Eating HabitsNo ratings yet
- Running Head: Personal Recovery 0Document8 pagesRunning Head: Personal Recovery 0Ravi KumawatNo ratings yet
- Free Research Papers On Mental IllnessDocument5 pagesFree Research Papers On Mental Illnesssvfziasif100% (1)
- Sociocultural PerspectiveDocument11 pagesSociocultural PerspectiveadeshNo ratings yet
- Yapko Hypnosis DepressionDocument3 pagesYapko Hypnosis Depression11111No ratings yet
- Nourishing Minds: The Interplay of Eating and Mental HealthFrom EverandNourishing Minds: The Interplay of Eating and Mental HealthNo ratings yet
- Psychosocial Interventions DraftDocument12 pagesPsychosocial Interventions DraftDwane PaulsonNo ratings yet
- Goal Representations and Motivational Drive in Schizophrenia: The Role of Prefrontal-Striatal InteractionsDocument16 pagesGoal Representations and Motivational Drive in Schizophrenia: The Role of Prefrontal-Striatal Interactions奚浩然No ratings yet
- Social Function EditDocument12 pagesSocial Function EditUMINAHNo ratings yet
- Promoting A Healthy LifestyleDocument3 pagesPromoting A Healthy LifestyleanandaNo ratings yet
- Integrative Medicine for Vulnerable Populations: A Clinical Guide to Working with Chronic and Comorbid Medical Disease, Mental Illness, and AddictionFrom EverandIntegrative Medicine for Vulnerable Populations: A Clinical Guide to Working with Chronic and Comorbid Medical Disease, Mental Illness, and AddictionNo ratings yet
- Mental health and psicological disturb: What they are and how they workFrom EverandMental health and psicological disturb: What they are and how they workNo ratings yet
- Breaking Free from Self-Doubt: Secrets to Crushing Negative ThoughtsFrom EverandBreaking Free from Self-Doubt: Secrets to Crushing Negative ThoughtsNo ratings yet
- Psychosocial Needs of Adult and AdolescentDocument8 pagesPsychosocial Needs of Adult and AdolescentVine CorpzNo ratings yet
- Breaking the Chains: Understanding Substance Use Disorders and Mental HealthFrom EverandBreaking the Chains: Understanding Substance Use Disorders and Mental HealthNo ratings yet
- Gibbons 2012Document8 pagesGibbons 2012Doc HadiNo ratings yet
- Perbedaan Fungsi Kognitif Pada Lansia Yang Kualitas Tidurnya Baik Dan Buruk Di Banjar Peken Desa Sumerta DenpasarDocument12 pagesPerbedaan Fungsi Kognitif Pada Lansia Yang Kualitas Tidurnya Baik Dan Buruk Di Banjar Peken Desa Sumerta DenpasarDoc HadiNo ratings yet
- CESD-10 Website PDFDocument3 pagesCESD-10 Website PDFDoc HadiNo ratings yet
- Workshop QEEG Abnormal in Psychiatric Setting Drsanti - AkeswariDocument63 pagesWorkshop QEEG Abnormal in Psychiatric Setting Drsanti - AkeswariDoc HadiNo ratings yet
- Rehabilitasi Medis Untuk GSA - Dr. LuhDocument32 pagesRehabilitasi Medis Untuk GSA - Dr. LuhDoc HadiNo ratings yet
- Garlow 2013Document5 pagesGarlow 2013Doc HadiNo ratings yet
- Healy 1994Document9 pagesHealy 1994Doc HadiNo ratings yet
- CESD-10 Website PDFDocument3 pagesCESD-10 Website PDFDoc HadiNo ratings yet
- A Local Review of Child Abuse in HongDocument12 pagesA Local Review of Child Abuse in HongDoc HadiNo ratings yet
- Early Post-Stroke Depression and Mortality: Meta-Analysis and Meta-RegressionDocument7 pagesEarly Post-Stroke Depression and Mortality: Meta-Analysis and Meta-RegressionDoc HadiNo ratings yet
- Psychiatric con-WPS OfficeDocument1 pagePsychiatric con-WPS OfficeDoc HadiNo ratings yet
- Comparison FFP2 KN95 N95 Filtering Facepiece Respirator Classes PDFDocument3 pagesComparison FFP2 KN95 N95 Filtering Facepiece Respirator Classes PDFazsigncNo ratings yet
- Cognitive Impairment and Personality Traits in Epilepsy (2.6)Document6 pagesCognitive Impairment and Personality Traits in Epilepsy (2.6)Doc HadiNo ratings yet
- A Local Review of Child Abuse in HongDocument12 pagesA Local Review of Child Abuse in HongDoc HadiNo ratings yet
- 672 The Maudsle-WPS OfficeDocument1 page672 The Maudsle-WPS OfficeDoc HadiNo ratings yet
- Journal 1 PDFDocument8 pagesJournal 1 PDFpososuperNo ratings yet
- JurnalDocument8 pagesJurnalDoc HadiNo ratings yet
- Horsdal2017-Metabolic Profile at First-Time Schizophrenia Diagnosis A PopulatDocument10 pagesHorsdal2017-Metabolic Profile at First-Time Schizophrenia Diagnosis A PopulatDoc HadiNo ratings yet
- What Does Schizophrenia Teach Us About AntipsikotikDocument5 pagesWhat Does Schizophrenia Teach Us About AntipsikotikDoc HadiNo ratings yet
- Trust and Acceptance of A Virtual Psychiatric Interview Between Embodied Conversational Agents and OutpatientsDocument7 pagesTrust and Acceptance of A Virtual Psychiatric Interview Between Embodied Conversational Agents and OutpatientsDoc HadiNo ratings yet
- SJMMS 4 206Document6 pagesSJMMS 4 206Doc HadiNo ratings yet
- Taking Legal Histories in Psychiatric Assessments: Nathaniel P. Morris, M.DDocument3 pagesTaking Legal Histories in Psychiatric Assessments: Nathaniel P. Morris, M.DDoc HadiNo ratings yet
- Schizophrenia Trends in Diagnosis and TherapyDocument13 pagesSchizophrenia Trends in Diagnosis and TherapyDoc HadiNo ratings yet
- Document-WPS OfficeDocument1 pageDocument-WPS OfficeDoc HadiNo ratings yet
- Constantino Decisionagainst Yong LiDocument19 pagesConstantino Decisionagainst Yong Liyong01776No ratings yet
- Nichqvanderbiltassessment-Full 1Document10 pagesNichqvanderbiltassessment-Full 1api-354377776No ratings yet
- Odell MillerDocument501 pagesOdell MillerRober SuarezNo ratings yet
- Mental Health & Psychiatric Nursing - Filling QuestionsDocument8 pagesMental Health & Psychiatric Nursing - Filling QuestionsFan Eli89% (9)
- University of The Assumption: Process Recording Orientation PhaseDocument4 pagesUniversity of The Assumption: Process Recording Orientation PhaseRonald BurkeNo ratings yet
- Reflection Essay Psy 230Document4 pagesReflection Essay Psy 230api-579897547No ratings yet
- Sample Intake PaperDocument5 pagesSample Intake PaperSinthia RahmanNo ratings yet
- Rants Within The Undead GodDocument700 pagesRants Within The Undead GodBenjaminCainNo ratings yet
- Hallucinations - Pseudohallucinations and ParahallucinationsDocument9 pagesHallucinations - Pseudohallucinations and ParahallucinationsMas EmmaNo ratings yet
- Existential Crisis - Symptoms, Causes, and TreatmentDocument13 pagesExistential Crisis - Symptoms, Causes, and TreatmentPratap DattaNo ratings yet
- Sample Quiz in Psychiatric NursingDocument4 pagesSample Quiz in Psychiatric NursingMerol Mae C. AdianNo ratings yet
- PsikoterapiDocument32 pagesPsikoterapiFuzti FauziaNo ratings yet
- MAPEH 7 DemoDocument5 pagesMAPEH 7 DemoMaro Mempin-TabinasNo ratings yet
- A Cognitive-Behavioral StrategyDocument9 pagesA Cognitive-Behavioral StrategyLizbeth Dey100% (1)
- Clinical PsychologistDocument3 pagesClinical PsychologisteduardpuiuNo ratings yet
- Barrowclough 2003Document8 pagesBarrowclough 2003RosarioBengocheaSecoNo ratings yet
- 512 Psychological Intervention Model'Document9 pages512 Psychological Intervention Model'Artemis LiNo ratings yet
- Trauma Symptom CheckDocument3 pagesTrauma Symptom Checkvk100% (1)
- Psychiatry McqsDocument9 pagesPsychiatry McqsSagar Karia100% (4)
- Quiz AnswersDocument77 pagesQuiz Answerssxw1828100% (2)
- Moner AloDocument9 pagesMoner AloSukanya Bhattacharyya100% (1)
- NFDN 2007 Assignment 2Document7 pagesNFDN 2007 Assignment 2api-287705803100% (2)
- Rape Trauma Syndrome NCPDocument5 pagesRape Trauma Syndrome NCPANNooonynmousNo ratings yet
- A Beautiful MindDocument5 pagesA Beautiful MindKirby Contaoi100% (3)
- Summit For Drug Rehabilitation ProgramDocument28 pagesSummit For Drug Rehabilitation ProgramMinnie AgdeppaNo ratings yet
- Importance of Positive PsychologyDocument4 pagesImportance of Positive Psychologyfaryal asifNo ratings yet
- What Is ADHDDocument6 pagesWhat Is ADHDIbnul MubarokNo ratings yet
- PHQ 9Document2 pagesPHQ 9zainasgher100% (1)
- Psychotherapy: Treatment ApproachesDocument3 pagesPsychotherapy: Treatment ApproachesShahmeer IzzatNo ratings yet