Professional Documents
Culture Documents
10 1001@jama 2020 9843
Uploaded by
Joko Arif KurniawanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
10 1001@jama 2020 9843
Uploaded by
Joko Arif KurniawanCopyright:
Available Formats
Letters
RESEARCH LETTER were fit with a new N95. We recorded health care worker char-
acteristics, mask type, shifts used, and donnings/doffings. Our
Correlation Between N95 Extended Use and Reuse primary outcome was N95 fit test failure.
and Fit Failure in an Emergency Department Medians for continuous variables were compared using the
Frontline health care workers are at high risk of contracting Wilcoxon log-rank test. Proportions for categorical variables were
severe acute respiratory syndrome coronavirus 2 (SARS- compared using the Fisher exact test. For comparisons, a 2-sided
CoV-2), which causes coronavirus disease 2019 (COVID-19).1 α < .05 was considered statistically significant. Given the high
Personal protective equipment (PPE), including N95 respira- failure rate of duckbill masks, we conducted a sensitivity analy-
to r s ( N 9 5 s) , i s e s s e nt i a l sis to examine the association between the amount of wear time
Audio
for prevention of COVID-19. and fit test failure in only dome-shaped masks. Data were ana-
The Centers for Disease Con- lyzed using Stata version 16 (StataCorp). This study was catego-
trol and Prevention recommends that health care workers dis- rized as exempt by the UCSF institutional review board.
pose of N95s after a single patient encounter. However, it rec-
ommends N95 extended use (wearing the same N95 for Results | Among 68 participants, 66.2% were women and 48.5%
multiple patient encounters) and limited reuse (storing an N95 were nurses. Dome-shaped N95s were used by 51 of 68 (75.0%);
between encounters for use over multiple encounters) dur- 17 of 68 (25.0%) used duckbill N95s. Overall, 38.2% of partici-
ing critical PPE shortages.2,3 There are limited data regarding pants failed the fit test; 12 of 17 (70.6%) duckbill masks failed,
N95 reuse and extended use. Existing studies were con- compared with 14 of 51 (27.5%) dome-shaped masks. Among
ducted in laboratories, not clinical environments.4,5 Inad- wearers of dome-shaped masks, fit test failure was associ-
equate supplies of N95s have forced many emergency depart- ated with increased number of shifts worn (median, 4 shifts
ments to implement various N95 reuse and extended use [interquartile range {IQR}, 3-5] vs 2 shifts [IQR, 1-3]; P < .001),
policies but without empirical evidence of their effective- increased donnings/doffings (median, 15 [IQR, 13-18] vs 8 [IQR,
ness. We examined the prevalence of N95 fit test failure while 4-12]; P < .001), and increased hours worn (14 [IQR, 10-30] vs
reusing 2 common types of N95 masks. 12 [IQR, 6-16]; P = .048) (Table).
Methods | We performed a cross-sectional study of N95 fit at Discussion | This study found duckbill N95s had a high failure
the University of California, San Francisco (UCSF) emergency rate. Failure of dome-shaped masks was associated with in-
department from April 4 to April 6, 2020. We enrolled a con- creased use. N95 failure may contribute to SARS-CoV-2 trans-
venience sample of health care workers (physicians, nurses, mission despite PPE use and deserves further study. Based on
nurse practitioners, physician assistants, and patient care tech- these preliminary data, health systems should closely evalu-
nicians) on their clinical shifts when the researchers were pre- ate N95 fit during extended use or reuse and limit duckbill mask
sent. All had passed a standard Occupational Safety and Health use if alternatives are available.
Administration–mandated N95 fit test within the last 1 to 2 Limitations include the study’s cross-sectional design; a
years. We performed a qualitative fit test of dome-shaped (3M cohort study is needed to determine directionality. The dura-
1860) and duckbill (Kimberly-Clark 46727 or Halyard 46867) tion of wear and number of donnings/doffings were self-
N95s (Figure) during various stages of extended use/reuse using reported and may not be precise or accurate estimates. Pre-
a standardized hood and 3M FT-32 bitter testing solution. If cise time of failure was not measured. Prior studies have shown
participants could taste the solution, they failed the fit test and an inherent N95 fit failure rate,6 which may have affected
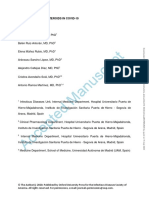
Figure. N95 Mask Types
Left, Dome-shaped. Right, Duckbill.
jama.com (Reprinted) JAMA Published online June 4, 2020 E1
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a Uppsala University User on 06/04/2020
Letters
Table. Characteristics of Participants and Prevalence of Fit Failure (Dome-Shaped Masks Only)
Characteristics Total (N = 51) Fit pass (n = 37) Fit fail (n = 14) P value
Sex, No. (%)
Women 33 (100) 23 (69.7) 10 (30.3)
.74a
Men 18 (100) 14 (77.8) 4 (22.2)
Health care worker type, No. (%)
Nurse 27 (100) 20 (74.1) 7 (25.9)
Physician 11 (100) 7 (63.6) 4 (36.4) .77a
b
PCT/APP/other 13 (100) 10 (76.9) 3 (23.1)
Hours mask worn, median (IQR) 12 (6-18) 12 (6-16) 14 (10-30) .048c
Shifts mask worn, median (IQR) 3 (2-4) 2 (1-3) 4 (3-5) <.001c Abbreviations: APP, advanced
c
practice provider; IQR, interquartile
Donnings/doffings, median (IQR) 10 (5.5-15.5) 8 (4-12) 15 (13-18) <.001 range; PCT, patient care technician.
Shifts mask worn, No. (%) a
By Fisher exact test.
1 11 (100) 11 (100) 0 b
Advanced practice provider
2 12 (100) 11 (91.7) 1 (8.3) includes nurse practitioners and
<.001a physician assistants. Other includes
3 13 (100) 10 (76.9) 3 (23.1)
registration clerks and pharmacists.
>3 15 (100) 5 (33.3) 10 (66.7) c
By 2-sample Wilcoxon rank-sum test.
outcomes. This observational study was subject to confound- Acquisition, analysis, or interpretation of data: All authors.
ing (eg, mask quality, unobserved characteristics of wearer). Drafting of the manuscript: Degesys, Wang, Kwan, Fahimi, Noble.
Critical revision of the manuscript for important intellectual content: All authors.
Shifts worn, hours worn, and donnings/doffings are likely cor- Statistical analysis: Wang, Fahimi.
related: because of the low number of failures, multivariable Administrative, technical, or material support: Degesys, Kwan, Noble.
adjustment was not performed. This study was designed to de- Supervision: Degesys, Wang, Noble, Raven.
tect mask failure based on qualitative fit testing. Failed fit tests Conflict of Interest Disclosures: None reported.
may not necessarily result in increased rates of infection. 1. Wu Z, McGoogan JM. Characteristics of and important lessons from the
coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of
72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA.
Nida F. Degesys, MD 2020;323(13):1239-1242. doi:10.1001/jama.2020.2648
Ralph C. Wang, MD, MAS 2. National Institute for Occupational Safety and Health. Guide to the Selection
Elizabeth Kwan, MD and Use of Particulate Respirators: DHHS (NIOSH) Publication 96-101. Centers
Jahan Fahimi, MD, MPH for Disease Control and Prevention. Published January 1996. Accessed May 7,
2020. https://www.cdc.gov/niosh/docs/96-101/default.html
Jeanne A. Noble, MD, MA
Maria C. Raven, MD, MPH 3. National Institute for Occupational Safety and Health. Recommended
guidance for extended use and limited reuse of N95 filtering facepiece
respirators in healthcare settings. Centers for Disease Control and Prevention.
Author Affiliations: Department of Emergency Medicine, University of Published March 2020. Accessed May 7, 2020. https://www.cdc.gov/niosh/
California, San Francisco. topics/hcwcontrols/recommendedguidanceextuse.html#risksextended
Corresponding Author: Nida F. Degesys, MD, Department of Emergency 4. Bergman MS, Viscusi DJ, Zhuang Z, Palmiero AJ, Powell JB, Shaffer RE.
Medicine, University of California, San Francisco, 505 Parnassus Ave, L126, Impact of multiple consecutive donnings on filtering facepiece respirator fit.
San Francisco, CA 94143-0208 (nida.degesys@ucsf.edu). Am J Infect Control. 2012;40(4):375-380. doi:10.1016/j.ajic.2011.05.003
Accepted for Publication: May 20, 2020. 5. Vuma CD, Manganyi J, Wilson K, Rees D. The effect on fit of multiple
Published Online: June 4, 2020. doi:10.1001/jama.2020.9843 consecutive donning and doffing of N95 filtering facepiece respirators. Ann
Author Contributions: Drs Degesys and Wang had full access to all of the data Work Expo Health. 2019;63(8):930-936. doi:10.1093/annweh/wxz060
in the study and take responsibility for the integrity of the data and the accuracy 6. Zhuang Z, Bergman M, Brochu E, et al. Temporal changes in
of the data analysis. filtering-facepiece respirator fit. J Occup Environ Hyg. 2016;13(4):265-274. doi:
Concept and design: All authors. 10.1080/15459624.2015.1116692
E2 JAMA Published online June 4, 2020 (Reprinted) jama.com
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a Uppsala University User on 06/04/2020
You might also like
- Comprehensive Healthcare Simulation: Surgery and Surgical SubspecialtiesFrom EverandComprehensive Healthcare Simulation: Surgery and Surgical SubspecialtiesDimitrios StefanidisNo ratings yet
- Liu 2021 Effectiveness of A 3d-Printed Mask Fitter in An Ophthalmology Setting During COVID-19Document6 pagesLiu 2021 Effectiveness of A 3d-Printed Mask Fitter in An Ophthalmology Setting During COVID-19Jenny MaNo ratings yet
- N95DECON UV Technicalreport v1.2 FinalDocument8 pagesN95DECON UV Technicalreport v1.2 FinalBrandonRojasNo ratings yet
- Jamainternal Sickbertbennett 2021 LD 210021 1618355295.10569Document2 pagesJamainternal Sickbertbennett 2021 LD 210021 1618355295.10569Febri engahuNo ratings yet
- Translate FR en Bloc Opératoir 21-03-23Document7 pagesTranslate FR en Bloc Opératoir 21-03-23BRAHIM SAOUDNo ratings yet
- Dugdale - Filtration Efficiency, Effectiveness, and Availability of N95 Face Masks For COVID-19 PreventionDocument2 pagesDugdale - Filtration Efficiency, Effectiveness, and Availability of N95 Face Masks For COVID-19 PreventionneilNo ratings yet
- Protecting Healthcare Staff From Severe Acute Respiratory Syndrome: Filtration Capacity of Multiple Surgical MasksDocument4 pagesProtecting Healthcare Staff From Severe Acute Respiratory Syndrome: Filtration Capacity of Multiple Surgical MasksRodrigo GarciaNo ratings yet
- Uso de MáscarasDocument9 pagesUso de MáscarasJoaoNo ratings yet
- Breast Implant Evaluation - EvidenceTableDocument23 pagesBreast Implant Evaluation - EvidenceTableopenlab.doisNo ratings yet
- Ppe 39Document3 pagesPpe 39Sajin AlexanderNo ratings yet
- Adverse Skin Reactions To Personal Protective Equipment Against SARSDocument4 pagesAdverse Skin Reactions To Personal Protective Equipment Against SARSinesNo ratings yet
- A Cluster Randomised Trial of Cloth Masks Compared With Medical Masks in Healthcare WorkersDocument13 pagesA Cluster Randomised Trial of Cloth Masks Compared With Medical Masks in Healthcare WorkersnafisahNo ratings yet
- Decision MakingDocument24 pagesDecision MakingMark NO A LA MinaNo ratings yet
- Decontamination and Reuse of Surgical Masks and N95 Filtering Facepiece Respirators During The COVID-19 Pandemic: A Systematic ReviewDocument6 pagesDecontamination and Reuse of Surgical Masks and N95 Filtering Facepiece Respirators During The COVID-19 Pandemic: A Systematic ReviewKarinaayu SerinNo ratings yet
- Masks For Prevention of Respiratory Virus Infections, Including SARS-CoV-2, in Health Care and Community SettingsDocument15 pagesMasks For Prevention of Respiratory Virus Infections, Including SARS-CoV-2, in Health Care and Community SettingsMarcio WandréNo ratings yet
- Effectiveness of Masks and Respirators Against Respiratory Infections in Healthcare Workers A Systematic Review and Meta-Analysis 2017Document9 pagesEffectiveness of Masks and Respirators Against Respiratory Infections in Healthcare Workers A Systematic Review and Meta-Analysis 2017DanteNo ratings yet
- Measuring Breathability and Bacterial Filtration Efficiency ...Document14 pagesMeasuring Breathability and Bacterial Filtration Efficiency ...MarisolNo ratings yet
- Evaluation of Cloth Masks and Modified Procedure Masks As Personal Protective Equipment For The PubliDocument18 pagesEvaluation of Cloth Masks and Modified Procedure Masks As Personal Protective Equipment For The Publiharaldd5No ratings yet
- Contact Lens and Anterior Eye: Rute J. Macedo-de-Araújo, Eef Van Der Worp, José M. González-Méijome TDocument9 pagesContact Lens and Anterior Eye: Rute J. Macedo-de-Araújo, Eef Van Der Worp, José M. González-Méijome TJorge Silva VereauNo ratings yet
- Training Safer Orthopedic SurgeonsDocument6 pagesTraining Safer Orthopedic SurgeonsDania ZaidNo ratings yet
- Esicm Lives 2018: Meetingabstracts Open AccessDocument690 pagesEsicm Lives 2018: Meetingabstracts Open AccessjasbvbfitnessNo ratings yet
- Low-Cost Measurement of Facemask Efficacy For Filtering Expelled Droplets During SpeechDocument11 pagesLow-Cost Measurement of Facemask Efficacy For Filtering Expelled Droplets During SpeechJacob ObboNo ratings yet
- Mask TimeDocument2 pagesMask TimeNuman MunirNo ratings yet
- FiltrationDocument16 pagesFiltrationjojokawayNo ratings yet
- Sciadv Abd3083 Full PDFDocument11 pagesSciadv Abd3083 Full PDFjudith retanaNo ratings yet
- m20 3213 PDFDocument15 pagesm20 3213 PDFYusra Angel DelfinNo ratings yet
- Particulate Face Masks For Protection Against AirbDocument5 pagesParticulate Face Masks For Protection Against AirbAnuj ShandilyaNo ratings yet
- LawsonDocument7 pagesLawsonrodolfo gorveñaNo ratings yet
- AO CMFS During COVID-19Document6 pagesAO CMFS During COVID-19โสภาพรรณวดี รวีวารNo ratings yet
- Assessment of The Performance of The O-RADS MRI Score For The Evaluation of Adnexal Masses, With Technical NotesDocument8 pagesAssessment of The Performance of The O-RADS MRI Score For The Evaluation of Adnexal Masses, With Technical NotesYves FeitosaNo ratings yet
- Jurnal InternasionalDocument6 pagesJurnal InternasionalBerlianaNo ratings yet
- Long Night Shifts Among Health Workers and Physical and Mental Health: The Influence of On-Shift Nap and Domestic WorkDocument1 pageLong Night Shifts Among Health Workers and Physical and Mental Health: The Influence of On-Shift Nap and Domestic WorksicodaNo ratings yet
- Jurnal RadiasiDocument8 pagesJurnal RadiasiIdham JufriNo ratings yet
- Article: ResearchDocument17 pagesArticle: Researchryan yovanNo ratings yet
- Association of American Physicians and SurgeonsDocument6 pagesAssociation of American Physicians and SurgeonsDavidNo ratings yet
- Scatter and Staff Dose Level in Paediatric Intervencionism PDFDocument8 pagesScatter and Staff Dose Level in Paediatric Intervencionism PDFsebastian CarrascoNo ratings yet
- DocumentDocument4 pagesDocumentmiminNo ratings yet
- Evaluation of A Novel Powered Air-Purifying RespirDocument1 pageEvaluation of A Novel Powered Air-Purifying RespirdarmaNo ratings yet
- Jhe2016 8572493Document12 pagesJhe2016 8572493Alexandra PaunNo ratings yet
- N95 Vs FFPDocument13 pagesN95 Vs FFPbalas4u89No ratings yet
- 2017 Article 5336Document8 pages2017 Article 5336Christian SierNo ratings yet
- Effectiveness of Surgical KF94 and N95 Respirator Masks in Blocking SARS CoV 2 A Controlled Comparison in 7 PatientsDocument6 pagesEffectiveness of Surgical KF94 and N95 Respirator Masks in Blocking SARS CoV 2 A Controlled Comparison in 7 Patientsdr. EndahNo ratings yet
- Science of The Total Environment: Kin-Fai Ho, Lian-Yu Lin, Shao-Ping Weng, Kai-Jen ChuangDocument4 pagesScience of The Total Environment: Kin-Fai Ho, Lian-Yu Lin, Shao-Ping Weng, Kai-Jen ChuangBryan Panchana TorresNo ratings yet
- Femtosecond Laser-Assisted Preparation of Conjunctival Autograft For Pterygium SurgeryDocument8 pagesFemtosecond Laser-Assisted Preparation of Conjunctival Autograft For Pterygium SurgerySavitri IndrasariNo ratings yet
- ARTICULO - Daño EPP en La Piel COVID de Los Trabajadores Que Gsestionan La Salud - AcadDocument2 pagesARTICULO - Daño EPP en La Piel COVID de Los Trabajadores Que Gsestionan La Salud - AcadDieter Fernando Sejas LópezNo ratings yet
- Areas of Research Interest in Airway Management: Direction and GapsDocument3 pagesAreas of Research Interest in Airway Management: Direction and GapsLaras Bani WasesoNo ratings yet
- International CongressDocument27 pagesInternational CongressAlex CruceruNo ratings yet
- JUSTINGER - Antibacterial Coating of Abdominal Closure Sutures and Wound Infection 2009Document6 pagesJUSTINGER - Antibacterial Coating of Abdominal Closure Sutures and Wound Infection 2009Lucas Kovalski de MouraNo ratings yet
- 1C - 107 - Heny Maghfiana R - AbstractDocument1 page1C - 107 - Heny Maghfiana R - AbstractHeny MaghfianaNo ratings yet
- Journal Pone 0106203 PDFDocument7 pagesJournal Pone 0106203 PDFAnonymous 4vrma12QgbNo ratings yet
- 2009-Loeb-Predominant Role of Bacterial Pneumonia As A Cause of Death in Pandemic InfluenzaDocument7 pages2009-Loeb-Predominant Role of Bacterial Pneumonia As A Cause of Death in Pandemic InfluenzaJun KedNo ratings yet
- Prevention Work AccidentDocument6 pagesPrevention Work AccidenthumairohimaniaNo ratings yet
- Artigo - Hand Exposure in Diagnostic Nuc MedDocument6 pagesArtigo - Hand Exposure in Diagnostic Nuc MedsamuelNo ratings yet
- Clinical Microbiology and Infection: Letter To The EditorDocument2 pagesClinical Microbiology and Infection: Letter To The Editordrsiddharthchoudhary15No ratings yet
- Cotofana 2021Document9 pagesCotofana 2021Emrys1987No ratings yet
- ResultadosDocument20 pagesResultadosRicardo PáscoaNo ratings yet
- Cancer Oral 1Document4 pagesCancer Oral 1Jessica Paola LagunaNo ratings yet
- Fiorino2000 PDFDocument11 pagesFiorino2000 PDFDiego Antonio Rodriguez CoronadoNo ratings yet
- Radiography Protectn FR Orthodontist Ajo2005Document5 pagesRadiography Protectn FR Orthodontist Ajo2005Dr S KNo ratings yet
- Evaluation of A Novel Algorithm For Primary MassDocument10 pagesEvaluation of A Novel Algorithm For Primary MassYves BurckelNo ratings yet
- Correspondence: COVID-19: Consider Cytokine Storm Syndromes and ImmunosuppressionDocument2 pagesCorrespondence: COVID-19: Consider Cytokine Storm Syndromes and ImmunosuppressionPhilippe Lefèvre AngelNo ratings yet
- PIIS1201971220301958Document11 pagesPIIS1201971220301958nadiaNo ratings yet
- The Pathophysiology of Happy' Hypoxemia in COVID-19: Review Open AccessDocument9 pagesThe Pathophysiology of Happy' Hypoxemia in COVID-19: Review Open AccessMuhammad Taufiq AmrullahNo ratings yet
- Pulmonary Pharmacology & TherapeuticsDocument10 pagesPulmonary Pharmacology & TherapeuticsJoko Arif KurniawanNo ratings yet
- Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19) A ReviewDocument13 pagesPathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19) A ReviewJose de Jesus Ayala LeyvaNo ratings yet
- Print Ini PentingDocument4 pagesPrint Ini Pentingridawahyuni09No ratings yet
- The Right Time For Steroids in Covid-19Document5 pagesThe Right Time For Steroids in Covid-19Joko Arif KurniawanNo ratings yet
- Lymphopenia Predicts Disease Severity of COVID-19: A Descriptive and Predictive StudyDocument3 pagesLymphopenia Predicts Disease Severity of COVID-19: A Descriptive and Predictive Studybeny nurjamanNo ratings yet
- The Right Time For Steroids in Covid-19Document5 pagesThe Right Time For Steroids in Covid-19Joko Arif KurniawanNo ratings yet
- Jama Bai 2020 LD 200013 PDFDocument2 pagesJama Bai 2020 LD 200013 PDFtestNo ratings yet
- Corticosteroid Treatment of Patients With Coronavirus Disease 2019 (COVID-19)Document5 pagesCorticosteroid Treatment of Patients With Coronavirus Disease 2019 (COVID-19)Joko Arif KurniawanNo ratings yet
- Shenimt e Mia Personale Per DDXDocument281 pagesShenimt e Mia Personale Per DDXJeronim H'gharNo ratings yet
- Long-Term Management of Gastroesophageal Refl Ux Disease With PantoprazoleDocument14 pagesLong-Term Management of Gastroesophageal Refl Ux Disease With PantoprazoleJoko Arif KurniawanNo ratings yet
- 2020 JAMA Effect of Convalescent Plasma Therapy On Time To Clinical ImprovementDocument11 pages2020 JAMA Effect of Convalescent Plasma Therapy On Time To Clinical ImprovementJoko Arif KurniawanNo ratings yet
- Donal Bebek Kecelakaan PDFDocument52 pagesDonal Bebek Kecelakaan PDFJoko Arif KurniawanNo ratings yet
- Satelit 16 DR NendenDocument66 pagesSatelit 16 DR NendenJoko Arif KurniawanNo ratings yet
- Satelit 16 DR NendenDocument66 pagesSatelit 16 DR NendenJoko Arif KurniawanNo ratings yet
- Lecture 9 - Stature Estimation and Assessment From Skeletal RemainsDocument60 pagesLecture 9 - Stature Estimation and Assessment From Skeletal RemainsJoko Arif KurniawanNo ratings yet
- Internal MedicineDocument1,591 pagesInternal MedicineRina_Fatimah_Nuriila96% (46)
- Literature Review Example Occupational TherapyDocument6 pagesLiterature Review Example Occupational Therapyafdtuaerl100% (1)
- Allama Iqbal Open University, IslamabadDocument22 pagesAllama Iqbal Open University, Islamabadazeem dilawarNo ratings yet
- Chapter 7Document9 pagesChapter 7Lawrence Ryan DaugNo ratings yet
- Scope of NursingDocument13 pagesScope of Nursingniju_grgNo ratings yet
- 1220.0 Anzsco Version 1.3 Structure v1Document74 pages1220.0 Anzsco Version 1.3 Structure v1JHNo ratings yet
- Dermatologycal Preparations PDFDocument268 pagesDermatologycal Preparations PDFVando F. Sardi100% (1)
- Ispec A Blessed Experience in BotswanaDocument70 pagesIspec A Blessed Experience in BotswanaBindeshwar Prasad YadavNo ratings yet
- Private Sector Health Services in Bangladesh - An Exploratory StudyDocument37 pagesPrivate Sector Health Services in Bangladesh - An Exploratory Studyhornzz0% (1)
- Post Training or Seminar Evaluation Tool: AcademicDocument2 pagesPost Training or Seminar Evaluation Tool: AcademicRosemarie R. ReyesNo ratings yet
- Notice of Privacy Practices (Generic)Document3 pagesNotice of Privacy Practices (Generic)cecilled_08No ratings yet
- Equality Bill 2019 4Document28 pagesEquality Bill 2019 4sachin tendulkarNo ratings yet
- Health 10 - Q1 - Module1aDocument18 pagesHealth 10 - Q1 - Module1aphotomusicianNo ratings yet
- Department of Education: Republic of The PhilippinesDocument7 pagesDepartment of Education: Republic of The PhilippinesMelvin CastilloNo ratings yet
- Health and Safety at Work Act 2015Document189 pagesHealth and Safety at Work Act 2015OONNo ratings yet
- Community Health NursingDocument7 pagesCommunity Health NursingFreeNursingNotes87% (47)
- Trends and Issues in Nursing (CPD)Document13 pagesTrends and Issues in Nursing (CPD)Maizatul Akmar IbrahimNo ratings yet
- Health: Quarter I - Module 3 Complementary and Alternative Health CareDocument24 pagesHealth: Quarter I - Module 3 Complementary and Alternative Health CareKrizia Daleene M. CorderoNo ratings yet
- Fixing - Nigeria (1) - 1 PDFDocument40 pagesFixing - Nigeria (1) - 1 PDFFlying Doctors Nigeria100% (1)
- NURS FPX 6614 Assessment 2 Enhancing Performance As Collaborators in CareDocument7 pagesNURS FPX 6614 Assessment 2 Enhancing Performance As Collaborators in Carefarwaamjad771No ratings yet
- Philippine Board of Nursing Course SyllabusDocument11 pagesPhilippine Board of Nursing Course SyllabusChin Chan100% (1)
- Learning Needs of A Multigenerational CommunityDocument9 pagesLearning Needs of A Multigenerational CommunityTina BayNo ratings yet
- Common River Medicinal Plant Handbook FINAL4Document40 pagesCommon River Medicinal Plant Handbook FINAL4Shime EthiopianNo ratings yet
- Research Dissemination PlanDocument5 pagesResearch Dissemination PlanSamwel KangyNo ratings yet
- Bos Timothy R PH (PD)Document5 pagesBos Timothy R PH (PD)James LindonNo ratings yet
- Kashish KewalramaniDocument36 pagesKashish Kewalramanipriyanshu kesarwaniNo ratings yet
- Nursing PortfolioDocument3 pagesNursing Portfolioapi-243111951No ratings yet
- Covid19 - Physiotherapy - Management - Information - GuidanceDocument13 pagesCovid19 - Physiotherapy - Management - Information - GuidanceMasrov TukirovNo ratings yet
- Uganda Health Sector Budget Framework Paper FY 2018/19 - FY 2022/23Document168 pagesUganda Health Sector Budget Framework Paper FY 2018/19 - FY 2022/23African Centre for Media Excellence100% (1)
- Impacts of Covid-19 Outbreak in Mental Health of Physicians and NursesDocument7 pagesImpacts of Covid-19 Outbreak in Mental Health of Physicians and NursesJournal of Economics, Finance And Management StudiesNo ratings yet
- Integrating Cerner Millennium With Oracle E-Business SuiteDocument2 pagesIntegrating Cerner Millennium With Oracle E-Business Suiteabdulgani11No ratings yet