Professional Documents
Culture Documents
Serologic Tests Part 1
Uploaded by
Joshua Trinidad0 ratings0% found this document useful (0 votes)
105 views4 pagesOriginal Title
SEROLOGIC TESTS PART 1
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
105 views4 pagesSerologic Tests Part 1
Uploaded by
Joshua TrinidadCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 4
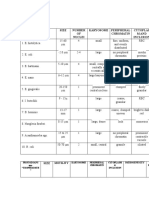
SEROLOGIC TEST 3.
Minimum Bactericidal Concentration (MBC) –
the lowest concentration of the antimicrobial
SEROLOGICAL TEST AND IMMUNODIAGNOSIS agent needed to kill the bacterial growth.
BACTERIAL SEROTYPING:
Lowest concentration to kill 99.9%; subcultur
o LANCEFIELD CLASSIFICATION
tubes near MIC to find 1st plate with no growth
Classification according to
carbohydrates present in the cell wall 4. Breakpoint (cutoff) – refers to the
of Streptococcus concentration of an antimicrobial agent that
o KAUFFMAN-WHITE SCHEME coincides with a susceptible or intermediate
Classification of serotypes of Salmonella MIC breakpoint for a particular drug.
based on surface antigen 5. Trailing Growth – Involves heavy bacterial
o E. coli 0157:H7 growth at lower concentrations followed by
one or more wells that show greatly reduced
DIAGNOSTIC TEST
o Schultz- Charlton growth in the form of a small button or a light
Diagnostic test for Streptococcus haze.
pyogenes 6. Skipped wells – Involve growth at higher
o Widal test concentrations and no growth at one or more
Detects antibody agains Salmonella of the lower concentrations; it may indicate
Antigen used: contamination, improper incubation, improper
O antigen – somatic antigen, heat
concentration of the antimicrobials and
stable, lipopolysaccharide
presence of unsual resistant isolate.
H antigen- Flagellar antigen, heat
labile, protein A. BROTH DILUTION METHOD
K/Vi antigen – capsular antigen, heat B. AGAR DILUTION METHOD
labile, polysaccharide C. DISK DIFFUSION METHOD (Kirby-Bauer Test)
o Weil-felix D. E TEST
Detects antibody against Rickettsia E. MINIMUM BACTERICIDAL CONCENTRATION TEST
Antigen used: F. TIME KILL ASSAY
OX-2 and OX-19: derived from G. SYNERGY TEST
Protesus vulgaris H. SERUM BACTERICIDAL TEST
OX-K : Derives from Protesus A. BROTH DILUTION METHOD
mirabilis
It involves challenging the organism of interest
SUSCEPTIBILITY TEST with antimicrobial agents in a broth
o Mantoux, Mendel, Tuberculin, Vollmer’s environment (Mueller-Hinton broth).
vonPirket –tuberculosis A specific amount of antibiotic is prepared in a
o Schick’s test – diphtheria decreasing concentration in broth by serial
o Dick’s test – scarlet fever dilution technique, and a standard amount of
o Mallein test – Glander’s disease the test organism is inoculated.
o Ascoli test – anthrax
Absence of turbidity of broth signifies inhibition
o Francis test – S. pneumoniae infection
of bacterial growth by the antibiotics being
Principle of serologic test tested.
o Latex agglutination Principle: to determine the lowest concentration of
o Precipitation test the antimicrobial drug (MIC) required to inhibit
o Labelled immunoassays ( EIA, FIA, RIA) bacterial growth.
a.Broth Macrodilution
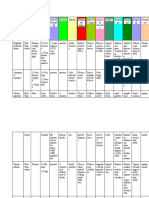
ANTIBIOTIC SUSCEPTIBILITY TESTING Susceptibility medium: MH broth (nonfastidious
TERMINOLOGIES: bacteria)
1. Minimum Inhibitory Concentration (MIC) – the Standard Inoculum size: 5 x 105 CFU/mL
lowest concentration of the antimicrobial agent Incubation time: 16-24 hrs (overnight) at 35⁰C
which inhibits the bacterial growth. 1 st dilution
Advantage: to test antimicrobials not included
tube with out visible growth
in the routine test or for fastidious bacteria;
2. Minimum Lethal Concentration (MLC) – the
used when MBC endpoints need to be
lowest concentration of the antimicrobial agent
subsequently determined.
which kills the bacterial growth when
subcultured to a fresh medium.
Disadvantage: impractical to use if there are ■ Mueller – hinton Agar
several antimicrobial agents or isolates to be Depth 4mm
tested. pH 7.2-7.4
b. Broth Microdilution Physiologic concentration of Mg and Ca
Susceptibility medium: MH broth (nonfastidious 35 0C ambient air
bacteria) 108 organism ( mc Farland 0.5)
Standard inoculum size: : 5 x 105 CFU/0.1 mL Weekly and with each new lot of agar or disc
well ( E. coli, S. aureus, P aeruginosa)
Incubation time: 16-24 hours (overnight) at
35⁰C TURBIDITY STANDARD:
Advantage: to test different antimicrobials (10- The use of a standard inoculum size is as
15) at the same time against a single isolate. important as culture purity and is accomplished
Disadvantage: inability to produce a penicillin by comparison of the turbidity of the organism
MIC that is consistently within the resistant suspension with a turbidity standard.
rangefor staphylococci that are low-level ß- 0.5% Mc Farland Turbidity Standard (Barium
lactamase producers. Sulfate Suspension)
o 99.5 mL of 1% H2SO4 + 0.5 mL 1.175% of
B. AGAR DILUTION METHOD Barium Chloride
The antimicrobial solutions brought together on o is equivalent to 1.5 x 108 colony
a molten and cooled culture medium forming units (CFU)/mL
A series of plates containing varying o it should be tightly sealed and stored in
concentration of each antimicrobials and the dark at room temperature.
control plates are prepared. Pure cultures are grown or are directly
One or more bacterial isolates (up to 32 prepared from agar plates to match the
different isolates) are tested per plate; MIC can turbidity of the 0.5 McFarland standard.
also be determined.
Procedure: A standard inoculum of bacteria is Preparation of Pure Culture for Susceptibility Testing:
spot-inoculated onto 100- mm plate. 1. Pure inocula (cultures) are obtained by selecting
Susceptibility medium: MHA (aerobes) 4-5 colonies of the same morphology, then
MHA + 5% SB (fastidious inoculate into broth medium and incubate for
bacteria) 3-5 hours to achieve a turbid suspension.
Standard inoculum size: 1 x 104 CFU/mL 2. Alternatively, 4-5 colonies 16-24 hours of age
may be selected from an agar plate and
C. DISK DIFFUSION METHOD (Kirby-Bauer Test) suspended into broth medium or 0.85% NSS to
Is limited to aerobic and facultatively anaerobic achieve a turbid suspension.
bacteria. ■ Direct inoculums suspension is preferred for
It is a qualitative method which provides the fastidious bacteria.
greatest flexibility and cost – effectiveness – it 3. Matching turbidity using the unaided eye is
allows the laboratory to test ant 12 facilitated by holding the bacterial suspension
antimicrobial agents on a 150-mm MHA plate. and McFarland tubes side by side and viewing
Principle: the larger the zone of inhibition, the them against a black-lined background –
lower the MIC – the zone of inhibition is inoculums suspension should be used within 15
inversely related to MIC. minutes.
Susceptibility standard medium: Mueller Hinton 4. If the bacterial suspension initially does not
Agar (MHA) match the standard’s turbidity, the suspension
Standard inoculum size: 1.5 x 108 CFU/mL may be diluted, or supplemented with more
Procedure: filter paper disks impregnated with organisms, as needed.
various antimicrobial agents of specific During streaking and placement of discs:
concentrations are carefully placed on an agar 1. Turn the plate 60 degrees between each
plate previously inoculated with the bacteria streaking.
being tested 2. The surface of the medium should be allowed
to dry 3-5 minutes but not longer than 15
minutes.
3. Within 15 minutes of inoculation, the MIC approaches or exceeds the level of
antimicrobial agents are applied on the MHA. antimicrobial agent that can be achieved
4. The discs must be positioned no closer than 24 and for which clinical response is likely to
mm from disc center to disc center and no be less than with a susceptible strain
closer than 10-15 mm from the edge of the – RESISTANT – the microorganism is
plate. The disks are pressed firmly to ensure inhibited by the usually achievable
contact with the agar. concentrations of the antimicrobial agent
5. Within 15 minutes of disk placement, plates are based on the dosages normally used with
inverted and incubated at 35⁰C for 16-18 that drug.
hours. Plates are inverted to avoid – NONSUSCEPTIBLE – when there are no
contamination of moisture on the agar surface intermediate or resistance interpretative
that can interfere with interpretation of test criteria, only a susceptible criteria, and the
results. MIC or disk diffusion zone size for
classifying the organism as susceptible is
Reading of Plates and Interpretation of Results: not achieved; it commonly occurs with
1. The lawn of growth must be confluent or almost newer antimicrobials. It does not mean
confluent. that the organism is resistant to the
2. Provided growth is satisfactory, the diameter or antimicrobial agent.
each inhibition zone is measured using a caliper 11. Quality control plates should be read prior to
or ruler. reading results of patient isolates o determine
3. Plates are examined 2-3 inches above a black, whether the test was performed correctly
nonreflecting surface and the zones are
measured from the back side of the plate. Causes of False Resistance
4. Transmitted light (plate held up to light source) 1. Use of unduly heavy inocula of cultures or
rather than reflected light will improve the undiluted specimen materials.
accuracy of tests with penicillinase- resistance- 2. Late examination of test plates after zones have
penicillins. become overgrown (18-24 hours) incubation.
5. For media containing blood, the plate is 3. Use of disc with inadequate drug concentration
examined with the lid removed. due to prolonged storage, failure to refrigerate
6. The appearance of individual colonies is as from disc container opened frequently.
unacceptable. 4. Use of wrong organism.
7. The zone size of a motile, swarming organism
such as Proteus should be ignored (thin film of NOTES TO REMEMBER:
growth) MHA is composed of beef infusions, nucleic
8. Discontinuous, poor growth or tiny colonies acids, vitamins, casein hydrolysate, (casein
near the end of the zone size are also ignored. neutralizes fatty acid) and agar.
9. Colonies within a clear zone should not be MHA containing 5% sheep’s blood is used for
ignored – these colonies may occur as a result testing streptococci and other fastidious
of contamination or testing a mixed culture. The organisms.
original colony should be retested, The MIC test represents a semiquantitative
10. Zone measurement is compared with the method and the concentration (microgram/mL)
interpretive tables of CLSI and results are of a drug required to inhibit the growth of
interpreted as susceptible, intermediate, bacterial isolate is reported together with a
resistant or nonsusceptible. susceptible, intermediate or resistant
– SUSCEPTIBLE – the patient’s infecting interpretation.
organism should respond to therapy with The diameter of the zone of inhibition around
that antimicrobial agent using the disk is measured in mm using a caliper; a wide
recommended dosage for the site of zone surrounding a disk signifies more
infection, indicated by the presence of susceptibility of the organism to the antibiotic.
zone of inhibition around the antibiotic Zone width is related to antibiotic
disk. concentration, diffusion rate through agar and
– INTERMEDIATE – the microorganism falls solubility.
into a range of susceptibility in which the
For long term-storage, disks are stored at 20⁰C
or below in an non-frost-free freezer while D. E TEST
working supply disks at 2-8⁰C for atleast 1 week. (+) result: ellipse of growth inhibition
Routine susceptibility testing on ß-hemolytic The MIC is read at the point on the scale where
streptococci is generally not necessary. the ellipse intersects the strip.
The strip can be placed on special enriched
Factors Affecting Zone of Inhibitions: media or incubation atmosphere – used as an
1. The amount of inoculum or test organism. alternative susceptibility test for fastidious
– only pure cultures can be tested. bacteria (S. pneumoniae and H. influenzae) and
– If the inoculum is too light it would anaerobic bacteria.
result to false susceptibility; if the
inoculum is too heavy it would result to E. MINIMUM BACTERICIDAL CONCENTRATION TEST
false resistance. An in vitro determination of the amount of
– Use of old cultures may result to false antimicrobial agent required to kill as well as
susceptibility. inhibit the bacteria.
2. Thickness of the susceptibility agar plate (4 mm) It is performed together with a broth
– If the agar is too thick, zone size would macrodilution or microdilution MIC test – a mL
be smaller, if agar is too thin, zone aliquot of each clear MIC tube or well is
sizes would be larger subcultured to an agar medium.
3. The growth rate of the test organism. Standard inoculums: 5 x 105 CFU/mL
– Air at 35⁰C for most bacteria (16-18 Final dilution: 1:1000 (0.01 mL from the original
hours); N.gonorrhea for 20-24 hours. tube in 10 mL)
– Lower temperatures may lead to larger Volume spread per plate: 0.1 mL
zones of inhibition. Dilution Factor: 1:10,000 (104)
– Temperatures higher than 35⁰C may
lead to false detection of MRSA. PROCEDURE;
– Prolonged incubation may result in false • An actual colony count must be performed on
resistance interpretation. the test inoculums at the time the MIC test is
– Some MRSA may go undetected if less inoculated.
than 24 hours of incubation. • The number of colonies that grow on subculture
– 5-7% CO2 for N. meningitides and are compared with the actual number of organisms
S.pneumonia. inoculated into the MIC test tubes or wells to
4. The pH of the medium (7.2-7.4) determine the extent of bactericidal activity at each
Incubation in CO2 results in decreased pH – antimicrobial concentration.
leads to decreased activity of aminoglycosides, INTERPRETATION OF RESULTS:
erythromycins, and clindamycin but increased • If the numbers of colonies on a subculture plate
activity of tetracyclines. total less than 0.1% of the initial inoculums
5. The number of disk per plate. (indicating 99.9% or more killing), a bactericidal
– 12 disks/150 mm plate effect has been achieved.
– Placement of more than 12 disks may • A 99.9% killing (or 0.1% survival) would be
result in overlapping zones (erroneous accomplished if 5 or fewer colonies grow on
results) subculture of each clear well or tube after reading
6. The concentration of divalent cations (Calcium of the MIC test.
and Magnesium) • Paradoxic (eagle) effect – is decreased
– It can affect testing of aminoglycosides bactericidal activity at a higher drug concentration.
and tetracyclines against P. • Tolerance – it is defined as an MBC:MIC ration
aeruginosa. of > 32.
– Elevated concentrations od the divalent
cations may result to diminish activity
of the aminoglycosides against
P.aeruginosa and decreased activity of
tetracyclines against all bacteria, and
– vise versa.
You might also like
- Medical Laws and Regulations SummaryDocument16 pagesMedical Laws and Regulations SummaryNeririNo ratings yet
- Using Colonial Morphology to Presumptively ID MicroorganismsDocument6 pagesUsing Colonial Morphology to Presumptively ID MicroorganismsJean BelciñaNo ratings yet
- Microscopic Examination of UrineDocument4 pagesMicroscopic Examination of UrineGlaiza Erika Baes GudaNo ratings yet
- Studying Fungi Methods Lab DiagnosisDocument74 pagesStudying Fungi Methods Lab DiagnosisKaycee Gretz LorescaNo ratings yet
- Mycology and VirologyDocument8 pagesMycology and VirologyMaybelle Acap PatnubayNo ratings yet
- Bacteriostatic Agents: Drugs Which Bind To The 50s Ribosomal UnitDocument3 pagesBacteriostatic Agents: Drugs Which Bind To The 50s Ribosomal UnitJoshua TrinidadNo ratings yet
- Serological TestsDocument2 pagesSerological TestsKimberly EspaldonNo ratings yet
- Immunology and Serology ReviewDocument30 pagesImmunology and Serology ReviewEuliz G.100% (1)
- Staphylococcus Spp. Gram Positive. ClusteredDocument15 pagesStaphylococcus Spp. Gram Positive. ClusteredIvy NNo ratings yet
- Analysis of Physical Properties of UrineDocument2 pagesAnalysis of Physical Properties of UrineameerabestNo ratings yet
- Microbiology ChartsDocument17 pagesMicrobiology Chartsclower112No ratings yet
- Agents of Mycoses Identification and CharacteristicsDocument44 pagesAgents of Mycoses Identification and CharacteristicsRia AlcantaraNo ratings yet
- ISBB Aaaaa PDFDocument55 pagesISBB Aaaaa PDFSelena de LimaNo ratings yet
- Molecular Biology and Diagnostic Intro To CytogeneticsDocument6 pagesMolecular Biology and Diagnostic Intro To Cytogeneticselijah montefalcoNo ratings yet
- COMPLETE BLOOD COUNT Lecture GuideDocument9 pagesCOMPLETE BLOOD COUNT Lecture GuideKaycee Gretz LorescaNo ratings yet
- SubcutaneousDocument2 pagesSubcutaneousMary ChristelleNo ratings yet
- Hematology Ii Lectures Introduction To HemostasisDocument28 pagesHematology Ii Lectures Introduction To HemostasisJoshua Trinidad100% (1)
- Chapter Blood: RBC Platelet HemostasisDocument89 pagesChapter Blood: RBC Platelet Hemostasisapi-19916399100% (1)
- MICROBIOLOGY MEDIADocument3 pagesMICROBIOLOGY MEDIAAisle Malibiran PalerNo ratings yet
- Bacte Day 2Document24 pagesBacte Day 2Jadey InfanteNo ratings yet
- Diagnostic Microbiology - : University of Santo Tomas - Medical TechnologyDocument6 pagesDiagnostic Microbiology - : University of Santo Tomas - Medical TechnologyWynlor AbarcaNo ratings yet
- 1 Antigens and AntibodiesDocument31 pages1 Antigens and AntibodiesJohn Louis RanetNo ratings yet
- Medical Technology Laws and Ethics EssentialsDocument15 pagesMedical Technology Laws and Ethics EssentialsMae MacalandaNo ratings yet
- Blood Bank TypingDocument34 pagesBlood Bank TypingSkylarNo ratings yet
- Immunology Serology ReviewDocument211 pagesImmunology Serology ReviewRachel Marie M. Gania100% (1)
- Incorrectly: CorrectlyDocument25 pagesIncorrectly: CorrectlypikachuNo ratings yet
- Abnormal Urine Color and ClarityDocument4 pagesAbnormal Urine Color and ClarityJulie Anne Soro ValdezNo ratings yet
- Bacteriology Genera Visualized by Bright-Field MicroscopeDocument6 pagesBacteriology Genera Visualized by Bright-Field MicroscopeRachelle AbonalesNo ratings yet
- Hematology II Notes - MagtalasDocument12 pagesHematology II Notes - MagtalasAbhugz VosotrosNo ratings yet
- ISBB Immunology ReviewDocument9 pagesISBB Immunology ReviewNathan DrakeNo ratings yet
- Blood Banking Course BookDocument2 pagesBlood Banking Course BookShukr Wesman BlbasNo ratings yet
- Aubf Lab CSFDocument6 pagesAubf Lab CSFAndrei Tumarong AngoluanNo ratings yet
- HEMOSTASIS Coagulation PathwayDocument3 pagesHEMOSTASIS Coagulation PathwayGianna SablanNo ratings yet
- AUBF Finals Vaginal SecretionsDocument37 pagesAUBF Finals Vaginal SecretionsLyra Dennise LlidoNo ratings yet
- Top 20 Blood Banking ConceptsDocument16 pagesTop 20 Blood Banking ConceptsM CNo ratings yet
- DIAGNOSTIC MYCOLOGY: SPECIMEN COLLECTION AND IDENTIFICATIONDocument154 pagesDIAGNOSTIC MYCOLOGY: SPECIMEN COLLECTION AND IDENTIFICATIONJade MonrealNo ratings yet
- HeamatologyDocument45 pagesHeamatologypikachuNo ratings yet
- Mtap - Immunohema Transfusion MedicineDocument9 pagesMtap - Immunohema Transfusion MedicineMoira Pauline LibroraniaNo ratings yet
- Mega Micro para Table 1 (1) (PDF - Io)Document81 pagesMega Micro para Table 1 (1) (PDF - Io)CheryldaneBaculiNo ratings yet
- Klubsybear Additional Recalls: Hematology A.karyolysisDocument2 pagesKlubsybear Additional Recalls: Hematology A.karyolysisMartin ClydeNo ratings yet
- Anion Gap CalculationDocument13 pagesAnion Gap CalculationDams ZainalNo ratings yet
- M6 Histopath ImpregantionAndEmbeddingDocument4 pagesM6 Histopath ImpregantionAndEmbeddingninaNo ratings yet
- 3 Chemical Examination of UrineDocument82 pages3 Chemical Examination of UrineJake Real Dela RocaNo ratings yet
- Cabison - Mycology ReviewerDocument10 pagesCabison - Mycology ReviewerPatricia Cabison100% (1)
- MedtechDocument7 pagesMedtechLyudmyla GillegoNo ratings yet
- MedTech Licensure Exam ChecklistDocument3 pagesMedTech Licensure Exam ChecklistVianney Angeli LorenzanaNo ratings yet
- Test Bank Exam 3Document81 pagesTest Bank Exam 3Sajjad AhmadNo ratings yet
- Hematology2 - Laboratory TestsDocument3 pagesHematology2 - Laboratory Testskthmnts100% (1)
- AUBF Notes 1Document9 pagesAUBF Notes 1ChiNo ratings yet
- Histopath MTLDocument6 pagesHistopath MTLElla Sales100% (1)
- Clinical Chemistry KeyNotes For Board ExaminationDocument12 pagesClinical Chemistry KeyNotes For Board ExaminationPrincess Alen Aguilar100% (1)
- Clinical Microscopy Safety and Urine AnalysisDocument26 pagesClinical Microscopy Safety and Urine AnalysisDarla YsavelNo ratings yet
- MTAP - 1.1 - BacteriologyDocument14 pagesMTAP - 1.1 - BacteriologyKassandra CordetaNo ratings yet
- Assessment Exam in Cc2and3Document7 pagesAssessment Exam in Cc2and3mika de guzmanNo ratings yet
- Basic Mycology GuideDocument46 pagesBasic Mycology GuideMartin Clyde100% (1)
- Clinical Microscopy (Analysis of Urine and Other Body Fluids)Document14 pagesClinical Microscopy (Analysis of Urine and Other Body Fluids)Jeanly DoctorNo ratings yet
- Wintrobe Test PDFDocument9 pagesWintrobe Test PDFMaria Chacón CarbajalNo ratings yet
- Hematology recall questionsDocument4 pagesHematology recall questionsMai RodrigoNo ratings yet
- Cc1-Task 4Document8 pagesCc1-Task 4Joshua TrinidadNo ratings yet
- A CLIA Waived Test Requires That OperatorsDocument3 pagesA CLIA Waived Test Requires That OperatorsJoshua TrinidadNo ratings yet
- CC1 11Document2 pagesCC1 11Joshua TrinidadNo ratings yet
- A. Two Forms of Carbohydrates: 1. Draw The FollowingDocument7 pagesA. Two Forms of Carbohydrates: 1. Draw The FollowingJoshua TrinidadNo ratings yet
- Case Study: QuestionsDocument2 pagesCase Study: QuestionsJoshua TrinidadNo ratings yet
- Cc1-Task 3Document3 pagesCc1-Task 3Joshua Trinidad100% (1)
- Serologic Tests Part 3Document2 pagesSerologic Tests Part 3Joshua TrinidadNo ratings yet
- Automated antimicrobial susceptibility testingDocument2 pagesAutomated antimicrobial susceptibility testingJoshua TrinidadNo ratings yet
- CC1 8Document4 pagesCC1 8Joshua Trinidad0% (1)
- Cc1-Task 1Document2 pagesCc1-Task 1Joshua TrinidadNo ratings yet
- Serologic Tests Part 5Document3 pagesSerologic Tests Part 5Joshua TrinidadNo ratings yet
- Draw and define basic instrumentation of a spectrophotometerDocument6 pagesDraw and define basic instrumentation of a spectrophotometerJoshua TrinidadNo ratings yet
- Table 1: Protozoans Spp. "CYSTS" Size Number OF Nuclei Karyosome Peripheral Chromatin Cytoplas M and InclusionDocument3 pagesTable 1: Protozoans Spp. "CYSTS" Size Number OF Nuclei Karyosome Peripheral Chromatin Cytoplas M and InclusionJoshua TrinidadNo ratings yet
- Bacteriostatic Agents: Drugs Which Bind To The 50s Ribosomal UnitDocument3 pagesBacteriostatic Agents: Drugs Which Bind To The 50s Ribosomal UnitJoshua TrinidadNo ratings yet
- Sporozoa TableDocument2 pagesSporozoa TableJoshua TrinidadNo ratings yet
- Nematodes (Round Worms) Comparison TableDocument4 pagesNematodes (Round Worms) Comparison TableJoshua TrinidadNo ratings yet
- Reviewer - Life of Dr. Jose RizalDocument35 pagesReviewer - Life of Dr. Jose Rizaljava_biscocho122993% (105)
- Mastigophora TableDocument1 pageMastigophora TableJoshua TrinidadNo ratings yet
- Wuchereria Bancrofti Brugia Malayi Loa Loa Onchocerca Volvulus Mansonella Perstans Mansonella Ozzardi Dracunculus MedinensisDocument4 pagesWuchereria Bancrofti Brugia Malayi Loa Loa Onchocerca Volvulus Mansonella Perstans Mansonella Ozzardi Dracunculus MedinensisJoshua TrinidadNo ratings yet
- Coccidia TableDocument2 pagesCoccidia TableJoshua TrinidadNo ratings yet
- Parasitology Terminologies TableDocument4 pagesParasitology Terminologies TableJoshua TrinidadNo ratings yet
- Hematology Ii Lectures Introduction To HemostasisDocument28 pagesHematology Ii Lectures Introduction To HemostasisJoshua Trinidad100% (1)
- Week 1 and 2 - IntroductionDocument5 pagesWeek 1 and 2 - IntroductionJoshua TrinidadNo ratings yet
- Chemical Basis of LifeDocument2 pagesChemical Basis of LifeEllaine ReyesNo ratings yet
- Reviewer - Immunoserology - Part 2 PDFDocument33 pagesReviewer - Immunoserology - Part 2 PDFJoshua TrinidadNo ratings yet
- Reviewer - Immunoserology - Part 2 PDFDocument33 pagesReviewer - Immunoserology - Part 2 PDFJoshua TrinidadNo ratings yet
- Cestodes - TableDocument5 pagesCestodes - TableJoshua TrinidadNo ratings yet
- Reviewer - Immunoserology - Part 2 PDFDocument33 pagesReviewer - Immunoserology - Part 2 PDFJoshua TrinidadNo ratings yet
- Reviewer - Immunoserology - Part 2 PDFDocument33 pagesReviewer - Immunoserology - Part 2 PDFJoshua TrinidadNo ratings yet
- 286129Document23 pages286129Cristian WalkerNo ratings yet
- VW Crafter 2f Component Locations EngDocument118 pagesVW Crafter 2f Component Locations EngHugo Emilio Garcia Gonzalez100% (2)
- Seagate WD Hard Drive Price List From Billion HoDocument4 pagesSeagate WD Hard Drive Price List From Billion HoALi RAzaNo ratings yet
- Environmental, Health and Safety Guidelines For Textiles ManufacturingDocument20 pagesEnvironmental, Health and Safety Guidelines For Textiles ManufacturingHitesh ShahNo ratings yet
- International Standard Iso/Iec Software Cycle Processes: Standards SectionDocument16 pagesInternational Standard Iso/Iec Software Cycle Processes: Standards SectionDavid SalgadoNo ratings yet
- Outline of The Gospel of John: Book of Signs: Jesus Reveals His Glory To The World (Israel) (1:19-12:50)Document4 pagesOutline of The Gospel of John: Book of Signs: Jesus Reveals His Glory To The World (Israel) (1:19-12:50)Aamer JavedNo ratings yet
- Set 1Document24 pagesSet 1TutorTutorNo ratings yet
- Cultural Understanding Impacts Consumer BehaviorDocument10 pagesCultural Understanding Impacts Consumer BehaviorNguyễn Hữu Thảo NguyênNo ratings yet
- Hindustani Music HistoryDocument28 pagesHindustani Music HistoryChamod ArunaluNo ratings yet
- Case3: What's in A Car 1. What Kind of Research Study Should Shridhar Undertake? Define TheDocument2 pagesCase3: What's in A Car 1. What Kind of Research Study Should Shridhar Undertake? Define TheRoshan kumar Rauniyar0% (3)
- Asme A112.4.14-2004 PDFDocument14 pagesAsme A112.4.14-2004 PDFAmer AmeryNo ratings yet
- PR & PublicityDocument16 pagesPR & PublicityVipul Partap100% (2)
- Instruction Manual: Shimadzu Analytical BalanceDocument169 pagesInstruction Manual: Shimadzu Analytical BalanceChanthar SoeNo ratings yet
- 2 Corinthians: Workbook OnDocument18 pages2 Corinthians: Workbook OnJhon Ray OtañesNo ratings yet
- Inergen Order Data SheetDocument31 pagesInergen Order Data Sheetkarim3samirNo ratings yet
- Template PharmaconDocument4 pagesTemplate PharmaconDanang RaharjoNo ratings yet
- RAF Bomber Command March 1943Document4 pagesRAF Bomber Command March 1943catracho84No ratings yet
- Vergara, Valerie G. Drug Study (Ma'Am Dean)Document3 pagesVergara, Valerie G. Drug Study (Ma'Am Dean)Valerie VergaraNo ratings yet
- Daniel J. Wood - Realm of The Vampire - History and The Undead-Galde Press (2013)Document156 pagesDaniel J. Wood - Realm of The Vampire - History and The Undead-Galde Press (2013)Jerry KanneNo ratings yet
- S1.8 Template of REAL Table For Power and Supporting CompetenciesDocument3 pagesS1.8 Template of REAL Table For Power and Supporting CompetenciesJamir SalongaNo ratings yet
- Solar Pump Inverter PV100 PV200 User Manuel Rev1Document49 pagesSolar Pump Inverter PV100 PV200 User Manuel Rev1faitgpsNo ratings yet
- 7306 31980 1 PBDocument10 pages7306 31980 1 PBRaihan Aditiya JuniorNo ratings yet
- Excerpts From The Way of The Samurai (Shīdo) : Primary Source Document With Questions (DBQS)Document2 pagesExcerpts From The Way of The Samurai (Shīdo) : Primary Source Document With Questions (DBQS)Valeria MontalvaNo ratings yet
- KR 280 R3080 F technical specificationsDocument1 pageKR 280 R3080 F technical specificationsDorobantu CatalinNo ratings yet
- Installation, Operation and Maintenance Instructions For 9957W Automatic Balancing ValveDocument2 pagesInstallation, Operation and Maintenance Instructions For 9957W Automatic Balancing ValveManuel Molina CamposNo ratings yet
- Grade 7 Lesson: Module 4 - Acids and BasesDocument3 pagesGrade 7 Lesson: Module 4 - Acids and BasesJoedelyn Wagas100% (4)
- Power Grid FailureDocument18 pagesPower Grid Failurechandra 798No ratings yet
- LP Lab ManuelDocument23 pagesLP Lab ManuelRavi Kumar LankeNo ratings yet
- Logging Levels in Log4j - Tutorialspoint ExamplesDocument3 pagesLogging Levels in Log4j - Tutorialspoint ExamplesJai PannuNo ratings yet