Professional Documents
Culture Documents
Workplace Readiness For Covid-19: Interim Guide
Workplace Readiness For Covid-19: Interim Guide
Uploaded by
Floyd Cedrick BalansagOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Workplace Readiness For Covid-19: Interim Guide
Workplace Readiness For Covid-19: Interim Guide
Uploaded by
Floyd Cedrick BalansagCopyright:
Available Formats
WORKPLACE READINESS
FOR COVID-19
INTERIM GUIDE
PART 3 as of MAY 26, 2020
PHILIPPINE COLLEGE OF OCCUPATIONAL MEDICINE, INC.
TABLE OF CONTENTS
NEW CLASSIFICATION OF INDIVIDUALS FOR COVID-19....................................................................... 2
WORKER EXPOSURE RISK TO COVID-19 ................................................................................................ 3
DUTIES OF THE OCCUPATIONAL HEALTH PHYSICIAN ......................................................................... 4
DUTIES OF THE OCCUPATIONAL HEALTH NURSE ................................................................................ 4
DUTIES OF THE FIRST AIDER .................................................................................................................... 4
DUTIES OF THE OCCUPATIONAL HEALTH PRACTITIONER ................................................................. 4
DUTIES OF THE HEALTH AND SAFETY COMMITTEE ............................................................................. 5
DUTIES OF THE EMPLOYERS .................................................................................................................... 5
SHARED ACCOUNTABILITY....................................................................................................................... 5
HIERACHY OF CONTROLS ......................................................................................................................... 6
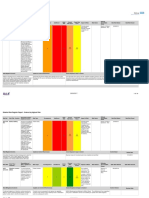
HAZARD IDENTIFICATION, RISK ASSESSMENT AND DETERMINATION OF CONTROL (HIRADC) 10
EQUALITY IN THE WORKPLACE ............................................................................................................. 18
MANAGING VISITORS, CLIENTS ETC. .................................................................................................... 18
CLEANING THE WORKPLACE ................................................................................................................. 18
SHIFT PATTERNS AND WORKING GROUPS.......................................................................................... 19
WORK-RELATED TRAVEL ........................................................................................................................ 19
COMMUNICATION AND TRAININGS ........................................................................................................ 20
INCREASE PHYSICAL AND MENTAL RESILIENCE ............................................................................... 20
RETURN TO WORK.................................................................................................................................... 21
RAPID ANTIBODY TESTING ..................................................................................................................... 29
ADVISORIES AND ISSUANCES ................................................................................................................ 30
RESOURCES: ............................................................................................................................................. 35
Philippine College of Occupational Medicine, Inc.
1
NEW CLASSIFICATION OF INDIVIDUALS FOR COVID -19
The following are the new DOH case definitions for notification which transitions the reporting of PUI and
PUM to Suspect, Probable, and Confirmed COVID-19 cases. These definitions are consistent with the latest
WHO Global Surveillance for COVID-19 disease interim guidance (as of March 20, 2020). Thus, the
COVID-19 Surveillance System, through the DOH Epidemiology Bureau, will capture and detect cases
through the enhanced influenza-like illness (ILI) and expanded severe acute respiratory infection (SARI)
sentinel surveillance systems, notification from hospital and laboratory facilities, and event-based
surveillance and response.
SUSPECT CASE is a person who is presenting with any of the conditions below:
a. All SARI cases where NO other etiology fully explains the clinical presentation.
b. Individuals with influenza-like illness (ILI):
a. With no other etiology that fully explains the clinical presentation AND history of travel to
or residence in an area that reported local transmission of COVID-19 disease during the
14 days prior to symptom onset OR
b. With contact* to a confirmed or probable case of COVID-19 disease during the 14 days
prior to the onset of symptoms
c. Individuals with fever or cough or shortness of breath or other respiratory signs or symptoms and
under any of the following conditions:
(i) aged 60 years and above,
(ii) with a comorbidity,
(iii) assessed as having high-risk pregnancy, or
(iv) a health worker.
PROBABLE CASE
A. Suspect case whom testing for COVID-19 is inconclusive
B. Suspect case who tested positive for COVID-19 but whose test was not conducted in a national or
subnational reference laboratory, or an officially accredited laboratory
CONFIRMED CASE
A. Any individual irrespective of the presence of clinical signs and symptoms who was laboratory-
confirmed for COVID-19 in a test conducted at the national reference laboratory or subnational
reference laboratory, or a DOH-certified laboratory testing facility
*Contact as defined by the WHO Global Surveillance for COVID-19 disease interim guidance (as of March
20, 2020) is a person who experienced any one of the following exposures during the 2 days before and
the 14 days after the onset of symptoms of a probable or confirmed case:
1. Face-to-face contact with a probable or confirmed case within 1 meter and for more than 15 minutes;
2. Direct physical contact with a probable or confirmed case;
3. Direct care for a patient with probable or confirmed COVID-19 disease without using proper PPE; OR
4. Other situations as indicated by local risk assessments
Note: For confirmed asymptomatic cases, the period of contact is measured as the 2 days before through
the 14 days after the date on which the sample was taken which led to confirmation.
Philippine College of Occupational Medicine, Inc.
2
WORKER EXPOSURE RISK TO COVID -19
LOW EXPOSURE RISK
• Individuals that are only in contact for a brief period of time (≦ 2minutes)
• Jobs that do not require contact with people known to be or suspected of being infected. Workers have
minimal occupational contact with the public and other coworkers.
• Practice physical distancing at all times
*Follow applicable engineering, administrative and PPE controls in your workplaces
MEDIUM EXPOSURE RISK
• Individuals are in contact for a longer period of time and are fairly distant from each other.
• Jobs that require frequent/close contact with people who may be infected, but who are not known or
suspected patients or close contacts of the same. Workers may have contact with the general public
(e.g. restaurants, high-population-density work environments, some high-volume retail settings)
including individuals returning from locations with widespread COVID-19 transmission.
• Practice physical distancing at all times
*Follow applicable engineering, administrative and PPE controls in your workplaces
HIGH EXPOSURE RISK
• Individuals are in prolonged close (more than 15 minutes) contact and may not be able to practice
physical distancing at all times. Large group of individuals in a given time (inmates)
• Jobs with a high potential for exposure to known or suspected sources of COVID-19. Healthcare
delivery, healthcare support, medical transport, and mortuary workers exposed to known or suspected
COVID-19 patients or bodies of people known to have, or suspected of having, COVID-19 at the time
of death.
*Follow applicable engineering, administrative and PPE controls in your workplaces
VERY HIGH EXPOSURE RISK
• Healthcare workers, morgue workers, performing aerosol-generating procedures on or collecting /
handling specimens from potentially infectious patients or bodies of people known to have, or
suspected of having, COVID-19 at the time of death.
*Follow applicable engineering, administrative and PPE controls in your workplaces
Philippine College of Occupational Medicine, Inc.
3
DUTIES OF THE OCCUPATIONAL HEALTH PHYSICIAN
The Occupational Health Physician, whether part-time or full-time, who shall be responsible for promoting
and maintaining the health and well-being of the workers, shall have the following duties and functions:
1. Organize, administer and maintain an occupational health service program integrating therein an
occupational safety program;
2. Continually monitor the work environment for health hazards through periodic inspection of the
workplace;
3. Prevent diseases or injury in the workplace by establishing proper medical supervision over
substances used, processes, and work environment;
4. Conserve the health of the workers through physical examinations, proper advice for placement
and health education;
5. Provide medical and surgical care to restore health and earning capacity of injured workers;
6. Maintain and analyze records of all medical cases and to prepare and submit to the employer
annual medical reports, using form DOLE/BWC/OH-47, as required by this Standards;
7. Conduct studies on occupational health within his means and resources;
8. Act as adviser to management and labor on all health matters;
9. And report directly to top management in order to be effective.
DUTIES OF THE OCCUPATIONAL HEALTH NURSE
The duties and functions of the Occupational Health Nurse are:
1. In the absence of a physician, to organize and administer a health service program integrating
occupational safety, otherwise, these activities of the nurse shall be in accordance with the
physician;
2. Provide nursing care to injured or ill workers;
3. Participate in health maintenance examination. If a physician is not available, to perform work
activities which are within the scope allowed by the nursing profession, and if more extensive
examinations are needed, to refer the same to a physician;
4. Participate in the maintenance of occupational health and safety by giving suggestions in the
improvement of working environment affecting the health and well-being of the workers; and
5. Maintain a reporting and records system, and, if a physician is not available, prepare and submit
an annual medical report, using form DOLE/BWC/HSD/OH-47, to the employer, as required by this
Standards.
DUTIES OF THE FIRST AIDER
The duties of the First Aider are to:
1. Give immediate temporary treatment in case of injury or illness, before the services of a physician
becomes available. If the case needs a physician, the first aider shall immediately call or refer the
injured to one;
2. Participate in the maintenance of occupational safety and health programs, if a member of the
Safety Committee; and
3. Maintain medical services and facilities.
DUTIES OF THE OCCUPATIONAL HEALTH PRACTITIONER
The duties of the occupational health practitioner are to:
1. Advise the employers, the workers and their representatives in the workplace the necessary
requirements in establishing and maintaining a safe and healthful working environment which will
facilitate optimal physical and mental health for workers;
Philippine College of Occupational Medicine, Inc.
4
2. Conduct periodic inspection of the workplace as required under Rule 1961.04;
3. Act as adviser to the employer, workers and their representatives in matters concerning the
organization, administration and maintenance of an occupational health program; and
4. Maintain a reporting and records system and prepare and submit an annual medical report for the
employer, using form DOLE/BWC/HSD/OH-47, as required by this Standards.
DUTIES OF THE HEALTH AND SAFETY COMMITTEE
The Health and Safety Committee is the planning and policymaking group in all matters pertaining to safety
and health. The principal duties of the Health and Safety Committee are:
1. Plans and develops accident prevention programs for the establishment.
2. Directs the accident prevention efforts of the establishment in accordance with the safety programs
safety performance and government regulations in order to prevent accidents from occurring in the
workplace.
3. Conducts safety meetings at least once a month.
4. Reviews reports of inspection, accident investigations and implementation of program.
5. Submits reports to the manager on its meetings and activities.
6. Provides necessary assistance to government inspecting authorities in the proper conduct of their
activities such as the enforcement of the provisions of this Standards.
7. Initiates and supervises safety training for employees.
8. Develops and maintains a disaster contingency plan and organizes such emergency service units
as may be necessary to handle disaster situations pursuant to the emergency preparedness
manual for establishments of the Office of Civil Defense.
DUTIES OF THE EMPLOYERS
Health and Safety committees play very important roles in eliminating work hazards. Developing workers’
interest and participation in the planning and development of safety program is the responsibility of the
employer. The employer must exercise the necessary leadership and provide support to make the program
work. The principal duties of the employer are:
1. Establishes and adopts in writing administrative policies on safety in conformity with the provisions
of this Standards outlining therein his responsibility and authority delegated.
2. Reports to the enforcing authority in two (2) copies of the policies adopted and the health and safety
organization established to carry out the program on safety and health within one month after the
organization or reorganization of the health and safety committee.
3. Reports to the enforcing authority having jurisdiction at least once in every three (3) months,
counting from January, the health and safety program of the organization out- lining the activities
undertaken including its safety performance, health and safety committee meetings and its
recommendations and measures taken to implement such recommendations.
4. Acts on recommended measures by the health and safety committee by adopting the elements of
the health and safety program in the production process or workplace and in case of non-adoption
of the Health and Safety Committee’s recommendation, to inform the committee of his reasons.
SHARED ACCOUNTABILITY
a. Health is a key development objective that is the shared accountability of the government,
communities, households, and individuals.
b. A whole-of-system, whole-of-government, whole-of-society approach is essential to develop
cohesive solutions to current and future challenges to public health and national security.
c. All efforts shall espouse the government’s strategic directions of national government-enabled,
local government-led, and people-centered response to the COVID-19 health event.
Philippine College of Occupational Medicine, Inc.
5
HIERARCHY OF CONTROLS
The Hierarchy of Controls is a system used to deploy effective controls within an organization, workplace,
or community to identify the most effective ways to control a hazard. Occupational safety and health
professionals use a framework called the “hierarchy of controls” to select ways of controlling workplace
hazards. In other words, the best way to control a hazard is to systematically remove it from the workplace,
rather than relying on workers to reduce their exposure. During a COVID-19 outbreak, when it may not be
possible to eliminate the hazard, the most effective protection measures are (listed from most effective to
least effective): engineering controls, administrative controls, safe work practices (a type of administrative
control), and PPE. There are advantages and disadvantages to each type of control measure when
considering the ease of implementation, effectiveness, and cost. In most cases, a combination of control
measures will be necessary to protect workers from exposure to SARS-CoV-2.
ELIMINATION
MOST SUBSTITUTION Requires a Installation of
EFFECTIVE physical change physical barriers,
to the sneeze guards,
workplace HEPA filters,
ventilation etc.
Protocols, policies
Change the on physical
way people distancing,
work handwashing etc.
Requires worker Depending on
to wear the worker’s risk
something based on HSC
recommendation
LEAST EFFECTIVE mmc
I. ENGINEERING CONTROLS
Isolating workers from work-related hazards. In workplaces where they are appropriate, these types of
controls reduce exposure to hazards without relying on worker behavior and can be the most cost-
effective solution to implement. Engineering controls for SARS-CoV-2 includes:
• Installing High Efficiency Particulate Air(HEPA) Filter
• Increasing ventilation rates in the work environment
• Installing physical barriers such as clear plastic sneeze guards
• Specialized negative pressure ventilation in some settings, such as for aerosol
generating procedure
• Installing permanent walled or temporary screened isolation rooms for suspect cases in
the worksites
• Installing additional hand washing/disinfecting facility or equipment in the worksite
ELIMINATION and SUBSTITUTION are the most effective under the engineering controls. However, they
tend to be the most difficult to implement and challenging as it may not be possible to eliminate and
substitute as this time.
Philippine College of Occupational Medicine, Inc.
6
ELIMINATION: Completely eliminating exposure to the hazard. Example: vaccine or cure
SUBSTITUTION: Replacing the hazard with a non-hazardous object, device or substance. (none
currently identified)
II. ADMINISTRATIVE CONTROLS
Administrative controls require action by the worker and employer. Changes made to the way that people
work. Typically, administrative controls are changes in work policy or procedures standards, and processes
to reduce or minimize exposure to a hazard. Examples of administrative controls for SARS-CoV-2 include:
• Identification of vulnerable workers based on Occupational Health Services data
• Encouraging sick workers to stay at home.
• Isolation area (not the clinic) preferably with good ventilation
• Minimizing contact among workers, clients, and customers by replacing face-to-face meetings
with virtual communications and implementing telework if feasible.
• Establishing alternating days or extra shifts that reduce the total number of employees in a facility
at a given time, allowing them to maintain distance from one another while maintaining a full
onsite work week.
• Discontinuing nonessential travel to locations with ongoing COVID-19 outbreaks.
• Developing emergency communications plans, including a forum for answering workers’ concerns
and internet-based communications, if feasible.
• Providing workers with up-to-date education and training on COVID-19 risk factors and protective
behaviors (e.g., cough etiquette and care of PPE).
• Training workers who need to use protecting clothing and equipment how to put it on, use/wear it,
and take it off correctly, including in the context of their current and potential duties. Training
material should be easy to understand and available in the appropriate language and literacy
level for all workers.
• Site specific preventive materials in place and with adequate supply
• Sanitation, disinfection and disposal measures and protocols
• Physical distancing protocols
• Health screening protocol with health screening daily
• Self-quarantine and return to work protocol
• Labor relations alignment and education on the pandemic response plan for their cooperation
• Communication and employee trainings and education
• Facility Signages
• Virtual meetings, site visits, and training through the use of web conferencing applications or
video calls.
• work from home, alternative workplace accommodation, working hour shifts.
• Hotline, call center, telemedicine services
• On-Site or Near-Site accommodation and Transport/shuttle services
III. PERSONAL PROTECTIVE EQUIPMENT (PPE)
Refers to protective garments or equipment worn by individuals to increase personal safety from infectious
agents. PPE is only one effective measure within a package of administrative and environmental and
engineering controls, as described in WHO’s Infection prevention and control of epidemic- and pandemic-
prone acute respiratory infections in healthcare.
PPE protects the user against health or safety risks at work. It can include items such as safety helmets,
gloves, eye protection, high-visibility clothing, safety footwear and safety harnesses. It also includes
respiratory protective equipment, such as face masks.
Philippine College of Occupational Medicine, Inc.
7
During an outbreak of an infectious disease, such as COVID-19, recommendations for PPE specific to
occupations or job tasks may change depending on geographic location, updated risk assessments for
workers, and information on PPE effectiveness in preventing the spread of COVID-19.
Detailed listing of the different minimum requirements of PPE based on risks can be seen at
https://www.doh.gov.ph/sites/default/files/health-update/ao2020-0015.pdf and the rational use of personal
protective equipment for coronavirus disease https://www.who.int/publications-detail/rational-use-of-
personal-protective-equipment-for-coronavirus-disease-(covid-19)-and-considerations-during-severe-
shortages
Philippine College of Occupational Medicine, Inc.
8
COMMUNITY PROTECTIVE EQUIPMENT – Equipment worn by a person to prevent community spread
from an asymptomatic carrier of COVID-19. This is the last line of defense and its effectiveness depends
on community use and their ability to adopt disinfection, distancing, and hygiene practices.
FACE COVERINGS
A face covering can be very simple and may be worn in enclosed spaces where social distancing isn’t
possible. It just needs to cover your mouth and nose. It is not the same as a face mask, such as the surgical
masks or respirators used by health and care workers. Similarly, face coverings are not the same as the
PPE used to manage risks like dust and spray in an industrial context. Supplies of PPE, including face
masks, must continue to be reserved for those who need them to protect against risks in their workplace,
such as health and care workers, and those in industrial settings like those exposed to dust hazards.
It is important to know that the evidence of the benefit of using a face covering to protect others is weak
and the effect is likely to be small, therefore face coverings are not a replacement for the other ways of
managing risk, including minimizing time spent in contact, using fixed teams and partnering for close-up
work, and increasing hand and surface washing. These other measures remain the best ways of managing
risk in the workplace and government would therefore not expect to see employers relying on face coverings
as risk management for the purpose of their health and safety assessments.
Philippine College of Occupational Medicine, Inc.
9
HAZARD IDENTIFICATION, RISK ASSESSMENT AND DETERMINATION OF CONTROL
(HIRADC)
The risks from SARS-CoV-2, the virus that causes Coronavirus Disease 2019 (COVID-19), for workers
depends on how extensively the virus spreads between people; the severity of resulting illness; pre-existing
medical conditions workers may have; and the medical or other measures available to control the impact
of the virus and the relative success of these measures.
Worker risk of occupational exposure to SARS-CoV-2 during a pandemic may depend in part on the
industry type and the need for contact within a meter of people known to be, or suspected of being, infected
with SARS-CoV-2. Other factors, such as conditions in communities where employees live and work, their
activities outside of work (including travel to COVID-19-affected areas), and individual health conditions,
may also affect workers' risk of getting COVID-19 and/or developing complications from the illness.
A risk assessment is not about creating huge amounts of paperwork, but rather about identifying sensible
measures to control the risks in your workplace. Whether you have fewer than five workers, or are self-
employed, your risk assessment will help you decide whether you have done everything you need to do.
I. IDENTIFY HAZARDS
Look around your workplace and think about what may cause harm (these are called hazards).
Think about:
• How people work and how plant and equipment are used.
Philippine College of Occupational Medicine, Inc.
10
• What chemicals and substances are used.
• What safe or unsafe work practices exist.
• The general state of your premises.
Look back at your accident and ill health records as these can help you identify less obvious hazards. Take
account of non-routine operations, such as maintenance, cleaning or changes in production cycles.
Think about hazards to health, such as manual handling, use of chemicals and causes of work-related
stress. For each hazard, think about how employees, contractors, visitors or members of the public might
be harmed.
VULNERABLE WORKFORCE
High risk pregnancy, 60 years old and above, any age with co-morbidities or pre-existing illness
(uncontrolled hypertension, uncontrolled diabetes, recurrent asthma attacks, COPD, cancer, blood
dyscrasias, chronic liver and kidney diseases or with immunocompromised status)
Employers are highly encouraged to allow work from home, alternative workplace accommodation,
working hour shifts.
Comorbidity at risk of COVID-19 exacerbation - presence of one or more additional conditions co-
occurring with (that is, concomitant or concurrent with) a primary condition that increases an individual’s
risk for if afflicted by COVID-19. This includes immunocompromised individuals (such as but not limited to
those with cancer, HIV/AIDS and other autoimmune disorders) and individuals with chronic conditions (such
as but not limited to hypertension, diabetes mellitus, and chronic kidney disease).
II. ASSESS THE RISKS
Once you have identified the hazards, decide how likely it is that someone could be harmed and how
serious it could be. This includes taking reasonable steps to protect your workers and others from
coronavirus. This is called a risk assessment and it’ll help you manage risk and protect people.
This is assessing the level of risk.
Decide:
• Who might be harmed and how.
• What have you done to control the risks.
• What further action you need to take to control the risks.
• Who needs to carry out the action.
• When the action is needed by.
You must:
• Identify what work activity or situations might cause transmission of the virus;
• Think about who could be at risk;
• Decide how likely it is that someone could be exposed;
• Act to remove the activity or situation, or if this isn’t possible, control the risk.
III. CONTROL THE RISKS
To reduce workplace risk to the lowest reasonably practicable level by taking preventative measures.
Look at what you’re already doing, and the controls you already have in place. Ask yourself:
• Can I get rid of the hazard altogether?
• If not, how can I control the risks so that harm is unlikely?
Philippine College of Occupational Medicine, Inc.
11
If you need further controls, consider:
• Redesigning the job.
• Replacing the materials, machinery or process.
• Organizing your work to reduce exposure to the materials, machinery or process.
• Identifying and implementing practical measures needed to work safely.
• Providing personal protective equipment and making sure workers wear it.
Put the controls you have identified in place. You’re not expected to eliminate all risks, but you need to do
everything ‘reasonably practicable’ to protect people from harm. This means balancing the level of risk
against the measures needed to control the real risk in terms of money, time or trouble.
• Administrative controls include ensuring resources for infection prevention and control (IPC)
measures, such as appropriate infrastructure, the development of clear IPC policies, facilitated
access to laboratory testing, appropriate triage and placement of patients, adequate staff-to-patient
ratios, and training of staff.
• Environmental and engineering controls aim at reducing the spread of pathogens and the
contamination of surfaces and inanimate objects. They include providing adequate space to allow
social distance of at least 1-2 m to be maintained between patients and between patients and
health care workers and ensuring the availability of well-ventilated isolation rooms for patients with
suspected or confirmed COVID-19.
WORKPLACE PREPARE DNESS
PRIOR TO GOING BACK TO WORK
Health and safety committee together with employers (top management) human resources, line managers,
pandemic response team, labor union and other key people to work together to address the pandemic
concerns.
Philippine College of Occupational Medicine, Inc.
12
• Recommendation and implementation of controls.
• Coordination of OH personnel and safety officer in ensuring control measures are in place before
lifting of the ECQ and are implemented thereafter.
WORK AREA
You should think about how you can organize your work area so that you can keep people at least 1- 2m
apart, where possible:
• Physically arrange work areas to keep people 1- 2 m apart;
• Where you cannot keep a 2 m physical distance, you should think about:
o Mark areas using floor paint or tape to help people keep a 1-2 m distance;
o Provide signage to remind people to keep a 1-2 m distance;
o Avoid people working face-to-face, for example working side-by-side.
• Assigning one person per work area;
• Reducing the number of people in the work area;
• Assigning and keeping people to shift teams (sometimes known as a cohort), that is people on the
same shift working in the same teams, to limit social interaction;
• Keeping the number of people working less than 2 m apart to a minimum;
• Using screens to create a physical barrier between people.
Philippine College of Occupational Medicine, Inc.
13
You need to think about how to keep the work area clean and prevent transmission. You should consider
disinfecting frequently touched surfaces and objects such as but not limited to tables, doorknobs, light
switches, phones, toilets among other at least every 2 hours.
MOVING AROUND
You need to think about how people travel through work environments.
• Permit only essential trips within buildings, sites and properties, to maintain social distancing as
much as possible.
• Restrict the amount that people rotate between jobs and equipment.
• Limit the number of people who use lifts and work vehicles.
• Reduce the number of people in high traffic areas including lifts, corridors, turnstiles and
walkways.
• Mark areas using floor paint or tape to help people keep a 1-2 m distance.
• Consider introducing temporary pedestrian walkways to allow people to maintain social distancing
when moving around.
Philippine College of Occupational Medicine, Inc.
14
COMMON AREAS
You should review the common areas used in your business including canteens, toilets, showers, and
changing facilities. You need to think about:
• Physically moving tables/chairs so they are 1-2 m apart;
• Staggering breaktimes so that people are not using break rooms, canteens, rest areas or changing
facilities at the same time to maintain social distancing;
• Where this is not possible, creating additional space for people to take their breaks in;
• Marking areas using floor paint or tape to help people keep a 1-2 m distance;
• Using outside areas for breaks if the locations are suitable and it is safe to do so;
• Encouraging workers to stay on-site during working hours.
Where you cannot keep a 1-2 m physical distance, you need to think about how to keep common areas
clean and prevent transmission as a result of touching of contaminated surfaces. You should think about:
• How frequently you need to clean the common areas of your business;
• Identifying objects and surfaces that are touched regularly and decide how frequently you clean
them;
• Setting clear guidance for the use of rest areas, toilets, showers, and changing facilities to make
sure they are kept clean.
GOOD HYGIENE
You need to think about:
• Ensuring that you have handwashing facilities that provide running water, soap and paper towels;
• Providing hand sanitizer in addition to washing facilities;
• Using signs and posters to increase awareness of good handwashing technique;
• Providing regular reminders on avoiding touching your face and to cough/sneeze into your arm;
• Providing hand sanitizer in multiple locations in addition to washrooms;
• Setting clear guidance for the cleaning of toilets, showers and changing facilities to make sure they
are kept clean;
Philippine College of Occupational Medicine, Inc.
15
• Setting clear guidance on how to handle goods, merchandise and materials and when cleaning
procedures need to be followed.
Philippine College of Occupational Medicine, Inc.
16
Philippine College of Occupational Medicine, Inc.
17
INFORMATION AND GUIDANCE
You need to think about:
• Providing workers and others with information on procedures, guidance or ways of working that
have been introduced;
• Sharing this information with them before they start work;
• Sharing this information with others who are not your workers (for example visitors, customers or
contractors)
• How you will pass information and guidance to people who don’t have English as their first language
and others who may struggle with written and verbal communication;
• Holding conversations with your workers, listening to and acting on their concerns.
EQUALITY IN THE WORKPLACE
• In applying this guidance, employers should be mindful of the particular needs of different groups
of workers or individuals.
• It is breaking the law to discriminate, directly or indirectly, against anyone because of a protected
characteristic such as age, sex or disability.
• Employers also have particular responsibilities towards disabled workers and those who are new
or expectant mothers.
MANAGING VISITORS, CLIENTS ETC.
• Encouraging visits via remote connection or remote working for visitors where this is an option.
• Limiting the number of visitors at any one time.
• Determining if schedules for essential services and contractor visits can be revised to reduce
interaction and overlap between people, for example, carrying out services at night.
• Maintaining a record of all visitors, if this is practical.
CLEANING THE WORKPLACE
BEFORE REOPENING:
To make sure that any site or location that has been closed or partially operated is clean and ready to
restart, including:
• An assessment for all sites, or parts of sites, that have been closed, before restarting work.
• Cleaning procedures and providing hand sanitizer, before restarting work.
• Checking whether you need to service or adjust ventilation systems, for example, so that they do
not automatically reduce ventilation levels due to lower than normal occupancy levels.
• Most air conditioning systems do not need adjustment, however where systems serve multiple
buildings or you are unsure, advice should be sought from your heating ventilation and air
conditioning (HVAC) engineers or advisers.
• Positive pressure systems can operate as normal.
KEEPING THE WORKPLACE CLEAN:
To keep the workplace clean and prevent transmission by touching contaminated surfaces.
• Frequent cleaning of work areas and equipment between uses, using your usual cleaning products.
Philippine College of Occupational Medicine, Inc.
18
• Frequent cleaning of objects and surfaces that are touched regularly, such as door handles, pump
handles and printers, and making sure there are adequate disposal arrangements.
• Clearing workspaces and removing waste and belongings from the work area at the end of a shift.
• If you are cleaning after a known or suspected case of COVID-19 then you refer to the specific
guidance.
HANDLING GOODS, MERCHANDISE AND OTHER MATERIALS, AND ONSITE VEHICLES
To reduce transmission through contact with objects that come into the workplace and vehicles at the
worksite.
• Cleaning procedures for the parts of shared equipment you touch after each use, thinking about
equipment, tools and vehicles, for example, pallet trucks and forklift trucks.
• Encouraging increased handwashing and introducing more handwashing facilities for workers
handling goods and merchandise or providing hand sanitizer where this is not practical.
• Regular cleaning of vehicles that workers may take home. Regular cleaning of reusable delivery
boxes.
SHIFT PATTERNS AND WOR KING GROUPS
To change the way work is organized to create distinct groups and reduce the number of contacts each
worker has.
• As far as possible, where people are split into teams or shift groups, fixing these teams or shift
groups so that where contact is unavoidable, this happens between the same people.
• Identifying areas where people have to directly pass things to each other, for example, job
information, spare parts, samples, raw materials, and find ways to remove direct contact, such as
through the use of drop-off points or transfer zones.
WORK-RELATED TRAVEL
CARS, ACCOMODATION AND VISITS
• Minimizing non-essential travel – consider remote options first.
• Minimizing the number of people travelling together in any one vehicle, using fixed travel partners,
increasing ventilation when possible and avoiding sitting face-to-face.
• Cleaning shared vehicles between shifts or on handover.
• Where workers are required to stay away from their home, centrally logging the stay and making
sure any overnight accommodation meets social distancing guidelines.
• There should be passenger logs for every scheduled trip for contact tracing.
DELIVERIES AND OTHER SITES
To help workers delivering to other sites such as factories, logistics sites or customers’ premises to maintain
social distancing and hygiene practices.
• Putting in place procedures to minimize person-to-person contact during deliveries to other sites.
• Maintaining consistent pairing where two-person deliveries are required.
• Minimizing contact during payments and exchange of documentation, for example, by using
electronic payment methods and electronically signed and exchanged documents.
Philippine College of Occupational Medicine, Inc.
19
COMMUNICATION AND TRAININGS
To make sure all workers understand COVID-19 related safety procedures.
UPON RETURNING TO WORK
• Providing clear, consistent and regular communication to improve understanding and consistency
of ways of working.
• Engaging with workers and worker representatives through existing communication routes to
explain and agree any changes in working arrangements.
• Developing communication and training materials for workers prior to returning to site, especially
around new procedures for arrival at work.
CONTINUING COMMUNICATIONS AND SIGNAGES
To make sure all workers are kept up to date with how safety measures are being implemented or updated.
• Ongoing engagement with workers, including through trade unions or employee representative
groups to monitor and understand any unforeseen impacts of changes to working environments.
• Awareness and focus on the importance of mental health at times of uncertainty. The government
has published guidance on the mental health and wellbeing aspects of coronavirus (COVID-19).
• Using simple, clear messaging to explain guidelines using images and clear language, with
consideration of groups for which English may not be their first language.
• Using visual communications, for example, whiteboards or signage, to explain changes to
production schedules, breakdowns or materials shortages to reduce the need for face-to-face
communications.
• Communicating approaches and operational procedures to suppliers, customers or trade bodies to
help their adoption and to share experience.
INCREASE PHYSICAL AND MENTAL RESILIENCE
a. Ensure access to basic needs of individuals, including food, water, shelter and sanitation.
b. Support adequate nutrition and diets based on risk.
c. Encourage appropriate physical activity for those with access to open spaces as long as physical
distancing is practiced.
d. Discourage smoking and drinking of alcoholic beverages.
e. Protect the mental health and general welfare of individuals.
f. Promote basic respiratory hygiene and cough etiquette.
g. Protect essential workforce through provision of food, PPE and other commodities, lodging, and
shuttle services as necessary.
h. Provide financial and healthcare support for workforce who contracted COVID-19 through
transmission at work.
i. Limit exposure of most at risk population groups, such as through limitation in entry or
prioritization in service or provision of support.
j. Provide appropriate social safety net support to vulnerable workforce for the duration of the
COVID-19 health event.
Philippine College of Occupational Medicine, Inc.
20
RETURN TO WORK
Philippine College of Occupational Medicine, Inc.
21
Philippine College of Occupational Medicine, Inc.
22
Philippine College of Occupational Medicine, Inc.
23
Philippine College of Occupational Medicine, Inc.
24
PHILIPPINE COLLEGE OF OCCUPATIONAL MEDICINE, INC.
Specialty Society of the Philippine Medical Association
Under the Division of the Philippine Academy of Family Physicians,
Affiliate Member of International Commission on Occupational Health (ICOH) and
Asian Association of Occupational Health (AAOH)
Accredited by:
Philippine Health Insurance Corporation, Department of Labor and Employment, and
Professional Regulation Commission as CPD Provider
May 19, 2020
OFFICERS: 2020-2021
Health and Safety of Workers and Impact to Employers:
Phil M. Pangilinan, MD
President On behalf of the Philippine College of Occupational Medicine, Inc., I EXTEND TO
EVERYONE LISTENING Greetings of Health and Safety!
Margaret L. Leachon, MD
Vice-President We IN THE COLLEGE works with management and workers as a team to
safeguard, promote, maintain, and enhance workers health, wellness, and safety.
Anna Sofia Victoria S. Fajardo, MD
We take responsibility for the care and welfare of the community and in conserving
Secretary
the environment for future generations.
Marilen Evangeline M. Cruz, MD
As Occupational Health Physicians, it is our duty together with the Health and
Treasurer
Safety Committee to prevent any work related illnesses or injuries that may happen
Arnold P. Tabun, Jr., MD in the workplace, and promote Occupational Health Services and Occupational
Auditor Health and Safety Programs in every Workplaces. As Stated in the Occupational
Safety Health standard of the Philippines Rule 1960 “Occupational Health Services”
Neil P. Rodrigo, MD we are tasked to assess the worker’s physical, emotional, and psychological state
PRO as well as his other existing conditions in order to facilitate proper placement and
ensure suitability of individuals according to their physical capabilities, mental
abilities and emotional make up for work which they can perform with acceptable
degree of efficiency without endangering their own health and safety and that that of
BOARD OF DIRECTORS: their co-workers. We act as consultants and advisers to Employers when it comes to
safety and health.
Joseph L. Alunes, MD
Ricardo T. Balagot, MD With RA 11058, OSH Law and its IRR DO 198-18 “AN ACT STRENGHTENING
Roberto Arturo P. Del Prado III, MD
COMPLIANCE OF OCCUPATIONAL SAFETY AND HEALTH STANDARDS AND
Evelio A. Echavez, Jr., MD
PROVIDING PENALTIES FOR VIOLATIONS THEREOF” We are mandated by law
Jude O. Jundis, MD
to maintain a safe and healthy workforce who are integral aspects of Nation Building
Claire B. Miñoza, MD
Jovencio J. Padilla, MD and ensure a safe and healthful workplace for all working people, by affording them
Reynold M. Sta Ana, MD full protection against all hazards in their work environment.
Maria Antonia O. Yamamoto, MD
The impact of this Pandemic to Employers is very alarming. Companies that are
Edmyr M. Macabulos, MD trying to recover from economic devastation are forced to suffer further by paying for
Immediate Past President costly and potentially misleading tests. This Rapid test kits has its advantages,
disadvantages, and limitations. These tests do not detect the virus, just the
antibodies produced against the virus thus it is not recommended as a screening
tool for early infection let alone used to screen workers prior to return to work in the
workplace.
We support the statement made by the WHO, PMA, PSMID, PCP, PAFP, PSPHP,
PSGIM, Covid 19 Action Network, and other stakeholders on their stand in the
proper use of rapid anti body test for clinical or public health purpose.
Thank You.
PHIL M. PANGILINAN, MD, MHA, FPSMS, DPCOM, PAFP
National President
Room 106 Philippine Medical Association Building, North Avenue, Quezon City
+632- 89297741 * Mobile: +639989545338 / +639258175026 / +639176276246
pcomsecretariat@gmail.com / pcomsecretatriat@yahoo.com / pcom@skydsl.com.ph
Website: www.pcom.ph
Philippine College of Occupational Medicine, Inc.
25
PHILIPPINE COLLEGE OF OCCUPATIONAL MEDICINE, INC.
Specialty Society of the Philippine Medical Association
Under the Division of the Philippine Academy of Family Physicians,
Affiliate Member of International Commission on Occupational Health (ICOH) and
Asian Association of Occupational Health (AAOH)
Accredited by:
Philippine Health Insurance Corporation, Department of Labor and Employment, and
Professional Regulation Commission as CPD Provider
May 20, 2020
Position Statement on Rapid Test Kits
OFFICERS: 2020-2021
Phil M. Pangilinan, MD The Philippine College of Occupational Medicine recognizes the urgent need to look into
President timely and accurate testing as an essential part in slowing down the pandemic and
hopefully will be able to detect asymptomatic cases that could hinder the further spread of
the virus.
Margaret L. Leachon, MD
Vice-President To date, these IgG/IgM tests aka rapid test kits has its advantages, disadvantages and
limitations. It is dependent on the detection of antibodies made by the patient in response to
Anna Sofia Victoria S. Fajardo, MD SARS-COV-2, the virus that causes COVID-19 disease. These tests do not detect the virus
Secretary and thus it is not recommended as screening tool for early infection let alone used to
screen workers prior to the return to work in the workplace.
Marilen Evangeline M. Cruz, MD These antibody tests may have a place in detecting unrecognized past infection and
Treasurer immunity however that role needs to be rigorously evaluated. PCOM acknowledges that
further review and assessment following closely the advice of leading international and
Arnold P. Tabun, Jr., MD local institutes, tests which have been validated through proper quality control before
Auditor deciding if at all they have a place in our overall approach to managing COVID -19 at the
workplace.
Neil P. Rodrigo, MD However, we also acknowledge the DOH DM 2020-0220 interim guidelines on return to
PRO work issued last May 11, 2020 stating the "option" of using the FDA approved rapid
antibody tests among representative samples for baseline can also be conducted up to
every 14 days. And the Rapid Antibody based test is only an adjunct test and shall not be
used as a standalone test to definitely diagnose or rule out COVID-19" ( ref: DOH DM
2020-0180 revised interim guidelines on expanded testing for COVID19, April 17 2020)
BOARD OF DIRECTORS:
That being said the use of these test kits as a mandatory protocol for companies before
Joseph L. Alunes, MD returning back to work is not advocated. The DOLE DTI interim guidelines also states that
Ricardo T. Balagot, MD e e " a e e f COVID 19 c f h he DOH c .
Roberto Arturo P. Del Prado III, MD
We support the statements made by the WHO, Philippine Medical Association, Philippine
Evelio A. Echavez, Jr., MD College of Physicians, Philippine Society of Microbiology and Infectious Diseases,
Jude O. Jundis, MD Philippine Society of General Internal Medicine, Philippine Academy of Family Physicians,
Claire B. Miñoza, MD Philippine Society of Public Health Physicians, and COVID-19 Action Network on their
Jovencio J. Padilla, MD stand in the use of rapid antibody tests for clinical or public health purposes. These tests
Reynold M. Sta Ana, MD have yet to be thoroughly evaluated backed up with evidence based medicine.
Maria Antonia O. Yamamoto, MD
Edmyr M. Macabulos, MD
JOSEPH L. ALUNES, MD, FPCOM
Immediate Past President National Director
RICARDO T. BALAGOT, MD, FPCOM
National Director
ROBERTO ARTURO P. DEL PRADO III, MD, MOH, MHA, FPCOM
National Director
EVELIO A. ECHAVEZ JR., MD, FPCOM
National Director
Room 106 Philippine Medical Association Building, North Avenue, Quezon City
+632- 9297741 * Mobile: +639989545338 / +639258175026 / +639176276246
pcomsecretariat@gmail.com / pcomsecretatriat@yahoo.com / pcom@skydsl.com.ph
Website: www.pcom.ph
Philippine College of Occupational Medicine, Inc.
26
Philippine College of Occupational Medicine, Inc.
27
Philippine College of Occupational Medicine, Inc.
28
RAPID ANTIBODY TESTING
The decision to test should be based on clinical and epidemiological factors, prioritizing those with risk and
especially exposure. Screening protocols should be adapted to local capacity and setting, considering
resources are limited in our country, choosing the screening test or strategy could make or break our
response to this pandemic.
PCR or Polymerase chain reaction remains the “gold standard” of test for COVID. Serological tests or
Rapid Antibody tests can have a potential use in retrospective assessment of attack rates which is the
number of new cases of the disease at a given time over population at start of time interval. It can also be
used for research and surveillance but are not recommended for case detection. This will be true in areas
where validation and standardization process for this test is available, which is not the case in our country
at present.
Furthermore, antibody testing needs paired serum sampling to aid its validity. Another very important
limitation of this test is its high cross reactivity with other viruses especially the Coronaviruses, hence
challenging its specificity. A table below also describes the variability of the test’s sensitivity depending on
the timing which is very tedious to document in the midst of asymptomatics.
Upon evaluation of limited available data on Rapid Antibody testing, a joint statement was made by the
experts of the Philippine Medical association, the Philippine College of Occupational Medicine. Philippine
College of Physicians, Philippine Society for Microbiology and Infectious Disease, Philippine Academy of
Family Physicians, Philippine Society of General Internal Medicine, Philippine Society of Public Health
Physicians to still advocate and recommend the 14 – day clinical test for screening of return to work.
Philippine College of Occupational Medicine, Inc.
29
ADVISORIES AND ISSUANCES
INTER-AGENCY TASK FORCE
• Omnibus Guidelines on the Implementation of Community Quarantine in the Philippines
DEPARTMENT MEMORANDUM
• DM 2020-0171:Interim Guidelines on Surge Capacity Management of All Health Facilities during
the COVID-19 Pandemic
• DM 2020-0180: Revised Interim Guidelines on Expanded Testing for COVID-19
• DM 2020-0189: Updated Guidelines on Contact Tracing of Close Contacts of Confirmed
Coronavirus Disease (COVID-19) Cases
• DM 2020-0191: Designation of Selected Regional TB Culture Laboratories for GeneXpert
Diagnosis of Coronavirus Disease 2019 (COVID-19)
• DM 2020-0188: Interim Guidelines on the Zoning of COVID-19 Laboratories
• DM 2020-0208: Interim Guidelines on Enhancing the Infection Prevention and Control Measures
through Engineering and Environmental Controls in All Health Facilities and Temporary
Treatment and Monitoring Facilities during the COVID-19 Pandemic
• DM 2020-0220: Interim Guidelines on the Return-to-Work
• DM 2020-0185: Interim Guidelines for Nursing Service in Temporary Treatment and Monitoring
Facilities for the Management of Suspect, Probable, and Confirmed Cases of Coronavirus
Disease 2019 (COVID-19)
• DM 2020-0170: Interim Guidelines on the Management of Health Care Waste in Health Facilities,
Community Quarantine Units and Temporary Treatment and Monitoring Facilities with cases of
Coronavirus Disease 2019 (COVID-19)
• DM 2020-0162 Interim Guidelines on the Accommodation Arrangement for Health Workers during
COVID-19 Health Emergency Response Period
• DM 2020-0161: Interim Guidelines on Step Down Care for COVID-19 Response
• DM 2020-0160: Interim Guidelines on Management for the National Capital Region Mega
Temporary Treatment and Monitoring Facilities in the Philippine International Convention Center
(PICC), World Trade Center (WTC), Rizal Memorial Coliseum (RMC), Ninoy Aquino Stadium, and
Philippine Arena
• DM 2020-0157: Guidelines on Cleaning and Disinfection in Various Settings as an Infection
Prevention and Control Measure Against COVID-19
• DM 2020-0178: Interim Guidelines on Health Care Provider Networks during the COVID-19
Pandemic
• DM 2020-0182: Revised Interim Guidelines on the Mass Repatriation and Mandatory Quarantine
of Land-based Overseas Filipinos (OFs) during the Coronavirus Disease 2019 (COVID-19)
Pandemic
• DM 2020-0181: Revised Interim Guidelines on the Mass Repatriation and Mandatory Quarantine
of Overseas Filipinos (OF) Working in Cruise Ships during the Coronavirus Disease 2019
(COVID-19) Pandemic
• DM 2020-0090: Interim Guidelines on the Management of PUM suspected with COVID19 for
Home Quarantine; Feb 17, 2020
• DM 2020- 108: Guidelines for management of patients with possible and Confirmed COVID19;
March 11, 2020
• DM 2020-125: Adoption of the health facilities preparedness and Response Checklist for the
Novel Corona Virus ARD 2019 ( COVID 2019) Response in Hospitals and other health facilities ;
March 17, 2020
• DM 2020-0157: Guidelines on Cleaning and Disinfection in Various Settings as an Infection
Prevention and Control Measure Against COVID-19
• DM 2020-0160: Interim Guidelines on Management for the National Capital Region Mega
Temporary Treatment and Monitoring Facilities in the Philippine International Convention Center
Philippine College of Occupational Medicine, Inc.
30
(PICC), World Trade Center (WTC), Rizal Memorial Coliseum (RMC), Ninoy Aquino Stadium, and
Philippine Arena
• DM 2020-0161: Interim Guidelines on Step Down Care for COVID-19 Response
• DM 2020-0162: Interim Guidelines on the Accommodation Arrangement for Health Workers
during COVID-19 Health Emergency Response Period; April 4 2020
• DM 2020-0170: Interim Guidelines on the Management of Health Care Waste in Health Facilities,
Community Quarantine Units and Temporary Treatment and Monitoring Facilities with cases of
Coronavirus Disease 2019 (COVID-19)
ADMINISTRATIVE ORDER
• AO 2020-0012: Guidelines for the Inclusion of COVID-19 in the List of Notifiable Diseases for
Mandatory Reporting to the Department of Health
• AO 2020-0013: Revised AO2020-0012 Guidelines for the Inclusion of COVID-19 in the List of
Notifiable Diseases for Mandatory Reporting to the Department of Health dated 17 March 2020
• AO 2020-0014: Guidelines in Securing a License to Operate a COVID-19 Testing Laboratory in
the Philippines
• AO 2020-0015: Guidelines on the Risk-based Public Health Standards for COVID-19 Mitigation
• AO 2020-0016: Minimum Health Capacity Standards for COVID-19 Preparedness and Response
Strategies
• AO 2020-0018: Guidelines on Contracting Province-Wide & City-Wide Health Systems
• AO 2020-0019: Guidelines on the Service Delivery Design of Health Care Provider Networks
JOINT MEMORANDUM CIRCULAR
• JMC 2020-0002: Privacy Guidelines on the Processing and Disclosure of COVID-19 Related
Data for Disease Surveillance and Response
• JMC 2020-0016: Guidelines on the Use of Telemedicine in COVID-19 Response
• JMC No. 2020-0001: Price Freeze Under a State of Calamity throughout the Philippines due to
COVID-19
• JMC No. 2020-03: Guidelines on the Implementation of Joint DOH-DTI-DA-DOJ-BOC Circular
No. 001 (S2020) on Seizure and Related Proceedings for Goods Necessary to address the
COVID-19 Public Health Emergency pursuant to RA 7581, as amended by RA 10623, otherwise
known as the Customs Modernization and Tariff Act in relation to the Bayanihan to Health As One
Act
DEPARTMENT CIRCULAR:
• DC 2020-0014 Directive to All Suspected nCoV Patients Seeking Consultations Treatment at
Hospitals
• DC 2020-0023 Reiteration of Directive to Attend to All Suspected 2019-nCoV Patients Seeking
Consultations at Hospitals
• DC 2020-0034 Guidelines at All Seaports for Prevention and Spread of 2019-nCoV:
• DC 2020-0038 Reiteration of the Price Freeze of Essential Emergency Medicines due to the
2019-nCoV Health Event
• DC 2020-0039 Reiteration of the Interim Guidelines on 2019-nCoV Response in the Workplace
• DC 2020-0040 Reiteration of the Interim Guidelines on Repatriation of Overseas Filipinos due to
2019-nCoV
• DC 2020-0041 Reiteration of the Interim Guidelines on 2019-nCoV Response in Residential
Communities
• DC 2020-0042 Reiteration of the Interim Guidelines on 2019-nCoV Response in Schools and
Higher Education Institutions
Philippine College of Occupational Medicine, Inc.
31
• DC 2020-0043 Reiteration of the Interim Guidelines on 2019-nCoV Response in Hotels and Other
Similar Establishments
• DC 2020-0044 Public Advisory Nos. 1-6 on 2019-nCoV
• DC 2020-0045 Public Advisory No. 8 on the Use of Masks
• DC 2020-0046 Public Advisory No. 7 on Concerts and Other Public Events and Gatherings
• DC 2020-0047 Reiteration of the Guidelines on the Disposal and Shipment of the Remains of
Confirmed Cases of 2019-nCoV
• DC 2020-0048 Reiteration of the Interim Guidelines on Contact Tracing for Confirmed 2019-nCoV
• DC 2020-0049 Reiteration of the Interim Guidelines for 2019-nCoV Response in Hospitals and
Other Health Facilities
• DC 2020-0067 ICD-10 Code for COVID-19 (Previously Known as 2019-nCoV)
• DC 2020-0068 Public Advisory No. 9 Lifting of Travel Restriction to Taiwan
• DC 2020-0069 Public Advisory No. 11 Reminders for Sending Specimens to the RITM for
COVID-19
• DC 2020-0070 Public Advisory No. 10 Non-Refusal of Level 2 and 3 Public and Private Hospitals
to PUI for COVID-19
• DC 2020-0071 Revised Decision Tool for the Assessment and Management of COVID-19
• DC 2020-0080 Revised Decision Tool for the Assessment and Management of COVID-19
• DC 2020-0105 Public Advisory No. 12 Interim Guidelines on the Management of PUM suspected
with COVID-19
• DC 2020-0106 Use of WHO Interim Guidelines for Health Workers Exposure Risk Assessment
and Management in the Context of COVID-19
• DC 2020-0107 Public Advisory No. 13 Updated Guidelines for Management and Referral of
Suspected and Confirmed COVID-19 Cases Under Code Red
• DC 2020-0108 Public Advisory No. 14 - Clarification on Management and Referral of Close
Contacts of Confirmed COVID-19
• DC 2020-0130 Public Advisory No. 15 Guidance on Gatherings for the Public and Event
Organizers
• DC 2020-0131 Public Advisory No. 16 Guidance for Institutions if a PUI or a Confirmed COVID-
19 Case is Detected in the Workplace
• DC 2020-0133 Reiteration of the Price Freeze of Essential Medicines and Medical Devices Due
to the COVID-19 Health Event
• DC 2020-0141 Public Advisory No. 17 Guidance on the Conduct of Daily Prayer (Salah) for
Filipinos with Islamic Faith
• DC 2020-0142 Public Advisory No. 18 Suggested Retail Price of N-88 Face Mask
• DC 2020-0143 Public Advisory No. 20 - Covid-19 Laboratory Testing
• DC 2020-0144 Public Advisory No. 19 Prohibition of Hoarding Drugs and Medicines, Profiteering
and Other Acts Committed in Trade Restraint
• DC 2020-0151 Off-label Use of Antivirals and Antimalarials for Clinical Management of COVID-19
• DC 2020-0152 Guidance to All Public and Private Healthcare Facilities and Others to Assist
Surveillance Officers in Epid. Investigation on COVID-19
• DC 2020-0156 Guidance on Visitation and Group Activities in Closed Institutions
• DC 2020-0157 Reiteration of the Price Freeze of Essential Emergency Medicines and Medical
Devices due to COVID-19 Health Event
• DC 2020-0158 Reiteration of Interim Guidelines on Harmonized and Daily Health Facility
Reporting of COVID-19 Related Essential Resources and Supplies Using DOH Data Collect
Application
• DC 2020-0159 Triage and Management of Pregnant Patients with Suspected COVID-19
• DC 2020-0160 Guidance on the Use of COVID-19 Rapid Antibody-based Test Kits
• DC 2020-0161 Reiteration of the Updated List Price Freeze of Essential Emergency Medicines
and Medical Devices Due to COVID-19
• DC 2020-0162 Directive for the Continuous Operation of Dialysis Facilities in the Philippines
During the ECQ in Light of COVID-19
Philippine College of Occupational Medicine, Inc.
32
• DC 2020-0163 Reiteration of Deadline Extension of Submission of Citizen's Chapter and
Suspension of Processing Times in the Delivery of Govt Services in Luzon in Light of ECQ
• DC 2020-0167 Continuous Provision of Essential Health Services During COVID-19
• DC 2020-0172 Guidance on Misting and Spraying for COVID-19
• DC 2020-0173 Designation of National Training Center for Biosafety and Biosecurity of NIH-UPM
as a Training Provider for Biosafety and Biosecurity
• DC 2020-0174 Reiteration of Interim Guidelines on Expanded Testing for COVID-19
• DC 2020-0175 Reiteration of FDA Circular 2020-014 on Interim Guidelines on Manufacture of
PPE, Ventilators and Respirators in Light of COVID-19 Situation
• DC 2020-0176 Circulation of the Manual of Standards for Primary Care Facilities
• DC 2020-0177 Clarification on the Application of Negotiated Procurement under Emergency
Cases
• DC 2020-0178 Approving the Extension of Deadline for the Submission of 2019 APCPI Results of
Procuring Entities
• DC 2020-0179 Approving Acceptance of an Expired Mayor's Permit with Official Receipt for
Renewal App and Unnotarized Omnibus Sworn Statement as Basis for Award under Negotiated
Procurement (Emergency Cases) Modality
• DC 2020-0180 Guidelines on Operations and Incentives of Covered Enterprises Engaged in
Manufacture, Importation and Distribution of Products Pursuant to RA 11469
• DC 2020-0181 Reiteration of Functions of the Infection Control Committee (ICC) and Infection
Control Team (ICT) in Healthcare Facilities
• DC 2020-0182 Approving the Adoption of Efficient, Effective and Expedient Procurement
Procedures During a State of Public Health Emergency
• DC 2020-0183 Designation of the National Training Center for Biosafety and Biosecurity of NIH-
UP Manila as a Hands-on Training Provider for Biosafety and Biosecurity
• DC 2020-0184 Clarification on Financing and Reimbursement of COVID-19 Antibody Test Kits by
DOH and PhilHealth
• DC 2020-0185 Reiteration of Proper Assessment and Referral of Patients in Health Facilities
• DC 2020-0186 Reiteration of the Amendment of the Updated List for Price Freeze of Essential
Emergency Medicines and Medical Devices due to COVID-19
• DC 2020-0187 Guidelines in the Interim Use of Laboratories of the National TB Control Program
as COVID-19 Testing Labs Performing Rapid PCR Testing for SARS-CoV-2
• DC 2020-0188 Reiteration of Delegation of Authority to Handle Specific Complaints to the
Regional Office - Regulation, Licensing and Enforcement Division
• DC 2020-0189 Directive for Continuous Operation of Laboratories for Drinking Water Analysis
(LDWA) During Community Quarantine in Light of COVID-19
• DC 2020-0190 Approving the Recommendation to Increase the Allowable Amount of Advance
Payment and Issuance of a Circular on the Guidelines for Emergency Procurement under RA
11469
• DC 2020-0191 Circulation of the Health Care Waste Management Manual 4th Edition
• DC 2020-0192 Ensuring that People in GIDAs, ICCs, or IPs are Well-informed on COVID-19 and
have Access to Temporary Treatment and Monitoring Facilities and Referral Hosp.
• DC 2020-0193 Reiteration of the Temporary Suspension of Taraweeh Prayers in Muslim
Mosques and Prayer Rooms During Ramadan 2020
• DC 2020-0194 Advisory on the Use of RT-PCR Testing Kits for COVID-19 Manufactured by
Manila HealthTek Inc.
• DC 2020-0195 Reiteration of the Price Freeze of Personal Protective Equipment (PPE) and
Guidelines for its Rational Use During COVID-19 Pandemic
• DC 2020-0196 Reiteration of Interim Guidelines for Dialysis Facilities During COVID-19
Pandemic
• DC 2020-0197 COVID-19 Information System
• DC 2020-0198 Providing a List of Mental Health Professionals to DOH Leaders
• DC 2020-0199 Online Resource Channels for Health Facility Development Policies, Standards,
and Guidelines
Philippine College of Occupational Medicine, Inc.
33
• DC 2020-0200 Prohibition on Sale of PPEs & Other Med. Supplies Donated by Public or Private
Entities & Distributed by DOH & Department Mandate on Strict Compliance of Mandatory Price
Freeze for Duration of Covida Quarantina
• DC 2020-0201 Utilization of the EB COVID KAYA Information System for Close Contact Data and
Reporting of Contact Tracing Data
• DC 2020-0202 Guidance for Certifying COVID-19
• DC 2020-0203 Clarification on the Financing of Proficiency Testing in Certification of COVID-19
Testing Laboratories
• DC 2020-0204 Advisory on Specimen Collection of Nasopharyngeal and Oropharyngeal Swabs
in Swabbing Centers
DC 2020-0205 Recognizing Subnational Laboratories as Training Providers for Hands-on PCR
Training
OSHA
• Guidance on Preparing Workplaces for COVID-19
CDC
• Interim Guideline No. 1: Interim Laboratory Biosafety Guidelines for Handling and Processing
Specimens Associated with Coronavirus Disease 2019 (COVID-19)
• Implementation of Mitigation Strategies for Communities with Local COVID-19 Transmission
WHO
• 3rd Edition Manual Laboratory Biosafety Manual
RITM
• March 15 Guidelines: Interim Biosafety Guidelines for Laboratories Handling and Testing SARS-
COV-2 (COVID-19) Specimen
DOH
• Implementing Rules and Regulations of RA 11332
• IRR for Mandatory Reporting of Notifiable Diseases and Health Events of Public Health Concern
Act
DOH, DILG, and DOT
• February 18 Joint Statement DOH, DILG, and DOT on Public Gathering
DILG
• DILG MC 2020-023: amended guide to against the 2019 nCOV ARD
• DILG MC 2020-64: provincial/city/municipal special care facilities and isolation units amid the
COVID19 pandemic
UNIFIED COVID ALGORITHMS
• Guidelines for Primary Care
• Guidelines for Hospital Care
• Guidelines for PPE Use by Healthcare Workers
• Guidelines on Return to Work
Philippine College of Occupational Medicine, Inc.
34
RESOURCES
• Department Memorandum No. 2020-0189: Updated Guidelines on Contact Tracing of Close Contacts
of Confirmed Coronavirus Disease (COVID-19) Cases.
https://www.doh.gov.ph/sites/default/files/health-update/dm2020-0189.pdf
• Administrative Order No. 2020-0015: Guidelines on the Risk-Based Health Standards for COVID-19
Mitigation. https://www.doh.gov.ph/sites/default/files/health-update/ao2020-0015.pdf
• http://www.oshc.dole.gov.ph/images/OSH-Standards-2019-Edition.pdf
• https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html
• https://assets.publishing.service.gov.uk/media/5eb965d5d3bf7f5d3c74a2dd/working-safely-during-
covid-19-factories-plants-warehouses-
110520.pdf?fbclid=IwAR0PJ_fZ4wdLrlbs2EgFeuuHrHpicgoxKD_2CsMICmfmxgWZPGD8HYfj6-Y
• https://www.osha.gov/SLTC/covid-19/hazardrecognition.html
• https://www.hse.gov.uk/simple-health-safety/risk/steps-needed-to-manage-risk.htm
• https://www.hse.gov.uk/news/assets/docs/working-safely-guide.pdf
• https://www.msn.com/en-ph/news/national/doh-modifies-classification-of-covid-19-cases/ar-
BB12xoHH?li=BBZAn2m
• https://apps.who.int/iris/bitstream/handle/10665/331498/WHO-2019-nCoV-IPCPPE_use-2020.2-
eng.pdf?fbclid=IwAR2N3NQVnP11SMTwqcgSFsuoYOu5WoKFM7VO8f-QJdCWyWk0bpLEiutQyN8
• https://ehs.cornell.edu/campus-health-safety/occupational-health/covid-19/covid-19-hierarchy-controls
(Disclaimer: Pertinent information were lifted from different sources to avoid misinterpretation of
content)
Philippine College of Occupational Medicine, Inc.
35
EDITOR in CHIEF
Marilen Evangeline M. Cruz, MD, MHA, FPCOM
TECHNICAL WORKING GROUP ON COVID-19
Phil M. Pangilinan MD, MHA, DPCOM
Margaret L. Leachon MD, FPCOM
Anna Sofia Victoria S. Fajardo MD, MBAH, DPCOM
Arnold P. Tabun Jr., MD, FPCOM
Felix F. Labanda Jr. MD, MOH, FPCOM
Luningning P. Cubero MD, FPCOM
Neil P. Rodrigo MD, FPCOM
Roselle S. Andres MD, FPCOM
Maria Lourdes DR. Billones MD, MOH, FPCOM
Rommel B. Punongbayan MD, MBA, FPCP
APPROVING BODY
PCOM National Officers and Board of Directors 2019-2020
For more information please call
DOHs COVID Emergency Operations Center at
(632) 8651-7800 loc 1149 -1150 or
(02) 894-COVID
www.doh.gov.ph
PCOM DETAILS
Cellphones:
+63 998 9545 338
+63 925 8175 026
+63 906 4743 471
+63 917 6276 246
Landline: (02) 8929 7741
Website: https://www.pcom.ph
Your feedback is important to us. Please email the PCOM Secretariat at:
pcomsecretariat@gmail.com
pcomsecretariat@yahoo.com
Address: Room 106, PMA Bldg., North Ave., Quezon City
Philippine College of Occupational Medicine, Inc.
36
You might also like
- Binary Data Biostatistics QuizDocument6 pagesBinary Data Biostatistics QuizTilak Venkatesh100% (3)
- Basic First Aid ProceduresDocument4 pagesBasic First Aid ProceduresSoyPedroNo ratings yet
- The LATCH Scoring SystemDocument7 pagesThe LATCH Scoring SystemAndini PramonoNo ratings yet
- IntexGroup Services ProfileDocument10 pagesIntexGroup Services ProfileMuhammad Shafqat100% (1)
- Medicine Inventory 2010-2011Document2 pagesMedicine Inventory 2010-2011Michelle Domingo PalmaNo ratings yet
- Case Study Group 1Document3 pagesCase Study Group 1Vincent Angelo DanaoNo ratings yet
- BiohazardDocument14 pagesBiohazardsujan maharjanNo ratings yet
- 1-Introduction To Occupational Safety and HealthDocument36 pages1-Introduction To Occupational Safety and HealthelickNo ratings yet
- Occupational Health NursingDocument1 pageOccupational Health NursingAlyanna EvangelistaNo ratings yet
- Infection at Work - Controlling The RisksDocument29 pagesInfection at Work - Controlling The RisksGissmoNo ratings yet
- 5.5c Infection Control Annual Work Plan 2013-14Document8 pages5.5c Infection Control Annual Work Plan 2013-14Tianti PuadiNo ratings yet
- Bosh 1 Module 7Document9 pagesBosh 1 Module 7Rayden BarridaNo ratings yet
- Occupational Health OverviewDocument11 pagesOccupational Health OverviewRidzwan HussainNo ratings yet
- Patient Safety StrategyDocument12 pagesPatient Safety StrategyAyman Allam100% (1)
- Johnson Johnson Case Study!@Document5 pagesJohnson Johnson Case Study!@Abhishek GoelNo ratings yet
- Diabetes Type I Powerpoint 2Document10 pagesDiabetes Type I Powerpoint 2api-317440960No ratings yet
- Toolbox Talks Personal Protective Equipment English PDFDocument1 pageToolbox Talks Personal Protective Equipment English PDFHosamMohamedNo ratings yet
- 2.1. Organising For SafetyDocument29 pages2.1. Organising For SafetyPERATCHI SELVANNo ratings yet
- First Aid LeafletDocument11 pagesFirst Aid LeafletshahnawazNo ratings yet
- 3a - Occupational Safety ME 70 Basic Occupational Safety and HealthDocument91 pages3a - Occupational Safety ME 70 Basic Occupational Safety and Healths.salise.allendaveNo ratings yet
- Knowledge Attitude and Practices of Health Workers On Puerperal Sepsis Preventions at Bundibugyo Hospital Bundibugyo DistrictDocument21 pagesKnowledge Attitude and Practices of Health Workers On Puerperal Sepsis Preventions at Bundibugyo Hospital Bundibugyo DistrictKIU PUBLICATION AND EXTENSIONNo ratings yet
- COVID 19 and The Work PlaceDocument88 pagesCOVID 19 and The Work PlaceSheik Mansour LovinhoNo ratings yet
- VCT ManualDocument70 pagesVCT ManualNay Lin HtikeNo ratings yet
- Basic Life Support and First AidDocument6 pagesBasic Life Support and First AidBryan Rey Del FierroNo ratings yet
- COVID19 Response Plan Template FinalDocument25 pagesCOVID19 Response Plan Template FinalJalina McClainNo ratings yet
- Hospital Emergency Preparedness Plan & Critical Stress ManagementDocument21 pagesHospital Emergency Preparedness Plan & Critical Stress ManagementYujenNo ratings yet
- Business Profile Presentation of Avie Training and Consultancy ServicesDocument10 pagesBusiness Profile Presentation of Avie Training and Consultancy ServicesAviects Avie JaroNo ratings yet
- Canteen Policy PDFDocument4 pagesCanteen Policy PDFudumariom0% (1)
- Female Welfare ProgrammeDocument6 pagesFemale Welfare ProgrammeAnnapurna DangetiNo ratings yet
- Risk RegisterDocument16 pagesRisk RegistersehrNo ratings yet
- ILO (Prevention of Occupational Disease)Document14 pagesILO (Prevention of Occupational Disease)Yopa Riyanda PuteriNo ratings yet
- Operations Management, MBA 2nd Sem.Document59 pagesOperations Management, MBA 2nd Sem.Coolest ChapNo ratings yet
- Random Blood Sugar Estimation and Its SignificanceDocument11 pagesRandom Blood Sugar Estimation and Its Significanceapi-38237850% (1)
- Ethics Workplace SafetyDocument12 pagesEthics Workplace SafetyKenny Martin100% (3)
- OSHA ManagementDocument9 pagesOSHA ManagementAhmad Wafiuddin100% (1)
- Vocinity Services PVT LTD ProfileDocument10 pagesVocinity Services PVT LTD ProfileAvinash KumarNo ratings yet
- SOP First Aid TrainingDocument4 pagesSOP First Aid TrainingshreyasNo ratings yet
- Reviewer in BOSHDocument5 pagesReviewer in BOSHLIANNE GEMIMA GIPANo ratings yet
- Occupational Health and Hazard PreventionDocument10 pagesOccupational Health and Hazard PreventionAndrew Narrido0% (1)
- Personal Hygiene For Food HandlersDocument23 pagesPersonal Hygiene For Food HandlersKitNo ratings yet
- Workplace Violence Definition:: 4 TypesDocument2 pagesWorkplace Violence Definition:: 4 TypeskaranNo ratings yet
- Clinical Casuality ManagementDocument6 pagesClinical Casuality ManagementswathiprasadNo ratings yet
- Fire & Emergency EvacuationDocument11 pagesFire & Emergency EvacuationCharisse KharyleNo ratings yet
- Welfare MeasuresDocument22 pagesWelfare Measureschaitanya555No ratings yet
- Five Steps To Crisis Management PlanningDocument2 pagesFive Steps To Crisis Management PlanningTambro IsbNo ratings yet
- 11.2 Baseline Medical Surveillance ProcedureDocument18 pages11.2 Baseline Medical Surveillance ProcedureaceNo ratings yet
- Animal Bite GuildlinesDocument7 pagesAnimal Bite GuildlinesHari Pawan Kishore GarimellaNo ratings yet
- Grievance ProcedureDocument11 pagesGrievance ProcedureApeksha TiwariNo ratings yet
- 11-First Aid PDFDocument33 pages11-First Aid PDFSaizul Baharudin100% (1)
- End of Year Report For Medical DepartmentDocument15 pagesEnd of Year Report For Medical DepartmentSarah Naboo100% (1)
- Medical Triage ManagmentDocument28 pagesMedical Triage ManagmentShafiq Ur RahmanNo ratings yet
- Amul Projects by Ravi Kant SainiDocument72 pagesAmul Projects by Ravi Kant SainiOjender MuneNo ratings yet
- Hirac: March 25-29, 2020 Northwest Inn, Rizal ST., Bacolod CityDocument6 pagesHirac: March 25-29, 2020 Northwest Inn, Rizal ST., Bacolod CityLenaj Ebron50% (2)
- Accident CausationDocument34 pagesAccident CausationRexy Susanto100% (1)
- An Introduction Crisis Is Any Event or Situation That Threaten or Could Threat To HarmDocument4 pagesAn Introduction Crisis Is Any Event or Situation That Threaten or Could Threat To HarmDavid JYNo ratings yet
- Vaccination of Healthcare WorkersDocument16 pagesVaccination of Healthcare WorkersBenjamin RuotiNo ratings yet
- Clinical Guidelines For Management of HTNDocument6 pagesClinical Guidelines For Management of HTNChaturangaNSenerath100% (1)
- Cost of Accident190423Document46 pagesCost of Accident190423Jallela SomeshNo ratings yet
- Basic First AidDocument70 pagesBasic First AidNeacsu IleanaNo ratings yet
- COVID 19 Healthcare Workers GuideDocument9 pagesCOVID 19 Healthcare Workers GuidenilrmNo ratings yet
- Gap ArthroplastyDocument5 pagesGap ArthroplastyMax FaxNo ratings yet
- How To Take Care of Our Respiratory and CirculatoryDocument1 pageHow To Take Care of Our Respiratory and CirculatoryJoe Anne GuzmanNo ratings yet
- 256 CircumcisionDocument5 pages256 CircumcisionMD Luthfy LubisNo ratings yet
- Flail ChestDocument3 pagesFlail ChestMd Ahsanuzzaman PinkuNo ratings yet
- Types of HospitalsDocument5 pagesTypes of Hospitalsjangas, jovanny c.88% (8)
- Physiotherapy For Cardiac SurgeryDocument15 pagesPhysiotherapy For Cardiac SurgeryMuruganNo ratings yet
- Leukocytes or White Blood Cells (WBC)Document22 pagesLeukocytes or White Blood Cells (WBC)Md Atikur AminNo ratings yet
- Eyelid TumorsDocument2 pagesEyelid TumorsVera AvliwaniNo ratings yet
- Deep Vein ThrombosisDocument13 pagesDeep Vein Thrombosisusmle prepNo ratings yet
- Pediatric RadiologyDocument82 pagesPediatric Radiologyabakferro0% (1)
- Cardiovascular Risk Factors and 10-Year Risk CHDDocument8 pagesCardiovascular Risk Factors and 10-Year Risk CHDsri haryuniNo ratings yet
- Tooth Survival Following Non-Surgical Root Canal Treatment: A Systematic Review of The Literature Y.Document19 pagesTooth Survival Following Non-Surgical Root Canal Treatment: A Systematic Review of The Literature Y.Shubham NaikNo ratings yet
- Medical Surgical ComprehensiveDocument15 pagesMedical Surgical ComprehensiveMatt Lao DionelaNo ratings yet
- Paget's Disease: EtiologyDocument8 pagesPaget's Disease: EtiologyMURALINo ratings yet
- Rüthrich2021 Article COVID-19InCancerPatientsClinicDocument11 pagesRüthrich2021 Article COVID-19InCancerPatientsClinicdianaNo ratings yet
- DMD Oral-Surgery-430-440Document77 pagesDMD Oral-Surgery-430-440gNo ratings yet
- Use of Vasopressors and Inotropes - UpToDateDocument25 pagesUse of Vasopressors and Inotropes - UpToDateVictor Mendoza - MendezNo ratings yet
- Read Online Textbook Behavior Modification What It Is and How To Do It 10Th Edition Garry Martin Ebook All Chapter PDFDocument22 pagesRead Online Textbook Behavior Modification What It Is and How To Do It 10Th Edition Garry Martin Ebook All Chapter PDFhilda.rufe918100% (2)
- Guideline Title: Cardiac Monitoring in ICUDocument14 pagesGuideline Title: Cardiac Monitoring in ICURirin RozalinaNo ratings yet
- Suma Akter: Career ObjectiveDocument4 pagesSuma Akter: Career ObjectiveNahidul IslamNo ratings yet
- Anahaw Mich Pharma ReportDocument10 pagesAnahaw Mich Pharma ReportMichelle L. AnahawNo ratings yet
- Food Supplements: Elisha Gay C. Hidalgo, RNDDocument25 pagesFood Supplements: Elisha Gay C. Hidalgo, RNDinkpen56789No ratings yet
- ICDAS Dental CariesDocument6 pagesICDAS Dental CariestulusNo ratings yet
- Opioid Analgesics and AntagonistsDocument18 pagesOpioid Analgesics and AntagonistsLaura KristyNo ratings yet
- Follicular Cholecystitis With Cholelithiasis A Rare Case ReportDocument3 pagesFollicular Cholecystitis With Cholelithiasis A Rare Case ReportSSR-IIJLS JournalNo ratings yet
- NURSING CARE PLAN - CholeraDocument2 pagesNURSING CARE PLAN - Choleraderic87% (30)
- Fee Structure 2023 24Document6 pagesFee Structure 2023 24Vasu SharmaNo ratings yet
- Focus On Nursing Pharmacology Karch 5th Edition Test BankDocument17 pagesFocus On Nursing Pharmacology Karch 5th Edition Test Bankhannahhuffmanabjskxqgnm100% (39)
- CDC ChartDocument1 pageCDC ChartFarrand IvanNo ratings yet