Professional Documents
Culture Documents
Articles
Uploaded by
Eula Angelica OcoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Articles
Uploaded by
Eula Angelica OcoCopyright:
Available Formats
Introduction
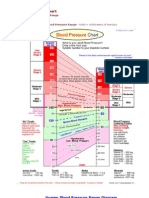
Hypertension is a highly prevalent disorder in older people. Hypertension, especially
isolated systolic hypertension, is commonly found in older which is about 60–79 years of
age and elderly that ages ≥80 people. Hypertension, defined as a blood pressure of
140/90 mmHg or more or being on antihypertensive medications. Antihypertensive drug
therapy should be considered in all aging hypertensive patients, as treatment greatly
reduces cardiovascular events. Most classes of antihypertensive medications may be
used as first-line treatment with the possible exception of α- and β-blockers. An initial
blood pressure treatment goal is less than 140/90 mmHg in all older patients and less
than 150/80 mmHg in the non-frail elderly. The current paradigm of delaying therapeutic
interventions until people are at moderate or high cardiovascular risk, a universal
feature of hypertensive patients over 60 years of age, leads to vascular injury or disease
that is only partially reversible with treatment.
The aim of this article is to summarize current knowledge about hypertension in aging
individuals. In this article, older people aged 60–79 years are considered separately
from the very old or elderly, defined as 80 years of age or more.
Blood Pressure with Aging
Blood pressure, particularly systolic blood pressure, rises with age, although the
diastolic component of blood pressure begins to plateau around the age of 50 years and
slowly declines thereafter. These temporal changes in blood pressure increase pulse
pressure and are associated with a dramatic rise in the prevalence from the beginning
of isolated systolic hypertension. In a community-based prospective cohort study, more
than 90% of normotensive adults in midlife develop hypertension in their lifetime. The
discrepant trends in systolic and diastolic blood pressure provides an explanation for the
change in the relative proportion of different forms of hypertension with age. In the
National Health and Nutrition Examination Survey less than 20% of hypertensive
individuals older than 60 years of age had an elevated diastolic blood pressure, and the
proportion declined steadily from the sixth decade onward
Epidemiology of Hypertension with Aging
Major overviews of observational studies have shown a continuous and positive
relationship between cardiovascular events and usual blood pressure above a baseline
level of approximately 115/75 mmHg at all ages and in both sexes. Although the
strength of the association weakens with age, the absolute difference in cardiovascular
risk between the highest and lowest usual blood pressure levels is much greater in older
subjects. Thus, the burden of disease that is potentially avoidable by blood pressure-
lowering treatment would be expected to be greater in older individuals.
In general, these population-based cohort studies were conducted in adults with no
previous vascular disease. Thus, the results may not necessarily be applicable to
subjects with significant comorbid diseases. Furthermore, in hypertensive patients
whose initial blood pressure was in the range considered to be uncontrolled, survival
was not significantly reduced for each 10 mmHg increase in systolic blood pressure or
diastolic blood pressure. The term 'reverse epidemiology' has been used to describe the
pattern of increased survival associated with higher blood pressure, and the
phenomenon likely reflects the confounding effects of other comorbid conditions.
Pathophysiology of Age-related Hypertension
The aorta and its major branches act as distensible tubes that promote the conversion
of the pulsatile output of the heart into a steady stream in the peripheral circulation. With
aging, there is a progressive loss of the visco-elastic properties of conduit vessels,
increased atherosclerotic arterial disease, and hypertrophy and sclerosis of muscular
arteries and arterioles. These vascular changes lead to a loss of the cushioning function
of the conduit vessels and stiffening of the arterial vasculature overall, which promote
the early return of reflected waves from the peripheral arterial circulation. Early wave
reflection amplifies the systolic pressure wave generated with each heartbeat, leading to
an increase in systolic pressure and a fall in diastolic pressure.
Diagnosis of Hypertension & Cardiovascular Risk Assessment
The diagnosis of hypertension has traditionally relied upon repeated office or clinic
blood pressure measurements taken by a healthcare professional using a mercury
sphygmomanometer. Increasingly, ambulatory blood pressure monitoring is being used
to expedite the diagnosis of hypertension and categorize it into different types.
Currently, it is only approved for reimbursement to diagnose white coat or isolated office
hypertension (elevated office or clinic readings and normal daytime blood pressure from
ambulatory recording). Isolated office hypertension is more common at older ages and
in females, and is often mistaken for uncontrolled hypertension, which may lead to
overtreatment. Ambulatory blood pressure monitoring is also useful to identify
individuals with masked hypertension, most commonly defined as normal office blood
pressure of less than 140/90 mmHg and high diurnal ambulatory blood pressure of
135/85 mmHg or more. While age does not seem to affect its prevalence, nonetheless it
is a common finding, particularly among treated hypertensive patients, and is
associated with increased risk of cardiovascular events. Finally, ambulatory blood
pressure monitoring provides important information on the pattern of nocturnal blood
pressure (nocturnal hypertension, nocturnal hypotension, dipping status and autonomic
dysfunction). Several studies have shown that nocturnal hypertension and nondipping of
blood pressure during sleep are important harbingers of poor cardiovascular prognosis
and that night-time pressures more accurately predict the occurrence of death and
cardiovascular events than daytime pressures, independent of other confounders. The
prevalence of nondippers among hypertensive men and women increases progressively
with age, reaching more than 40% in subjects aged 70 years or older.
Status of Hypertension in the Philippines
Cardiovascular disease is the leading cause of morbidity and mortality in the Philippines
and elevated BP is identified to be one of the major risk factors. The prevalence of HTN
in the country has been increasing. Several cross-sectional studies have shown that the
numbers are steadily increasing; from 11% in 1992 to 25% in 2008. The National
Nutrition and Health Survey (NNHES) of the Food and Nutrition Research Institute
conducted in 2012 indicated a small decline in the prevalence of individuals with HTN,
about 22.3%. Unfortunately, the survey is based on a single visit BP measurement
alone. The same survey also showed that the highest prevalence of HTN is found in the
70 years old and above age group, males have a higher rate of elevated BP, patients
who live in the rural areas, and those who have high economic status.
In a prospective, multistage, stratified, two-phase, nationwide survey published in 2007,
the prevalence of HTN in 3901 participants was 21%. HTN prevalence would increase
by 50% in individuals more than 50 years old. It is more common in the urban areas,
particularly in Metro Manila, and is more common in the middle economic stature.
Similar to the other countries in Southeast Asia, awareness and control are very low.
Only 16% of those surveyed are aware of having elevated BP. Treatment control was
seen in only 20% of the hypertensive. In the survey, Filipino patients were prescribed
more with a beta-blocker, but compliance rate is higher if they are on an angiotensin
receptor blocker.
The island nation of the Philippines has 7101 islands and the geography has
caused difficulty in the delivery of healthcare in the country. Government programs are
being implemented to include treatment of non-communicable diseases. Recently, the
Universal Health Care Act has been passed which guarantees equitable access to
quality and affordable health-care services for all Filipinos.
Treatment
Lifestyle Modification
Lifestyle modification is widely considered to be a good starting point in treating
hypertensive patients of all ages. With regard to nonpharmacological interventions for
lowering BP, although benefits have been shown in younger populations, there is little
evidence from controlled studies in hypertensive patients aged 60 plus. Some of the
proposed lifestyle changes, including weight reduction, Dietary Approaches to Stop
Hypertension/Mediterranean diet, dietary sodium reduction, physical activity, and
moderate alcohol consumption may, however, not be appropriate or relevant and may
even be detrimental. Thus, a weight reduction in patients >80 years easily induces a
loss of muscle mass (sarcopenia) and can even cause cachexia, unless an intensive
physical training program and adequate protein supplementation are concomitantly
applied.
Equally, an excessive salt reduction might induce hyponatremia, malnutrition,
and orthostatic hypotension with increased risk of falls. Physical activity adapted to the
functional capacities of the older person and to his or her preferences is of major
importance, even if not meeting the amount recommended by current guidelines, which
is similar for older and younger adult subjects. Finally, excessive alcohol intake should
be discouraged, not only because of its pressor effect but also mainly because of
increased risk of falls and confusion
Antihypertensive Medications
The relative and absolute benefits and the safety of antihypertensive drug
treatment in older hypertensive patients have been summarized in several systematic
reviews. In trials that only included isolated systolic hypertensive patients, systolic blood
pressure had to be 160 mmHg or more with diastolic blood pressure less than 95
mmHg. The lower boundary for old age was set at 60 years without an upper limit. In
trials including patients with both isolated systolic hypertension and systolic–diastolic
hypertension, the systolic blood pressure for inclusion ranged from 160 mmHg to more
than 200 mmHg with a wide range of threshold values for diastolic blood pressure. In
most instances, the first-line antihypertensive treatment was a thiazide diuretic (±
potassium-sparing agent), dihydropyridine calcium channel blocker or β-blocker. Active
treatment reduced total mortality by 13%, cardiovascular mortality by 18%, all
cardiovascular complications by 26%, stroke by 30% and coronary events by
23%.Based on such findings, guidelines recommend treating all hypertensive patients in
their seventh and eighth decade with antihypertensive medications from most classes of
agents although some authoritative bodies do not recommend α- or β-blockers as first-
line agents in the absence of specific indications for their use.
An important caveat in making treatment recommendations for older hypertensive
patients is the paucity of trial evidence on the advantages and possible harm associated with
blood pressure lowering in patients at low or even moderate risk for cardiovascular disease with
systolic blood pressure in the range of 140–159 mmHg. On the other hand, there are a large
number of clinical trials studying the effects of antihypertensive agents in patients at high risk for
a cardiovascular event. A substantial number of participants in the trials had treated or
untreated hypertension and were 60 years of age and older. In general, the experimental
treatment lowered systolic blood pressure more than that observed in the group receiving the
comparator intervention.
Conclusions
Hypertension is a highly prevalent disorder in older and elderly patients and is an
important contributor to their high absolute cardiovascular risk. Isolated systolic
hypertension is the dominant form, attributed to progressive arterial stiffening and
increasing atherosclerotic burden of conduit vessels with age and hypertrophy and
sclerosis of the muscular arteries and arterioles. Antihypertensive drug therapy should
now be considered in all hypertensive patients, regardless of age. Recent evidence
suggests antihypertensive medications from most classes of agents may be used to
control blood pressure, although some authoritative bodies do not recommend α- or β-
blockers as first-line agents in the absence of specific indications for their use. Future
studies will likely focus on determining the treatment strategy that will provide optimal
protection against developing cardiovascular disease. Finally, better physician
management has improved outcomes overall, but challenges continue to exist for
patients at high cardiovascular risk.
Bibiliography
http://www.hypertensionjournal.in/eJournals/ShowText.aspx?
ID=56&Type=FREE&TYP=TOP&IN=&IID=6&isPDF=NO
https://www.medscape.com/viewarticle/734880_3
https://www.ahajournals.org/doi/10.1161/CIRCRESAHA.118.313236
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- O L O G C: UR ADY F Uadalupe OllegesDocument2 pagesO L O G C: UR ADY F Uadalupe OllegesEula Angelica OcoNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- System Findings Interpretation and Analysis: ReferenceDocument2 pagesSystem Findings Interpretation and Analysis: ReferenceEula Angelica OcoNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Oco SWK7Document2 pagesOco SWK7Eula Angelica OcoNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Oco (Seatwork 2)Document3 pagesOco (Seatwork 2)Eula Angelica OcoNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Assessment Normal Findings Deviations From Normal HypoactiveDocument2 pagesAssessment Normal Findings Deviations From Normal HypoactiveEula Angelica OcoNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Quetiapine Drug StudyDocument3 pagesQuetiapine Drug StudyEula Angelica Oco100% (1)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Diagnostic Test PrefaceDocument9 pagesDiagnostic Test PrefaceEula Angelica OcoNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Alternative FeedingDocument36 pagesAlternative FeedingEula Angelica OcoNo ratings yet
- GBS IntroDocument2 pagesGBS IntroEula Angelica OcoNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Mental Retardation: Costes - Doqueza - Mendiola - Oco - TapasDocument28 pagesMental Retardation: Costes - Doqueza - Mendiola - Oco - TapasEula Angelica OcoNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Conduct Disorder: Ahmad, Nurhadda Cadenas, Miche Delos Santos, Mary Ann Pabillore, Jocel Papa, DevelynDocument34 pagesConduct Disorder: Ahmad, Nurhadda Cadenas, Miche Delos Santos, Mary Ann Pabillore, Jocel Papa, DevelynEula Angelica OcoNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Nutrients Functions Sources Protein and Amino Acids That Make Up ProteinDocument2 pagesNutrients Functions Sources Protein and Amino Acids That Make Up ProteinEula Angelica OcoNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Mechanical Aids For Ambulation Include: Canes Walkers CrutchesDocument17 pagesMechanical Aids For Ambulation Include: Canes Walkers CrutchesEula Angelica OcoNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Level of Anxiety - g5Document39 pagesLevel of Anxiety - g5Eula Angelica OcoNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Doh ProgramDocument39 pagesDoh ProgramEula Angelica Oco100% (1)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Generalized Anxiety DisorderDocument24 pagesGeneralized Anxiety DisorderEula Angelica OcoNo ratings yet
- Virtual Quiz Bee Objectives:: Team AbdellaDocument2 pagesVirtual Quiz Bee Objectives:: Team AbdellaEula Angelica OcoNo ratings yet
- Application of OMAHA System of Community DiagnosisDocument5 pagesApplication of OMAHA System of Community DiagnosisEula Angelica OcoNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Ways To Promote Wound HealingDocument3 pagesWays To Promote Wound HealingEula Angelica OcoNo ratings yet
- Reproductive System AgentsDocument56 pagesReproductive System AgentsEula Angelica OcoNo ratings yet
- How Can I Prevent High Blood Pressure?: Eat A Healthy Diet. EatingDocument3 pagesHow Can I Prevent High Blood Pressure?: Eat A Healthy Diet. EatingEula Angelica OcoNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Implementation of Dress Code Is Really Important Among Professional NursesDocument1 pageImplementation of Dress Code Is Really Important Among Professional NursesEula Angelica OcoNo ratings yet
- Adult Immediate Post Cardiac Arrest Care Algorithm 2015 UpdateDocument1 pageAdult Immediate Post Cardiac Arrest Care Algorithm 2015 UpdateRyggie Comelon0% (1)
- HFA Position Papers 2019Document264 pagesHFA Position Papers 2019Irina Cabac-PogoreviciNo ratings yet
- Guidelines For The Assessment, Diagnosis and Management of Peripheral Arterial DiseaseDocument60 pagesGuidelines For The Assessment, Diagnosis and Management of Peripheral Arterial DiseaseMourad LAKHOUADRANo ratings yet
- Basis of ECG and Intro To ECG InterpretationDocument10 pagesBasis of ECG and Intro To ECG InterpretationKristin SmithNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- TBPI Information PDFDocument8 pagesTBPI Information PDFxtraqrkyNo ratings yet
- Distal AnDocument99 pagesDistal AnMeycha Da FhonsaNo ratings yet
- Tachicardia A QRS LarghiDocument16 pagesTachicardia A QRS LarghiAlberto MichielonNo ratings yet
- Introducere in Cardiologie: Prof. Maria DOROBANTUDocument33 pagesIntroducere in Cardiologie: Prof. Maria DOROBANTUSolomon VioletaNo ratings yet
- Flashcards - Topic 8 The Circulatory System - Edexcel Biology GCSEDocument63 pagesFlashcards - Topic 8 The Circulatory System - Edexcel Biology GCSEPraise Kinkin Princess GanaNo ratings yet
- Cardiac Cycle Lab-1Document6 pagesCardiac Cycle Lab-1Matthew SANo ratings yet
- Ecg Ospe QuizDocument26 pagesEcg Ospe Quizsivakamasundari pichaipillaiNo ratings yet
- Interpretasi EKGDocument81 pagesInterpretasi EKGGyna MarsianaNo ratings yet
- Blood Supply of Upper LimbDocument36 pagesBlood Supply of Upper Limbteklay100% (2)
- Atherosclerosis and Coronary Artery Disease AtherosclerosisDocument8 pagesAtherosclerosis and Coronary Artery Disease Atherosclerosiskarim mohamedNo ratings yet
- Lab 11 AntianginalDocument4 pagesLab 11 AntianginalanaNo ratings yet
- Bls - Acls: Roli Joseph Z. Monta, RN BLS, Acls, Trauma, Hazmat CertifiedDocument72 pagesBls - Acls: Roli Joseph Z. Monta, RN BLS, Acls, Trauma, Hazmat CertifiedEkoy TheRealNo ratings yet
- Kami Export - Cardiovascular System Lecture Outline 1st PeriodDocument16 pagesKami Export - Cardiovascular System Lecture Outline 1st PeriodJada NovakNo ratings yet
- Venema E, Et Al. 2018Document6 pagesVenema E, Et Al. 2018widyadariNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hypertension CaseDocument3 pagesHypertension CaseArnold Christian QuilonNo ratings yet
- PV, HF, PpokDocument14 pagesPV, HF, PpokRizki AmeliaNo ratings yet
- Heart, Circulation, and Blood Unit Test: Biology 11 April 3, 2014Document8 pagesHeart, Circulation, and Blood Unit Test: Biology 11 April 3, 2014api-279500653No ratings yet
- Cardiovascular System (Anatomy and Physiology)Document93 pagesCardiovascular System (Anatomy and Physiology)Butch Dumdum86% (7)
- CHAPTER Respiration and CirculationDocument5 pagesCHAPTER Respiration and CirculationlatasabarikNo ratings yet
- Unenhanced MR Angiography: Martin Backens and Bernd SchmitzDocument20 pagesUnenhanced MR Angiography: Martin Backens and Bernd SchmitzEka Setyorini .A.No ratings yet
- Cardiomyopathy: Mrs. D. Melba Sahaya Sweety M.SC Nursing GimsarDocument55 pagesCardiomyopathy: Mrs. D. Melba Sahaya Sweety M.SC Nursing GimsarD. Melba S.S ChinnaNo ratings yet
- ECGDocument41 pagesECGmiguel mendezNo ratings yet
- Blood Pressure ChartDocument5 pagesBlood Pressure Chartmahajan1963100% (1)
- Peran Perawat Pada Pemeriksaan Penunjang IVUS, OCT (Imaging)Document31 pagesPeran Perawat Pada Pemeriksaan Penunjang IVUS, OCT (Imaging)Miftahul HudaNo ratings yet
- Nursing DiagnosisDocument3 pagesNursing DiagnosisKat Napoleon75% (4)
- Report-Ecg Ctscan G3 Friday PDFDocument25 pagesReport-Ecg Ctscan G3 Friday PDFTrí Tạ MinhNo ratings yet
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (3)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (29)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)