Professional Documents
Culture Documents
Diabetic Ketoacidosis Rapid Identification,.4
Diabetic Ketoacidosis Rapid Identification,.4
Uploaded by
Tiara MaharaniOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Diabetic Ketoacidosis Rapid Identification,.4
Diabetic Ketoacidosis Rapid Identification,.4
Uploaded by
Tiara MaharaniCopyright:
Available Formats
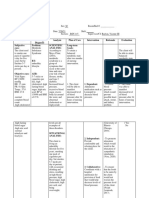
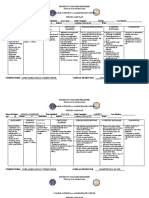
Diabetic Ketoacidosis
Downloaded from http://journals.lww.com/ajnonline by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC1y0abggQZXdtwnfKZBYtws= on 02/16/2021
Rapid identification, treatment, and education can improve
survival rates.
By Gordon Lee Gillespie, BSN, CEN, and Melody Campbell, MSN, CEN, CCRN
T
he rescue squad arrives at the emergency dropped to 20.4, a change attributed to streamlined
department (ED) with Chad Smith, 72 care and modern treatment modalities.8
years old, who was found unconscious
on the basement floor of his home. En PATHOPHYSIOLOGY
route to the hospital, Mr. Smith’s respi- DKA is initiated by trauma or conditions such as
rations became very shallow. An endotracheal tube new-onset diabetes or congestive heart failure,
was inserted, and its placement was confirmed by which place the body under stress and increase the
end-tidal CO2 detection. Since arriving at the ED, levels of catecholamines, cortisol, growth hor-
he has remained comatose and is not assisting the mones, and glucagon. Excesses of these hormones
ventilator. His vital signs are blood pressure, 80/48 decrease the effectiveness of insulin.4,9 In the pres-
mmHg; heart rate, 112 beats per minute; and tem- ence of insulin resistance or deficiency, hyperglycemia
perature, 91.8°F. He has a sinus tachycardia with- occurs, decreasing the movement of glucose from the
out ectopy. The glucometer indicates a finger stick intravascular spaces to the intracellular spaces. With
blood sugar (FSBS) reading of “panic high.” the cells then starving from lack of glucose, the
Mr. Smith is among the 5.9% of people in the body starts metabolizing its own fats and pro-
United States with diabetes.1 A significant percentage teins. As fats are broken down, a process called
of them will experience diabetic ketoacidosis (DKA), lipolysis occurs, in which free fatty acids form and
a state of hyperglycemia, hyperketonemia, and meta- travel to the liver, where they become keto acids
bolic acidosis.2,3 DKA typically affects those with type that place the body in a state of hyperketonemia.10
1 diabetes, although patients with type 2 diabetes When the body’s glucose level rises, fluid shifts
who suffer from hyperglycemic hyperosmolar nonke- from the intracellular to the intravascular spaces.
totic syndrome also experience DKA, and with Subsequently, when the kidneys’ ability to filter
increasing incidence.4,5 In January 2002, the the hyperglycemic blood is overcome, they begin
American Diabetic Association (ADA) reported that spilling the extra glucose into the renal system.
there are approximately 100,000 hospitalizations for Because of the molecular size of glucose and its
DKA annually.6 It’s also the leading cause of death osmotic pressure, fluid follows the glucose
among children with diabetes, nearly 40% of whom through the renal system and into the bladder,
present with DKA in addition to new-onset diabetes.7 causing the patient to experience polyuria.2 This
The ability of emergency nurses to learn and rec- leads to intracellular as well as generalized dehy-
ognize the signs and symptoms of DKA profoundly dration, which, along with the body’s inability to
affects outcome and survival rate. In 1980, the age- rid itself entirely of the ketones, leads to metabolic
adjusted death rate among patients with diabetes acidosis.3,9 During early DKA, the glomerular fil-
was 30.8 per 100,000 patients, with DKA listed as tration rate decreases as kidney function becomes
the cause of death. By 1996, this number had impaired. Coupled with a shift of potassium (K+)
from the cells into the extracellular spaces, this
Gordon Lee Gillespie is an emergency nurse at Mercy Franciscan causes elevated K+ levels. And as DKA progresses,
Hospital-Mount Airy, Cincinnati, OH. His mentor, Melody Campbell, profound diuresis occurs, causing a drop in serum
is critical care CNS and trauma coordinator at the Upper Valley
Medical Center, Troy, OH. K+ level. Once rehydration is initiated, K+ begins
ajn@lww.com AJN ▼ September 2002 ▼ Supplement 13
shifting back into the cells, causing severe levels. As rehydration and insulin therapy take effect,
hypokalemia.2, 4 these levels will begin decreasing. If the initial K+
level is less than 5.5 mEq/L, 20 mEq potassium chlo-
IDENTIFICATION ride should be added to the primary fluid. If the K+
The symptoms of this condition are polyuria, poly- level is less than 3.3 mEq/L, 40 mEq potassium chlo-
dipsia, and polyphagia.4 Because of Mr. Smith’s ride should be added.3 As the acidosis increases, the
coma, the nurses were unable to assess him for these pH continues to drop. However, the acidosis isn’t
symptoms. During his physical assessment, how- treated until pH drops to less than 7.0. Treating the
ever, he demonstrated hypother- acidosis when pH is higher than 7.0
mia, tachycardia, hypotension, and increases the risk of hypokalemia
vomiting, all of which are associ- and cardiac arrhythmia and brings
ated with DKA. Other symptoms about a shift in the oxyhemoglo-
associated with the condition bin dissociation curve that causes
include Kussmaul respirations (rapid decreased tissue oxygenation.3,4 If
and deep respiratory pattern), car- Maintain urinalysis, radiographs, or CBC
diac arrhythmia, altered mental sta- show signs of infection, start antibi-
tus, an acetone or fruity breath, otic therapy after cultures have
nausea, weakness, weight loss, continuous been obtained. Maintain continu-
blurred vision, flushed face, and leg ous cardiac monitoring to check for
cramps.2,4 Patients presenting with cardiac arrhythmia that may result from
typical symptoms of DKA, an changes in K+ levels.
altered level of consciousness, or monitoring to
several of the additional symptoms MANAGEMENT
should have a FSBS test performed check for Once DKA is identified, manage-
to rule out hyperglycemia and pos- ment of the patient is twofold. The
sible DKA. It’s important to note, arrhythmia that precipitating stressors must be iden-
however, that FSBS values can be tified and treated, as must the
erroneously low if the patient is serum glucose level and the addi-
severely dehydrated or hypoten-
may result from tional significant symptoms.
sive.11 Therefore, serum glucose lev- Precipitating stressors include
els should always be compared changes in K+ infection, trauma, myocardial in-
with the initial FSBS value. This is farction, congestive heart failure,
especially important if FSBS level levels. cerebrovascular accident, gastroin-
will be used to evaluate the effec- testinal bleeding, and new-onset
tiveness of subsequent treatment. diabetes. Other stressors include
Hematocrits below 20% and above emotional stress, cocaine use, mis-
70% may also cause lower FSBS management of insulin or of oral
values. diabetic agents, and concurrent use
of medications such as corti-
DIAGNOSIS AND INTERVENTION costeroids, thiazide diuretics, and phenytoin.4,10
When Mr. Smith arrived at the ED, an electrocar- Mr. Smith was immediately started on a 0.9%
diogram, chest radiograph, and routine urinalysis normal saline (NS) IV fluid bolus for hypotension
were performed, and FSBS, complete blood count and hyperglycemia. He was also given 10 units of
(CBC), chemistry panel, and serum ketone level regular insulin via intravenous push (IVP).
were assessed. These diagnostic tests are typically Patients with DKA typically need 3 to 6 L NS
used to confirm the presence of DKA and to deter- during the first few hours after onset.10 The ADA
mine its severity in patients with signs and symp- recommends that 0.9% NS be administered intra-
toms. Further diagnostic tests, such as urine, venously at 15 to 20 mL/kg/hr for 60 to 90 min-
sputum, wound, and blood cultures, as well as utes.6 Others have recommended that 0.9% NS be
assessment of arterial blood gas, cardiac enzyme, given intravenously at 15 mL/kg/hr for one hour,
amylase, and lipase levels will help identify the then at 7.5 mL/kg/hr for 2 hours, then at 3.75
cause of DKA. Also, consider administering preg- mL/kg/hr for the next 24 to 36 hours as long as the
nancy tests to women of childbearing age.2 corrected serum sodium isn’t elevated.12 Once the
Intervention will vary depending on test results. hypovolemia and hypotension are corrected, the
Patients with DKA usually present with elevated K+ 0.9% NS should be changed to 0.45% NS.10
14 AJN ▼ September 2002 ▼ Supplement http://www.nursingcenter.com
Routine treatment includes administering regular then confirming its placement with an end-tidal
insulin 0.1 to 0.15 units per kg IVP followed by a CO2 detector, auscultation of breath sounds, and a
0.1 unit/kg/hr IV infusion.10 An insulin infusion is pre- portable chest radiograph.2,6 Assess circulation, ob-
pared by adding regular insulin to 0.9% NS to reach tain vascular access, and start a 0.9% NS infusion.
the desired concentration, usually a 1:1 ratio. The If the patient is hypotensive, a fluid bolus must be
tubing needs to be primed and an extra 10 to 50 given.2 Finally, assess the patient’s neurologic status:
mL of fluid wasted through continuous priming Is he alert and responsive to verbal or painful stimuli?
to accommodate for the insulin being absorbed by Secondary assessment. Undress the patient,
polyvinyl chloride tubing.2,13 and if there’s hypothermia, control temperature
If the glucose level doesn’t drop by 50 to 100 using warmed blankets, overhead heating lamps,
mg/dL every hour, the insulin infu- and warmed IV fluids. Insert a
sion rate should be doubled.2,3,10 nasogastric tube if the patient is
Regardless of the initial FSBS read- vomiting, and insert an indwelling
ing, insulin therapy should be urinary catheter in order to moni-
maintained until electrolyte values tor output and obtain urinalysis.
have been obtained and K+ therapy If the patient has been intubated,
is initiated (if the K+ level is lower
Chronic vision place a nasogastric tube to decom-
than 5.5 mEq/L).6,12 Once the hourly press the stomach.4 Initiate cardiac
blood sugar measurements are less changes may monitoring to check for arrhyth-
than 250 mg/dL, the hourly rate of mia, which may result from elec-
intravenous insulin should be re- prevent elderly trolyte imbalances. Take steps to
duced by half. Start an infusion of make the patient comfortable, such
5% dextrose and 0.45% NS at 100 patients with as by administering antiemetics or
to 150 mL/hr to replace the 0.9% analgesia.
(or 0.45%) NS infusion. The insulin diabetes from Obtain a thorough history from
infusion should continue until at the patient and family in order to
least two of the following outcomes administering identify what may have precipitated
occur: the anion gap is less than the DKA episode. Perform a head-
14 mEq/L, the venous pH is 7.3 to-toe exam to identify abnormali-
or greater, or the bicarbonate level is
insulin on ties, establish a baseline assessment,
greater than 18 mEq/L.2,3,10 For and help identify root causes and
treating acidosis, if the pH is less their own. sequelae of the condition.
than 6.9, the ADA recommends The frequency of follow-up
adding 100 mmol of sodium bicar- assessments will vary depending on
bonate (NaHCO3) to 400 mL ster- the baseline assessment and stabil-
ile water and administering the ity of the patient. For example, alert
solution over two hours. If the pH patients may be able to report
is 6.9 to 7.0, 50 mmol of NaHCO3 should be symptom changes to nursing staff, whereas those
added to 200 mL sterile water and given over two who are unconscious will require assessment hourly
hours. Reevaluate the venous pH every two hours. (or more frequently, if necessary). Reassessment
When the pH reaches 7.0, no further NaHCO3 includes examination of ABC, and assessment of
need be administered. neurologic status and vital signs.2,4
NURSING CARE AND ONGOING ASSESSMENT EDUCATION
Nursing care of patients with DKA includes a Once the patient is extubated, he will need educa-
thorough nursing assessment as well as patient and tion in diabetes management in order to prevent
family education. recurrence and sequelae. Patients who don’t believe
Primary assessment involves evaluation of air- they have diabetes (as reported by family members)
way, breathing, and circulation (ABC), as well as pose a particular challenge to nurses, who will need
neurologic status. First, assess airway patency. If the to tailor education accordingly.
patient is not able to breathe on his own insert an Management during concurrent illness and daily
oral or nasopharyngeal airway.6 If vomiting occurs, FSBS monitoring are of the utmost importance,
oral suctioning may be required. If breathing is inef- even if the disease is well controlled by oral agents.
fective or the patient is vomiting and comatose, pro- Signs and symptoms of DKA need to be reviewed
tect the airway by inserting an endotracheal tube with the patient and family during each ED visit for
ajn@lww.com AJN ▼ September 2002 ▼ Supplement 15
hyperglycemia and whenever diabetes is identified force the importance of proper diet planning and
in the ED.4 Also, urge patients to get annual self-management of diabetes. Patients may also
influenza vaccines to prevent sepsis and pneumo- benefit from advice on how to accommodate
nia—common stressors that precipitate acute DKA dietary modifications when grocery shopping or
episodes.13 dining out.
Sick-day management. Advise patients to seek Chronic vision changes may prevent elderly
professional medical assistance for uncontrolled patients with diabetes from administering insulin on
fevers, urinary frequency or discomfort, persistent their own. A registered diabetes educator can help
cough, or ulcerations. If antibiotics have been pre- them choose alternative methods of measuring and
scribed for these illnesses, explain the importance of administering insulin, such as teaching friends and
using the entire prescription, even after symptoms family members to administer the insulin for them,
have improved or subsided. This will ensure that using a magnifying glass when drawing the insulin,
these illnesses are appropriately treated and will or using an insulin pen.
reduce the incidence of resistant bacterial strains. Diabetes affects a significant percentage of the
Encourage patients to continue their insulin therapy population, and DKA is one of the most serious
and medications even when they’re experiencing health problems resulting from it. Rapid identifica-
nausea and vomiting from other illnesses.13 To pre- tion is essential in order to improve patient out-
vent DKA and dehydration, instruct patients to comes and overall quality of life. Once the stressors
drink liquids containing carbohydrates (such as have been identified, they must be treated. To pre-
sodas, juices, and gelatins) and salt (such as bouil- vent further occurrence of DKA, educate patients
lon).3,9,13 If patients can’t keep these fluids down, or and their families so they can manage sick days
if nausea and vomiting persist for more than a day, more effectively and know when to seek medical
they will need to consult a health care professional. assistance. ▼
When patients with diabetes become ill with a
cold or flu, they should check their urine for ketones
REFERENCES
with each void—or at least daily—using urine ketone
1. National Center for Chronic Disease Prevention and Health
strips from the pharmacy.13 Patients also should Promotion. National diabetes fact sheet: national estimates
increase the frequency of FSBS monitoring to and general information on diabetes in the United States.
make sure the levels remain under 200 mg/dL. If Revised ed. Atlanta (GA): Department of Health and Human
readings exceed 200 mg/dL, they should contact Services; 1998. http://www.cdc.gov/diabetes/pubs/facts98.htm.
2. Miller J. Management of diabetic ketoacidosis. J Emerg
the health care professional.9 Encourage them to Nurs 1999;25(6):514-9.
get extra rest.13 Finally, remind patients to tell 3. Kitabchi AE, Wall BM. Management of diabetic ketoacido-
family members or friends when they become ill, sis. Am Fam Physician 1999;60(2):455-64.
and to ask family members to check on them 4. Quinn L. Diabetes emergencies in the patient with type 2
every four hours to make sure the condition has- diabetes. Nurs Clin North Am 2001;36(2):341-60, viii.
n’t worsened.3,13 5. Westphal SA. The occurrence of diabetic ketoacidosis in
non-insulin-dependent diabetes and newly diagnosed diabetic
Consultations. If patients don’t adhere to their adults. Am J Med 1996;101(1):19-24.
medical regimen, it’s important to identify the rea- 6. American Diabetes Association. Clinical practice recommen-
sons why. Patients often deny having a chronic ill- dations 2002. Diabetes Care 2002;25 Suppl 1:S1-147.
ness, and therefore don’t follow medical advice or 7. Emergency Nurses Association. Medical emergencies. In:
take their medications. Those who struggle to cope ENPC provider manual. 2nd ed. Park Ridge (IL): The
Association; 1999. p. 273-301.
with diabetes may benefit from a psychiatric con-
8. National Center for Chronic Disease Prevention and Health
sultation, which may help them accept the condi- Promotion. Diabetic ketoacidosis. In: Diabetes surveillance,
tion. A spiritual guide or a chaplain can also be 1999. Atlanta (GA): Centers for Disease Control and
helpful, especially when there’s a threat of death, Prevention; 1999.
http://www.cdc.gov/diabetes/statistics/survl99/Chap7/
severe illness, or life-changing complication. contents.htm.
If patients aren’t following the prescribed regi- 9. Freeland BS. Diabetic ketoacidosis. Am J Nurs
men because they can’t afford the cost of medica- 1998;98(8):52.
tions or diabetes monitoring equipment, arrange a 10. Jabbour SA, Miller JL. Uncontrolled diabetes mellitus. Clin
social service consultation as soon as possible. A Lab Med 2001;21(1):99-110.
social worker may be able to help patients to 11. Atkin SH, et al. Fingerstick glucose determination in shock.
Ann Intern Med 1991;114(12):1020-4.
either obtain these supplies or apply for Medicare
12. Konick-McMahan J. Riding out a diabetic emergency.
or Medicaid insurance. Provide literature describ- Nursing 1999;29(9):34-40.
ing community services. 13. Grinslade S, Buck EA. Diabetic ketoacidosis: implications for
Furthermore, a registered dietitian can rein- the medical-surgical nurse. Medsurg Nurs 1999;8(1):37-45.
16 AJN ▼ September 2002 ▼ Supplement http://www.nursingcenter.com
You might also like
- NCPDocument4 pagesNCPNurhaifa MocademaNo ratings yet
- Summary of Endocrine DisordersDocument2 pagesSummary of Endocrine DisordersKrysny MontebonNo ratings yet
- Linician Pdate: Echo-Doppler HemodynamicsDocument5 pagesLinician Pdate: Echo-Doppler HemodynamicsAlvy SyukrieNo ratings yet
- Drug StudyDocument9 pagesDrug StudyAira Nicole ROMASNo ratings yet
- Nursing Care Plan: Assessment Explanation of The Problem Objectives Interventions Rationale EvaluationDocument2 pagesNursing Care Plan: Assessment Explanation of The Problem Objectives Interventions Rationale EvaluationNelly CruzNo ratings yet
- Steroid Use in The Elderly: Postgraduate MedicineDocument8 pagesSteroid Use in The Elderly: Postgraduate MedicineValdi DwiramaNo ratings yet
- Geriatic Fluid and Electrolyte Imbalance NCPDocument4 pagesGeriatic Fluid and Electrolyte Imbalance NCPCA Candido JavierNo ratings yet
- NCP-ABRUPTIO PLACENTAE - PeregrinoDocument5 pagesNCP-ABRUPTIO PLACENTAE - PeregrinoJOYCE ANN PEREGRINONo ratings yet
- Revised Hypergly NCPDocument15 pagesRevised Hypergly NCPDacillo GailleNo ratings yet
- Post Partum Assessment - Docx CRUZDocument3 pagesPost Partum Assessment - Docx CRUZKariza PerdidoNo ratings yet
- Assessment Cues Nursing Diagnosis Desired Outcome Nursing Intervention Justification EvaluationDocument3 pagesAssessment Cues Nursing Diagnosis Desired Outcome Nursing Intervention Justification EvaluationKristil ChavezNo ratings yet
- AACE Abstracts 2019 Los AngelesDocument357 pagesAACE Abstracts 2019 Los Angelesmimran1974No ratings yet
- Hydrocortisone (Final)Document11 pagesHydrocortisone (Final)Zyla KrisshaNo ratings yet
- Health Teaching Plan: Dontogan, JohannahDocument5 pagesHealth Teaching Plan: Dontogan, JohannahRushnol Jade Piluden-TupacNo ratings yet
- Drugs Used For HypothyroidismDocument8 pagesDrugs Used For HypothyroidismBea SungaNo ratings yet
- Format, Drug StudyDocument23 pagesFormat, Drug StudyKrizzle Mae NeypesNo ratings yet
- Cannabinoid Hyperemesis Syndrome: Marijuana Is Both Antiemetic and ProemeticDocument6 pagesCannabinoid Hyperemesis Syndrome: Marijuana Is Both Antiemetic and ProemeticSilesiaNo ratings yet
- Viral Myocarditis in Children: PediatricDocument24 pagesViral Myocarditis in Children: PediatricRizky Ayu RNo ratings yet
- 10 31 Concept MapDocument1 page10 31 Concept Mapapi-725271439No ratings yet
- Balance Interventions For Diabetic Peripheral.3Document8 pagesBalance Interventions For Diabetic Peripheral.3Michael SelvarajNo ratings yet
- Biodata Name: A.L Age: 5 Mos Date of Birth: November 28, 2020 Status: Single Religion: INC Gender: Female Weight: 5.2kgDocument6 pagesBiodata Name: A.L Age: 5 Mos Date of Birth: November 28, 2020 Status: Single Religion: INC Gender: Female Weight: 5.2kgJohn Rendel LopezNo ratings yet
- CCU NCP Week 2Document4 pagesCCU NCP Week 2April Kate BanagodosNo ratings yet
- 2017 Estado Hiperosmolar Hiperglucemico - 392471761Document8 pages2017 Estado Hiperosmolar Hiperglucemico - 392471761FABIOLA100% (1)
- Endocrinología Y Nutrición: Scientific LettersDocument2 pagesEndocrinología Y Nutrición: Scientific LettersMakmur SejatiNo ratings yet
- Nursing Department: Assessment Explanation of The Problem Objective Interventions Rationale EvaluationDocument2 pagesNursing Department: Assessment Explanation of The Problem Objective Interventions Rationale EvaluationNelly CruzNo ratings yet
- A Review of Current Trends With Type 2 Diabetes Epidemiology, Aetiology, Pathogenesis, Treatments and Future PerspectivesDocument36 pagesA Review of Current Trends With Type 2 Diabetes Epidemiology, Aetiology, Pathogenesis, Treatments and Future PerspectivescastillojessNo ratings yet
- NCP - Dela CruzDocument4 pagesNCP - Dela CruzChristine Dela CruzNo ratings yet
- NCP DengueDocument3 pagesNCP DengueJane MinNo ratings yet
- EndokrinDocument5 pagesEndokrinAnonymous plYGwXNo ratings yet
- Knowledge Deficit Related To HypertensionDocument2 pagesKnowledge Deficit Related To HypertensionChenee Mabulay100% (1)
- Bad Medicine: Red Drugs: ReferenceDocument1 pageBad Medicine: Red Drugs: ReferenceAntar InenigogNo ratings yet
- NCPsDocument11 pagesNCPsJobelle AcenaNo ratings yet
- Albuterol SulfateDocument1 pageAlbuterol SulfatechristinechaellemorenoNo ratings yet
- Enhancing Case Detection of Selected Inherited Disorders Through Expanded Newborn Screening in The PhilippinesDocument7 pagesEnhancing Case Detection of Selected Inherited Disorders Through Expanded Newborn Screening in The PhilippinesDerekBryanNo ratings yet
- Pharma S02 SBR05 Le02Document14 pagesPharma S02 SBR05 Le02sky vallartaNo ratings yet
- De Guzman NCP GDMDocument4 pagesDe Guzman NCP GDMCameron De GuzmanNo ratings yet
- De Guzman, Cameron Josh B. APRIL 26, 2021 2BSN-B RLENCM109Document4 pagesDe Guzman, Cameron Josh B. APRIL 26, 2021 2BSN-B RLENCM109Cameron De GuzmanNo ratings yet
- Care of A Client With Diabetic Ketoacidosis FDocument33 pagesCare of A Client With Diabetic Ketoacidosis FHananNo ratings yet
- Health Teaching PlanDocument6 pagesHealth Teaching PlanLay YoungNo ratings yet
- Machate - Kia - Belle A. BSN 4a LP1 NCM 118Document9 pagesMachate - Kia - Belle A. BSN 4a LP1 NCM 118Arriane AndoyoNo ratings yet
- 3.1 Management of Obesity in Cardiovascular  PracticeDocument19 pages3.1 Management of Obesity in Cardiovascular  PracticeChemicol QuimicosNo ratings yet
- Conns Syndrome Gonzales NickaDocument10 pagesConns Syndrome Gonzales Nickamafeehney feehilyNo ratings yet
- Ayuno IntermitenteDocument11 pagesAyuno IntermitenteJavierNo ratings yet
- 27 A Case Study - Renal TransplantDocument13 pages27 A Case Study - Renal TransplantJesseniaCinthia100% (1)
- Drug StudyDocument4 pagesDrug StudyPAULA MAE F. ALMEIDANo ratings yet
- Risk For Deficient Fluid Volume Related To Ultrafiltration, Fluid Restrictions, And/or Actual BloodDocument2 pagesRisk For Deficient Fluid Volume Related To Ultrafiltration, Fluid Restrictions, And/or Actual BloodJakeNo ratings yet
- DRUG STUDY - AminophyllineDocument2 pagesDRUG STUDY - AminophyllineKian Herrera100% (1)
- The Appropriate Amount of Oxygen Is Continuously Delivered So That The Patient Does Not DesiderateDocument4 pagesThe Appropriate Amount of Oxygen Is Continuously Delivered So That The Patient Does Not DesideratezheeraNo ratings yet
- Cues/Needs Nursing Diagnosis Scientific Explanation Goals and Objectives Nursing Intervention Rationale Evaluation Short Term Independent Short TermDocument2 pagesCues/Needs Nursing Diagnosis Scientific Explanation Goals and Objectives Nursing Intervention Rationale Evaluation Short Term Independent Short TermLatrell GelacioNo ratings yet
- Diabetes Nursing Care Plan (AutoRecovered)Document2 pagesDiabetes Nursing Care Plan (AutoRecovered)SORIA CHOCNo ratings yet
- 01 Hyp 11 3 288 PDFDocument11 pages01 Hyp 11 3 288 PDFSaif ALFALAHYNo ratings yet
- Nursing Care Plan MulletDocument4 pagesNursing Care Plan MulletMARLA PHOEBE KYTE MULLETNo ratings yet
- Quiz 7. NCM 116 For StudentsDocument4 pagesQuiz 7. NCM 116 For StudentsZayne Lucas Gabrielle TadiamonNo ratings yet
- Cues Nursing Diagnos IS Analysis Planning Intervention Rationale EvaluationDocument7 pagesCues Nursing Diagnos IS Analysis Planning Intervention Rationale EvaluationLoriejae Marie DesulocNo ratings yet
- NCP - Chicken PoxDocument4 pagesNCP - Chicken Poxhanna_lim0% (1)
- NCM 109-NCP - PeregrinoDocument2 pagesNCM 109-NCP - PeregrinoJOYCE ANN PEREGRINONo ratings yet
- 2016 ' Pravin M RathiDocument2 pages2016 ' Pravin M RathiEgahasaniaNo ratings yet
- Drug Study TemplateDocument2 pagesDrug Study TemplateMary hope DomalaonNo ratings yet
- Pharmacology for Student and Pupil Nurses and Students in Associated ProfessionsFrom EverandPharmacology for Student and Pupil Nurses and Students in Associated ProfessionsNo ratings yet
- Primary Chest Wall TumorsDocument13 pagesPrimary Chest Wall Tumorsmhany12345No ratings yet
- نسخة ENDO-17-2Document16 pagesنسخة ENDO-17-2Sami MdNo ratings yet
- Tamil For MedicosDocument17 pagesTamil For Medicos51921684No ratings yet
- Focus Data Action ResponseDocument3 pagesFocus Data Action ResponseSitty Aizah MangotaraNo ratings yet
- Nursing Respiratory SystemDocument254 pagesNursing Respiratory SystemWendy EvansNo ratings yet
- Endocrine Hypertension in Small Animals 2010 Veterinary Clinics of North America Small Animal PracticeDocument18 pagesEndocrine Hypertension in Small Animals 2010 Veterinary Clinics of North America Small Animal PracticeEduardo PalaciosNo ratings yet
- Albumin in Liver Cirrhosis, SADocument37 pagesAlbumin in Liver Cirrhosis, SADwinita ViviantiNo ratings yet
- VIKKI13Document6 pagesVIKKI13Dillisrinivasarao NNo ratings yet
- Prosthetic Management - Transtibial Amputation Part 12Document25 pagesProsthetic Management - Transtibial Amputation Part 12Marizandi BothaNo ratings yet
- Arthritis and SaturnDocument4 pagesArthritis and SaturnJatinder SandhuNo ratings yet
- Liver Curs 2009Document215 pagesLiver Curs 2009Mohammad_Islam87No ratings yet
- Ns. ASMAT BURHAN, S.Kep., M.Kep., ETNDocument4 pagesNs. ASMAT BURHAN, S.Kep., M.Kep., ETNburhanNo ratings yet
- Renal and Urinary DisordersDocument11 pagesRenal and Urinary DisordersChristian Espanilla100% (4)
- The Gallbladder Diseases Bile Duct StoneDocument69 pagesThe Gallbladder Diseases Bile Duct Stoneحميد حيدرNo ratings yet
- IntussusceptionDocument2 pagesIntussusceptionrising starNo ratings yet
- Phenylketonuria: Martha Blair Gwaltney Medical Genetics R Ostrowski, Phd. and L. Mcnally, M.S. July 13, 2002Document8 pagesPhenylketonuria: Martha Blair Gwaltney Medical Genetics R Ostrowski, Phd. and L. Mcnally, M.S. July 13, 2002Luisa Gadis Tri WahyuniNo ratings yet
- Pathophysiology of Myocardial Infarction (STEMI)Document2 pagesPathophysiology of Myocardial Infarction (STEMI)michaela100% (3)
- Addictive and Unhealthy Behaviors OvertrainingDocument4 pagesAddictive and Unhealthy Behaviors OvertrainingSophia Marie YakitNo ratings yet
- Post Insertion ProblemsDocument22 pagesPost Insertion Problemsزياد حميد رشيدNo ratings yet
- Copy1-Epidemiology Module 1Document50 pagesCopy1-Epidemiology Module 14ttf68m5j5No ratings yet
- Developing A Pharmaceutical Care PlanDocument2 pagesDeveloping A Pharmaceutical Care PlanRiga 'Azoe' AlrianiNo ratings yet
- Polio in NigeriaDocument24 pagesPolio in NigeriaWande AyodeleNo ratings yet
- Hope 4 (2ND Sem) - Module 5Document2 pagesHope 4 (2ND Sem) - Module 5Gleany lisle SarifaNo ratings yet
- Assessing Fitness To Drive A Guide For Medical ProfessionalsDocument135 pagesAssessing Fitness To Drive A Guide For Medical Professionalsarun kumarNo ratings yet
- HypothyroidismDocument90 pagesHypothyroidismwiwi_13No ratings yet
- Guidance For Daily COVID-19 Screening of Staff and VisitorsDocument2 pagesGuidance For Daily COVID-19 Screening of Staff and VisitorsBartNo ratings yet
- SIMULASI+UAS+D3+KEP+2021 - Hikmah FitriaDocument6 pagesSIMULASI+UAS+D3+KEP+2021 - Hikmah FitriaHikmah FitriaNo ratings yet
- Esophageal Disorder Part IIDocument27 pagesEsophageal Disorder Part IIJuma AwarNo ratings yet
- An Overview of Autoimmune and Paraneoplastic EncefaliteDocument14 pagesAn Overview of Autoimmune and Paraneoplastic Encefaliterafael rocha novaesNo ratings yet
- BAXIE (M-UE-22) : Eight PathogensDocument1 pageBAXIE (M-UE-22) : Eight Pathogensray72roNo ratings yet