Professional Documents
Culture Documents
Critical Care Concept Map Part 2
Uploaded by
api-546041342Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Critical Care Concept Map Part 2
Uploaded by
api-546041342Copyright:
Available Formats
1
Critical Care Patient Case Study Data
Student: Erica O’Rell
Date of Care: 9/25/2020
Pt Initials: GR Room #: 31 Age: 65 Sex: male Date admitted: 8/10/2020
DNR status: CCA
Allergies: no known Height: 5 ft 3 in Weight: 154 lbs Isolation: none
Diagnoses: acute respiratory failure, CKD, hypokalemia
Reason for Admission/ Events Leading to Current Hospitalization and reason in unit for > 2 days:
Pt came to ICU on 8/10/2020 testing positive for COVID-19. Pt recovered from that, but is still in
respiratory failure. Pt could not be weaned from the vent, a tracheostomy was performed and will be
transferred to select once the hospital staff gets his RR under control.
Pertinent History of Illness/Surgery:
Trach placement, PEG tube placement, hyperlipidemia, DM, HTN, CAD
Vitals Day of Care:
T: 98.8
BP: 118/76
MAP: 81*
RR: 36*
HR: 88
SpO2: 98
Oxygenation: Trach
Mode: A/C
Rate: 16
FiO2: 50
TV: 320
PEEP: 8
PSV: none
Neurological:
LOC: 1 Orientation: UTA- speaks SpanishOrdered Sedation: none
Opens eyes: yes GCS: 15 (I witnessed him speak with a physician who speaks Spanish)
Pupils: PERRLA- sluggish Speech: UTA Tongue: Moist Face Symmetry:
symmetrical
Cardiovascular:
Rhythm: NSR Pulse: Regular Heart Sounds: Normal S1 and S2
JVD: none Cap Refill: <3 secs Pacemaker: none
CVP: no PCWP: no Cyanosis location: none
Peripheral Vascular:
Pulses: palp Radial: R 2+ L 3+ Pedal: R 2+ L 2+ Post Tibial: R: 2+ L 2+
Edema: Yes; generalized; 2+
Respiratory:
Breath Sounds: ronchi and crackles heard throughout; diminished breath sounds
Sputum: white and frothy
Chest Tubes: none Cough: yes; non-productive
GI:
Diet: tube feed; semi-elemental PEG tube Abdomen: soft, non-distended
Bowel Sounds: normo-active X4 Stool: none- last stool yesterday
Ostomy: None FMS: None Color/Characteristic: UTA
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis
2
GU:
Urine: yellow Clarity: clear Catheter: external Genital Irritation: no
Skin:
Temp: warm Color: appropriate Turgor: good
Mucous Membranes: moist Incisions: none Wounds: face and legs d/t proning
Musculoskeletal:
UE Movment: none Strength: weak Sensation: full
LE Movement: none Strength: weak Sensation: full
Pertinent subjective and objective data for the following:
Health Maintenance (Use of Alcohol, Tobacco, Drugs): not known
Activity/Exercise: Self Care Ability (eating, bathing, transferring, tolerance to activity):
Unable to transfer or perform ADLs, on bedrest, weak, has a PEG tube, trach
Sleep-Rest: Normal
Cognitive-Perceptual (mental status, ability to communicate, language barriers, comprehension,
anxiety, interactive skills, hearing, vision, memory):
Upon assignment to this patient, it seemed he was unable or unwilling to communicate. The nurse
was unsure if he understood us, because he speaks spanish and rarely responded to commands. He would
occassionally squeeze our hands or wiggle his toes, but later would shake up or down for yes and no. The
nurse told me he did not speak at all because of the trach, but while I was in there doing paperwork, a
doctor came in and spoke spanish to him and he responded. His RR was in the thirties, and that may have
been because of anxiety.
Role Relationship (marital status, occupation, employment status, support system, family concens):
Married, unknown employment, unknown support system.
Value/Belief (religion, spirital needs): no church listed
Continuous IV Drips:
Dextrose 5% 100 ml/hr L arm peripheral
24 hr. Intake: 1638
24 hr. Output: 1250
Cumulative Fluid Balance: +388
Pain/Pain Management: no objective signs of pain
Normal Day prior Day of care Reason for abdormal
Na 132-146
K 3.5-5 4.0 4.2
Cl 98-107 99 99
CO2 34-45 43.2 43
Glucose 70-100 175 159 Diabetes
BUN 8-23 50 58 CKD
Cr 0.7-1.2 0.4 0.4 CKD
Calcium 8.6-10.2 8.7 8.8
Albumin 3.5-5.2 2.6 No value Poor nutrition, poss. Liver
dysfn
Total protein 6.4-8.3 No value No value
ALP 40-129 No value 133 Possible liver dysfn, biliary
dsyfn
ALT 0-32 30 30
AST 0-31 28 28
Total Bilirubin 0-1.2 .6 .7
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis
3
Magnesium 1.6-2.6 1.8 1.7
Phosphate 2.5-4.5 3.0 2.9
Cholesterol 140-400 No value No value
Triglycerides < 150 No value No value
RBC 3.8-5.8 2.91 2.73 CKD
Hgb 11.5-15.5 8.2 7.7 CKD
Hct 34-48 26.2 24.5 CKD
Platelets 130-450 200 205
WBC 4.5-11.5 17.9 16.1 Infection?
Neutrophils 43-80 15.64 14.35 Infection?
Lymphocytes 20-42 34 34
Monocytes 2-12 6 8
Eosinophils 0-6 3 2
Basophils 0-2 0 0
PT 11-13 13.6 13.3 Lovenox
INR 1-1.5 2 2 lovenox
PTT 18-28 No value No value
A pH 7.35-7.45 7.448 7.448 Compensated met alk
B pCO2 35-45 43 43.2 Compensated met alk
Gs pO2 60-100 80.9 81.2 Compensated met alk
HCO3 22-26 29.0 29.2 Compensated met alk
Chest xray: pneumopericardium present and subcutaneous emphysema in the neck. Bilateral airspace
disease stable.
Other pertinent tests: US retroperitoneal d/t Stage 2 CKD. No evidence of hydronephrosis, perinephric
collections, renal calculi or solid renal masses.
Treatments:
Mouthcare and suctioning Q2H PRN for prophylaxis against ventilator associated pneumonia
A/C: rate 16, TV 320, FiO2 .5, PEEP 8
DVT prevention: enoxaparin subQ
Bedrest, side rails up X4
Foley care
Assess IVs Q2H
Pathophysiology: Acute hypercapnic respiratory failure is usually caused by defects in the central nervous
system, impairment of neuromuscular transmission, mechanical defect of the ribcage and fatigue of
the respiratory muscles. Fluid builds up in the air sacs in the lungs. The lungs can’t release oxygen to the
blood and organs aren’t being perfused. Carbon dioxide cannot be removed.
Nursing care: Oxygen therapy, ipratropium-albuterol given. Patient will be closely observed for potential
deterioration. Respiratory assessment occurring on a frequent/continual basis. Monitoring involves
continual pulse oximetry and regular peak expiratory flow rate measurement, and also basic respiratory
rate monitoring and general assessment.
Medications Allergies: no known
Brand Name Tylenol Lipitor Bumex Lovenox
Generic Name Acetaminophen Atorvastatin Bumetanide Enoxaparin
Dose 650 mg Q6H PRN 80 mg nightly 1 mg Q8H 70 mg BID
Route PEG PEG IV SubQ
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis
4
Classification Analgesic/ HMG-COA Diuretic Anticoagulant
antipyretic reductase
inhibitor
Action Inhibits synthesis Inhibits HMG- Inhibits sodium Antithrombic
of prostaglandins COA and and chloride properties due to
increases LDL reabsorption antifactory Xa
on LOH
Reason Pain, fever Hyperlipidemia CKD/HTN Prevent blood
Receiving clots
Contra Hypersensitivity, Myopathy, active Markedly Active bleeding,
use of alcohol liver disease elevated BUN, idiopathic
severe thrombocytopenia
electrolyte purpura
deficiency
Major Adverse Hepatotoxicity, Rhabdomyolysis, Hypovolemia, Angioedema,
SE acute renal increased LFTs hypokalemia hemorrhage
failure
Nursing Monitor for Monitor lipid Monitor I&O, Lab tests, monitor
Implications hepatotoxicity levels and LFTs weight, BP platelet count
Teaching Do not take Report muscle Eat potassium Report any signs
other meds pain, N/V, rich foods of bleeding, no
containing yellowing of skin OTC meds.
acetaminophen
Brand Name Apresoline Atarax Atrovent Protonix
Proventil
Generic Name hydralazine hydroxyzine ipratropium pantoprazole
albuterol
Dose 50 mg TID 50 mg Q6H 1 amp Q4H 40 mg daily
Route PEG IM Inhalation IV
Classification Vasodilator Antihistamine Bronchodilator PPI
Action Reduces BP by Depression of Selective beta-2 Decrease
direct effect on hypothalamus and antagonist and amount of acid
vascular reticular formation inhibits made in
smooth muscle acetylcholine stomach
Reason HTN Anxiety/depression Resp failure Prophylactic
receiving against stress
ulcers
Contra CAD, MI, Hypersensitivity Pregnancy and Severe hepatic
tachycardia hypersensitivity impairment
Major adverse Angina, shock Phlebitis, Anxiety and HA, abdominal
SE hemolysis hypotension pain,
constipation
Nursing Baseline BUN, Evaluate alertness Monitor CNS Assess frank or
Implication monitor HR and condition of stimulation, occult blood in
and BP oral mucosa monitor ABGs stool
Teaching Minor weight, Do not drive, do Avoid contact Avoid alcohol,
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis
5
check for not drink alcohol with eyes ASA, NSAIDs,
edema foods
stimulating GI
irritation
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis
6
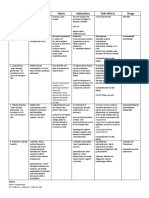
Problem 8: Anxiety
- RR very high
- Prescribed hydroxyzine
- On vent without a
Problem 2: Ineffective airway sedative
clearance Problem 1: Impaired Gas - ICU with a windowless
- Rochi and Rales Exchange room
- Nonproductive cough - ABGs: pH 7.44 PCO2 - Been in ICU for over a
- Frothy sputum on 43.2 PO2 81.2 HCO3 29.2 month
suctioning - Sub Q emphysema - Impaired verbal
- Diminished breath sounds - Trach placement communication: speaks
- Ipatropium-albuterol - RR in the 30s spanish
inhalation - FiO2 50%
Problem 3: Ineffective
breathing pattern Problem 7: Impaired skin
Reason for Needing Health Care integrity
- RR in ranging Acute Respiratory Failure, CKD,
from 26-36 - Prone positioning
Hypokalemia due to previous
- Diminished lung 65 year old male, DNR-CCA
sounds COVID-19
- Use of accessory diagnosis
Key Assessments: - Wounds on all
muscles - VS with focus on Respiratory extremities and face
- Set to go to Select Allergies: no known
but won’t take
him until his RR is
under control
Problem 4: Decreased Problem 5: Excess fluid volume Problem 6: Impaired
cardiac output - Diuretic prescribed physical mobility
- MAP 69-81 - Cumulative fluid - Trach placement
- Hx CAD and HTN balance: +388 - Restraints
- Hydralizaine TID - Generalized Edema - Very weak; almost
- Bumetanide TID - Oliguria no movement
- SCDs
Problem # 1: Impaired gas exchange
General Goal: Improved gas exchange
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis
7
Predicted Behavioral Outcome Objective (s): The pt will have ABGs within normal limits and
will have an SaO2> 90% on day of care
Nursing Strategies Patient Responses
1. Monitor RR, depth and effort 1. Pt will have normal RR without use of
accessory muscles
2. Monitor ABGs 2. Pt will have normalized ABGs
3. Observe nail beds and skin 3.Pt will have cap refill < 3 secs and skin
for cyanosis will be appropriate for ethnicity
4. Monitor SaO2 continuously 4. Pt will have SaO2 > 90%
5. Place pt in semi-fowlers 5. Pt will have increased thoracic capacity
position
6. Administer ordered 6. Pt will improve ventilatory status
ipratropium-albuterol
Evaluation of outcomes objectives: The patient’s RR has not normalized; it is irregular and ranges from 26-36
and there is use of accessory muscles. ABGs are not normal, however, the patient did have a cap refill over
under 3 seconds and there is no sign of cyanosis. SaO2 is over 90%. Goal partially met; will continue to
monitor.
Problem # 2: Ineffective airway clearance
General Goal: Improved airway clearance
Predicted Behavioral Outcome Objective (s): The patient will have increased bilateral breath
sounds with productive cough and secretions becoming thinner and clearer or day of care.
Nursing Interventions Patient Responses
1. Assess breath sounds 1. Pt will have clear, audible bilateral
breath sounds
2. Assess sections 2. Pt will have thinner and clear secretions
3. Suction PRN 3. Suctioning will be productive for pt
4. Administer bronchodilator 4. Bronchodilator will open up pt airways
5. Turn Q 2 hrs 5. Pt will have relief and secretions will brake up
Evaluation of outcomes objectives: The pt has ronchi and rales, and diminished breath sounds on both sides.
The secretions are frothy and white, and does not appear to be thinning. Suctioning is productive; but not a lot
of secretions are coming up. Bronchodilator administered as ordered; however, it does not seem to be working.
Pt turned Q2 hours, but not helping. Goal not met.
Problem # 3: Ineffective breathing pattern
General Goal: Improve breathing pattern
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis
8
Predicted Behavioral Outcome Objective (s): Patient maintains an effective breathing pattern, as
evidenced by a relaxed breathing at normal rate and depth and absence of dyspnea on day of
care.
Nursing Interventions Patient Responses
1. Assess RR and depth Q hour 1. Pt will have normal RR and depth
2. Assess breath sounds Q hour 2. Pt will not have adventitious breath sounds
3. Evaluate nutritional status 3. Albumin will be within normal limits
4. Evaluate level of anxiety 4. Pt will have relieved anxiety and therefore
normal breathing patterns
5. Provide respiratory meds 5. Pts airways will be opened up and SaO2 normal
and oxygen as ordered
6. Suction PRN 6. Suctioning will clear blockages in the airway
Evaluation of outcomes objectives: Pts RR has not normalized, and has rales and ronchi with diminished
breath sounds. Albumin is low, reducing respiratory strength. Although pt has no verbally communicated with
me, he seems restless alerting me to anxiety. SaO2 is within normal limits, and suctioning provides some
relief. Goal partially met.
Problem # 4: Decreased cardiac ouput
General Goal: Maintain adequate cardiac output
Predicted Behavioral Outcome Objective (s): The patient will maintain NSR, vital signs within
normal limits, and a normal MAP on the day of care.
Nursing Interventions Patient Responses
1. Assess vital signs 1. Pts VS will be within normal limits
2. Assess EKG 2. Pt will have NSR
3. Administer antihypertensives 3. Pts BP will be within normal limits
4. Apply SCDs 4. Pt will have improved blood flow
5. Check peripheral pulses and 5. Pulses will be normal and refill < 3 secs
cap refill
6. Record urine output 6. Pt will have adequate renal perfusion
Evaluation of outcomes objectives: Other than RR, vital signs are within normal range. However, the MAP is
low, ranging from 69-81. The EKG was normal, and the patient was in NSR during the entire day of care.
Hypertensive agents were administered, and BP remained stable. STDs were applied, and peripheral pulses
and capillary refill were in normal range. However, the patient is very oliguric, voiding under 30 ml an hour.
Goal partially met.
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis
9
Problem # 5: Excess fluid volume
General Goal: Pt will achieve ideal body weight without excess fluid
Predicted Behavioral Outcome Objective (s): The patient will have a balanced fluid intake and
output on the day of care.
Nursing Interventions Patient Responses
1. Monitor intake, observe 1. Pt will have a balanced I&O
for changes in output.
2. Assess for edema 2. Pt. will remain free from edema
3. Monitor HR and BP 3. Pt will have normal VS
4. Administer diuretic 4. Pt will have increased diuresis
Evaluation of outcomes objectives: The patient did not have a balanced I&O; cumulative fluid balance was
+388. Pt does have some generalized edema in the dependent areas, however, HR and BP are within normal
limits. A diuretic was given, but the patient was still oliguric during the time I provided care. Goal not met.
Problem # 6: Impaired physical mobility
General Goal: Increase physical mobility
Predicted Behavioral Outcome Objective (s): The patient’s will be able to perform ROM
exercises and increase strength on day of care.
Nursing Interventions Patient Responses
1. Assess ability to perform 1. Pt will be able to demonstrate ROM
ROM exercises
2. Help perform passive ROM 2. Pt will have increased strength to perform
on his own
3. Assess nutritional needs 3. Pt will have increased energy needed
4. Help pt in understanding his 4. Pt understands he is going to Select
limitations
Evaluation of outcomes objectives: Pt is very weak, and it unable to perform ROM. The only thing he does is
squeeze my hands, which are weak as well. I performed passive ROM with him in the hopes it will help him
gain some strength. His nutrition is poor as evidenced by his albumin level, which can be adding to the
problem; he does not have the energy he needs. Pt understands his limitations; he understands he is going to
select. Goal not met.
Problem # 7: Impaired skin integrity
General Goal: Pt will have improved skin integrity
Predicted Behavioral Outcome Objective (s): The patient will remain free from any further skin
breakdown and the wounds currently present will continue to heal on day of care.
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis
10
Nursing Interventions Patient Responses
1. Assess breakdown and its 1. Pts wounds will be healing
condition
2. Assess temperature 2. Pt will remain free from infection
3. Provide wound care 3. Pts wounds will be clean and begin to heal
4. Minimize moisture on skin 4. Pt will not have any more skin break down
5. Turn Q2H 5. Pt will not have any more skin break down
6. Use pressure reducing device 6. Pt will not have any more skin break down
Evaluation of outcomes objectives: Pts wounds are healing; they are dry and beginning to scab. They are small
and appear free from infection. The patient’s temp has remained within normal limits, skin is dry and has been
turned Q2 hours. Pressure reducing devices such as pillows and foam wedges were used. There is no evidence
of further breakdown. Goal has been met.
Problem #8: Anxiety
General Goal: Pt will reduce own anxiety level
Predicted Behavioral Outcome Objective (s): The patient will reduce RR and report decreasing
levels of anxiety on day of care.
Nursing Interventions Patient Responses
1. Maintain a calm, non- 1. Pt will develop a sense of security
threatening manner while
working with pt
2. Remain with pt at all times 2. Pt will remain safe and anxiety will decrease
when anxiety is high;
reassure safety and security
3. Administer antianxiety meds 3. Pt’s anxiety will decrease
4. Monitor RR 4. RR will decrease
5. Assess non-verbal signs of 5. Pt will appear at ease and rest
anxiety
Evaluation of outcomes objectives: I maintained a calm demeanor while working with the patient; although he
speaks Spanish and did not speak to me, he was able to understand English and could shake his head up or
down answering yes or no questions. He indicated he felt anxiety, and an antianxiety med was given. After, he
was able to rest for a couple of hours. His RR is high, however he is in respiratory failure so it is unclear as to
the etiology of the high RR for certain; both problems could be contributing. Goal partially met.
P. Schuster, Concept Mapping: A Critical Thinking Approach, Davis
You might also like
- Chronic Diseases - Lymes, Hpv, Hsv Mis-Diagnosis and Mistreatment: A New Approach to the EpidemicFrom EverandChronic Diseases - Lymes, Hpv, Hsv Mis-Diagnosis and Mistreatment: A New Approach to the EpidemicRating: 5 out of 5 stars5/5 (1)
- Complex Care Concept MapDocument12 pagesComplex Care Concept Mapapi-508434862No ratings yet
- Complex Care Plan 1Document12 pagesComplex Care Plan 1api-496883420No ratings yet
- MR - Suardi Tumor Paru + Efusi Pleura KiriDocument14 pagesMR - Suardi Tumor Paru + Efusi Pleura KiritiarapolarisiriuzNo ratings yet
- Final Draft Concept MapDocument15 pagesFinal Draft Concept Mapapi-546712849No ratings yet
- Concept MapDocument15 pagesConcept Mapapi-495456666No ratings yet
- Yen CKD AloDocument31 pagesYen CKD AloSafira RNo ratings yet
- Morning Report: June 2022 Physician in ChargeDocument24 pagesMorning Report: June 2022 Physician in ChargeIka AyuNo ratings yet
- Morning Report: Dr. Satya Leads Hospital TeamsDocument42 pagesMorning Report: Dr. Satya Leads Hospital TeamsPramudia DeniNo ratings yet
- Morning Report Case: June 7, 2011Document16 pagesMorning Report Case: June 7, 2011LittleChenaNo ratings yet
- Morning ReportDocument27 pagesMorning ReportDody PrasetyaNo ratings yet
- MR R 26 6-3 2017 MR W Fix AMS Septic AKIDocument15 pagesMR R 26 6-3 2017 MR W Fix AMS Septic AKISafira RNo ratings yet
- Case ScenariosDocument9 pagesCase ScenariosSophia IbuyanNo ratings yet
- Morning Report 24-9Document18 pagesMorning Report 24-9hendra nuraminNo ratings yet
- Morning Report: Dr. Dikara WS Maulidy, SP - PDDocument24 pagesMorning Report: Dr. Dikara WS Maulidy, SP - PDBethari Abi SafitriNo ratings yet
- Latihan POMR: Dr. Venna Febrian KDocument39 pagesLatihan POMR: Dr. Venna Febrian KLoudry ElfaNo ratings yet
- Morning Report CKDDocument20 pagesMorning Report CKDjoe joeNo ratings yet
- Morning Report CKDDocument12 pagesMorning Report CKDAnonymous vUEDx8No ratings yet
- Morning ReportDocument17 pagesMorning Reportjoe joeNo ratings yet
- Rajinder KaurDocument6 pagesRajinder KaurGurm RaajveerNo ratings yet
- Morning Report: Physician in ChargeDocument29 pagesMorning Report: Physician in ChargeWilujeng AnggrainiNo ratings yet
- Morning Report: Wednesday, March 8 2017Document14 pagesMorning Report: Wednesday, March 8 2017Safitri NindyaNo ratings yet
- Mortality-conference-2022.03.24 FINAL (自動儲存)Document51 pagesMortality-conference-2022.03.24 FINAL (自動儲存)許誌元No ratings yet
- Morning Report SummaryDocument27 pagesMorning Report SummaryFerdinando BaehaNo ratings yet
- NC Fauzi ERIADocument21 pagesNC Fauzi ERIADodi DiNo ratings yet
- POMR FAH BAshori CMLDocument22 pagesPOMR FAH BAshori CMLIka AyuNo ratings yet
- Morning ReportDocument22 pagesMorning ReportNiinna AwliaNo ratings yet
- Morning Report: Dr. Reza's PatientsDocument24 pagesMorning Report: Dr. Reza's PatientsIka AyuNo ratings yet
- ST Elevation Myocard InfarkDocument30 pagesST Elevation Myocard InfarkNancy Dwi Puspita100% (1)
- MysteryCase 10.22.18Document10 pagesMysteryCase 10.22.18Emily EresumaNo ratings yet
- Bellevue SJU Care Plan Revised f22Document13 pagesBellevue SJU Care Plan Revised f22Guerlene JeromeNo ratings yet
- Ahmad Basori VidiDocument30 pagesAhmad Basori VidiIka AyuNo ratings yet
- POMR 9 Pseudo Meigs Syndrome - OgieDocument21 pagesPOMR 9 Pseudo Meigs Syndrome - OgiehariogieNo ratings yet
- Morning Report Case: MarchDocument20 pagesMorning Report Case: Marchputri meiliawatiNo ratings yet
- Clinical Conference 21 August 2022: Eria (New Case)Document16 pagesClinical Conference 21 August 2022: Eria (New Case)mujahidah nursinNo ratings yet
- Clinical Conference September 30, 2022: Tropic Infection Division (New Case)Document18 pagesClinical Conference September 30, 2022: Tropic Infection Division (New Case)Hardiyanti HermanNo ratings yet
- Case Presentation: by Femi Liz Sanjana AugusthyDocument31 pagesCase Presentation: by Femi Liz Sanjana AugusthyBlessyNo ratings yet
- Morning Report: Physician in ChargeDocument11 pagesMorning Report: Physician in ChargeImam Mi'raj SuprayogaNo ratings yet
- Template Duty ReportDocument6 pagesTemplate Duty ReportJefri SusantoNo ratings yet
- Morning Report Summary for Severe Anemia and CKD PatientDocument20 pagesMorning Report Summary for Severe Anemia and CKD PatientSeptabian IskandarNo ratings yet
- POMR Satiti Acute CholangitisDocument30 pagesPOMR Satiti Acute CholangitisIka AyuNo ratings yet
- CMC Cns Infection 2023Document5 pagesCMC Cns Infection 2023Juan RecyNo ratings yet
- Tn. Ngadiran, r25Document21 pagesTn. Ngadiran, r25alanaaluNo ratings yet
- No Sub Bagian Lama Baru Pulang Pindah JMLDocument32 pagesNo Sub Bagian Lama Baru Pulang Pindah JMLkavi_1985No ratings yet
- Mrs Siti Wahyuni/ 48 Yo/ Ward 25 Bed 1.6Document7 pagesMrs Siti Wahyuni/ 48 Yo/ Ward 25 Bed 1.6DoctoRides 46No ratings yet
- AYU - CKD+DVT Left ArmDocument25 pagesAYU - CKD+DVT Left ArmIka AyuNo ratings yet
- LeptospirosisDocument19 pagesLeptospirosisFelicia adeline ChristianNo ratings yet
- 91-Year-Old Patient Report with Gastrointestinal BleedingDocument17 pages91-Year-Old Patient Report with Gastrointestinal BleedingPuteri Diah RahtiniNo ratings yet
- Carmiasih 49 Diabetic FootDocument21 pagesCarmiasih 49 Diabetic Footdevi_pramulawatiNo ratings yet
- SOS AYU - Ax - PeunjangDocument11 pagesSOS AYU - Ax - PeunjangIka AyuNo ratings yet
- A. Patient'S Identity: Pale Conjunctiva +/+Document20 pagesA. Patient'S Identity: Pale Conjunctiva +/+Mutiara JihadNo ratings yet
- Nursing Care Plan: Student: PhạM Thu QuỳNh Group: 41 Class: Y4QDocument14 pagesNursing Care Plan: Student: PhạM Thu QuỳNh Group: 41 Class: Y4QThảo LÊNo ratings yet
- 3 Year CPC October 8, 20202Document4 pages3 Year CPC October 8, 20202Raian SuyuNo ratings yet
- A Rare Case of Co-Infection That Did Not End WellDocument63 pagesA Rare Case of Co-Infection That Did Not End WellArnavjyoti DasNo ratings yet
- Case Presentation On Chronic Liver Disease: Shreyas M Salimath Pharm D 2 Year REG NO. 21Q0172Document18 pagesCase Presentation On Chronic Liver Disease: Shreyas M Salimath Pharm D 2 Year REG NO. 21Q0172AmalinNo ratings yet
- MR Sindrom Nefrotik 1 Agustus 17Document12 pagesMR Sindrom Nefrotik 1 Agustus 17Ridho CahyaNo ratings yet
- Morning Report: Date: Monday, 2 November 2020Document24 pagesMorning Report: Date: Monday, 2 November 2020Ika AyuNo ratings yet
- DRMC Grand Rounds: Case of Myxedema ComaDocument9 pagesDRMC Grand Rounds: Case of Myxedema ComaKristiannlae DanoNo ratings yet
- Long CaseDocument10 pagesLong CaseAseel AbdulkreemNo ratings yet
- Morning Report: Physician in ChargeDocument33 pagesMorning Report: Physician in ChargeIka AyuNo ratings yet
- DRUG STUDY SpironolactoneDocument4 pagesDRUG STUDY SpironolactoneJerremy LuqueNo ratings yet
- EndometriosisDocument45 pagesEndometriosisIngrid MiñanoNo ratings yet
- Medical AbbreviationsDocument6 pagesMedical AbbreviationsEina CarmonaNo ratings yet
- CPR First Aid SyllabusDocument2 pagesCPR First Aid Syllabusapi-3704804No ratings yet
- Professor Devendra Kumar Chhabra: TH THDocument2 pagesProfessor Devendra Kumar Chhabra: TH THVineet UttamNo ratings yet
- Diuretics MOA Notes Indications Side Effects DrugsDocument1 pageDiuretics MOA Notes Indications Side Effects Drugsmonica leeNo ratings yet
- 5 Minute Spotlight - Vacuum Extraction and Forceps DeliveryDocument2 pages5 Minute Spotlight - Vacuum Extraction and Forceps DeliveryMikeNo ratings yet
- Nursing Care Plan FormatDocument7 pagesNursing Care Plan FormatPrasann RoyNo ratings yet
- Clinical Study of Otomycosis: Fungal Ear Infection Causes, Symptoms & TreatmentDocument16 pagesClinical Study of Otomycosis: Fungal Ear Infection Causes, Symptoms & TreatmentMcraeNo ratings yet
- Studies: Coagulation The DigitalisDocument7 pagesStudies: Coagulation The Digitalisfebyan yohanesNo ratings yet
- Vi. Ûrxm: ®vôtôw ® Øû/LsDocument4 pagesVi. Ûrxm: ®vôtôw ® Øû/Lsbgk_usNo ratings yet
- Addictions: Psychology Assignment Name: Jigyasa Dhingra Class: Xi-FDocument10 pagesAddictions: Psychology Assignment Name: Jigyasa Dhingra Class: Xi-FAN - 11ZZ 963416 Chinguacousy SSNo ratings yet
- 29 - Toronto Notes 2011 - Urology PDFDocument44 pages29 - Toronto Notes 2011 - Urology PDFDewa Gede Reza Sanjaya0% (1)
- Samantha Bradley: Work ExperienceDocument3 pagesSamantha Bradley: Work Experienceapi-399988983No ratings yet
- Metaplastic (Chronic) Atrophic Gastritis - UpToDate PDFDocument16 pagesMetaplastic (Chronic) Atrophic Gastritis - UpToDate PDFDinaNo ratings yet
- The Child With A Fluid and Electrolyte Alteration: Body Water Is Located in Two Major CompartmentsDocument19 pagesThe Child With A Fluid and Electrolyte Alteration: Body Water Is Located in Two Major CompartmentsAyeza DuaNo ratings yet
- Hemodynamic Management Pocket Card PDFDocument8 pagesHemodynamic Management Pocket Card PDFjenn1722No ratings yet
- Sanofi Just Got Its First Cancer Drug Approved in A Decade.Document7 pagesSanofi Just Got Its First Cancer Drug Approved in A Decade.Antonietta BlacconeriNo ratings yet
- NURS 6521N Final Exam Question and Answers Feb 2020 (100/100)Document19 pagesNURS 6521N Final Exam Question and Answers Feb 2020 (100/100)Judy Durkin0% (1)
- Annotated Bibliography of Obstetrics & Gynaecology ResourcesDocument4 pagesAnnotated Bibliography of Obstetrics & Gynaecology ResourcesKaku ManishaNo ratings yet
- C1-Human HeartDocument3 pagesC1-Human HeartNursuzela Abd MalekNo ratings yet
- Survey Questionaire On Extent of School Health ProDocument2 pagesSurvey Questionaire On Extent of School Health ProDORY HILADONo ratings yet
- Assessing The Relationship Between Anxiety Levels and Panic Attacks Among The Youth in ShimlaDocument52 pagesAssessing The Relationship Between Anxiety Levels and Panic Attacks Among The Youth in ShimlaAni RudhNo ratings yet
- VNHSW Report-Health ProgramsDocument12 pagesVNHSW Report-Health Programsmaverick arquilloNo ratings yet
- Clinical Examinations Crib Sheet v7Document36 pagesClinical Examinations Crib Sheet v7aparish10100% (1)
- Artificial HeartDocument17 pagesArtificial HeartRAKESHKANNAN100% (1)
- MCQ Pract Pharma 1Document9 pagesMCQ Pract Pharma 1Syamil AzharNo ratings yet
- Intake AssessmentDocument2 pagesIntake Assessmentyourzxtruly0% (1)
- Fresenius 2008T Dialysis System - User's Troubleshooting ManualDocument20 pagesFresenius 2008T Dialysis System - User's Troubleshooting ManualCesar AlfaroNo ratings yet
- ME210 Gastrointestinal TimetableDocument6 pagesME210 Gastrointestinal TimetableEka Irina Akma KamaruddinNo ratings yet