Professional Documents
Culture Documents
Date Performed: Final Grade: Clinical Instructor: Nasogastric Tube (NGT) Feeding Definition
Date Performed: Final Grade: Clinical Instructor: Nasogastric Tube (NGT) Feeding Definition
Uploaded by
Almira GamaoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Date Performed: Final Grade: Clinical Instructor: Nasogastric Tube (NGT) Feeding Definition
Date Performed: Final Grade: Clinical Instructor: Nasogastric Tube (NGT) Feeding Definition
Uploaded by
Almira GamaoCopyright:
Available Formats
Date Performed: Final Grade:
Clinical Instructor:
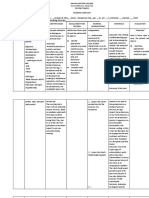
NASOGASTRIC TUBE (NGT) FEEDING
Definition:
Objectives:
1.
2.
3.
Safety/Security Measures:
1.
2.
3.
Equipment:
Pre-procedural Assessment:
1. Introduce yourself to the client and identify client’s identity. Explain what are
going to do, why it is necessary, and how the client can cooperate.
2. Gather the necessary equipment.
3. Provide Privacy
4. Review the patient’s chart for baseline data.
5. Wash hands
PROCEDURE GRAD REMARKS
E
1. Check doctor’s order for formula, rate, frequency of feeding
and expiration date of formula.4
Rationale:
2. Auscultate bowel sounds.
Rationale:
3. Assess client regarding discomfort from tube.
Rationale:
4. Observe insertion site for irritation.
Rationale:
5. Prepare the tube feeding at room temperature. 2
Rationale:
6. Place client to high fowler’s position in bed or to a sitting
position in a chair unless contraindicated. 2
Rationale:
7. Perform medical hand washing, wear clean gloves and
other appropriate infection control measures. 2
Rationale:
8. Check for tube placement and patency by doing any of the
following:1
a. Introduce 5-20 ml pf air into Nasogastric Tube (NGT)
and auscultate at the epigastric area, gurgling sound is
heard. 1
b. Aspirate a gastric content which is yellowish or greenish
in color.
Note: If more than 100 ml of the last feeding is
withdrawn, check with the nurse-in charge or refer to
agency policy before proceeding.2
c. Immerse tip of the tube in the glass of water; no bubbles
should be produced.
Rationale:
9. Infuse feeding through the subsequent steps: 1
a. Pinch proximal end of the feeding tube
b. Attach syringe to the NGT and aspirate gastric contents to
fill the tube
c. Fill the syringe with measured amount of formula
d. Release the tube and hold the syringe at 12 inches above
the client. Refill; repeat until the prescribed amount has
been given.
Rationale:
10. Flush 30 ml of water into the NGT after the feeding.
Rationale:
11. Clamp NGT before all of the water is instilled.
Rationale:
12. Ask client to remain in Fowler’s position 30 minutes to one
hour after feeding.4
Rationale:
13. Do after- care.
Rationale:
14. Discard gloves and perform medical hand washing.
Rationale:
15. Evaluate client’s tolerance and response to feeding
16. Observe client for complaints of nausea and vomiting
Rationale:
17. Record amount, type and time of feeding
18. Document client’s response and tolerance to tube feeding.
Rationale:
Ability to answer questions
Definition
Objectives
Principles
TOTAL
Signature of the Clinical Instructor:
Reference/s:
1
Adion,D. & Dizon, E. (2009). Manual and Checklists on Health Care Procedures. 1st
edition. Manila: Educational Publishing House.
2
Kozier, Barbara. & Erb, Glenora(2008).Kozier & Erb’s Fundamentals of Nursing
Checklist. 8th ed. Philippines: Pearson Education, Inc.
3
Potter, Patricia et.al (2017). Fundamentals of Nursing. 9th ed. Philippines: Elsevier Pte. Ltd.
4
Taylor, Carol., Lillis, C. & Le Mone, P. (2001). Fundamentals of Nursing The Art and Science
of Nursing Care. 3th ed.
You might also like
- Sas#1 - Ite 303-SiaDocument7 pagesSas#1 - Ite 303-SiaFranzh Lawrence BataanNo ratings yet
- Final Case Study NCM 116Document60 pagesFinal Case Study NCM 116Marissa AsimNo ratings yet
- Perception and CoordinationDocument7 pagesPerception and CoordinationSonia G. Ortiz0% (1)
- Comprehensive Practice Part1Document40 pagesComprehensive Practice Part1Arvin Campos0% (1)
- Interventional Med-Tech Primer (Atlanata)Document41 pagesInterventional Med-Tech Primer (Atlanata)divyabuni100% (1)
- CLIENTS WITH PROBLEMS IN CELLULAR ABERRATIONS Notes For StudentsDocument39 pagesCLIENTS WITH PROBLEMS IN CELLULAR ABERRATIONS Notes For StudentsAno NymousNo ratings yet
- Critical Thinking FHP WorksheetDocument17 pagesCritical Thinking FHP WorksheetfairwoodsNo ratings yet
- Contemporary World Reviewer Part 4Document3 pagesContemporary World Reviewer Part 4maryaniNo ratings yet
- University of The EastDocument33 pagesUniversity of The EastSEAN MELNOR LOSBAÑESNo ratings yet
- Psychosexual Disorders: Gender Identity Disorder, Paraphilias, and Sexual DysfunctionsDocument38 pagesPsychosexual Disorders: Gender Identity Disorder, Paraphilias, and Sexual DysfunctionsJordz PlaciNo ratings yet
- Fleet Enema Name: Angeline M. Taghap - Grade: - Year and Section: BSN 2 B Date: October 21, 2021Document2 pagesFleet Enema Name: Angeline M. Taghap - Grade: - Year and Section: BSN 2 B Date: October 21, 2021Angeline TaghapNo ratings yet
- Urinary Catheter InsertionDocument4 pagesUrinary Catheter InsertionAngel SamonteNo ratings yet
- Naso Orogastric Tube Guideline For The Care of Neonate Child or Young Person RequiringDocument12 pagesNaso Orogastric Tube Guideline For The Care of Neonate Child or Young Person RequiringmeisygraniaNo ratings yet
- Cycle of ViolenceDocument1 pageCycle of ViolenceSuhailah Mohd JamilNo ratings yet
- Administering Parenteral MedicationDocument3 pagesAdministering Parenteral Medicationtripj33No ratings yet
- Our Lady of Fatima UniversityDocument2 pagesOur Lady of Fatima UniversityMICHAEL M. ISIDRONo ratings yet
- Reaction PaperDocument2 pagesReaction PaperAngeline ZafeNo ratings yet
- Funda Skills ProceduresDocument34 pagesFunda Skills Proceduresjericho obiceNo ratings yet
- Cellular AberrationsDocument94 pagesCellular AberrationsridzkhaNo ratings yet
- NGT Feeding: by Group 2Document25 pagesNGT Feeding: by Group 2karl montano100% (1)
- Funda Review NotesDocument35 pagesFunda Review NotesShara SampangNo ratings yet
- A Project Proposal On Case Study and Management of A Type 1 Diabetes Mellitus ClientDocument6 pagesA Project Proposal On Case Study and Management of A Type 1 Diabetes Mellitus ClientMichael Kivumbi100% (3)
- List of Operating Room InstrumentsDocument6 pagesList of Operating Room InstrumentsChen LiNo ratings yet
- Principles of Aseptic TechniqueDocument3 pagesPrinciples of Aseptic TechniqueDane CaumeranNo ratings yet
- Multiple Choice Test QuestionsDocument6 pagesMultiple Choice Test QuestionsNicole MaeNo ratings yet
- Physical Assessment TableDocument11 pagesPhysical Assessment TableGlenn Percy VeronicaNo ratings yet
- MCN Drill 1Document23 pagesMCN Drill 1Cai Velasco DecenaNo ratings yet
- Review of SystemsDocument4 pagesReview of SystemsKat ArriolaNo ratings yet
- NotesDocument14 pagesNotesJan Rey L. TejereroNo ratings yet
- Perioperative Nursing: An OR NurseDocument27 pagesPerioperative Nursing: An OR NurseNorjana Malaatao100% (1)
- Operating Room ConceptsDocument47 pagesOperating Room ConceptsLoungayvan Batuyog100% (1)
- NSG 105 Module 3Document22 pagesNSG 105 Module 3Alaminah MULOKNo ratings yet
- ESSENTIAL INTRAPARTUM NEWBORN CARE (Assisting and Handling Delivery)Document4 pagesESSENTIAL INTRAPARTUM NEWBORN CARE (Assisting and Handling Delivery)Hannah Angelu CabadingNo ratings yet
- Fundamentals of Nursing: Client Teaching On Abdominal (Diaphragmatic) and Pursed-Lip BreathingDocument19 pagesFundamentals of Nursing: Client Teaching On Abdominal (Diaphragmatic) and Pursed-Lip BreathingSean Lloyd RigonNo ratings yet
- The Philippine Nursing Act of 2002Document8 pagesThe Philippine Nursing Act of 2002Reyhan FloresNo ratings yet
- Operating Room Instruments by JheaaDocument78 pagesOperating Room Instruments by JheaaSareno PJhēa100% (1)
- Suction SOP 2018Document13 pagesSuction SOP 2018ika lestariNo ratings yet
- Dr. H. Achmad Fuadi, SPB-KBD, MkesDocument47 pagesDr. H. Achmad Fuadi, SPB-KBD, MkesytreiiaaNo ratings yet
- Arabic To Communicate With PatientsDocument19 pagesArabic To Communicate With PatientsDK Aquino GomezNo ratings yet
- PH CM 1 Cu 2 - Pharmacodynamics - 1Document10 pagesPH CM 1 Cu 2 - Pharmacodynamics - 1Chesca DomingoNo ratings yet
- Faq IvtDocument9 pagesFaq IvtFilipino Nurses CentralNo ratings yet
- The Dying Patient's Bill of RightsDocument6 pagesThe Dying Patient's Bill of Rightsshanalee_1567% (3)
- LeiningerDocument4 pagesLeiningerAngelie SanchezNo ratings yet
- Communicable DiseaseDocument3 pagesCommunicable Diseasemiss RNNo ratings yet
- Lesson 12Document12 pagesLesson 12Vienna Corrine Q. AbucejoNo ratings yet
- 01 NI Course Unit 1 PDFDocument12 pages01 NI Course Unit 1 PDFQueency Khen GulayNo ratings yet
- GenitoUri Post TestDocument5 pagesGenitoUri Post Testlourd nabNo ratings yet
- Copd Concept MapDocument2 pagesCopd Concept MapAziil LiizaNo ratings yet
- Operating Room Write UpDocument2 pagesOperating Room Write UpEnrico Sapitula Del RosarioNo ratings yet
- Trans Cultural Nursing 1Document28 pagesTrans Cultural Nursing 1Heide Hamoy Sibonga100% (1)
- Or Write Up (Appendectomy) : Pines City Colleges College of NursingDocument9 pagesOr Write Up (Appendectomy) : Pines City Colleges College of Nursingthomasfinley44No ratings yet
- NCP For Acvute PainDocument6 pagesNCP For Acvute PainGlenn ValerioNo ratings yet
- Informed Consent Form: Where Soul Empowers TechnologyDocument9 pagesInformed Consent Form: Where Soul Empowers TechnologyZg ZernNo ratings yet
- Rubrics For Grand Case PresentationDocument2 pagesRubrics For Grand Case PresentationRichard Allan SolivenNo ratings yet
- KineticsDocument35 pagesKineticsMary Loise VillegasNo ratings yet
- Discharge Planning ChecklistDocument6 pagesDischarge Planning ChecklistcutevivesNo ratings yet
- Questionaire-Nursing ResearchDocument2 pagesQuestionaire-Nursing ResearchEJ Cubero, R☤NNo ratings yet
- Assignment For BSN 3 - A - RLEDocument2 pagesAssignment For BSN 3 - A - RLEKarina Madriaga100% (1)
- Complete Health AssessmentDocument3 pagesComplete Health AssessmentQueensterNo ratings yet
- Learning Activity N3A & N3BDocument3 pagesLearning Activity N3A & N3BMikaela JosonNo ratings yet
- NCM 116 ChecklistsDocument11 pagesNCM 116 ChecklistsJoy DamoNo ratings yet
- Definition of Organization and ManagmentDocument2 pagesDefinition of Organization and ManagmentAlmira GamaoNo ratings yet
- Community Health Nursing Case Presentation: Bukidnon State University College of NursingDocument16 pagesCommunity Health Nursing Case Presentation: Bukidnon State University College of NursingAlmira GamaoNo ratings yet
- 11 - Family Nursing Care PlanDocument9 pages11 - Family Nursing Care PlanAlmira GamaoNo ratings yet
- An Investigatory Project On Bukidnon Traditional Herbal MedicineDocument15 pagesAn Investigatory Project On Bukidnon Traditional Herbal MedicineAlmira GamaoNo ratings yet
- Skill: Assessing The Mouth and Oropharynx: Lips and Buccal MucosaDocument3 pagesSkill: Assessing The Mouth and Oropharynx: Lips and Buccal MucosaAlmira GamaoNo ratings yet
- Skill: Assessing The Thorax and LungsDocument3 pagesSkill: Assessing The Thorax and LungsAlmira GamaoNo ratings yet
- Anatomy and Physiology of Female Reproductive System: External Generative OrgansDocument28 pagesAnatomy and Physiology of Female Reproductive System: External Generative OrgansAlmira Gamao100% (1)
- NeckDocument2 pagesNeckAlmira GamaoNo ratings yet
- Skill: Assessing The Neurological System: LanguageDocument9 pagesSkill: Assessing The Neurological System: LanguageAlmira GamaoNo ratings yet
- Anatomy and Physiology of The Breast: Mammary GlandsDocument10 pagesAnatomy and Physiology of The Breast: Mammary GlandsAlmira GamaoNo ratings yet
- Chapter-3-BukCul (1) ....Document4 pagesChapter-3-BukCul (1) ....Almira GamaoNo ratings yet
- Chapter-I 0Document5 pagesChapter-I 0Almira GamaoNo ratings yet
- Administering Topical Medication ScriptDocument2 pagesAdministering Topical Medication ScriptAlmira GamaoNo ratings yet
- Topical ChecklistDocument2 pagesTopical ChecklistAlmira GamaoNo ratings yet
- Chapter 2 FINALDocument2 pagesChapter 2 FINALAlmira GamaoNo ratings yet
- Dr. Paulino J. Garcia Memorial Research and Medical Center ISO QMS Certified Tumor Boards (May 2022)Document12 pagesDr. Paulino J. Garcia Memorial Research and Medical Center ISO QMS Certified Tumor Boards (May 2022)Ardy Antonio MDNo ratings yet
- Licensed FacilitiesDocument32 pagesLicensed FacilitiesSunday AyomideNo ratings yet
- Satairapan Starting Intravenous InfusionDocument3 pagesSatairapan Starting Intravenous InfusionMichelle SatairapanNo ratings yet
- Radiol 13121947Document7 pagesRadiol 13121947Eduardo Agustín Vargas CamposNo ratings yet
- Jackdip Mondal - Project Report - Bba HM 681Document33 pagesJackdip Mondal - Project Report - Bba HM 681Sahil MostakNo ratings yet
- Vats Bullectomy: Initial Shillong ExperienceDocument21 pagesVats Bullectomy: Initial Shillong ExperiencelmdarlongNo ratings yet
- Suctioning: Leny Vicente-Baguio RN, MN Xavier University-Ateneo de Cagayan College of NursingDocument18 pagesSuctioning: Leny Vicente-Baguio RN, MN Xavier University-Ateneo de Cagayan College of NursingSheena Mae GonzagaNo ratings yet
- Atom Electrosurgical SystemDocument40 pagesAtom Electrosurgical SystemOgut AjaNo ratings yet
- Above Knee AmputationDocument4 pagesAbove Knee AmputationAdit Wendy YRNo ratings yet
- ISAPS 8 2 InteractiveDocument27 pagesISAPS 8 2 Interactivehuyenthanh1807No ratings yet
- Pre Operative Planning For Total Hip ArthroplastyDocument78 pagesPre Operative Planning For Total Hip ArthroplastyJulio EspinozaNo ratings yet
- HM3 in FontonDocument2 pagesHM3 in FontonselvakumarNo ratings yet
- 12 Hospital AdmissionDocument8 pages12 Hospital AdmissionСветлана РоманенкоNo ratings yet
- Interventional Cardiac Electrophysiology - A Multidisciplinary Approach Section 1, Technology and Therapeutic Techniques - PDF RoomDocument306 pagesInterventional Cardiac Electrophysiology - A Multidisciplinary Approach Section 1, Technology and Therapeutic Techniques - PDF RoomVeronica JanethNo ratings yet
- QP Code: Reg - No.: MS Degree Examinations in General SurgeryDocument4 pagesQP Code: Reg - No.: MS Degree Examinations in General SurgeryRaman BhavanaNo ratings yet
- Validity of Minnesota Multiphasic Personality Inventory - 2 - Restructured Form (MMPI-2-RF) Scores As A Function of Gender, Ethnicity, and Age of Bariatric Surgery CandidatesDocument8 pagesValidity of Minnesota Multiphasic Personality Inventory - 2 - Restructured Form (MMPI-2-RF) Scores As A Function of Gender, Ethnicity, and Age of Bariatric Surgery CandidatesCarlos Augusto Lopez AcevoNo ratings yet
- Rajani. CH: 11 JUNE 1987, IDocument6 pagesRajani. CH: 11 JUNE 1987, IRAJANI CHNo ratings yet
- Star Health and Allied Insurance Company LimitedDocument16 pagesStar Health and Allied Insurance Company LimitedSivaReddyNo ratings yet
- 4-Biliary InjuryDocument228 pages4-Biliary InjuryHamidHassanNo ratings yet
- Antral Puncture and LavageDocument9 pagesAntral Puncture and Lavagesimi yNo ratings yet
- Peterson's Principals of Oral and Maxyofacial Surgery Ch.0008 - Impacted TeethDocument18 pagesPeterson's Principals of Oral and Maxyofacial Surgery Ch.0008 - Impacted TeethДимитър АлександровNo ratings yet
- Acute Pain RUTH FinalDocument7 pagesAcute Pain RUTH FinalRuthangela GarciaNo ratings yet
- Syllabus On Inflammatory Bowel DiseaseDocument9 pagesSyllabus On Inflammatory Bowel DiseasePTDBNo ratings yet
- Flexifed 1 Elect Individual Option BrochureDocument25 pagesFlexifed 1 Elect Individual Option BrochurescannertplinkNo ratings yet
- Ocular ProstheticsDocument2 pagesOcular ProstheticsEshiramhe AugustineNo ratings yet
- Healthcare Benefit Orientation: April 01, 2019 To March 31, 2020Document49 pagesHealthcare Benefit Orientation: April 01, 2019 To March 31, 2020HRD-EFI PampangaNo ratings yet
- Job Description of ICU Staff NurseDocument1 pageJob Description of ICU Staff NurseGAGANJOT8550% (2)
- Pamili Juan Pricelist UpdatedDocument10 pagesPamili Juan Pricelist UpdatedKatrina AmistadNo ratings yet
- ECMO in Emergency SettingDocument42 pagesECMO in Emergency Settingppds btkvNo ratings yet