Professional Documents
Culture Documents
Trigger Finger-An Overview of The Treatment Options
Uploaded by
Satrya DitaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Trigger Finger-An Overview of The Treatment Options
Uploaded by
Satrya DitaCopyright:
Available Formats
CME
Trigger finger: An overview
of the treatment options
Amber Matthews, PA-C, MPAM; Kristen Smith, PA-C, MPAM;
Laura Read, PA-C; Joyce Nicholas, PhD; Eric Schmidt, PhD
Downloaded from http://journals.lww.com/jaapa by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3tjcLwhL8g9Z3Vs3ea2BckBWIrYfkaiKgBRS2RdyoanM= on 09/23/2020
ABSTRACT
Stenosing flexor tenosynovitis, more commonly known as
trigger finger, is one of the most common causes of hand
pain and dysfunction. Clinicians must be able to identify the
disorder, know the broad range of treatment options, and
counsel patients on the treatment best suited for their condi-
tion. Awareness of the economic burden each option entails
is central to optimizing treatment outcomes and patient
satisfaction.
Keywords: trigger finger, stenosing flexor tenosynovitis, A1
pulley, audible snap, flexion contracture, flexor tendon nodule
Learning objectives
Describe the typical presentation of a patient with trigger
finger.
List the commonly used treatments to manage symptoms
of trigger finger.
Describe the economic effect of the various treatment
options with regards to therapeutic decision-making.
A
53-year-old woman presents to her primary care
provider with a 1-week history of pain and tender-
ness at the base of her right ring finger that has
worsened in the past 2 days. She describes the pain as a
cramping sensation that radiates from her ring finger to
her palm and occurs with flexion and extension of the
digit. When the symptoms started 1 week ago, she only
experienced a painless clicking when bending her fingers.
But over the past 2 days, her finger has locked in the bent
position, forcing her to use her other hand to straighten
it. The patient says that her symptoms seem to be worse At the time this article was written, Amber Matthews and Kristen Smith
in the morning and get progressively better throughout the were students in the PA program at the University of Lynchburg in
day. She denies any recent trauma to the affected finger Lynchburg, Va. Ms. Matthews now practices pediatrics at Blue Ridge
© PEERAYOT / SHUTTERSTOCK
and has never encountered similar symptoms in the past. Medical Center in Arrington, Va. Ms. Smith now practices critical
care at Central Lynchburg General Hospital. Laura Read is director of
She took 400 mg of ibuprofen twice a day for the past 2
didactic education in the PA program at the University of Lynchburg.
days with no relief of symptoms. Joyce Nicholas is director of evaluation, assessment, and compliance
The patient’s fourth digit appears nonerythematous with in the PA program at the University of Lynchburg. Eric Schmidt is an
no swelling or warmth. She exhibits tenderness to palpa- assistant professor at the University of Lynchburg. The authors have
tion just proximal to the metacarpophalangeal flexion disclosed no potential conflicts of interest, financial or otherwise.
crease of the fourth digit. A tender nodule also is present DOI:10.1097/01.JAA.0000550281.42592.97
in this area. The patient is able to make a tight fist with Copyright © 2019 American Academy of Physician Assistants
JAAPA Journal of the American Academy of Physician Assistants www.JAAPA.com 17
Copyright © 2019 American Academy of Physician Assistants
CME
Key points hypertrophy and sheath narrowing that prevent the tendon
from sliding smoothly in the sheath and result in a catch-
Trigger finger is a common cause of hand pain and
ing or locking sensation.3 Because the greatest degree of
dysfunction with a bimodal distribution in patients under
force occurs at the first annular (A1) sheath overlying the
age 8 years and those ages 40 to 60 years.
proximal interphalangeal joint, this sheath is the one most
No universally accepted tool exists for classifying or
commonly affected in patients with trigger finger.1 Chuang
treating trigger finger.
and colleagues examined cadaver digits and found that
Surgery is typically indicated for patients who continue
when the finger flexes, the flexor tendon diameter increases
to experience pain and locking after treatment with
conservative measures and corticosteroid injections. as the tendon moves proximally through the sheaths. This
would explain why tendon hypertrophy makes trigger
Trigger finger is more common in patients with diabetes
and related disorders such as carpal tunnel syndrome fingers progressively difficult to extend.7
and limited joint mobility. In children, however, most research indicates that trigger
thumb is caused by a developmental size mismatch in the
diameter of the flexor pollicis longus (FPL) tendon and its
her right hand but the ring finger remains in the flexed annular sheath.8 Why this anomaly occurs remains unclear.
position when she is asked to extend her fingers. An Through a study of serial ultrasounds, Verma and colleagues
audible snap is appreciated when the finger is passively reinforced the idea that pediatric trigger thumb is a devel-
extended using the contralateral hand. opmental condition. All 56 trigger thumbs demonstrated
focal enlargement of the FPL without evidence of inflam-
ABOUT TRIGGER FINGER mation or trauma.9 This is in contrast to the pathophysiol-
The patient has a classic presentation of stenosing flexor ogy of trigger finger in adults. Alternatively, trigger finger
tenosynovitis, commonly known as trigger finger. This in a child is 10 times less likely to be seen than trigger
condition is one of the most common causes of hand pain thumb.8 Studies propose that a trigger digit other than the
in adults, affecting women six times more frequently than thumb in a child may suggest an underlying pathology,
men. It is most common in patients ages 40 to 60 years, such as an inflammation or infection.8
and often is found in the dominant hand, especially the
fourth digit.1 Lifetime prevalence of trigger finger is 2% DIAGNOSIS
to 3% in the general population, and up to 10% in patients Role of ultrasound The diagnosis of trigger finger is made
with diabetes.2 In children, the condition is most common clinically based on the patient’s presenting symptoms and
in those under age 8 years, affects boys and girls equally, physical examination. However, ultrasound is increasingly
and is more common in the thumb.3 being used to aid in diagnosis. Using ultrasound to measure
Trigger finger is thought to be idiopathic, although there the thickening of the affected sheath compared with unaf-
is a correlation with repetitive use of the affected hand as fected sheaths on the same hand has been shown to be as
well as history of diabetes, particularly type 1 diabetes.2,4 accurate as direct measurements during surgery.10 The
Although no studies indicate the specificity or sensitivity degree of thickening seen on ultrasound is correlated with
of trigger finger as a diagnostic predictor of diabetes, symptom severity.11
multiple trigger digits are more common in patients with Grading Although no universal grading system exists for
diabetes. Consider screening patients for diabetes if they trigger finger, several similar models have been proposed.12
have no known history of diabetes and multiple trigger None of these models have been accepted as the gold
digits.4 standard but they can be used to assess severity and assist
Other disorders of the upper extremities that are more in selecting the appropriate referral and treatment options.
common in patients with diabetes include carpal tunnel
syndrome, adhesive capsulitis of the shoulder, limited joint
mobility, and Dupuytren contracture.5 These conditions FIGURE 1. Lateral depiction of the fourth digit
seem to be related to poor glycemic control.6 The role of
diabetes in predisposing patients to these upper extremity
ILLUSTRATION BY AMBER MATTHEWS
Flexor
conditions is thought to be an indicator of microvascular tendon
A1 pulley
complications of the disease.5 A2
A3
When patients flex a finger, the flexor tendon passes A4 A5
through a series of sheaths called annular and cruciform
pulleys (Figure 1). These sheaths encapsulate the tendon,
preventing it from separating from the bone when the
finger is flexed, and letting the tendon glide smoothly back
and forth during flexion and extension.1 Trauma such as
repetitive use or compression forces can cause tendon Cruciform pulleys
18 www.JAAPA.com Volume 32 • Number 1 • January 2019
Copyright © 2019 American Academy of Physician Assistants
Trigger finger: An overview of the treatment options
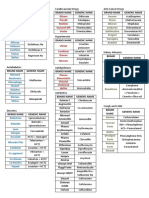
The grading system in Table 1, developed by Quinnell and
modified by Green, has been used in many trigger finger TABLE 1. Clinical classification of trigger finger
studies.12
Differential diagnosis Conditions that can lead to lock- Pain and history of catching, but not
ing, pain, loss of motion, and swelling of the metacarpo- Grade I;
demonstrable on physical examina-
phalangeal joints include a fracture or dislocation. In many Pretriggering
tion. Tenderness over A1 pulley.
instances, clinicians misjudge the flexor tendon nodule for
a bony mass.8 With a quick history and physical examina-
tion, a fracture can be easily ruled out, especially if the Grade II; Demonstrable catching, but the
patient has no history of trauma. Active patient can actively extend the digit.
In adults with pain and a locking sensation of a digit,
the differential diagnosis includes Dupuytren contracture,
diabetic cheiroarthropathy, metacarpophalangeal joint Demonstrable catching requiring
Grade III;
sprain, calcific peritendinitis, noninfectious tenosynovitis, passive extension (Grade IIIA) or
Passive
infectious tenosynovitis, rheumatoid arthritis, osteoarthri- inability to actively flex (Grade IIIB).
tis, and crystalline arthropathy (Table 2).13,14
In children, trigger thumb sometimes can be confused
Demonstrable catching with a fixed
with a far-reaching diagnosis of cerebral palsy or arthro- Grade III;
flexion contracture of the proximal
gryposis.15 The deformities caused by cerebral palsy and Contracture
interphalangeal joint.
arthrogryposis are believed to be caused by inappropriate
differentiation of connective tissues in the hand.8 Although
Reprinted with permission from Wolfe SW, Pederson WC, Hotchkiss RN,
these disorders have a similar presentation to trigger finger, et al. Green’s Operative Hand Surgery. 7th ed. Philadelphia, PA: Elsevier; 2016.
their developmental cause and features are very different.
Children with cerebral palsy and arthrogryposis are easily
differentiated from those with trigger finger by other pathologies such as tennis elbow and plantar fasciitis but
abnormalities beyond the digits of the hand. is just beginning to be studied in patients with trigger
finger. After transducer gel is applied to the patient’s skin
TREATMENT above the affected tendon, a probe is placed to deliver a
Treatments for trigger finger range from conservative to shock wave. The mechanism of this therapy is not com-
invasive. pletely understood but ESWT may cause inflammation
Noninvasive options Initial management of mild-to- and stimulate the body’s natural healing processes.20 ESWT
moderate trigger finger symptoms may consist of a com- is an option for patients who do not wish to undergo
bination of nonsteroidal anti-inflammatory agents injections or surgery.
(NSAIDs), massage, heat, and/or ice. Splinting the digit in Surgery Surgical options include open surgical release
an extended position also can help rest the tendon and let and percutaneous release of the A1 sheath. Open surgical
the inflamed sheath heal.16 Exercises and passive stretches release traditionally is used as first-line treatment in children,
have been attempted in many patients but no research especially those with congenital trigger thumb. Conserva-
supports a clinically proven or widely accepted exercise tive management can be attempted in children but is his-
model. Passive stretching and splinting are more commonly torically unsuccessful.8 In adults, surgery is typically reserved
used in children to avoid surgical management.8 for patients with severe trigger finger that has failed con-
Corticosteroid injections If conservative management servative management. Although open surgical release has
fails, the first-line treatment is corticosteroid injections been practiced longer, no significant disparity in failure
directly into the inflamed tendon sheath.17 For many rate or number of complications exists between it and
patients, a single injection provides relief for up to 10 percutaneous release.21 Risks of both types of surgery
years.18 A second and occasionally third corticosteroid include nerve injury and incomplete release, and neither
injection may be given 4 to 6 months apart, but typically is widely accepted as superior at this time. Patients may
the case is considered refractory and referred for surgical prefer percutaneous release because it is less invasive;
management after two to three unsuccessful treatment surgeons may prefer open surgery because of better visibil-
attempts. Adverse reactions to corticosteroid injections are ity of the surgical field.21
rare but include fat necrosis or pigment changes at the Endoscopic release techniques, which improve visualiza-
injection site, infection, and tendon rupture.17 tion for surgeons and reduce scarring and healing time for
Extracorporeal shock wave therapy (ESWT) A newer patients, have been attempted.22 Endoscopy also reduces
alternative to corticosteroid injections, ESWT is as effec- the risk of nerve or tendon injury. However, this approach
tive in symptom management.19 This noninvasive therapy requires surgeons to master a new technique and facilities
has been used for years for various other soft-tissue to obtain more sophisticated, costly instruments.22
JAAPA Journal of the American Academy of Physician Assistants www.JAAPA.com 19
Copyright © 2019 American Academy of Physician Assistants
CME
COSTS OF TREATMENT
TABLE 2. Differential diagnosis for trigger finger13, 14 Trigger finger is a common issue with a variety of accept-
able treatments. Clinicians should include the cost of each
A painless nodular lesion in the palmar
Dupuytren option when discussing treatment with patients. A patient’s
contracture fascia that progresses over time to form a
comorbidities play a role in which treatment option is
fibrous cord extending from palm to digit.
most cost effective. Luther and colleagues compared four
Diabetic Limited ability to fully extend the different treatment strategies for trigger finger in patients
cheiroar- metacarpophalangeal joints and inter- with diabetes: one corticosteroid injection followed by
thropathy phalangeal joint. surgical release, two corticosteroid injections followed by
Metacarpo- surgical release, immediate surgical release in an OR, and
phalangeal Suspect this if the patient has a history
immediate surgical release in a clinic.23 They found that
joint sprain of trauma and absence of triggering.
immediate surgical release in the clinic was the least costly
Characterized by significant pain and treatment for patients with diabetes.23 Corticosteroid
Calcific erythema so severe it may stimulate injections are less efficacious in patients with diabetes,
peritendinitis infection. Fluffy calcification on who often need surgery even after injections. In addition,
radiograph. corticosteroid injections can increase blood glucose levels
in patients with diabetes.
Characterized by swelling and pain
Noninfectious A cost analysis study by Kerrigan and colleagues found
tenosynovitis along the long axis of affected tendon
that the most cost-effective treatment for trigger finger in
or joints of finger.
the general population is a corticosteroid injection followed
Characterized by severe pain, erythe- by a second injection for failures or recurrence, followed
ma, and swelling along the long axis by definitive surgery, if needed.24 For one or two cortico-
Infectious
tenosynovitis of affected tendon or joints of finger, steroid injections to be the most cost-effective strategy in
particularly following a puncture or patients with diabetes, injection failure rates would need
bite wound. to be less than 36% and 34%, respectively.23
Characterized by joint pain, tenderness,
swelling, or stiffness lasting 6 weeks or CONCLUSION
longer. Typically polyarticular, affect- Trigger finger is one of the most common diagnoses of
ing small joints symmetrically and hand pain in adults. Nearly all patients complain of some
bilaterally. Boutonniere and Swan-neck level of discomfort and locking of a digit that is worse in
Rheumatoid
arthritis deformities of the distal interphalan- the morning or after repetitive use of their hands through-
geal joint and proximal interphalangeal out the day. Studies suggest that the best and most cost-
joint joints may be present. Metacar- effective treatment is immediate surgical release in the clinic
pophalangeal joints may exhibit ulnar (for patients with diabetes) and one to two corticosteroid
deviation. Also can affect organs and injections, followed by definitive surgery, if needed (for
body systems as well. patients without diabetes).23,24 Although this is not the
standard of care, cost and patient comorbidities should be
Characterized by swelling, tenderness,
included in therapeutic decision-making when treating
and erythema particularly first thing in
patients with trigger finger. JAAPA
the morning, and after resting or ex-
tended activity. Gradual symptom on- Earn Category I CME Credit by reading both CME articles in this issue,
Osteoarthritis set typically involving multiple joints. reviewing the post-test, then taking the online test at http://cme.aapa.org.
Heberden nodes on the distal interpha- Successful completion is defined as a cumulative score of at least 70%
langeal joint joint and Bouchard nodes correct. This material has been reviewed and is approved for 1 hour of
clinical Category I (Preapproved) CME credit by the AAPA. The term of
on the proximal interphalangeal joint
approval is for 1 year from the publication date of January 2019.
joint may be present. Bone spurs may
be evident on radiograph. REFERENCES
Characterized by episodes or attacks 1. Jeanmonod R, Waseem M. Trigger Finger. Treasure Island, FL:
StatPearls Publishing; 2017.
that last for days to weeks. Joint may be
2. Makkouk AH, Oetgen ME, Swigart CR, Dodds SD. Trigger
hot, erythematous, swollen, stiff, and finger: etiology, evaluation, and treatment. Curr Rev Musculo-
Crystalline
exquisitely tender. Fever can accom- skelet Med. 2008;1(2):92-96.
arthropathy
pany an acute attack. Joint aspiration 3. Parks E. The hand, wrist, and elbow. In: Practical Office
reveals negative birefringence (gout) or Orthopedics. New York, NY: McGraw-Hill Education; 2017.
positive birefringence (pseudogout). 4. Koh S, Nakamura S, Hattori T, Hirata H. Trigger digits in
diabetes: their incidence and characteristics. J Hand Surg Eur Vol.
2010;35(4):302-305.
20 www.JAAPA.com Volume 32 • Number 1 • January 2019
Copyright © 2019 American Academy of Physician Assistants
Trigger finger: An overview of the treatment options
5. Ramchurn N, Mashamba C, Leitch E, et al. Upper limb musculo- 15. Twu J, Angeles J. Developmental trigger thumb. Pediatr Ann.
skeletal abnormalities and poor metabolic control in diabetes. 2016;45(4):e135-e138.
Eur J Intern Med. 2009;20(7):718-721. 16. Colbourn J, Heath N, Manary S, Pacifico D. Effectiveness of
6. Mustafa KN, Khader YS, Bsoul AK, Ajlouni K. Musculoskeletal splinting for the treatment of trigger finger. J Hand Ther.
disorders of the hand in type 2 diabetes mellitus: prevalence and 2008;21(4):336-343.
its associated factors. Int J Rheum Dis. 2016;19(7):730-735. 17. Ryzewicz M, Wolf JM. Trigger digits: principles, management,
7. Chuang XL, Ooi CC, Chin ST, et al. What triggers in trigger finger? and complications. J Hand Surg Am. 2006;31(1):135-146.
The flexor tendons at the flexor digitorum superficialis bifurcation. 18. Wojahn RD, Foeger NC, Gelberman RH, Calfee RP. Long-term
J Plast Reconstr Aesthet Surg. 2017;70(10):1411-1419. outcomes following a single corticosteroid injection for trigger
8. Bauer AS, Bae DS. Pediatric trigger digits. J Hand Surg Am. finger. J Bone Joint Surg Am. 2014;96(22):1849-1854.
2015;40(11):2304-2309. 19. Yildirim P, Gultekin A, Yildirim A, et al. Extracorporeal shock
9. Verma M, Craig CL, DiPietro MA, et al. Serial ultrasound wave therapy versus corticosteroid injection in the treatment of
evaluation of pediatric trigger thumb. J Pediatr Orthop. trigger finger: a randomized controlled study. J Hand Surg Eur
2013;33(3):309-313. Vol. 2016;41(9):977-983.
10. Spirig A, Juon B, Banz Y, et al. Correlation between sonographic 20. Malliaropoulos N, Jury R, Pyne D, et al. Radial extracorporeal
and In Vivo measurement of A1 pulleys in trigger fingers. shockwave therapy for the treatment of finger tenosynovitis
Ultrasound Med Biol. 2016;42(7):1482-1490. (trigger digit). Open Access J Sports Med. 2016;7:143-151.
11. Kim SJ, Lee CH, Choi WS, et al. The thickness of the A2 pulley 21. Wang J, Zhao JG, Liang CC. Percutaneous release, open
and the flexor tendon are related to the severity of trigger finger: surgery, or corticosteroid injection, which is the best treatment
results of a prospective study using high-resolution ultrasonogra- method for trigger digits? Clin Orthop Relat Res. 2013;471(6):
phy. J Hand Surg Eur Vol. 2016;41(2):204-211. 1879-1886.
12. Wolfe SW, Pederson WC, Hotchkiss RN, et al. Green’s 22. Pegoli L, Cavalli E, Cortese P, et al. A comparison of endoscopic
Operative Hand Surgery. 7th ed. Philadelphia, PA: Elsevier; and open trigger finger release. Hand Surg. 2008;13(3):147-151.
2016:1908. 23. Luther GA, Murthy P, Blazar PE. Cost of immediate surgery
13. Blazar P, Aggarwal R. Trigger finger (stenosing flexor tenosyno- versus non-operative treatment for trigger finger in diabetic
vitis). www.uptodate.com/contents/trigger-finger-stenosing- patients. J Hand Surg Am. 2016;41(11):1056-1063.
flexor-tenosynovitis. Accessed September 19, 2018. 24. Kerrigan CL, Stanwix MG. Using evidence to minimize the
14. Arthritis Foundation. Types of arthritis. www.arthritis.org/ cost of trigger finger care. J Hand Surg Am. 2009;34(6):
about-arthritis/types. Accessed September 19, 2018. 997-1005.
JAAPA Journal of the American Academy of Physician Assistants www.JAAPA.com 21
Copyright © 2019 American Academy of Physician Assistants
You might also like
- Geriatric Nursing Review QuestionsDocument30 pagesGeriatric Nursing Review QuestionsPortia Dulce Toquero86% (88)
- Case Study Cleft LipDocument55 pagesCase Study Cleft LipJaya Prabha50% (10)
- Trigger Point Therapy for Myofascial Pain: The Practice of Informed TouchFrom EverandTrigger Point Therapy for Myofascial Pain: The Practice of Informed TouchRating: 4 out of 5 stars4/5 (5)
- AAO FDM Indroduction 1994 PDFDocument12 pagesAAO FDM Indroduction 1994 PDFHONGJYNo ratings yet
- Occlusal Splints and Temporomandibular Disorders: Why, When, How?Document5 pagesOcclusal Splints and Temporomandibular Disorders: Why, When, How?blogger bloggerNo ratings yet
- Treatment of Common Congenital Hand Conditions.43Document13 pagesTreatment of Common Congenital Hand Conditions.43Ioana BarcariNo ratings yet
- Monoarthritis Ellis 2019Document7 pagesMonoarthritis Ellis 2019castillojessNo ratings yet
- Conservative Temporomandibular Disorder Management: What DO I Do? Frequently Asked QuestionsDocument9 pagesConservative Temporomandibular Disorder Management: What DO I Do? Frequently Asked QuestionsTayyuba AslamNo ratings yet
- v1 - T.I.M.E. 2.0 Swanson (2019) Eif - 0619Document2 pagesv1 - T.I.M.E. 2.0 Swanson (2019) Eif - 0619Samuel GarciaNo ratings yet
- The Efficacy of Manual Therapy For Rotator Cuff Tendinopathy: A Systematic Review and Meta AnalysisDocument21 pagesThe Efficacy of Manual Therapy For Rotator Cuff Tendinopathy: A Systematic Review and Meta AnalysisJacinta SeguraNo ratings yet
- ArthrocentesisDocument10 pagesArthrocentesisPranave PNo ratings yet
- TMD For Fifth Stage Students 2023Document19 pagesTMD For Fifth Stage Students 2023wxmdkhbyvkNo ratings yet
- O Dfen 2012152 P 202Document26 pagesO Dfen 2012152 P 202Nugraha AnggaNo ratings yet
- Orthognathic Surgery and TMJ PatientsDocument14 pagesOrthognathic Surgery and TMJ PatientsDIANA PAOLA FONTECHA GONZÁLEZNo ratings yet
- Badel Michigan Splint and Treatment PDFDocument9 pagesBadel Michigan Splint and Treatment PDF謎超人No ratings yet
- Cooper2014 Revisão Do Trabalho Do ManfrediniDocument21 pagesCooper2014 Revisão Do Trabalho Do ManfrediniFernando VonoNo ratings yet
- Journal of Hand Therapy: Scienti Fic/clinical ArticleDocument5 pagesJournal of Hand Therapy: Scienti Fic/clinical Articleida ayu astitiNo ratings yet
- Análise Artigo AndersonDocument5 pagesAnálise Artigo AndersonJoana NoronhaNo ratings yet
- Arthritis and Rheumatism: Seminars inDocument8 pagesArthritis and Rheumatism: Seminars inAnuj MehtaNo ratings yet
- 6 Nagata2015Document10 pages6 Nagata2015Adrian Pereyra PozoNo ratings yet
- Terapia Manual para Los Trastornos Temporomandibulares - Una Revision de La Literarura.Document7 pagesTerapia Manual para Los Trastornos Temporomandibulares - Una Revision de La Literarura.Pamela ✬No ratings yet
- RCDSO Guidelines Diagnosis and Management of TMDDocument12 pagesRCDSO Guidelines Diagnosis and Management of TMDdoctorlupuNo ratings yet
- Tenderness On Palpation and Occlusal Abnormalities in Temporomandibular DysfunctionDocument7 pagesTenderness On Palpation and Occlusal Abnormalities in Temporomandibular Dysfunctiondavidcosmin186832No ratings yet
- Ensaio Clínico de Terapia Manual No Tratamento Da Condromalácia PatelarDocument4 pagesEnsaio Clínico de Terapia Manual No Tratamento Da Condromalácia PatelarLeticia ZaniniiNo ratings yet
- When The Therapist's Traumas Emerge in A Psychotherapy Session: The Use of Trauma-Related CountertransferenceDocument9 pagesWhen The Therapist's Traumas Emerge in A Psychotherapy Session: The Use of Trauma-Related CountertransferenceMaroeska De Sutter100% (1)
- Examination of The Wrist.37Document11 pagesExamination of The Wrist.37Filipe AlbuquerqueNo ratings yet
- Temporomandibular Disorder Terminology No Longer UsefulDocument2 pagesTemporomandibular Disorder Terminology No Longer UsefulUmer HussainNo ratings yet
- Extensor Tendon Injuries 2010 The Journal of Hand SurgeryDocument8 pagesExtensor Tendon Injuries 2010 The Journal of Hand SurgeryProfesseur Christian DumontierNo ratings yet
- IASTM Primer MyoBar PDF UpdatedDocument46 pagesIASTM Primer MyoBar PDF Updatedviorel100% (2)
- Dr. Manjunath Rai, Dr. Sneha Ginimav, Dr. Padmaraj Hegde: Ginwalla's Technique RevisitedDocument6 pagesDr. Manjunath Rai, Dr. Sneha Ginimav, Dr. Padmaraj Hegde: Ginwalla's Technique Revisitedabhishekjha0082No ratings yet
- Principles of Metacarpal and Phalangeal Fracture Management: A Review of Rehabilitation ConceptsDocument19 pagesPrinciples of Metacarpal and Phalangeal Fracture Management: A Review of Rehabilitation ConceptsInas MellanisaNo ratings yet
- Functional Outcome of Carpal Tunnel Syndrome After Exercise Versus Ultrasound DiathermyDocument8 pagesFunctional Outcome of Carpal Tunnel Syndrome After Exercise Versus Ultrasound DiathermyAdelia 102013330No ratings yet
- BASIC PRINCIPLES OF HAND SURGERYDocument22 pagesBASIC PRINCIPLES OF HAND SURGERYFlorin PanduruNo ratings yet
- Hand Edema Treatments ReviewedDocument14 pagesHand Edema Treatments ReviewedRiky SetyawanNo ratings yet
- 1 (3) Effectivenes of Manual Therapy and Home Physical Therapy in Patients With Temporomandibular Disorders A Randomized Controlled Trial PDFDocument7 pages1 (3) Effectivenes of Manual Therapy and Home Physical Therapy in Patients With Temporomandibular Disorders A Randomized Controlled Trial PDFNur Azryani NaimNo ratings yet
- The Effect of Trigger Finger Injection Site On Injection-Related PainDocument6 pagesThe Effect of Trigger Finger Injection Site On Injection-Related PainCemiwiw CemowowNo ratings yet
- A Model For Standardised Documentation in Manual and Massage TherapyDocument7 pagesA Model For Standardised Documentation in Manual and Massage TherapyAnandhu GNo ratings yet
- Craniomandibular Index-ValidityDocument7 pagesCraniomandibular Index-ValidityVALESKA FARIÑA ESPINOSANo ratings yet
- Evaluación de La Eficacia A Corto Plazo de La Terapia Dolor MiofascialDocument8 pagesEvaluación de La Eficacia A Corto Plazo de La Terapia Dolor MiofascialGabriel DelgadoNo ratings yet
- IJFMTDocument8 pagesIJFMTHeni KhoirunisaNo ratings yet
- Epicondilitis PDFDocument6 pagesEpicondilitis PDFJessica PelazzoNo ratings yet
- Videler2010 Pinza Tripode y Op Pulgar en CharcotDocument7 pagesVideler2010 Pinza Tripode y Op Pulgar en CharcotKhristian JaramilloNo ratings yet
- A Retrospective Audit Exploring The Use of RelaxationDocument4 pagesA Retrospective Audit Exploring The Use of Relaxationmaria joseNo ratings yet
- Interprofessional Collaboration in Dentistry: Role of Physiotherapists To Improve Care and Outcomes For Chronic Pain Conditions and Sleep DisordersDocument9 pagesInterprofessional Collaboration in Dentistry: Role of Physiotherapists To Improve Care and Outcomes For Chronic Pain Conditions and Sleep DisordersANTONIO ROMERONo ratings yet
- Static MCP Splint For Conservative Management of Trigger Finger TableDocument1 pageStatic MCP Splint For Conservative Management of Trigger Finger TableMonika SimpsonNo ratings yet
- Pain Mechanisms and Centralized Pain in Temporomandibular DisordersDocument7 pagesPain Mechanisms and Centralized Pain in Temporomandibular DisordersLaurita Ayala ChiquilloNo ratings yet
- Chapter 8. Pain Pathways and Mechanisms of The Pulpodentin Complex - CompressedDocument26 pagesChapter 8. Pain Pathways and Mechanisms of The Pulpodentin Complex - CompressedPaola cruzNo ratings yet
- Cranio®: The Journal of Craniomandibular & Sleep PracticeDocument11 pagesCranio®: The Journal of Craniomandibular & Sleep PracticeAnthony VillafañeNo ratings yet
- (Iii) Extensor Tendon Injuries: Mini-Symposium: Hand InjuriesDocument5 pages(Iii) Extensor Tendon Injuries: Mini-Symposium: Hand InjuriesAndre MaharadjaNo ratings yet
- Complex Injuries of The HandDocument285 pagesComplex Injuries of The HandWilson A. Quintero100% (1)
- Effects of Exercise Therapy On Painful Temporomandibular DisordersDocument7 pagesEffects of Exercise Therapy On Painful Temporomandibular DisordersLaura Espejo SalamancaNo ratings yet
- Borges 2018Document8 pagesBorges 2018Anthony VillafañeNo ratings yet
- 1756 153545044822 25Document4 pages1756 153545044822 25sonuNo ratings yet
- ChiropracticDocument3 pagesChiropracticChorng Jeng TanNo ratings yet
- Eficienc Ia de La 90: Microacupuntura de La Mano en Pacientes Afectados de SacrolumbalgiaDocument6 pagesEficienc Ia de La 90: Microacupuntura de La Mano en Pacientes Afectados de SacrolumbalgiaDani TenaNo ratings yet
- Comparison of Ultrasound and Extracorporeal Shock Wave Therapy in Lateral EpicondylosisDocument6 pagesComparison of Ultrasound and Extracorporeal Shock Wave Therapy in Lateral EpicondylosisWilliam ChienNo ratings yet
- Clinical Evaluation ProceduresDocument6 pagesClinical Evaluation ProceduresMonika WerdiningsihNo ratings yet
- Alivio AmputadosDocument12 pagesAlivio AmputadosJAVIER ANDRÉS ROMEO OSESNo ratings yet
- Journal of Hand Therapy: JHT R C A #257. Scienti Fic/clinical ArticleDocument9 pagesJournal of Hand Therapy: JHT R C A #257. Scienti Fic/clinical Articlegemichan26No ratings yet
- Wang 2018Document10 pagesWang 2018ilham Maulana ArifNo ratings yet
- E000514 FullDocument6 pagesE000514 FullRenan O. Pravatta PivettaNo ratings yet
- GR Up: Ultrasound of Maxillary SinusDocument14 pagesGR Up: Ultrasound of Maxillary SinusSatrya DitaNo ratings yet
- Mapping Aqsha 3: Patient Case SummariesDocument3 pagesMapping Aqsha 3: Patient Case SummariesSatrya DitaNo ratings yet
- Multimodality Imaging of The Paediatric FlatfootDocument17 pagesMultimodality Imaging of The Paediatric FlatfootSatrya DitaNo ratings yet
- Mappimg Kamar 1 Dan 5Document4 pagesMappimg Kamar 1 Dan 5Satrya DitaNo ratings yet
- s12879 021 06687 3Document8 pagess12879 021 06687 3Satrya DitaNo ratings yet
- SHERLY KoreksiDocument14 pagesSHERLY KoreksiSatrya DitaNo ratings yet
- GR Up: Ultrasound of Maxillary SinusDocument14 pagesGR Up: Ultrasound of Maxillary SinusSatrya DitaNo ratings yet
- Nejmoa1800927 PDFDocument12 pagesNejmoa1800927 PDFFelicia HoseaNo ratings yet
- 3726 7036 1 SMDocument7 pages3726 7036 1 SMSOLEHANo ratings yet
- Jurnal Pakai 6 (Patofisiologi, Diagnosis, Gejala)Document13 pagesJurnal Pakai 6 (Patofisiologi, Diagnosis, Gejala)Satrya DitaNo ratings yet
- PSmarkup - BAB 1-6 Eka TantiDocument43 pagesPSmarkup - BAB 1-6 Eka TantiSatrya DitaNo ratings yet
- PDF Inkomtabilitas Darah - CompressDocument10 pagesPDF Inkomtabilitas Darah - CompressSatrya DitaNo ratings yet
- Human Ascariasis: Diagnostics UpdateDocument12 pagesHuman Ascariasis: Diagnostics UpdatekaputriNo ratings yet
- SHERLY KoreksiDocument14 pagesSHERLY KoreksiSatrya DitaNo ratings yet
- Jurnal 1 (Semua) FIXDocument10 pagesJurnal 1 (Semua) FIXSatrya DitaNo ratings yet
- Self-Management Maintenance Inhalation Therapy With EhealthDocument10 pagesSelf-Management Maintenance Inhalation Therapy With EhealthCahaya MultimediaNo ratings yet
- Jurnal Pakai 7 (Semua)Document11 pagesJurnal Pakai 7 (Semua)Satrya DitaNo ratings yet
- Jurnal Pakai 4 (Edefinisi, Etiologi, Gejala, Diagnosis, Tatalaksana, Prognosis)Document10 pagesJurnal Pakai 4 (Edefinisi, Etiologi, Gejala, Diagnosis, Tatalaksana, Prognosis)Satrya DitaNo ratings yet
- Jurnal Pakai 5 (Patofisiologi, Gejala)Document7 pagesJurnal Pakai 5 (Patofisiologi, Gejala)Satrya DitaNo ratings yet
- Jurnal Pakai 2 (Diagnosis, Tatalaksana) Efusi PerikardiumDocument9 pagesJurnal Pakai 2 (Diagnosis, Tatalaksana) Efusi PerikardiumSatrya DitaNo ratings yet
- Jurnal Pakai 3 (Etiologi) Efusi PerikardiumDocument10 pagesJurnal Pakai 3 (Etiologi) Efusi PerikardiumSatrya DitaNo ratings yet
- Jurnal Pakai 4 (Edefinisi, Etiologi, Gejala, Diagnosis, Tatalaksana, Prognosis)Document10 pagesJurnal Pakai 4 (Edefinisi, Etiologi, Gejala, Diagnosis, Tatalaksana, Prognosis)Satrya DitaNo ratings yet
- Jurnal Pakai 6 (Patofisiologi, Diagnosis, Gejala)Document13 pagesJurnal Pakai 6 (Patofisiologi, Diagnosis, Gejala)Satrya DitaNo ratings yet
- Jurnal Pakai 1 (Anatomi)Document1 pageJurnal Pakai 1 (Anatomi)Satrya DitaNo ratings yet
- Jurnal Pakai 3 (Etiologi) Efusi PerikardiumDocument10 pagesJurnal Pakai 3 (Etiologi) Efusi PerikardiumSatrya DitaNo ratings yet
- Jurnal Pakai 5 (Patofisiologi, Gejala)Document7 pagesJurnal Pakai 5 (Patofisiologi, Gejala)Satrya DitaNo ratings yet
- Jurnal Pakai 7 (Semua)Document11 pagesJurnal Pakai 7 (Semua)Satrya DitaNo ratings yet
- Jurnal Pakai 2 (Diagnosis, Tatalaksana) Efusi PerikardiumDocument9 pagesJurnal Pakai 2 (Diagnosis, Tatalaksana) Efusi PerikardiumSatrya DitaNo ratings yet
- Advance in Pediatric DentistryDocument6 pagesAdvance in Pediatric DentistryAgtadila NovitanandaNo ratings yet
- RhabdomyosarcomaDocument11 pagesRhabdomyosarcomaFrancia ToledanoNo ratings yet
- Male Genitals and Inguinal AreaDocument8 pagesMale Genitals and Inguinal AreagayleNo ratings yet
- 2020 Eagle Practical CardiologyDocument24 pages2020 Eagle Practical CardiologyaeliasgvNo ratings yet
- Cinnamon Contact Stomatitis: A Case Report and ReviewDocument2 pagesCinnamon Contact Stomatitis: A Case Report and ReviewDwiNo ratings yet
- MSDS Buffer PH10Document6 pagesMSDS Buffer PH10Ardhy LazuardyNo ratings yet
- #1 Risk For Aspirations DCDocument2 pages#1 Risk For Aspirations DCtanyav26No ratings yet
- Guideline Eeg Pediatric 2012Document60 pagesGuideline Eeg Pediatric 2012Chindia Bunga100% (1)
- Diabetic Retinopathy Disease Classification Using Deep Neural Network and Retina ImagesDocument13 pagesDiabetic Retinopathy Disease Classification Using Deep Neural Network and Retina ImagesIJRASETPublicationsNo ratings yet
- Government College of Nursing Jodhpur: Procedure On-Cordocentesis Subject-Obstetrics & Gynecology Specialty-IDocument4 pagesGovernment College of Nursing Jodhpur: Procedure On-Cordocentesis Subject-Obstetrics & Gynecology Specialty-Ipriyanka100% (2)
- Production Recombinant Therapeutics in E. ColiDocument11 pagesProduction Recombinant Therapeutics in E. ColiStephany Arenas100% (1)
- Shakespeare's Sonnet 147: Obsessive Love as SicknessDocument1 pageShakespeare's Sonnet 147: Obsessive Love as SicknessItrumas SinghNo ratings yet
- DGM Sample Questions - 1Document8 pagesDGM Sample Questions - 1abdulNo ratings yet
- Medicinal plants guide with uses and preparationsDocument6 pagesMedicinal plants guide with uses and preparationsCaroline Kim100% (1)
- Acute Paracetamol Poisoning Case Studies ReviewDocument5 pagesAcute Paracetamol Poisoning Case Studies Reviewbiya ao0No ratings yet
- Final Concept MapDocument7 pagesFinal Concept Mapapi-405374041No ratings yet
- A Belated Confession: Key Open 2Document7 pagesA Belated Confession: Key Open 2Ngoc AnhNo ratings yet
- Pernicious Oral Habits-1 PDFDocument35 pagesPernicious Oral Habits-1 PDFWen Shu GohNo ratings yet
- Colds and Their BenefitsDocument105 pagesColds and Their BenefitsAlmiranteAckbarNo ratings yet
- OBGYN 1st Round 2021 AnsweredDocument14 pagesOBGYN 1st Round 2021 AnsweredMuhammed Mostafa100% (4)
- Theoretical FrameworkDocument27 pagesTheoretical Frameworkcm289867No ratings yet
- Case Study TabhsoDocument7 pagesCase Study TabhsoGina Barredo Bustamante100% (1)
- Physiotherapy Improves Mouth Opening in OSMFDocument9 pagesPhysiotherapy Improves Mouth Opening in OSMFViral ParekhNo ratings yet
- Fundamentals of NursingDocument16 pagesFundamentals of Nursingsorilla_franceschelNo ratings yet
- FNCPDocument8 pagesFNCPALESSANDRA SOFIA AMISTOSONo ratings yet
- AsbestosDocument4 pagesAsbestoskoketsoNo ratings yet
- Example of Delivery NoteDocument1 pageExample of Delivery NoteRuDy RaviNo ratings yet
- Dispensing DrugsDocument1 pageDispensing DrugsIan CalalangNo ratings yet
- Asimetrii MandibulareDocument25 pagesAsimetrii MandibulareBranici OanaNo ratings yet