Professional Documents
Culture Documents
Gastroduodenal Crohn'S Disease: Etiology
Uploaded by
KEn PilapilOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Gastroduodenal Crohn'S Disease: Etiology
Uploaded by
KEn PilapilCopyright:
Available Formats
GASTRODUODENAL CROHN’S DISEASE
Inflammatory bowel disease (IBD) is an immune-mediated chronic intestinal condition. Ulcerative
colitis (UC) and Crohn’s disease (CD) are the two major types of IBD. Active CD is characterized by
focal inflammation and formation of fistula tracts, which resolve by fibrosis and stricturing of the
bowel. The bowel wall thickens and becomes narrowed and fibrotic, leading to chronic, recurrent
bowel obstructions. Although CD usually presents as acute or chronic bowel inflammation, the
inflammatory process evolves toward one of two patterns of disease: a fibrostenotic obstructing
pattern or a penetrating fistulous pattern, each with different treatments and prognoses. The site
of disease influences the clinical manifestations. (Harrison’s Principles of Internal Medicine 20 th
ed. p. 2263, 2264).
Harrison’s
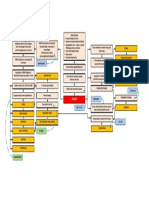
Genetic susceptibility
Principles of
Microbial flora
Etiology Internal
Immune dysregulation
Medicine 20th
Environmental factors
ed. P. 2259
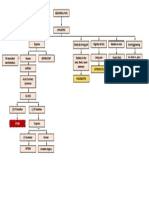
The highest incidence rates of CD and UC have been
reported in northern Europe, the United Kingdom,
and North America.
Peak incidence of UC and CD is in the second to
fourth decades, with 78% of CD studies and 51% of
UC studies reporting the highest incidence among
those age 20–29 years old.
A second modest rise in incidence occurs between Harrison’s
the seventh and ninth decades of life. Principles of
Epidemiology The female-to-male ratio ranges from 0.51 to 1.58 Internal
for UC studies and 0.34 to 1.65 for CD studies, Medicine 20th
suggesting that the diagnosis of IBD is not gender- ed. P. 2258
specific.
The greatest incidence of IBD is among white and
Jewish people, but the incidence of IBD in Hispanic
and Asian people is increasing, as noted above.
Urban areas have a higher prevalence of IBD than
rural areas, and high socioeconomic classes have a
higher prevalence than lower socioeconomic classes.
Harrison’s
Second to fourth decades
Principles of
Non-modifiable risk Seventh to ninth decades
Internal
factors OR predisposing RF for developing CA: long duration and extensive
Medicine 20th
factors disease, bypassed colon segment, colon strictures,
ed. P. 2258,
PSC, family history of colon cancer.
2276
Harrison’s
Principles of
Smoking
Modifiable risk factors OR Internal
OCP use
precipitating factors Medicine 20th
Antibiotic use in the first year of life
ed. P. 2258,
2276
Pathophysiology Under physiologic conditions, homeostasis Harrison’s
normally exists between the commensal
microbiota, epithelial cells that line the interior of
the intestines and immune cells within the tissues.
Each of these three major host compartments that
function together as an integrated
“supraorganism” (microbiota, IECs, and immune
cells) are affected by specific environmental (e.g.,
smoking, antibiotics, enteropathogens) and
genetic factors that, in a susceptible host,
cumulatively and interactively disrupt homeostasis
Principles of
during the course of one’s life, which in so doing
Internal
culminates in a chronic state of dysregulated
Medicine 20th
inflammation; that is IBD.
ed. P. 2259,
IBD is currently considered an inappropriate
2260
immune response to the endogenous
(autochthonous) commensal microbiota within
the intestines, with or without some component
of autoimmunity. During the course of infections
or other environmental stimuli in the normal host,
full activation of the lymphoid tissues in the
intestines occurs but is rapidly superseded by
dampening of the immune response and tissue
repair. In IBD such processes may not be regulated
normally.
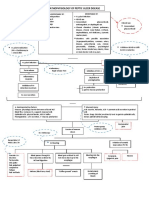
History (Subjective Active CD: focal inflammation and formation of Harrison’s
complaints) fistula tracts, which resolve by fibrosis and Principles of
stricturing of the bowel. The bowel wall thickens and Internal
becomes narrowed and fibrotic, leading to chronic, Medicine 20th
recurrent bowel obstructions. ed. P. 2263,
Usual presentation of ileocolitis is a chronic history 2264
of recurrent episodes of right lower quadrant pain
and diarrhea.
- Sometimes the initial presentation mimics
acute appendicitis with pronounced right
lower quadrant pain, a palpable mass, fever,
and leukocytosis.
- Pain is usually colicky; it precedes and is
relieved by defecation.
- Weight loss is common (10–20% of body
weight) and develops as a consequence of
diarrhea, anorexia, and fear of eating.
Bowel obstruction may take several forms.
- Early stages: bowel wall edema and spasm
produce intermittent obstructive
manifestations and increasing symptoms of
postprandial pain.
- Chronic: persistent inflammation gradually
progresses to fibrostenotic narrowing and
stricture. Diarrhea will decrease and be
replaced by chronic bowel obstruction.
Stricturing can occur in the colon in 4–16% of
patients and produce symptoms of bowel
obstruction. If the endoscopist is unable to traverse
a stricture in Crohn’s colitis, surgical resection
should be considered, especially if the patient has
symptoms of chronic obstruction.
- Colonic disease may fistulize into the stomach
or duodenum, causing feculent vomiting, or to
the proximal or mid-small bowel, causing
malabsorption by “short circuiting” and
bacterial overgrowth.
Harrison’s
Symptoms and signs of upper GI tract disease Principles of
include nausea, vomiting, and epigastric pain. Internal
PE Findings
Patients with advanced gastroduodenal CD may Medicine 20th
develop a chronic gastric outlet obstruction. ed. P. 2263,
2264
Laboratory abnormalities: elevated ESR and CRP.
Severe disease: hypoalbuminemia, anemia, and
leukocytosis.
Fecal calprotectin and lactoferrin levels:
distinguish IBD from IBS, assess whether CD is
active, and to detect postoperative recurrence of
CD.
Endoscopic features: rectal sparing, aphthous
Harrison’s
ulcerations, fistulas, and skip lesions.
Diagnostic tests to Principles of
Wireless capsule endoscopy (WCE) allows direct
request and its expected Internal
visualization of the entire small-bowel mucosa.
findings or results Medicine 20th
Early radiographic findings: thickened folds and
ed. P. 2265
aphthous ulcerations. “Cobblestoning” from
longitudinal and transverse ulcerations most
frequently involves the small bowel.
The earliest macroscopic findings of colonic CD are
aphthous ulcers. As the disease progresses,
aphthous ulcers become enlarged, deeper, and
occasionally connected to one another, forming
longitudinal stellate, serpiginous, and linear ulcers.
Medical treatment Infliximab (anti-TNF): chimeric monoclonal Harrison’s
(include the drug antibody which binds w/ high affinity to the Principles of
classification, mechanism soluble and transmembrane forms of tumour Internal
of action, dosage, route, necrosis factor-α (TNF-α) thereby inhibiting Medicine 20th
and frequency) binding of TNF-α to its receptors. Initially, 5 mg/kg ed. P. 2272
by infusion over at least 2 hr, repeated at 2 wk MIMS PH
after 1st infusion. No further doses should be
given if there is no response after 2 doses.
Responders: Maintenance: 5 mg/kg at 6 wk after
initial dose then 8 wkly thereafter.
Harrison’s
Principles of
Internal
Surgical resection of the diseased segment
Surgical treatment Medicine 20th
Stricturoplasty
ed. P. 2273,
2274
Harrison’s
Principles of
Bowel rest
Nonpharmacological Internal
TPN
treatment Medicine 20th
Enteral nutrition
ed. P. 2273
Serosal adhesions
Fistula formation Harrison’s
Perforation Principles of
Peritonitis Internal
Complications
Intaabdominal and pelvic abscess Medicine 20th
Intestinal obstruction ed. P. 2265
Massive hemorrhage
malabsorption
Harrison’s
Principles of
Internal
Prevention Environmental factor modification
Medicine 20th
ed. P. 2259
Because CD is a transmural process, serosal
adhesions develop that provide direct pathways
for fistula formation and reduce the incidence of
free perforation.
Harrison’s
Perforation occurs in 1–2% of patients. The
Principles of
peritonitis of free perforation, especially colonic,
Prognosis or outcome Internal
may be fatal.
Medicine 20th
Intraabdominal and pelvic abscesses occur in 10–
ed. P. 2265
30% of patients.
Other complications: intestinal obstruction in 40%,
massive hemorrhage, malabsorption, and severe
perianal disease
You might also like
- PANCE Prep Pearls Cardio Questions PDFDocument9 pagesPANCE Prep Pearls Cardio Questions PDFkat100% (3)
- Acute Kidney Injury Concept MapDocument1 pageAcute Kidney Injury Concept MapKEn PilapilNo ratings yet
- Magic of The Minimum Dose PDFDocument221 pagesMagic of The Minimum Dose PDFminunat100% (1)
- Hse Statistics Report Pp701 Hse f04 Rev.bDocument1 pageHse Statistics Report Pp701 Hse f04 Rev.bMohamed Mouner100% (1)
- Microorganisms: Microbiome, Metabolome and Inflammatory Bowel DiseaseDocument19 pagesMicroorganisms: Microbiome, Metabolome and Inflammatory Bowel DiseaseRenata RothenNo ratings yet
- Genes 13 02388 v2Document23 pagesGenes 13 02388 v2Elena666 a.No ratings yet
- Mechanisms and Consequences of Intestinal Dysbiosis: G. Adrienne Weiss Thierry HennetDocument19 pagesMechanisms and Consequences of Intestinal Dysbiosis: G. Adrienne Weiss Thierry HennetAlexa MaciucaNo ratings yet
- Inflammatory Bowel Disease: Microorganisms That Drive DiseaseDocument4 pagesInflammatory Bowel Disease: Microorganisms That Drive DiseaseIsabel CastilloNo ratings yet
- Ndtculec3 de GuiaDocument2 pagesNdtculec3 de GuiaKeanu Win CatipayNo ratings yet
- Ibd GDDocument15 pagesIbd GDAndi SusiloNo ratings yet
- Clinical Immunology: Review ArticleDocument13 pagesClinical Immunology: Review Articledoc0814No ratings yet
- Communication Between The Gut Microbiota and PeripDocument20 pagesCommunication Between The Gut Microbiota and PeripTuna TunNo ratings yet
- In Ammatory Bowel Disease: Educational GapsDocument14 pagesIn Ammatory Bowel Disease: Educational GapsMonica LeeNo ratings yet
- Barbara 2014Document7 pagesBarbara 2014Gaudeamus IgiturNo ratings yet
- Fcimb 12 1059825Document15 pagesFcimb 12 1059825resultados.metabolismolpNo ratings yet
- Immune Homeostasis, Dysbiosis and Therapeutic Modulation of The Gut MicrobiotaDocument15 pagesImmune Homeostasis, Dysbiosis and Therapeutic Modulation of The Gut MicrobiotaAjit Kumar BaidyaNo ratings yet
- 2021 Gut Microbiome PsoDocument4 pages2021 Gut Microbiome PsoDianaNo ratings yet
- 2018 Probioticos SIIDocument22 pages2018 Probioticos SIIPamela T MiyazakiNo ratings yet
- Review Article: Probiotics and Gastrointestinal InfectionsDocument11 pagesReview Article: Probiotics and Gastrointestinal InfectionsFarid FergianNo ratings yet
- Clinical Nutrition ESPEN: Dimitris Tsoukalas, Evangelia Sarandi, Spyridoula GeorgakiDocument15 pagesClinical Nutrition ESPEN: Dimitris Tsoukalas, Evangelia Sarandi, Spyridoula GeorgakiDaniel Irazabel ZelayaNo ratings yet
- Fecal Microbiota Transplantation To Prevent and TRDocument5 pagesFecal Microbiota Transplantation To Prevent and TRaimane.makerNo ratings yet
- Reviews: Immunity, Microbiota and Kidney DiseaseDocument12 pagesReviews: Immunity, Microbiota and Kidney DiseaseEss liNo ratings yet
- (2019) Probiotic and Synbiotic Therapy in The Critically Ill State of The ArtDocument8 pages(2019) Probiotic and Synbiotic Therapy in The Critically Ill State of The ArtAnna Maria Ariesta PutriNo ratings yet
- Gut Microbial Flora, Prebiotics and Probiotics in IBD - Their Current Usage and UtilityDocument10 pagesGut Microbial Flora, Prebiotics and Probiotics in IBD - Their Current Usage and UtilityHyacinth RotaNo ratings yet
- Periodontology 2000 - 2020 - Buduneli - Environmental Factors and Periodontal MicrobiomeDocument12 pagesPeriodontology 2000 - 2020 - Buduneli - Environmental Factors and Periodontal MicrobiomeAdil KaukabNo ratings yet
- The Human Gut Microbiome in Critical Illness 2024Document8 pagesThe Human Gut Microbiome in Critical Illness 2024Yazmin GoytiaNo ratings yet
- 1 s2.0 S104327602100134X MainDocument15 pages1 s2.0 S104327602100134X Mainsiddesh k mNo ratings yet
- Biochemistry: Dr. Professor - Month YearDocument3 pagesBiochemistry: Dr. Professor - Month YearAnn Ross FernandezNo ratings yet
- Woodhouse 2016Document6 pagesWoodhouse 2016Christine ParrillaNo ratings yet
- Immune Health SeminarDocument27 pagesImmune Health SeminarNuuraine NasirNo ratings yet
- The Gut Microbiota in Inflammatory Bowel DiseaseDocument14 pagesThe Gut Microbiota in Inflammatory Bowel DiseaseMércia FiuzaNo ratings yet
- Crohn DiseaseDocument8 pagesCrohn DiseaseFir FurqaniNo ratings yet
- Using ProbioticDocument11 pagesUsing ProbioticNovita ApramadhaNo ratings yet
- Microbiome Risk Profiles As Biomarkers For Inflammatory and Metabolic DisordersDocument15 pagesMicrobiome Risk Profiles As Biomarkers For Inflammatory and Metabolic DisordersMartinaNo ratings yet
- Tugas Buk Kasyani Jurnal Sistem Imun Dan ObesitasDocument5 pagesTugas Buk Kasyani Jurnal Sistem Imun Dan ObesitasfideNo ratings yet
- 2003 Probiotic and IBDDocument5 pages2003 Probiotic and IBDsujata sharmaNo ratings yet
- Dysbiotic Microbiota Interactions in Crohn S DiseaseDocument20 pagesDysbiotic Microbiota Interactions in Crohn S DiseasenortizotNo ratings yet
- Research 5Document8 pagesResearch 5Ali MohammedNo ratings yet
- Diseases 09 00060Document25 pagesDiseases 09 00060Igor BaltaNo ratings yet
- Histologic Diagnosis of Inflammatory Bowel DiseasesDocument14 pagesHistologic Diagnosis of Inflammatory Bowel DiseasesDiego Fernando Ortiz TenorioNo ratings yet
- Diet-Microbiota Interactions in Inflammatory Bowel DiseaseDocument17 pagesDiet-Microbiota Interactions in Inflammatory Bowel DiseaseIsabella María GantivarNo ratings yet
- 1 s2.0 S2405457721000358 MainDocument6 pages1 s2.0 S2405457721000358 MainYosephine SantosoNo ratings yet
- BMJ Open Gastroenterol 2021Document10 pagesBMJ Open Gastroenterol 2021Alejandro Jiménez BlasNo ratings yet
- HHS Public Access: Inflammatory Bowel Disease in Primary ImmunodeficienciesDocument13 pagesHHS Public Access: Inflammatory Bowel Disease in Primary ImmunodeficienciesYaumil ChoiriNo ratings yet
- Appendicitis: EtiologyDocument3 pagesAppendicitis: EtiologyKEn PilapilNo ratings yet
- Lymphocyte Homing and Its Role in The Pa PDFDocument15 pagesLymphocyte Homing and Its Role in The Pa PDFeufrat fuentesNo ratings yet
- Food 5Document16 pagesFood 5Narasimhulu KNo ratings yet
- Nihms 1771295Document25 pagesNihms 1771295arturocastillo12456No ratings yet
- Molecules 28 06811Document35 pagesMolecules 28 06811Nejc KovačNo ratings yet
- Gleason B OA Can Also Start in The GutDocument6 pagesGleason B OA Can Also Start in The Gutandreafernandez2eNo ratings yet
- Oxidative Stress and TB Outcomes in Patients With Diabetes Mellitus?Document4 pagesOxidative Stress and TB Outcomes in Patients With Diabetes Mellitus?icaeeNo ratings yet
- (Articulo) Patobioma 1 - How Holobionts Get Sick, Toward A Unifying Scheme of Disease PDFDocument4 pages(Articulo) Patobioma 1 - How Holobionts Get Sick, Toward A Unifying Scheme of Disease PDFFernanda PenagosNo ratings yet
- Microbial Pathogenesis: Lei Liu, Shangen Zheng TDocument6 pagesMicrobial Pathogenesis: Lei Liu, Shangen Zheng TDiego TulcanNo ratings yet
- International Journal of Pharmacy and Pharmaceutical SciencesDocument6 pagesInternational Journal of Pharmacy and Pharmaceutical SciencesNurainiManda-MinozNo ratings yet
- Intricate Connections Between The Microbiota and EndometriosisDocument23 pagesIntricate Connections Between The Microbiota and EndometriosiskannalijayaNo ratings yet
- Infantile Tremor Syndrome and Laryngomalacia A Novel AssociationDocument4 pagesInfantile Tremor Syndrome and Laryngomalacia A Novel AssociationOctavianus KevinNo ratings yet
- Clinical Evidence On The Potential Beneficial Effects ofDocument12 pagesClinical Evidence On The Potential Beneficial Effects ofDyane VatriciaNo ratings yet
- OWC Part16Document29 pagesOWC Part16Boby FaesalNo ratings yet
- Clinical Nutrition ESPEN: Poliana Guiomar de Almeida BrasielDocument2 pagesClinical Nutrition ESPEN: Poliana Guiomar de Almeida BrasielNo NameNo ratings yet
- Sa2 PDFDocument11 pagesSa2 PDFDeli LilianaNo ratings yet
- Antibiotic in CDDocument11 pagesAntibiotic in CDYaseerNo ratings yet
- Dental BiofilmsDocument44 pagesDental BiofilmsRamona MateiNo ratings yet
- The Biochemistry of Poliomyelitis Viruses: A Synopsis of Poliomyelitis Infection and ResearchFrom EverandThe Biochemistry of Poliomyelitis Viruses: A Synopsis of Poliomyelitis Infection and ResearchNo ratings yet
- Fast Facts: Inflammatory Bowel Disease: Translating the science into compassionate IBD careFrom EverandFast Facts: Inflammatory Bowel Disease: Translating the science into compassionate IBD careNo ratings yet
- Physical Inactivity: Aging Men Hypertension Smoker ObesityDocument1 pagePhysical Inactivity: Aging Men Hypertension Smoker ObesityKEn PilapilNo ratings yet
- Chest X-Ray Cardiomegaly Pleural EffusionDocument1 pageChest X-Ray Cardiomegaly Pleural EffusionKEn PilapilNo ratings yet
- Dengue Concep MapDocument1 pageDengue Concep MapKEn PilapilNo ratings yet
- Physical Inactivity: Aging Men Hypertension Smoker ObesityDocument1 pagePhysical Inactivity: Aging Men Hypertension Smoker ObesityKEn PilapilNo ratings yet
- Abdominal Pain Algorithm in STEMIDocument1 pageAbdominal Pain Algorithm in STEMIKEn PilapilNo ratings yet
- Peptic Ulcer Disease Pathogenesis Risk FactorsDocument1 pagePeptic Ulcer Disease Pathogenesis Risk FactorsKEn PilapilNo ratings yet
- Acute Kidney Injury Secondary To Congestive Heart Failure PathophysiologyDocument1 pageAcute Kidney Injury Secondary To Congestive Heart Failure PathophysiologyKEn PilapilNo ratings yet
- Acute Cholecystitis - : 20 Edition P. 2427)Document5 pagesAcute Cholecystitis - : 20 Edition P. 2427)KEn PilapilNo ratings yet
- Upper and Lower GI Bleeding Differential DiagnosesDocument3 pagesUpper and Lower GI Bleeding Differential DiagnosesKEn PilapilNo ratings yet
- Non St-Segment Elevation Acute Coronary Syndrome (Nste-Acs) : EtiologyDocument4 pagesNon St-Segment Elevation Acute Coronary Syndrome (Nste-Acs) : EtiologyKEn PilapilNo ratings yet
- Acute PancreatitisDocument4 pagesAcute PancreatitisKEn PilapilNo ratings yet
- Abdominal Pain Differential DiagnosesDocument1 pageAbdominal Pain Differential DiagnosesKEn PilapilNo ratings yet
- Gastroduodenal Crohn'S Disease: EtiologyDocument4 pagesGastroduodenal Crohn'S Disease: EtiologyKEn PilapilNo ratings yet
- Appendicitis: EtiologyDocument3 pagesAppendicitis: EtiologyKEn PilapilNo ratings yet
- Early Pregnancy With Vaginal Bleeding and Dilatation of The CervixDocument1 pageEarly Pregnancy With Vaginal Bleeding and Dilatation of The CervixKEn PilapilNo ratings yet
- Acute Cholecystitis - : 20 Edition P. 2427)Document5 pagesAcute Cholecystitis - : 20 Edition P. 2427)KEn PilapilNo ratings yet
- Threatened AbortionDocument1 pageThreatened AbortionKEn PilapilNo ratings yet
- Non St-Segment Elevation Acute Coronary Syndrome (Nste-Acs) : EtiologyDocument4 pagesNon St-Segment Elevation Acute Coronary Syndrome (Nste-Acs) : EtiologyKEn PilapilNo ratings yet
- Appendicitis: EtiologyDocument3 pagesAppendicitis: EtiologyKEn PilapilNo ratings yet
- Acute PancreatitisDocument4 pagesAcute PancreatitisKEn PilapilNo ratings yet
- Dead Products of Conception That Have Been Retained For Days or Weeks in The Uterus With A Closed Cervical OsDocument1 pageDead Products of Conception That Have Been Retained For Days or Weeks in The Uterus With A Closed Cervical OsKEn PilapilNo ratings yet
- Threatened AbortionDocument1 pageThreatened AbortionKEn PilapilNo ratings yet
- Complete AbortionDocument1 pageComplete AbortionKEn PilapilNo ratings yet
- Incomplete AbortionDocument2 pagesIncomplete AbortionKEn PilapilNo ratings yet
- Dead Products of Conception That Have Been Retained For Days or Weeks in The Uterus With A Closed Cervical OsDocument1 pageDead Products of Conception That Have Been Retained For Days or Weeks in The Uterus With A Closed Cervical OsKEn PilapilNo ratings yet
- Incomplete AbortionDocument2 pagesIncomplete AbortionKEn PilapilNo ratings yet
- Early Pregnancy With Vaginal Bleeding and Dilatation of The CervixDocument1 pageEarly Pregnancy With Vaginal Bleeding and Dilatation of The CervixKEn PilapilNo ratings yet
- Complete AbortionDocument1 pageComplete AbortionKEn PilapilNo ratings yet
- Cardiovascular Risk Factors in Airline PilotsDocument4 pagesCardiovascular Risk Factors in Airline Pilotsluis11256No ratings yet
- A Disease Prediction by Machine Learning Over Bigdata From Healthcare CommunitiesDocument3 pagesA Disease Prediction by Machine Learning Over Bigdata From Healthcare CommunitiesHarikrishnan ShunmugamNo ratings yet
- De So 3Document6 pagesDe So 3To Minh PhuongNo ratings yet
- Postherpetic Neuralgia NerissaDocument18 pagesPostherpetic Neuralgia Nerissanerissa rahadianthiNo ratings yet
- Morena E. Dail, RMT, MT (Amt), Mls (Ascpi) : Mors CodeDocument53 pagesMorena E. Dail, RMT, MT (Amt), Mls (Ascpi) : Mors CodemeriiNo ratings yet
- Apollo Excellence Report 2019 e VersionDocument289 pagesApollo Excellence Report 2019 e VersionrajNo ratings yet
- General Profile: - Pa - 6mos Old - Female - Filipino - Roman Catholic - Alang-Alang Mandaue CityDocument18 pagesGeneral Profile: - Pa - 6mos Old - Female - Filipino - Roman Catholic - Alang-Alang Mandaue CityRj FornollesNo ratings yet
- Practice Test 05 - Hints & Solutions - Lakshya NEET 2024Document15 pagesPractice Test 05 - Hints & Solutions - Lakshya NEET 2024Pandey 14No ratings yet
- Cerebrospinal FluidDocument12 pagesCerebrospinal FluidPavithran PNo ratings yet
- Fidelis Drug List 2018Document80 pagesFidelis Drug List 2018Annie AnnaNo ratings yet
- DISEASE DETECTION IN VEGETABLES (TOMATO) USING DEEP LEARNINgDocument38 pagesDISEASE DETECTION IN VEGETABLES (TOMATO) USING DEEP LEARNINgA ANo ratings yet
- Samar Deb Easy and Interesting ADocument846 pagesSamar Deb Easy and Interesting ACharlieNo ratings yet
- Efficacy of Doctorvox On Mutational FalsettoDocument8 pagesEfficacy of Doctorvox On Mutational FalsettoANA CRISTINA MENDEZ DIAZNo ratings yet
- Perioperative Fasting and Feeding in Adults, Obstetric, Paediatric and Bariatric Population-Practice Guidelines From The Indian Society of AnaesthesiologistsDocument29 pagesPerioperative Fasting and Feeding in Adults, Obstetric, Paediatric and Bariatric Population-Practice Guidelines From The Indian Society of Anaesthesiologistsambitiousamit1No ratings yet
- I Notes RETINA PDFDocument251 pagesI Notes RETINA PDFFelipe renquenNo ratings yet
- Molecular Biology of BacteriaDocument57 pagesMolecular Biology of BacteriaSean ArifinNo ratings yet
- Sandlewood Health BenefitsDocument7 pagesSandlewood Health BenefitskalaimaniNo ratings yet
- Ectopic PregnancyDocument54 pagesEctopic Pregnancypatriciaatan1497No ratings yet
- Black SeedDocument26 pagesBlack SeedAslam Aly Saib100% (1)
- Assessment Dianosis Planning Intervention Rationale EvaluationDocument2 pagesAssessment Dianosis Planning Intervention Rationale Evaluationkyaw100% (1)
- Sidra Internship ReportDocument40 pagesSidra Internship Reporthafeez ahmedNo ratings yet
- home-delhimed-downloadfile-IMA NATCON SCIENTIFIC PROGRAME PDFDocument15 pageshome-delhimed-downloadfile-IMA NATCON SCIENTIFIC PROGRAME PDFRaveenaNo ratings yet
- Arcega ErlindaDocument7 pagesArcega ErlindaIvonne TernidaNo ratings yet
- Department of Vegetable Science N.D. University of Agriculture & Technology Kumarganj, Faizabad-224229Document35 pagesDepartment of Vegetable Science N.D. University of Agriculture & Technology Kumarganj, Faizabad-224229Ujjwal UpadhyayNo ratings yet
- Is Fast Food The New Tobacco PDFDocument6 pagesIs Fast Food The New Tobacco PDFCustom Writing ServicesNo ratings yet
- Cataract Consent FormDocument4 pagesCataract Consent FormHitesh Sharma100% (1)
- Medsurg 3 Exam 1Document55 pagesMedsurg 3 Exam 1Melissa Blanco100% (1)