Professional Documents
Culture Documents
Module 08 - Respiration Assessment and Management in TFC: Speaker Notes
Uploaded by
Sae TumOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Module 08 - Respiration Assessment and Management in TFC: Speaker Notes
Uploaded by
Sae TumCopyright:
Available Formats
COMBAT LIFESAVER TACTICAL COMBAT CASUALTY CARE (TCCC)
SPEAKER NOTES
MODULE 08 – RESPIRATION ASSESSMENT AND MANAGEMENT
IN TFC
SLIDE 1 – TITLE SLIDE
SLIDE 2 – TCCC ROLES
Tactical Combat Casualty Care is broken up into four
roles of care. The most basic is taught to All Service
Members (ASM), which is designed to instruct in the
absolute basics of hemorrhage control and to recognize
more serious injuries.
You are in the Combat Lifesaver (CLS) role.
This teaches you more advanced care to treat the
most common causes of death on the battlefield, and to
recognize, prevent, and communicate with medical personnel the life-threatening complications of
these injuries.
The Combat Medic/Corpsman (CMC) role includes much more advanced and invasive care requiring
significantly more medical knowledge and skills.
Finally, the last role, Combat Paramedic/Provider (CPP) is for Combat paramedics and advanced
providers, to provide the most sophisticated care to keep our wounded warriors alive and get them to
definitive care.
Your role as a CLS is to treat the most common causes of death on the battlefield, which are massive
hemorrhage and airway/respiratory problems. Also, you are given the skills to prevent complications and
treat other associated but not immediately life-
threatening injuries.
SLIDE 3 – TLO/ELO
The TCCC-CLS course is built on a foundation of
learning objectives. These objectives lay out the basic
structure of the course and describe the knowledge
and skills you are expected to acquire by the end of
the course.
TCCC CLS SPEAKER NOTES #TCCC-CLS-14-01 25 JAN 20
COMBAT LIFESAVER TACTICAL COMBAT CASUALTY CARE (TCCC)
SPEAKER NOTES
The module has one Terminal Learning Objective, or TLO. The TLO is supported by a series of
Enabling Learning Objectives, or ELOs. This graphic shows how the ELOs are mapped to the TLOs. The
blue dots are cognitive or knowledge learning objectives, and the green dots are performance objectives
focused on skills.
SLIDE 4 – MARCH-PAWS
Respiration assessment is the “R” in the MARCH
PAWS sequence.
SLIDE 5 – RESPIRATION OVERVIEW
(VIDEO)
Trainer: Play video
SLIDE 6 – LIFE-THREATENING
CHEST INJURY
Respiratory distress means difficulty breathing.
The casualty is struggling to get air in or out or their
breathing is ineffective.
This can result from blunt or penetrating injury.
TCCC CLS SPEAKER NOTES #TCCC-CLS-14-01 25 JAN 20
COMBAT LIFESAVER TACTICAL COMBAT CASUALTY CARE (TCCC)
SPEAKER NOTES
SLIDE 7 – LIFE-THREATENING
CHEST INJURY
While it may be easy to see a gunshot wound or
shrapnel wound to the chest, it is important to
evaluate casualties for additional injuries, such as
bruising, swelling, or other deformities of the chest
not normally seen without removing the clothing.
These injuries may be signs of future life-threatening
respiration issues.
SLIDE 8 – IDENTIFYING TENSION
PNEUMOTHROAX
Tension pneumothorax is caused by significant torso
(chest) trauma or a blast injury resulting in severe
and progressive respiratory distress.
SLIDE 9 – IDENTIFYING SIGNS AND
SYMPTOMS OF OPEN
PNEUMOTHORAX IN TFC
With an open pneumothorax, also called a sucking
chest wound, air enters the pleural space around the
lung through a wound in the chest wall.
The elastic lung deflates and pulls away from the
chest wall. On inspiration, the air now enters the
chest THROUGH THE HOLE instead of INTO THE
LUNGS through the normal airways of the mouth and nose. As a result, the affected lung cannot be fully
re-inflated by inhalation.
It usually takes a hole in the chest the size of a nickel or bigger for a sucking chest wound to occur.
Not all chest wounds are sucking chest wounds; some do not penetrate as deeply as the lung cavity.
TCCC CLS SPEAKER NOTES #TCCC-CLS-14-01 25 JAN 20
COMBAT LIFESAVER TACTICAL COMBAT CASUALTY CARE (TCCC)
SPEAKER NOTES
SLIDE 10 and SLIDE 11 – VENTED AND
NONVENTED CHEST SEALS
Get to know the supplies within your JFAK and CLS
kit. Vented chest seals are preferred.
Penetrating chest wounds (open or sucking chest
wounds) are treated by applying a chest seal.
Once a wound has been occluded with a chest seal,
air can no longer enter (or exit) the pleural space
through the wound in the chest wall.
The injured lung will remain partially collapsed, but
the mechanics of respiration will be better.
Continue to monitor the casualty after treatment with a chest seal. If the casualty condition worsens, a
tension pneumothorax should be suspected.
Burping or removing the dressing may help; otherwise, a needle decompression of the chest may be
needed.
SLIDE 12 – POSITIONING AFTER
TREATMENT
If the casualty is unconscious, place the casualty in
the recovery position. If conscious, allow the
casualty to adopt the sitting position if that makes
breathing more comfortable.
SLIDE 13 – TREATMENT OF OPEN
PNEUMOTHORAX WITH CHEST SEAL
(VIDEO)
Trainer: Play video
TCCC CLS SPEAKER NOTES #TCCC-CLS-14-01 25 JAN 20
COMBAT LIFESAVER TACTICAL COMBAT CASUALTY CARE (TCCC)
SPEAKER NOTES
SLIDE 14 – SKILL STATION
At this time we will break into skill stations to practice
the following skills:
• Chest seal
SLIDE 15 – TENSION PNEUMOTHORAX IN
TACTICAL FIELD CARE
As a tension pneumothorax develops, air enters
the chest cavity through the wound with every
inspiration, but doesn’t leave with expiration and is
trapped.
Every breath adds more air to the air space inside
the rib cage and outside the lung, and the pressure
inside the chest builds up.
Injured lung tissue acts as a one-way valve, trapping
more and more air between the lung and the chest wall.
Pressure builds up and can potentially compress both lungs and the heart.
Both lung function and heart function are impaired with a tension pneumothorax, causing respiratory
distress and shock. The elevated air pressure OUTSIDE the collapsed lung in a tension pneumothorax
can impair the function of both lungs and the heart by preventing them from expanding normally. This
CAN kill the casualty.
SLIDE 16 – CONSIDER TENSION
PNEUMOTHORAX IN TACTICAL FIELD
CARE
Signs of tension pneumothorax include early and
late signs.
The early signs to look for are:
1. Increased difficulty breathing
2. Rapid or shallow breathing (like being out of
breath and not able to take a full breath)
3. Anxiety
4. Agitation
5. Apprehension
6. Decreased level of consciousness or unconsciousness
TCCC CLS SPEAKER NOTES #TCCC-CLS-14-01 25 JAN 20
COMBAT LIFESAVER TACTICAL COMBAT CASUALTY CARE (TCCC)
SPEAKER NOTES
The late signs may not be displayed or may be displayed only when the casualty’s condition has
worsened. Late signs that indicate progression of tension pneumothorax include neck veins protruding
(distended); tracheal deviation (a shift of the windpipe to the right or left).
These signs may be difficult to assess in a combat situation. You must be alert to the possibility of
tension pneumothorax whenever a casualty has a penetrating or other chest wound. Therefore, the sole
criterion for suspecting a tension pneumothorax is a chest wound with increasing respiratory difficulty.
It is important to evaluate casualties during TFC for early and late signs of tension pneumothorax. Like
bleeding control, tension pneumothorax is treatable. Left untreated, a tension pneumothorax can cause
severe respiratory distress, shock, and death.
The treatment is to let the air trapped under pressure escape by inserting a needle into the chest.
After initial treatment by CLS, both types of chest injuries (sucking chest wounds and tension
pneumothorax) will require advanced evaluation by medical personnel and evacuation.
SLIDE 17 – UNSUCCESSFUL
TREATMENT OR RECURANCE OF
TENSION PNEUMOTHORAX
If initial treatment of tension pneumothorax with
NDC is unsuccessful or if symptoms recur after
successful treatment, a second NDC should be
attempted.
If no improvement is noted after the second NDC,
proceed with circulation assessment and treatment following the MARCH protocol.
SLIDE 18 – TREATMENT OF TENSION
PNEUMOTHORAX
The treatment is to let the air trapped under pressure
escape by inserting a needle into the chest. This is
called Needle Decompression of the Chest (NDC).
The device used for NDC is a catheter-over-needle
device that is found in the JFAK.
NDC can be performed at either the space between
the second and third ribs on the front of the chest (away from the middle of the chest outside the nipple
line to avoid the heart) or on the side of the chest between the fifth and sixth ribs.
• Use a 14-gauge or 10-gauge 3¼” needle catheter
• Two options for NDC sites
o 2nd intercostal space on mid-clavicular line
o 5th intercostal space on the anterior axillary line
• Watch needle placement to avoid the heart and arteries
• Clean the area
• Place the needle perpendicular to body
• Hold in place for 5–10 seconds before removing needle and leaving catheter
• Document all interventions on the DD Form 1380
TCCC CLS SPEAKER NOTES #TCCC-CLS-14-01 25 JAN 20
COMBAT LIFESAVER TACTICAL COMBAT CASUALTY CARE (TCCC)
SPEAKER NOTES
SLIDE 19 – POSITIONING AFTER
TREATMENT
If the casualty is unconscious, place in the recovery
position. If conscious, allow the casualty to adopt the
sitting position if that makes breathing more comfortable.
SLIDE 20 – NEEDLE DECOMPRESSION
OF THE CHEST (NDC) (VIDEO)
Trainer: Play video
SLIDE 21 – SKILL STATION
At this time, we will break into skill stations to practice
the following skills:
• Needle Decompression of Chest
TCCC CLS SPEAKER NOTES #TCCC-CLS-14-01 25 JAN 20
COMBAT LIFESAVER TACTICAL COMBAT CASUALTY CARE (TCCC)
SPEAKER NOTES
SLIDE 22 – SUMMARY
In this module, we discussed respiration assessment
and management in TFC. We identified the signs and
symptoms of an open pneumothorax and of a tension
pneumothorax, as well as how to treat both. We
emphasized that tension pneumothorax is a
preventable cause of death. We also reinforced the
need for medical personnel to provide advanced
evaluation of these types of chest injuries, along with
the need for evacuation.
SLIDE 23 – CHECK ON LEARNING
Ask questions of the learners, referring to key
concepts from the module.
Now for a check on learning.
1. What is a tension pneumothorax?
- As a tension pneumothorax develops, air
enters the chest cavity through the wound
with every inspiration, but doesn’t leave
with expiration and is trapped, so every
breath adds more air to the air space
inside the rib cage and outside the lung, and the pressure inside the chest builds up and
causes the lung to collapse. Injured lung tissue acts as a one-way valve, trapping more and
more air between the lung and the chest wall. Pressure builds up and compresses both lungs
and the heart.
2. How should you treat an open chest wound?
- Treat open chest wounds by applying a vented chest seal completely over the wound during
expiration.
3. What should you do if you suspect a casualty has a tension pneumothorax?
- If a chest seal is in place, burp the seal. If there is no improvement after burping the seal
perform a needle decompression of the chest.
SLIDE 24 – QUESTIONS
TCCC CLS SPEAKER NOTES #TCCC-CLS-14-01 25 JAN 20
You might also like
- How To Make Your Own Voodoo DollsDocument4 pagesHow To Make Your Own Voodoo DollsJohn Willey100% (2)
- C15 Engine: Electrical Circuit DiagramDocument12 pagesC15 Engine: Electrical Circuit DiagramPhil B.100% (1)
- Tactical Combat Casualty Care November 2009Document262 pagesTactical Combat Casualty Care November 2009samatnadgob0036100% (1)
- 03C Tactical Field Care 100219Document262 pages03C Tactical Field Care 100219Jeremy McKinney100% (2)
- JRNL-Responding To Trauma Your Priorities in The First HourDocument8 pagesJRNL-Responding To Trauma Your Priorities in The First HourArs MoriendiNo ratings yet
- Cardiac Arrest and CPRDocument76 pagesCardiac Arrest and CPRDevi Yulianti100% (2)
- Redbook - ASSESSMENT AND MANAGEMENT OF TRAUMA PDFDocument323 pagesRedbook - ASSESSMENT AND MANAGEMENT OF TRAUMA PDFrizka100% (1)
- ATLS Case ScenarioDocument13 pagesATLS Case ScenarioJenny Schneider100% (2)
- Mathematics Stage 7 Sample Paper 1Document14 pagesMathematics Stage 7 Sample Paper 1Gideon Eka Dirgantara50% (2)
- Primary Care in Trauma PatientDocument109 pagesPrimary Care in Trauma PatientSumit AgarwalNo ratings yet
- PolytraumaDocument41 pagesPolytraumaFrederick Mars UntalanNo ratings yet
- Polytrauma: DR A.R.Baka Department of Surgery Federal Medical Center, YolaDocument57 pagesPolytrauma: DR A.R.Baka Department of Surgery Federal Medical Center, YolaAbuhafezbaka100% (1)
- BlastingDocument138 pagesBlastingcklconNo ratings yet
- 200+ TOP RADIOLOGY Online Quiz Questions - Exam Test 2023Document24 pages200+ TOP RADIOLOGY Online Quiz Questions - Exam Test 2023Ayub Alam100% (1)
- CP System For BulletsDocument37 pagesCP System For BulletsAnonymous TBAzJ8Ejd100% (1)
- Trauma OverviewDocument48 pagesTrauma OverviewFrancescoBarbero100% (1)
- Strategies For HarvestDocument86 pagesStrategies For HarvestBeka AsraNo ratings yet
- DV TUD Brochure 2015v2-SecuredDocument16 pagesDV TUD Brochure 2015v2-SecuredJR RZNo ratings yet
- The Space RaceDocument15 pagesThe Space RaceRadu Petrusan100% (1)
- Fabrication of 2 X 1000 MT Capacity Mounded LPG Storage VesselsDocument84 pagesFabrication of 2 X 1000 MT Capacity Mounded LPG Storage VesselsMilan DjumicNo ratings yet
- Basic Life SupportDocument46 pagesBasic Life SupportRuruni Kenchin Batusai50% (2)
- Principles and Application of Tactical Field Care (TFC) : TCCC Tier 4 TCCC Tier 1 TCCC Tier 3Document17 pagesPrinciples and Application of Tactical Field Care (TFC) : TCCC Tier 4 TCCC Tier 1 TCCC Tier 3Sae TumNo ratings yet
- 1007 BLSDocument25 pages1007 BLSZainescu DanNo ratings yet
- Tactical Combat Casualty Care August 2011Document299 pagesTactical Combat Casualty Care August 2011Jared A. Lang100% (1)
- Module 07 - Airway Management in TFC: Speaker NotesDocument7 pagesModule 07 - Airway Management in TFC: Speaker NotesSae TumNo ratings yet
- Module 03 - Care Under Fire: Speaker NotesDocument12 pagesModule 03 - Care Under Fire: Speaker NotesSae TumNo ratings yet
- Module 08: Respiration Assessment and Management: TCCC Tier 4 TCCC Tier 1 TCCC Tier 3Document24 pagesModule 08: Respiration Assessment and Management: TCCC Tier 4 TCCC Tier 1 TCCC Tier 3Luis-alfredo Perez Bolde HernandezNo ratings yet
- Module 01 - SpeakerDocument9 pagesModule 01 - SpeakerRoger RonconiNo ratings yet
- US Army Medical Course MD0569-200 - Chest and Airway ProblemsDocument55 pagesUS Army Medical Course MD0569-200 - Chest and Airway ProblemsGeorgesNo ratings yet
- Asm Course Speaker NotesDocument15 pagesAsm Course Speaker NotesJesse RobertNo ratings yet
- Module 02 - Medical Equipment: Speaker NotesDocument7 pagesModule 02 - Medical Equipment: Speaker NotesDERIL PRASETYONo ratings yet
- Module 02 - Medical Equipment: Speaker NotesDocument7 pagesModule 02 - Medical Equipment: Speaker NotesDERIL PRASETYONo ratings yet
- Emergency Anaesthetic Management To Extensive Thoracic Trauma-Hossam AtefDocument60 pagesEmergency Anaesthetic Management To Extensive Thoracic Trauma-Hossam AtefHossam atefNo ratings yet
- Airway Management in TFC: Skill InstructionsDocument8 pagesAirway Management in TFC: Skill InstructionsSae TumNo ratings yet
- TCCC Cls Didactics Mod 05 - 30 Jun 20Document31 pagesTCCC Cls Didactics Mod 05 - 30 Jun 20Giovanni RossiNo ratings yet
- Water Seal Drainage (WSD) : Entri-Entri BerikutnyaDocument7 pagesWater Seal Drainage (WSD) : Entri-Entri BerikutnyaputridwierlindaNo ratings yet
- Water Seal Drainage (WSD) : Entri-Entri BerikutnyaDocument12 pagesWater Seal Drainage (WSD) : Entri-Entri BerikutnyaputridwierlindaNo ratings yet
- Flail Chest ReportDocument4 pagesFlail Chest ReportMiggsNo ratings yet
- What Are The Ten New Commandments in Severe Polytrauma Management 1Document8 pagesWhat Are The Ten New Commandments in Severe Polytrauma Management 1antonio dengNo ratings yet
- 7 - Airway Management in TFCDocument18 pages7 - Airway Management in TFCCarlos MaravilhaNo ratings yet
- Trauma I - Abcs of Trauma Triage and TransportDocument16 pagesTrauma I - Abcs of Trauma Triage and TransportSamNo ratings yet
- Tactical Combat Casualty Care: SPC OwensDocument31 pagesTactical Combat Casualty Care: SPC OwenstashonowensNo ratings yet
- Lessonplan FinDocument14 pagesLessonplan Finx483xDNo ratings yet
- Module 14 - Analgesia and Antibiotic Administration: Speaker NotesDocument5 pagesModule 14 - Analgesia and Antibiotic Administration: Speaker NotesSae TumNo ratings yet
- DR Anil Kumar Assistant Professor Department of Surgical Disciplines All India Institute of Medical SciencesDocument39 pagesDR Anil Kumar Assistant Professor Department of Surgical Disciplines All India Institute of Medical SciencesRiry AmbarsaryNo ratings yet
- Module 04 - Principles and Application of TFC: Speaker NotesDocument7 pagesModule 04 - Principles and Application of TFC: Speaker NotesSae Tum100% (1)
- Trauma and Blast InjuriesDocument22 pagesTrauma and Blast InjuriesHafiz Mahruzza100% (1)
- Chest Trauma: DR - Amr BastawaisiDocument10 pagesChest Trauma: DR - Amr BastawaisiBara FakhryNo ratings yet
- Chest TraumaDocument14 pagesChest TraumaMary Rose BatagaNo ratings yet
- Airway 1Document6 pagesAirway 1Ilyes FerenczNo ratings yet
- Tension PneumothoraxDocument19 pagesTension PneumothoraxRupita SitanggangNo ratings yet
- European Course Trauma CareDocument7 pagesEuropean Course Trauma CareYaclinNo ratings yet
- Management of Chest InjuriesDocument13 pagesManagement of Chest Injuriesana9filimonNo ratings yet
- Blunt Chest TraumaDocument10 pagesBlunt Chest TraumaFortune RubengoNo ratings yet
- Treatment of Thoracic Trauma Lessons From The BatDocument5 pagesTreatment of Thoracic Trauma Lessons From The Batchou youNo ratings yet
- Learning Material 1 Adult CPRDocument10 pagesLearning Material 1 Adult CPR3B ABAN, Daryl Lloyd G.No ratings yet
- Emergency Anaesthetic Management of Extensive Thoracic TraumaDocument7 pagesEmergency Anaesthetic Management of Extensive Thoracic TraumaYoz MpNo ratings yet
- Thoracic TraumaDocument13 pagesThoracic TraumaTony DawaNo ratings yet
- Final Chest Tube CareDocument46 pagesFinal Chest Tube Careوجد عمرNo ratings yet
- Chest Tubes, Pneumonectomy, Lobectomy, PleuralDocument40 pagesChest Tubes, Pneumonectomy, Lobectomy, PleuralMuhammad AliNo ratings yet
- Anesthesia For Thoracic Trauma - OpenAnesthesiaDocument7 pagesAnesthesia For Thoracic Trauma - OpenAnesthesiaReddyNo ratings yet
- ACLS Practice QuizDocument29 pagesACLS Practice Quizezzat salemNo ratings yet
- IntroductionDocument5 pagesIntroductionFarhan YulmiadiNo ratings yet
- ER JournalDocument7 pagesER JournalGab LandazabalNo ratings yet
- KGDDocument7 pagesKGDjihyunyeeNo ratings yet
- Final Chest Tube CareDocument46 pagesFinal Chest Tube Careوجد عمرNo ratings yet
- Go To:: Respiratory ImpairmentDocument18 pagesGo To:: Respiratory ImpairmentNanik LestariNo ratings yet
- 010303A TCCC-MP Tactical Field Care #1 IG 160603Document43 pages010303A TCCC-MP Tactical Field Care #1 IG 160603herralainNo ratings yet
- TraumaDocument12 pagesTraumagibreilNo ratings yet
- Complications of Percutaneous Coronary Intervention: The Survival HandbookFrom EverandComplications of Percutaneous Coronary Intervention: The Survival HandbookAlistair LindsayNo ratings yet
- Monitoring Mechanical Ventilation Using Ventilator WaveformsFrom EverandMonitoring Mechanical Ventilation Using Ventilator WaveformsNo ratings yet
- One-Person Bag Valve Mask (BVM) : MarchDocument1 pageOne-Person Bag Valve Mask (BVM) : MarchSae TumNo ratings yet
- Skills Assessment Checklist: MODULE 11: Hypothermia PreventionDocument2 pagesSkills Assessment Checklist: MODULE 11: Hypothermia PreventionSae TumNo ratings yet
- Principles and Application of Tactical Field Care (TFC) : Skill InstructionsDocument3 pagesPrinciples and Application of Tactical Field Care (TFC) : Skill InstructionsSae TumNo ratings yet
- Head-Tilt/Chin-Lift: DO NOT Use If A Spinal or Neck Injury Is SuspectedDocument1 pageHead-Tilt/Chin-Lift: DO NOT Use If A Spinal or Neck Injury Is SuspectedSae TumNo ratings yet
- Skills Assessment Checklist: MODULE 14: Pain Medication and Antibiotic AdministrationDocument2 pagesSkills Assessment Checklist: MODULE 14: Pain Medication and Antibiotic AdministrationSae TumNo ratings yet
- Principles and Application of Tactical Field Care (TFC) : Skill InstructionsDocument3 pagesPrinciples and Application of Tactical Field Care (TFC) : Skill InstructionsSae TumNo ratings yet
- Atbf Ista PDFDocument12 pagesAtbf Ista PDFSae TumNo ratings yet
- One-Person Drag/Carry: Kit or Arm DragDocument5 pagesOne-Person Drag/Carry: Kit or Arm DragSae TumNo ratings yet
- Skills Assessment Checklist: MODULE 19: Pre-Evacuation Procedures, Communication, and DocumentationDocument3 pagesSkills Assessment Checklist: MODULE 19: Pre-Evacuation Procedures, Communication, and DocumentationSae TumNo ratings yet
- Atbf PDFDocument1 pageAtbf PDFSae TumNo ratings yet
- Two-Person Drag/Carry: Kit or Arm DragDocument3 pagesTwo-Person Drag/Carry: Kit or Arm DragSae TumNo ratings yet
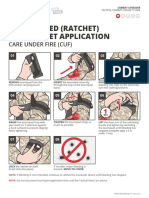
- One-Handed (Ratchet) Tourniquet Application: Care Under Fire (Cuf)Document1 pageOne-Handed (Ratchet) Tourniquet Application: Care Under Fire (Cuf)Sae TumNo ratings yet
- Skills Assessment Checklist: MODULE 11: Hypothermia PreventionDocument2 pagesSkills Assessment Checklist: MODULE 11: Hypothermia PreventionSae TumNo ratings yet
- Skills Assessment Checklist: MODULE 7: Airway ManagementDocument6 pagesSkills Assessment Checklist: MODULE 7: Airway ManagementSae TumNo ratings yet
- Skills Assessment Checklist: MODULE 4: Principles and Application of Tactical Field CareDocument1 pageSkills Assessment Checklist: MODULE 4: Principles and Application of Tactical Field CareSae TumNo ratings yet
- Skills Assessment Checklist: MODULE 6: Massive Hemorrhage Control in TFCDocument7 pagesSkills Assessment Checklist: MODULE 6: Massive Hemorrhage Control in TFCSae TumNo ratings yet
- Module 14 - Analgesia and Antibiotic Administration: Speaker NotesDocument5 pagesModule 14 - Analgesia and Antibiotic Administration: Speaker NotesSae TumNo ratings yet
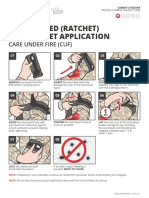
- Two-Handed (Ratchet) Tourniquet Application: Care Under Fire (Cuf)Document1 pageTwo-Handed (Ratchet) Tourniquet Application: Care Under Fire (Cuf)Sae TumNo ratings yet
- Analgesia Administration/ Antibiotic Admin: Skill InstructionsDocument3 pagesAnalgesia Administration/ Antibiotic Admin: Skill InstructionsSae TumNo ratings yet
- Evacuation Procedures: Skill InstructionsDocument3 pagesEvacuation Procedures: Skill InstructionsSae TumNo ratings yet
- Eye Injuries: Skill InstructionsDocument3 pagesEye Injuries: Skill InstructionsSae TumNo ratings yet
- Massive Hemorrhage Control in TFC: Skill InstructionsDocument8 pagesMassive Hemorrhage Control in TFC: Skill InstructionsSae TumNo ratings yet
- Principles and Application of Tactical Field Care (TFC) : TCCC Tier 4 TCCC Tier 1 TCCC Tier 3Document17 pagesPrinciples and Application of Tactical Field Care (TFC) : TCCC Tier 4 TCCC Tier 1 TCCC Tier 3Sae Tum0% (1)
- Massive Hemorrhage Control in TFC: Skill InstructionsDocument8 pagesMassive Hemorrhage Control in TFC: Skill InstructionsSae TumNo ratings yet
- Module 11 - Hypothermia Prevention: Speaker NotesDocument6 pagesModule 11 - Hypothermia Prevention: Speaker NotesSae TumNo ratings yet
- Airway Management in TFC: Skill InstructionsDocument8 pagesAirway Management in TFC: Skill InstructionsSae TumNo ratings yet
- Module 13 - Eye Injuries: Speaker NotesDocument5 pagesModule 13 - Eye Injuries: Speaker NotesSae TumNo ratings yet
- Bridge Final ProposalDocument14 pagesBridge Final ProposalDr. A B M Amrul KaishNo ratings yet
- History Taking - Cheat SheetDocument2 pagesHistory Taking - Cheat SheetANGELICA CLAIRE BARECUATRONo ratings yet
- Special Project ReportDocument9 pagesSpecial Project ReportSangam PatariNo ratings yet
- Anatomy of A FireworkDocument4 pagesAnatomy of A FireworkMuthu KumarNo ratings yet
- Chapter - I (Electrical Safety)Document30 pagesChapter - I (Electrical Safety)Hunter HarshaNo ratings yet
- Philips HTS3510 PDFDocument66 pagesPhilips HTS3510 PDFJesusNo ratings yet
- Costing of Sea Water RO Plant KPT Manora Design at 100,000 IGPD at 35,000 PPMDocument3 pagesCosting of Sea Water RO Plant KPT Manora Design at 100,000 IGPD at 35,000 PPMMohtashim KazmiNo ratings yet
- HVAC Validation 1649296351Document15 pagesHVAC Validation 1649296351jeyapragash RamadassNo ratings yet
- Bradley Sink Verge LVLD2Document4 pagesBradley Sink Verge LVLD2isaacgamezNo ratings yet
- The IMA Volumes in Mathematics and Its Applications: Avner Friedman Willard Miller, JRDocument172 pagesThe IMA Volumes in Mathematics and Its Applications: Avner Friedman Willard Miller, JRPedro PereyraNo ratings yet
- Investigation of Liquid-Liquid Phase Equilibria For Reactive Extraction of Lactic Acid With Organophosphorus SolventsDocument6 pagesInvestigation of Liquid-Liquid Phase Equilibria For Reactive Extraction of Lactic Acid With Organophosphorus Solventskudsiya firdousNo ratings yet
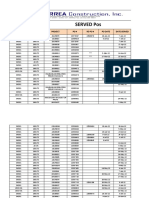
- Served POsDocument21 pagesServed POsYay DumaliNo ratings yet
- Electronic Prepayment Meter6Document4 pagesElectronic Prepayment Meter6Sumitha SudevanNo ratings yet
- Sithkop005 AnswersDocument46 pagesSithkop005 AnswersSid SharmaNo ratings yet
- English 12 Unit 1Document7 pagesEnglish 12 Unit 1Anonymous N6ccr9MVNo ratings yet
- Who Can Learn Diploma CivilDocument19 pagesWho Can Learn Diploma CivilGururaj TavildarNo ratings yet
- Study On Solar Irrigation System in BangladeshDocument61 pagesStudy On Solar Irrigation System in Bangladeshavocadocolor100% (2)
- ME-222-01 (Simple Mechanism)Document32 pagesME-222-01 (Simple Mechanism)Imran TahirNo ratings yet
- Para Jumbles Test-1Document4 pagesPara Jumbles Test-1vennelaNo ratings yet
- Ursina CollisionDocument3 pagesUrsina CollisionGilniro JúniorNo ratings yet