Professional Documents
Culture Documents
Osteoporosis Pharmacology Drugs Bone Remodeling Bisphosphonates
Uploaded by
Ahmed MashalyOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Osteoporosis Pharmacology Drugs Bone Remodeling Bisphosphonates
Uploaded by
Ahmed MashalyCopyright:
Available Formats
Lecture 32 Osteoporosis Pharmacology MacLeod
EFFECTS OF DRUGS ON BONE REMODELING:
BMU activation is relatively low
In each unit, balance between bone resorption and bone formation
In long-run, may be more promising because they prevent bone loss
AND stimulate bone formation
1. MARROW PRECURSOR TOOL:
Increase rate of initiation of cycles = more bone remodeling Increase activation of BMU but greater formation than resorption
Resorption > formation Transient short-term effect of positive bone balance
2. PRE-OSTEOBLASTS:
Pipeline drugs (being studied)
Directly activate pre-osteoblasts without activating BMU cycle
Increase in bone formation is not coupled to bone resorption
Suppress osteoclast activity = reduce BMU activation
Decrease bone resorption without affecting bone activation
= positive bone balance (short-term effect)
ANTI-RESORPTIVE (ANTI-CATABOLIC) DRUGS
EFFECT OF ANTI-RESORPTIVE DRUGS ON BONE:
Decrease activation frequency of BMU
(reducing bone turnover) by inhibiting
osteoclast activity
EFFECT ON BMD IS TRANSIENT Decrease resorption
w/o affecting formation
A-B: rapid increase in BMD as anti-resorptive drug suppresses formation of new
remodeling sites, and re-filling of sites already resorbed continues
B-D: slower secondary mineralization of new bone continues for years, and
some remodeling takes place but with fewer, shallower resorption cavities
HRT AND OSTEOPOROSIS:
Estrogen alone or with progestins Raloxifene
(0.625 mg conjugated equine estrogens +
2.5 mg medroxy-progesterone acetate)
Coronary heart disease ↑ -
Breast cancer ↑ (> 5 years therapy) ↓
BMD ↑ ↑ (but less than estrogen or alendronate)
Fracture ↓ hip, vertebral, non-vertebral ↓ vertebral only (by 50%)
Venous thromboembolism ↑ ↑
Menopausal symptoms ↓ ↑
NOTES Use of HRT restricted to treatment of mod-severe vasomotor symptoms Selective estrogen receptor modifier (SERM) that
Use lowest possible dose and normally limit to < 5 years mimics actions of estrogen in bone, but opposes
Osteoporosis prevention = secondary benefit actions in breast
Lecture 32 Osteoporosis Pharmacology MacLeod
BISPHOSPHONATES (ANTI-RESORBTIC DRUGS CONT):
GENERAL STRUCTURE: Aminobisphosphonates (alendronate, risedronate, zoledronate) MECHANISM OF ACTION:
OH in R1 = better binding and enhanced potency 1. Incorporated into bone, then released
N in R2 = increased potency when hydroxyapatite dissolved by
osteoclast acid
2. Taken up into osteoclasts
preferentially (by endocytosis)
o Impair recruitment,
Etidronate: CH3 differentiation & activity of
2nd gen: OH osteoclasts
o Increase osteoclast apoptosis
3. Osteoblast activity continues = re-
filling of remodeling space
4. Results in reduction in activation of
Etidronate: OH new BMU = decreased bone turnover
2nd gen: amine
ETIDRONATE: ALENDRONATE, RISEDRONATE, ZOLEDRONATE EFFICACY:
First-generation bisphosphonate 2nd and 3rd generation bisphosphonates
Doses that inhibit bone resorption also impair bone mineralization Much more potent inhibitors of bone resorption than etidronate
o If used continuously, results in accumulation of Inhibit bone resorption at doses that do not affect bone mineralization
unmineralized osteoid (osteomalacia) o Alendronate: 10 mg daily or 70 mg weekly
o To avoid, give cyclically: 14 days etidronate 400 mg/d, o Risedronate: 5 mg daily, 35 mg weekly, or 150 mg monthly
followed by 76 days of calcium carbonate 500 mg/day o Zoledronate: 5 mg once/year by IV infusion
In women with T-score ≤ 2.0 or previous fracture: decreased risk of In women with T-score score ≤ 2.0 or previous fracture: decreased risk
vertebral fracture (RR 50%, ARR 5%) o Hip RR 25-50%, ARR 1%
o Vertebral RR 45-70%, ARR 5-7%
ADME of oral bisphosphonates: etidronate, alendronate, risedronate o Non-vertebral RR 20-25%, ARR 2%
Very poorly absorbed (1-5%) so MUST be taken on AN EMPTY
STOMACH with water only (= 30 – 60 min before first meal of day to ADVERSE EFFECTS:
allow for adequate absorption) ORAL ADMINISTRATION:
o EXCEPT delayed release risedronate is taken with food GI upset (abdominal pain, NVD)
Plasma life is 1 hr Severe esophagitis: pt must take it in upright position with full glass of water
o 50% is excreted by kidney and remain upright for further 30 min
o 50% taken up by bone, where half-life is very long (> 10 yrs)
ZOLEDRONATE: transient flu-like symptoms on injection
USES OF BISPHOSPHONATES:
OSTEONECROSIS OF JAW: < 1:10,000 in pts treated for osteoporosis
Prevention & treatment of osteoporosis in postmenopausal women
o Anti-fracture efficacy shown for 7-10 years Exposed necrotic bone in jaw region, not healing after 6-8 wk
o Optimal duration of treatment not fully established 90% of cases seen on IV administration of high doses for > 2 years in CA pts
o Clinical trials suggest that on discontinuation after 5 yrs, bone o Most after dental extraction (therefore recommended to avoid)
remodeling remains suppressed for at least 5 yrs May be due to highly suppressed bone turnover
Associated with increased risk of vertebral but not Can lead to severe pain and other complications, and is difficult to treat
non-vertebral or all fractures compared to women
who remained on the drug ATYPICAL FEMUR FRACTURES:
To increase BMD in men with osteoporosis Overall < 1% of all hip fractures
Prevention & treatment of glucocorticoid-induced osteoporosis Bisphosphonate use increase absolute risk by 1-5 cases per 10,000 pt/year
Paget’s disease of the bone in men and women o Risk increases with increasing duration of use
Treatment of bone metastases of various types of cancer o Risk decreases on discontinuation
o High doses of high potency preparations NOTE that risk of typical hip fracture is 75-420 per 10,000 high risk pts/yr
o Reduce bone pain and risk of fractures o Therefore benefit of bisphosphonate >> risk of this fracture
POSSIBLE EFFECTS OF LONG-TERM THERAPY ON BONE QUALITY:
Lecture 32 Osteoporosis Pharmacology MacLeod
DENOSUMAB (ANTI-RESORPTIVE DRUGS CONT):
MECHANISM: USES:
Monoclonal antibody to RANKL that mimics the actions of OPG Approved for severe osteoporosis in postmenopausal women
o Binds to RANKL and prevents its binding to RANK o In clinical trials, reduced risk of vertebral fracture by 60%,
Results in a marked decrease in osteoclast formation and bone resorption non-vertebral fracture by 20% and hip fracture by 40% in
women with T-score < -2.5
In higher doses, to prevent skeletal-related events in pts with bone
DOSE FOR OSTEOPOROSIS: metastases from solid tumors
Given as 60 mg SC injection every 6 months May be useful in conditions characterized by temporary, rapid bone
Suppressive effect on bone resorption wears off by 6m after last dose resorption (e.g. aromatase inhibitor treatment)
ADVERSE EFFECTS:
Hypocalcaemia (2%)
Serious infections including cellulitis (because RANK-RANKL system is used by immune cells)
Eczema (10%)
Osteonecrosis of jaw when used in higher doses for bone metastases in cancer treatment (expected because it’s a potent inhibitor)
Atypical fractures reported (expected because bone turnover is suppressed almost completely)
ANABOLIC DRUGS:
EFFECT OF ANABOLIC DRUGS ON BONE:
MECHANISM OF ANABOLIC DRUGS:
Increase activation frequency (number of BMUs)
Increase amount of bone formed by each BMU (due to stimulation of
osteoblast activity)
AND/OR
Stimulate osteoblast activity directly, without a preceding resorption phase
TERIPARATIDE: rhPTH(1-34): sequence identical to the 34 n-terminal amino acids of human PTH
MECHANISM OF ACTION: MECHANISMS INVOLVED IN ANABOLIC EFFECTS OF PTH ON BONE:
Intermittent administration of PTH and teriparatide increases
bone remodeling, with a relatively greater increase in bone
formation than resorption (anabolic effect)
o Acts by increasing recruitment and differentiation of
osteoblasts and decreasing their apoptosis
o Anabolic window appears to last about 12-18 months,
after which effects fade
This is followed by a subsequent stimulation of bone resorption
EFFICACY:
In postmenopausal women with prior vertebral fractures
(secondary prevention):
o Decreased risk of both vertebral fracture by 65% and
non-vertebral fracture by 53%
o No significant decrease in risk of hip fracture (but study
not powered for this)
USES: ADVERSE EFFECTS:
Severe osteoporosis in post-menopausal women Well tolerated but may induce hypercalcemia and/or hypercalciuria
Glucocorticoid-induced osteoporosis in high-risk patients Treatment duration limited to 2 years
Bone density increase will be lost on D/C unless followed with anti-
Given by once daily SC injection and is expensive resorptive agent
Lecture 32 Osteoporosis Pharmacology MacLeod
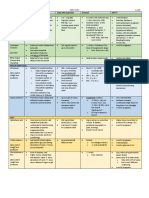
SUMMARY OF AGENTS USED FOR OSTEOPOROSIS: ( 1 - RR = RRR) (use McCormack's lecture for exam purposes??)
Efficacy
Vertebral Non-vertebral Hip
HRT (CEE + MPA) + + +
Raloxifene + - -
50% RR
Bisphosphonates Etidronate + - -
50% RR
5% ARR
Alendronate, + + +
Risedronate, 25-50% RR 45-70% RR 20-25% RR
Zoledronate 1% ARR 5-7% RR 2% ARR
Calcitonin + - -
Denosumab + + +
60% RR 20% RR 40% RR
Teriparatide + + No power
65% RR 53% RR
You might also like
- Slide Materi Dr. Nelfi, SPKFR - Osteoporosis and Fracture Prevention - PMR4GP 2022Document32 pagesSlide Materi Dr. Nelfi, SPKFR - Osteoporosis and Fracture Prevention - PMR4GP 2022Maulia Wisda Era ChresiaNo ratings yet
- MronjDocument20 pagesMronjdr.herokarimiNo ratings yet
- Denosumab: An Emerging Therapy in Pediatric Bone Disorders: Pediatrics (L Ward and E Imel, Section Editors)Document10 pagesDenosumab: An Emerging Therapy in Pediatric Bone Disorders: Pediatrics (L Ward and E Imel, Section Editors)Dita Putri DamayantiNo ratings yet
- Drugs Used in OsteoporosisDocument30 pagesDrugs Used in Osteoporosissigit_riyantonoNo ratings yet
- Ar 413Document4 pagesAr 413Filip KoneskiNo ratings yet
- Clinical LecfinalsDocument7 pagesClinical LecfinalsCaryl Franchette SamsonNo ratings yet
- Strontium Renelate and Osteoporosis by Mohammed Zamir MirzaDocument19 pagesStrontium Renelate and Osteoporosis by Mohammed Zamir MirzaMohammed Zamir MirzaNo ratings yet
- Drugs Effecting On Osteoporosis: Abdullaev Dzhumadil, Pharmd International Medical UniversityDocument25 pagesDrugs Effecting On Osteoporosis: Abdullaev Dzhumadil, Pharmd International Medical UniversityRtxGaming Zone 73No ratings yet
- Osteoporosis Core DrugsDocument1 pageOsteoporosis Core DrugsRoxana Magaly Chavez PillacaNo ratings yet
- NCMB316 OsteoporosisDocument11 pagesNCMB316 Osteoporosis3-B-4 NAVIA, Kyle Bless V.No ratings yet
- Precision Medicine Targets Osteoblastic Smurf1 to Promote Bone FormationDocument90 pagesPrecision Medicine Targets Osteoblastic Smurf1 to Promote Bone FormationJosephChengNo ratings yet
- Bisphosphonate Drug HolidayDocument5 pagesBisphosphonate Drug HolidayARNo ratings yet
- Fosamax Differentiation Prolia Category Indication Contraindication Mechanism of ActionDocument1 pageFosamax Differentiation Prolia Category Indication Contraindication Mechanism of ActionjeevaNo ratings yet
- Tto de La Osteoporosis - 2020Document16 pagesTto de La Osteoporosis - 2020GilbertoNo ratings yet
- Capture The Fracture - Use of Bone Turnover MarkerDocument7 pagesCapture The Fracture - Use of Bone Turnover MarkergusdeNo ratings yet
- Pathophysiology-Pathomechanics Dan Penegakan Diagnosis OsteoporosisDocument90 pagesPathophysiology-Pathomechanics Dan Penegakan Diagnosis Osteoporosissingle_ladyNo ratings yet
- Drugs Used to Treat OsteoporosisDocument18 pagesDrugs Used to Treat OsteoporosisLana AmerieNo ratings yet
- Physiological Bases of Bone Regeneration II. The Remodeling ProcessDocument7 pagesPhysiological Bases of Bone Regeneration II. The Remodeling ProcessNelly Solange TamayoNo ratings yet
- Update On Bone Anabolics in Osteoporosis TreatmentDocument16 pagesUpdate On Bone Anabolics in Osteoporosis TreatmentSandra Janneth Perdomo LaraNo ratings yet
- Lecture 31 Osteoporosis Pathophys FlattenedDocument3 pagesLecture 31 Osteoporosis Pathophys FlattenedAhmed Mashaly100% (1)
- 2998-Article Text-8874-1-10-20190629Document3 pages2998-Article Text-8874-1-10-20190629Indra DhootNo ratings yet
- Bone HealingDocument2 pagesBone HealingGerardLum100% (2)
- Regulatory Pathways Revealing New Approaches2008Document14 pagesRegulatory Pathways Revealing New Approaches2008Cami GutierrezNo ratings yet
- Glucocorticoid-induced osteoporosis pathophysiology and therapyDocument10 pagesGlucocorticoid-induced osteoporosis pathophysiology and therapyMuhammad Isnaini ZuhriNo ratings yet
- Dr. Ilham OsteoporosisDocument39 pagesDr. Ilham OsteoporosisGhea Putri HendrianiNo ratings yet
- Role of Bone Forming Agents in The Management of OsteoporosisDocument17 pagesRole of Bone Forming Agents in The Management of OsteoporosisMuhammad Fadli IdhanNo ratings yet
- Skeletal Diseases in Cushing's Syndrome: Osteoporosis Versus ArthropathyDocument5 pagesSkeletal Diseases in Cushing's Syndrome: Osteoporosis Versus Arthropathykuro hanabusaNo ratings yet
- Physiologic and molecular bases of muscle hypertrophy and atrophyDocument8 pagesPhysiologic and molecular bases of muscle hypertrophy and atrophyJor ChavezNo ratings yet
- NYOMAN KERTIA: RHEUMATOLOGIST SHARES EXPERTISEDocument47 pagesNYOMAN KERTIA: RHEUMATOLOGIST SHARES EXPERTISEYane Aulia YasminNo ratings yet
- Determinants of Skeletal Fragility and Bone QualityDocument2 pagesDeterminants of Skeletal Fragility and Bone QualityPacifier NothingfaceNo ratings yet
- DrugsDocument32 pagesDrugshaidar ALhlaichiNo ratings yet
- DM Osseus HealingDocument9 pagesDM Osseus HealingdeespepeNo ratings yet
- Pros and Cons of Denosumab Treatment For Osteoporosis and Implication For RANKL Aptamer TherapyDocument9 pagesPros and Cons of Denosumab Treatment For Osteoporosis and Implication For RANKL Aptamer TherapyP.No ratings yet
- Presentation On Osteoporosis: Submitted To: Dr. Divya Vohra Submitted By: Sharique Raza M.pharm Jamia HamdardDocument38 pagesPresentation On Osteoporosis: Submitted To: Dr. Divya Vohra Submitted By: Sharique Raza M.pharm Jamia Hamdardsri susantiiNo ratings yet
- BP MecanismDocument14 pagesBP MecanismAdryana StefyNo ratings yet
- Review Treatment With Vitamin D3 And/or Vitamin K2Document4 pagesReview Treatment With Vitamin D3 And/or Vitamin K2fpm5948No ratings yet
- NSAIDs in Orthodontic Tooth Movement, 2012Document4 pagesNSAIDs in Orthodontic Tooth Movement, 2012Tarif HamshoNo ratings yet
- Healing of Tooth Extraction Socket: Dr. Pankaj Datta Dr. Shilpa Khullar Dr. Mittal ADocument3 pagesHealing of Tooth Extraction Socket: Dr. Pankaj Datta Dr. Shilpa Khullar Dr. Mittal AwatidinaNo ratings yet
- Sclerostin Antibodies in Osteoporosis: Latest Evidence and Therapeutic PotentialDocument8 pagesSclerostin Antibodies in Osteoporosis: Latest Evidence and Therapeutic PotentialSandra SuryariniNo ratings yet
- OsteoporosisDocument35 pagesOsteoporosisSanjeev MehtaNo ratings yet
- Ortho PresentationDocument27 pagesOrtho PresentationDr.abarna VenkatNo ratings yet
- Osteoporosis Medications Video, Anatomy & Definition OsmosisDocument1 pageOsteoporosis Medications Video, Anatomy & Definition OsmosisLorenaNo ratings yet
- Bone Turnover Markers To Monitor Oral Bisphosphonate TherapyDocument6 pagesBone Turnover Markers To Monitor Oral Bisphosphonate Therapyhossein kasiriNo ratings yet
- Osteoporosis and Bone DisordersDocument37 pagesOsteoporosis and Bone DisordersRuzica PavlovicNo ratings yet
- Bone Grafts and Their SubstitutesDocument4 pagesBone Grafts and Their SubstitutesIndriastuti SoetomoNo ratings yet
- Farmakologi Dan Toksikologi 2022Document25 pagesFarmakologi Dan Toksikologi 2022Ghost TsushimaNo ratings yet
- University of Miami Division or Oral and Maxillofacial Surgery Position Paper On Drug Induced Osteonecrosis of The Jaws 2014Document26 pagesUniversity of Miami Division or Oral and Maxillofacial Surgery Position Paper On Drug Induced Osteonecrosis of The Jaws 2014Deb SNo ratings yet
- BiphosphonatesDocument14 pagesBiphosphonatesadrianajg.drNo ratings yet
- Biologic and Biophysical Technologies. FINALDocument28 pagesBiologic and Biophysical Technologies. FINALRafael Miguel MallillinNo ratings yet
- Farmakologi Penyakit-Penyakit Degenerasi Tulang Dan SendiDocument19 pagesFarmakologi Penyakit-Penyakit Degenerasi Tulang Dan SendiCici MastaNo ratings yet
- Bone Remodeling - Basic Science - OrthobulletsDocument4 pagesBone Remodeling - Basic Science - OrthobulletsCindy Julia AmandaNo ratings yet
- CKC Articular Cartilage Repair Info PDFDocument12 pagesCKC Articular Cartilage Repair Info PDFMarcelo EsquisattoNo ratings yet
- Your Skeletal System : Why Is It So Importan T?Document29 pagesYour Skeletal System : Why Is It So Importan T?lavonne445No ratings yet
- Metabolic Bone DiseaseDocument6 pagesMetabolic Bone Diseasekartini ciatawiNo ratings yet
- Metabolismo OseoDocument28 pagesMetabolismo OseoBelez Jum JumNo ratings yet
- Pathophysiology of Bone MetastasesDocument5 pagesPathophysiology of Bone MetastasesdyahNo ratings yet
- Chronic Bone Pathologies - Draw It To Know ItDocument1 pageChronic Bone Pathologies - Draw It To Know ItDuy LuuNo ratings yet
- OsteoporosisDocument20 pagesOsteoporosisGledia LindaNo ratings yet
- Anatomical Reference Planes: Human Bone Growth and DevelopmentDocument12 pagesAnatomical Reference Planes: Human Bone Growth and Developmentapi-3825389No ratings yet
- Translational Endocrinology of Bone: Reproduction, Metabolism, and the Central Nervous SystemFrom EverandTranslational Endocrinology of Bone: Reproduction, Metabolism, and the Central Nervous SystemGerard KarsentyNo ratings yet
- Nine Simple Ways To Make It Easier To (Re) Use Your Data Vol 6 No 2 (2013) : Special Issue - Data Sharing in Ecology and EvolutionDocument10 pagesNine Simple Ways To Make It Easier To (Re) Use Your Data Vol 6 No 2 (2013) : Special Issue - Data Sharing in Ecology and EvolutionalbgomezNo ratings yet
- Lecture 28 Thyroid PathophysDocument2 pagesLecture 28 Thyroid PathophysAhmed MashalyNo ratings yet
- Lecture 29 30 Thyroid TherapeuticsDocument3 pagesLecture 29 30 Thyroid TherapeuticsAhmed MashalyNo ratings yet
- Lecture 31 Osteoporosis Pathophys FlattenedDocument3 pagesLecture 31 Osteoporosis Pathophys FlattenedAhmed Mashaly100% (1)
- Lecture 39 Nhps in DMDocument1 pageLecture 39 Nhps in DMAhmed MashalyNo ratings yet
- Ontario COVID-19 Vaccination ServiceDocument4 pagesOntario COVID-19 Vaccination ServiceAhmed MashalyNo ratings yet
- Legal Issues in Clinical ResearchDocument48 pagesLegal Issues in Clinical ResearchAhmed MashalyNo ratings yet
- 4 Joneckis, Chris-02-16-16Document62 pages4 Joneckis, Chris-02-16-16OstazNo ratings yet
- Lecture 33 Osteoporosis TherapeuticsDocument1 pageLecture 33 Osteoporosis TherapeuticsAhmed MashalyNo ratings yet
- Research EthicsDocument114 pagesResearch EthicsAhmed MashalyNo ratings yet
- Ethical Principles in Clinical ResearchDocument46 pagesEthical Principles in Clinical ResearchAhmed MashalyNo ratings yet
- An Overview of File Formats JsonDocument3 pagesAn Overview of File Formats JsonAhmed MashalyNo ratings yet
- Manual-2016 4Document257 pagesManual-2016 4Ahmed MashalyNo ratings yet
- Research EthicsDocument114 pagesResearch EthicsAhmed MashalyNo ratings yet
- Amber 14Document826 pagesAmber 14Ahmed MashalyNo ratings yet
- Journal of The Taiwan Institute of Chemical EngineersDocument13 pagesJournal of The Taiwan Institute of Chemical EngineersAhmed MashalyNo ratings yet
- Medical - Chemestry Q&ADocument13 pagesMedical - Chemestry Q&AAhmed MashalyNo ratings yet
- 1 Gallin, John-10-13-15-Handouts-Color-1Document29 pages1 Gallin, John-10-13-15-Handouts-Color-1OstazNo ratings yet
- Friedel CraftsDocument8 pagesFriedel CraftsAhmed MashalyNo ratings yet
- Implementation of Total Quality Management in HospitalsDocument6 pagesImplementation of Total Quality Management in HospitalsAhmed Mashaly100% (1)
- Integrated modeling system for structural biologyDocument10 pagesIntegrated modeling system for structural biologyAhmed MashalyNo ratings yet
- Medical - Chemestry Q&ADocument13 pagesMedical - Chemestry Q&AAhmed MashalyNo ratings yet
- General Information On Medical Certificates and List of Accredited Clinics of The Embassy of BelgiumDocument4 pagesGeneral Information On Medical Certificates and List of Accredited Clinics of The Embassy of BelgiumAhmed MashalyNo ratings yet
- Conversion of GradesDocument61 pagesConversion of GradesAhmed Mashaly0% (1)
- Student Cover LetterDocument1 pageStudent Cover LetterAhmed MashalyNo ratings yet
- Connexus SigcodesDocument8 pagesConnexus SigcodesAhmed Mashaly100% (1)
- Sample Letter To Consular Section, Us Embassy/Consulate Supporting Application For Visa (Or Renewal/Extension) by Foreign IndividualDocument1 pageSample Letter To Consular Section, Us Embassy/Consulate Supporting Application For Visa (Or Renewal/Extension) by Foreign IndividualZodin100% (3)
- Pharmaceutical Biotechnology: Master's Degree CourseDocument2 pagesPharmaceutical Biotechnology: Master's Degree CourseAhmed MashalyNo ratings yet
- Cardiac DysrhythmiaDocument1 pageCardiac DysrhythmiaAhmed MashalyNo ratings yet
- Lubricated Coupling TrainingDocument47 pagesLubricated Coupling TrainingTheerayootNo ratings yet
- Syllabus For ETABSDocument2 pagesSyllabus For ETABSSandgrouse RajNo ratings yet
- Getting Started With PhotoshopDocument15 pagesGetting Started With PhotoshopJEANIFER BUGARINNo ratings yet
- WME01 01 Que 20220510Document15 pagesWME01 01 Que 20220510muhammad awaisNo ratings yet
- Cissp NotesDocument83 pagesCissp NotesRobert Mota HawksNo ratings yet
- Report On MinesDocument7 pagesReport On MinesYhaneNo ratings yet
- Rousyan Faikar (21060111130111) LampiranDocument50 pagesRousyan Faikar (21060111130111) Lampiranrousyan faikarNo ratings yet
- Kolej Matrikulasi Pulau Pinang Kementerian Pelajaran Malaysia 13200 Kepala BatasDocument9 pagesKolej Matrikulasi Pulau Pinang Kementerian Pelajaran Malaysia 13200 Kepala Bataskelisa157100% (2)
- Dynamic Programming Algorithm Explained in ECE 551 LectureDocument11 pagesDynamic Programming Algorithm Explained in ECE 551 Lectureadambose1990No ratings yet
- 1025 (1029) Anaerobic ChamberDocument8 pages1025 (1029) Anaerobic ChamberSoma GhoshNo ratings yet
- Bindura University of Science Education March - August 2015 Admissions PDFDocument12 pagesBindura University of Science Education March - August 2015 Admissions PDFLuke MadzikotoNo ratings yet
- Assessment of Fiber Optic Pressure Sensors: NUREG/CR-6312Document133 pagesAssessment of Fiber Optic Pressure Sensors: NUREG/CR-6312abhrajitsahaNo ratings yet
- Full Download Test Bank For Positive Psychology 4th Edition Lopez PDF Full ChapterDocument36 pagesFull Download Test Bank For Positive Psychology 4th Edition Lopez PDF Full Chaptershaps.tortillayf3th100% (21)
- Moral and Non Moral StandardsDocument6 pagesMoral and Non Moral StandardsGerry AbuanNo ratings yet
- Panjab University, Chandigarh: (Theory Examinations) TIME OF EXAMINATION: 9.30 A.M. To 12.30 P.MDocument3 pagesPanjab University, Chandigarh: (Theory Examinations) TIME OF EXAMINATION: 9.30 A.M. To 12.30 P.MManav ChhabraNo ratings yet
- Nato Military Policy On Public AffairsDocument21 pagesNato Military Policy On Public AffairsiX i0No ratings yet
- Eng. XI, U18 Meaning Into WordsDocument4 pagesEng. XI, U18 Meaning Into Wordssanad BhattaraiNo ratings yet
- Bahan Belajar Ujian Akhir SekolahDocument13 pagesBahan Belajar Ujian Akhir SekolahArga AnggaraNo ratings yet
- Spread footing design calculationDocument6 pagesSpread footing design calculationFrancklinMeunierM'ondoNo ratings yet
- CPO Science Foundations of Physics: Unit 7, Chapter 24Document47 pagesCPO Science Foundations of Physics: Unit 7, Chapter 24dheerajbhagwatNo ratings yet
- Unit 4 FSQCDocument28 pagesUnit 4 FSQCvaralakshmi KNo ratings yet
- Crescent Moon InstructionsDocument7 pagesCrescent Moon InstructionsSARANo ratings yet
- How To Avoid PlagiarismDocument2 pagesHow To Avoid PlagiarismShiny Deva PriyaNo ratings yet
- BA Mckesson Interview 2Document3 pagesBA Mckesson Interview 2Vikram hostNo ratings yet
- UNI National Education Advances EnglishDocument6 pagesUNI National Education Advances EnglishJose BancesNo ratings yet
- Hdpe Guide PDFDocument81 pagesHdpe Guide PDFbalotNo ratings yet
- Build Pulse Oximeter InstructionsDocument3 pagesBuild Pulse Oximeter InstructionsPrabhuDevNo ratings yet
- Env203Geo205 Map - ElementsDocument14 pagesEnv203Geo205 Map - ElementsFarhana SuptiNo ratings yet
- Acros Organics Acta N°006Document20 pagesAcros Organics Acta N°006Atomer FormationNo ratings yet
- Jurnal SinusitisDocument49 pagesJurnal SinusitisAramanda Dian100% (1)