Professional Documents
Culture Documents
Lecture 28 Thyroid Pathophys
Uploaded by
Ahmed MashalyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lecture 28 Thyroid Pathophys
Uploaded by
Ahmed MashalyCopyright:
Available Formats
Lecture 28 Thyroid Pathophysiology MacLeod
THYROID GLAND ANATOMY: SYNTHESIS & SECRETION OF THYROID HORMONES:
Butterfly-shaped gland located in neck region sitting on either 1. Uptake of iodide and transport to extracellular component of follicular cells
side of the trachea a. Iodide is concentrated in thyroid follicle cells by active transport via
Thyroid follicles (spheres of a layer of thyroid epithelial cells) Na+/I- symporter (NIS)
surrounding colloid (gelatinous material) NIS is highly expressed in thyroid gland (low levels in other tissues) allows
use of radioactive iodine for dx & txt of hyperthyroidism & thyroid cancer
with limited effects on other organs
THYROID HORMONES:
b. Iodide is effluxed into extracellular colloid by iodide channel in apical membrane
Thyroxine T4: major circulating form of TH
Triiodothyronine T3: responsible for biological activity 2. Formation of thyroid hormone in extracellular colloid
a. Thyroid peroxidase (TPO)* incorporates iodine into tyrosine residues in
REGULATION OF THYROID HORMONE PRODUCTION: thyroglobulin at:
1. Hypothalamus releases TRH to the pituitary gland increase o Carbon 3 monoiodotyrosine (MIT)
production of TSH o Carbon 3 and 5 diiodotyrosine (DIT)
2. TSH acts at specific receptors (TSH-R) on thyroid to increase b. TPO also couples:
expression of NIS, thyroid peroxidase, and thyroglobulin o MIT + DIT T3
increases hormone synthesis and release o DIT + DIT T4
Also increases growth & differentiation of thyroid follicles
3. Negative feedback: as levels of TH increase (in particular T3), it * TPO located on apical surface of thyroid follicular cell
feeds back on the pituitary and hypothalamus to decrease the
release of their hormones 3. Release into the circulation
a. Endocytosis of colloid that contains thyroglobulin (back into thyroid follicle cell)
REGULATION OF TH PRODUCTION BY IODIDE: b. Lysosomal degradation of thyroglobulin with release of T4 and T3
Synthesis of TH depends on adequate intake of dietary iodine Some T4 is deiodinated in thyroid to T3 (which is also released into blood)
o Highest amounts of naturally occurring iodine found in c. Released MIT and DIT can be deiodinated within the thyroid and iodide is
seafood and seaweed (concentrated from seawater) recycled for new hormone synthesis
Iodine deficiency major cause of thyroid dysfunction globally
o BUT not seen in Canada because Health Canada requires
the iodization of table salt DEIODINASES: REGULATION IN THYROID HORMONE LEVELS
Iodide exerts an “autoregulatory” effect at level of thyroid: Catalyze:
o Plasma iodide levels inversely regulate activity of NIS a. 5’-deiodination of T4 to T3 – type 1 or 2
b. T4 to reverse T3 (rT3) – type 1 or 3 (inactivating)
As iodine intake falls, uptake of iodide by the gland
c. T3 to T2 – type 3 (inactivating)
increases to maintain TH synthesis
o HOWEVER, very large doses of iodide inhibit iodination of
Three types:
thyroglobulin & release of TH
o Type 1: major source of circulating T3
Inhibition is only transient (downregulation of NIS
Blocked by propylthiouracil (PTU) – thoamide anti-thyroid drug
reduced uptake of iodide hormone
o Type 2: major source of intracellular T3 (found in brain, pituitary, muscle, fat, etc)
production & release resume)
o Type 3: major inactivating deiodinase
THYROID HORMONE TRANSPORT: PHYSIOLOGICAL FUNCTION OF THYROID HORMONES:
Circulating T4 and T3 almost entirely bound to plasma proteins: 1) Growth and development
o Thyroxine binding globulin (TBG) most important a. Fetal and neonatal CNS development
Bound and free TH is in reversible equilibrium b. Skeletal growth (with GH)
o Only free is metabolically active 2) Metabolism
In normal thyroid function, an increase (or decrease) in TBG a. Increase basal metabolic rate, oxygen consumption
levels will result in an increase (or decrease) in TOTAL (bound + b. Stimulate adipose tissue lipolysis
free) hormone, but minimal changes in free hormone c. Increase muscle protein breakdown
3) Actions on the heart
EXAMPLE: ESTROGEN-INDUCED INCREASE IN TBG IN PREGNANCY a. Increase rate and force of cardiac contraction
b. Sensitize heart to catecholamines
MECHANISM OF THYROID HORMONE ACTION:
Nuclear thyroid hormone receptors (TR) are bound to thyroid hormone response
elements (TRE) mainly has heterodimers with retinoid X receptors (RXR)
In absence of T3, binding of co-repressor (CoR) proteins repress its action
When T3 enters nucleus, it’s binding to TR promotes dissociation of CoR,
recruitment of coactivators (CoA), and altered gene expression
COMPARISON OF PROPERTIES OF T4 AND T3:
T4 T3
Serum concentration
Total 8 ug/Dl 0.14 ug/dL
% free 0.02 % 0.3 %
Serum half-life 7 days 0.75 days
Fraction from thyroid 100% 20%
Intracellular hormone fraction 20% 70%
Relative receptor binding affinity 1 10
Lecture 28 Thyroid Pathophysiology MacLeod
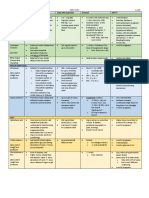
EVALUATION OF THYROID FUNCTION: THYROID FUNCTION TESTING:
TSH Most sensitive and useful index of primary thyroid disease and effectiveness of txt Recommended when non-specific S/S
Usually used as initial test for investigation of thyroid disease are present in pts at risk:
Normal levels usually 0.5 – 5.0 mU/L Hx of thyroid disease
If abnormal, followed by measurement of TH levels Strong family hx of thyroid disease
Free Preferable to measuring total T4 levels (which can vary due to changes in TBG = unrelated to thyroid Diagnosis of autoimmune disease
serum T4 disease) Past hx of neck irradiation
(FT4) Correlated with TSH better than FT3 levels because is principle hormone released in response to TSH Drug therapies such as lithium and
In most cases, FT4 is sufficient to confirm diagnosis amiodarone
Free Not indicated in hypothyroidism Women over age 50
serum T3 Used when hyperthyroidism is suspected (due to suppression of TSH) but FT4 is not elevated Elderly patients
(FT3) 2-5% of hyperthyroid pts experience elevation of ONLY T3 levels Women 6 wk – 6 mo post-partum
THYROID DISORDERS: GOITER HYPOTHYROIDISM: results from insufficient production of thyroid hormone
Any enlargement of the thyroid gland Types:
May be associated with no change, increase or decrease in hormone o Primary: level of thyroid gland
secretion, depending on cause o Secondary: suprathyroid (at hypothalamus or pituitary gland)
SIMPLE OR NON-TOXIC GOITER: thyroid enlargement without functional, o Congenital or acquired
inflammatory, or neoplastic changes Can vary in severity from very mild to overt
Occurs when the thyroid gland does not secrete sufficient hormone to CAUSES OF HYPOTHYROIDISM:
meet tissue demands Hashimoto’s (chronic lymphocytic) thyroiditis (= inflammation of thyroid)
Results in increased release of TSH or increased sensitivity of o Most common cause of hypothyroidism
thyroid to TSH o Older women at particular risk
Resulting increase in functioning mass of thyroid overcomes o Autoimmune disorder (raised circulating levels of thyroid
mild impairment of hormone production, and pt becomes peroxidase (TPO) antibody)
metabolically normal o Thyroid cell destruction mediated primarily by cytotoxic T cells
Can result from iodine deficiency, defect in hormone synthesis o Goiter may be present early in disease
Congenital hypothyroidism: hypothyroidism in newborn infants (1:3000)
o Results in severe mental + physical growth retardation if untreated
HYPERTHYROIDISM: results from an increase in secretion of thyroid hormones o Early treatment is crucial for normal intellectual development
Primary or secondary o Clinical dx is difficult, in Canada we measure TSH levels in neonates
Vary in severity Juvenile myxedema: hypothyroidism in children > 2 years
o Results in linear growth retardation + delayed puberty if untreated
CAUSES OF HYPERTHYROIDISM:
Myxedema coma: end stage of poorly or un-controlled hypothyroidism
Graves Disease: most common
o Almost always occurs in elderly and precipitated by factors that
o 10x more common in women; 20-50 years of age
impair respiration
o Autoimmune disease, with IgG antibodies (TRAb or TSI) that
bind to and stimulate the TSH receptor on thyroid
80% also have TPO antibodies TYPICAL LAB FINDINGS:
Toxic multinodular goiter: multiple autonomous thyroid nodules TSH Ft4 Ft3
Toxic adenoma: solitary, benign thyroid tumor Subclinical hypothyroidism Borderline elevated Normal
TSH-secreting pituitary adenoma Overt hypothyroidism Elevated Low
TYPICAL LAB FINDINGS: S/S: everything slows down
TSH Ft4 Ft3 Poor memory & concentration, slow pulse rate, myxedema
Subclinical hyperthyroidism Low Normal Fatigue, feeling cold, weight gain + poor appetite, hair loss, constipation
Clinical hyperthyroidism Elevated Usually Elevated
elevated
THYROID DISORDERS IN PREGNANCY:
Hypothyroidism Hyperthyroidism
S/S: Increased risk of obstetrical If uncontrolled, risk to both
Heat intolerance, weight loss, tremor, difficulty sleeping, anxiety, complications (fetal death, mother and fetus:
irritability, flushed skin, tachycardia gestational HTN) o Miscarriage, pre-term
Atrial fibrillation can occur in elderly Can result in cognitive defects labor, HTN
Increased bone loss and risk of osteoporotic fracture (lower IQ defects, impaired o Still birth, low birth
psychomotor development) in weight, fetal goiter
SPECIFIC TO GRAVE’S DISEASE: offspring In Graves Disease: maternal
Graves opthalmopathy (exophthalmos or proptosis) – 30% Very important to detect and TRAb can cross placenta and
o Lid retraction, periorbital edema, protrusion of eye adequately treat hypothyroidism cause fetal hyperthyroidism
o Can lead to discomfort, impaired vision both before and during pregnancy after 20 weeks gestation
o Due to cytokine production by infiltrating T cells (inflammation)
Graves dermopathy - < 5%
o Most frequent on lower legs POST-PARTUM THYROIDITIS (PPT): 5-10% of women past-partum
o Typically skin is deep pink, with “orange-skin” appearance Autoimmune disorder, usually mild and transient
Significant risk of recurrent PPT in subsequent pregnancies
Increased risk of developing primary hypothyroidism within 5-10 years
THYROID STORM OR THYROTOXIC CRISIS:
Life-threatening increase in severity of hyperthyroidism (uncommon)
Usually precipitated in uncontrolled or poorly controlled pts by
another medical problem (e.g. infection, surgery)
Characterized by fever, tachycardia, confusion, N&V
Fatality rate approx. 20%
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Connexus SigcodesDocument8 pagesConnexus SigcodesAhmed Mashaly100% (1)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Pharmacology MCQS WITH ANS (1) - CompressedDocument289 pagesPharmacology MCQS WITH ANS (1) - Compressed09Dhawal PatilNo ratings yet
- Sample Letter To Consular Section, Us Embassy/Consulate Supporting Application For Visa (Or Renewal/Extension) by Foreign IndividualDocument1 pageSample Letter To Consular Section, Us Embassy/Consulate Supporting Application For Visa (Or Renewal/Extension) by Foreign IndividualZodin100% (3)
- Health AssessmentDocument28 pagesHealth AssessmentPiyush Dutta100% (2)
- LIFELINE SBSG Practice HandbookDocument140 pagesLIFELINE SBSG Practice HandbookAmethyst CareyNo ratings yet
- Nine Simple Ways To Make It Easier To (Re) Use Your Data Vol 6 No 2 (2013) : Special Issue - Data Sharing in Ecology and EvolutionDocument10 pagesNine Simple Ways To Make It Easier To (Re) Use Your Data Vol 6 No 2 (2013) : Special Issue - Data Sharing in Ecology and EvolutionalbgomezNo ratings yet
- Lecture 29 30 Thyroid TherapeuticsDocument3 pagesLecture 29 30 Thyroid TherapeuticsAhmed MashalyNo ratings yet
- Lecture 31 Osteoporosis Pathophys FlattenedDocument3 pagesLecture 31 Osteoporosis Pathophys FlattenedAhmed Mashaly100% (1)
- Osteoporosis Pharmacology Drugs Bone Remodeling BisphosphonatesDocument4 pagesOsteoporosis Pharmacology Drugs Bone Remodeling BisphosphonatesAhmed Mashaly100% (1)
- Lecture 39 Nhps in DMDocument1 pageLecture 39 Nhps in DMAhmed MashalyNo ratings yet
- Ontario COVID-19 Vaccination ServiceDocument4 pagesOntario COVID-19 Vaccination ServiceAhmed MashalyNo ratings yet
- Legal Issues in Clinical ResearchDocument48 pagesLegal Issues in Clinical ResearchAhmed MashalyNo ratings yet
- 4 Joneckis, Chris-02-16-16Document62 pages4 Joneckis, Chris-02-16-16OstazNo ratings yet
- Lecture 33 Osteoporosis TherapeuticsDocument1 pageLecture 33 Osteoporosis TherapeuticsAhmed MashalyNo ratings yet
- Research EthicsDocument114 pagesResearch EthicsAhmed MashalyNo ratings yet
- Ethical Principles in Clinical ResearchDocument46 pagesEthical Principles in Clinical ResearchAhmed MashalyNo ratings yet
- An Overview of File Formats JsonDocument3 pagesAn Overview of File Formats JsonAhmed MashalyNo ratings yet
- Manual-2016 4Document257 pagesManual-2016 4Ahmed MashalyNo ratings yet
- Research EthicsDocument114 pagesResearch EthicsAhmed MashalyNo ratings yet
- Amber 14Document826 pagesAmber 14Ahmed MashalyNo ratings yet
- Journal of The Taiwan Institute of Chemical EngineersDocument13 pagesJournal of The Taiwan Institute of Chemical EngineersAhmed MashalyNo ratings yet
- Medical - Chemestry Q&ADocument13 pagesMedical - Chemestry Q&AAhmed MashalyNo ratings yet
- 1 Gallin, John-10-13-15-Handouts-Color-1Document29 pages1 Gallin, John-10-13-15-Handouts-Color-1OstazNo ratings yet
- Friedel CraftsDocument8 pagesFriedel CraftsAhmed MashalyNo ratings yet
- Implementation of Total Quality Management in HospitalsDocument6 pagesImplementation of Total Quality Management in HospitalsAhmed Mashaly100% (1)
- Integrated modeling system for structural biologyDocument10 pagesIntegrated modeling system for structural biologyAhmed MashalyNo ratings yet
- Medical - Chemestry Q&ADocument13 pagesMedical - Chemestry Q&AAhmed MashalyNo ratings yet
- General Information On Medical Certificates and List of Accredited Clinics of The Embassy of BelgiumDocument4 pagesGeneral Information On Medical Certificates and List of Accredited Clinics of The Embassy of BelgiumAhmed MashalyNo ratings yet
- Conversion of GradesDocument61 pagesConversion of GradesAhmed Mashaly0% (1)
- Student Cover LetterDocument1 pageStudent Cover LetterAhmed MashalyNo ratings yet
- Pharmaceutical Biotechnology: Master's Degree CourseDocument2 pagesPharmaceutical Biotechnology: Master's Degree CourseAhmed MashalyNo ratings yet
- Cardiac DysrhythmiaDocument1 pageCardiac DysrhythmiaAhmed MashalyNo ratings yet
- SEO-Optimized Title for Liquichek Cardiac Markers Plus Control DocumentDocument25 pagesSEO-Optimized Title for Liquichek Cardiac Markers Plus Control DocumentAde FeriyatnaNo ratings yet
- Second MbbsDocument2 pagesSecond MbbsPriya SelvarajNo ratings yet
- Lista de Preturi: Subcontractat Analiza Acreditata RENARDocument9 pagesLista de Preturi: Subcontractat Analiza Acreditata RENARalexrodyNo ratings yet
- Experiment 6-Linkage and Sex LinkageDocument4 pagesExperiment 6-Linkage and Sex LinkageNUR SABRINA MOHD SHAHNo ratings yet
- Worksheet in General Biology 2: Quarter 1 - Week 3: Theories of Evolution and The Development of Evolutionary ThoughtDocument10 pagesWorksheet in General Biology 2: Quarter 1 - Week 3: Theories of Evolution and The Development of Evolutionary ThoughtShastine ClaorNo ratings yet
- Bonne Pratique D'hygiéne PoissonDocument147 pagesBonne Pratique D'hygiéne PoissonLaila HomeNo ratings yet
- Carbohydrates in Food Science: Carbohydrates Are Sugar andDocument2 pagesCarbohydrates in Food Science: Carbohydrates Are Sugar andCaryl Alvarado SilangNo ratings yet
- Classification of NF by DR MKBDocument33 pagesClassification of NF by DR MKBiloveusonNo ratings yet
- BotanyDocument28 pagesBotanyAnnabelle Phen LeeNo ratings yet
- HAPL 3 & 4 - The Nervous SystemDocument10 pagesHAPL 3 & 4 - The Nervous SystemwelpNo ratings yet
- Anti-Isthmus Autoimmunity in A Novel Feline Acquired Alopecia Resembling Pseudopelade of HumansDocument10 pagesAnti-Isthmus Autoimmunity in A Novel Feline Acquired Alopecia Resembling Pseudopelade of HumansjenNo ratings yet
- Role of Intravenous Amino Acid Infusion in Cases of Oligohydramnios and Its Effect On Amniotic Fluid Index and Fetal Weight GainDocument6 pagesRole of Intravenous Amino Acid Infusion in Cases of Oligohydramnios and Its Effect On Amniotic Fluid Index and Fetal Weight GainRahimshaikhNo ratings yet
- The Biomedical Engineering Handbook: Second EditionDocument13 pagesThe Biomedical Engineering Handbook: Second EditionEng-Mugahed AlmansorNo ratings yet
- Maternal and Child Health ReferencesDocument4 pagesMaternal and Child Health ReferencesMeyke PotutuNo ratings yet
- Plant MovementDocument25 pagesPlant MovementMichael PradhanNo ratings yet
- Discover MARDIDocument33 pagesDiscover MARDIMARDI Scribd75% (4)
- Aiims 2005Document33 pagesAiims 2005pravinkhartadNo ratings yet
- Regenerative Medicine and Tissue Engineering - Cells and BiomaterialsDocument602 pagesRegenerative Medicine and Tissue Engineering - Cells and BiomaterialsMarlena RindasuNo ratings yet
- WEF Building BlockchainsDocument37 pagesWEF Building BlockchainsvsrajkumarNo ratings yet
- Fotosintesis 1213Document25 pagesFotosintesis 1213scanny16No ratings yet
- CARY 100 BrochureDocument20 pagesCARY 100 BrochureNghia BiiNo ratings yet
- Company C Inoc Harvest FinalDocument10 pagesCompany C Inoc Harvest FinalMubarak PatelNo ratings yet
- Bacterial StructureDocument72 pagesBacterial StructureKrittika ChatterjeeNo ratings yet
- Sindy BeckerDocument11 pagesSindy BeckerHafidz GalantNo ratings yet
- Stereographical SchrodingerDocument19 pagesStereographical SchrodingerSpirosKoutandosNo ratings yet
- EiareportDocument299 pagesEiareportcoolmagaNo ratings yet
- Angiosperm Classifications ExplainedDocument41 pagesAngiosperm Classifications ExplainedHarimohan Thakuriya JaipurNo ratings yet