Professional Documents
Culture Documents
Chapter 4 Ventilator Parameters PDF
Uploaded by
hoan leOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chapter 4 Ventilator Parameters PDF
Uploaded by
hoan leCopyright:
Available Formats
CHAPTER FOUR
VENTILATOR PARAMETERS
OBJECTIVES
Know the breath types.
Know the modes of ventilation.
Understand high frequency ventilation.
Know the different methods of high frequency ventilation.
Know the difference between a pressure-supported breath and a spontaneous
breath.
Know the difference between IMV and SIMV.
Know what PEEP is.
Know what CPAP is.
Understand the difference between PEEP and CPAP.
Identify the breath type by its waveform.
INTRODUCTION:
Today's ventilators provide a myriad of ways to provide ventilatory support to the
patient. The availability of so many different choices of ventilation allows the
practitioner to tailor the ventilator to the needs of the patient. In addition to
providing different methods of ventilation, today's ventilators also provide more
control to the practitioner in recognizing developing situations, which may affect
patient safety. In this chapter, we will learn the three breath types, as well as the
different modes of ventilation. Additionally, we will learn the different ventilator
parameters, which signal that a situation detrimental to the patient is developing.
Lastly, we will learn to recognize the breath type by its waveform.
Ventilator Study Guide – Rev. A02
Chapter 4, Page 1
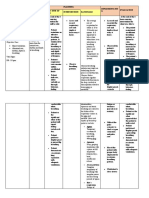
Breath Types: There are three fundamental
breath types; controlled, assisted and
spontaneous.
Controlled: A controlled (machine) breath
delivers gas to the patient according to the
control variable set by the operator, i.e.,
pressure controlled or volume/flow controlled,
at a fixed frequency or respiratory rate. In the
absence of a patient initiated inspiratory effort,
the ventilator will deliver a controlled breath.
Controlled breaths are terminated when the
preset cycle variable is reached, i.e., pressure,
volume, or time. The illustration at the right represents a controlled breath delivered
by a flow controller ventilator.
Assisted: An assisted breath may either
replace or be in addition to controlled breaths.
An assisted breath is initiated when the
patient's inspiratory effort is equal to the
sensitivity setting. This breath type will deliver
gas to the patient as determined by the preset
control variables and be terminated by the
preset cycle variables. The illustration
represents an assisted breath being delivered
by a flow controller ventilator.
Spontaneous: Spontaneous breaths are
based on patient demand. Flow and volume
are determined by the patient’s inspiratory effort. Flow is initiated when the patient's
inspiratory effort is equal to the sensitivity setting. The greater the inspiratory effort,
the greater the flow delivered. After an initial high flow rate, flow is then decreased
to maintain a preset baseline level. A spontaneous breath is generally terminated
when the patient's demand for flow falls below a particular threshold.
Ventilator Study Guide – Rev. A02
Chapter 4, Page 2
Modes of Ventilation.
Control Mode: The control mode of
ventilation delivers only controlled breaths to
the patient. This mode fully supports patients
in respiratory failure. The ventilator is
triggered by the preset machine rate, and
inspiration is ended according to the preset
cycle variables.
Assist/Control Mode: The assist/control
mode of ventilation allows the patient to
initiate a breath. The respiratory rate is established by the preset machine rate and
any spontaneous breathing from the patient. In the absence of a patient initiated
effort, a controlled breath will be delivered. If the ventilator senses a patient
initiated effort, an assisted breath will be delivered. Assisted and controlled breaths
are terminated after the preset cycle variable has been reached.
IMV (Intermittent Mandatory Ventilation): IMV mode of ventilation allows the
patient to breathe spontaneously between controlled breaths. The respiratory rate
is used to ensure that the ventilator will provide support should the patient fail to
breathe. With IMV it is possible for the ventilator to deliver a controlled breath
during a spontaneous inspiration, known as breath stacking, which results in
abnormally large tidal volumes and high peak airway pressures. To overcome the
breath stacking problem, Synchronous Intermittent Mandatory Ventilation (SIMV)
was developed.
SIMV (Synchronous Intermittent Mandatory Ventilation): In the SIMV mode,
machine breaths are synchronized with spontaneous breaths to avoid breath
stacking. Synchronization is accomplished by dividing the respiratory rate into
SIMV cycles. A patient is allowed to breathe spontaneously during these cycles. If
no inspiratory effort is sensed by the ventilator, a controlled breath will be delivered
at the beginning of the next SIMV cycle.
EMMV (Extended Mandatory Minute Ventilation): This mode of ventilation is
based on the patient's spontaneous ventilation. The practitioner sets a minimum
mandatory minute volume the patient needs to accomplish. Then he adjusts the
ventilator's volume and flow settings needed to accomplish the minute volume
setting. If the patient meets or exceeds the minute volume requirement breathing
spontaneously, then no controlled breaths are delivered. If the patient fails to meet
the minimum minute volume requirement, the ventilator begins to deliver controlled
breaths until the minute volume is reached. This mode is useful in weaning patients
from mechanical ventilation.
Ventilator Study Guide – Rev. A02
Chapter 4, Page 3
CPAP (Continuous Positive Airway Pressure): The patient breathes
spontaneously in this mode. Airway pressure is elevated relative to atmosphere to
increase functional residual capacity. The patient must trigger demand flow by
exceeding the preset sensitivity level. The gas flow rate is determined by how far
the patient's inspiratory effort pulls the trigger variable below the baseline level, and
by the slope of the effort. Flow is then metered in response to maintaining the
CPAP level. The breath is terminated when the patient's demand for flow falls
below a particular threshold.
PEEP (Positive End Expiratory Pressure). This mode is similar to CPAP, except
that it is used during mechanical breaths. The airway pressure is elevated relative
to atmosphere based on the pressure desired at the end of expiration. The reasons
for employing PEEP are the same as in CPAP, i.e., increasing FRC, increasing
PaO2, increasing compliance, lowering work of breathing and reducing atelectasis.
PCIRV (Pressure Controlled Inverse-Ratio Ventilation): This form of ventilation
delivers a mechanical breath in which the inspiratory time is longer than the
expiratory time. Measured as the ratio of inspiratory time to expiratory time, I:E
Ratios as high as 4:1 can be achieved. Patients who require this type of ventilation
are generally sedated and paralyzed. The effect of PCIRV is an elevation in end
expiratory pressure. This occurs because the expiratory time is not long enough to
completely expel a breath before another mechanical breath is delivered. The end
result is gas trapping in the patient's lungs and an increase in end expiratory
pressure. By elevating the end expiratory pressure, functional residual capacity is
believed to increase due to the recruitment of more alveoli. It is also believed that
longer, slower inspirations increase the distribution of gas in the lungs.
Apnea: Apnea ventilation is initiated when the preset apnea alarm is triggered.
The ventilator will begin to deliver controlled breaths at the operator selected
settings. Apnea ventilation is terminated when the patient begins to breathe
spontaneously or a manual breath is delivered to the patient.
Pressure Support or Positive Pressure Support: Pressure support augments a
patient's spontaneous effort with a preset amount of positive airway pressure.
Pressure Supported spontaneous breaths are initiated the same as regular
spontaneous breaths, i.e., based on the patient's inspiratory effort. Once the
sensitivity setting has been triggered, the ventilator quickly servos the flow to
maintain the amount of pressure support selected by the clinician. Flow delivered to
the patient is determined by, and directly proportional to, the pressure gradient
between the patient circuit and the lung pressure. The greater the gradient, the
greater the flow. The gradient will depend on the inspiratory effort of the patient, as
well as the level of PPS set. Other factor's affecting the flow are the resistance and
compliance of the lungs. Flow is terminated when the pressure gradient between
Ventilator Study Guide – Rev. A02
Chapter 4, Page 4
the lungs and the patient circuit is zero. By having the support pressure present,
the patient may not have to work as hard to maintain the spontaneous breath.
High Frequency Ventilation: High frequency ventilation is primarily indicated for
use with neonatal patients ranging from 23 to 41 weeks gestational age (although
there are some adult ventilators with high frequency capability). These patients
typically suffer from Respiratory Distress Syndrome, have pulmonary air leaks, or
perhaps suffer from pulmonary interstitial emphysema (PIE).
High frequency ventilation ventilates patients with unusually high breath rates and
low tidal volumes. The rate or frequency can range from 150 to 1500 breaths per
minute. As the frequencies increase, the hertz designation is used. As the
frequency increases, smaller tidal volumes are delivered to the point where alveolar
ventilation takes place at volumes less than the dead space. Gas exchange in this
mode of ventilation is poorly understood, but is believed to take place based on the
following:
• Gas mixing occurring due to turbulence caused by increasing bronchial
divisions.
• Gas mixing occurring due to turbulence caused by oscillations in flow.
• Gas mixing occurring due to turbulence created due to high instantaneous
peak flows.
• The Pendeluft effect or gas exchange occurring as some alveoli are filling,
while others are evacuating.
A major consideration in the frequency limitations of high frequency ventilation is
gas trapping. Gas trapping occurs when the elastic recoil of the lungs is not
sufficient to expel the amount of delivered gas passively during the allotted
expiratory phase of the respiratory cycle. In other words, as the frequency of
ventilation increases, the expiratory time becomes proportionally shorter. As the
expiratory times becomes shorter, the time allotted to expel the delivered gas is
decreased. Eventually, a breath will be delivered before the patient exhales to
baseline, trapping a portion of the previously delivered volume in his lungs. This
can continue until dangerously high airway pressures develop, which can eventually
lead to barotrauma.
High frequency ventilator design therefore can be classified by 1) the mechanism of
delivery, and 2) control over the expiratory phase of the respiratory cycle. Basically,
HFV ventilators are classified into five categories:
1. HFPPV (High Frequency Positive Pressure Ventilation):
HFPPV ventilators are basically conventional ventilators with the
ability to provide higher frequencies of ventilation, typically from 60 to
150 bpm. Exhalation in this type of ventilator is passive.
Ventilator Study Guide – Rev. A02
Chapter 4, Page 5
2. HFJV (High Frequency Jet Ventilation): HFJV ventilators
utilize a solenoid driven, high-pressure gas source to provide rates of
240 to 660 bpm. This type of ventilator utilizes a special triple lumen
endotracheal adapter to deliver volume pulses to the patient.
Exhalation is passive in this type of ventilator, thus limiting the
frequency to the above-mentioned rate.
3. HFOV (High Frequency Oscillator Ventilation): This device
utilizes a sealed diaphragmatic piston pump to deliver gas at
frequencies of 10 - 30 Hz. Exhalation is active, thus the higher
frequencies being utilized.
4. HFFI (High Frequency Flow Interrupter): This device
employs small volumes delivered at high frequencies by interrupting a
flow or high-pressure source. However, in contrast to HFJV, this
device does not require a special endotracheal tube. Expiration is
passive, thus limiting the frequency of breaths.
5. HYBRID: This device is also called a flow Oscillator. The
Hybrid vent delivers an instantaneous flow to the patient via a system
of proportional solenoid valves. Expiration is active and assisted
through the incorporation of a jet venture system. The frequency
range of this type of ventilator is 2 - 22 Hz.
Other Ventilator Parameters: Today's ventilators offer many options to the
clinician to tailor a ventilator to the patient's needs. Listed below are some of the
other parameters which the clinician uses in "setting up" a ventilator.
Tidal Volume: Measured in milliliters (mls), this parameter determines the amount
of volume to be delivered during a machine breath.
Machine or Respiratory Rate: Measured in breaths per minute (BPM), this
parameter determines the frequency for control breaths.
Peak Flow. Measured in liters per minute (LPM), this parameter controls the flow
rate to be delivered to the patient during a machine breath.
Oxygen Percentage (FiO2): Measured as a fraction Of 100% oxygen, this
parameter controls the oxygen concentration in the inspired gas .
PEEP/CPAP (Positive End Expiratory Pressure/Continuous Positive Airway
Pressure): Measured in cmH2O, these determine the airway pressure above
atmospheric pressure.
Ventilator Study Guide – Rev. A02
Chapter 4, Page 6
Sensitivity: Can be measured in cmH2O or LPM, depending on the type of
triggering system, this parameter determines the amount of inspiratory effort
required by the patient before the ventilator will deliver an assisted breath, or
demand flow in the case of a spontaneous breath.
lnspiratory Pause or Plateau: Measured in seconds, this parameter delays
exhalation, therefore lengthening inspiration.
Waveform: This parameter controls the flow pattern in which machine breaths are
delivered to the patient. The four commonly used waveforms:
• Square Wave: Delivers a constant flow of gas at the peak flow setting.
• Accelerating Wave: Delivers flow in a linearly increasing fashion until peak
flow is reached.
• Decelerating Wave: Delivers flow at the peak flow setting then linearly
decreases flow.
• Sine Wave: Delivers a sinusoidal flow pattern where the curve’s peak is
equal to the peak flow setting.
Sigh Volume: Measured in milliliters (mls), this parameter controls the volume of
gas delivered during a sigh breath.
Sigh Rate: Measured in sighs per hour (sph), this parameter controls the number
of sighs to be delivered in an hour.
Multiple Sighs: This parameter controls the number of sigh breathes delivered in
succession at the selected sigh rate.
Peak Inspiratory Pressure or Inspiratory Pressure: Measured in cmH2O, this
parameter controls the maximum inspiratory pressure to be delivered to the patient
during a pressure controlled machine breath.
lnspiratory Time: Measured in seconds, this parameter controls the duration of the
inspiratory phase of the breath cycle.
I:E Ratio: This parameter controls the ratio of inspiration to expiration in relation to
the machine rate. For example, if the machine rate = 10 bpm, this would produce a
total inspiratory/expiratory time of 6 seconds. By setting the I:E ratio to 1:1, this
equalizes the inspiration and exhalation times at 3 seconds each, by the following
equation:
Ventilator Study Guide – Rev. A02
Chapter 4, Page 7
I/E : E/E or 3/3 : 3/3 or 1:1
The ventilator would then deliver a breath with an inspiratory time of 3 seconds.
Ventilator Alarms: There are many different alarm options that are available to the
clinician today. These alarms enhance the ventilator's role in the patient's care by
improving the patient's safety. Alarms can either be set by the operator or are
automatically monitored.
Operator Set Alarms: These alarms are set by the clinician according to the
parameters he feels the patient's care should operate within. Some of these alarms
are passive (i.e., sound an alarm, with no corresponding intervention on the part of
the machine) and active (i.e., the machine responds by sounding an alarm, and
immediately corrects the situation).
Automatic Alarms: These alarms are not typically set by the operator. If these
alarms are triggered, it is usually indicative of a situation that could seriously
endanger the patient. Consequently, these alarms are active and they attempt to
correct the situation immediately.
Monitored Parameters: In order for the clinician to assess the patient's care and
progress, it is necessary for him to be able to see at a glance how the patient is
responding to treatment. Ventilators typically monitor several parameters and
display them graphically on their control panel. Shown below is the parameters
generally monitored.
Exhaled Tidal Volume: This parameter provides the numerical representation of
the patient's volume of exhaled air.
Minute Volume: Represents the patient's exhaled tidal volume (mechanical and
spontaneous) over time.
Spontaneous Minute Volume: This represents the patient's spontaneous exhaled
tidal volume over time.
Breath Type: This parameter indicates what type of breath the ventilator delivered,
i.e., controlled, assisted or spontaneous.
Peak Pressure: Indicates the peak inspiratory pressure achieved during the last
delivered breath.
Mean Airway Pressure: This indicates the mean (average) pressure in the airway
over the last minute.
PEEP/CPAP Pressure: Indicates the baseline pressure.
Ventilator Study Guide – Rev. A02
Chapter 4, Page 8
Plateau Pressure: This parameter indicates the airway pressure during an
inspiratory pause. This is used in the calculation of static compliance.
Breath Rate. Represents the total breaths (machine and spontaneous) delivered
by the ventilator during the last minute.
I:E Ratio: Represents the numerical ratio of inspiration time to expiration time.
lnspiratory Time: Represents the duration of machine or spontaneously delivered
breaths.
Duration of Positive Pressure: Represents the time positive pressure is applied to
the airway 1cmH2O above baseline for the last mandatory breath. This parameter
is typically seen in neonatal ventilators.
REVIEW
There are many ventilatory modes available to the clinician in today's ventilators.
This allows the clinician greater flexibility in the management of patient care.
There are three fundamental breath types; controlled, assisted, and spontaneous.
The modes of ventilation include Control, Assist/Control, IMV, SIMV, EMMV, CPAP,
PEEP, PCIRV, Apnea, Positive Pressure Support (PPS), and High Frequency
Ventilation (HFV).
High frequency ventilation is indicated for use with neonatal patients from 23 to 41
weeks gestational age suffering from RDS, pulmonary air leaks, and/or PIE. HFV
ventilators are classified according to their delivery systems, and their frequency
limitation is based on their control over expiration. The five classes of HFV
ventilator's are HFPPV (High Frequency Positive Pressure Ventilation), HFJV.
(High Frequency Jet Ventilation), HFOV (High Frequency Oscillator Ventilation) and
HFFI (High Frequency Flow Interrupters) and HYBRID.
The clinician has a great deal of flexibility in selecting parameters to attain the
highest degree of patient care. Included are the parameters dealing with the "set
up" of the ventilator. Additionally, patient safety is enhanced through ventilator
alarm functions, both automatic and those selected by the operator. Alarm
functions can be thought of as being active and passive. Active alarms provide a
visual/audible alarm, in addition to active intervention on the part of the ventilator to
correct the situation. Passive alarms provide an audible/visual alert to the operator
identifying a change in the patient status.
Ventilator Study Guide – Rev. A02
Chapter 4, Page 9
In order for the clinician to assess the management of the patient's care, he must be
able to obtain the information at a glance, which relates to the patient's response to
therapy. The ventilator provides this information through the monitored parameters
Ventilator Study Guide – Rev. A02
Chapter 4, Page 10
CHAPTER QUIZ
1. The three breath types are ____________________, ____________________
and ___________________.
2. A ________________________ breath is determined by a preset frequency and
independent of the patient's inspiratory effort.
3. _______________________________ breath is independent of the ventilators
preset frequency and the patient determines his own tidal volume and flow.
4. The difference between CPAP and PEEP is that PEEP is used during
___________________________ ventilation.
5. The ____________________________ mode was developed to avoid breath
stacking .
6. The ________________________ mode is based on the patient's spontaneous
entilation.
7. The ___________________________ mode delivers a mechanical breath in
which the inspiratory phase is longer than the expiratory phase.
8. The ____________________________ mode is triggered if the patient does not
breathe within a preset time.
9. The difference between a spontaneous breath and a pressure supported
spontaneous breath, is that pressure support ____________________ a
spontaneous breath with a preset amount of positive pressure.
10. A major consideration in the frequency limitation of high frequency ventilation is
_______________________.
11. The HFV ventilator, which delivers frequencies of 2 - 22 Hz, and expiration, is an
active jet.
12. venturi is called a ________________________________.
13. The _____________________________ ventilator has a frequency from 240 to
660 bpm and requires a triple lumen endotracheal adapter.
14. This parameter determines the amount of inspiratory effort required by the
patient to trigger a breath: it is called the ________________________setting.
Ventilator Study Guide – Rev. A02
Chapter 4, Page 11
15. The ____________________________________ is the numerical
representation of the inspiratory time to the expiratory time.
16. The four commonly used waveforms are:
a. _______________________
b. _______________________
c. _______________________
d. _______________________
Ventilator Study Guide – Rev. A02
Chapter 4, Page 12
You might also like
- Bustamante, Anjaneth C. Bsrtp-3ADocument13 pagesBustamante, Anjaneth C. Bsrtp-3AMite giteNo ratings yet
- Modes of Ventilation CCU PPT3Document8 pagesModes of Ventilation CCU PPT3chesang507No ratings yet
- Mechanical Ventilation BookletDocument92 pagesMechanical Ventilation BookletJose CastellonNo ratings yet
- Mechanical Ventilation in Pediatric PracticeDocument11 pagesMechanical Ventilation in Pediatric PracticeHandris YanitraNo ratings yet
- Ventilator Quick Guide PDFDocument2 pagesVentilator Quick Guide PDFÖzgür Barışcan KayaNo ratings yet
- Mechanical Ventilation TherapyDocument17 pagesMechanical Ventilation TherapyFaizal FlNo ratings yet
- Respiratory Waveforms in Mechanical VentilationDocument43 pagesRespiratory Waveforms in Mechanical VentilationLoralie Evangeline Perez-Miranda100% (1)
- Mechanical VentilationDocument8 pagesMechanical VentilationMir MirNo ratings yet
- Mechanical Ventilatior: CCC C CCCCCCCCCC PDocument4 pagesMechanical Ventilatior: CCC C CCCCCCCCCC PWendz Palma-TudaNo ratings yet
- Mechanical VentilationDocument37 pagesMechanical Ventilationmzapanta_2No ratings yet
- Mechanical Ventilation Modes and Settings ExplainedDocument84 pagesMechanical Ventilation Modes and Settings Explainedأبوأحمد الحكيم100% (1)
- Suplemento Standardized Vocabulario V2oouewDocument16 pagesSuplemento Standardized Vocabulario V2oouewJadder InnacioNo ratings yet
- Automatic Control of Mechanical VentilationDocument8 pagesAutomatic Control of Mechanical VentilationRedouan Ait MouhaNo ratings yet
- Standardized vocabulary for mechanical ventilationDocument31 pagesStandardized vocabulary for mechanical ventilationMaaaanuelNo ratings yet
- History and Modes of Mechanical VentilatorsDocument7 pagesHistory and Modes of Mechanical VentilatorsYasmin AbdelmajiedNo ratings yet
- Lec#10Document30 pagesLec#10hani bilalNo ratings yet
- Care of Patient ON VentilatorDocument104 pagesCare of Patient ON VentilatorRita LakhaniNo ratings yet
- Basics of Mechanical VentilationDocument5 pagesBasics of Mechanical Ventilationruhaina malikNo ratings yet
- Care of Patients With Mechanical VentilatorDocument4 pagesCare of Patients With Mechanical VentilatorIman Bee Sanayon0% (1)
- Glossary of TermsMechVentDocument2 pagesGlossary of TermsMechVentFer CaudilloNo ratings yet
- Mechanical Ventilation Rle ReportDocument21 pagesMechanical Ventilation Rle ReportROMULO NU�EZ JR.No ratings yet
- Chapter 2: Mechanical Ventilator: HistoryDocument7 pagesChapter 2: Mechanical Ventilator: HistoryYasmin AbdelmajiedNo ratings yet
- Mechanical VentilationDocument16 pagesMechanical VentilationBhawna JoshiNo ratings yet
- DEMONSTRATION ON MECHANICAL VENTILATIONDocument8 pagesDEMONSTRATION ON MECHANICAL VENTILATIONHimaniNo ratings yet
- Ventilators, Intensive CareDocument48 pagesVentilators, Intensive CarealetripoleNo ratings yet
- Mechanical Ventilation GuideDocument6 pagesMechanical Ventilation Guideedison aorianoNo ratings yet
- Page 102-105 Positive Pressure VentilationDocument3 pagesPage 102-105 Positive Pressure VentilationGrandisDekaNo ratings yet
- Mwlcems System Continuing Education Packet Mechanical VentilationDocument8 pagesMwlcems System Continuing Education Packet Mechanical VentilationSoumahoro Ibrahim JuniorNo ratings yet
- Ventilator Modes Study GuideDocument34 pagesVentilator Modes Study GuideRyn ShadowNo ratings yet
- Bedside Teaching On Mechanical Ventilation: Submitted ToDocument8 pagesBedside Teaching On Mechanical Ventilation: Submitted ToManisha Shakya50% (2)
- Ventilator[1]NewDocument5 pagesVentilator[1]NewthalapraveensurendarNo ratings yet
- Care of Client in Mechanical VentilatorDocument11 pagesCare of Client in Mechanical VentilatorVignesh Viggy100% (4)
- Mechanical Ventilation ModesDocument9 pagesMechanical Ventilation ModesRicko ZhoumiLeeNo ratings yet
- Mechanical Ventilation Settings for COVID-19Document3 pagesMechanical Ventilation Settings for COVID-19Carlos ZepedaNo ratings yet
- Ventilator LectureDocument57 pagesVentilator LecturemonishaNo ratings yet
- Mechanical+Ventilation-Basics+for+Beginners (Unlocked by ComDocument49 pagesMechanical+Ventilation-Basics+for+Beginners (Unlocked by Comdokidok100% (14)
- Mechanical Ventilatory Support E.HDocument78 pagesMechanical Ventilatory Support E.HLet BNo ratings yet
- Med 9780199600830 Chapter 97Document7 pagesMed 9780199600830 Chapter 97Kiki Sri Rejeki AgisinaNo ratings yet
- Mechanical Ventilator CareDocument9 pagesMechanical Ventilator CareAnusha Verghese100% (2)
- 3.mechanical VentilationDocument33 pages3.mechanical Ventilationisapatrick8126No ratings yet
- Basics of Mechanical Ventilation For Residents: DR Ghaleb Almekhlafi MD, SFCCM PSMMCDocument43 pagesBasics of Mechanical Ventilation For Residents: DR Ghaleb Almekhlafi MD, SFCCM PSMMCGHALEB A. Almekhlafi100% (1)
- Mechanical Ventilator - Docx 02Document12 pagesMechanical Ventilator - Docx 02jonathan stevenNo ratings yet
- Mechanical Ventilation Modes and TypesDocument40 pagesMechanical Ventilation Modes and TypesAmol TemkarNo ratings yet
- Modes of VentilatorDocument17 pagesModes of VentilatorFahrizal MuhammadNo ratings yet
- Mechanical VentilationDocument5 pagesMechanical VentilationCherry Kris Caperig SuarezNo ratings yet
- Basic Mechanical Ventilation PDFDocument8 pagesBasic Mechanical Ventilation PDFPabloIgLopezNo ratings yet
- Overview of Mechanical Ventilation Settings, Modes, TroubleshootingDocument24 pagesOverview of Mechanical Ventilation Settings, Modes, TroubleshootingRochim CoolNo ratings yet
- Mechanical VentilationDocument9 pagesMechanical VentilationFriends ForeverNo ratings yet
- Care of Ventilator PatientDocument39 pagesCare of Ventilator Patientsandhya100% (1)
- Samsung Notes PDFDocument4 pagesSamsung Notes PDFPedro Antonio Ortega BorchardtNo ratings yet
- How Ventilators Deliver BreathsDocument51 pagesHow Ventilators Deliver BreathsArnaldo SantizoNo ratings yet
- Mechanical Ventilator GuideDocument23 pagesMechanical Ventilator GuideJennille IlagaNo ratings yet
- Ventilator, Weaning, SuctioningDocument81 pagesVentilator, Weaning, SuctioningwaqarNo ratings yet
- Mechanical Ventilation GuideDocument52 pagesMechanical Ventilation GuideSalma Omrr100% (1)
- Different Modes of Mechanical Ventilation May 2023Document64 pagesDifferent Modes of Mechanical Ventilation May 2023Lebison ShishiveniNo ratings yet
- Mechanical Ventilation Overview: Indications, Mechanics, and ModesDocument31 pagesMechanical Ventilation Overview: Indications, Mechanics, and ModesechtimNo ratings yet
- Ivent201 - Manual de Usuario (220-290)Document71 pagesIvent201 - Manual de Usuario (220-290)Wilber AleluyaNo ratings yet
- Ventilator BasicsDocument38 pagesVentilator Basicsgina contrerasNo ratings yet
- 11 VentDocument69 pages11 VentOMER GOSHNo ratings yet
- Savina DS ModeDocument39 pagesSavina DS ModeNeoNo ratings yet
- 1Document70 pages1hoan leNo ratings yet
- X300 Network Export HostDocument18 pagesX300 Network Export Hosthoan leNo ratings yet
- Owner Furnish Document Equipment DDRDocument140 pagesOwner Furnish Document Equipment DDRhoan leNo ratings yet
- Siemens Asia Pacific Regional Service TrainingDocument5 pagesSiemens Asia Pacific Regional Service Traininghoan leNo ratings yet
- Chapter3 IntroductiontoVentilatorsDocument10 pagesChapter3 IntroductiontoVentilatorsALex LanceNo ratings yet
- Savina Technical Service Bulletin # 2Document1 pageSavina Technical Service Bulletin # 2gameel alabsiNo ratings yet
- X300 2.0 Transducer SpecificationsDocument2 pagesX300 2.0 Transducer Specificationshoan leNo ratings yet
- Chapter 2 Pulmonary Physiology PDFDocument11 pagesChapter 2 Pulmonary Physiology PDFhoan leNo ratings yet
- Chapter 6 Terminology GlossaryDocument8 pagesChapter 6 Terminology Glossaryhoan leNo ratings yet
- Chapter 4 Ventilator Parameters PDFDocument12 pagesChapter 4 Ventilator Parameters PDFhoan leNo ratings yet
- Chapter 5 The Patient Circuit PDFDocument8 pagesChapter 5 The Patient Circuit PDFhoan leNo ratings yet
- Cardiopulmonary AnatomyDocument14 pagesCardiopulmonary Anatomyhoan leNo ratings yet
- Chapter 2 Pulmonary Physiology PDFDocument11 pagesChapter 2 Pulmonary Physiology PDFhoan leNo ratings yet
- Chapter3 IntroductiontoVentilatorsDocument10 pagesChapter3 IntroductiontoVentilatorsALex LanceNo ratings yet
- Chapter 5 The Patient Circuit PDFDocument8 pagesChapter 5 The Patient Circuit PDFhoan leNo ratings yet
- Cardiopulmonary AnatomyDocument14 pagesCardiopulmonary Anatomyhoan leNo ratings yet
- Owner Furnish Document Equipment DDRDocument140 pagesOwner Furnish Document Equipment DDRhoan leNo ratings yet
- Cardiopulmonary AnatomyDocument14 pagesCardiopulmonary Anatomyhoan leNo ratings yet
- 13 PPTGGDocument78 pages13 PPTGGأحمدآلزهوNo ratings yet
- Elbow Joint Rehabilitation Device for Stroke PatientsDocument4 pagesElbow Joint Rehabilitation Device for Stroke PatientslaurentiaNo ratings yet
- Cardiopulmonary AnatomyDocument14 pagesCardiopulmonary Anatomyhoan leNo ratings yet
- Design Proposal For A Portable Elbow Exoskeleton: Soumya K Manna and Venketesh N. DubeyDocument5 pagesDesign Proposal For A Portable Elbow Exoskeleton: Soumya K Manna and Venketesh N. Dubeyhoan leNo ratings yet
- Linear Accelerators Subsystems Guide Medical PhysicsDocument54 pagesLinear Accelerators Subsystems Guide Medical Physicshoan leNo ratings yet
- 2055 2386 5 5Document5 pages2055 2386 5 5hoan leNo ratings yet
- Design Proposal For A Portable Elbow Exoskeleton: Soumya K Manna and Venketesh N. DubeyDocument5 pagesDesign Proposal For A Portable Elbow Exoskeleton: Soumya K Manna and Venketesh N. Dubeyhoan leNo ratings yet
- 1Document70 pages1hoan leNo ratings yet
- GCI Linac Description and Operating NotesDocument28 pagesGCI Linac Description and Operating Noteshoan leNo ratings yet
- Bronchial Asthma Case StudyDocument3 pagesBronchial Asthma Case StudyCharisma PastorNo ratings yet
- Mechanical VentilationDocument52 pagesMechanical VentilationShaliniNo ratings yet
- Manage Acute AsthmaDocument3 pagesManage Acute AsthmaNicu EnachiNo ratings yet
- Assignment On Chest PhysiotherapyDocument15 pagesAssignment On Chest PhysiotherapyAxsa AlexNo ratings yet
- Presentation HamedDocument29 pagesPresentation HamedHamed GharibiNo ratings yet
- Kuala, Volume. 17, No. 1, Halaman 54-59.: Daftar PustakaDocument4 pagesKuala, Volume. 17, No. 1, Halaman 54-59.: Daftar PustakaAngga FirmansyahNo ratings yet
- NCP Draft PediaDocument9 pagesNCP Draft PediaEmman BarroquilloNo ratings yet
- Chronic Bronchitis Vs EmphysemaDocument2 pagesChronic Bronchitis Vs EmphysemaHumpy DumpyNo ratings yet
- Effect of Diaphragmatic Breathing Exercise On Peak Expiratory Flow (PEF) in Individual With AsthmaDocument10 pagesEffect of Diaphragmatic Breathing Exercise On Peak Expiratory Flow (PEF) in Individual With AsthmaSri WahyuniNo ratings yet
- Self Declaration form for international arrivalsDocument2 pagesSelf Declaration form for international arrivalsKoteswar MandavaNo ratings yet
- Activity 1.1 Journey of A Breath of AirDocument4 pagesActivity 1.1 Journey of A Breath of AirJorjette Kate BatuNo ratings yet
- Epi Pen AlgorithmDocument1 pageEpi Pen Algorithmfreebass08No ratings yet
- Respiratory System: Agatha Babyet A. Alabata, Bsn-Iii StemDocument31 pagesRespiratory System: Agatha Babyet A. Alabata, Bsn-Iii StemJay VillasotoNo ratings yet
- PhysioEx Exercise 7 Activity 1Document3 pagesPhysioEx Exercise 7 Activity 1CLAUDIA ELISABET BECERRA GONZALESNo ratings yet
- NCM-112-RESP (Sanaani, Nur-Fatima, M.) (Drug Study)Document2 pagesNCM-112-RESP (Sanaani, Nur-Fatima, M.) (Drug Study)Nur SetsuNo ratings yet
- Artificial Respirator - CPR Functioning BY, SANDHYA S.-1703099 SATHVIKA A.-1703104Document15 pagesArtificial Respirator - CPR Functioning BY, SANDHYA S.-1703099 SATHVIKA A.-170310417O3099 Sandhya S.No ratings yet
- NCP Hyperthermia IBPDocument4 pagesNCP Hyperthermia IBPJohn Patrick CuencoNo ratings yet
- Ards Concept MapDocument1 pageArds Concept Mapchristine louise bernardoNo ratings yet
- Carestation 600 SeriesDocument3 pagesCarestation 600 SeriesABHINANDAN SHARMANo ratings yet
- Sacral OMM diagnosis and treatment techniquesDocument4 pagesSacral OMM diagnosis and treatment techniquesSameer AkhtarNo ratings yet
- Asthma Pathophysiology: Ixsy Ramirez, MD, MPH Pediatric Pulmonology University of Michigan, C.S. Mott Children's HospitalDocument21 pagesAsthma Pathophysiology: Ixsy Ramirez, MD, MPH Pediatric Pulmonology University of Michigan, C.S. Mott Children's HospitalAru VermaNo ratings yet
- Medical Report Zoe CornelisDocument2 pagesMedical Report Zoe CornelisMuzni RahmanNo ratings yet
- Metered Dose Inhalers FlyerDocument2 pagesMetered Dose Inhalers FlyernishadiNo ratings yet
- Novi Lestari 1911304150 B3Document3 pagesNovi Lestari 1911304150 B3FarahNo ratings yet
- Anaphylaxis: Signs of Mild To Moderate Allergic ReactionDocument1 pageAnaphylaxis: Signs of Mild To Moderate Allergic ReactionOdkoo OdgerelNo ratings yet
- Global Initiative For Asthma (GINA) Teaching Slide Set 2016 UpdateDocument171 pagesGlobal Initiative For Asthma (GINA) Teaching Slide Set 2016 UpdateSergio Bachir AssaneNo ratings yet
- Standard Operation Procedure in Philippine Heart CenterDocument79 pagesStandard Operation Procedure in Philippine Heart CenterAyeesha AnnaNo ratings yet
- Respiration 6 PDFDocument27 pagesRespiration 6 PDFSardar jiNo ratings yet
- ECRI Test ResultsDocument3 pagesECRI Test ResultsAdam HarringtonNo ratings yet
- Inhaler Technique Metered Dose Inhalers With Volumatic SpacerDocument4 pagesInhaler Technique Metered Dose Inhalers With Volumatic Spacerdiana iurașcuNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (13)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (41)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (327)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (5)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisFrom EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (3)
- The Tennis Partner: A Doctor's Story of Friendship and LossFrom EverandThe Tennis Partner: A Doctor's Story of Friendship and LossRating: 4.5 out of 5 stars4.5/5 (4)































![Ventilator[1]New](https://imgv2-1-f.scribdassets.com/img/document/724530506/149x198/63fb83c045/1713502898?v=1)