Professional Documents
Culture Documents
After I Lifted The Heavy Object, I Suddenly Felt A Pain in My Chest and I Am Also Experiencing of Difficulty in Breathing
Uploaded by
Julliza Joy Pandi0 ratings0% found this document useful (0 votes)
26 views8 pagesOriginal Title
NCP
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
26 views8 pagesAfter I Lifted The Heavy Object, I Suddenly Felt A Pain in My Chest and I Am Also Experiencing of Difficulty in Breathing
Uploaded by
Julliza Joy PandiCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 8
NAME OF PATIENT: MR.
X CASE: SEVERE CHEST PAIN
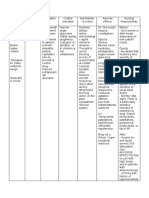
ASSESSMENT NURSING PLANNING NURSING RATIONALE EVALUATION
DIAGNOSIS INTERVENTIONS
SUBJECTIVE: Acute pain related After 5 days of Instruct patient to Pain and decreased After 5 days of
“After I lifted the heavy to tissue ischemia confinement, the notify nurse cardiac output may confinement, the
object, I suddenly felt a patient will immediately when stimulate the patient demonstrates
pain in my chest and I demonstrate relief chest pain occurs. sympathetic nervous a relief of pain as
am also experiencing of of pain as evidenced system to release evidenced by stable
difficulty in breathing” by stable vital signs, excessive amounts of vital signs, absence of
as stated by the patient. absence of muscle norepinephrine, muscle tension and
OBJECTIVE: tension and Assess and document which increases restlessness.
Restlessness restlessness. patient response platelet aggregation.
Rapid-breathing to medication. Provides information
Self-focused about disease
Uncooperative progression. Aids in
@ times evaluating
HEENT: PERRLA (pupils effectiveness of
equal, round, and Identify precipitating interventions, and
reactive to light and event, if any: may indicate need for
accommodation); frequency, duration, change in therapeutic
anicteric sclera intensity and location regimen.
of pain. Helps differentiate
Chest/Lungs: Adynamic this chest pain and
precordium, crackles Evaluate reports of pain aids in evaluating
upon auscultation in jaw, neck, shoulder, possible progression
arm or hand (typically to unstable angina.
Vital signs recorded as on left side).
ff.: Cardiac pain may
BP: 140/100 mmHg radiate. Pain is often
RR: 25 bpm Place patient at referred to more
CR: 140 bpm complete rest during superficial sites
TEMP: 37°C anginal episodes. served by the same
02 SAT: 90% spinal cord nerve
Monitor heart rate and level.
rhythm. Reduces myocardial
oxygen demand to
minimize risk of
tissue injury.
Patients with
Administer Morphine unstable angina have
Sulphate. an increased risk of
acute life-threatening
dysrhythmias, which
occur in response to
ischemic changes
and/or stress.
Potent narcotic
analgesic may be
used in acute onset
because of its several
beneficial effect.
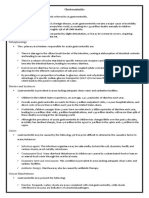
NAME OF PATIENT: MR. X CASE: SEVERE CHEST PAIN
ASSESSMENT NURSING PLANNING NURSING RATIONALE EVALUATION
DIAGNOSIS INTERVENTIONS
SUBJECTIVE: Activity At the end of five days Document heart rate Trends determine At the end of five days
“It has been 2 days intolerance confinement the and rhythm and patient’s response confinement the
since I’ve experienced related to patients will changes in BP before, to activity and patients demonstrate
severe chest pain” as imbalance demonstrate during and after may indicate measurable/progressive
stated by the patient. between measurable/progressive activity. myocardial oxygen increased in tolerance
OBJECTIVE: myocardial increase in tolerance for deprivation that for activity with heart
Restlessness oxygen supply activity with heart may require rate/rhythm and BP
Rapid-breathing and demand. rate/rhythm and BP decrease in within patient’s normal
Self-focused within patient’s normal activity level limits.
Uncooperative limits. and/or return to
@ times bedrest, changes
HEENT: PERRLA (pupils in medication
equal, round, and regimen, or use of
reactive to light and Encourage rest supplemental
accommodation); initially. Thereafter, oxygen.
anicteric sclera limit activity on basis Reduces
of pain and/or adverse myocardial
Chest/Lungs: Adynamic cardiac response. workload and
precordium, crackles Provide nonstress oxygen
upon auscultation diversional activities. consumption,
Vital signs recorded as
reducing risk of
ff.:
complications.
BP: 140/100 mmHg
Activities that
RR: 25 bpm Instruct patient to require holding
CR: 140 bpm avoid increasing the breath and
TEMP: 37°C abdominal pressure. bearing down can
02 SAT: 90%
result in
bradycardia and
rebound
tachycardia with
Explain pattern of elevated BP.
graded increase of Progressive
activity level: getting activity provides a
up to commode or controlled
sitting in chair, demand on the
progressive heart, increasing
ambulation, and strength and
resting after meals. preventing
overexertion.
Review s/sx reflecting
intolerance of present Palpitations, pulse
activity level or irregularities,
requiring notification development of
of nurse or physician. chest pain, or
dyspnea may
indicate need for
changes in
exercise regimen
or medication.
NAME OF PATIENT: MR. X CASE: SEVERE CHEST PAIN
ASSESSMENT NURSING PLANNING NURSING RATIONALE EVALUATION
DIAGNOSIS INTERVENTIONS
SUBJECTIVE: Decreased cardiac The patient will be Assess the patient’s vital To assist in creating an The patient has able to
“I am having a chest output related to the able to maintain signs and characteristics accurate diagnosis and maintain adequate
pain” as stated by the disease process of adequate cardiac of heart beat at least monitor effectiveness cardiac output in the
patient. coronary artery output at the end of 5 every 4 hours. Assess of medical treatment. end of 5 days
disease (CAD) days confinement. heart sounds via confinement.
OBJECTIVE:
auscultation. To increase the oxygen
HEENT: PERRLA (pupils
Administer supplemental level and achieve an
equal, round, and oxygen, as prescribed. Sp02 value of at least
reactive to light and Discontinue if Sp02 level is 94%.
accommodation); above the target range, or
anicteric sclera as ordered by the
Chest/Lungs: physician. Stress causes a
Adynamic precordium, persistent increase in
crackles upon Educate pt. on stress cortisol levels, which
auscultation management, deep has been linked to
Vital signs recorded as breathing exercises, and people with cardiac
relaxation techniques. issues.
ff.:
BP: 140/100 mmHg
RR: 25 bpm
CR: 140 bpm
TEMP: 37°C
02 SAT: 90%
NAME OF PATIENT: MR. X CASE: SEVERE CHEST PAIN
ASSESSMENT NURSING PLANNING NURSING RATIONALE EVALUATION
DIAGNOSIS INTERVENTIONS
SUBJECTIVE: Acute pain related to The patient will Assess the patient’s vital To monitor The patient
“After I lifted a heavy decreased myocardial demonstrate relief of signs and characteristics effectiveness of demonstrates relief of
object, I suddenly felt blood flow as pain as evidenced by a of pain at least 30 minutes medical treatment for pain as evidenced by a
a pain in my chest… I evidenced by pain pain score of lower after administration of the relief of pain. The pain score of lower than
score of 10 out of 10. than 3 out of 10. medications. time of monitoring of 3 out of 10.
score it as 10” as
vital signs may depend
stated by the patient.
on the peak of time of
OBJECTIVE: the drug administered.
HEENT: Elevate the head of the
PERRLA; anicteric bed if the patient is having To increased the
a shortness of breath. oxygen level and
sclera
Administer supplemental achieve an Sp02 value
Chest/Lungs: oxygen, as prescribed. of at least 94%.
Adynamic Discontinue if Sp02 level is
precordium, crackles above the target range, or
as ordered by the
upon auscultation
physician. Stress causes a
Vital signs recorded
Place the patient in persistent increase in
as ff.: complete bed rest during cortisol levels, which
BP: 140/100 angina attacks. Educate has been linked to
RR: 25 bpm pt. on stress people with cardiac
CR: 140 bpm management, deep issues.
TEMP: 37°C breathing exercises, and
02 SAT: 90% relaxation techniques.
NAME OF PATIENT: MR. X CASE: SEVERE CHEST PAIN
ASSESSMENT NURSING PLANNING NURSING RATIONALE EVALUATION
DIAGNOSIS INTERVENTIONS
SUBJECTIVE: Decreased cardiac At the end of Perform a Assessment is the At the end of
“After I lifted a heavy output related to the confinement, the comprehensive first step in confinement, the
object, I suddenly felt a disease process of patient will assessment. Assess managing pain. It patient will display
pain in my chest” as coronary artery display improved location, helps ensure that improved vital
stated by the patient. disease (CAD) vital signs and characteristics, the patient signs and muscle
OBJECTIVE: muscle tone onset, duration, receives effective tone
HEENT: frequency, quality pain relief.
and severity of
PERRLA; anicteric sclera pain. Some patients may
Observe for deny the existence
Chest/Lungs: Adynamic
nonverbal indicators of pain. These
precordium, crackles behaviors can help
of pain: moaning,
upon auscultation guarding, crying, with proper
Vital signs recorded as facial grimace. evaluation of pain.
ff.:
BP: 140/100 mmHg Vital signs are
RR: 25 bpm Obtain vital signs. usually affected
CR: 140 bpm when pain is
TEMP: 37°C Use present.
02 SAT: 90% nonpharmacological Works by
pain relief methods increasing the
(relaxation release of
exercises, breathing endorphins,
exercises, music boosting the
therapy). therapeutic effects
of pain relief
Provide optimal medications.
pain relief by Various types of
administering pain require
prescribed pain different analgesic
relief medication. approaches. Some
respond well to
non-opioid pain
relievers while
Document patient’s others demand a
response to pain combination of
management. non-opioid and low
dose opioid.
It helps the entire
healthcare team
evaluate their pain
management
strategy.
You might also like
- Congestive Heart Failure NCPDocument6 pagesCongestive Heart Failure NCPShaira Ann Calamba100% (1)
- Quality Life Scale PDFDocument7 pagesQuality Life Scale PDFFayza RihastaraNo ratings yet
- SAMPLE NCP For Angina PectorisDocument3 pagesSAMPLE NCP For Angina Pectorisseanne_may100% (4)
- Nursing Care Plan For Angina Pectoris NCPDocument2 pagesNursing Care Plan For Angina Pectoris NCPkarthi karthi100% (1)
- Scenario NCPDocument3 pagesScenario NCPZanie CruzNo ratings yet
- Nursing Care Plan for Acute Chest PainDocument3 pagesNursing Care Plan for Acute Chest PainMelDred Cajes BolandoNo ratings yet
- NCM103Activity 1 NCPDocument2 pagesNCM103Activity 1 NCPMary Mathel Del RosarioNo ratings yet
- Understanding Angina Through Nursing Assessment and InterventionDocument2 pagesUnderstanding Angina Through Nursing Assessment and InterventionIvan Jules P. PALMARESNo ratings yet
- College of Health Sciences Nursing Care Plan for Acute Myocardial InfarctionDocument4 pagesCollege of Health Sciences Nursing Care Plan for Acute Myocardial InfarctionLouise GudmalinNo ratings yet
- Nursing Assessment and Interventions for Acute Chest PainDocument3 pagesNursing Assessment and Interventions for Acute Chest PainAjay SupanNo ratings yet
- Assessment Planning InterventionsDocument11 pagesAssessment Planning InterventionsKenrick BajaoNo ratings yet
- DS Debie18 20Document6 pagesDS Debie18 20Irene Grace BalcuevaNo ratings yet
- Assessment Nursing Diagnosis Desired Outcome Intervention Rationale EvaluationDocument2 pagesAssessment Nursing Diagnosis Desired Outcome Intervention Rationale EvaluationtflorenzNo ratings yet
- Hematologic Acute or Chronic Problems: ScenarioDocument36 pagesHematologic Acute or Chronic Problems: ScenariobhavanaNo ratings yet
- Nursing Interventions Relieve Chest Pain Acute Myocardial InfarctionDocument4 pagesNursing Interventions Relieve Chest Pain Acute Myocardial InfarctionDienizs LabiniNo ratings yet
- Medical Diagnosis: Acute Myocardial Infarction: A 66-Year-Old Male August 13, 2005 10 PM ER Unit Possible MIDocument1 pageMedical Diagnosis: Acute Myocardial Infarction: A 66-Year-Old Male August 13, 2005 10 PM ER Unit Possible MIBadri AlthubaityNo ratings yet
- Independent:: Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDocument6 pagesIndependent:: Assessment Diagnosis Inference Planning Intervention Rationale EvaluationBryanRachelle__403No ratings yet
- Drug Study of Acute PyelonephritisDocument6 pagesDrug Study of Acute PyelonephritisGhra CiousNo ratings yet
- NURSING CARE PLAN FOR CHEST PAIN AND VOMITINGDocument2 pagesNURSING CARE PLAN FOR CHEST PAIN AND VOMITINGApril Kate BanagodosNo ratings yet
- Adrian G. Mallar BSN 2 Focus: Chest Pain Nursing Care Plan - Rheumatic Heart DiseaseDocument3 pagesAdrian G. Mallar BSN 2 Focus: Chest Pain Nursing Care Plan - Rheumatic Heart DiseaseFarzana AfrinNo ratings yet
- NCP Chest PainDocument2 pagesNCP Chest PainLinsae Troy50% (2)
- Ds Week 6 Nrg301 ValenzonaDocument2 pagesDs Week 6 Nrg301 ValenzonaJoshennaNo ratings yet
- Group 1 - VITALS SIGNS and INTERVENTIONSDocument19 pagesGroup 1 - VITALS SIGNS and INTERVENTIONSTrishNo ratings yet
- Diagnostic TestsDocument5 pagesDiagnostic TestsKathleen DimacaliNo ratings yet
- ChestPainReliefDocument3 pagesChestPainReliefCzynna Dela CruzNo ratings yet
- Nababaliw Na Ako Sa Drug StudyDocument52 pagesNababaliw Na Ako Sa Drug StudyKate Husslein ErumNo ratings yet
- Chest InjuryDocument17 pagesChest InjuryAira Dy PinedaNo ratings yet
- Drug StudyDocument6 pagesDrug StudyGeraldine Gallaron - CasipongNo ratings yet
- NCP - MIDocument3 pagesNCP - MILlena Grace NatividadNo ratings yet
- Brand Name/generic Name Classification/ Indication Mode of Action Contraindications Nursing ResponsibiltiesDocument5 pagesBrand Name/generic Name Classification/ Indication Mode of Action Contraindications Nursing Responsibiltiesceline_chan36No ratings yet
- Drug Study Acute BronchitisDocument6 pagesDrug Study Acute BronchitisCarl Simon CalingacionNo ratings yet
- Francisco, Faye Andrea Go BSN 3-BDocument2 pagesFrancisco, Faye Andrea Go BSN 3-BFaye Andrea FranciscoNo ratings yet
- Nursing Care Plan Template PDFDocument2 pagesNursing Care Plan Template PDFRikka DetablanNo ratings yet
- Sympatholytic DrugsDocument8 pagesSympatholytic DrugsJianne CaloNo ratings yet
- TRAMADOLDocument4 pagesTRAMADOLRudie Lee PascualNo ratings yet
- Drug StudyDocument3 pagesDrug Studymarichelle plazaNo ratings yet
- Drug Study Final - 065014Document39 pagesDrug Study Final - 065014Elizabeth MadejaNo ratings yet
- Nursing responsibilities for cardiac drugsDocument19 pagesNursing responsibilities for cardiac drugsMarie Kelsey Acena MacaraigNo ratings yet
- MethergineDocument2 pagesMethergineKyla VillafrancaNo ratings yet
- Drugs 1Document5 pagesDrugs 1Charme Jean RaygonNo ratings yet
- Decreased Cardiac OutputDocument3 pagesDecreased Cardiac OutputRizalyn QuindipanNo ratings yet
- Beriso Drug StudyDocument5 pagesBeriso Drug StudyKasandra Dawn Moquia BerisoNo ratings yet
- Lorma Medical Center Carlatan, San Fernando City, La Union Nursing Care PlanDocument1 pageLorma Medical Center Carlatan, San Fernando City, La Union Nursing Care PlanKenmiharu SorianoNo ratings yet
- Drug StudyDocument2 pagesDrug StudyKristine YoungNo ratings yet
- NCM 118 - Rle: College of Nursing 1 Semester AY 2021-2022Document4 pagesNCM 118 - Rle: College of Nursing 1 Semester AY 2021-2022cammel ramosNo ratings yet
- What Is TriagingDocument5 pagesWhat Is TriagingshairaNo ratings yet
- Amlodipine - Drug StudyDocument2 pagesAmlodipine - Drug StudyAcads useNo ratings yet
- Generic Name: Adult: IVDocument3 pagesGeneric Name: Adult: IVBasema HashhashNo ratings yet
- Principles of Pathophysiology - Bullock, ShaneDocument2 pagesPrinciples of Pathophysiology - Bullock, ShaneMel Izhra N. MargateNo ratings yet
- Haloperidol: College of Health SciencesDocument2 pagesHaloperidol: College of Health SciencesKervy JuntillaNo ratings yet
- Nursing Care Plan For Doppler Scan and Stress TestingDocument10 pagesNursing Care Plan For Doppler Scan and Stress TestingAmy Rose AbuevaNo ratings yet
- Assignment No.1 OB High Risk Grp.1Document15 pagesAssignment No.1 OB High Risk Grp.1YongNo ratings yet
- Nursing Responsibilities for Salbutamol and PrednisoneDocument7 pagesNursing Responsibilities for Salbutamol and PrednisoneAlvin LimNo ratings yet
- NCP FormatDocument4 pagesNCP Formatsandie_bestNo ratings yet
- 4th Rot Drug StudyDocument3 pages4th Rot Drug StudyAaron GarciaNo ratings yet
- NCP 2 MiDocument16 pagesNCP 2 MiWendy EscalanteNo ratings yet
- Ccu Cad NCPDocument5 pagesCcu Cad NCPheyyymeeeNo ratings yet
- Celecoxib drug profile for pain and inflammation managementDocument2 pagesCelecoxib drug profile for pain and inflammation managementSeanmarie CabralesNo ratings yet
- Drug StudyDocument4 pagesDrug StudyKristine Young100% (1)
- Trigeminal Nerve Pain: A Guide to Clinical ManagementFrom EverandTrigeminal Nerve Pain: A Guide to Clinical ManagementAlaa Abd-ElsayedNo ratings yet
- Wilms Tumor (Nephroblastoma)Document4 pagesWilms Tumor (Nephroblastoma)Julliza Joy PandiNo ratings yet
- Multiple SclerosisDocument1 pageMultiple SclerosisKEn PilapilNo ratings yet
- Religions Experiences and SpiritualityDocument2 pagesReligions Experiences and SpiritualityJulliza Joy PandiNo ratings yet
- Multiple Sclerosis and Type 1 DMMENDOZACORLANDocument21 pagesMultiple Sclerosis and Type 1 DMMENDOZACORLANJulliza Joy PandiNo ratings yet
- Rheumatic Fever ModuleDocument7 pagesRheumatic Fever ModuleJulliza Joy Pandi100% (1)
- Hemolytic Disease of The Fetus and Newborn: DescriptionDocument2 pagesHemolytic Disease of The Fetus and Newborn: DescriptionJulliza Joy PandiNo ratings yet
- Seizure Disorders ModuleDocument9 pagesSeizure Disorders ModuleJulliza Joy PandiNo ratings yet
- Sudden Infant Death Syndrome (SIDS)Document4 pagesSudden Infant Death Syndrome (SIDS)Julliza Joy PandiNo ratings yet
- Spina Bifida Guide: Types, Causes & Nursing CareDocument5 pagesSpina Bifida Guide: Types, Causes & Nursing CareJulliza Joy PandiNo ratings yet
- Cystic Fibrosis Guide: Symptoms, Causes, TreatmentDocument5 pagesCystic Fibrosis Guide: Symptoms, Causes, TreatmentJulliza Joy PandiNo ratings yet
- Hypospadias and EpispadiasDocument3 pagesHypospadias and EpispadiasJulliza Joy PandiNo ratings yet
- IntussusceptionDocument4 pagesIntussusceptionJulliza Joy PandiNo ratings yet
- Hirschsprung Disease (Aganglionic Megacolon)Document6 pagesHirschsprung Disease (Aganglionic Megacolon)Julliza Joy PandiNo ratings yet
- Congenital Talipes Equinovarus (Clubfoot)Document4 pagesCongenital Talipes Equinovarus (Clubfoot)Julliza Joy PandiNo ratings yet
- Cleft Lip and Palate CareDocument4 pagesCleft Lip and Palate CareJulliza Joy PandiNo ratings yet
- GastroenteritisDocument4 pagesGastroenteritisJulliza Joy PandiNo ratings yet
- Acute GlomerulonephritisDocument4 pagesAcute GlomerulonephritisJulliza Joy PandiNo ratings yet
- Drug StudyDocument14 pagesDrug StudyJulliza Joy PandiNo ratings yet
- Sudden Infant Death Syndrome (SIDS)Document4 pagesSudden Infant Death Syndrome (SIDS)Julliza Joy PandiNo ratings yet
- Congenital Talipes Equinovarus (Clubfoot)Document4 pagesCongenital Talipes Equinovarus (Clubfoot)Julliza Joy PandiNo ratings yet
- Spina Bifida Guide: Types, Causes & Nursing CareDocument5 pagesSpina Bifida Guide: Types, Causes & Nursing CareJulliza Joy PandiNo ratings yet
- Wilms Tumor (Nephroblastoma)Document4 pagesWilms Tumor (Nephroblastoma)Julliza Joy PandiNo ratings yet
- Patient Discharge SummaryDocument4 pagesPatient Discharge SummaryJulliza Joy PandiNo ratings yet
- Cleft Lip and Palate CareDocument4 pagesCleft Lip and Palate CareJulliza Joy PandiNo ratings yet
- Drug Study FormatDocument1 pageDrug Study FormatJulliza Joy PandiNo ratings yet
- Acute GlomerulonephritisDocument4 pagesAcute GlomerulonephritisJulliza Joy PandiNo ratings yet
- Family Health Assessment FormDocument8 pagesFamily Health Assessment FormJulliza Joy PandiNo ratings yet
- Community Hypertension Nursing Goals Strategies ActivitiesDocument3 pagesCommunity Hypertension Nursing Goals Strategies ActivitiesJulliza Joy PandiNo ratings yet
- Cystic Fibrosis Guide: Symptoms, Causes, TreatmentDocument5 pagesCystic Fibrosis Guide: Symptoms, Causes, TreatmentJulliza Joy PandiNo ratings yet
- H2S Monitor Manual - Tango TX1Document50 pagesH2S Monitor Manual - Tango TX1MattNo ratings yet
- IOC Investors' Report Final 16 Aug 2019Document21 pagesIOC Investors' Report Final 16 Aug 2019Amri Satria NugrahaNo ratings yet
- Selcoperm SES 125-2000 Electrochlorinator: Installation and Operating InstructionsDocument32 pagesSelcoperm SES 125-2000 Electrochlorinator: Installation and Operating InstructionsNorbert MeyerNo ratings yet
- Occlusal Plane Template TechniqueDocument39 pagesOcclusal Plane Template TechniqueREWA KAWADENo ratings yet
- Amit Surati 29Document3 pagesAmit Surati 29api-286592025No ratings yet
- HSE and SOP ON EMBARKATIONDocument5 pagesHSE and SOP ON EMBARKATIONNajmirzan IsraNo ratings yet
- Graduation Certificates: Speech TherapyDocument10 pagesGraduation Certificates: Speech Therapyliza khalilNo ratings yet
- Lab1 MEM14089A Cluster AT3A Student 191106Document12 pagesLab1 MEM14089A Cluster AT3A Student 191106Shan YasirNo ratings yet
- Effective Leadership Theory Cases and Applications 1st Edition Humphrey Test BankDocument9 pagesEffective Leadership Theory Cases and Applications 1st Edition Humphrey Test Bankhillyobsidian8hi42g100% (36)
- DLL Health 9 & 10Document6 pagesDLL Health 9 & 10Gladys GutierrezNo ratings yet
- SV The Coronation of King Charles IIIDocument9 pagesSV The Coronation of King Charles IIIMaria GromovaNo ratings yet
- Emotional Loneliness First Aid by SlidesgoDocument58 pagesEmotional Loneliness First Aid by SlidesgoKarin FauziahNo ratings yet
- Modals of Suggestion HomeworkDocument2 pagesModals of Suggestion HomeworkmateoNo ratings yet
- Components of Argumentative EssayDocument13 pagesComponents of Argumentative EssaySheia Jinx75% (4)
- Exercise 5 Characteristics of Soil ColloidsDocument4 pagesExercise 5 Characteristics of Soil ColloidslexiclesmcgeeNo ratings yet
- Assessing Animal Housing and Management in a LaboratoryDocument22 pagesAssessing Animal Housing and Management in a Laboratoryrifky waskitoNo ratings yet
- JIDMR SCOPUS Ke 4 Anwar MallongiDocument4 pagesJIDMR SCOPUS Ke 4 Anwar Mallongiadhe yuniarNo ratings yet
- 2022醫療急救 無線電醫療作業Document2 pages2022醫療急救 無線電醫療作業Yu-ting FengNo ratings yet
- Guard RailDocument24 pagesGuard RailRESHMANo ratings yet
- Computerized Medical Imaging and GraphicsDocument10 pagesComputerized Medical Imaging and Graphicshimanish shekhar DasNo ratings yet
- Hope Week 2Document5 pagesHope Week 2Bea CabacunganNo ratings yet
- Contemporary World Exemplar T L ModuleDocument111 pagesContemporary World Exemplar T L ModuleChrizelle Mae Rodriguez100% (1)
- Medical Certificate: Healthservices@lnu - Edu.phDocument3 pagesMedical Certificate: Healthservices@lnu - Edu.phNiko ChavezNo ratings yet
- Pharmacology Course IntroductionDocument2 pagesPharmacology Course IntroductionHassen ZabalaNo ratings yet
- Lec 3Document21 pagesLec 3Valerie VargasNo ratings yet
- Biodata MSWDocument3 pagesBiodata MSWAnith BaylisNo ratings yet
- Chapter 1Document2 pagesChapter 1longaitiNo ratings yet
- Functions of ProteinsDocument2 pagesFunctions of Proteinsjacynda linsanganNo ratings yet
- Conduct Disorder and Somatic Health in ChildrenDocument3 pagesConduct Disorder and Somatic Health in ChildrenJeric C. ManaliliNo ratings yet