Professional Documents
Culture Documents
Apoyo A Diada - Guia para SLP
Uploaded by
Paula Belén Rojas CunazzaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Apoyo A Diada - Guia para SLP
Uploaded by
Paula Belén Rojas CunazzaCopyright:
Available Formats
Perspectives of the ASHA Special Interest Groups
SIG 13, Vol. 3(Part 1), 2018, Copyright © 2018 American Speech-Language-Hearing Association
Assisting the Breastfeeding Dyad: A Guide for
Speech-Language Pathologists
Jamie Mahurin-Smith
Illinois State University Communication Sciences & Disorders
Normal, IL
Catherine Watson Genna
Private Practice
Woodhaven, NY
Disclosures
Financial: Jamie Mahurin-Smith has no relevant financial interests to disclose. Catherine Watson
Genna has written two books on related topics and maintains a private practice as a lactation
consultant.
Nonfinancial: Jamie Mahurin-Smith has no relevant nonfinancial interests to disclose. Catherine
Watson Genna has no relevant nonfinancial interests to disclose.
Speech-language pathologists (SLPs) who work with pediatric feeding/swallowing
disorders may evaluate and treat breastfeeding infants. Many SLPs, however, receive
little breastfeeding-related training either as students or as practicing clinicians. The
purpose of this article was to provide effective strategies for SLPs working with families
whose eventual goal is direct breastfeeding.
More than 80% of U.S. mothers plan to breastfeed. The provision of competent support
to breastfeeding dyads is a key element in improving public health outcomes and reducing health
care costs (Bartick et al., 2017; see Table 1 for additional details), because care providers who
lack formal training in breastfeeding support tend to fall back on personal experiences, clinical
intuition, and extrapolation from bottle-feeding (cf. Radzyminski & Callister, 2015). Although the
speech-language pathologist’s (SLP’s) scope of practice includes assessment and treatment of
pediatric feeding problems, breastfeeding knowledge is not a direct focus of the SLP training
process (Council on Academic Accreditation, 2017). The limited research available on practicing
SLPs’ breastfeeding knowledge indicates that their proficiency in this domain is variable (Blake,
2014; Fishbein, Flock, & Benton, 2013).
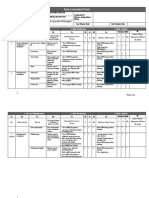
Table 1. Human milk is associated with favorable differences in outcomes related to health and
neurodevelopment for both infants and mothers.
Child outcomes
Autism (Schultz et al., 2006)
Bed-wetting (Barone et al., 2006)
Celiac disease
Cognition (Kramer et al., 2008)
Gastrointestinal illness
Language development (Dee et al., 2007; Gibson-Davis et al., 2006; Oddy et al., 2010)
Leukemia
(continued)
47
Downloaded From: https://perspectives.pubs.asha.org/ by a University College London User on 07/11/2018
Terms of Use: https://pubs.asha.org/ss/rights_and_permissions.aspx
Lymphoma
Markers for cardiac risk (Parikh et al., 2009)
Mitigation of the impact of prematurity (Isaacs et al., 2010; Quigley et al., 2012; Vohr et al., 2007)
Necrotizing enterocolitis (Quigley et al., 2014)
Neurological dysfunction (Lanting et al., 1994)
Otitis media
Respiratory infections
Schizophrenia (Sørensen et al., 2005)
Speech processing (Ferguson et al., 2007)
Specific language impairment (Tomblin et al., 1997)
Stuttering (Mahurin-Smith et al., 2013)
Sudden infant death syndrome
Urinary tract infections
Variegated babbling (Vestergaard et al., 1999)
Maternal outcomes
Breast cancer
Ovarian cancer
Type 2 diabetes
Note. Unless noted otherwise, pediatric outcomes are drawn from Eidelman et al. (2012). Maternal
outcomes are drawn from Chowdhury et al. (2015).
How Can SLPs Assist Breastfeeding Dyads Effectively?
A Framework for Clinical Practice
SLPs who work with infants may have observed a troublesome downward spiral in their
patients: The baby is gaining weight poorly, and the pediatrician and family are concerned. The
mother may be worried about her milk supply. The baby may seem fussy and unsettled at the
breast, and it is difficult even for an experienced clinician to estimate milk transfer by observing a
breastfeeding session. These combined influences can thwart the most highly motivated mother’s
plans to breastfeed. The intended message of this article, however, is that most breastfeeding
problems are solvable. A mother may not be able to breastfeed directly until her baby has grown
and matured; a mother may not be able to breastfeed exclusively. However, generally, a mother
who wants to breastfeed can find a way to give her milk to her baby and provide at least some
direct breastfeeding, given support at home and skilled clinical assistance.
Lactation consultants (LCs) often recommend a three-step plan for providing breastfeeding
support in complex situations: (a) feed the baby, (b) protect the milk supply, and (c) keep something
happening at the breast.
Feed the Baby
Healthy full-term infants are expected to double their birth weight in the first 6 months
of life and to triple it, roughly, by their first birthdays (see Jung & Czajka-Narins, 1985). Even
in optimal circumstances, this is a substantial undertaking. SLPs typically work with infants
48
Downloaded From: https://perspectives.pubs.asha.org/ by a University College London User on 07/11/2018
Terms of Use: https://pubs.asha.org/ss/rights_and_permissions.aspx
in less-than-optimal circumstances: premature babies who may not be able to sequence suck–
swallow–breathe consistently, fragile babies who fatigue easily, and babies with neurological
complications that prevent them from transferring milk effectively. In many cases, direct and/or
exclusive breastfeeding may be impossible in the short term. An LC’s first step is always to ensure
that the baby is receiving adequate nutrition.
Identifying the need for supplementation comes first. Some parents may express reluctance
regarding recommendations that babies be supplemented, out of well-founded concern that early
supplementation can make it more difficult to establish exclusive breastfeeding (Chantry, Dewey,
Peerson, Wagner, & Nommsen-Rivers, 2014). Except in rare cases such as classical galactosemia, a
condition in which babies are unable to metabolize galactose, mothers interested in breastfeeding
should be encouraged to express milk for their babies (World Health Organization, 2003). Parents’
input into the method of supplementation should be valued as well. Some parents may prefer
the use of a syringe, a finger feeder, or a cup to the use of a bottle, and providers are advised to
accommodate those preferences when possible (see Genna, 2009, for further details on these
tools, and Genna, 2017, for additional information on supplementation strategies and decision
making; readers are reminded that syringe feeding in particular may present safety concerns for
babies with compromised swallowing abilities). Some SLPs may be unfamiliar with the idea of
at-breast supplementation, in which a baby who is able to latch on receives supplementation
at the same time via tube (see Figures 1 and 2). At-breast supplementation increases a baby’s
motivation to breastfeed and typically increases the amount of milk the infant transfers from the
breast (Genna, 2009), whereas frequent bottle-feeding reduces breastfeeding (Collins et al., 2004;
Howard et al., 2003; Renfrew et al., 2009).
Figure 1. At-breast supplementation.
49
Downloaded From: https://perspectives.pubs.asha.org/ by a University College London User on 07/11/2018
Terms of Use: https://pubs.asha.org/ss/rights_and_permissions.aspx
Figure 2. At-breast supplementation.
Protect the Milk Supply
Supplementation may be necessary for babies who struggle with breastfeeding. However,
for families whose long-term goal is direct and exclusive breastfeeding, the establishment of
a milk supply tailored to the baby’s needs is critical. Although lactational physiology is not a
part of the typical SLP graduate curriculum, some knowledge of lactation is important for SLPs
who provide feeding assessment and intervention to infants. For more details, see Riordan and
Wambach (2016). To summarize, women begin producing milk during pregnancy in a process called
lactogenesis I (mammary differentiation). This first milk, colostrum, is known for being rich in
immunologically active constituents. Of particular interest to SLPs, it is also thicker in consistency
and smaller in volume than the milk that will arrive a few days after birth, thus providing a
perfect transitional food for a newborn baby who is unaccustomed to coordinating swallowing
and breathing. Sometime between Days 2 and 4, the second stage of milk production, called
lactogenesis II (secretory activation), begins. This is known colloquially as the period when a
woman’s milk “comes in” and refers to the onset of copious milk production. Many women, although
not all, notice changes in the size and firmness of their breasts during lactogenesis II. Babies with
impaired feeding skills may struggle to adapt to the changes in milk viscosity, volume, and flow
rate at this time. Across a window of approximately 2 weeks, a woman’s milk becomes less thick
and less yellow, gradually becoming the bluish-white fluid that will be produced until weaning.
Although the appearance of the milk will stay the same, the hormonal mechanisms governing
its production will shift. Milk supply during lactogenesis II is assisted by high baseline prolactin.
Immediate skin-to-skin contact between mother and baby leads to the baby finding and attaching
to the breast in the first hour or two after birth (Widstrom et al., 2011), beginning the calibration
of milk production (Bystrova et al., 2007). Frequent feedings (12 or more a day) over the next few
days help develop copious milk (Bystrova et al., 2007), whereas maternal–infant separation delays
lactogenesis II (Nommsen-Rivers, Chantry, Peerson, Cohen, & Dewey, 2010). Once milk production
is well established, rate of milk synthesis is controlled locally in the breast by chemical and
mechanical (pressure) feedback. This phase of milk production is called galactopoiesis.
From this brief review, two pieces of information are particularly critical for SLPs: First,
calibration for future milk production happens early. In the early hours and weeks of breastfeeding,
a mother is determining how much milk she will be able to produce when her baby is 6 months
old. When a baby is born unable to breastfeed directly, it is imperative that the mother be provided
with good information about milk production and expression strategies. Although nursing staff
and LCs will generally be the ones sharing this information with mothers, it is important for hospital-
50
Downloaded From: https://perspectives.pubs.asha.org/ by a University College London User on 07/11/2018
Terms of Use: https://pubs.asha.org/ss/rights_and_permissions.aspx
based SLPs to be aware of the existence of this sensitive window. It is also valuable for them to
provide support and encouragement and to seek out accurate answers to parents’ questions about
pumping schedules and the uniqueness of human milk. The second piece of critical information
regards babies who are directly breastfeeding, but not efficiently. When babies are not taking in
enough calories at the breast, they are effectively telling their mothers to make less food for them
than they actually need.
Some mothers make too much milk for their babies. This situation, although frustrating, is
comparatively straightforward to manage (see Smillie, Campbell, & Iwinski, 2005; van Veldhuizen-
Staas, 2007). More mothers, especially those whose infants are not feeding well, are concerned
about having an inadequate milk supply. This concern may be unwarranted: Some well-fed babies
prefer frequent feedings, and some well-fed babies are fussy despite the adequacy of their mothers’
milk supply. Perceived or actual insufficient milk is a major factor in early weaning (Li, Fein, Chen,
& Grummer-Strawn, 2008). Mismanagement of early breastfeeding, especially when there is
mother–baby separation or when a baby cannot nurse efficiently, is a major factor in milk supply
problems (Neifert, 2001); interventions that disrupt breastfeeding can have a serious negative
effect on milk supply. Conversely, supporting early breastfeeding attempts can improve infant
competence (Mizuno & Ueda, 2001; Nyqvist, 2008, 2013).
When a baby cannot breastfeed directly, it is important to protect the mother’s future
milk supply by establishing a manual expression and pumping regimen as soon as possible after
the baby’s birth. Mothers should be taught to hand-express milk within an hour of birth (Parker,
Sullivan, Krueger, Kelechi, & Mueller, 2011) and should begin using a rental-grade double-electric
pump in addition to hand expression at least eight times a day (Hill, Aldag, & Chatterton, 2001).
Two pieces of information may prove especially useful for SLPs. First, many mothers are unaware
that a rental-grade pump is better suited to bring in a full milk supply than the double-electric
pumps available for purchase in retail outlets. A woman who has already purchased a pump may
be reluctant to rent another one, but retail pumps are designed for employed mothers whose babies
are able to breastfeed directly. Second, mothers may not know that retail pumps have smaller
motors that are warrantied for 1 year and are not sturdy enough to share. Sharing open-system
pumps such as the popular Medela Pump In Style is also unhygienic (U.S. Food and Drug
Administration, 2013); a user’s milk enters the pump itself and may foster the growth of pathogens
within the pump housing. This is not a concern with pumps designed for multiple users.
One of the most frequent complaints about pumping is the time it requires. Although
pumping is unavoidably a time commitment, there are alternative strategies to make it more
manageable. When a mother is pumping for a medically fragile newborn, careful infection control
practices are critical. Some mothers, however, have babies who are medically stable but unable
to breastfeed directly. An example of such a case in which an SLP might be involved could be a
mother whose baby has a cleft palate or a hypertonic baby who clenches his or her jaw during
direct breastfeeding. Power pumping takes advantage of human milk’s remarkable ability to retard
microbial growth (Lawrence, 1999). Instead of pumping for 20–30 min every 3–4 hr, a power-pumping
mother finds a place to leave her pump set up. Across that 3- to 4-hr window, she pumps in small
bursts: 3 min at one time and 5 min at another, as frequently as possible. This approach can be
immensely valuable for mothers with older children in addition to their infants, because they may
find it easier to sit for several brief pumping sessions than one 20-min session. Power pumping is
especially helpful for increasing milk production (Riordan & Wambach, 2016). Collaborating with an
international board-certified lactation consultant (IBCLC) can yield additional strategies.
Whatever approaches providers may recommend to make pumping easier for mothers,
the reality is that pumping can be burdensome. It combines the challenges of breastfeeding
(a substantial time commitment that is the mother’s sole responsibility, a need for attention to
the impact of medications/alcohol use on her baby’s food supply) with the challenges of bottle-
feeding (the need to plan outings so that an appropriate amount of milk is kept at an appropriate
temperature, the imperative to clean equipment daily), with the result that frequent pumping
51
Downloaded From: https://perspectives.pubs.asha.org/ by a University College London User on 07/11/2018
Terms of Use: https://pubs.asha.org/ss/rights_and_permissions.aspx
is not a preferred long-term solution for many mothers. For mothers who want to breastfeed
directly, the third step of the plan is critical.
Keep Something Happening at the Breast
A mother’s preference for direct breastfeeding over pumping and bottle-feeding may be
challenging for an SLP with little breastfeeding-related training. The following sections offer
strategies to facilitate this transition.
Adapt What You Know. Some of the strategies that SLPs use with bottle-feeding babies
can be modified to meet the needs of breastfeeding babies. A prime example is modified positioning
during feeding. Prone positioning can be an extraordinarily useful strategy for breastfeeding
babies who are struggling to latch on well and transfer milk effectively. Whereas published
materials on breastfeeding may still list only the cradle, football, and cross-cradle holds, current LC
practice emphasizes stable, ergonomic, gravity-assisted positions that activate the baby’s breast-
finding and attaching behaviors. A frequently recommended version of this approach is called
“laid-back breastfeeding” (Colson, 2010; Glover & Wiessinger, 2013), illustrated in Figure 3. This
name is intended to refer simultaneously to the mother’s positioning, in a semireclined posture
with the baby prone on her body for the feeding, and to the more relaxed attitude it often engenders
in a dyad that may have shown signs of feeding-related distress in previous breastfeeding sessions.
Figure 3. Semiprone positioning.
Another example of an easily adapted strategy is buccal support. Many babies on SLPs’
caseloads have some degree of hypotonia and may benefit from manual support of the cheeks
during feeding (Hwang, Lin, Coster, Bigsby, & Vergara, 2010). This strategy can be especially
effective for assisting preterm babies who do not have the well-developed sucking pads typically
seen in full-term infants. A breastfeeding mother can use the dancer hand position to provide
simultaneous support to her breast and the baby’s jaw and cheeks (see Figure 4; Walker, 2008).
Use of this strategy may require attention to resulting increases in flow rate, as discussed further
in the following paragraph.
52
Downloaded From: https://perspectives.pubs.asha.org/ by a University College London User on 07/11/2018
Terms of Use: https://pubs.asha.org/ss/rights_and_permissions.aspx
Figure 4. Cheek support.
A third example of a strategy that can be adapted is adjustment of the flow rate (see Wolf
& Glass, 2017), which may need to be either faster or slower. Problem solving for SLPs working
with breastfeeding dyads will often involve assessment of optimal flow rate. For many infants,
semiprone or prone positioning with mild head extension improves their ability to coordinate
swallowing and breathing. Mothers can press on the breast to block some ducts to slow milk flow
if the baby is struggling. For infants who are easily overwhelmed, mothers can express some milk
to slow milk flow; milk flows more slowly from a less full breast. Short, frequent feedings will also
reduce fatigue, which can in turn reduce the risk of aspiration for some babies. It is also possible
to increase the rate of milk flow so that feedings are more efficient, an approach that is especially
helpful for a baby who tires easily but who has good suck–swallow–breathe sequencing. Mothers
can be taught to use breast compression to assist milk transfer (Morton et al., 2009), thus
facilitating more efficient breastfeeding sessions. Selected at-breast supplementers can also be
used to provide an achievable challenge, gradually increasing the pressure needed to remove milk
from the device until it matches that needed to transfer milk from the breast. Further information
can be found on Catherine Watson Genna’s website (n.d.).
Begin With the End in Mind: Work Toward the Family’s Goals. If a mother’s priority
is direct breastfeeding, optimal SLP intervention strategies will support her in reaching that goal.
If mothers who had hoped to breastfeed participate in interventions that focus on bottle-feeding,
53
Downloaded From: https://perspectives.pubs.asha.org/ by a University College London User on 07/11/2018
Terms of Use: https://pubs.asha.org/ss/rights_and_permissions.aspx
they may wind up with bottle-feeding babies. Babies who are struggling at the breast do not learn
how to breastfeed by practicing a different set of skills with a bottle. Whenever it is an option,
SLPs can collaborate with IBCLCs to help families meet their breastfeeding goals, frequently
as the members of a collaborative team with unique knowledge of swallowing physiology. In a
neonatal intensive care unit, for instance, an SLP might prepare a baby by providing suck training
to encourage tongue cupping along with oral/facial stimulation (Fucile, Gisel, & Lau, 2005;
Harding, Law, & Pring, 2006; Howe & Wang, 2013; Lima, Cortes, Bouzada, & Friche, 2015). She
or he might then assist with positioning while the LC monitors the baby’s latch and assesses
milk transfer. Both of the authors have benefited from the email list Lactnet (LISTSERVE, n.d.) is
an international forum in which many different health care providers discuss complex breastfeeding
problems as well as potential solutions.
Conclusion
This article has emphasized the importance of providing competent assistance to mothers
who wish to breastfeed. Premature weaning has significant costs, in terms of both health care
dollars and avoidable suffering (Eidelman et al., 2012); it is not unusual for mothers to describe
intense feelings about breastfeeding, for many years after their children have left infancy behind
(Promislow, Gladen, & Sandler, 2005). When mothers need help to breastfeed their babies, skilled
SLPs can make a critical difference.
References
Barone, J. G., Ramasamy, R., Farkas, A., Lerner, E., Creenan, E., Salmon, D., . . . Schneider, D. (2006).
Breastfeeding during infancy may protect against bed-wetting during childhood. Pediatrics, 118(1), 254–259.
Bartick, M. C., Schwarz, E. B., Green, B. D., Jegier, B. J., Reinhold, A. G., Colaizy, T. T., . . . Stuebe, A. M.
(2017). Suboptimal breastfeeding in the United States: Maternal and pediatric health outcomes and costs.
Maternal & Child Nutrition, 13(1), e12366.
Blake, A. N. (2014). Breastfeeding knowledge and clinical management among speech-language pathologists
(Master’s thesis). Retrieved from ProQuest Dissertations and Theses database (UMI No. 1557076).
Bystrova, K., Widstrom, A. M., Matthiesen, A. S., Ransjö-Arvidson, A. B., Welles-Nyström, B., Vorontsov, I.,
& Uvnäs-Moberg, K. (2007). Early lactation performance in primiparous and multiparous women in relation
to different maternity home practices. A randomised trial in St. Petersburg. International Breastfeeding
Journal, 2, 9.
Catherine Watson Genna. (n.d.). Helping mom work “Smarter, not harder”. Retrieved from http://www.
cwgenna.com/smartnothard.html
Chantry, C. J., Dewey, K. G., Peerson, J. M., Wagner, E. A., & Nommsen-Rivers, L. A. (2014). In-hospital
formula use increases early breastfeeding cessation among first-time mothers intending to exclusively
breastfeed. The Journal of Pediatrics, 164(6), 1339–1345.
Chowdhury, R., Sinha, B., Sankar, M. J., Taneja, S., Bhandari, N., Rollins, N., . . . Martines, J. (2015).
Breastfeeding and maternal health outcomes: A systematic review and meta-analysis. Acta Paediatrica,
104(S467), 96–113.
Collins, C. T., Ryan, P., Crowther, C. A., McPhee, A. J., Paterson, S., & Hiller, J. E. (2004). Effects of bottles,
cups, and dummies on breast feeding in preterm infants: A randomized controlled trial. British Medical
Journal, 329, 193–198.
Colson, S. (2010). What happens to breastfeeding when mothers lie back. Clinical Lactation, 1, 9–12.
Council on Academic Accreditation. (2017). Standards for accreditation of graduate education programs
in audiology and speech-language pathology. Retrieved from https://caa.asha.org/wp-content/uploads/
Accreditation-Standards-for-Graduate-Programs.pdf
Dee, D. L., Li, R., Lee, L., & Grummer-Strawn, L. M. (2007). Associations between breastfeeding practices
and young children’s language and motor development. Pediatrics, 119(Suppl. 1), S92–S98.
Eidelman, A. I., Schanler, R. J., Johnston, M., Landers, S., Noble, L., Szucs, K., & Viehmann, L. (2012).
Breastfeeding and the use of human milk. Pediatrics, 129(3), e827–e841.
54
Downloaded From: https://perspectives.pubs.asha.org/ by a University College London User on 07/11/2018
Terms of Use: https://pubs.asha.org/ss/rights_and_permissions.aspx
Ferguson, M., & Molfese, P. J. (2007). Breast-fed infants process speech differently from bottle-fed infants:
Evidence from neuroelectrophysiology. Developmental Neuropsychology, 31, 337–347.
Fishbein, M., Flock, S., & Benton, K. (2013). Self-assessment of pediatric feeding therapists in the state of
Illinois. SIG 13 Perspectives on Swallowing and Swallowing Disorders (Dysphagia), 22(4), 129–141.
Fucile, S., Gisel, E. G., & Lau, C. (2005). Effect of an oral stimulation program on sucking skill maturation
of preterm infants. Developmental Medicine & Child Neurology, 47(3), 158–162.
Genna, C. W. (2009). Selecting and using breastfeeding tools: Improving care and outcomes. Amarillo, TX:
Hale Publishing.
Genna, C. W. (2017). Supporting sucking skills in breastfeeding infants. Burlington, MA: Jones & Bartlett.
Gibson-Davis, C. M., & Brooks-Gunn, J. (2006). Breastfeeding and verbal ability of 3-year-olds in a multicity
sample. Pediatrics, 118, 1444–1451.
Glover, R., & Wiessinger, D. (2013). They can do it, you can help: Building breastfeeding skill and confidence
in mother and helper. In C. W. Genna (Ed.), Supporting sucking skills in breastfeeding infants (pp. 105–148).
Burlington, MA: Jones & Bartlett.
Harding, C. M., Law, J., & Pring, T. (2006). The use of non-nutritive sucking to promote functional sucking
skills in premature infants: An exploratory trial. Infant, 2(6), 238–243.
Hill, P. D., Aldag, J. C., & Chatterton, R. T. (2001). Initiation and frequency of pumping and milk production
in mothers of non-nursing preterm infants. Journal of Human Lactation, 17(1), 9–13.
Howard, C. R., Howard, F. M., Lanphear, B., Eberly, S., deBlieck, E. A., Oakes, D., & Lawrence, R. A. (2003).
Randomized clinical trial of pacifier use and bottle-feeding or cupfeeding and their effect on breastfeeding.
Pediatrics, 111, 511–518.
Howe, T.-H., & Wang, T.-N. (2013). Systematic review of interventions used in or relevant to occupational
therapy for children with feeding difficulties ages birth-5 years. American Journal of Occupational Therapy,
67, 405–412.
Hwang, Y. S., Lin, C. H., Coster, W. J., Bigsby, R., & Vergara, E. (2010). Effectiveness of cheek and jaw
support to improve feeding performance of preterm infants. American Journal of Occupational Therapy,
64(6), 886–894.
Isaacs, E. B., Fischl, B. R., Quinn, B. T., Chong, W. K., Gadian, D. G., & Lucas, A. (2010). Impact of breast
milk on intelligence quotient, brain size, and white matter development. Pediatric Research, 67, 357–362.
Jung, E., & Czajka-Narins, D. M. (1985). Birth weight doubling and tripling times: An updated look at the
effects of birth weight, sex, race and type of feeding. American Journal of Clinical Nutrition, 42, 182–189.
Kramer, M. A., Aboud, F., Mironova, E., Vanilovich, I., Platt, R. W., Matush, L., . . . Shapiro, S. (2008).
Breastfeeding and child cognitive development: New evidence from a large randomized trial. Archives of
General Psychiatry, 65, 578–584.
Lanting, C. I., Huisman, M., Boersma, E. R., Touwen, B. C. L., & Fidler, V. (1994). Neurological differences
between 9-year-old children fed breast-milk or formula-milk as babies. Lancet, 344, 1319–1322.
Lawrence, R. A. (1999). Storage of human milk and the influence of procedures on immunological components
of human milk. Acta Paediatrica, 88(S430), 14–18.
Li, R., Fein, S. B., Chen, J., & Grummer-Strawn, L. M. (2008). Why mothers stop breastfeeding: Mothers’
self-reported reasons for stopping during the first year. Pediatrics, 122(Suppl. 2), S69–S76.
Lima, A. H., Cortes, M. G., Bouzada, M. C. F., & Friche, A. A. (2015). Preterm newborn readiness for oral
feeding: Systematic review and meta-analysis. CoDAS, 27, 101–107.
LISTSERVE 16.0. (n.d.). LACTNET. Retrieved from http://community.lsoft.com/scripts/wa-LSOFTDONATIONS.
exe?INDEX
Mahurin-Smith, J., & Ambrose, N. G. (2013). Breastfeeding may protect against persistent stuttering.
Journal of Communication Disorders, 46, 351–360.
Mizuno, K., & Ueda, A. (2001). Development of sucking behavior in infants who have not been fed for
2 months after birth. Pediatrics International, 43, 251–255.
Morton, J., Hall, J. Y., Wong, R. J., Thairu, L., Benitz, W. E., & Rhine, W. D. (2009). Combining hand
techniques with electric pumping increases milk production in mothers of preterm infants. Journal of
Perinatology, 29(11), 757–764.
55
Downloaded From: https://perspectives.pubs.asha.org/ by a University College London User on 07/11/2018
Terms of Use: https://pubs.asha.org/ss/rights_and_permissions.aspx
Neifert, M. R. (2001). Prevention of breastfeeding tragedies. Pediatric Clinics of North America, 48, 273–297.
Nommsen-Rivers, L. A., Chantry, C. J., Peerson, J. M., Cohen, R. J., & Dewey, K. G. (2010). Delayed onset
of lactogenesis among first-time mothers is related to maternal obesity and factors associated with ineffective
breastfeeding. American Journal of Clinical Nutrition, 92, 574–584.
Nyqvist, K. H. (2008). Early attainment of breastfeeding competence in very preterm infants. Acta Paediatrica,
97, 776–781.
Nyqvist, K. H. (2013). Lack of knowledge persists about early breastfeeding competence in preterm infants.
Journal of Human Lactation, 29, 296–299.
Oddy, W. H., Kendall, G. E., Li, J., Jacoby, P., Robinson, M., deKlerk, N. H., . . . Stanley, F. J. (2010). The
long-term effects of breastfeeding on child and adolescent mental health: A pregnancy cohort study followed
for 14 years. Journal of Pediatrics, 156, 568–574.
Parikh, N. I., Hwang, S.-J., Ingelsson, E., Benjamin, E. J., Fox, C. S., Vasan, R. S., & Murabito, J. M.
(2009). Breastfeeding in infancy and cardiovascular disease risk factors. American Journal of Medicine,
122, 656–663.e1.
Parker, L. A., Sullivan, S., Krueger, C., Kelechi, T., & Mueller, M. (2011). Effect of early breast milk expression
on milk volume and timing of lactogenesis stage II among mothers of very low birth weight infants: A pilot
study. Journal of Perinatology, 32(3), 205–209.
Promislow, J. H., Gladen, B. C., & Sandler, D. P. (2005). Maternal recall of breastfeeding duration by elderly
women. American Journal of Epidemiology, 161, 289–296.
Quigley, M. A., Henderson, G., Anthony, M. Y., & McGuire, W. (2014). Formula versus donor breast milk for
feeding preterm or low birth weight infants. Cochrane Database of Systematic Reviews, 2014(4), CD002971.
https://doi.org/10.1002/14651858.CD002971.pub
Quigley, M. A., Hockley, C., Carson, C., Kelly, Y., Renfrew, M. J., & Sacker, A. (2012). Breastfeeding is
associated with improved child cognitive development: A population-based cohort study. Journal of Pediatrics,
160, 25–32.
Radzyminski, S., & Callister, L. C. (2015). Health professionals’ attitudes and beliefs about breastfeeding.
The Journal of Perinatal Education, 24(2), 102–109.
Renfrew, M. J., Dyson, L., McCormick, F., Misso, K., Stenhouse, E., King, S. E., & Williams, A. F. (2009).
Breastfeeding promotion for infants in neonatal units: A systematic review. Child: Care, Health and
Development, 36, 165–178.
Riordan, J., & Wambach, K. (2016). Breastfeeding and human lactation (4th ed.). Burlington, MA: Jones & Bartlett.
Schultz, S. T., Klonoff-Cohen, H. S., Wingard, D. L., Akshoomoff, N. A., Macera, C. A., Ji, M., & Bacher, C.
(2006). Breastfeeding, infant formula supplementation, and autistic disorder: The results of a parent survey.
International Breastfeeding Journal, 1, 16.
Smillie, C. M., Campbell, S. H., & Iwinski, S. (2005). Hyperlactation: How left-brained rules for breastfeeding
can wreak havoc with a natural process. Newborn and Infant Nursing Reviews, 5, 49–58.
Sørensen, H. J., Mortensen, E. L., Reinisch, J. M., & Mednick, S. A. (2005). Breastfeeding and risk of
schizophrenia in the Copenhagen perinatal cohort. Acta Psychiatrica Scandinavica, 112(1), 26–29.
Tomblin, J. B., Smith, E., & Zhang, X. (1997). Epidemiology of specific language impairment: Prenatal and
perinatal risk factors. Journal of Communication Disorders, 30(4), 325–344.
U.S. Food and Drug Administration. (2013). Buying and renting a breast pump. Retrieved from http://www.
fda.gov/MedicalDevices/ProductsandMedicalProcedures/HomeHealthandConsumer/ConsumerProducts/
BreastPumps/ucm061952.htm
van Veldhuizen-Staas, C. G. (2007). Overabundant milk supply: An alternative way to intervene by full
drainage and block feeding. International Breastfeeding Journal, 2(1), 11.
Vestergaard, M., Obel, C., Henriksen, T. B., Sørensen, H. T., Skajaa, E., & Ostergaard, J. (1999). Duration
of breastfeeding and developmental milestones during the latter half of infancy. Acta Paediatrica, 88(12),
1327–1332.
Vohr, B. R., Poindexter, B. B., Dusick, A. M., McKinley, L. T., Higgins, R. D., Langer, J. C., & Poole, W. K.
(2007). Persistent beneficial effects of breast milk ingested in the neonatal intensive care unit on outcomes
of extremely low birth weight infants at 30 months of age. Pediatrics, 120, e953–e959.
56
Downloaded From: https://perspectives.pubs.asha.org/ by a University College London User on 07/11/2018
Terms of Use: https://pubs.asha.org/ss/rights_and_permissions.aspx
Walker, M. (2008). Breastfeeding the late preterm infant, Journal of Obstetric, Gynecologic, and Neonatal
Nursing, 37, 692–701.
Widstrom, A. M., Lilja, G., Aaltomaa-Michalias, P., Dahllof, A., Lintula, M., & Nissen, E. (2011). Newborn
behaviour to locate the breast when skin-to-skin: A possible method for enabling early self-regulation.
Acta Paediatrica, 100, 79–85.
Wolf, L., & Glass, R. (2017). The Goldilocks problem: Milk flow that is not too fast, not too slow, but just
right, or why milk flow matters and what to do about it. In C. W. Genna (Ed.), Supporting sucking skills in
breastfeeding infants. Burlington, MA: Jones & Bartlett.
World Health Organization. (2003). Global strategy for infant and young child feeding. Geneva, Switzerland:
Author.
History:
Received November 09, 2017
Revised January 19, 2018
Accepted January 23, 2018
https://doi.org/10.1044/persp3.SIG13.47
57
Downloaded From: https://perspectives.pubs.asha.org/ by a University College London User on 07/11/2018
Terms of Use: https://pubs.asha.org/ss/rights_and_permissions.aspx
You might also like
- Assessing The Breastfeeding Dyad - A Guide For Speech-Language PathologistsDocument5 pagesAssessing The Breastfeeding Dyad - A Guide For Speech-Language PathologistsPaloma LópezNo ratings yet
- Encouraging Breastfeeding: The Role of Fathers: AbstractDocument11 pagesEncouraging Breastfeeding: The Role of Fathers: AbstractUthuriel27No ratings yet
- Nursing Research PaperDocument14 pagesNursing Research Paperapi-735739064No ratings yet
- Down Syndrome and Feeding ProblemsDocument8 pagesDown Syndrome and Feeding Problemsfelix08121992No ratings yet
- Thesis On Exclusive BreastfeedingDocument5 pagesThesis On Exclusive Breastfeedingebonybatesshreveport100% (2)
- A Literature Review of The Factors That in Uence Breastfeeding: An Application of The Health Belief ModelDocument10 pagesA Literature Review of The Factors That in Uence Breastfeeding: An Application of The Health Belief ModelJanzell Anne Borja AlbaniaNo ratings yet
- Breastfeeding Uncovering Barriers and Offering SolutionsDocument6 pagesBreastfeeding Uncovering Barriers and Offering SolutionsSuéllen EmidioNo ratings yet
- Research ReportDocument8 pagesResearch ReportAbid SherazNo ratings yet
- Exclusivebreastfeeding 181003124754Document39 pagesExclusivebreastfeeding 181003124754apalanavedNo ratings yet
- Tuthill, E., & McGrath, J. (2013) - The Importance of Breastfeeding Education For All Women of Childbearing AgeDocument2 pagesTuthill, E., & McGrath, J. (2013) - The Importance of Breastfeeding Education For All Women of Childbearing AgesebastixmasterNo ratings yet
- Mothers'Breastfeedng ExperiencesDocument11 pagesMothers'Breastfeedng ExperiencesDivina D Galvez-BeronioNo ratings yet
- Thesis BreastfeedingDocument5 pagesThesis BreastfeedingSteven Wallach100% (2)
- Knowledge Attitude and Practice of ExcluDocument16 pagesKnowledge Attitude and Practice of ExclupblesynnNo ratings yet
- Cruz Final Grant ProposalDocument40 pagesCruz Final Grant Proposalapi-341233003No ratings yet
- Exclusive Breast-Feeding Is MotivationDocument8 pagesExclusive Breast-Feeding Is MotivationsmokaNo ratings yet
- Breast Feeding Literature ReviewDocument5 pagesBreast Feeding Literature Reviewgatewivojez3No ratings yet
- Research Paper Topics On BreastfeedingDocument5 pagesResearch Paper Topics On Breastfeedingafnhemzabfueaa100% (1)
- Lits 1016 2Document13 pagesLits 1016 2satraNo ratings yet
- Breastfeeding Is An Unsurpassed Method of Providing Ideal Food For The Healthy Growth and Development of InfantsDocument4 pagesBreastfeeding Is An Unsurpassed Method of Providing Ideal Food For The Healthy Growth and Development of InfantsSatra SabbuhNo ratings yet
- Exclusive Breastfeeding and Risk of Dental Malocclusion: ObjectivesDocument10 pagesExclusive Breastfeeding and Risk of Dental Malocclusion: ObjectivesingridspulerNo ratings yet
- Zainab ProjectDocument35 pagesZainab ProjectOpeyemi JamalNo ratings yet
- Jurnal 2 PDFDocument17 pagesJurnal 2 PDFyayu yuliantiNo ratings yet
- Perceptions and Practices Regarding Breastfeeding Among Postnatal Women at A District Tertiary Referral Government Hospital in Southern IndiaDocument7 pagesPerceptions and Practices Regarding Breastfeeding Among Postnatal Women at A District Tertiary Referral Government Hospital in Southern IndiaJamby VivasNo ratings yet
- Nursing Group Research PaperDocument16 pagesNursing Group Research Paperapi-368267454No ratings yet
- Research Paper On Exclusive BreastfeedingDocument8 pagesResearch Paper On Exclusive Breastfeedingmadywedykul2100% (1)
- Breastfeeding Benefits Research PaperDocument8 pagesBreastfeeding Benefits Research Paperafnhdcebalreda100% (1)
- Research Paper On Exclusive Breastfeeding PDFDocument8 pagesResearch Paper On Exclusive Breastfeeding PDFegtwfsaf100% (1)
- Nresearch PaperDocument13 pagesNresearch Paperapi-399638162No ratings yet
- Breastfeeding Thesis PDFDocument6 pagesBreastfeeding Thesis PDFMonica Franklin100% (1)
- Nresearch PaperDocument14 pagesNresearch Paperapi-400982160No ratings yet
- Notes On Exclusive BreastfeedingDocument6 pagesNotes On Exclusive BreastfeedingNdem BasseyNo ratings yet
- Nutrients 15 00988Document17 pagesNutrients 15 00988VIRGINA PUTRINo ratings yet
- Examples of Breastfeeding DissertationDocument5 pagesExamples of Breastfeeding DissertationWriteMyPaperForMeIn3HoursCanada100% (1)
- Wooo 4Document7 pagesWooo 4Essie MohammedNo ratings yet
- Dissertation On Exclusive BreastfeedingDocument6 pagesDissertation On Exclusive BreastfeedingPaperWritingServicesCanada100% (1)
- Thesis On BreastfeedingDocument4 pagesThesis On Breastfeedingppxohvhkd100% (2)
- Literature Review On Breast FeedingDocument8 pagesLiterature Review On Breast Feedingcpifhhwgf100% (1)
- Qualitatif Mothers' Experience of Not Breastfeeding in A Breastfeeding CultureDocument12 pagesQualitatif Mothers' Experience of Not Breastfeeding in A Breastfeeding CultureRiani WidiaNo ratings yet
- HLTH 634 Literature ReviewDocument9 pagesHLTH 634 Literature Reviewapi-282532235No ratings yet
- Thesis On Breastfeeding PracticesDocument4 pagesThesis On Breastfeeding Practicestmexyhikd100% (2)
- Thesis Statement Breastfeeding in PublicDocument5 pagesThesis Statement Breastfeeding in Publicafkntwbla100% (2)
- Breastfeeding GuidelinesDocument15 pagesBreastfeeding GuidelinesDr Atef Hadedy100% (2)
- Breastfeeding Thesis PaperDocument4 pagesBreastfeeding Thesis PaperBestCustomPaperWritingServiceCanada100% (2)
- Nutrients: Breastfeeding Di Breastfeeding CessationDocument10 pagesNutrients: Breastfeeding Di Breastfeeding CessationEliyyasa Vina ErikmetikaNo ratings yet
- Qi ProjectDocument8 pagesQi Projectapi-542442476No ratings yet
- Amir2016 Article SelectedAbstractsFromTheBreastDocument16 pagesAmir2016 Article SelectedAbstractsFromTheBreastLinda Puji astutikNo ratings yet
- Adpied Paper From EmailDocument17 pagesAdpied Paper From Emailapi-401213596No ratings yet
- FactorsthatinfluencemotherstobreastfeedDocument18 pagesFactorsthatinfluencemotherstobreastfeedapi-353823437No ratings yet
- 9B. Effectiveness of Educational Intervention On Breastfeeding Among Primi Pregnant WomanDocument6 pages9B. Effectiveness of Educational Intervention On Breastfeeding Among Primi Pregnant Womanagaua16No ratings yet
- Who MpasiDocument38 pagesWho MpasiNita AriantiNo ratings yet
- Factors Associated With Cessation of Exclusive Breastfeeding at 1 and 2 Months Postpartum in TaiwanDocument7 pagesFactors Associated With Cessation of Exclusive Breastfeeding at 1 and 2 Months Postpartum in TaiwanHilda HildaNo ratings yet
- G NudDocument17 pagesG NudBabangida AbubakarNo ratings yet
- Breastfeeding discomforts and management by primigravida mothersDocument19 pagesBreastfeeding discomforts and management by primigravida mothersNazria Gilman Kapusan75% (4)
- Lancet 2023 BreastfeedingDocument14 pagesLancet 2023 BreastfeedingKeneniNo ratings yet
- Factors Associated With Cessation of Exclusive Breastfeeding at 1 and 2 Months Postpartum in TaiwanDocument7 pagesFactors Associated With Cessation of Exclusive Breastfeeding at 1 and 2 Months Postpartum in TaiwanHilda HildaNo ratings yet
- Maternal Child Nutrition - 2016 - P Rez Escamilla - Impact of The Baby Friendly Hospital Initiative On Breastfeeding andDocument16 pagesMaternal Child Nutrition - 2016 - P Rez Escamilla - Impact of The Baby Friendly Hospital Initiative On Breastfeeding andNur FauziyahNo ratings yet
- Building Future Health and Well-Being of Thriving Toddlers and Young Children: 95th Nestlé Nutrition Institute Workshop, September 2020From EverandBuilding Future Health and Well-Being of Thriving Toddlers and Young Children: 95th Nestlé Nutrition Institute Workshop, September 2020No ratings yet
- Infant and Young Child FeedingDocument111 pagesInfant and Young Child Feedingerkalem100% (1)
- Enabling Women To Breastfeed Through Better Policies and ProgrammesDocument4 pagesEnabling Women To Breastfeed Through Better Policies and ProgrammesIrsani BerlianaNo ratings yet
- Rol de Guia Parental de TransiciónDocument10 pagesRol de Guia Parental de TransiciónPaula Belén Rojas CunazzaNo ratings yet
- Transicion A La LMDocument10 pagesTransicion A La LMPaula Belén Rojas CunazzaNo ratings yet
- A Guide To Finger-Feeding: Information For Parents and CarersDocument8 pagesA Guide To Finger-Feeding: Information For Parents and CarersPaula Belén Rojas CunazzaNo ratings yet
- Guidelines For Gastrostomy Tube Feeding For Infants With Neuromuscular DiseaseDocument1 pageGuidelines For Gastrostomy Tube Feeding For Infants With Neuromuscular DiseasePaula Belén Rojas CunazzaNo ratings yet
- Manual Interventions For Musculoskeletal Factors in Infants With Suboptimal Breastfeeding: A Scoping ReviewDocument12 pagesManual Interventions For Musculoskeletal Factors in Infants With Suboptimal Breastfeeding: A Scoping ReviewPaula Belén Rojas CunazzaNo ratings yet
- Figs Cancer PatientsDocument4 pagesFigs Cancer PatientsPaula Belén Rojas CunazzaNo ratings yet
- Milieu Communication Training For Late TalkersDocument7 pagesMilieu Communication Training For Late TalkersPaula Belén Rojas CunazzaNo ratings yet
- CRD en Pctes EPOCDocument7 pagesCRD en Pctes EPOCPaula Belén Rojas CunazzaNo ratings yet
- Cerebral Palsy JurnalDocument17 pagesCerebral Palsy JurnaltrieNo ratings yet
- Speech Pathology Australia Guidance For Service PDFDocument14 pagesSpeech Pathology Australia Guidance For Service PDFAngelica GarciaNo ratings yet
- Pds Magnetoencephalography MegDocument2 pagesPds Magnetoencephalography MegPaula Belén Rojas CunazzaNo ratings yet
- Manual Interventions For Musculoskeletal Factors in Infants With Suboptimal Breastfeeding: A Scoping ReviewDocument12 pagesManual Interventions For Musculoskeletal Factors in Infants With Suboptimal Breastfeeding: A Scoping ReviewPaula Belén Rojas CunazzaNo ratings yet
- Recommendations in Rehab With OlderssDocument21 pagesRecommendations in Rehab With OlderssPaula Belén Rojas CunazzaNo ratings yet
- Psychopharmacology Drugs For Disorders - Edited.editedDocument4 pagesPsychopharmacology Drugs For Disorders - Edited.editedMORRIS ANUNDANo ratings yet
- Maternal Child NursingDocument31 pagesMaternal Child Nursingmatrixtrinity88% (24)
- BSC (N) Iii Year Child Health Nursing: Unit Vi - Management of Behavioural and Social Problems in ChildrenDocument79 pagesBSC (N) Iii Year Child Health Nursing: Unit Vi - Management of Behavioural and Social Problems in ChildrenERIC ANGEL100% (1)
- Proposal Presentation Nairobi - Respicius Shumbusho DamianDocument13 pagesProposal Presentation Nairobi - Respicius Shumbusho DamianShumbusho ConsultingtzNo ratings yet
- TelemedicineDocument11 pagesTelemedicineSakshi AsthanaNo ratings yet
- Index2010 BJOTDocument6 pagesIndex2010 BJOTTO Joss AguilarNo ratings yet
- Symbiosis PGDHHM Project TitlesDocument3 pagesSymbiosis PGDHHM Project TitlesBen JosephNo ratings yet
- NCP-Deficient Fluid VolumeDocument1 pageNCP-Deficient Fluid Volumejanmichael8No ratings yet
- Practice Enteral and Parenteral CalculationsDocument2 pagesPractice Enteral and Parenteral CalculationsRavenNo ratings yet
- Lim Meng Heck (SR - Operation Manager) : ISK Ssessment ORMDocument2 pagesLim Meng Heck (SR - Operation Manager) : ISK Ssessment ORMVaradaraju ThirunavukkarasanNo ratings yet
- Research Proposal On Fast FoodDocument8 pagesResearch Proposal On Fast FoodManish Ravat100% (5)
- Chapter-14-Pathogenesis-of-Infectious-DiseasesDocument18 pagesChapter-14-Pathogenesis-of-Infectious-DiseasesedemcantosumjiNo ratings yet
- Prenatal Development and Birth: The Developing Person Through The Life Span Kathleen Stassen Berger - Tenth EditionDocument42 pagesPrenatal Development and Birth: The Developing Person Through The Life Span Kathleen Stassen Berger - Tenth EditionJoel PayneNo ratings yet
- Resume For KidDocument5 pagesResume For Kidnjoqvnjbf100% (2)
- Books by Robie H. HarrisDocument2 pagesBooks by Robie H. HarrisCandlewick PressNo ratings yet
- Safety Data Sheet Conbextra Gp2: Revision Date: 01/01/2020 Revision: 0ADocument8 pagesSafety Data Sheet Conbextra Gp2: Revision Date: 01/01/2020 Revision: 0AAnonymous kRIjqBLkNo ratings yet
- Case 1-2 Business Case Data Chaos Creates RiskDocument5 pagesCase 1-2 Business Case Data Chaos Creates RiskfauziahezzyNo ratings yet
- Actual Nursing DiagnosisDocument4 pagesActual Nursing DiagnosisJp CasperNo ratings yet
- Career Day Brochure FinalDocument2 pagesCareer Day Brochure Finalapi-375229945No ratings yet
- Running Head: WORKSHEET 18 1Document3 pagesRunning Head: WORKSHEET 18 1Mashaal Fasih100% (1)
- The Future of Positive Psychology: A Declaration of IndependenceDocument17 pagesThe Future of Positive Psychology: A Declaration of IndependenceEbonnie DiazNo ratings yet
- Implementasi SPM Kesehatan Bayi Baru Lahir di Puskesmas DukuhsetiDocument10 pagesImplementasi SPM Kesehatan Bayi Baru Lahir di Puskesmas DukuhsetiFidia sariNo ratings yet
- RPT F2 Science DLP 2018Document19 pagesRPT F2 Science DLP 2018Mei Shan SiowNo ratings yet
- 【课件】自然游戏治疗01场Document67 pages【课件】自然游戏治疗01场xjawyh0208No ratings yet
- Mental Health Weekly - May 16, 2016Document8 pagesMental Health Weekly - May 16, 2016Sharon A StockerNo ratings yet
- Learning ObjectivesDocument6 pagesLearning Objectivesangot123No ratings yet
- Nurses Sourcing Letter InternationalDocument2 pagesNurses Sourcing Letter InternationalAldrin SantosNo ratings yet
- Coping With Stress in Middle and Late AdolescenceDocument58 pagesCoping With Stress in Middle and Late AdolescenceKanor DalisayNo ratings yet
- Fitness Testing Guide PDFDocument10 pagesFitness Testing Guide PDFdodovadaNo ratings yet
- My Courses: Home UGRD-PHYED6101-2113T Week 2: Health-Related Fitness Components Prelim Quiz 1Document4 pagesMy Courses: Home UGRD-PHYED6101-2113T Week 2: Health-Related Fitness Components Prelim Quiz 1Miguel Angelo GarciaNo ratings yet