Professional Documents
Culture Documents
Resp - Part A - Answers
Resp - Part A - Answers
Uploaded by
SsOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Resp - Part A - Answers
Resp - Part A - Answers
Uploaded by
SsCopyright:
Available Formats
Part A: Interpretation
You are an intern on the surgical ward, about to take your first sip of water since you
arrived, when your second-favourite nurse asks you to review a 60-year-old male who
was admitted with shortness of breath. On your arrival, the patient appears drowsy and
is on 10L of oxygen via a mask. Your second-favourite nurse is already setting up a
trolley for ABG sampling.
You perform an ABG, which reveals the following results:
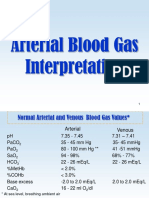
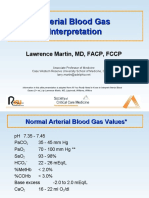
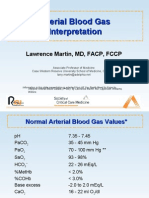
PaO2: 7.0 kPa (11-13 kPa) || 52.5 mmHg (82.5 – 97.5 mmHg)
pH: 7.29 (7.35 – 7.45)
PaCO2: 9.1 kPa (4.7 – 6.0 kPa) || 68.2 mmHg (35.2 – 45 mmHg)
HCO3–: 26 (22 – 26 mEq/L)
Base excess: +1 (-2 to +2)
QUESTION: What does the ABG show?
- O2 is low = respiratory failure – what why?
- pH is low = acidosis
- CO2 is high = respiratory acidosis
- Bicarb is within normal, as is base excess (kidneys need time to respond) hence is
acute response
- Therefore this is uncompensated
QUESTION: What type of failure does this indicate?
- Low O2 + high CO2 = Type II Respiratory Failure
QUESTION: What other signs and symptoms would you expect given the PaCO2?
- Hypercapnia is associated with
o Headache
o Confusion, drowsiness
o Reduced level of consciousness
o Asterixis
o Tachycardia
o HTN
QUESTION: What are 3 conditions that would result in this picture presented here?
- Reduced respiratory drive e.g. brain stem lesion, opiates/sedative overdose
- COPD, asthma (due to increased airway resistance)
- Neuromuscular weakness e.g. spinal cord injury, Guillain Barre syndrome, severe
fatigue
- Chest wall mechanical defects e.g. flail chest/chest trauma, severe kyphosis
- Increased dead space in lungs e.g. emphysema, PE, ARDS
- Increased CO2 load e.g. Shock, severe sepsis, malignant hyperthermia
- (endless list)
You might also like
- Goljan - Audio TranscriptsDocument296 pagesGoljan - Audio TranscriptsGurbir Singh Gill90% (30)
- Arterial Blood Gas Analysis - making it easyFrom EverandArterial Blood Gas Analysis - making it easyRating: 4.5 out of 5 stars4.5/5 (4)
- SPIROMETRYDocument5 pagesSPIROMETRYJayarubini JeyapalNo ratings yet
- PPL Exam Secrets Guide: Human Performance & LimitationsFrom EverandPPL Exam Secrets Guide: Human Performance & LimitationsRating: 4.5 out of 5 stars4.5/5 (3)
- Blood Gas Questions With Answers - 1998Document11 pagesBlood Gas Questions With Answers - 1998somarajakNo ratings yet
- 100 Clinical Cases in Medicine - PasTest - Cardiac OnlyDocument30 pages100 Clinical Cases in Medicine - PasTest - Cardiac OnlySsNo ratings yet
- Acidosis Vs AlkalosisDocument15 pagesAcidosis Vs Alkalosisdina sharafNo ratings yet
- Arterial Blood Gas InterpretationDocument65 pagesArterial Blood Gas InterpretationDaniel AryanNo ratings yet
- Paeds MCQs Part 1Document34 pagesPaeds MCQs Part 1SsNo ratings yet
- Fluid, Electrolytes, Acid Base BalanceDocument18 pagesFluid, Electrolytes, Acid Base Balanceashdmb217100% (5)
- Arterial Blood Gases: A Step by Step GuideDocument19 pagesArterial Blood Gases: A Step by Step GuideKathleen Ann50% (2)
- Ards and RF FileDocument12 pagesArds and RF FileEdwin Delos Reyes Abu100% (1)
- Respiratory FailureDocument7 pagesRespiratory FailuremuhammadridhwanNo ratings yet
- Resp InsuffDocument30 pagesResp InsuffCLEMENTNo ratings yet
- Respiratory Failure in Children PDFDocument47 pagesRespiratory Failure in Children PDFOxana TurcuNo ratings yet
- Acure Resp Failure and ARDS 1-13-2020Document37 pagesAcure Resp Failure and ARDS 1-13-2020slatcheshotmail.comNo ratings yet
- Respiratory FailureDocument8 pagesRespiratory FailureAnusha VergheseNo ratings yet
- ABG QuizDocument13 pagesABG QuizSSNo ratings yet
- ABG QuizDocument12 pagesABG QuizParsaant SinghNo ratings yet
- ABG InterpretationDocument13 pagesABG InterpretationAbid KhanNo ratings yet
- Oxygen Therapy PDFDocument36 pagesOxygen Therapy PDFStefanus LimNo ratings yet
- Respiratory Failure: Dr. Sat Sharma Univ of ManitobaDocument38 pagesRespiratory Failure: Dr. Sat Sharma Univ of ManitobaGonzalo Venegas RojasNo ratings yet
- ABG InterpretationDocument38 pagesABG Interpretationmahmod omerNo ratings yet
- Arterial Blood Gas For HODocument40 pagesArterial Blood Gas For HOansuh22No ratings yet
- Respiratory Alkalosis Metabolic Acidosis Respiratory Acidosis Metabolic AlkalosisDocument1 pageRespiratory Alkalosis Metabolic Acidosis Respiratory Acidosis Metabolic Alkalosispwarden1349No ratings yet
- Respiratory FailureDocument36 pagesRespiratory FailureMiden AlbanoNo ratings yet
- ABGs - Oxygen TherapyDocument4 pagesABGs - Oxygen TherapyPebblesNo ratings yet
- Critical Care Alterations in RespiratoryDocument96 pagesCritical Care Alterations in RespiratoryNatukunda DianahNo ratings yet
- Oxygen Therapy: Dr. Subhankar ChatterjeeDocument49 pagesOxygen Therapy: Dr. Subhankar ChatterjeesubhankarNo ratings yet
- Interpretation of Arterial Blood Gases and Acid-Base DisordersDocument44 pagesInterpretation of Arterial Blood Gases and Acid-Base DisordersSuren VishvanathNo ratings yet
- ABG Interpretation and Respiratory FailureDocument1 pageABG Interpretation and Respiratory FailureLeonNo ratings yet
- AbgDocument66 pagesAbgIan OrwaNo ratings yet
- Respiratory FailureDocument39 pagesRespiratory FailureMuntasir BashirNo ratings yet
- ABG Interpretation: DR Omer Elgaili Yousif ElhagDocument43 pagesABG Interpretation: DR Omer Elgaili Yousif ElhagMuntasir BashirNo ratings yet
- 2 Gagal Nafas 2018Document49 pages2 Gagal Nafas 2018aliqulsafik100% (1)
- Respiratory FailureDocument5 pagesRespiratory FailureLovely Acabado Tampoco100% (1)
- Mechanism of Hypoxia and Types of Repiratory FailureDocument48 pagesMechanism of Hypoxia and Types of Repiratory FailureSiciid AliNo ratings yet
- Oxygenation and Oxygen TherapyDocument11 pagesOxygenation and Oxygen TherapyJenn77x1No ratings yet
- Interpretasi Agd Juni 2020Document34 pagesInterpretasi Agd Juni 2020Christiana TrijayantiNo ratings yet
- Arterial Blood Gas InterpretationDocument69 pagesArterial Blood Gas InterpretationostuffeNo ratings yet
- Arterial Blood Gas InterpretationDocument66 pagesArterial Blood Gas InterpretationlenafitriyaniNo ratings yet
- Respiratory FailureDocument41 pagesRespiratory FailureM HNo ratings yet
- Arterial Blood Gas InterpretationDocument66 pagesArterial Blood Gas InterpretationkabatchinoooNo ratings yet
- Resp - Part A - StemDocument1 pageResp - Part A - StemSsNo ratings yet
- Respiratory FailureDocument38 pagesRespiratory Failuredrmithil100% (1)
- ABG Examples ABG Exam Questions For Medical Students and PACESDocument10 pagesABG Examples ABG Exam Questions For Medical Students and PACES8b8xppmgpcNo ratings yet
- Cute Respiratory Failure ARF: by Baraa Zaghal Haneen Amer Inst: Mahdia AlkonyDocument18 pagesCute Respiratory Failure ARF: by Baraa Zaghal Haneen Amer Inst: Mahdia Alkonymahmoud fuqahaNo ratings yet
- Airway, Breathing & Circulation in Ews: Dr. Rumaisah Satyawati SP - An, KICDocument71 pagesAirway, Breathing & Circulation in Ews: Dr. Rumaisah Satyawati SP - An, KICNda ErdisNo ratings yet
- Respir1 EN V0Document66 pagesRespir1 EN V0Petr MarsalekNo ratings yet
- Lecture SBA BankDocument20 pagesLecture SBA Bankyecib80467No ratings yet
- Pleno B Blok 7 2012Document37 pagesPleno B Blok 7 2012illiyyahsyahabNo ratings yet
- The Acid Base Balance: Faculty of Medicine Anesthesia and Intensive Care DepartmentDocument36 pagesThe Acid Base Balance: Faculty of Medicine Anesthesia and Intensive Care DepartmentCamelia A. ParuschiNo ratings yet
- Veterinary Clinics: Respiratory Acidosis: A Quick ReferenceDocument4 pagesVeterinary Clinics: Respiratory Acidosis: A Quick ReferenceAndersonValentimOliveiradaSilvaNo ratings yet
- Arterial Blood Gas AnalysisDocument23 pagesArterial Blood Gas AnalysisVartika SainiNo ratings yet
- Plasma University: Guriel-Galgadud RegionDocument17 pagesPlasma University: Guriel-Galgadud RegionDr AbdulkadirNo ratings yet
- Biochemical Case 1Document2 pagesBiochemical Case 1Affie SaikolNo ratings yet
- Acidosis and Alkalosis EnjoyableDocument15 pagesAcidosis and Alkalosis Enjoyabledead remorseNo ratings yet
- Phisylogy Respiratory2 Ø Ø Ù Ù Ù Ø Ù Ù Ù ÙDocument5 pagesPhisylogy Respiratory2 Ø Ø Ù Ù Ù Ø Ù Ù Ù Ùmaisa.alsalem4No ratings yet
- (RS) Pneumonia With Severe HypoxiaDocument4 pages(RS) Pneumonia With Severe Hypoxiaapi-3769252100% (2)
- Respiratory Monitoring in Mechanical Ventilation: Techniques and ApplicationsFrom EverandRespiratory Monitoring in Mechanical Ventilation: Techniques and ApplicationsJian-Xin ZhouNo ratings yet
- Cytochrome P450 2D6 Known Drug Interaction Chart: Drugs Metabolized by CYP2D6 Enzyme Drug Inhibitors of CYP2D6 EnzymeDocument1 pageCytochrome P450 2D6 Known Drug Interaction Chart: Drugs Metabolized by CYP2D6 Enzyme Drug Inhibitors of CYP2D6 EnzymeSsNo ratings yet
- Case 1Document2 pagesCase 1SsNo ratings yet
- Resp - Part A - StemDocument1 pageResp - Part A - StemSsNo ratings yet
- Type I (Polymicrobial - Anaerobes and Aerobes) Usually Older Adults And/orDocument6 pagesType I (Polymicrobial - Anaerobes and Aerobes) Usually Older Adults And/orSsNo ratings yet
- Bonus Paeds MCQs With ExplanationsDocument17 pagesBonus Paeds MCQs With ExplanationsSsNo ratings yet
- Antibiotics - FosfomycinDocument2 pagesAntibiotics - FosfomycinSsNo ratings yet
- Fosfomycin: Mode of Action IndicationsDocument2 pagesFosfomycin: Mode of Action IndicationsSsNo ratings yet