Professional Documents
Culture Documents
1143 1412657144 PDF
1143 1412657144 PDF
Uploaded by
Widyawati HestiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
1143 1412657144 PDF
1143 1412657144 PDF
Uploaded by
Widyawati HestiCopyright:
Available Formats
Healing of Tooth Extraction Socket
Dr. Shilpa Khullar Dr. Mittal A. Dr. Pankaj Datta
Professor Professor & H.O.D. Principal & H.O.D.
Dept. of Prosthodontics Dept. of Conservative Dentistry Dept. of Prosthodontics
Inderprastha Dental College & Hospital, Sahibabad, Ghaziabad UP.
Abstract as: response to growth, injury, or biome-chanical
B one is a highly organized
composite material that consists
of organic matrix and inorganic
mineral substances. It serves as depository for
calcium, phosphates, and other minerals and
1. Compact /Cortical bone
2. Spongy / Cancellous bone
Compact Bone : Consists of lamellae or
layers of cells, and a matrix made of inorganic
and organic components. The cells present
adaptation. Compared to mature bone, it has
relatively low mineral content, a more
random fibre orientation and minimal
strength3.
Lamellar Bone (Fig 2)
firm skeletal support for soft of the human are called osteocytes; they are located in It is the principal load bearing tissue of
body. lacunae and have cell processes for nutrient the adult skeleton. It is formed relatively
Introduction diffusion within small channels or canaliculi. slowly (0.6 µm/day) and mineralizes by a
During bone healing, the ph changes at The matrix component or osteoid is primary and secondary mechanism4. Full
the site of the injury. Bleeding, local changes approximately 40% by weight and consists of maturation of lamellar bone requires 6-12
in pressure and edema follow injury. Some Type 1 collagen, gylcosa-minoglycans and months.
cells burst, spilling toxins into the adhesive protein, osteonectin. The inorganic Bundle Bone
surrounding area, and certain bioelectric and component is also 40% by weight and It is a special kind of woven bone that can
biochemical phenomena are known to occur. consists of hydroxyapatite, the apatite crystal be found in the zones of attachment of
In response to these and other factors, of calcium and phosphate. Compact bone has tendons, ligaments or joint capsules if
pluripotential cells, marrow cells, and cells outer circumferential lamellae, inner mineralized bone is penetrated by collagen
lining the periosteum and endothelium act as circumferential lamellae, haversian lamellae, fibres. This has striations that are extensions
sources of fibroblasts, osteoblasts and and interstitial lamellae, which account for of Sharpey's fibres and is similar to lamellar
osteoclasts. Within 48 hours, a clot is the hardness and density of this bone.It is bone in strength. It is characteristic of fibro-
organized and the fibroblasts begin to lay covered by periosteum and has collagen osseous attachments and would be expected
down threadlike collagen fibres. Meanwhile, fibres, osteoblasts, and osteoclasts. in a stable fibro-osseous attachment.5
blood-borne cells continue to lyse and Periosteum is attached tightly to the bone Composite Bone
remove debris. With circulation partially surface by Sharpey's fibres and serves as This is formed on cortical surfaces during
interrupted, bone cells at the osteotomy can protection for bone. Osteoblasts and wound healing, growth, and biomechanical
lose vitality. This dead skeletal tissue can act Osteoclasts in periosteum are involved with adaptation. Intially, a porous lattice of woven
as scaffolding, and collagen fibres fill in remodeling, bone resorption and apposition. bone captures blood vessels along a periosteal
around the implant and walls of the Spongy / Cancellous Bone : Within or endosteal surface. This lattice then fills
osteotomy. The dead bone is slowly replaced compact bone, spongy bone has a three with load-bearing, lamellar bone. Lamellar
and the regions including the collagen fibres dimmesional network called bone trabeculae. compaction of composite bone is an
gradually ossify. Thus as old bone is Spongy bone architecture is cavernous and important step in achieving a load bearing
removed; new bone regenerates in its place less dense such that the hardness is less when osseous interface.6
around the implant.1 compared to compact bone. The bone Physiologic Adaptation of Bone
Biology of Bone trabeculae configuration creates a large To fulfill its dual functional role of
Bone is a highly organized composite surface area for an abundance of osteoblasts support and metabolism, bone responds to a
material that consists of organic matrix and and osteoclasts, which are associated with complex array of mechanical, bioelectric,
inorganic mineral substances. It serves as bone formation and resorption. Large blood metabolic and local mediators like cytokines
depository for calcium, phosphates, and other vessels transverse within bone trabeculae.2 and growth factors.Under steady-state
minerals and firm skeletal support for soft of microscopically; depending on the age, conditions, osteoblast differentiation is
the human body.The fundamental principle of function and systemic factors, bone can be mechanically mediated and is stress-strain
bone architecture in humans, is that compact classified into 4 types: dependant.7Surgical placement of a dental
and cancellous structures are distributed 1. Woven Bone implant elicits an osteogenic response which
within the skeleton in such a fashion that they 2. Lamellar Bone is vascularity dependant.
can best sustain mechanical loads, thus 3. Bundle Bone Modeling of Bone (Fig 3)
reflecting the loading conditions in all three 4. Composite Bone It is a surface-specific activity,
dimensions. Woven (embryonic) Bone (Fig 1) (apposition or resorption ) that produces a net
Bone Morphology This is a highly cellular osseous tissue change in the size and/or shape of bone. It is
Macroscopically bone can be classified that is formed rapidly (30-50 µm/ day) in an uncoupled process, meaning that cell
Heal Talk / May-June 2012 / Volume 04 / Issue 05 37
Khullar, et al. : Healing of Tooth Extraction Socket
activation (A) proceeds independently to within the system. In case of implant socket have thickened and now occupy about
bone formation (F) or resorption (R). It refers placement sites, occlusal force stimulus and two thirds of the original socket volume. The
to a generalized change in overall dimensions general health management are both secondary spongiosa of the next stage begins
of a bone's cortex or spongiosa, hence a important to optimal bone remodeling to develop. In areas where sinusoids are still
mechanism of differential growth and criteria.10 evident, new bone forms.
structural adaptation.It is a fundamental Stages of Healing 5. Bone reorganization Stage (Fig. 8D)
mechanism of growth, atrophy, and The progression of osseous healing after This stage occurs 6 weeks after tooth
reorientation. tooth extraction is nearly equivalent to that extraction. Primary spongiosa reorganize into
Remodeling of Bone (Fig 3 & Fig 4) observed for usual wound healing in the an irregular and larger framework as
Remodeling is defined as turnover or following sequential manner. secondary spongiosa, again starting at or near
internal restructuring of previously existing 1. Granulation stage the base of the socket extending upwardly.
bone. It is a couled tissue level phenomenon. 2. Initial angiogenic/neurovascular stage Prerequisites for Optimal Bone Healing
Remodeling, bone resorption and appostion 3. New bone formation stage Response
helps maintain blood calcium levels and does 4. Bone growth stage The vascularization and bone formation
not change the mass quantity of bone. In 5. Bone reorganization stage that follow implant insertion require the
spongy bone, remodeling occurs on the 1. The Granulation Stage (Fig. 6, Fig. 7) presence of following factors to promote
surface of bone trabeculae due to the The granulation stage extends for 5 days healing:
abundance of osteoblasts and osteoclasts from the time of extraction. Early granulation 1. Adequate Cells
available, which get stimulated by the tissue is observed at the base of the socket, 2. Nutritional elements
occlusal forces applied to the spongy bone. extending crestally along the socket wall. A 3. Required signal stimuli.
This stimulation causes bone cells to blood clot occupies the central portion of the Summary
differentiate into osteoclasts involved in bone socket. The earliest angiogenesis observed is Primary bone healing occurs at a fracture
resorption and osteoprogenitor cells to sprouting or budding extensions of the site with a clean break. The sites are
differentiate into osteoblasts involved in bone preexisting blood vessels sinusoidal positioned by pressed fixation or closely
formation. The same phenomenon occurs in capillaries developing from broken ends of approximated. In primary bone healing, there
compact bone at the remodeling site. blood vessels in the remains of the is well-organized bone formation with
Remodeling includes localized changes in periodontal ligament at the cribriform plate. minimal granulation tissue formation.
individual osteons or trabeculae: turnover, This angiogenesis starts at the base of the Secondary healing occurs where a large
hypertrophy, atrophy, or reorientation. socket where thick, strong trabeculae already defect or large fracture site precludes close
Remodeling Cycle/ Sigma Cycle ( 17 wks) exist and along with their accompanying approximation of the two sites. In contrast to
(Table 1) (Fig 5) cappiliary plexes. This is the area at the socket primary bone healing, secondary bone
Since remodeling of bone is a coupled base which is injured the least during tooth healing may have granulation tissue
tissue phenomenon, the following stages removal and maintains its vascular pattern formation.
occur; intact, is the most active area initially. References
1. Activation Phase (A): Stimulus to the 2. Initial Angiogenic / Neurovascu- 1. Babbush: Implant Dentistry: a long term survey and
comparative study with fixed bridgework, J Oral
bone causes circulating preosteoclast cells to larization Stage Implantol 7: 1, 1977.
cross the blood vessel wall, enter the This period extends for 1 week from the 2. Bloom and Fawcett, DW: A textbook of histology.
connective tissue and form osteoclasts. The time of extraction. The blood clot becomes Philadelphia: W.B. Saunders, Co, pp 245-287, 1975
osteoprogenitor cells differentiate into smaller. The new sinusoids extending along 3. Roberts WE, Smith RK, Zilberman Y, Mozsary PG,
Smith RS. Osseous adaptation to continuous loading
osteoblasts from the paravascular connective the socket wall form the base move beyond of rigid endosseous implants. Am J Orthod 1984;86:
tissue cells.In this phase of hours to days the the height of the clot, until about two thirds of 95-111
osteoclasts form the cutting head. the socket is filled with newly formed 4. Roberts WE, Gonsalves MR: Aging of bone tissue.
In: Holm PedersenP, Loe H, eds. Geriatric dentistry .
2. Resorption Phase (R): The sinusoids. At the base of the socket, the first Copenhagen: Munksgaard, 1986; 83-93
osteoclasts result in active resorption at the new bone trabeculae may be observed (Fig 5. James RA. Tissue behavior in the environment
remodeling site and results in gradual 8A). produced by permucosal dental devices. In:
decrease in bone density. During this phase, 3. New Bone Formation Stage McKinney Jr RV, eds. The dental implant.
Littleton,MA: PSG Publishing Co. Inc, 1985; 58:175
the cutting cone opens a cavity of 120 to This occurs 2 weeks form the time of 6. Roberts We, Turley PK, Brezniak N. Bone
180µm in diameter. Once this phase is extraction. Now the entire socket is filled physiology and metabolism. J Calif Dent Assoc
complete it is followed by the with granulation tissue replete with newly 1987;15(10): 54-61
7. Roberts WE, Morey ER,: Proliferation and
3. Quiescence or Reversal Phase (Q): formed sinusoids. The bony wall of the base differentiation sequence of osteoblast histogenesis
Here the quiescent stage of osteoblasts and the side of the socket presents a dense under physiologic considerations in rat periodontal
changes into an active stage. There is lattice of trabeculae (Fig 8B). There is ligament, Am J Anat174:105-118,1985
reversal of bone resorption stage into a bone intimate interrelationship between immature 8. Heimke, Schulte: The influence of fine surface
structures on the osseointegration of implants. Int J
deposition stage as there is a cessation of sinusoids exhibiting anastomosis and new Artif Organs, 5: 207-212, 1982
osteoclastic activity and beginning of bone. No new bone trabeculae are observed in 9. Schroeder : The reactions of bone, connective tissue
oesteoblastic bone formation, resulting into areas of nonanastomosing sinusoids of blind and epithelium to endosteal implants with titanium-
sprayed surfaces. J Maxillofacial Surg, 9: 15-25,
the next stage of ; ends of sinusoids. Woven bone is delineated 1981
4. Formation Phase (F): Active by incompletely ossified trabeculae. Bone 10. Albrektsson T: Direct bone anchorage of dental
Osteoblasts produce proteins for collagen trabeculae formation is governed by the implants. J Prosthet Dent, 50: 255-261, 1983.
formation which is a step in bone formation. expansion and location of sinusoids. This Legends
The duration of the A→R→Q→F activity reaches its peak in the 2nd week Fig. 1: Woven bone at sites of intremambrenous bone
formation. Osteoblasts produce the
remodeling cycle, also called the sigma cycle following tooth extraction and bone nonmenirelized bone matrix osteoid, which is
is about 6 weeks in rabbits and 17 weeks in development becomes rapid. later mineralized (dark blue)
humans.To maintain a constant level of bone 4. Bone Growth Stage (Fig 8C) Fig. 2: Lamellar bone formation. Osteoblasts lay down
new lamellar bone onto previously resorbed
remodeling, there should be local This occurs 4-5 weeks following tooth mature lamellar bone during bone remodeling.
stimulation8,9 as well as crucial levels of extraction. Additional trabeculae are Newly formed lamellar bone is more intensely
thyroid hormone, calcitonin and vitamin D deposited, and the base and the walls of the stained (dark purple) than the preexisting bone
(bright purple)
38 Heal Talk / May-June 2012 / Volume 04 / Issue 05
Khullar, et al. : Healing of Tooth Extraction Socket
Fig. 3: This schematic drawing of diaphyseal (From Roberts WE, Garetto LP, DeCastro RH: : mechanism of cortical bone remodeling.
(midshaft) cross-section reveals differential J Indiana Dent Assoc 68:19, 1989) (Roberts WE et al: Am J Orthod 86:95, 1984)
sites of bone modeling (M) and remodeling (R). Fig. 4: Remodeling of newly formed woven bone into Fig. 6 :
Remodeling is turnover of previously existing mature lamellar bone. Osteoblasts first form Fig. 7 :
bone. Modeling (change in shape or form) can woven bone, which starts growing from the Fig. 8 A.
be anabolic (formation) or catabolic edges of local bone Fig. 8 B
(resorption). Bone modeling is mechanism of Fig. 5: Schematic drawing of cutting/filling cone Fig. 8C;
differential growth and structural adaption. (evolving secondary osteon) demonstrates Fig. 8D:
Fig. 1 Fig. 2 Fig. 3 Fig. 4 Fig. 5
Fig. 6 Fig. 7 Fig. 8A Fig. 8B Fig. 8C Fig. 8D
asia edition
ISSN : 2278-1161 UPDENT
1
UPENG/2011/41591
1
2012
A Journal of Clinical Dentistry
updent@gmail.com
Avulsion
Silent Features
by Dr. Parul Verma
Do not Scrub the Tooth
Transport in a Medium
HBSS
Immed
Poster Latest Trends
iate
R ep
l
an
ta
tio To the dental office
Fresh
n
Cold Milk
eplantation
Latest Articles Dental News
e R
Bee
iat
Propolis
Total Displacement of the
ed
Tooth out of its socket
m
Im
no
If Coconut Water
ORS
Patient’s
Saliva
Clinical Tips
Saline
Emdogain
Heal Talk A Journal of Clinical Dentistry
Media 14
A Journal of Clinical Dentistry
Heal Talk / May-June 2012 / Volume 04 / Issue 05 39
You might also like
- Radiographic Pathology For Technologists 6th Edition Kowalczyk Test BankDocument6 pagesRadiographic Pathology For Technologists 6th Edition Kowalczyk Test Bankbeatrixkhuyen9rm100% (29)
- Anatomy and Physiology CH 1 To 3 Flash CardsDocument14 pagesAnatomy and Physiology CH 1 To 3 Flash Cardsmalenya1100% (1)
- MCQ Oral Histology (Textbook)Document33 pagesMCQ Oral Histology (Textbook)Magnet Shot100% (5)
- Anatomical Landmarks of Maxillary and Mandibular CastDocument73 pagesAnatomical Landmarks of Maxillary and Mandibular Castvarsha ammu80% (5)
- Anatomy & Physiology CH 17 Marieb & Hoehn LectureDocument148 pagesAnatomy & Physiology CH 17 Marieb & Hoehn LectureCocoa Doogle100% (2)
- Bone and Bone Graft HealingDocument12 pagesBone and Bone Graft HealingJayanth PerumalNo ratings yet
- AN OVERVIEW OF BONE CELLS AND THEIR REGULATING FACTORS OF DIFFERENTIATION, Mohamed 2008Document9 pagesAN OVERVIEW OF BONE CELLS AND THEIR REGULATING FACTORS OF DIFFERENTIATION, Mohamed 2008Faizal Reza PahleviNo ratings yet
- Biomechanics and Biomaterials in Orthopedic SurgeryDocument11 pagesBiomechanics and Biomaterials in Orthopedic SurgeryManiventhan NachimuthuNo ratings yet
- Principles of Bone GraftingDocument6 pagesPrinciples of Bone GraftingJayanth Perumal100% (2)
- Maxillary Sinus Bone GraftingDocument181 pagesMaxillary Sinus Bone GraftingTuấn Hành TrầnNo ratings yet
- Chemistry Project On Estimation of Contant of Bone Ash PDFDocument9 pagesChemistry Project On Estimation of Contant of Bone Ash PDFPooja BhagwatNo ratings yet
- Maxilary Sinus Graft ArunDocument181 pagesMaxilary Sinus Graft ArunJose Fernando Fragozo MendozaNo ratings yet
- Capitulo Do Livro Bone BiologyDocument15 pagesCapitulo Do Livro Bone BiologyLuiz Guilherme FiorinNo ratings yet
- Obs-13 240122 184549Document51 pagesObs-13 240122 184549Edison MesacheNo ratings yet
- Biología Celular Metabolismo OseoDocument12 pagesBiología Celular Metabolismo Oseoandreaelisa17No ratings yet
- Lecture Activities No. 6 Skeletal System: Guide Questions AnswersDocument13 pagesLecture Activities No. 6 Skeletal System: Guide Questions AnswersPrancheska Abigayle Peneyra SantiagoNo ratings yet
- Biology of Tooth Movement - Ortho / Orthodontic Courses by Indian Dental AcademyDocument62 pagesBiology of Tooth Movement - Ortho / Orthodontic Courses by Indian Dental Academyindian dental academyNo ratings yet
- English 20.05.2020Document100 pagesEnglish 20.05.2020Bernythefly axcNo ratings yet
- Physiological Bases of Bone Regeneration II. The Remodeling ProcessDocument7 pagesPhysiological Bases of Bone Regeneration II. The Remodeling ProcessNelly Solange TamayoNo ratings yet
- Effect of The Nano/microscale Structure of Biomaterial Scaffolds On Bone RegenerationDocument15 pagesEffect of The Nano/microscale Structure of Biomaterial Scaffolds On Bone RegenerationjmanuelNo ratings yet
- Bone Grafts and Their SubstitutesDocument4 pagesBone Grafts and Their SubstitutesIndriastuti SoetomoNo ratings yet
- Biology of Normal Bone Remodeling 2017Document5 pagesBiology of Normal Bone Remodeling 2017Amani FezaiNo ratings yet
- Biology of Tooth MovementDocument16 pagesBiology of Tooth MovementLanaNo ratings yet
- Biology of Orthodontic Tooth MovementDocument16 pagesBiology of Orthodontic Tooth MovementGowri ShankarNo ratings yet
- Chemistry Project On Estimation of Content of Bone AshDocument13 pagesChemistry Project On Estimation of Content of Bone AshShlok Sah50% (2)
- Skeletal System ReviewerDocument19 pagesSkeletal System ReviewerChloe Mikaela MonsantoNo ratings yet
- Osteoblasts, Osteoclasts, and Osteocytes: Unveiling Their Intimate-Associated Responses To Applied Orthodontic ForcesDocument12 pagesOsteoblasts, Osteoclasts, and Osteocytes: Unveiling Their Intimate-Associated Responses To Applied Orthodontic ForcesMariya NazimNo ratings yet
- Bone Injury and Fracture Healing Biology: ArticleDocument16 pagesBone Injury and Fracture Healing Biology: Articleali amerNo ratings yet
- Bones As A Living Dynamic TissueDocument13 pagesBones As A Living Dynamic TissueSanish Basnet100% (1)
- Pathophysiology and Treatment of Osteoporosis: Challenges For Clinical Practice in Older PeopleDocument15 pagesPathophysiology and Treatment of Osteoporosis: Challenges For Clinical Practice in Older PeopleDeddy ZulkarnaenNo ratings yet
- Normal Bone Anatomy and PhysiologyDocument9 pagesNormal Bone Anatomy and PhysiologyindrapratisthaNo ratings yet
- Chemistry Project On Estimation of Content of Bone AshDocument18 pagesChemistry Project On Estimation of Content of Bone AshKim TaesiNo ratings yet
- ChemistryDocument29 pagesChemistryIshkruti WaghmareNo ratings yet
- 06 KnightDocument5 pages06 Knightcristina ArraisNo ratings yet
- Bone Regeneration Molecular and Cellular InteractionsDocument17 pagesBone Regeneration Molecular and Cellular InteractionsRuben Aquino MartinezNo ratings yet
- A Brief Introduction Into Orthopaedic ImplantsDocument20 pagesA Brief Introduction Into Orthopaedic ImplantsLuisAngelPonceTorresNo ratings yet
- Tereos - Structure of PresentationDocument72 pagesTereos - Structure of PresentationSumitNo ratings yet
- HHS Public Access: The Potential of Probiotics As A Therapy For OsteoporosisDocument26 pagesHHS Public Access: The Potential of Probiotics As A Therapy For OsteoporosisBagastyoNo ratings yet
- BONE (Histology)Document65 pagesBONE (Histology)fhfebriiNo ratings yet
- Bone Remodelling: Scientific SectionDocument7 pagesBone Remodelling: Scientific SectionRohini TondaNo ratings yet
- Bone RegenereationDocument15 pagesBone Regenereationhayet debbichNo ratings yet
- Role of RANKL-RANK-osteoprotegerinDocument7 pagesRole of RANKL-RANK-osteoprotegerinsebastian BarrigaNo ratings yet
- Bone Ash Estimation of Content of Bone Ash Project Submitted by PrashanthDocument3 pagesBone Ash Estimation of Content of Bone Ash Project Submitted by PrashanthHarsh Kumar0% (3)
- Alveolarbone Graftingand Reconstruction Procedurespriorto ImplantplacementDocument10 pagesAlveolarbone Graftingand Reconstruction Procedurespriorto ImplantplacementKranti PrajapatiNo ratings yet
- BP MecanismDocument14 pagesBP MecanismAdryana StefyNo ratings yet
- (ANA) - Online ActivityDocument4 pages(ANA) - Online ActivityJomari ManalansanNo ratings yet
- t3 Som 2014 2Document14 pagest3 Som 2014 2Julio AbarzuaNo ratings yet
- Arnett, T.Document10 pagesArnett, T.Alex AmorimNo ratings yet
- Factors of Bone Resorption of The Residual Ridge Ortman1962Document12 pagesFactors of Bone Resorption of The Residual Ridge Ortman1962AbdelKhalek BouararaNo ratings yet
- Bones: Defination: Bone Is Highly Vascular, Living, Constantly ChangingDocument21 pagesBones: Defination: Bone Is Highly Vascular, Living, Constantly ChangingMd Ahsanuzzaman PinkuNo ratings yet
- Zhu 2021Document31 pagesZhu 2021Nazmi ZegarraNo ratings yet
- Basic of Bone GraftingDocument29 pagesBasic of Bone GraftingdoctorniravNo ratings yet
- Session #14 SAS - AnaPhy (Lab)Document8 pagesSession #14 SAS - AnaPhy (Lab)G INo ratings yet
- Aaid Joi D 17 00053Document11 pagesAaid Joi D 17 00053Yun De LinNo ratings yet
- Teaching Series BoneDocument26 pagesTeaching Series BoneNAND KUMARNo ratings yet
- Bone Physiology DR NzauDocument84 pagesBone Physiology DR NzauNzau MuangeNo ratings yet
- 1.1 Bone Function: 2 OsteoarchaeologyDocument5 pages1.1 Bone Function: 2 OsteoarchaeologyKeila MenaNo ratings yet
- Basic Bone BiologyDocument3 pagesBasic Bone BiologyRuxandra Maria100% (1)
- General Anatomy: 1. SupportDocument4 pagesGeneral Anatomy: 1. SupportNu Ri LeeNo ratings yet
- Advances in Biology of Orthodontic Tooth Movement - A ReviewDocument10 pagesAdvances in Biology of Orthodontic Tooth Movement - A ReviewMarwan AlareqiNo ratings yet
- 6 PATHO 3b Part 1 - Musculoskeletal IIA - Dr. Dy-LedesmaDocument12 pages6 PATHO 3b Part 1 - Musculoskeletal IIA - Dr. Dy-LedesmaBanana BananaNo ratings yet
- Kenkre Bassett 2018 The Bone Remodelling CycleDocument20 pagesKenkre Bassett 2018 The Bone Remodelling Cyclealealer2708No ratings yet
- Normal Bone Anatomy and PhysiologyDocument9 pagesNormal Bone Anatomy and PhysiologyElsa GonçalvesNo ratings yet
- Bone Remodeling Process: Mechanics, Biology, and Numerical ModelingFrom EverandBone Remodeling Process: Mechanics, Biology, and Numerical ModelingNo ratings yet
- Advanced farriery knowledge: A study guide and AWCF theory course companionFrom EverandAdvanced farriery knowledge: A study guide and AWCF theory course companionNo ratings yet
- Hayek DKKDocument7 pagesHayek DKKwatidinaNo ratings yet
- A Conservative Technique For Repairing Class IV Composite RestorationsDocument6 pagesA Conservative Technique For Repairing Class IV Composite RestorationswatidinaNo ratings yet
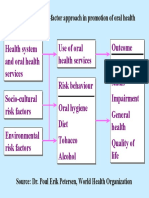
- Figure 5: The Risk-Factor Approach in Promotion of Oral HealthDocument1 pageFigure 5: The Risk-Factor Approach in Promotion of Oral HealthwatidinaNo ratings yet
- Soal 3Document5 pagesSoal 3watidinaNo ratings yet
- Kanagalingam2015 PDFDocument10 pagesKanagalingam2015 PDFwatidinaNo ratings yet
- Antiseptics in The Era of Bacterial Resistance A Focus On Povidone IodineDocument14 pagesAntiseptics in The Era of Bacterial Resistance A Focus On Povidone IodinewatidinaNo ratings yet
- Scanned With CamscannerDocument7 pagesScanned With CamscannerwatidinaNo ratings yet
- A Brief Study On Catharanthus Roseus: A Review: Anti-Microbial ActivityDocument5 pagesA Brief Study On Catharanthus Roseus: A Review: Anti-Microbial ActivitywatidinaNo ratings yet
- A Brief Study On Catharanthus Roseus: A Review: Anti-Microbial ActivityDocument5 pagesA Brief Study On Catharanthus Roseus: A Review: Anti-Microbial ActivitywatidinaNo ratings yet
- Prevention and Control of Noncommunicable DiseasesDocument3 pagesPrevention and Control of Noncommunicable DiseaseswatidinaNo ratings yet
- 2 2 15 923 PDFDocument4 pages2 2 15 923 PDFwatidina100% (1)
- Daftar PustakaDocument1 pageDaftar PustakawatidinaNo ratings yet
- GBRI WELL AP Exam Prep Study Guide Unlocked PDFDocument150 pagesGBRI WELL AP Exam Prep Study Guide Unlocked PDFAngelo Mar MallariNo ratings yet
- Organ System WorksheetDocument23 pagesOrgan System Worksheetsrisuhartini0% (1)
- Bams AllxcfgxfDocument104 pagesBams AllxcfgxfRaheel Bhai0% (1)
- Science7 Q2 Week3 LAS2Document1 pageScience7 Q2 Week3 LAS2Irish Beth Tambo-onNo ratings yet
- Table No.1A Work Done Ground Section of Tooth (L.S, T.S) S. No. Date Title SignatureDocument38 pagesTable No.1A Work Done Ground Section of Tooth (L.S, T.S) S. No. Date Title SignatureSmila Mahajan NangiaNo ratings yet
- (11.10) Imaging of The Endocrine System (TG1-CG14) Final VersionDocument12 pages(11.10) Imaging of The Endocrine System (TG1-CG14) Final VersionLANCE GILL TolentinoNo ratings yet
- Biology Notes For O LevelsDocument13 pagesBiology Notes For O Levelstahira mujahidNo ratings yet
- Case Study RevisedDocument8 pagesCase Study RevisedKjetil Rossignol100% (1)
- Haematology: Normal Sequence of Development of Cells of Haematopoietic SystemDocument71 pagesHaematology: Normal Sequence of Development of Cells of Haematopoietic SystemMaxamed AadanNo ratings yet
- Body Systems PuzzleDocument6 pagesBody Systems PuzzleNenita AlonzoNo ratings yet
- Cell Analogy ProjectDocument3 pagesCell Analogy ProjectAP - 10KG 732763 John Fraser SSNo ratings yet
- 6 B&B CirrhosisDocument30 pages6 B&B CirrhosisSara Joseph100% (1)
- Htaa Pathology Handbook 2018Document252 pagesHtaa Pathology Handbook 2018OTOH RAYA OMARNo ratings yet
- HydraDocument6 pagesHydraMishti2100% (2)
- Coronary Artery Disease - Case StudyDocument19 pagesCoronary Artery Disease - Case StudyJulieteeySarania100% (3)
- Chapter 13 - Cranial Nerve ReviewDocument14 pagesChapter 13 - Cranial Nerve ReviewCiprian HronaNo ratings yet
- Human ReproductionDocument2 pagesHuman ReproductionGrace KatjiovaNo ratings yet
- Iliac Crest: From Wikipedia, The Free EncyclopediaDocument4 pagesIliac Crest: From Wikipedia, The Free EncyclopediaMarigold CortezNo ratings yet
- Anatomy & Physiology: Chapter 7: Skeletal SystemDocument25 pagesAnatomy & Physiology: Chapter 7: Skeletal SystemDarandy CruzNo ratings yet
- Short Note Biology Form 5-Chapter 3 Coordination and ResponseDocument6 pagesShort Note Biology Form 5-Chapter 3 Coordination and Responsesalamah_sabri75% (4)
- Cancers: Cell Origins of High-Grade Serous Ovarian CancerDocument28 pagesCancers: Cell Origins of High-Grade Serous Ovarian CancerAlfonso AnggriawanNo ratings yet
- MCQ in Orl CourseDocument46 pagesMCQ in Orl CoursesulnaikNo ratings yet
- Clinics in Sports Medicine PDFDocument173 pagesClinics in Sports Medicine PDFmostafa143941366No ratings yet
- Yellow Green Blue and Red Handwritten Zones of Regulation SEL Social and Emotional Learning Education PresentationDocument15 pagesYellow Green Blue and Red Handwritten Zones of Regulation SEL Social and Emotional Learning Education PresentationAngel ChrisleneNo ratings yet
- Lesson Plan: Preliminary DetailsDocument7 pagesLesson Plan: Preliminary DetailsMurali SambhuNo ratings yet