Professional Documents
Culture Documents
Shehaan Syndrom
Shehaan Syndrom
Uploaded by
Anonymous be1sWu6l6Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Shehaan Syndrom
Shehaan Syndrom
Uploaded by
Anonymous be1sWu6l6Copyright:
Available Formats
PRIMER
Sheehan syndrome
Züleyha Karaca1, Bashir A. Laway2, Hatice S. Dokmetas3, Hulusi Atmaca4
and Fahrettin Kelestimur1
Abstract | Sheehan syndrome or postpartum hypopituitarism is a condition characterized by
hypopituitarism due to necrosis of the pituitary gland. The initial insult is caused by massive
postpartum haemorrhage (PPH), leading to impaired blood supply to the pituitary gland, which has
become enlarged during pregnancy. Small sella turcica size, vasospasms (caused by PPH) and/or
thrombosis (associated with pregnancy or coagulation disorders) are predisposing factors;
autoimmunity might be involved in the progressive worsening of pituitary functions. Symptoms are
caused by a decrease or absence of one or more of the pituitary hormones, and vary, among others,
from failure to lactate and nonspecific symptoms (such as fatigue) to severe adrenal crisis.
In accordance with the location of hormone-secreting cells relative to the vasculature, the secretion of
growth hormone and prolactin is most commonly affected, followed by follicle-stimulating hormone
and luteinizing hormone; severe necrosis of the pituitary gland also affects the secretion of thyroid-
stimulating hormone and adrenocorticotropic hormone. Symptoms usually become evident years
after delivery, but can, in rare cases, develop acutely. The incidence of Sheehan syndrome depends, to
a large extent, on the occurrence and management of PPH. Sheehan syndrome is an important cause
of hypopituitarism in developing countries, but has become rare in developed countries. Diagnosis is
based on clinical manifestations combined with a history of severe PPH; hormone levels and/or
stimulation tests can confirm clinical suspicion. Hormone replacement therapy is the only available
management option so far.
Sheehan syndrome refers to postpartum hypopitu professionals3,4. The syndrome has been increasingly
itarism or a decrease or absence of one or more of recognized as one of the leading causes of hypopitu
the hormones secreted by the pituitary gland (further itarism in developing countries5,6 and thus represents a
referred to as hypopituitarism) (TABLE 1). The disorder considerable public health concern worldwide. Sheehan
is caused by necrosis of the pituitary gland (FIG. 1a) as a syndrome is associated with increased morbidity con
consequence of severe hypotension or shock owing to sidering its nonspecific signs and symptoms and most
massive uterine bleeding during or soon after child patients remain undiagnosed and untreated for a long
birth. The disorder was first described by Harold time. In this Primer, we provide a comprehensive
Leeming Sheehan in 1937 (REF. 1), although he used the overview of Sheehan syndrome.
terms postpartum pituitary necrosis and hypopituitar
ism2. Sheehan syndrome is characterized by variable Epidemiology
degrees of anterior and sometimes posterior pituitary Studies conducted so far, although limited in number,
gland dysfunction. Deficiencies of the hormones that show that hypopituitarism is a relatively rare condi
are secreted by the anterior pituitary gland can result tion in the developed world (TABLE 2). One population
in secondary hypothyroidism, adrenal failure, hypo study in Spain reported a prevalence of hypopitu
gonadism, lactation failure and growth hormone (GH) itarism of 45.5 per 1,000,000 and an incidence of 4.2
Correspondence to F.K. deficiency. Although rare, the posterior pituitary gland new cases per 1,000,000 per person per year in 2001
Department of Endocrinology, might also be affected, which can result in central dia (REF. 7). Pituitary tumours and their treatments are the
Erciyes University Medical betes insipidus (a lack of arginine vasopressin (AVP) most common causes of hypopituitarism (~60%) and
School, 38039, Kayseri,
that causes polyuria). The incidence of Sheehan syn ~30% of hypopituitarism cases have a non-tumour
Turkey.
fktimur@erciyes.edu.tr drome has declined in the past few decades in the devel origin. Sheehan syndrome explains 6% of all causes of
oped world as a result of modernized obstetrical care, hypopituitarism. A more recent study in the same area
Article number: 16092
doi:10.1038/nrdp.2016.92 although the numbers might be underestimated owing published in 2013, comprising 405,218 adults followed
Published online 22 Dec 2016 to less recognition of the syndrome among medical for a period of 10 years, showed a prevalence and an
NATURE RE VIE WS | DISEASE PRIMERS VOLUME 2 | 2016 | 1
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
PRIMER
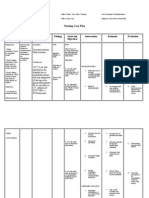
Author addresses Mechanisms/pathophysiology
Vascularization of the pituitary gland
1
Department of Endocrinology, Erciyes University Medical The pituitary gland receives its arterial blood supply
School, 38039, Kayseri, Turkey. from the superior and inferior hypophyseal arteries
2
Department of Endocrinology, Sher‑I‑Kashmir Institute (FIG. 1b). The infundibulum, the median eminence (a part
of Medical Sciences (SKIMS), Srinagar, Jammu and Kashmir,
of the hypothalamus from which regulatory hormones
India.
3
Department of Endocrinology, Istanbul Medipol are released) and the pars tuberalis are supplied by the
University Medical School, Istanbul, Turkey. superior hypophyseal artery (a branch of the internal
4
Department of Endocrinology, Ondokuz Mayıs University carotid artery) and the posterior lobe by the inferior
Medical School, Samsun, Turkey. hypophyseal artery (arising from the meningohypo
physeal trunk, which is a branch of the internal carotid
artery). By contrast, the pars distalis receives very little to
incidence of hypopituitarism of 37.5 cases per 100,000 no arterial blood supply by the internal carotid artery 15,16.
inhabitants and 2.07 cases per 100,000 inhabitants per Instead, the pars distalis is mainly supplied by the venous
year, respectively 8. No cases of Sheehan syndrome were system; one route of blood supply is through the long
identified, which might be explained by an improve portal veins that descend via the infundibulum and
ment in obstetrical care during the 12 years between connect the capillary beds in the pars distalis with those
these two studies. of the portal capillary system in the median eminence.
Indeed, severe postpartum haemorrhage (PPH) is an In addition, the pars distalis receives venous blood from
important risk factor for the development of Sheehan the posterior pituitary gland through the short portal
syndrome. As early as in 1939, Sheehan estimated that vessels; this route accounts for 30% of the total blood
41% of women who survived severe PPH and/or hypo supply to the anterior pituitary gland17,18. Its unique
volemic shock had either partial or severe hypopitu circulation allows the pars distalis to receive hormones
itarism compared with 15% of women with moderate from the hypothalamus and the posterior pituitary
PPH9. Improvements in obstetrical care and methods gland, besides substances from peripheral circulation.
of preventing hypovolemic shock despite severe blood However, this circulation type makes the pituitary
loss (such as early blood transfusion and/or administra vulnerable to ischaemia due to hypovolemia and hypo
tion of intravenous fluids) have considerably decreased tension during the postpartum period, as pregnancy
the incidence of Sheehan syndrome in developed leads to physiological growth of the pituitary gland and
countries10,11. However, owing to the continuing practice compression of the vasculature19. Venous drainage of
of home deliveries12 and poor health care structure in the anterior pituitary gland is by the hypophyseal veins
some primary-care hospitals, Sheehan syndrome con and the posterior pituitary gland via the short portal and
tinues to be a cause of preventable h ypopituitarism in hypophyseal veins to the cavernous sinus.
women in developed countries (TABLE 2).
The prevalence of Sheehan syndrome is higher in Pituitary hormones
developing countries than in developed countries Anterior pituitary hormones are controlled by the releas
(TABLE 2). For example, in Kashmir, India, the preva ing and inhibiting factors secreted from the hypothala
lence of Sheehan syndrome was estimated to be ~3.1% mus20 (TABLE 1). Anterior pituitary hormones stimulate
of parous women ≥20 years of age; ~63% of the women the secretion of their target hormones, which mediate
with Sheehan syndrome in this study had given birth most of the outcome, except for prolactin (PRL) and par
at home. The high prevalence of Sheehan syndrome tially GH, which both also have direct effects. Pituitary
has been suggested to be representative not only of hormone secretion is regulated by a feedback mech
the whole of India but also of some other developing anism. Anterior pituitary hormones regulate the secre
c ountries with similar obstetrical care available to tion of hypothalamic factors by a feedback mechanism.
the general population6. A retrospective study from a The regulation of the hypothalamic–pituitary–adrenal
tertiary-care hospital in the Philippines showed that (HPA) axis as a representative of hormonal axes is shown
pituitary adenomas were the most common cause of in FIG. 2 (REF. 21).
hypopituitarism (40% of 143 patients with hypopitu The posterior pituitary gland releases AVP and
itarism), whereas Sheehan syndrome was the third- oxytocin, both of which are mainly synthesized in the
most common aetiology (8% of all patients with hypothalamus. Oxytocin is one of the few hormones to
hypopituitarism)13. Sheehan syndrome was even the create a positive-feedback loop. Indeed, uterine contrac
most common cause of hypopituitarism in women tions stimulate the release of oxytocin, which, in turn,
in Turkey 14. The disorder is more common in older increases uterine contractions. This positive-feedback
women than in young women (<40 years of age), with loop continues throughout labour 22.
a mean age of diagnosis of 52.8 years (standard devi
ation (SD) ± 12.3 years)14. Another retrospective study Pituitary gland enlargement in pregnancy
conducted in Turkey showed that the number of new Pregnancy is a physiological state that puts strains on
patients with Sheehan syndrome diagnosed each decade the pituitary gland owing to changing demands of
was directly proportional to the number of home- the mother and fetus and the release of hormones by the
conducted deliveries, although five new cases were seen placenta (such as adrenocorticotropic hormone (ACTH),
in patients who had delivered in the hospital5. human chorionic gonadotropin (hCG), estradiol and
2 | 2016 | VOLUME 2 www.nature.com/nrdp
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
PRIMER
Table 1 | Hormones released by the pituitary gland
Pituitary hormone Secretory Hypothalamic Target hormone Target Disease caused Characteristic
pituitary cell regulatory by deficiency symptoms
hormone of the pituitary
hormone
Anterior lobe
Growth hormone Somatotropic GH-releasing Insulin-like growth Direct effect on GH deficiency Weight gain, impaired
(GH) cells hormone (GHRH) factor 1 (IGF‑1) many organs, quality of life and
and GH-release- mainly the liver decreased lean
inhibiting body mass
hormone
(somatostatin)
Prolactin (PRL) Lactotroph Dopamine Not known Direct effect on the PRL deficiency Failure to lactate
cells mammary gland
Follicle-stimulating Gonadotropic Gonadotropin- Inhibin, estradiol and Release of sex Secondary Amenorrhoea,
hormone (FSH) cells releasing testosterone steroids and inhibin hypogonadism infertility and hair loss
hormone (GnRH) by the gonads
Luteinizing Gonadotropic GnRH Estradiol (in women) Release of sex
hormone (LH) cells and testosterone steroids by the
(in men) gonads
Thyroid-stimulating Thyrotropic Thyrotropin- Tetraiodothyronine Release of thyroid Secondary Weight gain,
hormone (TSH) cells releasing (T4) and hormones by the hypothyroidism constipation and cold
hormone (TRH) tri-iodothyronine (T3) thyroid gland intolerance
Adrenocorticotropic Corticotropic Corticotropin- Cortisol and adrenal Release of Secondary Hypocortisolaemia-
hormone (ACTH) cells releasing androgens glucocorticoids by adrenal related symptoms
hormone (CRH) the adrenal gland insufficiency (for example, weakness,
and AVP fatigue, weight loss,
hypotension and
hypoglycaemia) and
impaired well-being
Posterior lobe
Arginine Produced in the None None Water reabsorption Polyuria Diabetes insipidus
vasopressin (AVP) hypothalamus in the kidney
Oxytocin (OXT) Produced in the None None; Uterine contraction No Absence of uterine
hypothalamus positive-feedback during labour and recognizable contraction during
loop milk flow clinical picture delivery
progesterone, among others). Enlargement of the pitu hormone (LH) and follicle-stimulating hormone (FSH))
itary gland during pregnancy is well established19; the and somatotropic cells (which secrete GH) were shown
gland increases by 45% during the first trimester, reach to be decreased, whereas the numbers of thyrotropic
ing up to 120–136% of its original size near term and its cells (which secrete thyroid-stimulating hormone
highest volume during the first few weeks of the post (TSH)) and corticotropic cells (which secrete ACTH)
partum period23,24. The height of the pituitary gland on a remained unchanged during pregnancy 28.
coronal section of an MRI is a good indicator of pituitary Overall, the pituitary gland becomes vulnerable to
size. The height of the normal pituitary gland is 4–8 mm changes in blood flow during and shortly after preg
in women25, but may increase up to 10 mm during gesta nancy owing to the increased size of the gland, leading to
tion and up to 12 mm during the immediate postpartum both increased demand and compression of the vascu
period. The pituitary gland was shown to regain its nor lature of the gland. This explains why haemorrhage and
mal size, shape and volume within 6 months following resulting hypovolemia during delivery causes Sheehan
delivery 26,27 (FIG. 3). syndrome, whereas this is not the case if hypovolemia
Enlargement of the pituitary gland during preg occurs owing to any other cause.
nancy is explained by hyperplasia of the PRL-secreting
(lactotroph) cells in the anterior pituitary gland28. The Mechanisms of Sheehan syndrome
levels of maternal PRL, which is responsible for prepar The pathogenesis of Sheehan syndrome remains
ation of breast tissue for lactation, increase up to ten uncertain. Not every patient has a history of massive
fold parallel to the increased levels of oestrogen during PPH nor does every massive PPH lead to Sheehan syn
pregnancy. By 6 weeks after delivery, estradiol secretion drome. Extensive necrosis of the pituitary gland results
decreases and the basal serum PRL concentration is in a permanent lack or insufficiency of pituitary hor
usually normal, even when the mother is breastfeed mones; the mechanisms underlying the progression
ing 29. In contrast to hyperplasia of lactotroph cells, the of the disease in untreated patients have not yet been
numbers of gonadotropic cells (which secrete luteinizing fully elucidated. Importantly, the pituitary gland cannot
NATURE RE VIE WS | DISEASE PRIMERS VOLUME 2 | 2016 | 3
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
PRIMER
a b
Hypothalamic
Hypothalamus
vessels
Optic
chiasma Infundibulum
Posterior lobe
(neurohypophysis)
Primary plexus of
the hypophyseal
portal system
Superior
hypophyseal Long hypophyseal
artery portal veins
*
Anterior
lobe Artery of Short hypophyseal
(adenohypophysis) trabecula portal veins
Pars *
tuberalis Efferent
Pars hypophyseal vein to Capillary plexus of
distalis the cavernous sinus* * the infundibulum
Sphenoid sinus Secondary plexus *
of the hypophyseal
Sella turcica portal system Inferior hypophyseal artery
Figure 1 | Anatomy and vascularization of the pituitary gland. a | The pituitary gland isNaturelocated in the sphenoid
Reviews | Disease bone
Primers
(sella turcica) and is composed of the anterior lobe (adenohypophysis) and the posterior lobe (neurohypophysis).
The anterior lobe is composed of three parts: the pars distalis, which is the main component of adenohypophysis that
secretes anterior pituitary hormones; the pars intermedia, which is suppressed in humans; and the pars tuberalis, which
surrounds the infundibulum144. The optic chiasma (where the optic nerves cross) is located on top of the superior part of
the pituitary gland. b | The infundibulum, median eminence, pars tuberalis and posterior lobe are supplied by the internal
carotid artery, whereas the pars distalis receives most of its blood supply from venous drainage from the infundibulum
and the posterior lobe of the pituitary gland. The venous blood supply makes the anterior pituitary gland vulnerable
to disturbances in blood supply. Part b courtesy of M. E. Aykurt, Erciyes University, Kayseri, Turkey.
regenerate2 and Sheehan syndrome is thus a permanent massive uterine bleeding during or following delivery.
secretion disorder 30. There are numerous confounding In fact, massive PPH may be predictive for developing
factors that affect the initiation and progression of Sheehan syndrome33. PPH results from atony (a loss
the disease, which require further investigation: the of muscle tone) of the uterus, which allows the flow of
severity and spread of necrosis; the age of the patient; blood to the placenta to continue even after d elivery.
a history of previous births associated with PPH; and Many factors during both pregnancy and deliv
the number of births. Sheehan syndrome is believed ery predispose to PPH34 (such as anaemia, obesity and
to have an autoimmune component in its pathology, advanced maternal age), but PPH may occur despite
and a genetic predisposition is likely but requires the absence of these risk factors. PPH is traditionally
further investigation. defined as blood loss of 500 ml after a vaginal delivery
or 750–1,000 ml after a caesarian s ection; massive PPH
Predisposing factors. The pathogenesis of postpartum is defined as the loss of ≥2,000 ml of blood32,35. Most
pituitary necrosis is not well understood. The highly pregnant women tolerate a loss of 1,000 ml of blood
vascularized pituitary tissue is susceptible to ischae with maintenance of heart rate and blood pressure;
mia even with relatively small changes in blood flow 31. blood pressure starts to drop when the loss exceeds
Restricted pituitary blood supply following untreated 1,500 ml (REF. 36). Untreated PPH, which is defined
severe hypotension associated with PPH is the most as >500–1,000 ml of fluid loss in the 24 hours follow
common cause for the development of Sheehan syn ing delivery, might also cause Sheehan syndrome30,33.
drome32. Pituitary gland enlargement, small sella tur In addition to restricted blood supply owing to fluid
cica (the depression in the skull that houses the pituitary loss, blood flow to the pituitary gland might be compro
gland) size, vasospasm, thrombosis and coagulation mised owing to arterial vasospasm following untreated
abnormalities (either acquired, such as disseminated severe hypotension. Arterial compression as a conse
intravascular coagulation (DIC, which is an acquired quence of pituitary gland enlargement during preg
syndrome characterized by disordered blood coagula nancy in the setting of a small sella turcica size might
tion) or inherited) are among the proposed predisposing also restrict blood flow. However, Sheehan syndrome
factors for restricted pituitary blood supply 32 (FIG. 4). only very rarely develops without any obvious post
The major contributing factor in the aetiopatho partum blood loss37. Importantly, Sheehan syndrome
genesis of Sheehan syndrome is PPH. Typical obstetrical may also develop despite the rapid correction of
history of women with Sheehan syndrome includes a hypovolemic shock and DIC38.
4 | 2016 | VOLUME 2 www.nature.com/nrdp
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
PRIMER
A smaller than normal sella turcica size is a predis and MTHFR*A1298C) and plasminogen activator
posing factor for Sheehan syndrome as it may lead to inhibitor type 1 (PAI1; also known as SERPINE1),
the compression of the hypophyseal arteries against the which are well-established risk factors for thrombosis46,
wall of the sella turcica and diaphragm sellae30. The vol is increased in patients with Sheehan syndrome com
ume of the sella turcica has been shown to be smaller, pared with the general population47, suggesting that
with some exceptions, in women with Sheehan syn genetic factors involved in the coagulation cascade might
drome than in those without Sheehan syndrome5,39,40. be a predisposing factor. Other recent reports also show
The mean sella turcica volume of the patients with coagulation abnormalities in patients with Sheehan
Sheehan syndrome (mean ± SD = 340.5 ± 214 mm³) was syndrome48,49 and with pregnancy 50. In genetically pre
found to be significantly less than that of healthy women disposed women, pregnancy increases susceptibility
(mean ± SD = 602.5 ± 192 mm³), and, interestingly, the either to thrombophilia or thrombosis.
minimum sella turcica size in ~50% of the patients with
Sheehan syndrome was <308 mm³, which was the lowest Disease initiation. The initial insult in Sheehan syn
sella turcica size found in healthy women5. drome involves necrosis of the anterior lobe of the pitu
In the absence of PPH, DIC can also contribute to itary gland owing to infarction or an arrest of blood
postpartum pituitary necrosis33,41. The coagulation sys flow. Although rare, the posterior pituitary gland can
tem is continuously activated by exposure to the decidua also be affected51. Tissue infarction can be caused by
(the term for the endometrium during pregnancy) or the vasospasm due to hypotension or shock, thrombosis or
endothelium in patients with DIC42. In addition, patients arterial compression. The potential role of vasospasm
with DIC have an increased risk of developing o bstetrical is difficult to assess, but the involvement of thrombo
disorders, including massive PPH43. sis (caused by platelet aggregation or sequestration
The association of haematological abnormalities along previously damaged endothelial cells) is highly
with Sheehan syndrome might provide insight into its likely 2. Depending on the size and site of necrosis,
aetiology 44,45. The frequency of genetic mutations of this acute insult can lead to hypofunction of the pitu
coagulation factor V (F5), coagulation factor II (F2), itary gland: it can result in deficiency of hormones2,33.
methylenetetrahydrofolate reductase (MTHFR*C677T If ~50% of the normal pituitary gland remains intact,
Table 2 | Epidemiological studies assessing the prevalence of Sheehan syndrome
Study Study period Study type Findings
(study population)
Incidence or prevalence of Sheehan syndrome in the general population
Ramiandrasoa et al.4 1980–2011 (France) Retrospective study 40 patients were diagnosed with Sheehan syndrome
in the southeast of France between 1980 and 2011
Kristjansdottir et al.145 2009 (Iceland) Population-based study Sheehan syndrome was diagnosed in 5.1 individuals
per 100,000 population
Famuyiwa et al.146 1992* (Nigeria) Observational study Two new cases of Sheehan syndrome in a year
Zargar et al.6 2005* (Indian Kashmir) Population-based study Sheehan syndrome was diagnosed in 3.1% of parous
women ≥20 years of age
Diri et al.5 1960–2000 (Turkey) Large cohort of patients diagnosed with 114 patients; the prevalence of Sheehan syndrome
hypopituitarism decreased with hospital deliveries in recent times
Laway et al.95 2010* (Indian Kashmir) Observational study Incidence of one new case a month
Prevalence of Sheehan syndrome in populations with PPH
Sheehan et al.9 1938* (England) Retrospective study in women who 41% of patients with Sheehan syndrome had a
showed symptoms of hypopituitarism history of severe postpartum shock, whereas 15%
had moderate postpartum shock
Asaoka et al.10 1961–1970 (Japan) Retrospective study using questionnaires None among 392 women who responded had
of 1,010 women with a history of PPH Sheehan syndrome‡
Feinberg et al.11 1998–2002 (Chicago) Retrospective study using questionnaires None among 55 women with previous PPH who
of 109 women with previous PPH responded had Sheehan syndrome‡
Prevalence of Sheehan syndrome in a population with GH deficiency or hypopituitarism
Abs et al.3 1999* (Europe) Large multinational cohort of adult GH 3.1% of patients with adult GH deficiency had
deficiency (n = 1,034) Sheehan syndrome
Regal et al.7 1992–1999 (Spain) Population-based study involving 146,000 6% of patients with hypopituitarism had
individuals Sheehan syndrome
Elumir-Mamba et al.13 2010* (Philippines) Retrospective data 8% of patients with hypopituitarism had
Sheehan syndrome
GH, growth hormone; PPH, postpartum haemorrhage. *Publication date instead of study period. ‡Studies limited by questionnaire-based methodology and poor
response rate.
NATURE RE VIE WS | DISEASE PRIMERS VOLUME 2 | 2016 | 5
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
PRIMER
function is usually not impaired2. However, if >70% gland53 and hypothalamus54 in patients with Sheehan
of the anterior pituitary gland is affected, partial or syndrome may appear many years after the onset of
panhypopituitarism (the absence of anterior pituitary hypopituitarism; however, their presence cannot be
hormones) occurs52. excluded immediately after the initial insult. Whether
these antibodies are a cause or a consequence of
Disease progression. Sheehan syndrome is commonly Sheehan syndrome remains to be answered. However,
characterized by slow progression of pituitary dysfunc the exposure of normally sequestered antigens due to
tion, even several years after the initial insult 5 (FIG. 4). tissue necrosis could trigger autoimmunity and may
This finding suggests that there are other contrib cause delayed hypopituitarism55. In accordance with
uting factors in the pathogenesis of the disease that these findings, some subsets of peripheral lymphocyte
lead to anterior lobe cell loss in addition to the initial cells were found to be at different levels in patients with
insult. An autoimmune process might be involved in Sheehan syndrome compared with healthy controls,
the worsening of pituitary dysfunction. Some studies which is suggestive of an altered immune regulation56.
have reported that autoantibodies against the pituitary In addition, the percentage of cells that express both
CD3 and DR1, which correlates with the duration of
illness in patients with Sheehan syndrome, is sug
Hippocampus Amygdala
gestive of an ongoing inflammation accompany
ing the slow p rogression of pituitary dysfunction in
Sheehan syndrome56.
Hypothalamus
Paraventricular Characteristics of pituitary necrosis. In the first
nucleus
reports, acute ischaemic infarction led to extensive
acute necrosis of the pituitary gland, which involved
~90% of the anterior lobe. In the necrotized tissue,
CRH adenohypophysis cells were replaced by necrotic debris,
coagulated blood, inflammatory cells and ghost cells.
Immunohistochemical staining showed some cells con
taining adenophyseal hormones on the edge of the
necrotic areas, but hormones were completely absent
in the centre of the necrotic area1,4. In the chronic phase
Pituitary of the syndrome, a fibrous scar is formed. In addition,
gland the fibrous scar leads to a time-dependent atrophic
change of the pituitary gland and results in an empty
sella turcica, which can be radiologically detected33.
Lactotroph and somatotropic cells in the pituitary
gland are usually completely lost, whereas gonadotropic
ACTH and corticotropic cell functions can be preserved57.
This pattern of cell loss is explained by the location
of the cells in the pituitary gland: corticotropic and
Adrenal thyrotropic cells are located in the median wedge
gland and gonadotropic cells are scattered throughout the
pituitary, whereas somatotropic and lactotroph cells are
located in the lateral wings, which receive blood supply
Glucocorticoids only from the portal circulation32,57.
Regulation of brain and peripheral function Diagnosis, screening and prevention
(stress response)
Clinical manifestations
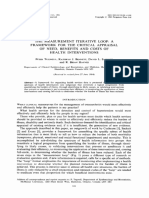
Figure 2 | Regulation of the
Naturehypothalamic–pituitary–
Reviews | Disease Primers
Sheehan syndrome can be diagnosed by clinical symp
adrenal axis. Glucocorticoid secretion is regulated by toms of hypopituitarism32 (BOX 1). According to the
adrenocorticotropic hormone (ACTH) secretion from severity of damage to the pituitary gland, patients can
the pituitary gland, which is stimulated by corticotropin- present at the hospital with symptoms ranging from
releasing hormone (CRH) secretion from the isolated hypopituitarism to panhypopituitarism5,52,58–64
hypothalamus. CRH is suggested to be regulated from (TABLE 3). GH and PRL are the most commonly affected
the upper centres of the brain. Glucocorticoids have hormones. PRL deficiency leads to postpartum failure
negative-feedback effects on the upper centres of the of lactation, and gonadotropin (FSH and LH) deficiency
brain, the hypothalamus and the pituitary gland. ACTH not
leads to amenorrhoea. Profound pituitary gland necro
only stimulates glucocorticoids but also stimulates adrenal
androgens and mineralocorticoids. However, given that sis can also lead to TSH and, less frequently, ACTH
aldosterone secretion is primarily regulated by the renin– deficiencies, which might result in symptoms such as
angiotensin system, ACTH deficiency does not result in weight gain, constipation, cold intolerance followed
mineralocorticoid deficiency, but leads to glucocorticoid by hypocortisolaemia-related symptoms (for exam
deficiency and adrenal androgen deficiency in women. ple, weakness, fatigue, weight loss, hypotension and
6 | 2016 | VOLUME 2 www.nature.com/nrdp
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
PRIMER
a b Physical examination of patients with chronic
Sheehan syndrome frequently shows sparse axillary and
pubic hair, breast atrophy, increased wrinkling around
the mouth and eyes, hypopigmentation, dry skin,
slowing of reflexes, bradycardia or sometimes coma59.
Patients might present with adrenal crisis due to cortisol
deficiency or myxoedema coma, a state of decompen
sated hypothyroidism triggered by infection, surgery or
trauma32. Hyponatraemia (an electrolyte disorder that
can lead to malaise, nausea, vomiting, cognitive changes
and even death69) is the most commonly observed
electrolyte abnormality in patients with Sheehan syn
Figure 3 | Enlargement of the pituitary gland during pregnancy.
Nature Reviews | Disease
Coronal Primers
MRI scan drome, and the rate of hyponatraemia has been reported
showing the pituitary gland (arrows) of a pregnant women in the third trimester (part a)
to be between 21% and 59%60,63. Sheehan syndrome
and 6 months after delivery (part b).
should be kept in mind in patients who are presented
to the emergency department with hyponatraemia63,70.
hypoglycaemia). Although rare, the posterior lobe can Clinical symptoms related to hypoglycaemia can also be
also be affected, which can lead to diabetes insipidus2,65. seen in Sheehan syndrome, especially patients who are
Sheehan syndrome can also result in severe clinical in a coma52. Sheehan syndrome was the second-most
outcomes (such as adrenal crisis, circulatory collapse, frequent factor of hypoglycaemia-associated coma, after
myxoedema coma and hyponatraemia) and can lead to diabetes mellitus71. Although polyuria and polydipsia
death if not properly treated. Mortality rate is increased (excessive thirst) due to diabetes insipidus are rare clin
by 1.2–2.7 times in these patients with Sheehan ical symptoms (4.5–5%) of Sheehan syndrome5,72, the
syndrome compared with the general population66. osmotic threshold that is required to perceive thirst was
Some patients are diagnosed with symptoms of high in patients with Sheehan syndrome and partial dia
acute hypopituitarism immediately after giving birth67. betes insipidus; partial diabetes insipidus without poly
Sheehan syndrome can result in death if it is not diag uria was observed in one-third of patients with Sheehan
nosed and treated in the acute stage. Clinical presen syndrome51. In addition, Sheehan syndrome increases
tation of acute Sheehan syndrome includes headache, the risk of osteoporosis and osteopenia. The Z score
visual disturbances, loss of consciousness, failure of (a measure of bone density) was ≤2 in 40% of the
lactation and features of acute adrenal insufficiency, patients (a Z score of >–2.0 is considered normal)73–75.
such as hypotension, hypoglycaemia, extreme fatigue, The aetiology is not yet elucidated, but multiple pitu
nausea, vomiting and hyponatraemia37. The syndrome itary hormone deficiencies, particularly secondary
should be investigated in patients who present with hypogonadism, and delayed diagnosis are claimed to
postpartum hypotension and hypoglycaemia60,67. have a role74,76.
However, most patients present with nonspecific
symptoms years after delivery 5,58,64. This delay between Laboratory findings
submission for diagnosis and preceding pituitary insult Endocrine abnormalities. Pituitary hormone insuf
is common and variably reported to be 7–19 years4–6,68. ficiencies vary depending on the hypophyseal cells
Symptoms can emerge late because of incomplete affected and on the studies 5,52,58,60,61,63,64,77 (TABLE 4) .
hypophyseal damage immediately after giving birth A probable reason for the discrepancy between studies
with a slow progression of damage over time64. In addi is the different time elapsed from the initial insult to
tion, other stress factors trigger the presentation of the diagnosis. In Sheehan syndrome, stimulation tests
Sheehan syndrome. For example, latent ACTH defi are necessary to determine if there is a hormone defi
ciency might become obvious during an infection or ciency, especially when hormone levels are borderline.
surgery. Nonspecific clinical findings are more evident This is particularly true when evaluating cortisol or
in patients who are diagnosed in the chronic stage. In a GH deficiencies.
study that included 114 patients with chronic Sheehan In most patients with Sheehan syndrome, baseline
syndrome, nonspecific symptoms were seen in >50% of (measured in the morning at basal conditions) FSH and
patients5. The high prevalence of nonspecific symptoms LH levels are not increased to postmenopausal levels
is considered to be one of the possible reasons for late (representative for physiological ovarian failure) and
diagnosis. History of failure of lactation and absence of LH levels do not increase following stimulation with
resumption of normal menstrual cycles after delivery gonadotropin-releasing hormone, thus can be used as
(especially when delivery was associated with PPH), a diagnostic test in rare situations58,78,79. To show corti
symptoms of secondary hypothyroidism and adrenal sol and GH deficiencies, an insulin tolerance test and
insufficiency, involution of secondary sexual character a glucagon stimulation test can be used80,81. Correct
istics due to secondary hypogonadism and subtle release of cortisol can also be assessed with an ACTH
features of GH deficiency are seen and should raise stimulation test. However, when this test is carried out
suspicion for Sheehan syndrome57. Absence of these soon after the initial insult, adequate response might
symptoms does not exclude Sheehan syndrome and be observed because the adrenal glands might not yet
10% of cases may be asymptomatic in the long term32,60. have atrophied.
NATURE RE VIE WS | DISEASE PRIMERS VOLUME 2 | 2016 | 7
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
PRIMER
Patients with central hypothyroidism can have Electrolyte abnormalities. Patients also often exhibit
normal, decreased or slightly increased levels of TSH, abnormalities in blood electrolyte levels. Hyponatraemia
whereas tetraiodothyronine (T4) levels are decreased. is the most common, but hypokalaemia, hypomagne
Enhanced sialylation of TSH might explain the increased saemia, hypocalcaemia and hypophosphataemia were
levels as this reduces metabolic clearance but also also observed in patients with Sheehan syndrome63.
decreases biological activity. Administration of thyro The aetiology of hyponatraemia is not known, but
tropin-releasing hormone fails to increase the levels of might involve increased antidiuretic hormone (ADH)
TSH or PRL in patients with Sheehan syndrome82. The release as a consequence of reduced blood pressure and
circadian rhythm of TSH was shown to be disrupted and cardiac output owing to glucocorticoid deficiency 85.
there is an increase in total TSH release in patients with In addition, cortisol deficiency causes an increase in
Sheehan syndrome83,84. the levels of corticotropin-releasing hormone (CRH),
which in turn stimulates ADH secretion86. It was shown
that cortisol and thyroid hormone deficiencies lead to
Pregnancy decreased free water clearance independent from ADH.
In addition, it has been demonstrated that GH, PRL and
thyroid hormone deficiencies were related with hypona
traemia63. Hyponatraemia associated with diabetes
insipidus can rarely be seen72.
Small sella
turcica size Haematological abnormalities. Many patients with
Normal pituitary
gland Pituitary gland enlargement Sheehan syndrome also show anaemia (45–87%),
thrombocytopenia (63–105%), pancytopenia (15%)
and coagulation disorders 44,58,87. Coagulation dis
Compression of the vascular
structure of the pituitary gland
orders were presented as a case report in literature88.
Genetic factors
Although anaemia generally occurs as normochro
mic normocytic, it can be hypochromic microcytic
Ischaemia or rarely macrocytic58,87. Cortisol and thyroid hor
mone deficiencies are suggested to be involved in the
Coagulation abnormalities Sequestered development of anaemia by decreasing the synthesis of
(congenital and/or acquired) antigens erythropoietin or by decreasing the biological effects
(autoimmunity)
of endogenous erythropoietin89. Bone marrow hypo
Severe postpartum
haemorrhage plasia and pancytopenia can occur; both are reversed
after the replacement of deficient hormones 90,91.
Coagulation disorders can be diagnosed by measuring
adaptive factor VIII and von Willebrand factor defi
Anti-pituitary ciencies, decreased prothrombin time and activated
GH deficiency Postpartum necrosis
of the pituitary gland
antibodies prot hrombin time, and an increase in the levels of
fibrinogen and d‑dimer 48,88.
Muscle, bone
and adipose
tissue FSH and LH Radiological findings
PRL deficiency deficiency Pituitary MRI is the preferred radiological imag
ACTH
ing procedure used for differential diagnosis, but CT
TSH deficiency
deficiency Ovary may also be helpful in the diagnosis of Sheehan syn
drome32,92. MRI findings vary with the stage of the
disease. Although evidence is limited, some studies
describe the acute structural changes as an enlarged
non-haemorrhagic pituitary gland with central infarc
Mammary gland Thyroid gland Adrenal gland tion30,38,67,93,94 (FIG. 5a,b). Within several weeks, the gland
shrinks to the confines of the sella turcica, followed
Hypopituitarism Worsening of hypopituitarism by further progressive atrophy over several months
or years with a final image of an empty sella turcica,
Figure 4 | Pathogenesis of Sheehan syndrome. The pituitary gland is physiologically
Nature Reviews | Disease Primers which represents complete atrophy of the pituitary
enlarged during pregnancy as a result of massive hyperplasia of the lactotroph cells, gland3,4 (FIG. 5c,d). At diagnosis, patients with Sheehan
which are stimulated by oestrogens produced by the placenta. The vascular structure of syndrome can have partially (25–30%) or completely
the pituitary gland might become compressed because of pituitary gland enlargement (70–75%) empty sella turcica on imaging studies4,5,59,61,95.
and/or small sella turcica size. Vasospasm (caused by massive postpartum
Only a few patients have been reported to have struc
haemorrhage) and/or thrombosis (associated with pregnancy, genetic predisposition
or disorders of blood coagulation) might result in ischaemia. Autoimmunity might turally normal pituitary gland4,59,61. Thus, an empty
worsen hypopituitarism over the years. Solid arrows indicate the well-known sella turcica can be considered as a characteristic for
mechanisms; dashed arrows indicated mechanisms that have not yet been proven. Sheehan syndrome diagnosis30. The remnant pituitary
ACTH, adrenocorticotropic hormone; FSH, follicle-stimulating hormone; GH, growth tissues may be necrotic and thus non-functioning or
hormone; LH, luteinizing hormone; PRL, prolactin; TSH, thyroid-stimulating hormone. intact and thus functioning 96. Because of this, there is
8 | 2016 | VOLUME 2 www.nature.com/nrdp
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
PRIMER
Box 1 | Diagnostic criteria for Sheehan syndrome can resemble Sheehan syndrome; sudden onset of a
severe headache, loss of vision and unconsciousness
Criteria proposed by Kelestimur et al.* may be present in both93 and MRI scans can be simi
• Typical obstetrical history of severe postpartum lar. However, enlargement of the sella turcica and ero
haemorrhage sion of the sellar floor, lateral deviation of the pituitary
• Severe hypotension or shock, for which blood stalk, contrast enhancement of periphery (because of
transfusion or fluid replacement is necessary the presence of healthy pituitary tissue) and the per
• Failure of postpartum lactation sistent presence of a mass near the pituitary gland on
• Failure to resume regular menses after delivery repeated imaging several months apart, point towards
• Varying degree of anterior pituitary insufficiency that apoplexy associated with pituitary adenoma rather than
ranges from partial to complete hypopituitarism Sheehan syndrome. These features, coupled to a history
• A partially or completely empty sella turcica on a CT of antecedent delivery complicated by PPH and hypo
or MRI scan volemic shock in the case of Sheehan syndrome, help
Criteria proposed by Diri et al.‡ in the differential diagnosis93.
Essential criteria for the diagnosis: Lymphocytic hypophysitis may be present in the
• Typical history of severe postpartum uterine bleeding,
immediate postpartum period with hypopituitarism
particularly at last delivery and pituitary enlargement 97,98. Although most auto
• At least one pituitary hormone deficiency
immune diseases go into remission during pregnancy,
lymphocytic hypophysitis manifests at this time owing
• A partially or completely empty sella turcica on a CT
or MRI scan in the chronic phase
to the release of pituitary antigens and relatively more
Criteria that are not essential, but, if present, are strongly vascular supply to the pituitary gland from systemic
suggestive of the diagnosis: rather than portal circulation32. Differentiating lym
• Severe hypotension or shock at index delivery phocytic hypophysitis from Sheehan syndrome can be
difficult as both present with a headache, hypopituitar
• Postpartum amenorrhoea
ism and pituitary mass in the immediate postpartum
• Failure of postpartum lactation
period and an empty sella turcica later on99–101. Despite
*See REF. 32. ‡See REF. 5. these similarities, some features distinguish the two
conditions30,102 (TABLE 5).
no correlation between the degree of postpartum pitu Prevention
itary necrosis and the severity of clinical expression and To prevent Sheehan syndrome, minimizing the risk and
between the severity of h ypopituitarism and the degree aggressive management of PPH is paramount. PPH is
of empty sella turcica5,92. the leading cause of maternal mortality, e specially
in low-income countries. A multi-country survey of
Differential diagnosis low-income countries that included 275,000 deliveries
Acute presentation of Sheehan syndrome immedi showed that 1.2% were associated with PPH. Of the
ately after an eventful delivery, although not that women who had PPH, 18% had adverse maternal out
common, makes the diagnosis of Sheehan syndrome comes and 3% died103. Although in western countries
more straightforward. Diagnosis of Sheehan syndrome mortality due to PPH is decreasing, the actual inci
years after the initial insult is more challenging and dence of PPH is increasing possibly because of more
conditions such as pituitary tumours and lympho interventions (such as the induction of labour and
cytic hypophysitis (an autoimmune disorder affecting caesarian section)104.
the pituitary gland) need to be considered. Pituitary Three broad strategies improve the outcome in
tumours are the most common cause of hypopitui PPH: prevention, treatment and effective management
tarism. Clinical presentation of an apoplexy (acute of PPH. The WHO has published guidelines and key
bleeding inside the pituitary tumour) associated with interventions for the prevention of PPH, which include
a pituitary adenoma around the peripartum period a combination of interventions, such as cord clamping
Table 3 | Clinical characteristics of patients with Sheehan syndrome
Study n Postpartum Nonspecific Amenorrhoea Failure to Loss of Hypoglycaemia Cognitive Diabetes
haemorrhage symptoms (%) lactate pubic and (%) changes insipidus
(%) (%) (%) axillary hair (%) (%)
(%)
Diri et al.5 114 NR 52 85 48 10 8 NR 4
Du et al. 59
97 99 NR 82 74 86 26 8 1
Lim et al.63 78 100 NR 100 94 NR 4 21 0
Gei-Guardia et al.60 60 82 88 73 67 93 15 17 0
Dokmetas et al. 58
20 100 80 80 70 100 5 20 0
NR, not reported.
NATURE RE VIE WS | DISEASE PRIMERS VOLUME 2 | 2016 | 9
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
PRIMER
Table 4 | Anterior pituitary hormone deficiency in Sheehan syndrome
Study n GH deficiency PRL deficiency FSH and LH TSH deficiency ACTH
(%) (%) deficiency (%) (%) deficiency (%)
Dokmetas et al.58 20 100 100 100 90 55
Diri et al.
5
114 100 71 100 90 71
Kelestimur et al.62 91 100* NR 80 86 87
Lim et al.63 78 100 95 9 90 91
Sert et al. 64
28 100 100 100 100 100
Ozbey et al.52 40 93 100 43 76 93
Gokalp et al. 61
124 100 79 100 73 76‡
Hormone levels at the time of diagnosis. ACTH, adrenocorticotropic hormone; FSH, follicle-stimulating hormone; GH, growth
hormone; LH, luteinizing hormone; NR, not reported; PRL, prolactin; TSH, thyroid-stimulating hormone. *Only patients with GH
deficiency were taken into that study. ‡According to basal cortisol levels.
and cutting (within 1–3 minutes); controlled cord trac Glucocorticoid replacement
tion (measures to reduce the risk of retained placenta); In acute-onset patients with high clinical suspicion of
and the use of an uterotonic agent (such as oxytocin, adrenal insufficiency, glucocorticoid treatment should be
which causes rhythmic contractions of the uterus)34. started immediately after taking a serum sample for the
All obstetrical care hospitals must have institutional measurement of cortisol and ACTH levels78,108. As adre
protocols for the management of women who develop nal insufficiency in Sheehan syndrome is due to ACTH
PPH of >1,000 ml. These protocols should combine deficiency, mineralocorticoid replacement is not required.
the most recent recommendations, also taking note The dose of glucocorticoid agent should be titrated
of experiences of the other countries. Staff should be according to the clinical findings of the patient instead
adequately trained and simulated PPH drills should of laboratory results. Lifelong glucocorticoid treatment is
be included in the training curriculum105. However, in necessary in the case of secondary adrenal insufficiency.
developing countries, there is a shortage of medical staff. Adverse effects of glucocorticoids, such as osteopor
Whereas these countries account for 25% of the global osis, hyperglycaemia and weight gain, should be moni
burden of disease, they have only 1.3% of the world’s tored5. Although some experts favour hydrocortisone and
skilled care providers, including doctors, nurses and cortisone acetate for replacement therapy in hypocor
midwives106. Anaemia during pregnancy, which is again tisolism, outcome data to support the use of one gluco
more common in the developing world, is an important corticoid over another do not exist. In addition, even three
preventable risk factor and timely administration of oral daily doses of hydrocortisone, which are often suggested
or parental iron can help in a long way in the prevention for glucocorticoid replacement, cannot approximate the
of PPH35. Moreover, uterotonic agents have an important circadian rhythm of endogenous cortisol production109.
role in the prevention of PPH. Oxytocin is recommended To avoid adverse effects, more physiological replacement
but its sensitivity to heat, the need for refrigeration and policies are preferred. Nowadays, dual-release hydrocor
the requirement for a trained person for its administra tisone (a tablet with an immediate-release coating sur
tion limit its use in resource-poor nations. Availability rounding an extended-release core) given once daily 110
of aerosol or topical preparations will in the future or a continuous subcutaneous hydrocortisone infusion
overcome these limitations107. Finally, more studies are may be used111. These modalities have a better physiolog
needed for widespread use of misoprostol as an utero ical diurnal rhythm associated with weight loss, decrease
tonic agent, especially in developing countries where in blood pressure, improved glucose metabolism and
PPH is common. As opposed to oxytocin, misoprostol enhanced health-related quality of life (QOL) compared
does not need a skilled person to administer and can be with the classic 2–3 daily glucocorticoid administration112.
given by the patient herself and is a preferred drug in Patients should be informed about the risk of adrenal
resource-poor settings. Once PPH has occurred, a close crisis if they do not increase their daily dose in some situ
follow-up is necessary for the detection and treatment ations that increase the need for cortisol, such as infec
of Sheehan syndrome. tion, surgery and trauma112. When hypothyroidism and
hypoadrenalism occur together, thyroid hormone therapy
Management should follow glucocorticoid replacement to avoid adrenal
General principles in the treatment of hypopituitar crisis112. Hydrocortisone dose may need to be increased
ism are valid in the treatment of patients with Sheehan after GH treatment in patients with GH deficiency 113.
syndrome. Deficient hormones should be replaced
appropriately. Hormone replacement therapy does not Thyroid hormone replacement
improve pituitary function and does not prevent the pro Regarding thyroid hormone replacement, titration of
gression of pituitary necrosis. Pituitary functions need levothyroxine dose depends on free T4 and free tri-
to be assessed at regular intervals as hypopituitarism can iodothyronine (T3) levels rather than on TSH levels, which
be progressive5. may be normal, decreased or increased114. In elderly
10 | 2016 | VOLUME 2 www.nature.com/nrdp
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
PRIMER
patients and those with coronary artery disease, levo tumours. GH replacement therapy should be started in
thyroxine should be given at low doses and dose titra low doses, which should be increased gradually accord
tions should be carried out slowly. Transformation of T4 ing to the evaluation of clinic response and IGF‑1 levels
to T3 increases in patients who are administered GH and that are assessed once every 4–8 weeks120. A prospective
these conditions can convert the masked hypothyroid study showed that 18 months of GH replacement ther
ism into an overt state or increase levothyroxine require apy decreased the levels of total cholesterol and LDL-
ment in those who are already on replacement therapy 115. cholesterol and increased the levels of HDL-cholesterol,
Different levothyroxine preparations exist, such as tablets, while waist circumference and waist-to-hip ratio were
oral soft gel capsules and liquid formulations. decreased significantly 121. GH replacement therapy for
6 months improved cognitive function (assessed by P300
Oestrogen and progesterone replacement auditory potentials) in patients with Sheehan syndrome
Although oestrogen and progesterone replacement with severe GH deficiency 49,122. GH replacement ther
therapy in hypogonadal postmenopausal women with apy for 1 year improved QOL, body composition and
Sheehan syndrome is controversial, replacement ther the lipid profile in a study that included 91 patients
apy is usually recommended in premenopausal women from 19 countries62, whereas another study showed
with Sheehan syndrome, unless there is a contra that 6 months of GH replacement therapy improves
indication (such as deep vein thrombosis, pulmonary the sebum content on the forehead, which is signifi
embolism, severe cirrhosis, active viral hepatitis and cantly decreased in GH-deficient patients with Sheehan
uncontrolled severe hypertension). In young women, syndrome123. In addition, GH replacement therapy
a high dose of estrogen is preferred, whereas lower doses in severely GH-deficient patients, most of whom had
are used when menopause has started; treatment is dis Sheehan syndrome, improves sympathetic tone without
continued in women ≥50 years of age116. Oral estrogen an obvious arrhythmogenic effect 49. Conversely, some
suppresses hepatic insulin-like growth factor 1 (IGF‑1) parameters were not improved upon GH replacement
release in response to GH117, which can be prevented by therapy. In that study, Tanriverdi et al.49 showed that
using transdermal estrogens118. 6 and 12 months of GH replacement therapy increased
sympathetic activity and normalized sympathovagal
GH replacement balance. GH replacement therapy for 6 months failed
Opinions about efficacy and the routine use of GH to improve the abnormal sleep patterns in patients with
treatment in patients with Sheehan syndrome are Sheehan syndrome, who show more non-rapid eye
divided because of the risk–benefit ratio and cost- movement (NREM) sleep, less REM sleep and sleep effi
effectiveness119. GH deficiency is more severe in patients ciency than healthy controls124. No data are available for
with Sheehan syndrome than in patients with pituitary longer duration of GH replacement therapy on abnor
mal sleep parameters124. GH replacement therapy did not
have any effects on bone mineral density 121.
a b
AVP replacement
Diabetes insipidus can develop as a consequence of
damage to the posterior gland, leading to impaired AVP
secretion. In addition, diabetes insipidus can develop
in patients with Sheehan syndrome who are treated
with glucocorticoids, which increase water diuresis51.
Symptoms of diabetes insipidus may be masked by
concomitant ACTH deficiency. Glucocorticoid therapy
has been shown to suppress AVP secretion in patients
with ACTH deficiency 125. Polyuria and polydipsia
c d should be assessed following glucocorticoid treatment
in patients with Sheehan syndrome. Desmopressin,
which is a modified form of AVP, can be administered
orally, nasally and parenterally to treat diabetes insipi
dus, usually around bedtime. If needed, morning and
afternoon doses can be added. Antidiuretic effects
of desmopressin commence between 6 and 12 hours
when administered via the nasal route. If switching to
oral from intranasal, oral desmopressin should start at
least 12 hours after the last intranasal dose. However,
Figure 5 | Radiological characteristics of Sheehan syndrome. a,b | Acute phase.
Nature Reviews | Disease Primers the duration of effect is less when administered by the
Post-contrast MRI scans of the pituitary gland in a patient 2 months after postpartum
haemorrhage showing gland atrophy and non-haemorrhagic central infarction oral route. Care should be taken when treating uncon
characterized by central hypointensity on T1‑weighted images (part a) and scious patients. Serum sodium level and fluid volume
hyperintensity on T2‑weighted images (part b). c,d | Chronic phase. Coronal (part c) and should be evaluated and the desmopressin dose should
sagittal (part d) T1‑weighted MRI scans showing an empty sella turcica. Sella turcica size be adjusted accordingly. In addition, as the risk of
is normal in all images. Arrows indicate the pituitary gland. severe hypernatraemia is high in patients with diabetes
NATURE RE VIE WS | DISEASE PRIMERS VOLUME 2 | 2016 | 11
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
PRIMER
Table 5 | Differentiating features between lymphocytic hypophysitis and Sheehan syndrome
Feature Sheehan syndrome Lymphocytic hypophysitis
Epidemiology Common in developing countries Common in developed countries
Patients Women only Men, women and children
Association with other No Yes
autoimmune disorders
Parity Follows pregnancy Can also occur without pregnancy
Postpartum haemorrhage Common Not required
Common tropic hormone Lactotroph, thyrotropic and somatotropic Corticotropic and thyrotropic hormones
deficiencies hormones
Common hormones Corticotropic and gonadotropic hormones Somatotropic and gonadotropic hormones
preserved
Hyperprolactinaemia No Yes
Diabetes insipidus Very rare Yes
Pituitary MRI Empty sella turcica Pituitary mass with contrast enhancement;
later, an empty sella turcica
insipidus, who are adipsic (the absence of thirst), daily patients, treatment is continued until placental variant
fluid intake, regular desmopressin use, body weight and GH that is secreted from the placenta from 12 weeks of
serum sodium levels should be monitored116. pregnancy is synthetized, whereafter treatment is gradu
ally discontinued by administering decreased doses
Pregnancy and lactation until 20 weeks of pregnancy 116. Generally, placental
Ovulation induction can be used in women who want variant GH can comprise enough IGF‑1 after 20 weeks
to become pregnant, although some patients can have of pregnancy 135. It is not yet clear which patients with
spontaneous pregnancies126. When pregnant, regular Sheehan syndrome should use GH replacement during
follow‑up to adjust glucocorticoid doses is needed. pregnancy, but GH replacement seems to have no major
Physiological gestation is associated with increased adverse effects and no negative influences on maternal
maternal HPA axis activity despite the fact that cortico and fetal outcome.
tropic cell numbers remain the same. Both total and free Ovulation induction is necessary in patients with
cortisol levels have been shown to increase by 11 weeks Sheehan syndrome with gonadotropin deficiency, so
of gestation; however, this does not cause feedback oestrogen replacement is discontinued. When preg
inhibition as the set point for ACTH secretion is also nancy occurs, sex steroids are secreted from the placenta,
altered127,128. Besides maternal HPA axis overactivity, which eliminates the need for exogenous replacement.
the placenta also contributes to the production of both In normal pregnancy, the levels of maternal serum
ACTH and CRH129. gonadotropins decrease during the early weeks and
Levothyroxine doses also need adjustment. The bio become undetectable in the second trimester owing to
chemical similarity of TSH and hCG results in increased increased levels of sex steroids (such as 17 β‑estradiol
thyroid hormone synthesis, which in turn inhibits and progesterone) and regulatory peptides (such as
maternal TSH secretion from the pituitary gland dur inhibin)136. There are no data about the replacement of
ing the first trimester of normal pregnancy 130. In addi PRL during gestation and the postpartum period for
tion, there is an increased requirement for T4 during lactation in PRL-deficient patients.
pregnancy not only due to increased serum thyroxine-
binding globulin but also due to the placental degrad Quality of life
ation of T4, the transfer of T4 from mother to fetus Most patients with Sheehan syndrome have nonspecific
and increased maternal clearance of T4 (REF. 131). The symptoms, such as weakness, cold intolerance, anae
requirement for l‑thyroxine increases by about 30% mia and feeling unwell, which affect QOL, especially
during gestation132. because of long diagnostic delay 32. These patients can
Maternal GH secretion is decreased during normal remain undiagnosed or misdiagnosed for a long time
gestation. Instead, the placenta starts to produce placen and receive inappropriate treatments. Furthermore,
tal variant GH, which is detectable in the circulation hormone deficiencies progress and worsen over the
by 5 weeks of pregnancy, and the levels progressively years, which suggests a progressive deterioration of this
increase throughout gestation and peak at 35–37 weeks. chronic condition5. Although there are no prospective
Placental variant GH is secreted continuously; placen studies specifically investigating morbidity and mortality
tal variant GH binds to the hepatic GH receptor with in Sheehan syndrome, undiagnosed Sheehan syndrome
similar affinity to pituitary GH, inhibiting its secretion results in increased mortality and morbidity. Increased
by stimulating IGF‑1 production133,134. GH treatment is awareness of this condition will result in earlier diag
usually discontinued after confirmation of pregnancy as nosis and hence better QOL, and lower morbidity
its use is not licenced during gestation; however, in some and mortality.
12 | 2016 | VOLUME 2 www.nature.com/nrdp
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
PRIMER
Treatment improves QOL in patients with Sheehan cell transplantation (such as lactotroph and gonado
syndrome. The effects of GH replacement therapy in tropic cells, among others) therapy 141. In a transgenic
adults with hypopituitarism with non‑Sheehan syn mouse model, it was shown that the pituitary gland is
drome has been well documented and include improve competent to repair tissue after cell loss by diphtheria
ment in QOL, well-being, change of body composition toxin-induced injury and that somatotropic cells were
and cognitive function137, which have also been shown in considerably regenerated during the months after injury,
patients with Sheehan syndrome121,122. Although supra suggesting recovery of somatotropic cells from stem or
physiological glucocorticoid exposure is deleterious on progenitor cells142. It seems that the regenerative cap
QOL, increasing glucocorticoid doses in patients who acity of the pituitary gland relies on stem cell-associated
complain of impaired QOL, which may or may not be pathway activaton140. Pituitary stem cell transplantation
related to adrenal axis deficiency, are common prac has experimentally been investigated in other causes
tice138,139. Thus, physicians need to consider and evaluate of pituitary insufficiency; however, it may also have a
the causes of impaired QOL during patient follow-up, potential use in Sheehan syndrome. Human embryonic
such as insufficient glucocorticoid and thyroid hormone stem cell-derived pituitary tissues provide a platform
replacement and GH deficiency. for therapeutic application and disease modelling 141.
After transplantation into hypopituitary mice (hypo
Outlook physectomized severe combined immunodeficient mice),
Because of its scarcity in the western society, Sheehan syn in vitro-generated corticotropic cells can secrete ACTH
drome has become a neglected disorder and is not suffi in response to CRH141. Sheehan and Davis143 published a
ciently included in medical education. Owing to recent very comprehensive book dedicated to Sheehan syndrome
increases in migration to developed countries, physicians in 1982, in which they suggested that this condition
need to suspect the disease in women who have delivered serves as an excellent model for the study of pure insuf
in their countries of origin, especially if those are devel ficiency of the anterior lobe. In fact, Sheehan syndrome
oping countries. Although the underlying mechanisms is an exceptional pituitary disorder that is characterized
responsible for the development of postpartum pituitary by a long-term severe hypopituitarism and, hence, it is a
necrosis have not been completely defined, recent studies perfect model to see the effects of replacement treatment
have provided new insight into the pathogenesis, such as on morbidity, mortality and QOL in women. An animal
pituitary autoimmunity and coagulation abnormalities. model that mimics Sheehan syndrome, which does not
Insight into the pathophysiology of postpartum pituitary currently exist, would be beneficial not only to under
necrosis may provide new options in the treatment of stand the underlying mechanisms of Sheehan syndrome
permanent pituitary failure associated with other causes, but may also be useful to understand the pathophysiology
such as treatment with pituitary stem cell140 and target of the other types of hypopituitarism.
1. Sheehan, H. L. Postpartum necrosis of the anterior 11. Feinberg, E. C., Molitch, M. E., Endres, L. K. 21. Young, W. F. Jr. in The Netter Collection of Medical
pituitary. J. Pathol. Bact. 45, 189–214 (1937). & Peaceman, A. M. The incidence of Sheehan’s Illustrations: The Endocrine System
This is the first description of Sheehan syndrome. syndrome after obstetric hemorrhage. Fertil. Steril. (ed. Young, W. F. Jr) 1–7 (Elsevier, 2011).
2. Kovacs, K. Sheehan syndrome. Lancet 361, 520–522 84, 975–979 (2005). 22. Higuchi, T. & Okere, C. O. Role of the supraoptic
(2003). 12. Roy, T. K., Kulkarni, S., Pandey, A., Gupta, K. nucleus in regulation of parturition and milk ejection
This study discusses two cases of Sheehan & Nangia, P. International Institute for Population revisited. Microsc. Res. Tech. 56, 113–121 (2002).
syndrome and provides a brief review and history Sciences (IIPS) and ORC Macro National Family 23. Dinc, H., Esen, F., Demirci, A., Sari, A.
of the disease. Health Survey (NHFS‑2) 1998–99 (IIPS, 2000). & Resit Gumele, H. Pituitary dimensions and volume
3. Abs, R. et al. GH replacement in 1034 growth 13. Elumir‑Mamba, L. A. S., Andag‑Silva, A. A., measurements in pregnancy and post partum.
hormone deficient hypopituitary adults: demographic Fonte, J. S. & Mercado‑Asis, L. B. Clinical profile and MR assessment. Acta Radiol. 39, 64–69 (1998).
and clinical characteristics, dosing and safety. etiology of hypopituitarism at the Univesity of Santa This is an important paper that shows the changes
Clin. Endocrinol. (Oxf.) 50, 703–713 (1999). Thomas Hospital. Philippine J. Intern. Med. 48, in pituitary dimensions on MRI during pregnancy
4. Ramiandrasoa, C. et al. Delayed diagnosis of 23–27 (2010). and the postpartum period.
Sheehan’s syndrome in a developed country: 14. Tanriverdi, F. et al. Etiology of hypopituitarism 24. Gonzalez, J. G. et al. Pituitary gland growth during
a retrospective cohort study. Eur. J. Endocrinol. 169, in tertiary care institutions in Turkish population: normal pregnancy: an in vivo study using magnetic
431–438 (2013). analysis of 773 patients from Pituitary Study resonance imaging. Am. J. Med. 85, 217–220 (1988).
5. Diri, H. et al. Extensive investigation of 114 patients Group database. Endocrine 47, 198–205 (2014). 25. Wolpert, S. M., Molitch, M. E., Goldman, J. A.
with Sheehan’s syndrome: a continuing disorder. 15. Bergland, R. M. & Page, R. B. Can the pituitary & Wood, J. B. Size, shape, and appearance of the
Eur. J. Endocrinol. 171, 311–318 (2014). secrete directly to the brain? (Affirmative normal female pituitary gland. AJR Am. J. Roentgenol.
This study provides detailed features of a large anatomical evidence). Endocrinology 102, 143, 377–381 (1984).
group of patients with Sheehan syndrome. 1325–1338 (1978). 26. Diver, M. J. et al. An unusual form of big, big (macro)
6. Zargar, A. H. et al. Epidemiologic aspects of 16. Leclercq, T. A. & Grisoli, F. Arterial blood supply prolactin in a pregnant patient. Clin. Chem. 47,
postpartum pituitary hypofunction (Sheehan’s of the normal human pituitary gland. An anatomical 346–348 (2001).
syndrome). Fertil. Steril. 84, 523–528 (2005). study. J. Neurosurg. 58, 678–681 (1983). 27. Elster, A. D., Sanders, T. G., Vines, F. S. & Chen, M. Y.
7. Regal, M., Paramo, C., Sierra, S. M. 17. Gross, P. M. et al. Topography of short portal vessels Size and shape of the pituitary gland during pregnancy
& Garcia‑Mayor, R. V. Prevalence and incidence of in the rat pituitary gland: a scanning electron- and post partum: measurement with MR imaging.
hypopituitarism in an adult Caucasian population microscopic and morphometric study of corrosion cast Radiology 181, 531–535 (1991).
in northwestern Spain. Clin. Endocrinol. (Oxf.) 55, replicas. Cell Tissue Res. 272, 79–88 (1993). 28. Scheithauer, B. W. et al. The pituitary gland
735–740 (2001). 18. Porter, J. C., Kamberi, I. A. & Grazia, Y. R. in Frontiers in pregnancy: a clinicopathologic and
8. Fernandez‑Rodriguez, E. et al. Epidemiology, mortality in Neuroendocrinology (eds Martini, L. & Ganong, W.) immunohistochemical study of 69 cases. Mayo Clin.
rate and survival in a homogeneous population of 145–175 (1978). Proc. 65, 461–474 (1990).
hypopituitary patients. Clin. Endocrinol. (Oxf.) 78, 19. Karaca, Z., Tanriverdi, F., Unluhizarci, K. 29. Tyson, J. E., Hwang, P., Guyda, H. & Friesen, H. G.
278–284 (2013). & Kelestimur, F. Pregnancy and pituitary disorders. Studies of prolactin secretion in human pregnancy.
9. Sheehan, H. L. & Murdoch, R. Post-partum necrosis Eur. J. Endocrinol. 162, 453–475 (2010). Am. J. Obstet. Gynecol. 113, 14–20 (1972).
of the anterior pituitary; pathological and clinical This is a detailed review about the physiological 30. Diri, H., Karaca, Z., Tanriverdi, F., Unluhizarci, K.
aspects. BJOG 45, 456–487 (1938). and anatomical changes and diseases associated & Kelestimur, F. Sheehan’s syndrome: new insights
10. Asaoka, K. [A study on the incidence of post-partum with the pituitary gland. into an old disease. Endocrine 51, 22–31 (2016).
hypopituitarism, (Sheehan’s syndrome)]. Nihon 20. Asa, S. L. Pituitary histopathology in man: normal This is the latest review about Sheehan syndrome
Naibunpi Gakkai Zasshi 53, 895–909 (in Japanese) and abnormal. Endotext https://www.ncbi.nlm.nih.gov/ that discusses the clinical studies carried out
(1977). books/NBK279003 (updated 10 June 2007). up to 2015.
NATURE RE VIE WS | DISEASE PRIMERS VOLUME 2 | 2016 | 13
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
PRIMER
31. Tessnow, A. H. & Wilson, J. D. The changing face of of autoimmunity in the pathogenesis of pituitary stimulation test. Am. J. Obstet. Gynecol.
Sheehan’s syndrome. Am. J. Med. Sci. 340, 402–406 Sheehan syndrome. 132, 348–353 (1978).
(2010). 55. De Bellis, A. et al. Immunological and clinical aspects 81. Simsek, Y. et al. A comparison of low-dose ACTH,
32. Kelestimur, F. Sheehan’s syndrome. Pituitary 6, of lymphocytic hypophysitis. Clin. Sci. (Lond.) 114, glucagon stimulation and insulin tolerance test in
181–188 (2003). 413–421 (2008). patients with pituitary disorders. Clin. Endocrinol.
This is the first and most comprehensive review 56. Atmaca, H., Arasli, M., Yazici, Z. A., Armutcu, F. (Oxf.) 82, 45–52 (2015).
about Sheehan syndrome.
& Tekin, I. O. Lymphocyte subpopulations in Sheehan’s 82. Oliveira, J. H., Persani, L., Beck‑Peccoz, P.
33. Matsuwaki, T., Khan, K. N., Inoue, T., Yoshida, A. syndrome. Pituitary 16, 202–207 (2013). & Abucham, J. Investigating the paradox of
& Masuzaki, H. Evaluation of obstetrical factors 57. Laway, B. A., Mir, S. A., Gojwari, T., Shah, T. R. hypothyroidism and increased serum thyrotropin
related to Sheehan syndrome. J. Obstet. Gynaecol. & Zargar, A. H. Selective preservation of anterior (TSH) levels in Sheehan’s syndrome: characterization
Res. 40, 46–52 (2014). pituitary functions in patients with Sheehan’s of TSH carbohydrate content and bioactivity. J. Clin.
34. Weeks, A. The prevention and treatment of postpartum syndrome. Indian J. Endocrinol. Metab. 15, Endocrinol. Metab. 86, 1694–1699 (2001).
haemorrhage: what do we know, and where do we go S238–S241 (2011). 83. Abucham, J., Castro, V., Maccagnan, P. & Vieira, J. G.
to next? BJOG 122, 202–210 (2015). 58. Dokmetas, H. S., Kilicli, F., Korkmaz, S. & Yonem, O. Increased thyrotrophin levels and loss of the nocturnal
35. Joseph, K. S. et al. Investigation of an increase in Characteristic features of 20 patients with Sheehan’s thyrotrophin surge in Sheehan’s syndrome.
postpartum haemorrhage in Canada. BJOG 114, syndrome. Gynecol. Endocrinol. 22, 279–283 (2006). Clin. Endocrinol. (Oxf.) 47, 515–522 (1997).
751–759 (2007). 59. Du, G. L. et al. Sheehan’s syndrome in Xinjiang: clinical 84. MacCagnan, P., Oliveira, J. H., Castro, V.
36. Lain, S. J., Roberts, C. L., Hadfield, R. M., Bell, J. C. characteristics and laboratory evaluation of 97 & Abucham, J. Abnormal circadian rhythm and
& Morris, J. M. How accurate is the reporting of patients. Hormones (Athens) 14, 660–667 (2015). increased non-pulsatile secretion of thyrotrophin
obstetric haemorrhage in hospital discharge data? 60. Gei‑Guardia, O., Soto‑Herrera, E., Gei‑Brealey, A. in Sheehan’s syndrome. Clin. Endocrinol. (Oxf.) 51,
A validation study. Aust. N. Z. J. Obstet. Gynaecol. 48, & Chen‑Ku, C. H. Sheehan syndrome in Costa Rica: 439–447 (1999).
481–484 (2008). clinical experience with 60 cases. Endocr. Pract. 17, 85. Oelkers, W. Hyponatremia and inappropriate secretion
37. Roberts, D. M. Sheehan’s syndrome. Am. Fam. 337–344 (2011). of vasopressin (antidiuretic hormone) in patients with
Physician 37, 223–227 (1988). 61. Gokalp, D. et al. Four decades without diagnosis: hypopituitarism. N. Engl. J. Med. 321, 492–496
38. Lust, K., McIntyre, H. D. & Morton, A. Sheehan’s Sheehan’s syndrome, a retrospective analysis. (1989).
syndrome — acute presentation with hyponatraemia Gynecol Endocrinol. 2 June 2016 [epub ahead 86. Schrier, R. W. Body water homeostasis: clinical
and headache. Aust. N. Z. J. Obstet. Gynaecol. 41, of print]. disorders of urinary dilution and concentration. J. Am.
348–351 (2001). 62. Kelestimur, F. et al. Sheehan’s syndrome: baseline Soc. Nephrol. 17, 1820–1832 (2006).
39. Bakiri, F., Bendib, S. E., Maoui, R., Bendib, A. characteristics and effect of 2 years of growth 87. Gokalp, D. et al. Sheehan’s syndrome as a rare cause
& Benmiloud, M. The sella turcica in Sheehan’s hormone replacement therapy in 91 patients in of anaemia secondary to hypopituitarism.
syndrome: computerized tomographic study in 54 KIMS — Pfizer International Metabolic Database. Ann. Hematol. 88, 405–410 (2009).
patients. J. Endocrinol. Invest. 14, 193–196 (1991). Eur. J. Endocrinol. 152, 581–587 (2005). 88. Oliveira, M. C. et al. Acquired factor VIII and
40. Sherif, I. H., Vanderley, C. M., Beshyah, S. & Bosairi, S. 63. Lim, C. H. et al. Electrolyte imbalance in patients von Willebrand factor (aFVIII/VWF) deficiency and
Sella size and contents in Sheehan’s syndrome. with Sheehan’s syndrome. Endocrinol. Metab. (Seoul) hypothyroidism in a case with hypopituitarism.
Clin. Endocrinol. (Oxf.) 30, 613–618 (1989). 30, 502–508 (2015). Clin. Appl. Thromb. Hemost. 16, 107–109 (2010).
41. McKay, D. G., Merrill, S. J., Weiner, A. E., Hertig, A. T. 64. Sert, M., Tetiker, T., Kirim, S. & Kocak, M. Clinical 89. Erslev, A. J. Anemia of Endocrine Disorders
& Reid, D. E. The pathologic anatomy of eclampsia, report of 28 patients with Sheehan’s syndrome. (McGraw‑Hill, 2001).
bilateral renal cortical necrosis, pituitary necrosis, and Endocr. J. 50, 297–301 (2003). 90. Gokmen Akoz, A., Atmaca, H., Ustundag, Y.
other acute fatal complications of pregnancy, and its 65. Kan, A. K. & Calligerous, D. A case report of Sheehan & Ozdamar, S. O. An unusual case of pancytopenia
possible relationship to the generalized Shwartzman syndrome presenting with diabetes insipidus. associated with Sheehan’s syndrome. Ann. Hematol.
phenomenon. Am. J. Obstet. Gynecol. 66, 507–539 Aust. N. Z. J. Obstet. Gynaecol. 38, 224–226 (1998). 86, 307–308 (2007).
(1953). 66. Tomlinson, J. W. et al. Association between premature 91. Laway, B. A. et al. Sheehan’s syndrome with
42. Erez, O., Mastrolia, S. A. & Thachil, J. Disseminated mortality and hypopituitarism. West Midlands pancytopenia — complete recovery after hormone
intravascular coagulation in pregnancy: insights Prospective Hypopituitary Study Group. Lancet 357, replacement (case series with review). Ann. Hematol.
in pathophysiology, diagnosis and management. 425–431 (2001). 89, 305–308 (2010).
Am. J. Obstet. Gynecol. 213, 452–463 (2015). 67. Furnica, R. M. et al. Early diagnosis of Sheehan’s 92. Dash, R. J., Gupta, V. & Suri, S. Sheehan’s syndrome:
43. Cunningham, F. G. & Nelson, D. B. Disseminated syndrome. Anaesth. Crit. Care Pain Med. 34, 61–63 clinical profile, pituitary hormone responses and
intravascular coagulation syndromes in obstetrics. (2015). computed sellar tomography. Aust. N. Z. J. Med. 23,
Obstet. Gynecol. 126, 999–1011 (2015). 68. Huang, Y. Y., Ting, M. K., Hsu, B. R. & Tsai, J. S. 26–31 (1993).
44. Laway, B. A. et al. Prevalence of hematological Demonstration of reserved anterior pituitary function 93. Dejager, S., Gerber, S., Foubert, L. & Turpin, G.
abnormalities in patients with Sheehan’s syndrome: among patients with amenorrhea after postpartum Sheehan’s syndrome: differential diagnosis in the
response to replacement of glucocorticoids and hemorrhage. Gynecol. Endocrinol. 14, 99–104 acute phase. J. Intern. Med. 244, 261–266 (1998).
thyroxine. Pituitary 14, 39–43 (2011). (2000). 94. Sasaki, S. et al. A novel hook-shaped enhancement on
45. Shivaprasad, C. Sheehan’s syndrome: newer advances. 69. Smith, D. M., McKenna, K. & Thompson, C. J. contrast-enhanced sagittal magnetic resonance image
Indian J. Endocrinol. Metab. 15, S203–S207 (2011). Hyponatraemia. Clin. Endocrinol. (Oxf.) 52, 667–678 in acute Sheehan’s syndrome: a case report. Endocr. J.
46. Carp, H. et al. Prevalence of genetic markers for (2000). 61, 71–76 (2014).
thrombophilia in recurrent pregnancy loss. 70. Kurtulmus, N. & Yarman, S. Hyponatremia as the 95. Laway, B., Misgar, R., Mir, S. & Wani, A. Clinical,
Hum. Reprod. 17, 1633–1637 (2002). presenting manifestation of Sheehan’s syndrome in hormonal and radiological features of partial
47. Gokalp, D. et al. Analysis of thrombophilic genetic elderly patients. Aging Clin. Exp. Res. 18, 536–539 Sheehan’s syndrome: an Indian experience.
mutations in patients with Sheehan’s syndrome: (2006). Arch. Endocrinol. Metab. 60, 125–129 (2016).
is thrombophilia responsible for the pathogenesis of 71. Guven, M., Bayram, F., Guven, K. & Kelestimur, F. 96. Sheehan, H. L. Atypical hypopituitarism. Proc. R. Soc.
Sheehan’s syndrome? Pituitary 14, 168–173 (2011). Evaluation of patients admitted with hypoglycaemia Med. 54, 43–48 (1961).
48. Pasa, S. et al. Prothrombin time, activated to a teaching hospital in Central Anatolia. 97. [No authors listed.] Case records of the Massachusetts
thromboplastin time, fibrinogen and d‑dimer levels Postgrad. Med. J. 76, 150–152 (2000). General Hospital. Weekly clinicopathological exercises.
and von-Willebrand activity of patients with Sheehan’s 72. Weiner, P., Ben‑Israel, J. & Plavnick, L. Sheehan’s Case 25–1995 — a 44‑year-old woman with
syndrome and the effect of hormone replacement syndrome with diabetes insipidus. A case study. headache, blurred vision, and an intrasellar mass.
therapy on these factors. Int. J. Hematol. Oncol. 20, Isr. J. Med. Sci. 15, 431–433 (1979). N. Engl. J. Med. 333, 441–447 (1995).
212–219 (2010). 73. Chihaoui, M. et al. Bone mineral density in Sheehan’s 98. Unluhizarci, K. et al. Distinct radiological and clinical
49. Tanriverdi, F. et al. The effects of 12 months of growth syndrome; prevalence of low bone mass and appearance of lymphocytic hypophysitis. J. Clin.
hormone replacement therapy on cardiac autonomic associated factors. J. Clin. Densitom. 19, 413–418 Endocrinol. Metab. 86, 1861–1864 (2001).
tone in adults with growth hormone deficiency. (2016). 99. Hashimoto, K., Takao, T. & Makino, S. Lymphocytic
Clin. Endocrinol. (Oxf.) 62, 706–712 (2005). 74. Gokalp, D. et al. Sheehan’s syndrome and its impact adenohypophysitis and lymphocytic
50. Katz, D. & Beilin, Y. Disorders of coagulation in on bone mineral density. Gynecol. Endocrinol. 25, infundibuloneurohypophysitis. Endocr. J. 44, 1–10
pregnancy. Br. J. Anaesth. 115 (Suppl. 2), ii75–ii88 344–349 (2009). (1997).
(2015). 75. Kanis, J. A., Melton, L. J. 3rd, Christiansen, C., 100. Karaca, Z., Tanriverdi, F., Unluhizarci, K., Kelestimur, F.
51. Atmaca, H., Tanriverdi, F., Gokce, C., Unluhizarci, K. & Johnston, C. C. & Khaltaev, N. The diagnosis of & Donmez, H. Empty sella may be the final outcome
Kelestimur, F. Posterior pituitary function in Sheehan’s osteoporosis. J. Bone Miner. Res. 9, 1137–1141 in lymphocytic hypophysitis. Endocr. Res. 34, 10–17
syndrome. Eur. J. Endocrinol. 156, 563–567 (2007). (1994). (2009).
52. Ozbey, N. et al. Clinical and laboratory evaluation of 76. Acibucu, F., Kilicli, F. & Dokmetas, H. S. Assessment 101. Shehata, H. A. & Okosun, H. Neurological disorders in
40 patients with Sheehan’s syndrome. Isr. J. Med. Sci. of bone mineral density in patients with Sheehan’s pregnancy. Curr. Opin. Obstet. Gynecol. 16, 117–122
30, 826–829 (1994). syndrome. Gynecol. Endocrinol. 30, 532–535 (2014).
(2004).
53. Goswami, R., Kochupillai, N., Crock, P. A., Jaleel, A. 77. Sunil, E. et al. Sheehan’s syndrome: a single centre 102. Karaca, Z. & Kelestimur, F. The management of
& Gupta, N. Pituitary autoimmunity in patients with experience. J. Clin. Sci. Res. 2, 16–21 (2013). hypophysitis. Minerva Endocrinol. 41, 390–399
Sheehan’s syndrome. J. Clin. Endocrinol. Metab. 87, 78. Kilicli, F., Dokmetas, H. S. & Acibucu, F. Sheehan’s (2016).
4137–4141 (2002). syndrome. Gynecol. Endocrinol. 29, 292–295 (2013). 103. McLintock, C. & James, A. H. Obstetric hemorrhage.
54. De Bellis, A. et al. Anti-hypothalamus and anti- 79. Shahmanesh, M., Ali, Z., Pourmand, M. J. Thromb. Haemost. 9, 1441–1451 (2011).
pituitary antibodies may contribute to perpetuate the & Nourmand, I. Pituitary function tests in Sheehan’s 104. Sheldon, W. R. et al. Postpartum haemorrhage
hypopituitarism in patients with Sheehan’s syndrome. syndome. Clin. Endocrinol. (Oxf.) 12, 303–311 management, risks, and maternal outcomes: findings
Eur. J. Endocrinol. 158, 147–152 (2008). (1980). from the World Health Organization Multicountry
This is one of the first reports that 80. DiZerega, G., Kletzky, O. A. & Mishell, D. R. Jr. Survey on maternal and newborn health. BJOG
provides comprehensive evidence for the role Diagnosis of Sheehan’s syndrome using a sequential 121 (Suppl. 1), 5–13 (2014).
14 | 2016 | VOLUME 2 www.nature.com/nrdp
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
PRIMER
105. Anderson, J. M. & Etches, D. Prevention and clinical practice guideline. J. Clin. Endocrinol. Metab. 135. Karaca, Z. et al. GH replacement therapy during
management of postpartum hemorrhage. Am. Fam. 91, 1621–1634 (2006). pregnancy in a patient with Sheehan’s syndrome.
Physician 75, 875–882 (2007). 121. Tanriverdi, F. et al. Effects of 18‑month of growth Endocrine Abstracts 35, P856 (2014).
106. World Health Organization. WHO Recommendations hormone (GH) replacement therapy in patients with 136. Foyouzi, N., Frisbaek, Y. & Norwitz, E. R. Pituitary
for the Prevention and Treatment of Postpartum Sheehan’s syndrome. Growth Horm. IGF Res. 15, gland and pregnancy. Obstet. Gynecol. Clin. North Am.
Haemorrhage (WHO, 2012). 231–237 (2005). 31, 873–892 (2004).
107. Shields, L. E., Wiesner, S., Fulton, J. & Pelletreau, B. 122. Golgeli, A. et al. Utility of P300 auditory event related 137. Holmer, H. et al. Psychosocial health and levels of
Comprehensive maternal hemorrhage protocols potential latency in detecting cognitive dysfunction employment in 851 hypopituitary Swedish patients on
reduce the use of blood products and improve in growth hormone (GH) deficient patients with long-term GH therapy. Psychoneuroendocrinology 38,
patient safety. Am. J. Obstet. Gynecol. 212, 272–280 Sheehan’s syndrome and effects of GH replacement 842–852 (2013).
(2015). therapy. Eur. J. Endocrinol. 150, 153–159 (2004). 138. Crespo, I., Valassi, E., Santos, A. & Webb, S. M.
108. Rajasekaran, S. et al. UK guidelines for the 123. Tanriverdi, F. et al. Investigation of the skin Health‑related quality of life in pituitary diseases.
management of pituitary apoplexy. Clin. Endocrinol. characteristics in patients with severe GH deficiency Endocrinol. Metab. Clin. North Am. 44, 161–170
(Oxf.) 74, 9–20 (2011). and the effects of 6 months of GH replacement (2015).
109. Forss, M., Batcheller, G., Skrtic, S. & Johannsson, G. therapy: a randomized placebo controlled study. 139. Ragnarsson, O. et al. The relationship between
Current practice of glucocorticoid replacement therapy Clin. Endocrinol. (Oxf.) 65, 579–585 (2006). glucocorticoid replacement and quality of life in
and patient-perceived health outcomes in adrenal 124. Ismailogullari, S., Tanriverdi, F., Kelestimur, F. 2737 hypopituitary patients. Eur. J. Endocrinol. 171,
insufficiency — a worldwide patient survey. & Aksu, M. Sleep architecture in Sheehan’s syndrome 571–579 (2014).
BMC Endocr. Disord. 12, 8 (2012). before and 6 months after growth hormone 140. Willems, C. et al. Regeneration in the pituitary after
110. Nilsson, A. G. et al. Prospective evaluation of replacement therapy. Psychoneuroendocrinology 34, cell-ablation injury: time-related aspects and molecular
long‑term safety of dual-release hydrocortisone 212–219 (2009). analysis. Endocrinology 157, 705–721 (2016).
replacement administered once daily in patients 125. Erkut, Z. A., Pool, C. & Swaab, D. F. Glucocorticoids 141. Ozone, C. et al. Functional anterior pituitary generated
with adrenal insufficiency. Eur. J. Endocrinol. 171, suppress corticotropin-releasing hormone and in self-organizing culture of human embryonic stem
369–377 (2014). vasopressin expression in human hypothalamic cells. Nat. Commun. 7, 10351 (2016).
111. Oksnes, M. et al. Continuous subcutaneous neurons. J. Clin. Endocrinol. Metab. 83, 2066–2073 142. Fu, Q. et al. The adult pituitary shows stem/progenitor
hydrocortisone infusion versus oral hydrocortisone (1998). cell activation in response to injury and is capable
replacement for treatment of addison’s disease: 126. Karaca, Z. & Kelestimur, F. Pregnancy and other of regeneration. Endocrinology 153, 3224–3235
a randomized clinical trial. J. Clin. Endocrinol. Metab. pituitary disorders (including GH deficiency). (2012).
99, 1665–1674 (2014). Best Pract. Res. Clin. Endocrinol. Metab. 25, 143. Sheehan, H. L. & Davis, J. C. Postpartum
112. Fleseriu, M. et al. Hormonal replacement in 897–910 (2011). Hypopituitarism (Springfield, 1982).
hypopituitarism in adults: an Endocrine Society clinical 127. Allolio, B. et al. Diurnal salivary cortisol patterns This book discusses the postpartum period
practice guideline. J. Clin. Endocrinol. Metab. 101, during pregnancy and after delivery: relationship and the related postpartum hypopituitarism.
3888–3921 (2016). to plasma corticotrophin-releasing-hormone. 144. Fitzgerald, K. T. The structure and function of the
This is the latest guideline about the treatment Clin. Endocrinol. (Oxf.) 33, 279–289 (1990). pars tuberalis of the vertebrate adenohypophysis.
of hypopituitarism. 128. Nolten, W. E., Lindheimer, M. D., Rueckert, P. A., Gen. Comp. Endocrinol. 37, 383–399 (1979).
113. Giavoli, C. et al. Effect of recombinant human growth Oparil, S. & Ehrlich, E. N. Diurnal patterns and 145. Kristjansdottir, H. L., Bodvarsdottir, S. P.
hormone (GH) replacement on the hypothalamic– regulation of cortisol secretion in pregnancy. J. Clin. & Sigurjonsdottir, H. A. Sheehan’s syndrome in
pituitary–adrenal axis in adult GH‑deficient patients. Endocrinol. Metab. 51, 466–472 (1980). modern times: a nationwide retrospective study
J. Clin. Endocrinol. Metab. 89, 5397–5401 (2004). 129. Demura, R. et al. Placental secretion of prolactin, in Iceland. Eur. J. Endocrinol. 164, 349–354 (2011).
114. Atmaca, H., Tanriverdi, F., Gokce, C., Unluhizarci, K. ACTH and immunoreactive β-endorphin during 146. Famuyiwa, O. O., Bella, A. F. & Akanji, A. O. Sheehan’s
& Kelestimur, F. Do we still need the TRH stimulation pregnancy. Acta Endocrinol. (Copenh.) 100, 114–119 syndrome in a developing country, Nigeria: a rare
test? Thyroid 17, 529–533 (2007). (1982). disease or problem of diagnosis? East Afr. Med. J. 69,
115. Jorgensen, J. O. et al. Effects of growth hormone 130. Glinoer, D. et al. Regulation of maternal thyroid during 40–43 (1992).
therapy on thyroid function of growth hormone- pregnancy. J. Clin. Endocrinol. Metab. 71, 276–287
deficient adults with and without concomitant (1990). Acknowledgements
thyroxine-substituted central hypothyroidism. J. Clin. 131. Burrow, G. N., Fisher, D. A. & Larsen, P. R. Maternal The authors express their profound gratitude to their medical
Endocrinol. Metab. 69, 1127–1132 (1989). and fetal thyroid function. N. Engl. J. Med. 331, illustrator, M. E. Aykurt, for his original artwork of Figure 1b
116. Higham, C. E., Johannsson, G. & Shalet, S. M. 1072–1078 (1994). and the help of Dr A. Sehgal, Dr S. Malik and Dr H. Ashraf,
Hypopituitarism. Lancet 388, 2403–2415 (2016). 132. De Groot, L. et al. Management of thyroid dysfunction who are senior residents in the Department of Endocrinology
117. Leung, K. C., Johannsson, G., Leong, G. M. & Ho, K. K. during pregnancy and postpartum: an Endocrine at Sher-I-Kashmir Institute of Medical Sciences (SKIMS),
Estrogen regulation of growth hormone action. Society clinical practice guideline. J. Clin. Endocrinol. for their help in preparation of the manuscript.
Endocr. Rev. 25, 693–721 (2004). Metab. 97, 2543–2565 (2012).
118. Wolthers, T. et al. Oral estrogen antagonizes the 133. Eriksson, L., Frankenne, F., Eden, S., Hennen, G. Author contributions
metabolic actions of growth hormone in growth & Von Schoultz, B. Growth hormone 24‑h serum Introduction (F.K.); Epidemiology (B.A.L.); Mechanisms/patho‑
hormone-deficient women. Am. J. Physiol. Endocrinol. profiles during pregnancy — lack of pulsatility for physiology (Z.K., H.A. and F.K.); Diagnosis, screening and
Metab. 281, E1191–E1196 (2001). the secretion of the placental variant. Br. J. Obstet. prevention (B.A.L., H.S.D. and H.A.); Management (B.A.L.,
119. Soares, D. V. et al. Two years of growth hormone Gynaecol. 96, 949–953 (1989). H.S.D. and F.K.); Quality of life (H.A. and B.A.L.); Outlook
replacement therapy in a group of patients with 134. Frankenne, F. et al. The physiology of growth (All); Overview of Primer (F.K.).
Sheehan’s syndrome. Pituitary 9, 127–135 (2006). hormones (GHs) in pregnant women and partial
120. Molitch, M. E. et al. Evaluation and treatment of adult characterization of the placental GH variant. J. Clin. Competing interests
growth hormone deficiency: an Endocrine Society Endocrinol. Metab. 66, 1171–1180 (1988). The authors declare no competing interests.
NATURE RE VIE WS | DISEASE PRIMERS VOLUME 2 | 2016 | 15
©
2
0
1
6
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
You might also like
- Impaired Lactation Review of Delayed Lactogenesis and Insufficient LactationDocument10 pagesImpaired Lactation Review of Delayed Lactogenesis and Insufficient LactationRob BordenNo ratings yet
- Endocrine SystemDocument25 pagesEndocrine Systemangel_maui100% (13)
- Sheehan's Syndrome PathophysiologyDocument2 pagesSheehan's Syndrome PathophysiologyirismgallNo ratings yet
- Sheehan Syndrome Lancet Eponym 2003Document3 pagesSheehan Syndrome Lancet Eponym 2003Alejandro GuillenNo ratings yet
- Sheehan Syndrom L. HaddockDocument9 pagesSheehan Syndrom L. Haddockfreddyop72No ratings yet
- Excreta & Sewage Disposal LectDocument79 pagesExcreta & Sewage Disposal LectKathy YoungNo ratings yet
- SchistosomiasisDocument4 pagesSchistosomiasisLeo TiuNo ratings yet
- Cholecystectomy and Common Bile Duct ExplorationDocument22 pagesCholecystectomy and Common Bile Duct ExplorationmohamedhazemelfollNo ratings yet
- What Is Gastrointestinal BleedingDocument8 pagesWhat Is Gastrointestinal BleedingApril Joy RutaquioNo ratings yet
- NCP Sample 1Document9 pagesNCP Sample 1Vincent BarcenillaNo ratings yet
- Pathophysiology of Pott'S DiseaseDocument4 pagesPathophysiology of Pott'S Diseasee3runeNo ratings yet
- Nuevaespana, Jayne Angelie A. BSN 2A: GI: NauseaDocument7 pagesNuevaespana, Jayne Angelie A. BSN 2A: GI: NauseaJayne Angelie A. NuevaespañaNo ratings yet
- FNCP BeastfeedingDocument1 pageFNCP BeastfeedingRizzy UgayNo ratings yet
- CirrhosisFS 508 PDFDocument16 pagesCirrhosisFS 508 PDFDessy AmalinaNo ratings yet
- NCPDocument4 pagesNCPJhuRise Ann ManganaNo ratings yet
- Creatinine Clearance Test-1Document17 pagesCreatinine Clearance Test-1wanderer_1010No ratings yet
- Philippine Code of Ethics of The Medical Profession 2016Document12 pagesPhilippine Code of Ethics of The Medical Profession 2016dockaykuNo ratings yet
- Maternal/Ob Notes: A Person's Sexuality Encompasses The Complex Behaviors, Attitudes Emotions and Preferences That AreDocument37 pagesMaternal/Ob Notes: A Person's Sexuality Encompasses The Complex Behaviors, Attitudes Emotions and Preferences That Aresabao kizuiteNo ratings yet
- NCP Nursing DiagnosisDocument24 pagesNCP Nursing Diagnosisphvega06No ratings yet
- Burn Ctu 312 - 2Document1 pageBurn Ctu 312 - 2Shaira Ann CalambaNo ratings yet
- Obstructive Jaundice and Perioperative ManagementsDocument8 pagesObstructive Jaundice and Perioperative ManagementsTri UtomoNo ratings yet
- Ob NotesDocument4 pagesOb NotesJeffrey ViernesNo ratings yet
- Case presentationPHCDocument149 pagesCase presentationPHCChitPerRhosNo ratings yet
- Case Scenario (Lung Cancer)Document12 pagesCase Scenario (Lung Cancer)Mitzi CastuloNo ratings yet
- Schizophrenia ArticleDocument6 pagesSchizophrenia Articleyasira0% (1)
- Immune FunctionDocument27 pagesImmune Functionhalloween candyNo ratings yet
- Creatinine ClearanceDocument3 pagesCreatinine ClearanceJarred Tandingan CabasogNo ratings yet
- Acute AppendicitisDocument23 pagesAcute AppendicitisSandie Daniel GabalunosNo ratings yet
- Water SanitationDocument4 pagesWater SanitationTrina CardonaNo ratings yet
- Antineoplastic AgentsDocument3 pagesAntineoplastic AgentsJan Patrick ArrietaNo ratings yet
- Family Nursing ProcessDocument6 pagesFamily Nursing ProcessAbigail BascoNo ratings yet
- Neonatal Hiatal Hernia - A Rare Case ReportDocument4 pagesNeonatal Hiatal Hernia - A Rare Case ReportAgus DarwiyantoNo ratings yet
- Pa Tho Physiology Chicken PoxDocument4 pagesPa Tho Physiology Chicken PoxPao RamirezNo ratings yet
- Discharge PlanDocument5 pagesDischarge PlanrraksNo ratings yet
- Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationDocument7 pagesAssessment Nursing Diagnosis Planning Intervention Rationale EvaluationMaria Fatima MagsinoNo ratings yet
- Liceo de Cagayan University: Acute AppendicitisDocument2 pagesLiceo de Cagayan University: Acute AppendicitisKylie AstrudNo ratings yet
- Hur Tin Yang Vs PeopleDocument11 pagesHur Tin Yang Vs Peoplediamajolu gaygonsNo ratings yet
- ParagonimiasisDocument15 pagesParagonimiasisMhelrose Jornales100% (1)
- Bipolar 1 DisorderDocument11 pagesBipolar 1 DisorderGirlly AlcantaraNo ratings yet
- CP (Sub-Grp)Document79 pagesCP (Sub-Grp)Pamela laquindanumNo ratings yet
- Water Sanitation and Hygiene EssayDocument2 pagesWater Sanitation and Hygiene Essayshjahsjansha100% (1)
- Pa Tho Physiology of TuberculosisDocument3 pagesPa Tho Physiology of TuberculosisFlauros Ryu JabienNo ratings yet
- Graduate School Nursing Care Plan Assessment Nursing Diagnosis Planning Intervention Rationale Expected OutcomeDocument3 pagesGraduate School Nursing Care Plan Assessment Nursing Diagnosis Planning Intervention Rationale Expected OutcomeMary Rose F. MalaluanNo ratings yet
- Step-By-step Description of HemodialysisDocument11 pagesStep-By-step Description of Hemodialysisprakash_smileyNo ratings yet
- NCP AgnDocument2 pagesNCP AgnMichael Vincent DuroNo ratings yet
- Activity IntoleranceDocument1 pageActivity IntoleranceRonlene CoronelNo ratings yet
- Nursing Intervention Prostate CancerDocument2 pagesNursing Intervention Prostate CancerKathleen DimacaliNo ratings yet
- Topic:: "Gestational Conditions Affecting Pregnancy Outcomes"Document29 pagesTopic:: "Gestational Conditions Affecting Pregnancy Outcomes"Marie Ashley CasiaNo ratings yet
- RA 2382 As Amended by RA 4224Document7 pagesRA 2382 As Amended by RA 4224Romarie AbrazaldoNo ratings yet
- The Medical Act of 1959Document10 pagesThe Medical Act of 1959Jarvin David ResusNo ratings yet
- WK 17.valerianoDocument5 pagesWK 17.valerianoVALERIANO TRISHANo ratings yet
- Medical Ward - Discharge PlanDocument5 pagesMedical Ward - Discharge Plandon7dane100% (1)
- Tenofovir Disoproxil Fumarate: Therese M. Chapman, Jane K. Mcgavin and Stuart NobleDocument12 pagesTenofovir Disoproxil Fumarate: Therese M. Chapman, Jane K. Mcgavin and Stuart NobleBagusHibridaNo ratings yet
- Abdominal MassDocument5 pagesAbdominal MassArthana PutraNo ratings yet
- Grabe Ka FinalDocument57 pagesGrabe Ka FinalJoanne Bernadette AguilarNo ratings yet
- ScenarioDocument1 pageScenarioAngel Lynn YlayaNo ratings yet
- Premature LaborDocument59 pagesPremature LaborAmiel Francisco ReyesNo ratings yet
- Ordonio, Alyn Kyla S. BSN-1C TFN-MW7:40-9:10: Name of Theorist Theory Description Florence NightingaleDocument4 pagesOrdonio, Alyn Kyla S. BSN-1C TFN-MW7:40-9:10: Name of Theorist Theory Description Florence NightingaleKyla OrdonioNo ratings yet
- Compilation Drugstudy, NCP Cva (1) - BadetDocument14 pagesCompilation Drugstudy, NCP Cva (1) - BadetLizette Villanueva-UntalanNo ratings yet
- NCP PudDocument3 pagesNCP PudSolsona Natl HS MaanantengNo ratings yet
- PRIORITY 2: Impaired Gas Exchange Related To Excessive or Thick Secretions Tree Secondary To PneumoniaDocument4 pagesPRIORITY 2: Impaired Gas Exchange Related To Excessive or Thick Secretions Tree Secondary To PneumoniaElay Pedroso100% (1)
- Taylor 2018Document16 pagesTaylor 2018Zahra Alpi SyafilaNo ratings yet
- Seminar: Jan Claassen, Soojin ParkDocument17 pagesSeminar: Jan Claassen, Soojin ParkRaul DoctoNo ratings yet
- 1998 Volvo s70-v70Document52 pages1998 Volvo s70-v70Raul DoctoNo ratings yet
- BMW 6 Cylinder Dual Vanos Piston Seal Repair Fix PDocument13 pagesBMW 6 Cylinder Dual Vanos Piston Seal Repair Fix PRaul DoctoNo ratings yet
- Central Venous Pressure (CVP)Document3 pagesCentral Venous Pressure (CVP)Raul DoctoNo ratings yet
- An Update On COVID-19 and Pregnancy: Djamieson@emory - EduDocument10 pagesAn Update On COVID-19 and Pregnancy: Djamieson@emory - EduRaul DoctoNo ratings yet
- Why Exercise Builds Muscles: Titin Mechanosensing Controls Skeletal Muscle Growth Under LoadDocument15 pagesWhy Exercise Builds Muscles: Titin Mechanosensing Controls Skeletal Muscle Growth Under LoadRaul Docto100% (1)
- Ascoping Review of The Pathophysiology of COVID-19Document16 pagesAscoping Review of The Pathophysiology of COVID-19Raul DoctoNo ratings yet
- X3 E83 X3 3.0i FRNT Axle Support, Wishbone Tension StrutDocument3 pagesX3 E83 X3 3.0i FRNT Axle Support, Wishbone Tension StrutRaul DoctoNo ratings yet
- Tugwell 1985Document13 pagesTugwell 1985Raul DoctoNo ratings yet
- 007 Obgyn-CatalogDocument100 pages007 Obgyn-CatalogRaul DoctoNo ratings yet
- 2022 ACC A-Ha HFSAGuideline For The Management of Heart FailureDocument167 pages2022 ACC A-Ha HFSAGuideline For The Management of Heart FailureRaul DoctoNo ratings yet
- How To Install Google Play On The Amazon Fire HD 8Document7 pagesHow To Install Google Play On The Amazon Fire HD 8Raul DoctoNo ratings yet
- Obstetrics & GynecologyDocument10 pagesObstetrics & GynecologyRaul DoctoNo ratings yet
- Case 35-2021: A 50-Year-Old Woman With Pain in The Left Upper Quadrant and HypoxemiaDocument7 pagesCase 35-2021: A 50-Year-Old Woman With Pain in The Left Upper Quadrant and HypoxemiaRaul DoctoNo ratings yet
- Vlaar2021 Article TransfusionStrategiesInBleedinDocument25 pagesVlaar2021 Article TransfusionStrategiesInBleedinRaul DoctoNo ratings yet
- Heparin Resistance - Clinical Perspectives and Management StrategiesDocument7 pagesHeparin Resistance - Clinical Perspectives and Management StrategiesRaul DoctoNo ratings yet
- Human Infection With Strongyloides Stercoralis and Other Related Strongyloides SpeciesDocument11 pagesHuman Infection With Strongyloides Stercoralis and Other Related Strongyloides SpeciesRaul DoctoNo ratings yet
- Ventilator Weaning and Spontaneous Breathing Trials An Educational ReviewDocument7 pagesVentilator Weaning and Spontaneous Breathing Trials An Educational ReviewRaul DoctoNo ratings yet
- Author 'S Accepted ManuscriptDocument46 pagesAuthor 'S Accepted ManuscriptRaul DoctoNo ratings yet
- Lecture 1: NeuroembryologyDocument13 pagesLecture 1: NeuroembryologyRaul Docto100% (1)
- Prolonged Pregnancy:When Should We Intervene?Document11 pagesProlonged Pregnancy:When Should We Intervene?Raul DoctoNo ratings yet
- Endocrinology & Metabolic Syndrome: A Late-Onset of Sheehan's Syndrome Presenting With Life-Threatening HypoglycemiaDocument3 pagesEndocrinology & Metabolic Syndrome: A Late-Onset of Sheehan's Syndrome Presenting With Life-Threatening HypoglycemiaNona SaudaleNo ratings yet
- Empty Sella SyndromeDocument21 pagesEmpty Sella SyndromeMohamed TarekNo ratings yet
- Prasuti p2 Part ADocument101 pagesPrasuti p2 Part ApranayNo ratings yet
- Streeroga Paper 2 Part ADocument101 pagesStreeroga Paper 2 Part AVYSHAK MONo ratings yet
- Hemorragia PostpartoDocument34 pagesHemorragia PostpartoGiiszs AlvarezNo ratings yet
- A Case of Sheehan's Syndrome: A Rare But Life - Threatening ComplicationDocument2 pagesA Case of Sheehan's Syndrome: A Rare But Life - Threatening ComplicationEditor IJTSRDNo ratings yet
- Content 3Document128 pagesContent 3Mohamed AbbasNo ratings yet
- Objective Mock ExamDocument48 pagesObjective Mock ExamJude Thaddeaus AdjeiNo ratings yet
- Management of of Clients With Metabolic and EndocrineDocument79 pagesManagement of of Clients With Metabolic and Endocrineagbogoodness100% (1)
- Normal and Abnormal PuerperiumDocument21 pagesNormal and Abnormal PuerperiumPriyadarshini MhNo ratings yet
- Sheehan's Syndrome: A Case Report: KeywordsDocument2 pagesSheehan's Syndrome: A Case Report: Keywordsnurul habibahNo ratings yet
- Plabable Gems Endocrine PDF P7aDocument44 pagesPlabable Gems Endocrine PDF P7aayşenur sevinçNo ratings yet
- Endocrinology Module Study Guide 2023 FinalDocument24 pagesEndocrinology Module Study Guide 2023 Finaldomitam105No ratings yet
- Gynaecology MCQsDocument19 pagesGynaecology MCQssimi yNo ratings yet
- ACCPCritical Care Medicine Board ReviewDocument491 pagesACCPCritical Care Medicine Board ReviewdianaMDNo ratings yet
- Sample # 1 of Latest CK UW Notes-2022Document167 pagesSample # 1 of Latest CK UW Notes-2022Fareena KhanNo ratings yet
- Sheehan Syndrome Lancet Eponym 2003Document3 pagesSheehan Syndrome Lancet Eponym 2003Alejandro GuillenNo ratings yet
- EE - QE 661 QuestionsDocument74 pagesEE - QE 661 QuestionsHassan R. G.No ratings yet
- Obstetrics Emergencies: By: Farah Mashitah Hafiz AdeebDocument96 pagesObstetrics Emergencies: By: Farah Mashitah Hafiz AdeebAriff MahdzubNo ratings yet
- Sheehan's Syndrome.Document4 pagesSheehan's Syndrome.MosesNo ratings yet
- Hypopituitarism 1Document47 pagesHypopituitarism 1TuhinaRajNo ratings yet
- Pathology Exam (Endocrine System)Document2 pagesPathology Exam (Endocrine System)RinaFitriaNo ratings yet
- Colostrum 1Document57 pagesColostrum 1Light CareNo ratings yet
- NCMB 316 Cu12 EndocrineDocument84 pagesNCMB 316 Cu12 EndocrineJanine Dela CruzNo ratings yet
- Sheehan Syndrome Sarina SchragerDocument3 pagesSheehan Syndrome Sarina Schragerfreddyop72No ratings yet
- EndocrineDocument49 pagesEndocrineApsaraNo ratings yet
- Sheehan Syndrom L. HaddockDocument9 pagesSheehan Syndrom L. Haddockfreddyop72No ratings yet
- DNB ObstetricsDocument241 pagesDNB ObstetricsDilushini CalderaNo ratings yet