Professional Documents
Culture Documents
Bladder Control Factsheet
Uploaded by
Yosalfa Adhista KurniawanOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bladder Control Factsheet
Uploaded by
Yosalfa Adhista KurniawanCopyright:
Available Formats
Factsheet: Bladder Control after a Prostate Operation
Types of operation
Operations to the prostate gland are of two types, each having its own purpose. They are referred to
as, transurethral resection of the prostate (TURP).
(1) partial removal of an enlarged prostate gland, to relieve an obstruction to the flow of urine, and
(2) total removal, to cure cancer.
The vast majority of prostate operations are of the first type. The prostate tissue causing a blockage to the flow
of urine is removed, usually in a “keyhole” manner through the penis but sometimes by an “open” operation
through the abdomen. After the operation your urine should run freely.
There are other alternatives to operating such as the below minimally invasive techniques;
Holmium laser enucleation of the prostate - a laser is used to remove excess prostate tissue using
a similar route to a TURP.
KTP laser vaporisation - a small tube known as a cystoscope is inserted into your urethra. The
cystoscope fires pulses of laser energy to burn away prostate tissue.
When the operation is done for cancer, the whole prostate gland is removed so that if possible all the
cancerous tissue is removed and a cure is achieved. After either type of surgery you may have problems of
bladder control, perhaps involving involuntary leakage of urine (urinary incontinence), but this is much more
likely after the second, more extensive, operation.
Immediately after the Operation
After the operation a tube (a catheter) will have been left in your bladder in order to drain it. There will be blood
in the tube initially but this will reduce over time. The catheter will be removed after a few days, but the final
pattern of urine flow and control may well not become established for a number of weeks after the catheter is
removed. This is because the urinary system is not entirely under voluntary control and it takes time to adjust
to the new situation. This period can extend to three months or even longer. However, even during this early
period, useful treatments are available if you have difficulty controlling your bladder: some are described below.
Once you are discharged home after the operation, you should slowly return to your normal pattern of eating
and drinking. You may have been asked to increase your fluid intake initially, but you should be able to go back
to your normal level pretty quickly. Some drinks, like tea, coffee and cola drinks, as well as strong alcoholic
drinks, cause bladder irritation, and should not be drunk in excess.
You can build up your physical activities gently and progressively, including walking, swimming or any regular
activity you used to undertake before your operation. You should be able to go back to your normal pattern
within three or four weeks.
Avoid constipation. The best way is by having a diet rich in fibre, including wholemeal bread, bran and plenty of
fruit and vegetables. If constipation is a problem, consult your doctor or practice nurse, as excessive straining
should be avoided.
Complications
After a prostatectomy it is usual for men to cease to ejaculate semen from the penis during sexual intercourse.
Retrograde ejaculation - is the most common complication following prostatectomy and is caused by damage
to the nerves or muscles surrounding the neck of the bladder. It means that the semen ejaculated during
Updated January 2014
sexual intercourse does not come out of the penis but flows into the bladder instead. The physical pleasure
associated with ejaculation is not affected. However, it can affect your fertility, so discussion with your Urologist
should take place if this is a concern. It may also make the urine look cloudy when next passed. This is not
harmful in any way but it usually means that the man is infertile and cannot father a baby. If you have not
finished your family, ask about freezing your sperm. Infertility cannot be guaranteed, however, so if you were
using contraception before the operation, it will still be advisable afterwards.
Urinary tract infection – you may have a urine infection if you experience burning or pain when you pass urine,
or if the urine is cloudy, or if it smells unpleasant.. You should see your GP, who will usually ask for a urine
specimen to be tested, and may prescribe an antibiotic.
Bleeding -It is not unusual to experience some bleeding about ten days to two weeks after prostatectomy and
you may find some white debris in your urine. Usually this is of no significance and can be managed by
increasing your fluid intake. If it is very marked, however, or you have difficulty passing urine, you should seek
nursing or medical advice.
Incontinence - Urinary incontinence is obviously a serious complication of prostate surgery. It is critical to
establish its precise type and severity in order to try to predict its progress and, if need be, to decide on the best
treatment. Speak to your consultant before your surgery to discuss this further.
There are five relevant types of incontinence:
(1) total incontinence;
(2) stress incontinence;
(3) urge incontinence;
(4) mixed incontinence; and
(5) after-dribble.
(1) Total incontinence: The valve which should keep the urine in the bladder (the urinary sphincter) no
longer functions at all. The urine trickles out in a constant and slow stream. The bladder is empty, and there is
no remaining ability to control the flow of urine. This type is extremely uncommon after a partial removal, less
so after the rarer total removal of the prostate. It may call for a further operation or for permanent management
(see below under “Persistent Incontinence”).
(2) Stress incontinence: Urine only leaks when the pressure in your abdomen rises to above a certain
level (on coughing, sneezing, lifting, etc). This can be mild, moderate or severe. Stress incontinence is usually
due to a weak, or partially damaged, valve (urinary sphincter) mechanism. It is treated initially (and commonly
successfully) by pelvic floor exercises (see below) but in rare, severe cases may call for further surgery.
(3) Urgency and urge incontinence: You feel the need to pass urine suddenly (“urgency”) and may not
always able to control it (“urge incontinence”). You may well need to pass urine frequently - often in small
amounts - and you may be woken at night or may wet the bed while asleep. Urge incontinence is the result of
overactivity by the muscles which squeeze the bladder to empty it. Before the operation, they had to squeeze
hard to force the urine past the enlarged prostate gland and they may take time - even several months - to
adjust to the removal of the obstruction. (If you had urge incontinence beforehand, it may or may not be cured
by the operation.)
The problem generally disappears over a period of time, but in the meantime useful treatments include pelvic
floor exercises, bladder retraining (see below), and drugs called “anticholinergics” which help control excessive
bladder activity.
(4) Mixed incontinence: This is a combination of stress incontinence and urge incontinence and is
treated accordingly.
(5) After-dribble: The loss of a small amount of urine almost immediately after the bladder has been
emptied is common both before and after prostate operations and tends to increase with age. It may be
because your bladder does not quite empty, or because urine becomes trapped in the bladder outlet,
where the prostate used to be, and leaks out afterwards. This problem usually improves with time but
may be helped if you sit down on the lavatory and lean forwards to pass urine. You can also expel the
last few drops by massaging gently behind the scotum or by performing a pelvic floor muscle squeeze
(see Pelvic Floor Exercises).
Updated January 2014
Pelvic floor exercises
The pelvic floor is a hammock of muscles supporting the bowel and bladder in the abdomen. Strengthening
them will help you with stress and sometimes urge incontinence. You will probably be taught the exercises by
the physiotherapist or nurse specialist at your hospital, but you can also teach yourself to do them.
The first thing to do is to correctly identify the muscles that need to be exercised.
1. Sit comfortably with the muscles of your thighs, buttocks and abdomen relaxed.
2. Tighten the ring of muscle around the back passage as if you are trying to control diarrhoea or wind.
You should be able to feel the muscle move. Try not to squeeze your buttocks or tighten your thighs or tummy
muscles.
3. Now imagine you are passing urine, trying to stop the flow mid-stream, and then restarting it. Do not
try to stop the stream when you are actually passing water as this may, if repeated, cause problems with
correct emptying. If your technique is correct, each time that you tighten your pelvic floor muscles you may feel
a dip at the base of your penis, and your scrotum move up slightly.
Now you can find your pelvic floor muscles, here are the exercises to do:
1. Your pelvic floor muscles need to have stamina. So sit, stand or lie with your knees slightly apart.
Slowly tighten and pull up the pelvic floor muscles as hard as you can. Try lifting and squeezing them as long
as you can. Rest for 4 seconds and then repeat the contraction. Build up your strength until you can do 10 slow
contractions at a time, holding them for 10 seconds each with rests of 4 seconds in between.
2. Your pelvic floor muscles also need to react quickly to sudden stresses from coughing, laughing or
exercise that puts pressure on the bladder. So practise some quick contractions, drawing in the pelvic floor and
holding it for just one second before relaxing. Try to achieve a strong muscle tightening with up to ten quick
contractions in succession.
Aim to do a set of slow contractions (exercise 1) followed by a set of quick contractions (exercise 2) 3-4
times each day. It takes time for exercise to make muscles stronger.
You are unlikely to notice an improvement for some weeks, and you will need to exercise regularly for
several months to get the pelvic floor muscles to their full strength. It is well worth persisting. You can do
the exercises any time, anywhere: if you are doing them right, there will be no external sign, no tensing of
your legs, buttocks or abdomen.
Bladder training
This is a technique by which you retrain your own bladder, usually using a bladder training chart (see page
4). You learn to suppress or ignore the desire to pass urine, so that a more normal pattern is achieved
without the symptoms or accidents of urge incontinence.
Check how often you pass urine and then attempt to increase the time interval between visits to the toilet.
For instance, if you are passing urine roughly every one to one and a half hours, set your target at two
hours, and try to resist the temptation to go before the two hours are up. If you are going ten times a day,
aim for nine times the next day. If you are liable to start leaking urine when you hang on, wearing an
absorbent pad or drip collector may add to your confidence. As you achieve each target interval, you
should gradually increase it until you are only going every three to four hours on average. It can be very
difficult at first, but it really does get easier with practice.
If you find that you can hang on until the set time, but then urgency becomes severe on the way to the
toilet, try counting. Go to the toilet, but count to 10 before you actually start to pass urine. Once you can
do this, increase your counting to 20, 30, 40, etc. Once you can wait for a minute when you are at the
toilet, also start to delay setting off for the toilet. Wait five minutes after you feel the bladder is full before
you stop whatever you are doing, then 10 or 15 minutes, if you can manage this. Pelvic floor exercises
(see above) may also help you to hang on for longer periods.
Bladder training requires considerable willpower and determination - but giving in to your bladder will only
make it worse. “Mind over matter” really can help your problem, but only you can make it work. The less
often you pass urine, the less you will need to go, and eventually you will be able to forget about your
bladder for hours on end. It may take several weeks, or even a couple of months, to get to this stage - so
don’t give up.
Updated January 2014
Persistent Incontinence
If your incontinence does not get better, mention it to the urologist at your post-operative visit, or if it is
severe ask your GP to refer you back to the Urologist without delay so that it can be discussed and
investigated further. There are many reasons why you may be incontinent, and it is clearly important to
establish which applies in your case so that the correct treatment can be chosen.
Such treatment may be measured to control bladder overactivity, exercises or (especially if you have
persistent stress incontinence) you may be advised to have further surgery, perhaps to implant an artificial
sphincter. This can be very successful, but it is obviously an individual decision whether the problem is
causing enough trouble to warrant more surgery.
Occasionally the condition is found to be untreatable or else the treatment available is not suitable for you.
There are then many different types of equipment which may help you to cope with and disguise your
problem, thereby enabling you to lead a full, normal life, despite incontinence. Pads and pants, penile
sheaths, body-worn appliances and dribble pouches are available for different needs. Some are available
on prescription from your GP, others can be obtained via the district nurse or continence adviser.
Assessment by a health professional is important to ensure the most appropriate containment product or
appliance is chosen. Your doctor or nurse should be able to tell you how to contact your local Continence
Adviser.
Further Help
Your own GP or local continence advisor can give you advice. We also have a fact sheet on Pelvic
Floor Exercises for Men which you may find useful. Please visit our Factsheet section on our website
for more information.
On the following pages you will find a bladder diary. You can discuss the use of this with your
continence nurse or health professional and between you if needed, agree a training programme
suited to your needs. Bladder training works by helping you to return to a normal pattern of passing
urine.
Factsheet revised January 2014 - with ongoing acknowledgements to Tom Rosenbaum (Ealing Hospital)
and Chris Chapple (Royal Hallamshire Hospital).
Updated January 2014
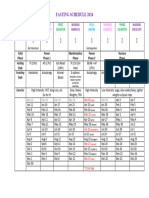
Bladder Diary
Date: I woke up at: I went to sleep at:
Time Record drinks each time you when you changed Each time you leak urine, circle
(type and amount) use the toilet to a pad whether you were:
pass urine
12am Almost Dry Damp Wet Soaked
1am Almost Dry Damp Wet Soaked
2am Almost Dry Damp Wet Soaked
3am Almost Dry Damp Wet Soaked
4am Almost Dry Damp Wet Soaked
5am Almost Dry Damp Wet Soaked
6am Almost Dry Damp Wet Soaked
7am Almost Dry Damp Wet Soaked
8am Almost Dry Damp Wet Soaked
9am Almost Dry Damp Wet Soaked
10am Almost Dry Damp Wet Soaked
11am Almost Dry Damp Wet Soaked
Updated January 2014
Time Record drinks each time you when you changed Each time you leak urine, circle
(type and amount) use the toilet to a pad whether you were:
pass urine
12pm Almost Dry Damp Wet Soaked
1pm Almost Dry Damp Wet Soaked
2pm Almost Dry Damp Wet Soaked
3pm Almost Dry Damp Wet Soaked
4pm Almost Dry Damp Wet Soaked
5pm Almost Dry Damp Wet Soaked
6pm Almost Dry Damp Wet Soaked
7pm Almost Dry Damp Wet Soaked
8pm Almost Dry Damp Wet Soaked
9pm Almost Dry Damp Wet Soaked
10pm Almost Dry Damp Wet Soaked
11pm Almost Dry Damp Wet Soaked
Reminders
1. Don’t forget to record the time you woke up in the morning and the time you went to sleep.
2. Don’t forget to record what happened overnight when you get up in the morning.
3. Try and make a record of things just after they happen in case you forget them later on.
4. Record things to the nearest hour.
5. Record type and amount of drinks taken (e.g. 2 cups of tea, 1 mug of coffee, 1 can of coke, 1 glass of water/wine /juice, 2½ pints of beer)
6. Start a new sheet for each new day.
Updated January 2014
'The Bladder and Bowel Community provides information and support for people with bladder and
bowel issues. We publish a wide range of user friendly booklets and factsheets.
For more information please call us on 01926 357220, email help@bladderandbowelfoundation.org
or write to us at The Bladder and Bowel Community, 7 The Court, Holywell Business Park, Northfield
Road, Southam, CV47 0FS.
www.bladderandbowelfoundation.org
Registered office address: Pegasus House, Solihull Business Park, Solihull, West Midlands,
United Kingdom, B90 4GT. Company number: 10377236. Registered in the UK
Updated January 2014
You might also like
- Continence and Prostate: A Guide For Men Undergoing Prostate SurgeryDocument7 pagesContinence and Prostate: A Guide For Men Undergoing Prostate Surgeryc223096No ratings yet
- Continence Problems After StrokeDocument8 pagesContinence Problems After StrokeYocha BangunNo ratings yet
- Reversal of IleostomyDocument7 pagesReversal of IleostomyGTL StickersNo ratings yet
- Reduced Bladder EmptyingDocument2 pagesReduced Bladder EmptyingThe Saloniti BabiesNo ratings yet
- Top 17 Questions in Urology: in This Chapter, We'll Go Over Common Health Problems in UrologyDocument13 pagesTop 17 Questions in Urology: in This Chapter, We'll Go Over Common Health Problems in UrologyadenwijayaNo ratings yet
- The Coombe Physiotherapy & Your Pelvic Floor Feb 2021Document20 pagesThe Coombe Physiotherapy & Your Pelvic Floor Feb 2021Andreea ManeaNo ratings yet
- Abdominal Rectopexy Operation: Your Questions AnsweredDocument5 pagesAbdominal Rectopexy Operation: Your Questions AnsweredlakanthNo ratings yet
- Urinary Incontinence Has Sesven TypesDocument55 pagesUrinary Incontinence Has Sesven TypesDhonat Flash100% (1)
- Urinary Incontinence Brochure 2009Document5 pagesUrinary Incontinence Brochure 2009swap2390No ratings yet
- Urodynamic Testing ReportDocument25 pagesUrodynamic Testing Reportzharah180% (1)
- Faecal IncontinenceDocument21 pagesFaecal IncontinenceDee wilsonNo ratings yet
- Bladder Training PDFDocument5 pagesBladder Training PDFDjfnswn UkhtyNo ratings yet
- Pelvic Floor Exercises For MenDocument5 pagesPelvic Floor Exercises For MenGabrielMouraNo ratings yet
- FghikDocument3 pagesFghikfahfahrulNo ratings yet
- Rectal ProlapseDocument9 pagesRectal ProlapseAnjani Putri RetnaninggalihNo ratings yet
- Physiotherapy Before and After Prostate Cancer Surgery PDFDocument8 pagesPhysiotherapy Before and After Prostate Cancer Surgery PDFJohn SterlingNo ratings yet
- 5960 1 Hartmanns ProcedureDocument8 pages5960 1 Hartmanns ProcedurecosmicdaeNo ratings yet
- IncontenenceDocument5 pagesIncontenenceMuhammad Omar KhanNo ratings yet
- Urinary Incontinence: The American College of Obstetricians and GynecologistsDocument3 pagesUrinary Incontinence: The American College of Obstetricians and GynecologistsIzat FuadiNo ratings yet
- After TURP: What to expectDocument2 pagesAfter TURP: What to expectvilla88No ratings yet
- SCI Bladder SurgeryDocument4 pagesSCI Bladder SurgeryKrish NevageNo ratings yet
- Bowel IncontinenceDocument10 pagesBowel Incontinenceibrahim 12No ratings yet
- Pelvic Floor Muscle Exercises and Advice For MenDocument8 pagesPelvic Floor Muscle Exercises and Advice For Mensantjitr679No ratings yet
- Urinary Problems-IfmDocument16 pagesUrinary Problems-Ifmapi-675909478No ratings yet
- Information For You: Pelvic Organ ProlapseDocument8 pagesInformation For You: Pelvic Organ Prolapsesandeepv08No ratings yet
- Pelvic Floor Exercises: A Guide For Men AboutDocument3 pagesPelvic Floor Exercises: A Guide For Men AboutemagooNo ratings yet
- Trans Urethral Resection of The ProstateDocument2 pagesTrans Urethral Resection of The ProstatehypopiaNo ratings yet
- Total Proctocolectomy With IleostomyDocument5 pagesTotal Proctocolectomy With Ileostomyrachelmores12No ratings yet
- What Causes Urinary Retention?Document4 pagesWhat Causes Urinary Retention?darkz_andreaslimNo ratings yet
- Elimination Review: Urinary Function and Nursing CareDocument27 pagesElimination Review: Urinary Function and Nursing Careالموعظة الحسنه chanelNo ratings yet
- Urinary Elimination DisordersDocument42 pagesUrinary Elimination DisordersMara Jon Ocden CasibenNo ratings yet
- Cystoscopy WordDocument4 pagesCystoscopy WordMon ManguilinNo ratings yet
- PS-27238-Spotlightguide-Pelvic Floor Excercises A5 JCDocument4 pagesPS-27238-Spotlightguide-Pelvic Floor Excercises A5 JCKishor KumarNo ratings yet
- Cystoscopy OSCEDocument5 pagesCystoscopy OSCEKevin TangNo ratings yet
- Comprehensive Overview of Constipation: William E. Whitehead, PHD Center Co-DirectorDocument3 pagesComprehensive Overview of Constipation: William E. Whitehead, PHD Center Co-DirectornehaNo ratings yet
- Urinary Incontinence: 2 PathophysiologyDocument8 pagesUrinary Incontinence: 2 PathophysiologyZiedTrikiNo ratings yet
- Pelvic Floor Exercises For Men Info SheetDocument3 pagesPelvic Floor Exercises For Men Info SheetTracey BrownNo ratings yet
- HOLEP-info-sheetDocument9 pagesHOLEP-info-sheetcjmrioNo ratings yet
- INCONTINENCE3Document12 pagesINCONTINENCE3allthingali217No ratings yet
- The Rules of Dating - Penelope WardDocument16 pagesThe Rules of Dating - Penelope WardRichard CortezNo ratings yet
- Clinical ReasoningDocument2 pagesClinical ReasoningJOHN PEARL FERNANDEZNo ratings yet
- Overactive BladderDocument4 pagesOveractive BladderRanda Hayudha SNo ratings yet
- 5960 1 Hartmanns ProcedureDocument8 pages5960 1 Hartmanns ProcedureZakiNo ratings yet
- Prostatectomy Procedures and Risks ExplainedDocument11 pagesProstatectomy Procedures and Risks ExplainedPhyan HyunNo ratings yet
- Anal Sphincter Exercises for LeakageDocument6 pagesAnal Sphincter Exercises for LeakageNicolae NedeaNo ratings yet
- Urinary RetentionDocument6 pagesUrinary RetentiongradnurseNo ratings yet
- Transobturator Midurethral SlingDocument32 pagesTransobturator Midurethral SlingclaudiuNo ratings yet
- Fecal ImpactionDocument5 pagesFecal Impactioncharie2No ratings yet
- A Guide To The Pelvic Floor Muscles - Men: Oxford University HospitalsDocument8 pagesA Guide To The Pelvic Floor Muscles - Men: Oxford University HospitalsshamsulNo ratings yet
- Pelvic Floor Exercises For WomenDocument3 pagesPelvic Floor Exercises For Womenreza.7868910100% (2)
- Anorectal MalformationDocument19 pagesAnorectal MalformationRahma Dewi RadhewNo ratings yet
- Accidental Bowel Leakage: The American College of Obstetricians and GynecologistsDocument4 pagesAccidental Bowel Leakage: The American College of Obstetricians and GynecologistsPaulNo ratings yet
- The Pelvic Floor Muscles - A Guide For WomenDocument12 pagesThe Pelvic Floor Muscles - A Guide For WomenQORI KARUNIA WANTINo ratings yet
- Prostate, Functions, Diseases A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandProstate, Functions, Diseases A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Skills LabDocument20 pagesSkills LabJei JayNo ratings yet
- Nephrectomy: The Advantages of Laparoscopic Surgery IncludeDocument5 pagesNephrectomy: The Advantages of Laparoscopic Surgery IncludeLouie ParillaNo ratings yet
- Urinary Diversion: Ileovesicostomy/Ileal Loop/Colon Loop: Why Do I Need This Surgery?Document6 pagesUrinary Diversion: Ileovesicostomy/Ileal Loop/Colon Loop: Why Do I Need This Surgery?Panji SetyawanNo ratings yet
- Cystocele, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandCystocele, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Urinary Retention, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandUrinary Retention, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsRating: 1 out of 5 stars1/5 (1)
- A Simple Guide to Disorders of Pelvic Floor Organs, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Disorders of Pelvic Floor Organs, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Bener 016Document7 pagesBener 016Yosalfa Adhista KurniawanNo ratings yet
- Grabbe 2016Document12 pagesGrabbe 2016Yosalfa Adhista KurniawanNo ratings yet
- Zelio Timer Relays - RUZC2MDocument3 pagesZelio Timer Relays - RUZC2MYosalfa Adhista KurniawanNo ratings yet
- Paulownia Tree Potential Alternative Raw Material for Pencil ManufacturingDocument8 pagesPaulownia Tree Potential Alternative Raw Material for Pencil ManufacturingYosalfa Adhista KurniawanNo ratings yet
- COVID 19 Coding Icd10Document4 pagesCOVID 19 Coding Icd10Yosalfa Adhista KurniawanNo ratings yet
- Ijer v2Document13 pagesIjer v2Yosalfa Adhista KurniawanNo ratings yet
- Accepted Manuscript: Accident Analysis and PreventionDocument25 pagesAccepted Manuscript: Accident Analysis and PreventionYosalfa Adhista KurniawanNo ratings yet
- Cum Cultivi Paulownia, Culturi Intercalate71235Document74 pagesCum Cultivi Paulownia, Culturi Intercalate71235Dragos Ranca100% (1)
- WHO 2019 nCoV SARI - Toolkit 2020.1 Eng PDFDocument196 pagesWHO 2019 nCoV SARI - Toolkit 2020.1 Eng PDFbeny nurjaman100% (1)
- 0Document2 pages0Yosalfa Adhista KurniawanNo ratings yet
- 0921Document12 pages0921Yosalfa Adhista KurniawanNo ratings yet
- Mankir 209Document10 pagesMankir 209Yosalfa Adhista KurniawanNo ratings yet
- Rosadi 219Document20 pagesRosadi 219Yosalfa Adhista KurniawanNo ratings yet
- Jaya 215Document10 pagesJaya 215Yosalfa Adhista KurniawanNo ratings yet
- Anemia During PregnancyDocument8 pagesAnemia During Pregnancyekaseptiani312No ratings yet
- An OCT Study of Anterior Nodular Episcleritis and PDFDocument4 pagesAn OCT Study of Anterior Nodular Episcleritis and PDFYosalfa Adhista KurniawanNo ratings yet
- 0Document2 pages0Yosalfa Adhista KurniawanNo ratings yet
- DepthDocument12 pagesDepthYosalfa Adhista KurniawanNo ratings yet
- 0Document2 pages0Yosalfa Adhista KurniawanNo ratings yet
- Penaloza 2018Document7 pagesPenaloza 2018Yosalfa Adhista KurniawanNo ratings yet
- 0Document2 pages0Yosalfa Adhista KurniawanNo ratings yet
- 0Document2 pages0Yosalfa Adhista KurniawanNo ratings yet
- Alinco DR-135T DR-135E Instruction - Manual PDFDocument47 pagesAlinco DR-135T DR-135E Instruction - Manual PDFYosalfa Adhista KurniawanNo ratings yet
- Discrete POWER & Signal TechnologiesDocument4 pagesDiscrete POWER & Signal TechnologiesArief SaladdinNo ratings yet
- Koljonen 2012Document7 pagesKoljonen 2012Yosalfa Adhista KurniawanNo ratings yet
- NSFWDocument3 pagesNSFWYosalfa Adhista KurniawanNo ratings yet
- N-Channel - Depletion: Semiconductor Technical DataDocument4 pagesN-Channel - Depletion: Semiconductor Technical DataLaAngelitaOropezaNo ratings yet
- Accepted Manuscript: Accident Analysis and PreventionDocument25 pagesAccepted Manuscript: Accident Analysis and PreventionYosalfa Adhista KurniawanNo ratings yet
- A Novel Neurotrophic Drug For Cognitive Enhancement and Alzheimer's DiseaseDocument17 pagesA Novel Neurotrophic Drug For Cognitive Enhancement and Alzheimer's DiseaseYosalfa Adhista KurniawanNo ratings yet
- Parviz I 2003Document13 pagesParviz I 2003Yosalfa Adhista KurniawanNo ratings yet
- Business Analysis FoundationsDocument39 pagesBusiness Analysis FoundationsPriyankaNo ratings yet
- Variables in Language Teaching - The Role of The TeacherDocument34 pagesVariables in Language Teaching - The Role of The TeacherFatin AqilahNo ratings yet
- Internal Peripherals of Avr McusDocument2 pagesInternal Peripherals of Avr McusKuldeep JashanNo ratings yet
- MECHANICAL PROPERTIES OF SOLIDSDocument39 pagesMECHANICAL PROPERTIES OF SOLIDSAbdul Musavir100% (1)
- Hisar CFC - Approved DPRDocument126 pagesHisar CFC - Approved DPRSATYAM KUMARNo ratings yet
- X RayDocument16 pagesX RayMedical Physics2124No ratings yet
- Electrical Design Report For Mixed Use 2B+G+7Hotel BuildingDocument20 pagesElectrical Design Report For Mixed Use 2B+G+7Hotel BuildingEyerusNo ratings yet
- SeparatorDocument2 pagesSeparatormmk111No ratings yet
- Kltdensito2 PDFDocument6 pagesKltdensito2 PDFPutuWijayaKusumaNo ratings yet
- Final - WPS PQR 86Document4 pagesFinal - WPS PQR 86Parag WadekarNo ratings yet
- Digital Water Monitoring and Turbidity Quality System Using MicrocontrollerDocument8 pagesDigital Water Monitoring and Turbidity Quality System Using MicrocontrollerIrin DwiNo ratings yet
- 2010 HSC Exam PhysicsDocument42 pages2010 HSC Exam PhysicsVictor345No ratings yet
- 19 Unpriced BOM, Project & Manpower Plan, CompliancesDocument324 pages19 Unpriced BOM, Project & Manpower Plan, CompliancesAbhay MishraNo ratings yet
- Mechanical Engineer with Experience in Heavy Mining Machinery MaintenanceDocument1 pageMechanical Engineer with Experience in Heavy Mining Machinery MaintenanceCertified Rabbits LoverNo ratings yet
- Moon Fast Schedule 2024Document1 pageMoon Fast Schedule 2024mimiemendoza18No ratings yet
- Ahu, Chiller, Fcu Technical Bid TabulationDocument15 pagesAhu, Chiller, Fcu Technical Bid TabulationJohn Henry AsuncionNo ratings yet
- L Williams ResumeDocument2 pagesL Williams Resumeapi-555629186No ratings yet
- Sia Mock+Test 1 Csat Updated CompressedDocument216 pagesSia Mock+Test 1 Csat Updated Compressedpooja bhatiNo ratings yet
- 5.a Personal Diet Consultant For Healthy MealDocument5 pages5.a Personal Diet Consultant For Healthy MealKishore SahaNo ratings yet
- Design ThinkingDocument16 pagesDesign ThinkingbhattanitanNo ratings yet
- Advanced Presentation Skills: Creating Effective Presentations with Visuals, Simplicity and ClarityDocument15 pagesAdvanced Presentation Skills: Creating Effective Presentations with Visuals, Simplicity and ClarityGilbert TamayoNo ratings yet
- TILE FIXING GUIDEDocument1 pageTILE FIXING GUIDEStavros ApostolidisNo ratings yet
- Week 4 Gen EconDocument10 pagesWeek 4 Gen EconGenner RazNo ratings yet
- EST I - Literacy Test I (Language)Document20 pagesEST I - Literacy Test I (Language)Mohammed Abdallah100% (1)
- ClientsDocument7 pagesClientsLiane PanahacNo ratings yet
- Serendipity - A Sociological NoteDocument2 pagesSerendipity - A Sociological NoteAmlan BaruahNo ratings yet
- English Extra Conversation Club International Women's DayDocument2 pagesEnglish Extra Conversation Club International Women's Dayevagloria11No ratings yet
- 13Document47 pages13Rohan TirmakheNo ratings yet
- Presentation 1Document20 pagesPresentation 1nikitakhanduja1304No ratings yet
- European Business in China Position Paper 2017 2018 (English Version)Document408 pagesEuropean Business in China Position Paper 2017 2018 (English Version)Prasanth RajuNo ratings yet