Professional Documents
Culture Documents
(Original Research Nouveautes en Recherche I: Canada
Uploaded by
my accountOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
(Original Research Nouveautes en Recherche I: Canada
Uploaded by
my accountCopyright:
Available Formats
[original research * nouveautes en recherche I
COST OF ALLOGENEIC AND AUTOLOGOUS
BLOOD TRANSFUSION IN CANADA
Roma Tretiak, MHA; Andreas Laupacis, MD, MSc, FRCPC; Marc Riviere, MD; Krista McKerracher, MBA;
Eric Souetre, MD, MBA, PhD; and the Canadian Cost of Transfusion Study Groupp*
Objective: To determine the cost, from a societal perspective, of blood transfusion in Canada.
Study design: Cost-structure analysis.
Setting: Data were collected from eight hospitals and from six blood centres operated by the Canadian
Red Cross Society in four provinces.
Outcome measures: Costs associated with four stages of transfusion - collection, production, distribu-
tion and delivery - in 1993 were assessed. Costs were divided into the following categories: person-
nel, purchases, external services, overhead, donors' time, patients' time (for autologous transfusion),
wastage and infection.
Results: The mean overall cost of a transfusion performed on an inpatient basis was $210 per unit of red
blood cells for an allogeneic transfusion and $338 per unit of blood for an autologous transfusion. The
mean cost of an allogeneic transfusion performed on an outpatient basis was $280 per unit of red blood
cells.
Conclusion: The costs determined in this study can be used in future studies comparing the cost-effective-
ness of allogeneic transfusion with that of alternative methods.
Objectif: Determiner le cout, pour la societe, des transfusions de sang au Canada.
Conception Analyse de structure des co'uts.
Contexte: On a obtenu des donnees de huit hopitaux et de six centres transfusionnels de la Societe cana-
dienne de la Croix-Rouge dans quatre provinces.
Mesures des resultats: On a evalue les coiuts lies 'a quatre stades de la transfusion - collecte, production,
distribution et livraison - en 1993. Les cotuts ont ete repartis entre les categories suivantes: personnel,
achats, services exterieurs, frais generaux, temps des donneurs, temps des patients (dans le cadre de Ia
transfusion autologue), gaspillage et infection.
Resultats: Le cofut global moyen d'une transfusion executee en service aux hospitalises s'est etabli 'a 210 $
l'unite de globules rouges dans le cas d'une transfusion allogene et 'a 338 $ l'unite de sang dans celui
d'une transfusion autologue. Le co(ut moyen d'une transfusion allogene executee en service externe s'est
etabli a 280 $ l'unite de globules rouges.
Conclusion Les co(uts etablis dans cette etude pourront servir dans le cadre d'etudes futures comparant
l'efficacite des couits des transfusions allogenes 'a celles d'autres methodes.
he recent public scnrtiny of Canada's blood system poietin, administration of drugs (e.g., aprotinin) to de-
1has led to increased interest in alternatives to allo- crease blood loss during surgery, hemodilution, use of
geneic red blood cell (RBC) transfusion: autologous perfluorocarbon emulsions and use of hemoglobin solu-
blood donation, cell savers, use of recombinant erythro- tions.i-2 To assess the cost-effectiveness of these new
Ms. Tretiak and Dr. Riviere are with the Benefit Research Group, Montreal, Que.; Dr. Laupacis is director of the Clinical Epidemiology Unit, Loeb Medical Research Institute, Ottawa Civic Hospital,
Ottawa, Ont; Ms. McKerracher is with Ortho Biotech, Don Mills, Ont; and Dr. Souetre is with the Benefit Research Group, Gennevilliers, France.
*Members. Dr. Lynn Boshkov, University ofAlberta Hospitals, Edmonton, Alta.; Dr. Gershon Growe, Vancouver Hospital and Health Sciences Centre, Vancouver, BC; Dr. John Kitts, Ottawa Civic
Hospital, Ottawa, Ont; David Home, Oshawa General Hospital, Oshawa, Ont; Dr. Yves Lapointe, Hdpital Notre-Dame, Montreal, Que.; Dr. Peter Pinkerton, Sunnybrook Health Science Centre, North
York, Ont; Dr. Renaud Whittom, Hopital Saint Fran,ois dAssise, Quebec, Que.; and Dr. Muhammad Zahir, Royal Inland Hospital, Kamloops, BC
Reprint requests to: Ms. Roma Tretiak, Benefit Research Group, Canada, 1402-2000 Mansfield St., Montreal QC H3A 3A2; fax 514 843-6645
0 1996 Canadian Medical Association (text and abstract/resumd)
CAN MED ASSOC J * MAY 15, 1996; 154 (10) 1501
technologies, the costs of allogeneic and autologous blood transfusion centres or in hospitals (in the case
blood transfusions must be known. of autologous blood).
The Canadian blood system is not for profit and re- * Production: all steps in processing the blood after it
lies on unpaid, volunteer donors. The system is managed has been collected and before it is distributed to hos-
nationally by the Canadian Red Cross Society (CRCS) pitals, including testing for transmissible diseases and
through 17 regional blood centres and is financed by the separation of blood components.
provincial and territorial governments through the * Distribution: the transportation of units of RBCs from
Canadian Blood Agency. There is no charge to health regional blood centres to hospitals.
care facilities or patients for blood products. * Delivery: all handling of blood (including laboratory
In the 1993-94 fiscal year, 1 045 749 units of whole tests) from arrival at the hospital to its administration
blood were collected and processed by the CRCS, from to the patient.
which 821 763 units of allogeneic packed RBCs were de- All data were from the 1993-94 fiscal year and were
rived and used for transfusions in hospitals.3 Autologouscalculated in 1993 Canadian dollars.
whole-blood donation services are administered both by Eight hospitals in four provinces participated in the
the CRCS blood centres and by individual hospitals. The study: Vancouver Hospital and Health Sciences Centre;
CRCS reported that it had collected 13 433 units of autol-
Royal Inland Hospital, Kamloops, BC; University of Al-
ogous blood in 1993-94; however, the amount collected berta Hospitals, Edmonton; Sunnybrook Health Science
through programs in individual hospitals is unknown. Centre, North York, Ont.; Oshawa General Hospital,
Several studies have assessed the cost of allogeneic Oshawa, Ont.; Ottawa Civic Hospital; Hopital Notre-
RBC" and autologous whole-blood7 transfusion. Forbes Dame, Montreal; and Hopital Saint Francois d'Assise,
and associates4 calculated the mean hospital cost of allo-
Quebec. Six are teaching hospitals and two (Royal Inland
geneic RBCs used in transfusions to be $155 (US) per Hospital and Oshawa General Hospital) are community
unit in 1988, and Lubarsky and collaborators5 deter- hospitals. Hospitals willing to participate in the study
mined it to be $151 (US) per unit in 1991. These studies were selected to represent a range of size and type of hos-
considered hospital costs only, whereas Sheingold and pitals. The hospitals represented all regions of the country
colleagues,6 with the use of a costing system developed except Atlantic Canada.
for Chedoke-McMaster Hospitals, Hamilton, Ont., cal- The national office of the CRCS provided data on
culated the mean cost of all aspects of allogeneic RBC the six CRCS transfusion centres affiliated with the eight
transfusion in Chedoke-McMaster Hospitals and CRCS participating hospitals.
centres to be $210 per unit. Data from the transfusion centres concerned the col-
Etchason and coworkers7 estimated the cost of collec-lection, production and distribution stages, whereas hos-
tion and production of allogeneic RBCs to be $150 (US) pitals provided data on the cost of the delivery stage.
per unit in 1992 and of autologous blood to be $198 The delivery-stage cost was assessed for several depart-
(US) per unit. ments in each hospital: hematology/oncology, surgery,
To date, there has been no published assessment of operating room, intensive care unit, general medicine,
the cost of allogeneic or autologous transfusion for all of
emergency and ambulatory care. We used a step-down
Canada. analysis of accounting data, which assigned costs to task
Our study determined the costs associated with blood(e.g., production) or type of product (e.g., RBCs) or
transfusion in the Canadian health care system. We as- both.
sessed the costs of all stages of transfusion, from collec- The total cost of each stage of transfusion was broken
down into the following categories: purchases, external
tion of blood to transfusion to the recipient, for inpatient
and outpatient transfusion and for allogeneic RBC and services, personnel, overhead, donors' time, patients'
autologous blood transfusion. In addition to calculating time, wastage and infection. The two time categories are
the cost per unit of blood, we calculated the cost for two
explained as part of the appropriate stages later in this
units of blood, since most patients receive two units dur-
article. The final two categories applied to the delivery
ing a transfusion.8 Costs were determined from the over- stage only. Purchases included all small equipment, sup-
all perspective of society, as recommended in the Guide- plies and the depreciation of capital equipment. External
lines for Economic Evaluation of Pharmaeeuticals: Canada .9
services included any service or portion of the activities
in a given centre provided from outside the organization
METHODS (e.g., a service contract for the maintenance of equip-
ment). Personnel costs included direct and indirect (e.g.,
We divided the blood system into the following four management) labour costs. Overhead costs included all
stages. nonlabour costs that could not be attributed directly to
* Collection: the collection of blood from donors at the any stage of transfusion. At the CRCS, overhead costs
1502 CAN MED ASSOC J * 15 MAI 1996; 154 (10)
included the costs incurred by the medical director's of- Data on autologous blood collection were obtained
fice, the blood donor recruitment office and the national from two participating hospitals that operate autologous
office as well as computer services and maintenance of blood collection programs (CRCS data on autologous
the premises at each centre. In hospitals, overhead costs blood collection were not available). It was assumed that
included the nonlabour costs of corporate overhead the time required for a patient to give a unit of autolo-
(such as the president's office and the department of fi- gous blood is the same as that required for allogeneic
nance) and support services (such as housekeeping and blood collection.
laundry). The overhead components provided by the
CRCS and the hospitals initially included both labour COST OF PRODUCTION
and nonlabour costs. However, in order to group all per-
sonnel costs, 65% of the overhead component was trans- Costs included in the production stage for allogeneic
ferred to the cost of personnel unless otherwise speci- transfusion were quality control, component processing,
fied. This proportion was based on information provided testing for transmissible diseases (HIV- 1, HIV-2, hepati-
by the finance departments of the participating hospitals tis C virus, human T-cell lymphotropic virus, Treponema
and the CRCS. pallidum and hepatitis B surface antigen), blood banking
These costs were used to calculate a cost per unit of and serologic testing of RBCs.
blood used in transfusions. The total cost of transfusion For autologous transfusion, we assumed that the first
was also calculated for two units of blood. Excluded unit of autologous blood was tested for transmissible dis-
from the costs of the second unit were costs of drawing a eases at the nearest CRCS centre and that the transfu-
sample from the patient for cross-matching and for sion took place at the hospital where the blood was col-
blood administration. The distribution cost and the cost lected. The mean cost of transmissible-disease testing
of testing for transmissible diseases during the produc- was obtained from the CRCS.
tion stage were also excluded for the second unit of au-
tologous blood (these costs would be included in the COST OF DISTRIBUTION
cost of the second unit if collection took place through a
CRCS centre). Distribution costs included all costs associated with
transporting blood or RBCs from the CRCS centres to
COST OF COLLECTION the participating hospitals. The cost of transporting au-
tologous blood from the hospital to the CRCS for trans-
For allogeneic transfusion, costs included in the col- missible-disease testing was assumed to be the same as
lection stage were blood-donor recruitment, donor the distribution cost of allogeneic RBCs.
screening, collection of blood at the transfusion centres
or at mobile clinics and transportation associated with COST OF DELIVERY
the mobile clinics. Costs were allocated to RBCs,
platelets, plasma and cryoprecipitate on the basis of the We calculated the mean cost per unit of RBCs for
number of units of each produced. The CRCS uses vol- blood banks in each hospital from hospital budgets for
unteers to perform some phases of blood collection as personnel and purchases. Costs were allocated on the
well as to donate blood. We included the cost of non- basis of the time spent by the laboratory staff to prepare
donor volunteers' and donors' time in the analysis, in ac- RBC units and the volume of units prepared, in compari-
cordance with the societal perspective of the study. The son with the time spent on and volume prepared of
nondonor volunteers' time was calculated from responses other products (i.e., platelets, plasma and plasma prod-
to a questionnaire concerning the number of volunteer ucts). We thereby determined the proportion of the
hours logged during 1 year, completed by five CRCS budget spent on RBC units. In two cases, the hospital
blood centres. The cost of this time was based on the budget for the blood bank was unavailable, so costs were
salaries and benefits that would be paid to CRCS em- estimated with the help of charge technologists.
ployees performing the same functions. Hourly wages Personnel time was assessed from data gathered dur-
varied from $8 to $13. A weighted mean cost was calcu- ing face-to-face interviews with nurses. The nurses were
lated on the basis of the number of units produced by asked to estimate the time required by all staff members
each centre. The cost of donors' time, valued on the ba- to administer blood or RBCs to a patient. Staff members
sis of the mean Canadian income,"1 was also included in included orderlies and porters, who transport blood or
the cost of collection. The transfusion centres estimated RBCs from the blood bank to the wards, and ward
that a donor spends approximately 2.5 hours donating clerks, who receive the blood or RBCs and communicate
blood, including time spent giving blood and travelling with the hospital blood bank. The cost of staff time was
to and from the centre. evaluated on the basis of the mean salaries and benefits
CAN MED ASSOC J * MAY 15, 1996; 154 (10) 1503
for these employees; these data were obtained from the transfusion to be 3 in 10 000 units'4 and of HIV infection
finance department of each hospital. For outpatient to be 1 in 200 000 units.'5
transfusion, the time required for a patient to receive a
transfusion was estimated to be approximately 4 hours SENSITIVI[Y ANALYSIS
(including transportation time) by the nurse manager of
the sole outpatient transfusion clinic in our study. Patient Three sensitivity analyses were performed. In the
time was valued on the basis of the mean income in first, the cost of each stage of transfusion was varied ac-
Canada." cording to the minimum and maximum costs obtained
The cost of materials used to administer blood or from the participating centres for each stage of allo-
RBCs was provided by the purchasing departments of geneic and autologous transfusion. The cost of wastage
the participating hospitals. A mean ratio of overhead was held constant in this analysis. In the second analysis,
costs to direct medical-services costs was applied to all the proportion of wastage was varied according to the
of the wards in each hospital to calculate the overhead lowest and highest proportion of wastage reported by
component. A mean cost of delivery for all inpatient the hospitals for allogeneic RBCs and autologous blood.
wards was used, since costs did not vary significantly The costs of collection, production and distribution
from one type of ward to another. The delivery cost of were held constant in this analysis. In the third analysis
autologous transfusion was calculated on the basis of the we assumed that autologous blood collected in hospital
cost of delivery during surgery. was not tested for transmissible diseases and that the
Included in the cost of delivery was the cost of production cost was therefore equal to zero.
wastage, defined as any unit of blood or RBCs that could
not be used for a transfusion because it was out of date RESULTS
or otherwise unusable. Information on the number of
units of allogeneic RBCs and autologous blood wasted in The mean cost of transfusing, on an inpatient basis,
each hospital was obtained from blood-bank records. A one unit of allogeneic RBCs was $210 and of autologous
weighted mean proportion of blood or RBCs wasted was blood was $338. The difference in cost was mainly due
calculated on the basis of the number of units available to the differences in the cost of collection between
for transfusion in each centre. Then the cost of wastage CRCS centres and hospitals and in the cost of wastage
was calculated by multiplying the cost per unit of collec- between allogeneic and autologous transfusion (2% of
tion, production and distribution but not delivery by the the total cost for allogeneic transfusion and 18% of the
proportion of wastage. cost for autologous transfusion). The mean cost of trans-
We also included the cost of infection acquired from fusion of two units of blood was $392 for allogeneic
transfusion as part of the cost of delivery. In this regard, RBCs and $619 for autologous blood.
hepatitis C and HIV infection were the only infections The mean cost of allogeneic blood collection at a
considered. CRCS centre was $64 per unit. Included in this cost was
We could find no recent studies on the cost of infec- nondonor volunteer time ($5 per unit) and donor time
tion with hepatitis C. We therefore used data on the ($30 per unit). In the case of autologous blood collec-
clinical course, management and associated costs of tion, the mean cost of hospital-based collection was
hepatitis B from a recent US article by Bloom and associ- $135 per unit, which included the patient's time, valued
ates.'2 Their data were obtained through a review of the at $30 per unit.
literature and were reviewed by an expert panel with the The mean costs per unit of inpatient allogeneic and
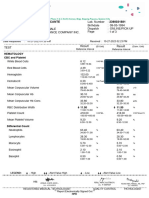
use of a modified Delphi technique. We then assumed autologous transfusion by stage are shown in Table 1.
that the cost of infection with hepatitis B and hepatitis C The greatest variation in the cost of transfusion was
were the same. found in the cost of delivery, mainly in the cost of
We used the lifetime cost of HIV infection calculated preparing a unit of RBCs in the hospital blood banks.
by Hellinger,'3 who estimated the total charges associated Hospitals that prepared relatively high volumes (more
with the various stages of HIV infection in the United than 8000 units) of RBCs benefited from economies of
States in 1992. scale and therefore had lower costs.
We assumed that the patterns of treatment of these For both inpatient allogeneic and autologous transfu-
two infections were similar across Canada and the sion, personnel and purchases were the biggest cost dri-
United States. The costs of infection included the direct vers, representing 60% and 16% respectively of the cost
medical costs of these diseases and excluded their indi- per unit of allogeneic RBCs and 52% and 12% respec-
rect costs. All future costs were discounted at a fixed an- tively of the cost per unit of autologous blood (Table 2).
nual rate of 5%. The difference in the cost of inpatient and outpatient
We estimated the risk of hepatitis C infection from transfusion (Table 3) was mainly due to the cost of the
1504 CAN MED ASSOC J * 15 MAI 1996; 154 (10)
$158 to $309 per unit, and that of autologous transfu-
patients' time. Because an extra visit is required to re-
ceive an outpatient transfusion, the cost of the patients'
sion from $281 to $420 per unit. These variations were
time was included in the analysis for outpatients. In con-
mainly due to differences in costs of delivery and of per-
trast, the cost of inpatients' time was not included be-
sonnel. The difference in the mean cost of delivery of al-
cause these patients were already in the hospital. logeneic and autologous transfusion ($50) was less than
The mean cost of wastage was $5 per unit for allo- the difference in the mean cost of wastage between the
geneic RBCs and $61 per unit for autologous blood two types of transfusion ($56). The cost of delivery of
(Table 4). The mean rate of wastage was 5% for allo- autologous blood was calculated on the basis of the cost
geneic RBCs and 37% for autologous blood. The of transfusion in the operating room only, whereas that
wastage figures for both allogeneic RBCs and autologousof allogeneic RBCs was based on the mean cost from all
blood used in these calculations were obtained from alldepartments. Delivery costs were slightly lower in the
participating hospitals. The CRCS wastage figures for operating room than in other departments because pa-
hospitals show that the national rate of wastage was 12%
tients undergoing surgery are continually evaluated,
for allogeneic RBCs and approximately 60% for autolo- whether or not they receive a transfusion. The cost of
gous blood collected by the CRCS in 1993-94. continuous monitoring cannot be fully attributed to the
transfusion. In contrast, if a patient receives a transfusion
SENSITIVITY ANALYSIS in a ward, a nurse must spend time by the patient's bed-
side during the transfusion. This entails a cost that
The total cost of allogeneic transfusion varied from would not otherwise exist.
Type of transfusion
Allogeneic Autologous
Mean cost, $ Range of Mean cost, $ Range of
Stage (and % of total) cost, $ (and % of -total) cost, $
Collection 64 (31) 55-72 135 (40) 128-167
Production 17 (8) 14-23 24 (7) -t
Distribution 5 (2) 3-8 5 (2) 3-8
Delivery 124 (59) 86-206 174 (52) 150-245
Total 210 (100) 158-309 338 (1Ot) 281420
*See Methods for explanation of stages.
tA natdonal mean was obtained from the Canadian Red Cross Society.
*Figures do not sum to 100 due to runding.
(ad,
Mean C .I O total)
Cost category Allogeneic transfusion Autologous transfusion
Purchases 33 (16) 42 (12)
External services 1 (1) 1 (0)
Personnel (incIuding
nondonor volunteers) 127 (60) 174 (52)
Overhead' 14 (7) 30 (9)
Donors' time - 30 (14) 30 (9)
Wastage 5 (2) 61 (18)
Riskof infection 1 (1) 0
Patients' time 0 0
Total 211 (lOOt) 338 (100)
*See Methods for explanation of categories.
tFigures do not sum to 100 due to rounding.
CAN MED ASSOC J * MAY 15, 1996; 154 (10) 1505
The mean proportion of wastage for allogeneic RBCs always be higher than that of collecting allogeneic blood
varied from 1% to 18% among hospitals, for a variation because of the specialized service associated with this
in cost from $1 to $16 per unit. For autologous blood, the "custom-made" product.
mean proportion of wastage varied from none to 64%, Transfusion of allogeneic RBCs was considerably
for a variation in cost from no cost to $104 per unit. more expensive on an outpatient basis than on an inpa-
The results of the sensitivity analysis of the cost of tient basis because the cost of the patients' time associ-
autologous blood are shown in Table 5. If autologous ated with the clinic visit was included in the cost of out-
blood collected in hospitals were not tested for transmis- patient transfusion. For inpatients, patients' time was not
sible diseases, the total cost of transfusion would de- included because we assumed that patients were already
crease from $338 to $309 per unit. in hospital for another reason. However, if patients were
admitted for the purpose of receiving an elective transfu-
DISCUSSION sion, the cost of their time and of the hospital stay
would need to be included. In this case, the total cost of
As expected, the mean cost of a unit of autologous inpatient transfusion would be significantly higher than
blood was higher than that of a unit of allogeneic RBCs. that of outpatient transfusion. If the costs of outpatient
Collection and delivery account for most of the costs of transfusion and its alternative (e.g., use of recombinant
both types of transfusion. The cost of the personnel human erythropoietin) were compared, the patients'
needed for collection of autologous blood was higher time required to receive either treatment would need to
than that of personnel to collect allogeneic blood. How- be considered.
ever, this difference was due to the collection of autolo- The cost of blood varied among blood centres and
gous blood in hospitals; it may be cheaper to collect au- hospitals, mainly as a result of differences in hospital
tologous blood at regional CRCS centres. One reason size, type of patients and salaries paid to employees. For
that collecting autologous blood at the CRCS centres inpatient transfusion of allogeneic RBCs, the sensitivity
may be less costly is that the CRCS has strict eligibility analysis found a $151 -per-unit difference in cost be-
criteria for donation and accepts only healthy donors. tween the maximum and minimum values for each of the
By contrast, hospital programs require enhanced support four stages of transfusion. The corresponding difference
in order to collect blood safely from patients who would in cost for inpatient transfusion of autologous blood was
be considered ineligible by CRCS criteria. The cost of $139 per unit. These wide ranges in costs must be taken
the patients' time for autologous donation was assumed
to be similar to the cost of the volunteer donors' time
for allogeneic donation. Wastage of autologous blood
because patients did not ultimately require a transfu-
sion contributed considerably to the cost of this blood. Mean cost (and range), $
This finding supports the selection for autologous
blood donation programs of patients who are most Allogeneic Autologous
likely to need blood during or after surgery. However, Stage transfusion transfusion
the cost of collecting autologous blood will probably Collection 4 (1-12) 50 (0-86)
Production 1 (0-3) 9 (0-15)
Distribution 0 (0-1) 2 (0-3)
mean cost, $ (ana % ot total) Total 5 (1-16) 61 (0-104)
Inpatient - Outpatient
Cost category transfusion transfusion
Purchases 17 (14) 25 (13)
External services 0 0
Personnel 90 (73) 102 (53) Cost with Cost without
Overhead 11 (9) 13 (7) Stage testing, $ testing, $
Wastage 5 (4) 5 (3) Collection 135 135
Risk of infection 1 (1) 1 (1) Production 24 0
Patients' time 0 48 (25) Distribution .1.....
5 0
Total 124 (100*) 194 (100*) Delivery 174 174
*Figures do not sum to 100 due to rounding. Total 338 309
1506 CAN MED ASSOC J * 15 MAI 1996; 154 (10)
into account when the results of our analysis are used in of blood products.' The cost of transfusion reactions was
decision making in individual centres and hospitals. also omitted, since such reactions were not accurately
As we discussed earlier, two recently published stud- recorded in hospital records. One study has estimated
ies have examined the costs associated with allogeneic that the cost of such reactions adds an additional $3 (US)
RBC transfusion.4' The studies used different methods to per unit to the total cost.5 The cost of a specialist consul-
calculate costs and included different direct and indirect tation for autologous donation was also omitted. There-
costs, making comparison difficult. In both studies only fore, the costs reported in this study are an underestimate
the hospital costs were determined and the hospitals' of the true societal cost of transfusion.
cost of acquiring a blood unit from the blood centre was Fourth, we calculated the cost of autologous transfu-
used as a proxy for the costs of collecting, processing sion in two hospitals, rather than in CRCS blood cen-
and distributing the unit. tres. Because hospitals have higher overhead and fewer
Etchason and coworkers7 estimated the direct health economies of scale than blood centres, the direct costs
care costs of collection (recruitment, screening and in- of collection of autologous units by the CRCS would
terviewing of donors, administrative record keeping and likely be lower than those of hospitals. However, if au-
phlebotomy) and of production (testing for transmissible tologous blood donation was available only through
diseases and compatibility, processing and inventory CRCS blood centres, the cost saving would possibly be
management) at $150 (US) for allogeneic transfusion offset by higher patient costs, especially travel time, be-
and $198 (US) for autologous transfusion in 1992. cause there are fewer centres (17 CRCS blood centres)
Given the differences in methods and in the health care than there are local hospitals.
systems of the two countries, our results are comparable The costs of allogeneic and autologous transfusion
with those of the studies previously published. are borne by several organizations and individuals, in-
The only Canadian study that has costed RBC trans- cluding the CRCS, hospitals, volunteers and patients.
fusion was conducted by Sheingold and colleagues.6 Thus, when examining the costs of blood and consider-
These investigators estimated the costs to the CRCS of ing any future changes to the transfusion system in
collection, processing and distribution. The study Canada, it is important to take into account the overall
showed that the direct cost of each unit transfused was societal costs and the potential transfer of costs from one
$180 and the expected cost of transfusion-related illness sector to another. Our results are important not because
was $30 per unit, for a total of $210 per unit transfused of the costs themselves, but because these costs can be
in 1991. The high cost of transfusion-related illness was incorporated into economic evaluations that consider
due to the high estimate of the rate of hepatitis C infec- both costs and consequences."' Only by comparing the
tion from transfusion (5%). This risk has decreased since cost-effectiveness of allogeneic transfusion with altema-
the introduction of screening tests for the hepatitis C tives such as autologous transfusion, use of recombinant
virus. erythropoietin, administration of aprotinin during sur-
There are limitations to our study. First, neither the gery, cell savers and other technologies can informed de-
blood centres nor the hospitals were chosen randomly. cisions be made about their use.
Rather, the hospitals were selected to provide a variety
of sizes and types. They represented all regions of the
thank the staff members of the National Office of the Canadian Red
country except Atlantic Canada. Because most of the We Cross Society and of the Canadian Blood Agency for their excellent co-
participating hospitals transfuse large volumes of RBCs, operation; without their input, we could not have completed this study
they likely represent the settings in which most blood is successfully. We also thank the charge technologists, nurses and the staff
of finance departments of the participating hospitals and centres, who
transfused. Therefore, the weighted mean costs likely also facilitated the successful completion of this study.
represent a true mean cost of blood transfusion in This study was supported by a grant from Ortho Biotech, Don Mills,
Canada. However, the cost of transfusion in remote Ont.
areas is likely higher.
Second, estimates of the mean time spent by staff
members during the delivery stage as well as time spent
by outpatients were obtained from interviews with 1. Perioperative red cell transfusion. NIH Consens Statement 1988;
nurses. The nurses may have overestimated or underesti- 7 (4): 1-6
mated the total time. 2. American College of Physicians: Practice strategies for elec-
Third, not all costs were included in the study. We did tive red blood cell transfusion. Ann Intern Med 1992; 1 16:
not include the costs of administration of the Canadian 404-406
Blood Agency, of research and development of blood 3. 1993-1994 Statistical Report, Blood Services, Canadian Red Cross
products, of transport of blood between hospitals, of le- Society, Ottawa, 1995
gal costs associated with the blood system and of misuse 4. Forbes JM, Anderson GF, Anderson GC et al: Blood transfu-
CAN MED ASSOC J * MAY 15, 1996; 154 (10) 15071
sion costs: a multicentre study. Transfusion 1991; 31: Economic Evaluation of Health Care Programs, Oxford University
318-323 Press, Toronto, 1987
5. Lubarsky DA, Hahn C, Bennett DH et al: The hospital cost 11. Income Distributions by Size in Canada, 1992 [cat no 13-207],
(fiscal year 1991/92) of a simple perioperative allogeneic red Statistics Canada, Ottawa, 1993: 19
blood cell transfusion during elective surgery at Duke Uni- 12. Bloom BS, Hillman AL, Fendrick AM et al: A reappraisal of
versity. Anesth Analg 1994; 79: 629-637 hepatitis B virus vaccination strategies using cost-effective-
6. Sheingold S, Churchill D, Muirhead N et al: The impact of ness analysis. Ann Intern Med 1993; 118: 298-306
recombinant human erythropoietin on medical care costs for 13. Hellinger FJ: The lifetime cost of treating a person with
hemodialysis patients in Canada. Soc Sci Med 1992; 34: HIV. JAMA 1993; 270: 474478
983-991
14. Donahue JG, Munoz A, Ness PM et al: The declining risk of
7. Etchason J, Petz L, Keeler E et al: The cost-effectiveness of post-transfusion hepatitis C virus infection. N Engl J Med
preoperative autologous blood donations. N Engl J Med 1995; 1992; 327: 369-373
332: 369-373
15. Remis RS: Estimation of HIV incidence among repeat blood
8. Ghali WA, Palepu A, Paterson WG: Evaluation of red blood donors in Montreal: a pilot study. [abstract PO-C21-31 11]
cell transfusion practices with the use of preset criteria. Can 9th International Conference on AIDS, Berlin, June 6-11,
Med Assoc J 1994; 150: 1449-1454 1993
9. Guidelines for Economic Evaluations of Pharmaceuticals: Canada, 1 st 16. Laupacis A, Feeny D, Detsky AS et al: How attractive does a
ed, Canadian Coordinating Office for Health Technology new technology have to be to warrant adoption and utiliza-
Assessment, Ottawa, 1994 tion? Tentative guidelines for using clinical and economic
10. Drummond MF, Stoddard GL, Torrance GW: Methods for evaluations. Can Med Assoc J 1992; 146: 473-481
510-5101 Buchan St., Montreal QC H4P 2R9; website: http://www2.uu.se:80/insts/radiol/
tel 514 738-3111, fax 514 738-5199 kongress.html
Du 9 au 13 juin 1996: 59e assembles annuelle June 13-16, 1996: Beyond Medical Care
June 9-12, 1996: 4th Canadian Conference on de l'Association canadienne des radiologistes Policies for Health
Health Promotion - Health Promotion and Vancouver Montreal
Population Health: a Meeting of Ideals (pre- Association canadienne des radiologistes, International Association of Health Policy, tel
sented by the Montreal Health Promotion Re- 510-5101, rue Buchan, Montreal QC H4P 2R9; 514 343-6492, fax 514 343-6544; congres
search Centre in collaboration with the Inter- tel 514 738-3111, fax 514 738-5199 @ere.umontreal.ca
disciplinary Health Research Group of the
University of Montreal) June 10-11, 1996: Animal Welfare and Toxi- June 14, 1996: 38th Annual Departmental Re-
Montreal cology Studies: Current Issues and Trends for search Day and 16th Clement McCulloch Lec-
Louise Potvin, 4th Canadian Conference on the Next Century ture
Health Promotion, Interdisciplinary Health Re- Baltimore Toronto
search Group, University of Montreal, PO Box Conferences, Scientists Center for Animal Guest speaker: Prof. D. McLeod, FRCS,
6128, Station Centre-ville, Montreal QC Welfare, Golden Triangle Building One, FRCOphth
H3C 3J7 340-7833 Walker Dr., Greenbelt MD 20770; tel Dr. David S. Rootman, Department of Oph-
301 345-3500, fax 301 345-3503 thalmology, University of Toronto, 115-1 Spad-
Du 9 au 12 juin 1996 : 4e Congres canadien ina Cres., Toronto ON M5S 2J5; tel 416
sur la promotion de la sante - la promotion June 10-12, 1996: Occupational and Environ- 603-5401
de la sante et la sant6 des populations : au mental Medical Association of Canada Confer- Judy Cardwell, coordinator, tel 416
confluent des visions (pr6sent6 par le Centre ence 1996 978-2635, fax 416 978-1522; J.Cardwell
de recherche en promotion de la sante de St. John's @utoronto.ca
Montreal en collaboration avec le Groupe de Dr. Ciaran O'Shea, OEMAC '96, PO Box 2442,
recherche interdisciplinaire en sante de l'Uni- Station C, St. John's NF A1C 6E7; tel 709 Du 16 au 19 juin 1996 : Assemblee generale
versite de Montr6al) 722-4074; fax 709 722-6801; coshea@public. annuelle et congres biennal de l'Association
Montreal compusult.nf.ca des infirmieres et infirmiers du Canada
Louise Potvin, 4e Congres canadien en pro- Halifax
motion de la sante, Groupe de recherche inter- June 11-14, 1996: Scandinavian Society of Patricia Mohr, coordonnatrice de con-
disciplinaire en sante, Universite de Montreal, Radiology 52nd Congress ferences, Association des infirmieres et infir-
CP 6128, Succursale Centre-ville, Montreal QC Uppsala, Sweden miers du Canada, 50, the Driveway, Ottawa ON
H3C 3J7 Hakan Ahistrbm, scientific secretary, or K2P 1E2; tel 613 237-2133 ou 800 361-8404,
Christl Richter-Frohm, secretary, Department of fax 613 237-3520; CNA@magi.com
June 9-13, 1996: Canadian Association of Ra- Diagnostic Radiology, University Hospital, S-
diologists 59th Annual Meeting 751 85 Uppsala, Sweden; tel 46 18 66-4757,
Vancouver fax 46 18 55-7279; Hakan.Ahistrom@radiol.
Canadian Association of Radiologists, uu.se or Christl. Richter Frohm@radiol.uu.se;i
1508 CAN MED ASSOC J 15 MAI 1996; 154 (10) For prescribing information see page 1546
*
-e
You might also like
- Best Practices of Apheresis in Hematopoietic Cell TransplantationFrom EverandBest Practices of Apheresis in Hematopoietic Cell TransplantationSyed A. AbutalibNo ratings yet
- 965 FullDocument7 pages965 FullRakhman FaridNo ratings yet
- Modelling of The Collections Process in The Blood Supply Chain: A Literature ReviewDocument33 pagesModelling of The Collections Process in The Blood Supply Chain: A Literature ReviewLuis EduardoNo ratings yet
- Sangre FrescaDocument9 pagesSangre FrescaRobinson Trujillo CabanillaNo ratings yet
- Blood Bank Functioning and Hospital Transfusion CommitteeDocument13 pagesBlood Bank Functioning and Hospital Transfusion CommitteeTraite Hmar100% (1)
- Discarding The Initial Aliquot of Blood Does Not Reduce Contamination Rates in Intravenous-Catheter-Drawn Blood CulturesDocument2 pagesDiscarding The Initial Aliquot of Blood Does Not Reduce Contamination Rates in Intravenous-Catheter-Drawn Blood CulturesKay HanNo ratings yet
- MSBOS Rasht IranDocument7 pagesMSBOS Rasht Irankarun1889No ratings yet
- Goodnough, Shander & Brecher, 2003Document9 pagesGoodnough, Shander & Brecher, 2003Jetco LawNo ratings yet
- Autologous Blood Salvage in Cardiac Surgery: Clinical Evaluation, Efficacy and Levels of Residual HeparinDocument8 pagesAutologous Blood Salvage in Cardiac Surgery: Clinical Evaluation, Efficacy and Levels of Residual HeparinjavelezhNo ratings yet
- Stroke 2005 Wojner Alexandrov 1512 8Document8 pagesStroke 2005 Wojner Alexandrov 1512 8Kevin LiputraNo ratings yet
- Estimated Blood Loss in Craniotomy: Diana Sitohang, Rachmawati AM, Mansyur ArifDocument3 pagesEstimated Blood Loss in Craniotomy: Diana Sitohang, Rachmawati AM, Mansyur ArifJihadatul KholilahNo ratings yet
- Brereton Et Al-2016-International Journal of Laboratory HematologyDocument11 pagesBrereton Et Al-2016-International Journal of Laboratory HematologycindyNo ratings yet
- Guidance For Storing Blood Samples in Laboratories Performingcomplete Blood Count With DifferentialDocument6 pagesGuidance For Storing Blood Samples in Laboratories Performingcomplete Blood Count With Differentialimran ahmed siddiquiNo ratings yet
- SaudiJKidneyDisTranspl252438-4286359 115423Document6 pagesSaudiJKidneyDisTranspl252438-4286359 115423yosefNo ratings yet
- Journal of Clinical Orthopaedics and Trauma: Naveen Bansal, Gagandeep Kaur, Sudhir Garg, Satinder GombarDocument5 pagesJournal of Clinical Orthopaedics and Trauma: Naveen Bansal, Gagandeep Kaur, Sudhir Garg, Satinder Gombarbaron1992No ratings yet
- Dietrich 2005Document8 pagesDietrich 2005my accountNo ratings yet
- Transfusion Medicine - 2017 - Robinson - The Administration of Blood Components A British Society For HaematologyDocument19 pagesTransfusion Medicine - 2017 - Robinson - The Administration of Blood Components A British Society For HaematologyRand AliNo ratings yet
- Clinical Blood UseDocument76 pagesClinical Blood Usemohamed hiekalNo ratings yet
- Gupea 2077 69251 1.pdf JsessionidDocument48 pagesGupea 2077 69251 1.pdf JsessionidАнастасияNo ratings yet
- Standards and Best Practice For Acute Normovolemic Hemodilution: Evidence-Based Consensus RecommendationsDocument6 pagesStandards and Best Practice For Acute Normovolemic Hemodilution: Evidence-Based Consensus Recommendationsbaron1992No ratings yet
- Continuing High Mortality From Trauma Haemorrhage and Opportunities For Improvement in Transfusion Practice: A Observational StudyDocument21 pagesContinuing High Mortality From Trauma Haemorrhage and Opportunities For Improvement in Transfusion Practice: A Observational StudydanielNo ratings yet
- Article in Press: Age of Blood and Survival After Massive TransfusionDocument5 pagesArticle in Press: Age of Blood and Survival After Massive TransfusionJosé BlasNo ratings yet
- A Compendium of Tranfusion Prectice Guidelines ARC Edition 4.0 Jan 2021Document75 pagesA Compendium of Tranfusion Prectice Guidelines ARC Edition 4.0 Jan 2021H Stuard B CocNo ratings yet
- Blood TransfusionDocument11 pagesBlood Transfusionsaid tariqNo ratings yet
- Journal Reading Anestesi RianDocument21 pagesJournal Reading Anestesi RianRian AprizaNo ratings yet
- Relacion Entre SvO y LactatoDocument9 pagesRelacion Entre SvO y LactatoMacros FitNo ratings yet
- Compendium of Transfusion MedicineDocument50 pagesCompendium of Transfusion MedicineLudmilla MartinsNo ratings yet
- Factors Associated With The High Cost of Liver Transplantation in AdultsDocument10 pagesFactors Associated With The High Cost of Liver Transplantation in AdultsMahmoud SelimNo ratings yet
- Blood Banking 1Document23 pagesBlood Banking 1jerusalemknightsincashmereNo ratings yet
- Time To Cross Off Routine Preoperative Blood Crossmatch in MastectomyDocument4 pagesTime To Cross Off Routine Preoperative Blood Crossmatch in MastectomyAmmar AmjadNo ratings yet
- Providing Hemostatic and Blood Conservation For Jehovah's Witness PDFDocument8 pagesProviding Hemostatic and Blood Conservation For Jehovah's Witness PDFJasonNo ratings yet
- BEST Kidney StudyDocument10 pagesBEST Kidney StudyJoseph Zenas JungNo ratings yet
- 10 Transfusion GatosDocument4 pages10 Transfusion GatosJoce MaripanguiNo ratings yet
- Cord Blood Stem Cell TransplantationDocument9 pagesCord Blood Stem Cell TransplantationNadja Jamilah D. MustaphaNo ratings yet
- Assessment of The Utilization Patterns of Blood AT Mazabuka General Hospital, ZambiaDocument11 pagesAssessment of The Utilization Patterns of Blood AT Mazabuka General Hospital, ZambiaMukale Chipego MoongaNo ratings yet
- Assessment of The Utilization Patterns of Blood AT Mazabuka General Hospital, ZambiaDocument11 pagesAssessment of The Utilization Patterns of Blood AT Mazabuka General Hospital, ZambiaMukale Chipego MoongaNo ratings yet
- AutotransfusionDocument5 pagesAutotransfusionydtrgnNo ratings yet
- Javadzadeh Shahshahani & Taghvai, 2017Document6 pagesJavadzadeh Shahshahani & Taghvai, 2017leonardo.furstenauNo ratings yet
- Rtc-Sec Admin WKBK 08 03 04Document35 pagesRtc-Sec Admin WKBK 08 03 04orelglibNo ratings yet
- BloodDocument6 pagesBloodAminaNo ratings yet
- EJMR VolumeDocument9 pagesEJMR Volumemostafa AdamNo ratings yet
- Cost Analysis of A Neonatal Point-of-Care MonitorDocument10 pagesCost Analysis of A Neonatal Point-of-Care MonitorMARIO LOPEZ VILLAMILNo ratings yet
- Value of Red Blood Cell Distribution Width On Emergency Department Admission in Patients With Venous ThrombosisDocument6 pagesValue of Red Blood Cell Distribution Width On Emergency Department Admission in Patients With Venous ThrombosisJicko Street HooligansNo ratings yet
- Hemoglobin Measurement in Venous Blood Compared With Pooled And.. Ragu..scimago q1 Tpi Scopu SuthorDocument11 pagesHemoglobin Measurement in Venous Blood Compared With Pooled And.. Ragu..scimago q1 Tpi Scopu Suthorrince noveliaNo ratings yet
- PIV Blood DrawsDocument7 pagesPIV Blood Drawsphidelt649No ratings yet
- Erroneous Automated Optical Platelet Counts PDFDocument8 pagesErroneous Automated Optical Platelet Counts PDFfar faraNo ratings yet
- Standard Operating Procedures For Blood Bank Processes in PakistanDocument204 pagesStandard Operating Procedures For Blood Bank Processes in PakistanMohamed Elmasry100% (4)
- Bodansky-2017-Potential Cost Savings by MinimiDocument4 pagesBodansky-2017-Potential Cost Savings by MinimiGökhanNo ratings yet
- Journal of Cardiothoracic and Vascular Anesthesia: Original ArticleDocument11 pagesJournal of Cardiothoracic and Vascular Anesthesia: Original ArticleRicardoNo ratings yet
- 2008 Tale of The Seven MaresDocument9 pages2008 Tale of The Seven MaresEduardo Alfredo Gutierrez PardoNo ratings yet
- Laboratory Hematology CriteriaDocument7 pagesLaboratory Hematology CriteriaRosNo ratings yet
- An Insight Into Donor Blood Units Wastage in A Hospitalbased Blood Bank From Pakistan 2021Document6 pagesAn Insight Into Donor Blood Units Wastage in A Hospitalbased Blood Bank From Pakistan 2021AHNS123No ratings yet
- Study of The Ratio of Cross-Matching To Transfusio PDFDocument7 pagesStudy of The Ratio of Cross-Matching To Transfusio PDFampratikna 14No ratings yet
- Red Blood Cell Transfusion PracticesDocument6 pagesRed Blood Cell Transfusion PracticesArdanta Dat Topik TariganNo ratings yet
- Blood BankDocument15 pagesBlood BankAnsari ShariqNo ratings yet
- Joy 1998Document9 pagesJoy 1998Nguyễn Đức LongNo ratings yet
- Transfusion - 2021 - Murphy - Hemovigilance Drives Improved Transfusion SafetyDocument3 pagesTransfusion - 2021 - Murphy - Hemovigilance Drives Improved Transfusion Safetyvivekgupta58636No ratings yet
- Critical Care for Potential Liver Transplant CandidatesFrom EverandCritical Care for Potential Liver Transplant CandidatesDmitri BezinoverNo ratings yet
- Utilizationof Blood TransfusionDocument5 pagesUtilizationof Blood TransfusionKusumastuti TutikNo ratings yet
- Cherukuri Et Al. 2018 - Home Haemodialysis Treatment and Outcomes, Retrospective Analysis of KIHDNEyDocument10 pagesCherukuri Et Al. 2018 - Home Haemodialysis Treatment and Outcomes, Retrospective Analysis of KIHDNEyShareDialysisNo ratings yet
- Block 2013Document18 pagesBlock 2013my accountNo ratings yet
- 10.1016@s0009 89819700091 0Document14 pages10.1016@s0009 89819700091 0my accountNo ratings yet
- Liver Fibrosis A Compilation On The Biomarkers StaDocument17 pagesLiver Fibrosis A Compilation On The Biomarkers Stamy accountNo ratings yet
- Thrombocytopenia in CirrhosisDocument4 pagesThrombocytopenia in Cirrhosismy accountNo ratings yet
- Prevalence of and Risk Factors For Anaemia in Patients With Advanced Chronic Liver DiseaseDocument11 pagesPrevalence of and Risk Factors For Anaemia in Patients With Advanced Chronic Liver Diseasemy accountNo ratings yet
- Evaluation of Macrocytic AnemiasDocument8 pagesEvaluation of Macrocytic Anemiasmy accountNo ratings yet
- Association of Liver Cirrhosis Severity With AnemiaDocument5 pagesAssociation of Liver Cirrhosis Severity With Anemiamy accountNo ratings yet
- Abnormal Hematological Indices in CirrhosisDocument6 pagesAbnormal Hematological Indices in Cirrhosismy accountNo ratings yet
- Olevel GuideDocument1 pageOlevel GuideBurhan GhaniNo ratings yet
- Activity #9 - Reticulocyte CountDocument3 pagesActivity #9 - Reticulocyte CountMaria ClaraNo ratings yet
- PHLEBOTOMYDocument21 pagesPHLEBOTOMYmyka brilliant cristobalNo ratings yet
- Abnormal CBC - PresentationDocument23 pagesAbnormal CBC - PresentationMateen ShukriNo ratings yet
- Evaluare Pacient - Scor HAS-BLED: H A S B L E DDocument2 pagesEvaluare Pacient - Scor HAS-BLED: H A S B L E Dviorel79No ratings yet
- Prevent HemolysisDocument1 pagePrevent HemolysisQaiser ZamanNo ratings yet
- Labreport V SMSH 23 21296371 PDFDocument2 pagesLabreport V SMSH 23 21296371 PDFPurnima Swami (Lecturer & Promoter)No ratings yet
- Gabilan, Gerlie Alicante 2390031881Document3 pagesGabilan, Gerlie Alicante 2390031881gerlitag05No ratings yet
- Amy Wong Strilchuk - NBS 2021 PosterDocument1 pageAmy Wong Strilchuk - NBS 2021 PosterCBR UBCNo ratings yet
- Autoimmune - Hemolytic - Anemia - Mixed - Type-A - Case - Repo 2Document5 pagesAutoimmune - Hemolytic - Anemia - Mixed - Type-A - Case - Repo 2Afsha AnishNo ratings yet
- Artigo de Revisao Purpura Trombocitopenica TromboticaDocument11 pagesArtigo de Revisao Purpura Trombocitopenica TromboticaPlaneta SosNo ratings yet
- Permintaan Lab 2023Document9 pagesPermintaan Lab 2023imanNo ratings yet
- White Paper Parameters and Species Exigo h400 - Wpe - 34071 1 PDFDocument12 pagesWhite Paper Parameters and Species Exigo h400 - Wpe - 34071 1 PDFОльга ДовженкоNo ratings yet
- Hypereosinophilic Syndromes.......Document39 pagesHypereosinophilic Syndromes.......alaaNo ratings yet
- Chapter 6 Hema 1Document7 pagesChapter 6 Hema 1EMAN SALEHNo ratings yet
- Myeloproliferative Disorders (Bhs Inggris)Document57 pagesMyeloproliferative Disorders (Bhs Inggris)Denny DedenNo ratings yet
- Exchange TransfusionDocument21 pagesExchange TransfusionJOSLIN100% (3)
- Human Blood Group Antigen and AntibodyDocument15 pagesHuman Blood Group Antigen and AntibodyNur Melani Sari WardaniNo ratings yet
- Clinical WorksheetDocument13 pagesClinical WorksheetMohajirah AbubakarNo ratings yet
- Blood AdministrationDocument35 pagesBlood AdministrationnurminieNo ratings yet
- Have You Been Tested For Beta Thalassemia Trait?: Cooley's Anemia FoundationDocument2 pagesHave You Been Tested For Beta Thalassemia Trait?: Cooley's Anemia FoundationBuburuza RalucaNo ratings yet
- TTAB Tetradecyltrimethylammonium BromideDocument7 pagesTTAB Tetradecyltrimethylammonium Bromidedr. SheryarOrakzaiNo ratings yet
- Blood Donar SelectionDocument16 pagesBlood Donar SelectionSiva KeerthanaNo ratings yet
- PolycythemiaDocument2 pagesPolycythemiaDina AssefaNo ratings yet
- CoagulopathyDocument121 pagesCoagulopathyMegat Mohd Azman AdzmiNo ratings yet
- Experiment No.6 Blood Grouping and Blood Typing Objective: Materials: ProcedureDocument3 pagesExperiment No.6 Blood Grouping and Blood Typing Objective: Materials: ProcedureClaveria Jeric FernandezNo ratings yet
- Plasma Fractionation in KoreaDocument3 pagesPlasma Fractionation in KoreahzulqadadarNo ratings yet
- Blue People Activity 1Document5 pagesBlue People Activity 1ARYAN SINGHNo ratings yet
- Hematology EMQDocument7 pagesHematology EMQfrabzi100% (1)
- AutomatedBloodCount PDFDocument1 pageAutomatedBloodCount PDFKowshik ChakrabortyNo ratings yet