Professional Documents
Culture Documents
Split-Thickness Skin Excision in Severe Open Fractures: The Bone & Joint Journal February 1988
Uploaded by
IntanPermataWijayaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Split-Thickness Skin Excision in Severe Open Fractures: The Bone & Joint Journal February 1988
Uploaded by
IntanPermataWijayaCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/19817368
Split-thickness skin excision in severe open fractures
Article in The Bone & Joint Journal · February 1988
DOI: 10.1302/0301-620X.70B1.3339053 · Source: PubMed
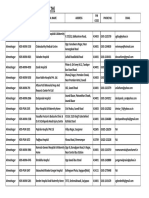
CITATIONS READS
18 437
6 authors, including:
Rami Mosheiff David Segal
Hadassah Medical Center Hadassah Medical Center
143 PUBLICATIONS 2,394 CITATIONS 83 PUBLICATIONS 1,335 CITATIONS
SEE PROFILE SEE PROFILE
Some of the authors of this publication are also working on these related projects:
local antibiotic delivery in orthopedic conditions View project
Polio hip fractures View project
All content following this page was uploaded by David Segal on 14 May 2016.
The user has requested enhancement of the downloaded file.
SPLIT-THICKNESS SKIN EXCISION IN
SEVERE OPEN FRACFURES
I. ZIV, A. ZELIGOWSKI, R. MOSHEIFF, J. LOWE, M. R. WEXLER, D. SEGAL
From the Hadassah University Hospital and the Hebrew University Medical School, Jerusalem
Split-thickness skin excision can be used as a one-stage procedure for the accurate diagnosis of flap
viability and the immediate freatment friction-avulsion of
injuries in severe open fractures. After cleaning the
wound, the avulsed flap is temporarily sutured back to its original bed and a split thickness graft is taken from
it and meshed to a 1 :3 ratio.Surface dermal capillary bleeding then serves as an indicator of viability, clearly
displaying a line for the excision of devascularised skin and correlating well with a concomitant fluorescein
test. The wounds are re-opened and, after fixation of the fracture, the viable part of the flap is returned to its
original bed and the remaining defects are covered with the meshed graft.
We have treated 16 patients with extensive degloving injuries in this way, 15 needing only the single
surgical procedure. All retained flaps survived, noother donor sites were needed and the split-thickness grafts
took with 90% to 100% success.
Open fractures associated with friction-avulsion of the TECHNIQUE OF OPERATION
soft tissues are very severe injuries and have a high
complication rate (Gustilo and Anderson 1976; Byrd, At operation culture swabs are taken of all wounds which
Cierny and Tebbetts 1981 ; Byrd, Spicer and Cierny are then copiously irrigated with saline and subjected to
1985). Torsional and compressive forces may separate meticulous debridement. Avulsed flaps are then sutured
and tear the skin, muscles and neurovascular structures back in their original anatomical position, using inverted
from their underlying bed (MacCollum 1938; Entin intradermal sutures (Zeligowski and Ziv 1987). The
1955; Prendiville and Lewis 1955). The result is partial fluorescein test is performed and the borders of
devascularisation of skin and muscle flaps. devascularisation are marked with methylene blue and
Awareness of the importance of the viability of pinprick tattooing. A split-thickness skin excision
these residual flaps and their preservation increased after (STSE) is used to take a graft from the entire flap (Fig. 1).
McGrouther and Sully (1980) had recommended the use On the flap surface, dermal capillary bleeding indicates
of the fluorescein test (McCraw, Myers and Shanklin the viable part of the flap ; this correlated well with the
1977; Kalisman et al. 1978). This test is one of the most fluorescein test. Non-bleeding devitalised areas are then
commonly used methods of determining skin viability, excised.
but its interpretation may be difficult and the dye can All the fascial compartments in the extremity are
occasionally provoke a hypersensitivity reaction decompressed by longitudinal incisions and the muscle
(McCraw et al. 1977). and neurovascular bundles are inspected. Muscle viabil-
We present a simple one-stage procedure for the ity is determined by colour, turgor, bleeding and
immediate management of the soft tissues and the open
fractures produced by friction-avulsion injury.
I. Ziv, MD, FRCS(C), Senior Orthopaedic Surgeon
A. Zeligowski, MD, Senior Plastic Surgery Resident
R. Mosheiff, MD, Assistant Resident in Orthopaedic Surgery
J. Lowe, MD, Senior Orthopaedic Surgeon
M. R. Wexler, MD, Professor of Plastic and Maxillofacial Surgery
D. Segal, MD, Professor of Orthopaedic Surgery
Hadassah University Hospital, P0 Box 12010, Jerusalem 91120, Israel.
© 1988 British Editorial Society of Bone and Joint Surgery
0301-620X/88/1008 $2.00 Technique of split-thickness skin excision on an avulsion
J Bone Joint Surg [Br] 1988;70-B:23-6. flap which has been temporarily sutured in place.
VOL. 70-B, No. I, JANUARY 1988 23
24 I. ZIV, A. ZELIGOWSKI, R. MOSHEIFF, J. LOWE, M. R. wExLER, D. SEGAL
contractility. All crushed and dead muscles are excised. ILLUSTRATIVE CASE REPORTS
Free fragments of cortical bone are removed if this does
Case 1. A 32-year-old physical education teacher suffered a severe
not jeopardise stability.
compound injury to her left leg in a motorcycle accident (Fig. 2) with an
The reparative part ofthe one-stage procedure starts open fracture of the lateral femoral condyle and a complete tear of the
with fracture reduction. Fractures are stabilised by quadriceps. Four hours after admission, cleaning and debridement
external and internal fixation using inter-fragmentary were performed, the wounds were temporarily sutured and STSE was
carried out (Figs 3 and 4) followed by excision of all non-viable skin.
compression screws to hold fragments in continuity and
Loose bone fragments were removed from the knee and the quadriceps
buttressing the reduction with an external fixator.
was repaired. All compartments of the lower leg were decompressed
Available viable muscles are rotated or transposed to and the remaining open wounds were covered with meshed skin graft
cover denuded bone. The remaining viable skin flaps are (Fig. 5). Continuous passive movement was started, using a range of
then defatted and sutured back into position under movement that avoided tension on the quadriceps repair. At 10 days,
all the wounds had healed primarily. Three weeks after the injury the
minimal tension. The split-thickness skin graft, taken
patient was discharged home with an active range of knee movement
from the degloved flaps, is meshed (1 :3) and used as graft from 0#{176}
to 70#{176}.
Six weeks postoperatively she could straight-leg raise
to cover all the remaining exposed areas. The grafts are with 20#{176}
extensor lag and flex to 95 (Figs 6 and 7).
secured by peripheral sutures or clips ; petroleum gauze Case 2. A 21-year-old man presented with a severe open fracture of the
and wet cotton fluffs are applied to improve the skin left humerus and a complete radial nerve palsy, after his arm had been
caught between machine rollers (Fig. 8). Some large bone fragments
graft moulding. The limb is then immobilised, using
were brought separately in a plastic bag. There were two main skin
plaster splints as necessary.
flaps, proximal and distal, and the proximal one had a large hole at its
Postoperatively, the extremity is elevated. base (Fig. 9).
Intravenous cephalosporines are given during the oper- At operation the wounds were thoroughly irrigated, cleaned and
ation and for an additional 10 days. The wounds are temporarily sutured ; STSE was then performed. In this case the viable
flap was shown to be larger than that indicated by the fluorescein test.
inspected on the third postoperative day. If any
The radial nerve ends were trimmed, transposed anteriorly and
additional skin graft is needed, this is applied in the ward repaired without tension. The humerus was shortened by 1 cm, the free
under aseptic conditions, using remnants of the original bony fragments being autoclaved and replaced. Inter-fragmentary
harvest which have been preserved in a refrigerator. compression screws and an external fixator were used (Fig. 10). Parts of
Case 1. Figure 2 - Severe open injury with
circumferential degloving, except for a narrow
posterior bridge. Figure 3 - The flaps have been
sutured to their original bed. Figure 4 - The
lateral side of the thigh and leg after the STSE.
Note the non-bleeding skin of the proximal
thigh flap and the anterior knee and leg flaps.
Figure 5 - Leg after debridement and repair,
the excision of avascular skin and the applica-
tion of meshed skin graft.
Fig. 2
Fig. 3 Fig. 4 Fig. 5
Fig. 6 Fig. 7
Case I . Range of movement six weeks after the injury.
THE JOURNAL OF BONE AND JOINT SURGERY
SPLIT-THICKNESS SKIN EXCISION IN SEVERE OPEN FRACTURES 25
Case 2. Radiograph and operative view of open comminuted Figure 10 - Post-reduction radiograph. Figure 11 - Appearance at three
midshaft fracture of the humerus. The proximal skin flap was months.
avulsed from more than two-thirds of the circumference of the
arm.
the triceps and biceps muscles were transposed to cover the fracture. was applied over the exposed muscles (Fig. 1 5). The skin graft took well
The viable parts ofthe flaps were sutured to the surrounding soft tissues and the wounds healed uneventfully.
and the meshed graft applied to complete the skin cover. Postoperative Other cases. Another 14 severe open fractures in I 3 patients have been
healing was satisfactory and the skin graft took well with no further treated by this technique. Twelve fractures were ofType III or Type IV
flap necrosis. The patient was discharged two weeks after admission (Gustilo and Anderson 1976; Byrd et al. 1981) and two were degloving
and was able to use his hand with a dynamic extension splint. The amputations, one below the elbow and one at the hip. In all the
external fixator was removed six weeks after operation. Three months patients, the avulsion flaps involved more than two-thirds of the limb
after the injury the brachioradialis and supinator muscles were circumference, and all the wounds were over 10 cm in length. Two
functioning (Fig. 1 1). Delayed union at the proximal part of the children had unstable open pelvic fractures with severe perineal
segmental fracture needed a late intra-medullary fixation, but healed in injuries, but the majority were leg fractures caused by motor-vehicle
seven months. accidents.
Case 3. A 27-year-old man was hit by a car and sustained a very severe Patients’ ages were from 2 to 56 years (mean 1 7.8 years) and they
open fracture of the left tibia and fibula (Figs 12 and 13). After have been followed up for an average of 9.3 months, with prospective
irrigation and debridement, reduction was secured with multiple inter- documentation. In seven of these patients the STSE test was compared
fragmentary screws and an external fixator (Fig. 14). The wound edges to the fluorescein test. In three cases STSE helped to preserve flaps by
were approximated for the STSE by which skin graft was harvested. 3 cm more than indicated by fluorescein. In general the devascularised
Soleus muscle was transposed to cover the fracture and meshed graft area varied between 25% and 50% of the surface area of the degloved
Radiograph and photograph of an open fracture of the left tibia and Postoperative radiograph and photograph. Meshed skin graft is
fibula. One large fragment still has a muscle pedicle. covering the transposed muscles. Dermal bleeding can be seen at the
donor site on the anterior flap.
VOL. 70-B, No. I, JANUARY 1988
26 I. ZIV, A. ZELIGOWSKI, R. MOSHEIFF, J. LOWE, M. R. WEXLER, D. SEGAL
flaps. In one patient only, some necrotic flap edges appeared five days thickness or split-thickness skin. The full-thickness graft
after operation. The area was small enough to allow bedside excision gave better cosmetic results but prevented drainage and
and grafting with spare meshed skin. One patient with severe crushing
created haematomata. Haematoma-induced necrosis is
of the foot developed a superficial Pseudomonas infection ; this healed
after appropriate antibiotic therapy and the bedside application of
believed to be mediated by free-radical mechanisms
more skin grafts. No other complications of soft tissue healing were (Angel et al. 1986). In contrast, meshed split skin grafts
seen in any of the other patients, and uneventful healing occurred prevent haematoma formation and act as an excellent
within 7 to 14 days. Only one patient required more than the single biological dressing.
procedure in the operating theatre on admission.
The venous drainage of a flap is frequently
disturbed in severe avulsion injuries and we feel that
DISCUSSION
split-thickness skin excision may assist in decongesting
The treatment of severe open fractures is difficult and the flap, thereby improving its cellular blood supply by
complicated ; we report the use of a one-stage soft-tissue decreasing the resistance in its microcirculation.
procedure which was successful in 16 consecutive cases. Conclusions. One-stage split-thickness skin excision is an
Damage to the blood supply of the fractured bone and adjunct to the fluorescein test for the immediate soft-
the surrounding soft tissue correlates well with complica- tissue management of friction-avulsion injuries associat-
tions such as non-union and infection (Gustilo and ed with severe open fractures. The accurate delineation
Anderson 1976, Byrd et al. 1985), and it is well of avascular areas requires that it be performed early
recognised that necrotic tissues should be widely excised. after admission. The technique is simple. Split-thickness
Yet without adequate soft-tissue cover bony healing is skin is excised from the entire flap after it has been
impaired. In friction-avulsion injuries large flaps of soft sutured to its original or anatomical bed (Zeligowski and
tissue are often partially viable. Total flap excision Ziv 1987)and the freshly excised grafts are meshed I :3
(Kudsk, Sheldon and Walton 1981) should be avoided; and used as biological dressings. Inspection of the donor
the viable parts of the skin flaps should be preserved sites was a reliable technique for the diagnosis of flap
because they provide good cover for muscle and bone. viability, allowing accurate excision with maximal
The need for the early detection of avascularity led preservation of tissue. Both healing and rehabilitation
to the fluorescein test (McCraw et al. 1977; McGrouther were faster, reducing the average stay in hospital.
and Sully 1980). Both papers reported similar results with
fluorescein and the marginal bleeding test, but admitted
that there could be up to 3 cm difference between the REFERENCES
original fluorescein line and the actual margin of
devascularisation. The inexperienced surgeon may not Angel MF, Narayanan K, Swartz WM, et al. The etiologic role of free
radicals in hematoma-induced flap necrosis. Plast Reconstr Surg
recognise that mottled fluorescent areas will survive l986;77 :795-801.
(Kudsk et al. 1981 ; Byrd et al. 1985). Bruises may give Byrd HS, Cierny G ill, Tebbetts JB. The management of open tibial
areas which fluoresce poorly but remain viable. Fluores- fractures with associated soft-tissue loss : external pin fixation with
early flap coverage. Plast Reconstr Surg I 98 1 :68:73-9.
cein itself may produce vomiting, nausea and an
Byrd HS, Spicer TE, Cierney C Ill. Management of open tibial
anaphylactoid reaction (McGrouther and Sully 1980). fractures. Plast Reconstr Surg 1985:76:719-28.
Split thickness skin excision is a commonly prac- Entin MA. Roller and wringer injuries : clinical and experimental
ticed technique. When it is applied to avulsed flaps, it studies. P/ast Reconstr Surg 1955:15:290-312.
produces sharp delineation between bleeding and non- Fantone JC, Ward PA. Review article : role of oxygen-derived free
radicals and metabolites in leukocyte-dependent inflammatory
bleeding dermis. Skin excision along this line of reactions. Am J Patho/ 1982;107:397-4l8.
demarcation permits the preservation of the maximum GuMBo RB, Anderson JT. Prevention of infection in the treatment of
amount of viable skin. Meshed split skin from the whole one thousand and twenty-five open fractures of long bones:
retrospective and prospective analysis. J Bone Joint Surg [Am]
of the flaps frequently provides enough graft, and no 1976;58-A :453-8.
other donorsite is required. Kalisman M, Wexier MR, Yeschua R, Neuman Z. Treatment of
It is important that flap excision be performed early. extensive avulsions of skin and subcutaneous tissues. J Dermatol
Surg Oncol 1978;4:322-7.
Revascularisation of skin flaps caused by friction-
Kudsk KA, Sheldon GF, Walton RL. Degloving injuries of the
avulsion is almost impossible because of the paucity of
extremities and torso. J Trauma 1981 ;2l :835-9.
direct cutaneous vessels, so there is no benefit to be MacCollum DW. Wringer arm : report of 26 cases. N Engi J Med
gained by waiting (McGrouther and Sully 1980). Long- l938;218 :549-54.
standing anoxia of the margins of such a flap leads to McCraw JB, Myers B, Shanklin KD. The value of fluorescein in
predicting the viability of arterialized flaps. Plast & Reconstr Surg
increased concentrations of oxygen-derived free radicals
1977;60:7I0-9.
and to the release oflysosomal proteases. This may start a McGrouther DA, Sully L. Degloving injuries of the limbs : long-term
vicious cycle of cell membrane damage and intercellular review and management based on whole-body fluorescence. Br J
Plast Surg l980;33:9-24.
oedema that causes the necrosis to spread towards the
Prendiville JB, Lewis E. Pneumatic-tyre torsion avulsion injury. Br J
base of the flap (Fantone and Ward 1982). Kudsk et al. Surg 1955;42:582-7.
(1981) suggested excision of the whole of such a flap and Zeligowski AA, 7kv I. How to harvest skin graft from the avulsed flap in
found no difference between the results of grafting full- degloving injuries. Ann P/ast Surg l987;I9:89-90.
THE JOURNAL OF BONE AND JOINT SURGERY
View publication stats
You might also like
- A Comprehensive Guide On OsteotomyDocument3 pagesA Comprehensive Guide On OsteotomySiora SurgicalsNo ratings yet
- Managing Orthopaedics at Rittenhouse Medical CenterDocument19 pagesManaging Orthopaedics at Rittenhouse Medical CenterAnushree JainNo ratings yet
- Ankle Foot Orthosis (AFO)Document10 pagesAnkle Foot Orthosis (AFO)aienjalilNo ratings yet
- Alphamaquet 1150 Brochure en PDFDocument24 pagesAlphamaquet 1150 Brochure en PDFvictorNo ratings yet
- Centric Relation and Centric OcclusionDocument3 pagesCentric Relation and Centric OcclusionYumi Sayade DentistryNo ratings yet
- Bedsore TractionDocument8 pagesBedsore TractionDeevish N DinakarNo ratings yet
- MRCEM Intermediate SBA BlueprintDocument2 pagesMRCEM Intermediate SBA BlueprintCaisha Nivenia Moses33% (3)
- Principles of Plastic Surgery ForDocument54 pagesPrinciples of Plastic Surgery ForStevysNo ratings yet
- 6002 Trauma: American Academy of Orthopaedic SurgeonDocument55 pages6002 Trauma: American Academy of Orthopaedic SurgeonHéctor Pando SánchezNo ratings yet
- Skeletal and Skin TractionDocument16 pagesSkeletal and Skin TractionJam Corros100% (2)
- NCP - Risk For FallsDocument5 pagesNCP - Risk For FallsMae CeaesarNo ratings yet
- Hospital Management Administration Project TitlesDocument1 pageHospital Management Administration Project Titlesgvani333388% (8)
- Plastic, Reconstructive, and Cosmetic Procedures: Skin GraftsDocument7 pagesPlastic, Reconstructive, and Cosmetic Procedures: Skin GraftsRiza Angela BarazanNo ratings yet
- ABCs of Wound DebridementDocument3 pagesABCs of Wound DebridementSheril MarekNo ratings yet
- Quinlan 2006Document5 pagesQuinlan 2006Mirela CiobanescuNo ratings yet
- Negative Pressure Wound TherapyDocument5 pagesNegative Pressure Wound TherapyarfahNo ratings yet
- Traumatic Wounds of The Upper Extermity Coverage StrategiesDocument14 pagesTraumatic Wounds of The Upper Extermity Coverage Strategiessimohamed3000No ratings yet
- 2018 KLWC Hansen's RevisedDocument1 page2018 KLWC Hansen's RevisedLinda Luckstead BenskinNo ratings yet
- Aps 41 126Document7 pagesAps 41 126Kamelia SitorusNo ratings yet
- Wire Subcision For Complete Release of Depressions, Subdermal Attachments, and ScarsDocument8 pagesWire Subcision For Complete Release of Depressions, Subdermal Attachments, and ScarsLuciano AbbaNo ratings yet
- Wound: CtosureDocument8 pagesWound: CtosureAnonymous kdBDppigENo ratings yet
- Rjad 529Document3 pagesRjad 529Jefferson RuizNo ratings yet
- Reconstruction of Post Electrical Burns Scalp Defect: Case ReportDocument3 pagesReconstruction of Post Electrical Burns Scalp Defect: Case ReportFahmiNo ratings yet
- Utilizing Free Skin Grafts in The Repair of Surgical Wounds: Madalene C. Y. HengDocument11 pagesUtilizing Free Skin Grafts in The Repair of Surgical Wounds: Madalene C. Y. HengDefri ChanNo ratings yet
- Principles Flap DesignDocument4 pagesPrinciples Flap DesignhaneefmdfNo ratings yet
- Wound Debridement in The CommunityDocument7 pagesWound Debridement in The CommunityPOKJA PAPNo ratings yet
- Management of Soft Tissue Extremity Degloving Injuries With Full-Thickness Grafts Obtained From Avulsed FlapDocument28 pagesManagement of Soft Tissue Extremity Degloving Injuries With Full-Thickness Grafts Obtained From Avulsed FlapRio Mulya RihartaNo ratings yet
- Characteristics and Uses of Biologic DressingsDocument11 pagesCharacteristics and Uses of Biologic DressingsEsq. Nelson OduorNo ratings yet
- Bahan Modul 3Document4 pagesBahan Modul 3Chandrawati PramanaNo ratings yet
- Art 6Document3 pagesArt 6miguelNo ratings yet
- Reconstruction of Soft-Tissue Injury Associated With Lower Extremity FractureDocument10 pagesReconstruction of Soft-Tissue Injury Associated With Lower Extremity Fracturefabian hernandez medinaNo ratings yet
- Jurnal Reading: The Principles and Practice of Open Fracture CARE, 2018Document22 pagesJurnal Reading: The Principles and Practice of Open Fracture CARE, 2018Boy PieroNo ratings yet
- Upper Extremity Amputations and Prosthetics: Steven A. Ovadia, MD Morad Askari, MDDocument7 pagesUpper Extremity Amputations and Prosthetics: Steven A. Ovadia, MD Morad Askari, MDprovaNo ratings yet
- Z-Plasty, Skin Grafting, and Local Flaps: Take-Home MessagesDocument1 pageZ-Plasty, Skin Grafting, and Local Flaps: Take-Home MessagesKdc OuinbiloNo ratings yet
- Management of Lower Limb Trauma Open Wounds and FracturesDocument44 pagesManagement of Lower Limb Trauma Open Wounds and FracturesRumaicha ChachaNo ratings yet
- 2020-07-07 Reconstructive Ladder FlapDocument96 pages2020-07-07 Reconstructive Ladder FlapTonie AbabonNo ratings yet
- Chiou 2014Document13 pagesChiou 2014Janardana GedeNo ratings yet
- 16 - Trauma MedicineDocument17 pages16 - Trauma MedicinePeterNo ratings yet
- 1.management of Emergency Orthopaedi Dr. Ifran PDFDocument21 pages1.management of Emergency Orthopaedi Dr. Ifran PDFvandraNo ratings yet
- Vacutex - Designed For PatientsDocument4 pagesVacutex - Designed For PatientsRobin LimNo ratings yet
- PII000712269190175JDocument5 pagesPII000712269190175JJanardana GedeNo ratings yet
- Complexflexorandextensor Tendoninjuries: Matthew J. Carty,, Philip E. BlazarDocument11 pagesComplexflexorandextensor Tendoninjuries: Matthew J. Carty,, Philip E. BlazarTeja Laksana NukanaNo ratings yet
- Presentasi Traumatic Wound Management - A Comprehensive Wound Management Forum Discussion & Hands-On ModelsDocument57 pagesPresentasi Traumatic Wound Management - A Comprehensive Wound Management Forum Discussion & Hands-On ModelsDadek PradnyanaNo ratings yet
- Successful Treatment of Full Thickness Frontal Skull Bone Defect With Dermal Fat Grafting and Artificial Bone GraftsDocument5 pagesSuccessful Treatment of Full Thickness Frontal Skull Bone Defect With Dermal Fat Grafting and Artificial Bone GraftsDeevish N DinakarNo ratings yet
- Rosenwasser - Use of A Pedicled Adipose Flap As A Sling For Anterior Subcutaneous Transposition of The Ulnar NerveDocument4 pagesRosenwasser - Use of A Pedicled Adipose Flap As A Sling For Anterior Subcutaneous Transposition of The Ulnar NervedanielpohlmanNo ratings yet
- THE Results OF Plating Humeral Shaft Fractures IN Patients With Multiple InjuriesDocument4 pagesTHE Results OF Plating Humeral Shaft Fractures IN Patients With Multiple InjuriesasaloNo ratings yet
- Cyst Formtaion Post SCTGDocument6 pagesCyst Formtaion Post SCTGDr. DeeptiNo ratings yet
- Case Report: Formation of A Cyst-Like Area After A Connective Tissue Graft For Root CoverageDocument3 pagesCase Report: Formation of A Cyst-Like Area After A Connective Tissue Graft For Root CoverageDr. DeeptiNo ratings yet
- Flaps and GraftsDocument5 pagesFlaps and GraftsmaxfaxNo ratings yet
- P7.2. Soft Tissue TraumaDocument12 pagesP7.2. Soft Tissue TraumaCharles HuayraNo ratings yet
- ORTHO-Fractures - Dislocations (Dr. Gerochi)Document6 pagesORTHO-Fractures - Dislocations (Dr. Gerochi)Monique BorresNo ratings yet
- Wound Essentials 11 1 Wound Assessment Part 2 ExudateDocument5 pagesWound Essentials 11 1 Wound Assessment Part 2 ExudateAnggie Mardafira PurbaNo ratings yet
- Clinical Study: Vacuum Assisted Closure Therapy Versus Standard Wound Therapy For Open Musculoskeletal InjuriesDocument9 pagesClinical Study: Vacuum Assisted Closure Therapy Versus Standard Wound Therapy For Open Musculoskeletal InjuriesAndika FahruroziNo ratings yet
- Observation of Viable Alloskin Vs Xenoskin Grafted Onto Subcutaneous Tissue Wounds After Tangential Excision in Massive BurnsDocument10 pagesObservation of Viable Alloskin Vs Xenoskin Grafted Onto Subcutaneous Tissue Wounds After Tangential Excision in Massive BurnsAngelica SerbulNo ratings yet
- Principles of Fracture FIXDocument63 pagesPrinciples of Fracture FIXAndi NurcahyantiNo ratings yet
- Sun Et Al 2000Document4 pagesSun Et Al 2000Alex PerryNo ratings yet
- Plastic Surgery2021Document97 pagesPlastic Surgery2021Esraa SalemNo ratings yet
- Comparison of Bupivacaine Moistened Dressing and Conventional Dressing For Pain Relief On Skin Graft Donor SitesDocument4 pagesComparison of Bupivacaine Moistened Dressing and Conventional Dressing For Pain Relief On Skin Graft Donor SitesMaFe GachoNo ratings yet
- Combination of Periocular Myocutaneous Flaps For One-Stage Reconstruction of Extensive Defects of The EyelidDocument5 pagesCombination of Periocular Myocutaneous Flaps For One-Stage Reconstruction of Extensive Defects of The EyelidBrînduşa CiobanuNo ratings yet
- Skin Graft and Flap: Ibnu F Hantoro Diponegoro University Faculty of MedicineDocument11 pagesSkin Graft and Flap: Ibnu F Hantoro Diponegoro University Faculty of MedicineLuqman AlwiNo ratings yet
- Use of Dermal Regenerative Templates For BurnsDocument7 pagesUse of Dermal Regenerative Templates For BurnsJhonatan Vazquez AlbornozNo ratings yet
- Treatment of Extensive Postburn Deformities Using Extralarge Sheets of Full Thickness Skin GraftsDocument8 pagesTreatment of Extensive Postburn Deformities Using Extralarge Sheets of Full Thickness Skin GraftsIndah YulantariNo ratings yet
- Tosounidis 2021Document7 pagesTosounidis 2021HOSPITAL GENERAL DE LIBRESNo ratings yet
- Anchorage of Partial Avulsion of The Heel Pad With Use of Multiple Kirschner WiresDocument4 pagesAnchorage of Partial Avulsion of The Heel Pad With Use of Multiple Kirschner WiresPrabhjeet singhNo ratings yet
- Flap Reconstruction of The HandDocument12 pagesFlap Reconstruction of The HandMarcelo BarberoNo ratings yet
- Dekesel 2006Document9 pagesDekesel 2006kundhavai22No ratings yet
- Document PDFDocument6 pagesDocument PDFRiri AmalinaNo ratings yet
- A New Technique in The Clinical Assessment of Bums : From The Plastic Surgery Centre, St. Lawrence Hospital, ChepstowDocument5 pagesA New Technique in The Clinical Assessment of Bums : From The Plastic Surgery Centre, St. Lawrence Hospital, ChepstowgeefeezNo ratings yet
- Operative Dictations in OphthalmologyFrom EverandOperative Dictations in OphthalmologyEric D. RosenbergNo ratings yet
- Screen Shot 2022-01-23 at 23.32.Document1 pageScreen Shot 2022-01-23 at 23.32.IntanPermataWijayaNo ratings yet
- 338-Article Text-2729-2-10-20200430Document7 pages338-Article Text-2729-2-10-20200430pasid harlisaNo ratings yet
- Escharotomy CPG New FormatDocument10 pagesEscharotomy CPG New FormatmyscribeNo ratings yet
- Cleft Lip Booklet PDFDocument17 pagesCleft Lip Booklet PDFJenin NtNo ratings yet
- Medial Sural Artery Perforator Flap: 26.1 Vascular AnatomyDocument5 pagesMedial Sural Artery Perforator Flap: 26.1 Vascular AnatomyIntanPermataWijayaNo ratings yet
- Escharotomy CPG New FormatDocument10 pagesEscharotomy CPG New FormatmyscribeNo ratings yet
- Cleft Lip Booklet PDFDocument17 pagesCleft Lip Booklet PDFJenin NtNo ratings yet
- Practitioner Sample O and P Written ExamDocument4 pagesPractitioner Sample O and P Written ExamBapina Kumar RoutNo ratings yet
- File 59Document9 pagesFile 59gnanasekarNo ratings yet
- (B-0520) Operating UnitDocument48 pages(B-0520) Operating UnitAhmad Gamal Elden MAhanyNo ratings yet
- UntitledDocument1 pageUntitledfarispilotNo ratings yet
- M0003 NHLDocument497 pagesM0003 NHLUday kumarNo ratings yet
- Isobaric Ropivacaine 5mg:ML For Spinal Anesthesia.12Document5 pagesIsobaric Ropivacaine 5mg:ML For Spinal Anesthesia.12Ode No ratings yet
- Instrument Function Picture Cutting and Dissecting InstrumentsDocument10 pagesInstrument Function Picture Cutting and Dissecting InstrumentsNicole Villanueva, BSN - Level 3ANo ratings yet
- CSMA List of Approved Private Hospitals For 2018-19Document12 pagesCSMA List of Approved Private Hospitals For 2018-19m_asitNo ratings yet
- Return To Sport After Surgical Management of Posterior Shoulder InstabilityDocument13 pagesReturn To Sport After Surgical Management of Posterior Shoulder InstabilityAziz CupinNo ratings yet
- Open Staghorn Stone SurgeryDocument17 pagesOpen Staghorn Stone SurgeryHardiTariqHammaNo ratings yet
- High Definition Body Sculpting ArtDocument2 pagesHigh Definition Body Sculpting ArtmdwilliamsNo ratings yet
- 90-126-02 Angulus 2 Angled Screwdriver PDFDocument24 pages90-126-02 Angulus 2 Angled Screwdriver PDFDrGurkirpal Singh MarwahNo ratings yet
- Basic Principles Program - Twin Course v4 - FontevaDocument3 pagesBasic Principles Program - Twin Course v4 - FontevaAravind RaviNo ratings yet
- 1.the Security To Maternity Unit.: Dialog!Document2 pages1.the Security To Maternity Unit.: Dialog!elyssa indfNo ratings yet
- Dr. Mowlavi Selected To RealSelf Medical Advisory BoardDocument2 pagesDr. Mowlavi Selected To RealSelf Medical Advisory BoardPR.comNo ratings yet
- Teleflex OEM - Balloon Brochure - LRDocument4 pagesTeleflex OEM - Balloon Brochure - LRkresna_wiratma06No ratings yet
- Hospitals List: - (Tpa Vidal Health)Document81 pagesHospitals List: - (Tpa Vidal Health)UDAY GANDHINo ratings yet
- CPS PG Diploma 2018 Admission SeatsDocument24 pagesCPS PG Diploma 2018 Admission SeatsNilesh TapdiyaNo ratings yet
- Professional Meeting Reflection - GracDocument3 pagesProfessional Meeting Reflection - Gracapi-540011183No ratings yet
- 5 Mandible PDFDocument4 pages5 Mandible PDFAbhi Isi WaqtNo ratings yet
- Traumatic Disorders: Compartment SyndromeDocument57 pagesTraumatic Disorders: Compartment SyndromeMayahati NazayaNo ratings yet