Professional Documents
Culture Documents
In Practice-2012-Hayes-250-9
Uploaded by
Sara ConnorCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
In Practice-2012-Hayes-250-9
Uploaded by
Sara ConnorCopyright:
Available Formats
Downloaded from inpractice.bmj.com on February 23, 2014 - Published by group.bmj.
com
Companion animal practice
Investigation and management
of splenic disease in dogs
Graham Hayes and Jane Ladlow
Splenic disorders are a significant cause of morbidity and mortality in middle-
aged and older dogs, and a spectrum of presentations is possible, from chronic
non-specific clinical signs to a rapidly fatal haemoabdomen. Splenomegaly is
Graham Hayes graduated from commonly recognised during clinical examination or imaging in practice, but
the University of Cambridge in it can be difficult to decide whether the primary problem is within the spleen
2001 and worked at the RSPCA itself (eg, a focal mass, in which case a splenectomy is generally the treatment
Greater Manchester Animal of choice) or whether the splenomegaly represents systemic disease (eg, a
Hospital for seven years. He lymphoma or immune-mediated haemolytic anaemia, in which case a biopsy
currently works in private practice may be useful but a splenectomy may be contraindicated). Splenic surgery
in Cheshire. He holds the RCVS requires an appreciation of the vascular anatomy, and adequate monitoring
certificate in small animal surgery as well as supportive treatment may be critical to the outcome of surgery.
and is a diplomate of the European This article discusses the anatomy of the spleen and how to investigate
College of Veterinary Surgery. splenomegaly, as well as how to perform a (partial) splenectomy and the
possible complications involved.
Anatomy Short gastric vessels
in the gastrosplenic
ligament
The spleen is a mobile, parenchymal organ that is
normally located in the left cranial quadrant of the Stomach
abdomen and partially covered by the costal arch. It
is attached to the greater curvature of the stomach by
Jane Ladlow graduated from the the gastrosplenic ligament and loosely suspended by Left gastroepiploic vessels
University of Cambridge in 1995 the greater omentum. The actual position of its ven-
and has worked in general practice tral extremity varies depending on stomach size and
and at the Animal Health Trust. degree of engorgement. The spleen is supplied by the Splenic
She is currently a lecturer in soft splenic artery (from the celiac artery), which splits into artery
tissue surgery at Cambridge and about 25 branches before entering the hilus on the vis- Pancreas
is a diplomate of the European ceral surface (Fig 1). It is drained by the gastrosplenic Splenic
branches
College of Veterinary Surgeons. vein, which contributes to the hepatic portal vein. The entering
blood supply to the spleen is closely associated with the hilus
doi:10.1136/inp.e3107
Provenance: Commissioned the gastroepiploic vessels of the stomach and vessels Branches to the
and peer-reviewed supplying the left lobe of the pancreas. greater omentum and
splenocolic ligament
Box 1: Functional anatomy of the spleen Fig 1: Schematic diagram showing the vascular
anatomy of the canine spleen
The spleen is part of the reticuloendothelial system and has many important functions,
but is not essential for life. The following two functions are associated with the
anatomically distinct parenchymal areas of the organ: Pathophysiology
■■ ‘White pulp’ – lymphoid tissue involved in immunosurveillance and the production of
B and T lymphocytes. The white pulp of the spleen functions as a large lymph node; The multiple functions of the spleen (Box 1) help to
■■ ‘Red pulp’ – venous sinuses containing macrophages, megakaryocytes and white
explain some of the pathological conditions that affect
blood cells. The red pulp performs erythrocyte conditioning and maintenance,
this organ. The large amount of lymphoid tissue present
erythrocyte and platelet storage, and extramedullary haematopoiesis. The splenic
reservoir can contain up to 20 per cent of erythrocytes and 30 per cent of platelets means reactive hyperplasia or lymphoproliferative
in a dog, and these can be mobilised by sympathetic contraction of the smooth disease may cause diffuse splenic enlargement or focal
muscle in the capsule and internal trabeculae. nodular hyperplasia. Extramedullary haematopoiesis
In humans, a partial splenectomy is performed in preference to a complete may also be associated with diffuse splenomegaly in
splenectomy as the latter has occasionally been associated with fatal septicaemias. consumptive anaemias or bone marrow disease; a
This complication has not been reported in dogs or cats, so a complete splenectomy
splenectomy in such cases would be disadvantageous
is routinely performed in these animals.
and potentially detrimental to the patient.
250 In Practice May 2012 | Volume 34 | 250–259
Downloaded from inpractice.bmj.com on February 23, 2014 - Published by group.bmj.com
Companion animal practice
The large amounts of connective tissue and vascular
sinuses present in the spleen make it a frequent loca- Box 2: Differential diagnoses of splenomegaly
tion to find primary sarcomas as well as secondary neo-
Diffuse splenomegaly disease, obstruction of the caudal
plasms. In addition, the compliant vascular spaces make
■■ Infiltrative vena cava)
the organ susceptible to haematoma formation and vas- ●● Neoplastic (eg, leukaemia, ●● Drug-induced (especially
cular congestion, which may be drug-induced and sec- lymphoma, systemic mastocytosis, barbiturates)
ondary to portal hypertension, right-sided heart failure multiple myeloma, malignant
or torsion of the vascular pedicle (which may or may not histiocytosis) Focal splenomegaly
●● Non-neoplastic (eg, extramedullary ■■ Primary or secondary neoplasia
be associated with gastric dilation/volvulus [GDV]).
Diverse clinical signs associated with a space- haematopoiesis, hypereosinophilic ●● Haemangiosarcoma, haemangioma,
syndrome) other sarcomas*
occupying abdominal mass, blood dyscrasia, para-
■■ Infectious ■■ Non-neoplastic
neoplastic syndromes or hypovolaemic shock with a ●● Bacterial (eg, septicaemia, bacterial ●● Nodular lymphoid hyperplasia*
haemoabdomen may result from splenic disease. endocarditis) ●● Haematoma
●● Viral (eg, canine adenovirus type 1) ●● Abscess
●● Parasitic (eg, haemobartonellosis, ●● Hydatid cysts
Clinical signs ehrlichiosis, leishmaniosis, babesiosis) ●● Granuloma
■■ Hyperplastic ●● Fibrohistiocytic nodules*
●● Immune-mediated haemolytic
The clinical signs of splenic disease are highly variable
anaemia or immune-mediated *A continuous spectrum of disease is
and may be non-specific or have an insidious onset. thrombocytopenia recognised ranging from nodular lymphoid
Subtle signs, such as a reduced appetite, weight loss, ●● Primary or secondary hypersplenism hyperplasia through fibrohistiocytic
intermittent vomiting, lethargy, depression, abdomi- ■■ Congestive nodules to malignant fibrous histiocytoma.
nal distension, polydipsia and polyuria, may be noted ●● Splenic torsion (eg, primary or This represents the progression of
by the owner. Other findings on clinical examin secondary to gastric dilation/volvulus) histopathological features from benign
●● Portal hypertension (eg, right-sided inflammatory disease to high-grade
ation may include pyrexia, pale mucous membranes,
congested heart failure, hepatic malignancy (Spangler and Kass 1998).
abdominal distension, palpable splenomegaly and
pain on abdominal palpation. Generalised lymph
adenopathy may be present with lymphoproliferative
diseases. Splenic congestion may be associated with mediated disease and ehrlichiosis. Clotting profiles (or
right-sided heart failure or portal hypertension. Signs a buccal mucosa bleeding time) should be considered
of an acutely distended, painful abdomen, coupled when haemoabdomen, haemangiosarcoma or blood
with pale mucous membranes and tachycardia, may dyscrasia is present.
occur with the rupture of a splenic mass or a traumatic
splenic rupture. A splenic haemangiosarcoma may also Ultrasonography
be associated with signs of ventricular arrhythmias or The assessment of splenic size is subjective (Box 3) and
coagulopathy (petechiae or ecchymoses). radiography is generally insensitive for distinguishing
between generalised splenomegaly and a focal mass.
Ultrasonography is usually considered most useful
Investigation for imaging the spleen as it allows focal masses to be
defined and allows the parenchyma and capsule to be
Splenomegaly is the primary differential diagnosis for evaluated, even in the presence of abdominal fluid (Fig
a mid-abdominal mass but further imaging is usually 2). It is useful for guiding fine-needle aspirations and
indicated to confirm the problem (Box 2). evaluating other abdominal organs, and is especially
sensitive to changes in the splenic architecture (eg,
Biochemistry and haematology due to neoplastic infiltration or infarction). Vascular
Although biochemistry and haematology testing may not changes can be assessed using colour Doppler ultra-
indicate specific changes with splenic diseases, they are sonography. When a focal cavitary mass is detected,
recommended to rule out other differential diagnoses ultrasonographic assessment of the heart (particularly
and to obtain baseline values for haematocrit and total
protein. Hypercalcaemia may be suggestive of lympho-
proliferative disease and hyperglobulinaemia can also be
associated with lymphoproliferative disease and chronic
Box 3: Normal variations in the size
infections such as ehrlichiosis and leishmaniosis.
of a canine spleen
If anaemia or other cytopenias are apparent on hae- ■■ Young, athletic dogs generally have larger spleens
matology, examination of a blood smear is indicated to than older dogs
confirm and further characterise the changes. Anaemia ■■ German shepherd dogs have relatively larger
may be due to chronic disease (mild to moderate non- spleens than other breeds
■■ Barbiturates and certain tranquillisers cause
regenerative), bone marrow disorders or consump-
marked splenic congestion. However, Wilson
tion in haemolytic anaemia (eg, immune-mediated
and others (2004) found that an anaesthetic
haemolytic anaemia [IMHA], babesiosis or lympho- protocol comprising acepromazine plus an
proliferative disease). Spherocytes and schistocytes opiate premedication followed by propofol
may be present in IMHA and haemangiosarcomas, induction caused significantly less engorgement
respectively. Haemolysis and diffuse splenomegaly than protocols using medetomidine, diazepam,
can be associated with splenic torsion, which may ketamine or thiopentone
■■ Excitement and sympathetic catecholamines
resemble IMHA. Thrombocytopenia may be associ-
cause splenic contraction
ated with sepsis, lymphoproliferative disease, immune-
In Practice May 2012 | Volume 34 | 250–259 251
Downloaded from inpractice.bmj.com on February 23, 2014 - Published by group.bmj.com
Companion animal practice
Fig 2: Ultrasonographic image of a large nodule on the Fig 3: Doppler ultrasonography showing vascular stasis
parietal surface of the splenic body. Ultrasonography in the splenic vasculature of a dog with splenic torsion
allows the splenic parenchyma to be imaged
accurately, even in the presence of abdominal fluid orrhage. Percutaneous biopsy of the spleen is less
frequently performed due to the risk of severe haem-
the right atrium and auricle) and thoracic radiography orrhage. Surgical or laparoscopic biopsy is safer and
are indicated, given the behaviour of one of the main yields superior samples if a histopathological diag-
differential diagnoses (ie, haemangiosarcoma). nosis is required before a splenectomy is performed.
Doppler ultrasonography is particularly useful for Surgical biopsy may be performed using a Tru-cut
examining flow in the splenic vein in cases of suspected needle, an overlapping mattress suture technique or a
torsion (Fig 3) or thrombosis, but has not been shown to skin biopsy punch, with an almost identical technique
distinguish between benign and malignant focal disease to that routinely used to sample the liver. Topical hae-
(ie, haematoma and haemangiosarcoma) in the spleen mostatic agents (eg, Surgifoam; Johnson & Johnson)
reliably. Microbubble contrast-enhanced ultrasonogra- may be beneficial for haemostasis.
phy has shown slightly improved results at distinguish-
ing between neoplastic and benign lesions (Rossi and
others 2008), but cytological or, most often, histopatho- Splenectomy
logical evaluation tends to be necessary to enable this
distinction. Indications for a splenectomy include focal mass
lesions and torsion. Initially, a standard ventral midline
Biopsies celiotomy is performed and the abdomen is explored.
A fine-needle aspiration biopsy is a relatively low-risk Self-retaining retractors (eg, Balfour retractors) and
procedure that can be performed using ultrasound excision of the falciform fat may improve exposure of
guidance to investigate hyperechoic foci within the the abdominal viscera. In the presence of gross haemo-
parenchyma. Cytology is sensitive for the diagnosis of abdomen, it may not be possible to explore the abdo-
round cell tumours and extramedullary haematopoiesis men properly until a splenectomy has been performed.
but less sensitive for connective tissue tumours, which The spleen should be exteriorised and packed off with
tend to exfoliate cells poorly. Consequently, cytology damp laparotomy swabs.
is unlikely to distinguish between a haematoma and
haemangiosarcoma for a focal mass lesion, but may be Total splenectomy
diagnostic for a splenic lymphoma (Fig 4) or mast cell There are two acceptable methods for a total splenec-
tumour metastasis (Fig 5). Preoperative cytology has tomy. One involves ligation of the individual splenic
been reported to agree with postoperative histopathol- vessels as they branch to enter the hilus, working
ogy in about 60 per cent of cases (Ballegeer and others
2007).
A small risk of haemorrhage or neoplastic seeding
along needle tracts is inherent with needle aspiration
techniques and aspiration is relatively contraindicated
in animals with cavitary lesions due to the risk of haem-
Fig 5: Metastatic mast cell tumours can be diagnosed
Fig 4: Gross capsular changes in a canine spleen by ultrasound-guided fine-needle aspiration of
diffusely infiltrated by lymphoma (Picture, Prue Neath) suspicious hyperechoic foci in the splenic parenchyma
252 In Practice May 2012 | Volume 34 | 250–259
Downloaded from inpractice.bmj.com on February 23, 2014 - Published by group.bmj.com
Companion animal practice
Box 4: Automatic stapling
This auto suture powered ligating dividing stapler (LDS; is then divided between the staples by a small blade.
Tyco Healthcare) contains 15 pairs of titanium staples Although the device is expensive (about £125), this cost
and is designed for ligating small vessels and pedicles. is offset by reduced surgical time and the amount of
The cartridge jaw is placed around the pedicle and the suture material used. Use of such a device should be
device activated by squeezing the handle. Two staples are considered when surgical time must be minimised in
automatically placed 9·5 mm apart on the pedicle, which an unstable patient.
Auto suture powered ligating dividing stapler (LDS)
(above) and its use during a splenectomy (right)
from the tail to the head of the spleen. The main branch- Partial splenectomy
es of the splenic artery and vein are double-ligated and A partial splenectomy may be an option if there are
transfixed in larger dogs. A variety of suture materi- focal benign lesions or traumatic lacerations near the
als can be used for these ligations, including vicryl, head or tail of the spleen, but is not recommended
polydioxanone suture material and metal haemostatic in cases of malignant disease. The hilar vessels sup-
clips. Use of an automatic stapling device (Box 4) or plying the part of the spleen to be removed should
a vessel-sealing device (Covidien) minimises surgical be ligated and divided. Atraumatic Doyen forceps
time. are placed either side of the transaction line and the
A faster technique involves ligating the splenic spleen divided between these forceps. The cut surface
artery and vein within the omental bursa, followed of the spleen is then oversewn with a simple continuous
by the vessels at the head and tail of the spleen. This pattern to appose the cut edges of the capsule. For
method reduces surgical time and the amount of larger spleens, overlapping mattress sutures can be
suture material used but is not without risk. The placed through the parenchyma adjacent to the forceps
branches of the splenic artery supplying the left limb of to ensure ligation of larger vessels. A thoracoabdomi-
the pancreas must be identified and preserved to pre- nal stapler can be used to reduce the overall surgical
vent pancreatic ischaemia, but these vessels can be dif- time.
ficult to locate in a ‘fatty’ omentum, so this technique
is not recommended unless the surgeon is confident Possible complications
with the regional anatomy. Postoperative haemorrhage
Splenic surgery is aided by surgical suction; it is Postoperative haemorrhage may occur due to inad-
impossible to ensure adequate haemostasis has been equate intraoperative haemostasis, which may be
achieved and to perform a thorough metastasis check exacerbated by bleeding disorders. Postoperative
if blood remains in the abdomen. In some cases of packed cell volume (PCV) and total protein, heart
traumatic or non-neoplastic haemoabdomen, it may and respiratory rates, pulse quality, capillary refill
be possible to autotransfuse anticoagulated blood time (CRT) and mucous membrane colour should
through a microaggregate filter, but it is not recom- be monitored routinely after surgery. Postoperative
mended to leave blood in the abdomen. bleeding can be confirmed using ultrasonography
Following a splenectomy, biopsies or aspirates and measuring the PCV of fluid collected by
can be taken from the abdominal lymph nodes if indi- abdominocentesis.
cated, and any suspicious organ (eg, hepatic) lesions If the bleeding is acute and severe with signs of
can be biopsied. If possible, all hepatic lobes should be hypovolaemic shock (eg, tachycardia, tachypnoea, pale
visually examined and palpated for lesions. Hepatic mucous membranes and delayed CRT), further surgery
nodular hyperplasia is common in older dogs, so the is indicated to locate and ligate the source of the bleed.
presence of hepatic nodules does not always indicate If coagulation disorders are suspected, prothrombin
metastases. Ligatures on the splenic pedicle should be time, partial prothrombin time and platelet counts
rechecked before routine abdominal closure. should be obtained (if possible). If indicated, red blood
Histopathology is essential following a splenectomy cells and clotting factors can be supplemented using
as it is impossible to distinguish different pathologies on fresh whole blood, fresh plasma, fresh frozen plasma
gross examination. Ideally, the whole spleen should be and/or cryoprecipitate.
submitted for analysis, but if this is not possible it should
be sliced (like a loaf of bread) and several sections sub- Ventricular arrhythmias
mitted. The remainder of the organ should be kept in Ventricular arrhythmias are common after emer-
case unexpected or inconclusive results are obtained. gency splenic surgery and may occur up to 72 hours
254 In Practice May 2012 | Volume 34 | 250–259
Downloaded from inpractice.bmj.com on February 23, 2014 - Published by group.bmj.com
Companion animal practice
postoperatively. Although most intermittent aemic insults and have decreased platelet reserves, and
arrhythmias will be self-limiting, lidocaine infu- are therefore used as models of haemorrhagic shock.
sions are commonly used in some hospitals both for
analgesia and arrhythmia prophylaxis in high-risk Reduced capacity for extramedullary
patients. Occasional ventricular premature contrac- haematopoiesis
tions do not require treatment and are usually self- Splenic haematopoiesis may be significant in some
limiting, but indications for treatment include ven- haemolytic anaemias and bone marrow disorders.
tricular tachycardia (>180 beats per minute) or A splenectomy could be fatal in patients that are
haemodynamically significant arrhythmias affecting dependent on extramedullary haematopoiesis, and is
perfusion (eg, pulse deficits, poor peripheral pulses contraindicated in most anaemias.
and CRT).
Increased risk of GDV
Reduced vascular reservoir function A splenectomy could theoretically increase the risk
Splenectomised laboratory dogs have been shown to of gastric rotation, so prophylactic gastropexy could
have a reduced ability to compensate for acute hypovol- be considered at the time of a splenectomy in high-
Box 5: Case example
A 10-year-old female entire labrador retriever was
presented following two episodes of collapse in
the previous week from which it had recovered
spontaneously.
On examination, the animal was pale and tachycardic
(heart rate 116 beats per minute) but had a normal capillary
refill time (CRT) (less than two seconds). Splenomegaly
was suspected based on abdominal palpation.
Haematology, biochemistry and urinalysis were
performed. Both the biochemistry and urinalysis were
unremarkable except for mild elevations in hepatic
enzymes (alanine aminotransferase 61 iu/litre [reference
range 21 to 59 iu/litre] and alkaline phosphatase
238 iu/litre [reference range 3 to 142 iu/litre]) and
isosthenuria (specific gravity 1·009). The haematology Female labrador at presentation
report is shown in Table 1.
Ultrasonographic imaging of the abdomen was fluid had a packed cell volume (PCV) of 0·30 and
performed and revealed a large cavitated mass within was consistent with a diagnosis of haemoabdomen
the mid-body of the spleen and a mass adjacent to the secondary to a ruptured splenic mass.
spleen in the omentum. A large amount of free fluid The dog was placed on intravenous fluids and its
was present in the abdomen and sampled through blood pressure was monitored until surgery could be
abdominocentesis under ultrasound guidance. This performed. Bilateral chest radiographs, clotting profiles
and blood typing were also undertaken and the results
are given in Table 2.
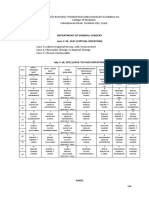
Table 1: Haematology results
The dog was premedicated with methadone,
Parameter Result* induced with propofol and maintained on isoflurane
White blood cells 29·8 (6·0-17·0) x 109/litre during surgery. Several additional boluses of fentanyl
were given during anaesthesia. Initially, intravenous
Neutrophils 25·9 (3·0-11·5) x 109/litre
crystalloid solution was given at 5 ml/kg/hour. Pulse
Lymphocytes 1·2 (1·0-4·8) x 109/litre oximetry, capnography, electrocardiogram, temperature
Eosinophils 0 (0·1-1·3) x 109/litre and Doppler blood pressure were monitored under
anaesthesia. To maintain the animal’s blood pressure,
Basophils 0 (0-0·5) x 109/litre
the fluid rate was increased to 10 ml/kg/hour and a
Red blood cells 3·7 (5·5-8·5) x 1012/litre 2 ml/kg bolus of hetastarch was given on two occasions
Haemoglobin 78 (120-180) g/litre during surgery.
The abdomen was prepared for surgery. A ventral
Haematocrit 0·23 (0·37-0·55) litre/litre midline coeliotomy was performed and Balfour
Mean corpuscular volume 61 (60-77) fl
Mean corpuscular 20·9 (19·5-24·5) pg Table 2: Clotting profiles and
haemoglobin blood typing results
Mean corpuscular 340 (320-370) g/litre Parameter Result*
haemoglobin concentration
One-stage 10·6 (7·6-11·6) seconds
Red blood cell distribution 18·1 (13·2-17·8) per cent prothrombin time
width
Activated partial 12·8 (12·5-25·0) seconds
Platelets 164 (175-500) x 109/litre thromboplastin time
Reticulocytes (absolute value) 184 x 109/litre Platelets 205 (175-500) x 109/litre
Reticulocytes 4·9 (0-1·0) per cent Blood group Dog erythrocyte antigen 1:1
negative
*Reference ranges are given in brackets
Note: absolute neutrophilia and monocytosis, red blood *Reference ranges are given in brackets
cell anisocytosis and polychromasia ++, platelets consistent Note: platelet count, prothrombin time and
with count, anaemia is slightly regenerative partial prothrombin time are within normal limits
256 In Practice May 2012 | Volume 34 | 250–259
Downloaded from inpractice.bmj.com on February 23, 2014 - Published by group.bmj.com
Companion animal practice
risk large and giant breeds. However, Goldhammer lateral supply to the stomach makes this clinically
and others (2010) reported no association between insignificant.
a splenectomy and an increased subsequent risk of
GDV and gastropexy is not routinely performed by the Increased risk of septicaemia
authors. Humans undergoing splenectomy have a 5 per cent
lifetime risk of overwhelming postsplenectomy infec-
Pancreatitis tion due a septicaemia or meningitis caused by encap-
The splenic artery is the principal supply to the sulated bacteria (eg, Streptococcus pneumoniae). This is
left limb of the pancreas and proximal ligation of thought to occur due to the loss of splenic macrophages
the splenic vascular pedicle can cause ischaemic and a reduced ability to remove opsonised bacteria
pancreatitis. It is safer to perform a splenec from the bloodstream. Hence, a partial splenectomy
tomy by ligation of the splenic vessels closer to the is performed in preference to a complete splenectomy
hilus. Ligation of the short gastric vessels in the gas- in humans. Asplenic humans receive additional vaccin
trosplenic ligament may reduce the vascular supply ations against encapsulated bacterial pathogens, anti
to part of the greater curvature; however, the col- biotic prophylaxis for wounds and dental treatment and
Right lateral abdominal radiograph showing an
Ultrasonographic image showing an irregular abdominal effusion and splenomegaly. The splenic
focal splenic lesion with omental adhesions capsule has an irregular outline
Large haematoma found in the omentum adherent
Haemoabdomen confirmed on entry into the to the splenic mass. This was confirmed to be a
abdominal cavity haemangiosarcoma by histopathology
retractors were used to improve exposure of the After surgery, the PCV was rechecked (0·21) and
abdomen viscera. A Poole suction tip was used to the dog was closely monitored for 36 hours, with vital
remove fluid from the abdomen and the spleen was parameters (heart and respiratory rates, systolic blood
isolated and packed off with moist laparotomy swabs. pressure, peripheral pulse quality, mucous membrane
The anatomy of the spleen was distorted by the focal colour and CRT) being recorded every two hours for the
mass and omental adhesions. A large blood clot was first 12 hours. Potential complications considered were
present within the omentum adjacent to the ruptured abdominal haemorrhage, disseminated intravascular
mass, as had been indicated by ultrasonography. coagulation, ventricular arrhythmias, sepsis and acute
The splenic artery was double-ligated early to renal failure. Blood products were available if signs
prevent further blood loss while the splenectomy of ongoing haemorrhage or coagulopathy became
was being performed. apparent.
After the splenectomy and removal of large The animal’s subsequent recovery was uneventful. The
blood clots from the abdomen, the abdominal viscera PCV and total protein were rechecked the next morning
was routinely examined and palpated but no gross and the dog was discharged two days after surgery.
metastatic lesions were evident. A total of 750 ml A haemangiosarcoma was confirmed by
of fluid was suctioned from the abdomen, and the histopathology. The owners declined further
abdomen was copiously lavaged with several litres of chemotherapy and the dog was euthanased
sterile saline to remove all blood clots. The splenectomy approximately 11 weeks after the splenectomy,
site was checked for bleeding before routine closure. with signs suggestive of metastatic disease.
In Practice May 2012 | Volume 34 | 250–259 257
Downloaded from inpractice.bmj.com on February 23, 2014 - Published by group.bmj.com
Companion animal practice
others 1988). A haemangiosarcoma is highly malignant
and overt metastasis has been reported in up to 80 per
cent of patients at presentation; it may coexist in both
the spleen and right atria in up to 25 per cent of dogs
(Walters and others 1988).
Dogs with a concurrent right atrial haemangio
sarcoma may present with signs of acute right-sided
Fig 6: Focal splenic lesion that was confirmed heart failure due to pericardial effusion. All types of
as a benign haematoma. (Picture, Prue Neath) haemangiosarcoma can be associated with cardiac
arrhythmias, disseminated intravascular coagulation
are at a higher risk of tropical vectorborne diseases (eg, (DIC) or sudden death.
malaria). These risks have not been reported in dogs, The prognosis for a confirmed haemangiosarcoma
but it is thought that canine babesia infections may be is poor, with median survival times of three to 12
more serious in asplenic animals. weeks after surgery alone. Doxorubicin chemotherapy
(four doses, three weeks apart) can be used to palli-
ate metastases and attempt to improve the survival
Specific splenic conditions time to four to six months; however, the one-year sur-
vival is less than 8 per cent (MacEwen 2001). Novel
Siderotic plaques (iron and calcium deposits) and some treatments, such as the use of angiogenesis inhibitors,
fibrinous material are normal changes and must not tumour vaccines and intracavitary chemotherapy, have
be confused with pathology. Small deposits of splenic been reported, with mixed results.
parenchyma in the omentum (‘splenosis’) can also be The prognosis for a splenic haematoma is better
an incidental finding and must not be confused with than for a haemangiosarcoma, with over 80 per cent
metastases. Splenosis is thought to arise from traumatic of dogs surviving the postoperative period and two-
rupture of the spleen and the subsequent grafting of thirds surviving at least one year (Prymak and others
fragments onto the omentum. 1988). However, this lower than expected survival rate
for a benign lesion may reflect undiagnosed systemic
Neoplasia disease or may represent histological misdiagnosis
Splenic neoplasia is relatively common in dogs and is the from the submission of inadequate tissue samples.
most frequent indication for a splenectomy. However, it
is impossible to differentiate between benign and malig- Torsion
nant lesions grossly and patients should not be eutha- Splenic torsion may be a primary condition or may occur
nased due to the presence of a focal, solitary splenic secondarily to GDV; it is most commonly reported in
lesion without a diagnosis. About 50 per cent of splenic large deep-chested breeds (similar to GDV). A variety
submissions to pathology laboratories demonstrate of presentations is possible, from an acute abdomen and
benign changes (eg, haematoma [Fig 6] and nodular circulatory shock to a chronic, grumbling condition with
hyperplasia) and the remaining 50 per cent are malig- non-specific signs of intermittent abdominal pain, vom-
nancies. About 25 per cent of dogs presenting with non- iting, anorexia, abdominal distension and polydipsia/
traumatic haemoabdomen have a benign haematoma polyuria (Neath and others 1997). The chronic disease
rather than a malignancy (Hammond and Pesillo-Crosby is frequently accompanied by anaemia, thrombocyto
2008, Aronsohn and others 2009). Haemangiosarcomas penia and leucocytosis due to inflammation and seques-
account for up to 80 per cent of malignancies, with the tration within the spleen. Liver enzymes are frequently
remainder comprising lymphomas, mast cell tumours, elevated, presumably due to systemic inflammation or
leiomyosarcomas, fibrosarcomas, osteosarcomas and circulatory compromise. Haemoglobinuria is common
malignant fibrous histiocytomas (Spangler and Kass due to haemolysis and patients may develop cardiac
1997). Splenic tumours are most frequently seen in arrhythmias or progress to DIC.
older large-breed dogs, with German shepherd dogs Abdominal imaging will identify an enlarged spleen,
and labrador retrievers over-represented (Prymak and possibly with an abdominal effusion. Ultrasonography
Fig 7: (a) Engorged spleen of a
weimaraner presenting with
a splenic torsion. (b) Torsed
vascular pedicle of the same
spleen. (Pictures, Laura Owen) A B
258 In Practice May 2012 | Volume 34 | 250–259
Downloaded from inpractice.bmj.com on February 23, 2014 - Published by group.bmj.com
Companion animal practice
References
Box 6: Splenic disease in cats ARONSOHN, M. G., DUBIEL, B., ROBERTS,
B. & POWERS, B. E. (2009) Prognosis for acute
Splenic lesions appear to be less common in cats than nontraumatic hemoperitoneum in the dog: a
dogs, with most lesions causing diffuse rather than retrospective analysis of 60 cases (2003-2006).
focal enlargement. A large survey of feline splenic Journal of the American Animal Hospital Association
submissions showed the most common malignancies 45, 72-77
to be visceral mast cell tumour (15 per cent), BALLEGEER, E. A., FORREST, L. J., DICKINSON,
lymphoma (9 per cent), myeloproliferative disease R. M., SCHUTTEN, M. M., DELANEY, F. A. &
(6 per cent) and haemangiosarcoma (3 per cent), YOUNG, K. M. (2007) Correlation of ultrasonographic
although a high proportion of submitted spleens appearance of lesions and cytologic and histologic
were considered ‘normal’ (15 per cent) or ‘congested’ diagnoses in splenic aspirates from dogs and cats:
(9 per cent) (Spangler and Culbertson 1992). 32 cases (2002-2005). Journal of the American
Although a splenectomy is indicated for the Veterinary Medical Association 230, 690-696
management of focal haemangiosarcoma and is GOLDHAMMER, M. A., HAINING, H., MILNE,
useful as an adjunctive treatment for feline visceral E. M., SHAW, D. J. & YOOL, D. A. (2010) Assessment
mastocytosis, the treatment of myeloproliferative of the incidence of GDV following splenectomy in
diseases and lymphoma by chemotherapy may be dogs. Journal of Small Animal Practice 51, 23-28
delayed by surgical splenectomy. Hence, ultrasound- GOLDSMID, S. E., DAVIS, P. & PECHMAN, R.
guided fine-needle aspiration may be a better course (1994) Successful derotation of a splenic torsion in a
of action unless focal gross pathology is present. racing greyhound. Journal of Small Animal Practice
35, 112-115
HAMMOND, T. N. & PESILLO-CROSBY, S. A.
(2008) Prevalence of hemangiosarcoma in anemic
is useful for imaging the hypoechoic parenchyma and
dogs with a splenic mass and hemoperitoneum
Doppler ultrasonography of the hilus and vascular
requiring a transfusion: 71 cases (2003-2005).
pedicle by skilled operators is both specific and sensi- Journal of the American Veterinary Medical Association
tive for diagnosing torsion or thromboembolism. 232, 553-558
Following appropriate stabilisation, the treatment MACEWEN, E. G. (2001) Miscellaneous tumours:
of choice is a splenectomy, taking care not to untwist haemangiosarcoma. In Small Animal Clinical
the vascular pedicle, although successful derotation Oncology, 3rd edn. Eds S. J. Withrow and
E. G. MacEwan. Lea & Febiger. pp 295-297
of a splenic torsion has been reported (Goldsmid and
NEATH, P. J., BROCKMAN, D. J. & SAUNDERS,
others 1994). The vascular pedicle should be gradually
H. M. (1997) Retrospective analysis of 19 cases
divided and ligated and care must be taken to ligate the of isolated torsion of the splenic pedicle in dogs.
splenic artery distal to the pancreatic branch (Fig 7). Journal of Small Animal Practice 38, 387-392
If torsion or necrosis of the left lobe of the pan- PRYMAK, C., MCKEE, L. J., GOLDSCHMIDT,
creas is also present, a partial pancreatectomy should M. H. & GLICKMAN, L. T. (1988) Epidemiologic,
be performed. clinical, pathologic, and prognostic characteristics of
splenic hemangiosarcoma and splenic hematoma in
dogs: 217 cases. Journal of the American Veterinary
Trauma Medical Association 193, 706-712
Splenic laceration resulting from a penetrating injury ROSSI, F., LEONE, V. F., VIGNOLI, M., LADDAGA,
and splenic rupture due to blunt abdominal trauma are E. & TERRAGNI, R. (2008) Use of contrast-enhanced
probably underdiagnosed as the injury is either unrec- ultrasound for characterization of focal splenic lesions.
ognised and self-limiting or rapidly fatal. The preva- Veterinary Radiology & Ultrasound 49, 154-164
SPANGLER, W. L. & CULBERTSON, M. R. (1992)
lence of healed splenic fractures and implanted splenic
Prevalence and type of splenic diseases in cats: 455
fragments (splenosis) as incidental findings during
cases (1985-1991). Journal of the American Veterinary
exploratory celiotomies suggests that blunt trauma is Medical Association 201, 773-776
underdiagnosed. Iatrogenic splenic injuries may occur SPANGLER, W. L. & KASS, P. H. (1997) Pathologic
during abdominocentesis, ultrasound-guided biopsy factors affecting postsplenectomy survival in dogs.
of abdominal organs, sharp incision through the linea Journal of Veterinary Internal Medicine 11, 166-171
alba and percutaneous gastrostomy tube placement. SPANGLER, W. L. & KASS, P. H. (1998) Pathologic
and prognostic characteristics of splenomegaly in dogs
Haemoabdomen following trauma must be care-
due to fibrohistiocytic nodules: 98 cases. Veterinary
fully managed, using intravenous fluids, abdominal
Pathology 35, 488-498
compression bandaging or appropriate blood prod- WALTERS, D. J., CAYWOOD, D. D., HAYDEN,
ucts, and monitored (ie, cardiovascular status includ- D. W. & KLAUSNER, J. S. (1988) Metastatic pattern
ing blood pressure and serial monitoring of PCV in dogs with splenic haemangiosarcomas: clinical
and total protein). An approach termed ‘hypotensive implications. Journal of Small Animal Practice 29,
resuscitation’ should be adopted, in which the need to 805-814
WILSON, D. V., EVANS, A. T., CARPENTER, R. A.
support the circulation is balanced without exacerbat-
& MULLINEAUX, D. R. (2004) The effect of four
ing bleeding, similar to that for patients with pulmo- anesthetic protocols on splenic size in dogs. Veterinary
nary contusions. Failure to stabilise with supportive Anaesthesia and Analgesia 31, 102-108
treatment or excessive abdominal haemorrhage is an
obvious indication for an emergency celiotomy. Further Reading
Surgical options for treating splenic trauma include ARMBRUST, L. (2009) The spleen. In BSAVA Manual
of Canine and Feline Abdominal Imaging. Eds R.
the use of topical haemostatic agents (eg, Surgifoam),
O’Brien and F. Barr. BSAVA Publications. pp 167-176
primary surgical repair and a partial or complete
MISON, M. & NILES, J. D. (2005) The spleen.
splenectomy. Temporary occlusion of the splenic artery In BSAVA Manual of Canine and Feline Abdominal
(by an assistant, a Rummel tourniquet or vascular Surgery. Eds J. M. Williams and J. D. Niles. BSAVA
clamps) can be performed to facilitate surgery. Publications. pp 220-233
In Practice May 2012 | Volume 34 | 250–259 259
Downloaded from inpractice.bmj.com on February 23, 2014 - Published by group.bmj.com
Investigation and management of splenic
disease in dogs
Graham Hayes and Jane Ladlow
In Practice 2012 34: 250-259
doi: 10.1136/inp.e3107
Updated information and services can be found at:
http://inpractice.bmj.com/content/34/5/250.full.html
These include:
References This article cites 13 articles, 2 of which can be accessed free at:
http://inpractice.bmj.com/content/34/5/250.full.html#ref-list-1
Email alerting Receive free email alerts when new articles cite this article. Sign up in
service the box at the top right corner of the online article.
Notes
To request permissions go to:
http://group.bmj.com/group/rights-licensing/permissions
To order reprints go to:
http://journals.bmj.com/cgi/reprintform
To subscribe to BMJ go to:
http://group.bmj.com/subscribe/
You might also like
- Splenectomy in Dogs and Cats: Indications, Surgical Technique, and Postoperative CareDocument3 pagesSplenectomy in Dogs and Cats: Indications, Surgical Technique, and Postoperative CareBeratha MuktiNo ratings yet
- SpleenDocument42 pagesSpleenRashed LabNo ratings yet
- Surgical Diseases of PancreasDocument17 pagesSurgical Diseases of PancreasIris BakerNo ratings yet
- Splenectomy Splenectomy Is Surgical Removal of The Spleen. AnesthesiaDocument3 pagesSplenectomy Splenectomy Is Surgical Removal of The Spleen. AnesthesiaZAHID KHANNo ratings yet
- Surgical Diseases of The SpleenDocument28 pagesSurgical Diseases of The SpleenRassoul Abu-NuwarNo ratings yet
- Top 5 Causes of Splenomegaly in Dogs - Clinicians BriefDocument5 pagesTop 5 Causes of Splenomegaly in Dogs - Clinicians Briefludiegues752No ratings yet
- Schwartz 9th Ed: Chapter Outline: The SpleenDocument22 pagesSchwartz 9th Ed: Chapter Outline: The SpleenKathryn Reunilla100% (1)
- Abiola Seminar in SpleenDocument23 pagesAbiola Seminar in SpleenBamgbose OpeyemiNo ratings yet
- Pancreas: Anatomy of The PancreasDocument11 pagesPancreas: Anatomy of The PancreasHart ElettNo ratings yet
- Git 301 Final 2021 Section TwoDocument8 pagesGit 301 Final 2021 Section TwoBright LunetaNo ratings yet
- Jejunal and Ileal AtresiasDocument37 pagesJejunal and Ileal AtresiasABDUL RAHIM UMAR FAROUKNo ratings yet
- Renal SystemDocument76 pagesRenal SystemDaNy ChiriacNo ratings yet
- (Surg2-Trans) 3.09 SpleenDocument7 pages(Surg2-Trans) 3.09 SpleenJake Brandon M. Andal, RNDNo ratings yet
- SpleenDocument33 pagesSpleenAin AmanyNo ratings yet
- 27.liver and Gastrointestinal PhysiologyDocument12 pages27.liver and Gastrointestinal PhysiologyAnggreany AshariNo ratings yet
- Week 5Document12 pagesWeek 5Prima LebananNo ratings yet
- Pancreas and SpleenDocument44 pagesPancreas and SpleenOgbuefi PascalNo ratings yet
- EsplenomegaliaDocument24 pagesEsplenomegaliaJhonatan Efraín López CarbajalNo ratings yet
- LAB 5 MeDocument4 pagesLAB 5 MeMuhammad WajahatNo ratings yet
- Javma-Javma 20 09 0497Document3 pagesJavma-Javma 20 09 0497Fiorella YavarNo ratings yet
- Magnetic Resonance LymphangiographyDocument14 pagesMagnetic Resonance LymphangiographyHector Hernandez-SoriaNo ratings yet
- Acute GlomerulonephritisDocument32 pagesAcute Glomerulonephritismelese woldehawariatNo ratings yet
- Mucocele 2Document13 pagesMucocele 2FEY YENG SOFIA FUNG GUADALUPENo ratings yet
- JCDR 9 PD26Document2 pagesJCDR 9 PD26ceciliaNo ratings yet
- Approach To The Adult Patient With Splenomegaly and Other Splenic DisordersDocument53 pagesApproach To The Adult Patient With Splenomegaly and Other Splenic DisordersPrabuunair2013No ratings yet
- (Surg 3A) Spleen and Friends-Dr. Segismundo, Dr. Broqueza (Aisle Paler, Joseph Tolentino)Document15 pages(Surg 3A) Spleen and Friends-Dr. Segismundo, Dr. Broqueza (Aisle Paler, Joseph Tolentino)Aria Jean MostajoNo ratings yet
- The Spleen: Hugo W. TilanusDocument9 pagesThe Spleen: Hugo W. TilanusTotolici StefanNo ratings yet
- Histology and Gross Pancreas 2019Document59 pagesHistology and Gross Pancreas 2019Azwaah Hassan100% (1)
- Open SplenectomyDocument14 pagesOpen SplenectomyLucieVunhuNo ratings yet
- 7 SemesterDocument68 pages7 SemesterbelizrivadeNo ratings yet
- Endoscopic Ultrasound Staging of Gastric LymphomaDocument3 pagesEndoscopic Ultrasound Staging of Gastric LymphomaEvainoirNo ratings yet
- TO Splenectomy 2Document31 pagesTO Splenectomy 2sphericalfaNo ratings yet
- Disorders of The PancreasDocument77 pagesDisorders of The PancreasGeofry OdhiamboNo ratings yet
- The Vermiform Appendix: AnatomyDocument10 pagesThe Vermiform Appendix: AnatomyBereket temesgenNo ratings yet
- Avian Renal System Clinical ImplicationsDocument19 pagesAvian Renal System Clinical ImplicationsAnais FaveroNo ratings yet
- Vagus Indigestionعسر الهضم المسبب باصابة العصب الحائرDocument27 pagesVagus Indigestionعسر الهضم المسبب باصابة العصب الحائرAli H. Sadiek أ.د. علي حسن صديق100% (3)
- Oliver 2004Document11 pagesOliver 2004SDNKSJNDJKNo ratings yet
- Francisco G. La Rosa, M.D.: Pancreas Pathology and Diabetes Mellitus (Course Dsbs 5516)Document10 pagesFrancisco G. La Rosa, M.D.: Pancreas Pathology and Diabetes Mellitus (Course Dsbs 5516)madaniNo ratings yet
- Puentes Portosistémicos: Reporte de Un Caso ClínicoDocument5 pagesPuentes Portosistémicos: Reporte de Un Caso ClínicobumetroNo ratings yet
- Billiary SystemDocument60 pagesBilliary SystemDONALD UNASHENo ratings yet
- Characterization of Primary Pulmonary Adenosquamous Carcinoma-Associated Pleural EffusionDocument5 pagesCharacterization of Primary Pulmonary Adenosquamous Carcinoma-Associated Pleural EffusionIoana SanduNo ratings yet
- Disorders of EsophagusDocument27 pagesDisorders of EsophagusFranci Kay SichuNo ratings yet
- A Case of Amoebic Liver Abscess Complicated by Bilhaemia and Venous ThrombosisDocument2 pagesA Case of Amoebic Liver Abscess Complicated by Bilhaemia and Venous ThrombosisEdgar Azael GarciaNo ratings yet
- WSC 22-23 Conf 9 Illustrated Results - FinalDocument21 pagesWSC 22-23 Conf 9 Illustrated Results - FinalGustavo MurgaNo ratings yet
- Cells of The LiverDocument4 pagesCells of The LiverAveryNo ratings yet
- Ligaments of The Liver: Teachmeseries LTDDocument14 pagesLigaments of The Liver: Teachmeseries LTDstella pangestikaNo ratings yet
- Diuretics: Dr. Ashley M. StokesDocument26 pagesDiuretics: Dr. Ashley M. StokesDhaif dhaifNo ratings yet
- Hydatid Disease of The Liver: ReviewDocument8 pagesHydatid Disease of The Liver: ReviewRafki HidayatNo ratings yet
- Avian Renal SystemDocument19 pagesAvian Renal SystemYaiza Garcia CasadoNo ratings yet
- Cloacal Prolapse in TortoiseDocument21 pagesCloacal Prolapse in TortoiseNabin NeupaneNo ratings yet
- Anatomy of Spleen: Research TitleDocument8 pagesAnatomy of Spleen: Research TitleOmar MohammedNo ratings yet
- Interventional Radiology Management of High Flow PriapismDocument11 pagesInterventional Radiology Management of High Flow PriapismMANGNo ratings yet
- Department of Histology, Cytology and EmbryologyDocument8 pagesDepartment of Histology, Cytology and Embryologysubmen81No ratings yet
- Scrotal MassesDocument19 pagesScrotal MassesJohnNo ratings yet
- CH 32 Gallbladder and Extrahepatic Biliary SystemDocument33 pagesCH 32 Gallbladder and Extrahepatic Biliary SystemElisha BernabeNo ratings yet
- Review Article: Splenic Anomalies of Shape, Size, and Location: Pictorial EssayDocument10 pagesReview Article: Splenic Anomalies of Shape, Size, and Location: Pictorial EssayyurikepratiwiNo ratings yet
- Anatomie Cai BiliareDocument4 pagesAnatomie Cai BiliareLarisa StanNo ratings yet
- Small & Large Intestines - LectureDocument70 pagesSmall & Large Intestines - Lecturehussain AltaherNo ratings yet
- Bazo Errante 2016 REVISED Ijtra1601084Document4 pagesBazo Errante 2016 REVISED Ijtra1601084luisalfredo_montesNo ratings yet
- Pathogens: Diagnostic Tools For The Identification of Babesia Sp. in Persistently Infected CattleDocument14 pagesPathogens: Diagnostic Tools For The Identification of Babesia Sp. in Persistently Infected CattleSara ConnorNo ratings yet
- Disordersofrumen Distensionanddysmotility: Derek FosterDocument14 pagesDisordersofrumen Distensionanddysmotility: Derek FosterSara ConnorNo ratings yet
- Vagus Indigestion in Bovines: A Review in Historical PerspectiveDocument8 pagesVagus Indigestion in Bovines: A Review in Historical PerspectiveSara ConnorNo ratings yet
- Veterinary Clinics of North America - Food Animal Practice Volume Issue 2017 (Doi 10.1016 - J.cvfa.2017.06.003) Snyder, Emily Credille, Bren PDFDocument11 pagesVeterinary Clinics of North America - Food Animal Practice Volume Issue 2017 (Doi 10.1016 - J.cvfa.2017.06.003) Snyder, Emily Credille, Bren PDFAshadiSyamsirNo ratings yet
- Sall Intestinal Surgery Techniques: Cllipi) TicallDocument14 pagesSall Intestinal Surgery Techniques: Cllipi) TicallSara ConnorNo ratings yet
- Surgical Conditions of The StomachDocument12 pagesSurgical Conditions of The StomachSara ConnorNo ratings yet
- Field Study of Dairy Cows With Reduced Appetite in Early LactationDocument10 pagesField Study of Dairy Cows With Reduced Appetite in Early LactationSara ConnorNo ratings yet
- In Practice-2000-Baines-502-17Document12 pagesIn Practice-2000-Baines-502-17Sara ConnorNo ratings yet
- MacFarlane - Chronic Pain in DogsDocument9 pagesMacFarlane - Chronic Pain in DogsSara ConnorNo ratings yet
- 9 - Pdfsam - Vsu12006 - Assessment of Surgical SkillsDocument1 page9 - Pdfsam - Vsu12006 - Assessment of Surgical SkillsSara ConnorNo ratings yet
- Suture Materials and Patterns PDFDocument9 pagesSuture Materials and Patterns PDFSara ConnorNo ratings yet
- Hipodens Non Enhancing Brain LesionDocument7 pagesHipodens Non Enhancing Brain LesionJuwita Valen RamadhanniaNo ratings yet
- Nbme 13Document22 pagesNbme 13Schi WeiNo ratings yet
- Mefenamic Acid Drug StudyDocument1 pageMefenamic Acid Drug StudyBer AnneNo ratings yet
- Іnfect dis test eng 5 courseDocument44 pagesІnfect dis test eng 5 courseSanyam KhannaNo ratings yet
- PPR Koumakis Dementia Care FrameworksDocument15 pagesPPR Koumakis Dementia Care FrameworksLuis Eduardo Ronquillo OrdoñezNo ratings yet
- Arellano University College of Nursing Legarda - Pasay - PasigDocument3 pagesArellano University College of Nursing Legarda - Pasay - PasigCharles Loriaga Cruz IINo ratings yet
- Tetralogy of Fallot (TOF) : Dr. Sayeedur Rahman Khan Rumi MD Final Part Student Nhfh&RiDocument49 pagesTetralogy of Fallot (TOF) : Dr. Sayeedur Rahman Khan Rumi MD Final Part Student Nhfh&RiPrazNo ratings yet
- Genetic TestingDocument18 pagesGenetic Testingneha100% (1)
- Schrier's Diseases of The Kidney Volume 1Document1,328 pagesSchrier's Diseases of The Kidney Volume 1Andra100% (1)
- Definition:: Pleural EffusionDocument4 pagesDefinition:: Pleural EffusionGetom NgukirNo ratings yet
- Slide Webinar TiroidDocument28 pagesSlide Webinar TiroidmariaNo ratings yet
- Pneumonitis and Pneumonia After AspirationDocument12 pagesPneumonitis and Pneumonia After AspirationmitahalidNo ratings yet
- Renal Cell Carcinoma Tuberous SclerosisDocument48 pagesRenal Cell Carcinoma Tuberous SclerosisPiyushNo ratings yet
- Enzyme IsoenzymesDocument60 pagesEnzyme IsoenzymesSrishti GoenkaNo ratings yet
- Ampicillin SulbactamDocument3 pagesAmpicillin Sulbactamrhon_123rd88% (17)
- Management and Prevention of Complications During Initial Treatment of Head and Neck Cancer - UpToDateDocument19 pagesManagement and Prevention of Complications During Initial Treatment of Head and Neck Cancer - UpToDateAchmad MusaNo ratings yet
- Tertiary SyphilisDocument19 pagesTertiary SyphilisLakshya J BasumataryNo ratings yet
- PROTEINURIA and Nephrotic SyndDocument57 pagesPROTEINURIA and Nephrotic SyndRobert FfrenchNo ratings yet
- Doña Remedios Trinidad Romualdez Medical Foundation Inc. College of Medicine Calanipawan Road, Tacloban City, LeyteDocument2 pagesDoña Remedios Trinidad Romualdez Medical Foundation Inc. College of Medicine Calanipawan Road, Tacloban City, LeyteIrish AlonzoNo ratings yet
- Kawasaki DiseaseDocument15 pagesKawasaki DiseaseAlyssa QuindiaganNo ratings yet
- Ch. 7 Lecture - Nervous System (Marieb)Document92 pagesCh. 7 Lecture - Nervous System (Marieb)Asfand ShaikhNo ratings yet
- Drug StudyDocument4 pagesDrug StudyKaloy AnneNo ratings yet
- Peadiatric Advanced Life Support (Pals)Document18 pagesPeadiatric Advanced Life Support (Pals)SREEDEVI T SURESHNo ratings yet
- Case Report in Genetics: AnamnesisDocument6 pagesCase Report in Genetics: AnamnesisRamziya KadoraNo ratings yet
- Depolarizing Muscle RelaxantDocument40 pagesDepolarizing Muscle RelaxantMohammad HayajnehNo ratings yet
- Laban Movement Analysis Using KinectDocument11 pagesLaban Movement Analysis Using KinectRodrigo Balthar FurmanNo ratings yet
- Asthma: Differential Diagnosis and ComorbiditiesDocument9 pagesAsthma: Differential Diagnosis and ComorbiditiesQuel PaivaNo ratings yet
- HypoparathyroidismDocument2 pagesHypoparathyroidismLorelyn Santos CorpuzNo ratings yet
- Gmo Persuasive SpeechDocument2 pagesGmo Persuasive Speechnaomi88GnR44% (9)
- Homeostatic Imbalances: in The Integumentary SystemDocument27 pagesHomeostatic Imbalances: in The Integumentary SystemMarilou Dacles IINo ratings yet