Professional Documents
Culture Documents
Nonvasive Blood Gas Sensing With Electrodes: 0961/c07/frame Page 173 Tuesday, August 21, 2001 6:34 AM
Uploaded by
Rolando EsquivelOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nonvasive Blood Gas Sensing With Electrodes: 0961/c07/frame Page 173 Tuesday, August 21, 2001 6:34 AM
Uploaded by
Rolando EsquivelCopyright:
Available Formats
0961/C07/frame Page 173 Tuesday, August 21, 2001 6:34 AM
Nonvasive Blood Gas
7 Sensing with Electrodes
7.1 INTRODUCTION
The metabolism of all living cells in the body requires oxygen and an energy
substrate, generally glucose. As the result of oxidative metabolism, heat and CO2
are produced as well as regulated molecular byproducts, and O2 in the blood is
consumed. The lungs are the organ in which the external atmosphere interfaces with
the body’s blood supply; O2 is taken in and CO2 is exhaled. The partial pressure of
oxygen (pO2) in an alveolus is typically 104 mmHg. Venous blood entering a
capillary in the alveous wall has a pO2 of c. 40 mmHg. Thus, an initial pressure
gradient of 104 − 40 = 64 mmHg causes O2 gas to diffuse into the capillary, combine
with hemoglobin in red blood cells (RBCs) and be dissolved in the water in the
blood. The blood exiting the capillary contains c. 104 mmHg pO2. All the oxygenated
alveolar blood mixes with venous blood from the non-oxygenating tissues of the
lungs, bringing the pO2 down to about 95 mmHg. This is the pO2 of arterial blood
pumped to the body from the left ventricle.
In the peripheral systemic capillaries, oxygen diffuses into the interstitial fluid,
which has a pO2 of c. 40 mmHg. Thus, venous blood returned to the heart and lungs
has a pO2 of c. 40 mmHg. The average pO2 in the systemic capillaries is about 70
mmHg (blood enters with a pO2 of 95 and exits with 40 mmHg).
Normally, about 97% of the O2 carried in arterial blood is combined with
hemoglobin molecules inside red blood cells (erythrocytes), and the remainder of
the O2 is dissolved in the plasma. In terms of partial pressures, 92.2 mmHg is carried
as oxyhemoglobin (HbO), and 2.8 mmHg O2 is carried dissolved in arterial blood.
The venous blood sent to the lungs under resting (basal metabolic) conditions has
about 75% HbO, and a pO2 of 40 mmHg. Under conditions of intense exercise, the
venous HbO can drop to as low as 19% saturation; the interstitial fluid (and venous)
pO2 drops to c. 15 mmHg (Guyton, 1991, Ch. 40).
Any disease or condition that interferes with the normal exchange of gases in
the alveoli, the transport of O2 to the systemic capillaries, the return of CO2 to the
lungs, and the exchange of O2 and CO2 in the systemic micro-circulation will give
rise to life-threatening hypoxia or acidosis. Section 7.2 describes noninvasive chem-
ical means of monitoring pO2 in the body. (Note also that Section 15.8 covers pulse
oximetry, a noninvasive optical technique of measuring the percent O2 saturation
(sO2) of hemoglobin in the peripheral circulation.)
Also considered in this chapter is the NI transcutaneous measurement of pCO2
in the peripheral blood, tcpCO2. High blood tcpCO2 is a sign of metabolic acidosis,
which can have several causes, including damaged alveoli in the lungs. (Damaged
173
© 2002 by CRC Press LLC
0961/C07/frame Page 174 Tuesday, August 21, 2001 6:34 AM
174 Noninvasive Instrumentation and Measurement in Medical Diagnosis
alveoli will also give low tcpO2 readings.) Normal blood pH is c. 7.4. If the pH
decreases for any reason, the rate of breathing increases automatically to exhale CO2
at a greater rate, and the kidneys also compensate for elevated acidity in the extra-
cellular fluid by actively excreting hydrogen ions at an increased rate. Thus, another
cause of high pCO2 can be kidney failure, in which the tubular epithelial cells actively
transport H+ ions from their interiors into the collecting tubes for excretion in urine
at a reduced rate. Low blood flow to the kidneys or damaged tubular cells can
decrease this normal mechanism for blood pH regulation. High pCO2 can occur
normally in exercise, but it drops in minutes due to increased breathing effort and
H+ elimination by the kidneys. Acidosis can also result from gluconeogenesis in
diabetes mellitus. Here, low intracellular glucose concentration causes liver cells to
break down fatty acids to acetoacetic acid and acetyl-Co-A. Acetyl-Co-A is used as
an energy source, and acetoacetic acid enters the blood, causing the pH to fall.
Although CO2 is not involved directly, the lower pH causes the ratio of pCO2 to
[HCO3− ] to increase. Loss of intestinal bicarbonate in severe diarrhea can also cause
acidosis, and an elevated pCO2 to [HCO3− ] ratio (Guyton, 1991, Ch. 30).
7.2 TRANSCUTANEOUS O2 SENSING
7.2.1 INTRODUCTION: THE CLARK ELECTRODE
Several methods, given direct contact with a blood sample, can accurately measure
the pO2 of blood. For a description of these invasive instrumental means, see Webster
(1992). In this text, however, we are devoted to examining noninvasive medical
instruments, and there is presently only one effective means of transcutaneously
measuring peripheral tissue blood pO2. This system is based on the electrochemical
Clark electrode, first described in 1956 (Hahn, 1998).
The basic Clark electrode can measure pO2 in gases or liquids. It is an electro-
chemical, polarographic system in which a fixed potential is maintained across the
electrodes through which a dc current flows that is proportional to the concentration
of the rate-limiting reagent, O2, which participates in oxidation/reduction reactions
that take place at the electrode surfaces (oxidation takes place at the anode; reduction
occurs at the cathode). A plastic membrane porous to O2 separates the sample
compartment from the reaction compartment (around the electrodes). The reaction
compartment is filled with an aqueous buffer solution (at about pH 7), containing
chloride ions (which can be from KCl). The O2 that reacts at the electrode surfaces
must diffuse in through the membrane from the sample compartment. Figure 7.1
illustrates a cross section through the basic Clark cell. The anode (+ electrode) is a
AgCl-coated Ag ring or “washer;” the cathode (− electrode) is the small exposed
tip (12 to 25 µm diameter) of an insulated platinum wire. The membrane is typically
25 µm polyethelene or polypropylene. The chemical reactions that occur at the Pt
cathode are reductions (Hahn, 1998):
O 2 + H 2 O + 2e − → HO 2− + OH − 7.1
© 2002 by CRC Press LLC
0961/C07/frame Page 175 Tuesday, August 21, 2001 6:34 AM
Nonvasive Blood Gas Sensing with Electrodes 175
Ib Rb
R2 Rc
VR
R1
(0 V)
(Virtual gnd.)
Vo
Voltage - 0.7 V
reference
OA OA
I O2 + I b I O2 + I b
Clark electrode
Plastic
O-ring
⇑
AgCl anode pO 2 Polypropylene membrane
Pt cathode Buffered electrolyte
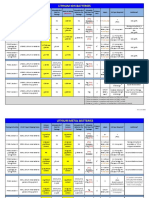
FIGURE 7.1 Cross-section and support electronics for a Clark polarographic O2 sensor. The
left-hand op amp and reference source supply the 0.7 V bias voltage for the cell. The right-
hand op amp serves as a current-to-voltage converter. Rb sets dc current Ib to cancel out the
zero-oxygen current of the Clark cell.
HO 2− + H 2 O + 2e − → 3OH − 7.2
HO 2− catalytic
→ 1 2 O 2 + OH −
decomposition
7.3
or, as a net reaction:
O 2 + 2 H 2 O + 4e − direct
→ 4OH − 7.4
© 2002 by CRC Press LLC
0961/C07/frame Page 176 Tuesday, August 21, 2001 6:34 AM
176 Noninvasive Instrumentation and Measurement in Medical Diagnosis
The OH− ions are buffered to maintain neutral pH, and the chloride ions carry charge
to the AgCl anode. Four electrons flow for every diatomic oxygen molecule reacted;
thus, the Clark cell current at a given temperature is given by:
IC = Ib + KC pO2 7.5
By U.S. convention, in metal wires, current flows in the opposite direction to
electrons. The Clark cell is generally operated at a fixed potential of 0.7 volts; its
current is linearly proportional to the pO2 in the measurement compartment. A small
dc background current, Ib, flows at pO2 = 0, which is due to ion drift in the electric
field between the electrodes. The current vs. pO2 graph taken with Vcell = 0.70 V
and pH 6.8 is essentially linear, enabling a two-point calibration of a Clark O2
electrode (at pO2 = 0 and pO2 = 160 mmHg (atmospheric)). The left op amp in
Figure 7.1 acts as a 0.7 V voltage source; the right op amp is a low-dc drift FET-
input type with very low IB that is used as a current-to-voltage converter (transim-
pedance). Its output, after subtracting the background current, Ib, is Vo = KC pO2.
The normal tempco of a Clark cell is 2% per degree Celsius, and the linearity is
better than 1% over the physiological pO2 range (Hahn, 1998).
The response time of a Clark cell to a step change in measured pO2 is largely
governed by the thickness of the membrane, but also depends on O2 and ion diffusion
times in the electrolyte. Typical Clark cell response time (time to reach half the
steady-state value) is on the order of tens of seconds. For a theoretical treatment of
Clark cell response dynamics, see Hahn (1998). Because of the low-pass character-
istic of the Clark cell’s response, it responds to a smoothed, or time-averaged pO2.
7.2.2 THE TRANSCUTANEOUS TCPO2 SENSOR
The transcutaneous tcpO2 sensor uses a Clark cell that is internally heated and
temperature regulated to operate at a temperature of 40˚ to 45˚ C, ± 0.1˚ when on
the skin. The elevated temperature of the Clark cell membrane is necessary to cause
vasodilation and reddening of the skin under the sensor. A thin layer of an isotonic
aqueous contact gel is placed between the skin and the heated sensor’s membrane
to facilitate outward diffusion of O2 from the skin through the membrane. The sensor
has built-in thermistors to monitor the Clark cell’s electrolyte temperature and the
skin temperature under the membrane. The thermistor outputs are used to control
the power supplied to a heater coil surrounding the cell.
Initially, transcutaneous operation of the heated Clark cell was found to be
effective in babies and small children because of their thinner skin. Unfortunately,
because of the delicate skin of infants, prolonged application of a heated sensor can
cause second-degree (blister) burns, unless the sensor is moved every hour or so.
There is a time × temperature product that must be observed to avoid skin damage.
The heated Clark sensor must be given a two-point calibration at its chosen operating
temperature before use.
Heated transcutaneous pO2 sensor systems (the TCM instrument series), made
by Radiometer Copenhagen, are sold worldwide. They are used for such applications
© 2002 by CRC Press LLC
0961/C07/frame Page 177 Tuesday, August 21, 2001 6:34 AM
Nonvasive Blood Gas Sensing with Electrodes 177
as monitoring neonatal pO2 to sense apnea, respiratory distress, etc. They are now
also used in adults for applications in hyperbaric medicine, vascular surgery, wound
care, and in reconstructive plastic surgery to monitor angiogenesis.
7.3 TRANSCUTANEOUS CO2 SENSING
7.3.1 INTRODUCTION: THE STOW-SEVERINGHAUS ELECTRODE
The basis for transcutaneous pCO2 sensing is the Stow-Severinghaus (S-S) electrode,
developed in 1957–1958 (Hahn, 1998). At the heart, literally, of an S-S electrode is
the glass pH electrode half cell, as shown in Figure 7.2. The half-cell EMF of the
glass pH electrode is really two half-cell potentials in series: an EMF is developed
across the special tip glass envelope that is proportional to the pH, and the EMF of
the internal, AgCl coupling electrode immersed in the 0.1 N HCl internal filling
solution. In general,
E GL = E GL
0
+ (2.3026 RT F ) [ pH] 7.6
Where pH is defined as − log10(aH+) ≅ − log10([H+]), R is the gas constant = 8.3147
joule/(mole ˚K), T is the Kelvin temperature, F is the Faraday number = 96,496,
and 2.3026 comes from converting natural logs to log10. At 25˚ C, (2.3026 RT/F) =
0.059156 V.
Interestingly, the pH of the 5 to 20 mM bicarbonate solution surrounding the
glass pH electrode is proportional to the negative logarithm of the partial pressure
of the CO2 in the external solution over the range of 10 to 90 mmHg (Webster, 1992,
Ch. 10]. First, CO2 must diffuse from the external test solution into the bicarbonate
solution through the Teflon membrane, where the following equilibria occur:
CO2 + H2O ⇐⇒ H2CO3 ⇐⇒ H+ + HCO3− 7.7A
HCO3− ⇐⇒ H+ + CO3− 7.7B
NaHCO3 ⇐⇒ Na+ + HCO3− 7.7C
Adding the equations, we find:
xs Solid Constant
CO 2 + H 2 O + NaHCO 3 ⇐⇒ 2 H + + CO 3= + HCO 3− + N a + 7.8
Note that the constant, a, relating the equivalent concentration of CO2 gas dissolved
in blood to the partial pressure is found from:
a=
[CO ]
2
7.9
pCO 2
© 2002 by CRC Press LLC
0961/C07/frame Page 178 Tuesday, August 21, 2001 6:34 AM
178 Noninvasive Instrumentation and Measurement in Medical Diagnosis
+
Vo
Cap
Fill hole
AgAgCl electrodes
Glass pH electrode
Solution of sodium
bicarbonate and NaCl
0.1 N HCl
pH-sensitive glass
O-ring
CO2
20µm Teflon membrane
FIGURE 7.2 A Stow-Severinghaus electrode to sense pCO2. A glass pH electrode responds
to the pH of the inner solution, which is shown to be a function of log10 (pCO2) in Equation
7.14.
a for blood is c. 0.03 (mmol/liter)/mmHg pCO2. At chemical equilibrium we have:
{ } [ ] [CO ][HCO ][Na ]
K a( pCO 2 ) = H +
2 =
3
−
3
+
7.10
K is the equilibrium constant for reaction 7.8. Also, from Equation 7.7B at equilib-
rium:
K′ =
[H ][CO ] → [CO ] = K ′ [HCO ] [H ]
+ =
3 = − +
7.11
[HCO ]−
3
3 3
© 2002 by CRC Press LLC
0961/C07/frame Page 179 Tuesday, August 21, 2001 6:34 AM
Nonvasive Blood Gas Sensing with Electrodes 179
Substituting Equation 7.11 into Equation 7.10, we can write:
[ ][
Ka( pCO 2 ) = H + HCO 3− ] [Na ] K ′
2 +
7.12
Taking the logarithm10 of terms in Equation 7.12, and noting that pH is defined by
pH ≡ −log10[H+],
[ ] [
log(Ka ) + log( pCO 2 ) = − pH + 2 log CO 3= + log Na + + log(K ′)] 7.13
or
[
pH = − log( pCO 2 ) − log(Ka K ′) + 2 log HCO 3− + log Na +] [ ] 7.14
which is of the form
pH = − log(pCO2) + A 7.15
because Ka/K′, [HCO3− ] and [Na+] are constant. Thus a Stow-Severinghaus pCO2
meter computes the pCO2 by exponentiating (pH − A), sic:
pCO2 = B10(−k(pH − A)) 7.16
The constants B and k are for display scaling.
Because the pH electrode and the chemical dissociation reactions involved are
all temperature sensitive, any application of the Stow-Severinghaus pCO2 sensor in
vivo, in vitro (with blood), or transcutaneously requires precise temperature regula-
tion to maintain calibration.
7.3.2 TRANSCUTANEOUS TCPCO2 SENSING
The tcpCO2 sensor can be combined with a tcpO2 sensor in the same housing. Such
units are described by Hahn (1998) and Webster (1992) and Radiometer Copenhagen
offers their model TCM™/3, combined tcpCO2 and tcpO2 monitor. The combined
sensor can use the same 0.1 N bicarbonate buffer used in the Stow-Severinghaus pCO2
sensor with the addition of NaCl for the Clark cell electrolyte. Figure 7.3 illustrates
the author’s version of a combined tcpO2 + tcpCO2 sensor. Note that it uses a common
electrolyte and membrane. The entire cell is heated and thermostatically regulated (not
shown in figure). The elevated (c. 44˚ C) temperature causes vasodilation under the
sensor and increases upward diffusion of O2 and CO2 through the stratum corneum
of the skin to the sensor’s membrane. The electrometer amplifier used to amplify the
pH electrode voltage has an ultra-low bias current (in 10s of fA), and super-high input
resistance (c. 1014 Ω). Thus, its bias current will be c. 10−14 A, which is negligible
compared with the 10−8 A Clark cell current. OA-2 thus can serve as a virtual ground
© 2002 by CRC Press LLC
0961/C07/frame Page 180 Tuesday, August 21, 2001 6:34 AM
180 Noninvasive Instrumentation and Measurement in Medical Diagnosis
Electrometer
amplifier
VCO2
VR
- 0.7 V
(Virtual
OA1 ground)
(0 V)
VO2
(Voltage source) OA2
IO2 + Ib IO2 + Ib
(Current to
voltage converter)
0.1N HCl Glass pH electrode
O-ring
Electrolyte
Membrane Pt cathode
AgCl anode (O2)
and ref. (CO2)
FIGURE 7.3 A proposed combined pO2 and pCO2 electrode. OA2 outputs a voltage propor-
tional to pO2, and the electrometer amplifier outputs a voltage VCO2 ∝ −log10 (pCO2) + A.
for both the Clark cell and the Severinghaus electrode; its voltage output depends only
on the Clark cell current.
7.4 SUMMARY
There are several reliable chemical gas sensors that work well when immersed in
blood, in vitro or in vivo, but only two, as we have seen above, have been adapted
to reliable approved nonvasive percutaneous operation.
A wide variety of other sensors work well to sense pO2 and pCO2 in the gas
phase. O2 has been sensed by using the fact that it is weakly paramagnetic, i.e., O2
gas molecules are attracted by a magnetic field, and thus can be separated from N2,
Ar and CO2 in air. Oxygen’s magnetic susceptibility is the basis for several com-
mercial gaseous oxygen meters: The thermomagnetic O2 “bridge,” the Hartmann &
Braun Magnos 7G, the differential pressure “bridge,” the Siemens Oxymat 5M, the
Datex OM-101 differential pressure fast-response O2 sensor, and the Servomex 1111
© 2002 by CRC Press LLC
0961/C07/frame Page 181 Tuesday, August 21, 2001 6:34 AM
Nonvasive Blood Gas Sensing with Electrodes 181
Faraday balance type O2 sensor (Moseley et al., 1991). O2 also can be the rate-
limiting reactant in a fuel cell so output voltage is proportional to pO2, or in a
polarographic chemical reaction (e.g., the Clark cell). The speed of sound in O2 at
a given pressure and temperature is different from other gases, and this property has
been used to sense the pO2 in air (Hong and Northrop, 1991). The fact that O2
absorbs light at 760 nm is the basis for another optical pO2 sensor using the airpath
absorption of light at 760 nm and at another wavelength where O2 does not absorb,
and Beer’s law.
A major means of sensing atmospheric (and respiratory gas) pCO2 makes use
of the IR absorption of the CO2 molecule. Again, two wavelengths are used, one
where CO2 absorbs (e.g., at 4.2 µm) and the other where it doesn’t (e.g., at 3.5 µm).
Water vapor interferes in some CO2 IR absorption bands, so CO2 sensing in respi-
ratory gases requires the gas input to the IR cell to be dried; the drying can be done
chemically, or by heating the gas.
Fiber optic (FO) optical sensors have been used to sense pH through the use of
a pH-sensitive indicator dye, such a phenol red bound to the surface of 5–10 µm
diameter polyacrylamide microspheres mixed with 1 µm diameter polystyrene
microspheres for light scattering. The dye and microspheres are enclosed in a small
plastic tube permeable only to H+ ions. One end of the microtube is sealed; the other
is joined to two optical fibers (input and output). Phenol red in aqueous solution has
an isobestic wavelength at c. 480 nm (wavelength where reflectance is independent
of pH). The wavelength at which maximum change in reflectance vs. pH occurs is
c. 560 nm. By using these two wavelengths to illuminate the indicator dye and
computing the difference in reflected intensities over their sum, pH from 6.1 to 7.6
can be measured (Wolfbeis, 1991). This type of sensor is called an optrode. Note
that, if this sensor is surrounded by a bicarbonate solution that is separated from the
skin by a CO2-permeable membrane, this pH sensor should be usable to measure
tcpCO2. Other indicator dyes have also been used in similar pH optrode sensors.
These include, but are not limited to: sulfo-phenolphthalein, bromthymol blue, and
bromphenol blue (Wolfbeis, 1991).
Another optrode strategy to measure pH (and possibly pCO2) makes use of light-
induced fluorescence, which is pH-sensitive. In one system, immobilized 8-hydroxy-
1,3,6-pyrenetrisulfonate (HPTS) is excited by pulses of 455 nm light. The fluores-
cence response at 520 nm becomes stronger as the pH goes from 5 to 8. HPTS also
has a fluorescence isobestic excitation wavelength at 435 nm. The response here is
also at 520 nm, but its intensity does not change with pH. The 99% response time
of the HPTS sensor was about 1.7 minutes (to a step change of pH; 6 → 8 → 6,
etc.), and its accuracy was c. ± 0.1 pH unit. Other fluorescent pH indicators have
also been used: aminofluorescein and 7-hydroxycoumarin-3-carboxylic acid (HCC)
(Wolfbeis, 1991). Again, an H+ permeable membrane serves to isolate the immobi-
lized fluorescent chemical. This type of sensor, too, has the potential for measuring
tcpCO2.
It is possible that certain solid-state pH sensors can be adapted to tcpCO2
operation. It is known that silicon oxynitride is pH-sensitive over a large pH range
when used as a coating for the gate of a chemically sensitive field-effect transistor
© 2002 by CRC Press LLC
0961/C07/frame Page 182 Tuesday, August 21, 2001 6:34 AM
182 Noninvasive Instrumentation and Measurement in Medical Diagnosis
(CHEMFET) (Kelly et al., 1991). A heated membrane would still be required over
the skin, but the analyte gas would diffuse into a low-volume bicarbonate solution-
filled measurement compartment with which the coated gate of the CHEMFET was
in contact.
© 2002 by CRC Press LLC
You might also like
- Viva 2Document7 pagesViva 2roseNo ratings yet
- O2 Transpot & DeliveryDocument42 pagesO2 Transpot & Deliverypprashant00100% (2)
- Dissolved OxygenDocument9 pagesDissolved OxygenNelson Cabingas100% (1)
- Blood Gas AnalyzerDocument11 pagesBlood Gas AnalyzerAleesha0% (1)
- Blood Gas AnalyzerDocument36 pagesBlood Gas AnalyzerNabila Souza NugrahaNo ratings yet
- Unit 2. Biomedical Blood Gas Analyzers 2.1 Acid Base BalanceDocument5 pagesUnit 2. Biomedical Blood Gas Analyzers 2.1 Acid Base BalanceAnup SapkotaNo ratings yet
- Blood Gas AnalyzerDocument5 pagesBlood Gas Analyzerb.obsr.o.bbins.67.8No ratings yet
- Gas Analyser: How It Works A Presentation With A Hint of Spanish Accent Andreu Roca Bajona - June 2020Document22 pagesGas Analyser: How It Works A Presentation With A Hint of Spanish Accent Andreu Roca Bajona - June 2020Sihome ThodireNo ratings yet
- Electrochemistry 1Document64 pagesElectrochemistry 1Avinash MohanNo ratings yet
- Factors Modifying The Accuracy of ABG ResultsDocument11 pagesFactors Modifying The Accuracy of ABG Resultsilmi_andinurulNo ratings yet
- Me FullDocument101 pagesMe FullKowsi MathiNo ratings yet
- Unit 2 notes-ME..Document23 pagesUnit 2 notes-ME..Kowsi MathiNo ratings yet
- Blood Gas ElectrodesDocument63 pagesBlood Gas Electrodeswellawalalasith0% (1)
- The Anion Gap and The Bicarbonate GapDocument8 pagesThe Anion Gap and The Bicarbonate GapChamika HuruggamuwaNo ratings yet
- Blood Gas AnalyzerDocument41 pagesBlood Gas Analyzerjonathan stevenNo ratings yet
- Appendices 2017Document29 pagesAppendices 2017Nazario HuarachiNo ratings yet
- Electrolysis of Water: AA Battery Tap Water Salt HydrogenDocument12 pagesElectrolysis of Water: AA Battery Tap Water Salt HydrogenFlorin AndreiNo ratings yet
- BC368 Biochemistry of The Cell II: CH 19 (PP 731-747)Document50 pagesBC368 Biochemistry of The Cell II: CH 19 (PP 731-747)Gorav SharmaNo ratings yet
- Oxygen MeasurementDocument4 pagesOxygen MeasurementAurelia AlexandraNo ratings yet
- CH ElectreochemistryDocument43 pagesCH ElectreochemistryOP HBSNo ratings yet
- The Nitrate Reduction Process: A Way For Increasing Interfacial PHDocument8 pagesThe Nitrate Reduction Process: A Way For Increasing Interfacial PHAbuzar KhanNo ratings yet
- Redox Potential ElectrodesDocument11 pagesRedox Potential ElectrodesNadya NazriNo ratings yet
- PH Measurement, pCO2, Po2Document3 pagesPH Measurement, pCO2, Po2jeswanth reddyNo ratings yet
- Models - Bfc.sofc Unit CellDocument32 pagesModels - Bfc.sofc Unit CellXiaoqiang zhangNo ratings yet
- Biochemical Markers For Clinical Monitoring of Tissue PerfusionDocument14 pagesBiochemical Markers For Clinical Monitoring of Tissue PerfusionTrọng MPNo ratings yet
- S3 CP1 Arterial Blood GasDocument2 pagesS3 CP1 Arterial Blood Gas2013SecBNo ratings yet
- Electrolysis of Water - WikipediaDocument9 pagesElectrolysis of Water - WikipediaNovia PurwitasariNo ratings yet
- Acid-Base Balance & Blood GasesDocument39 pagesAcid-Base Balance & Blood GasesSulaiman TahsinNo ratings yet
- Respiration PHYSIO (MediCallAcademy - Org) - 18-20Document3 pagesRespiration PHYSIO (MediCallAcademy - Org) - 18-20Tauseef AfridiNo ratings yet
- Interpretation of Arterial Blood Gases and Acid-Base DisordersDocument44 pagesInterpretation of Arterial Blood Gases and Acid-Base DisordersSuren VishvanathNo ratings yet
- Lec 3 - Measurement and DesignDocument35 pagesLec 3 - Measurement and DesignMohsin SarfrazNo ratings yet
- Carbon Dioxide 1687608695Document3 pagesCarbon Dioxide 1687608695bayoalpha23No ratings yet
- Li ACS Catal 2016Document6 pagesLi ACS Catal 2016Mary BNo ratings yet
- DOC042 52 20169 July 2014 Technical Note Red Rod TechniqueDocument2 pagesDOC042 52 20169 July 2014 Technical Note Red Rod TechniquegregNo ratings yet
- Gaseous Diffusion and Transport2 MBBS1 Jolley 2020 - 1Document35 pagesGaseous Diffusion and Transport2 MBBS1 Jolley 2020 - 1K ZarabianNo ratings yet
- Respiratory Monitoring BackupDocument51 pagesRespiratory Monitoring BackupmohammedNo ratings yet
- Chapter 24 Oxygen Toxicity and Hyper 2017 Nunn S Applied Respiratory PhysiDocument18 pagesChapter 24 Oxygen Toxicity and Hyper 2017 Nunn S Applied Respiratory PhysiFontecha AnaNo ratings yet
- Electrochemistry Index Search Box Main IndexDocument3 pagesElectrochemistry Index Search Box Main IndexshahinNo ratings yet
- The Anodic Behaviour of Cobalt inDocument9 pagesThe Anodic Behaviour of Cobalt inAydanNo ratings yet
- Blood Gas AnalyzerDocument40 pagesBlood Gas Analyzermohammed alolfeNo ratings yet
- Experiment 21A Faraday'S LawDocument10 pagesExperiment 21A Faraday'S LawGreen ManNo ratings yet
- Direct Determination of COD PDFDocument7 pagesDirect Determination of COD PDFAfzaal AshrafNo ratings yet
- Lect-13-Chemical BiosensorsDocument37 pagesLect-13-Chemical BiosensorsmeharNo ratings yet
- MODIFIED Applied Chemistry-SET-2 Key - R20 RegulationDocument35 pagesMODIFIED Applied Chemistry-SET-2 Key - R20 RegulationM VAMSHI M VAMSHINo ratings yet
- BatteriesDocument12 pagesBatteriespnarendrareddy.mscNo ratings yet
- ABG InterpretationDocument38 pagesABG Interpretationmahmod omerNo ratings yet
- Mathematical Modelling and Simulation AnDocument7 pagesMathematical Modelling and Simulation AnHusamZarourNo ratings yet
- CH1 2011Document44 pagesCH1 2011Amsalu WalelignNo ratings yet
- Electrolysis of Water - Wikipedia PDFDocument78 pagesElectrolysis of Water - Wikipedia PDFJovit DoniñaNo ratings yet
- Study On Production of Free Hydroxyl Radical and Its Reaction With Salicylic Acid at Lead Dioxide ElectrodeDocument7 pagesStudy On Production of Free Hydroxyl Radical and Its Reaction With Salicylic Acid at Lead Dioxide ElectrodePeter KozlikhinNo ratings yet
- Technological Development and Prospect of Alkaline Fuel CellsDocument7 pagesTechnological Development and Prospect of Alkaline Fuel CellsGevazio JuniorNo ratings yet
- Report H20Document6 pagesReport H20Nattapat SutapakornNo ratings yet
- Blue Doodle Project PresentationDocument21 pagesBlue Doodle Project PresentationJaya KerupaaNo ratings yet
- Oxygen TransportDocument40 pagesOxygen TransportMike MayerNo ratings yet
- 05 HypoxiaDocument75 pages05 HypoxiaShri PravallikaNo ratings yet
- Aldehydes and KetonesDocument7 pagesAldehydes and KetonesAshok PradhanNo ratings yet
- Han 2012Document8 pagesHan 2012Luis MoralesNo ratings yet
- Gas Transport in Blood PPT 1Document34 pagesGas Transport in Blood PPT 1CLEMENTNo ratings yet
- XXIVth International Congress of Pure and Applied Chemistry: Plenary and Main Section Lectures Presented at Hamburg, Federal Republic of Germany, 2–8 September 1973From EverandXXIVth International Congress of Pure and Applied Chemistry: Plenary and Main Section Lectures Presented at Hamburg, Federal Republic of Germany, 2–8 September 1973No ratings yet
- Introduction To Noninvasive MeasurementsDocument5 pagesIntroduction To Noninvasive MeasurementsRolando EsquivelNo ratings yet
- Body Temperature Measurements: 0961/c06/frame Page 157 Tuesday, August 21, 2001 6:31 AMDocument16 pagesBody Temperature Measurements: 0961/c06/frame Page 157 Tuesday, August 21, 2001 6:31 AMRolando EsquivelNo ratings yet
- DataSheet 40001291HDocument322 pagesDataSheet 40001291HFran BorgesNo ratings yet
- Noninvasive Measurement of Blood PressureDocument5 pagesNoninvasive Measurement of Blood PressureRolando EsquivelNo ratings yet
- Compuerta SN74LS00 DataSheetDocument34 pagesCompuerta SN74LS00 DataSheetMartin ChichoNo ratings yet
- Pic 16 F 84Document90 pagesPic 16 F 84AzraeiMananNo ratings yet
- Ficha Tecnica 74LS04 Compuerta NOTDocument2 pagesFicha Tecnica 74LS04 Compuerta NOTSteven BallardNo ratings yet
- Mathematical Model of SOFC (Solid Oxide Fuel Cell) For Power Plant SimulationsDocument7 pagesMathematical Model of SOFC (Solid Oxide Fuel Cell) For Power Plant SimulationsErwin Zavalla OchoaNo ratings yet
- Mg-Anode 3.htmDocument2 pagesMg-Anode 3.htmDompet ZebraNo ratings yet
- CorrosionNotes Handout1 2017 v1 PDFDocument40 pagesCorrosionNotes Handout1 2017 v1 PDFAbdo MohdyNo ratings yet
- Term PaperDocument9 pagesTerm PaperKojo PappoeNo ratings yet
- Evaluation of Cathodic Protection of Mild Steel WithDocument6 pagesEvaluation of Cathodic Protection of Mild Steel WithJorge SuarezNo ratings yet
- ElectrochemistryDocument66 pagesElectrochemistryDeepti JainNo ratings yet
- CH 11Document25 pagesCH 11Melissa ChehwaneNo ratings yet
- Teknik JWB Kertas 3Document13 pagesTeknik JWB Kertas 3THANABALAN A/L MUNUSWAMY MoeNo ratings yet
- An Inexpensive Fiel Portable Programmable PotentiostatDocument6 pagesAn Inexpensive Fiel Portable Programmable PotentiostatVictor SabNo ratings yet
- Guidelines For Subsea Pipeline Cathodic Protection SurveyDocument38 pagesGuidelines For Subsea Pipeline Cathodic Protection SurveyjavadNo ratings yet
- Electrochemistry PresentationDocument36 pagesElectrochemistry PresentationMuhammad HaziqNo ratings yet
- Design of Impressed Current Cathodic Protection Forsteel Immersed in Freshwaterabdelsalam I S Ahdasha Project Report Submitted in Partial Fulfillment of Therequirements For The Award of The Degree ofDocument43 pagesDesign of Impressed Current Cathodic Protection Forsteel Immersed in Freshwaterabdelsalam I S Ahdasha Project Report Submitted in Partial Fulfillment of Therequirements For The Award of The Degree ofSarah DeanNo ratings yet
- Corosi 2Document13 pagesCorosi 2iisprastyaNo ratings yet
- Electrochem DPP Physics WallahDocument3 pagesElectrochem DPP Physics WallahMehulNo ratings yet
- Chapter by Chapter MCQ PDFDocument196 pagesChapter by Chapter MCQ PDFmahmoud ali100% (1)
- Electrochemistry and The Nernst EquationDocument53 pagesElectrochemistry and The Nernst EquationMaha RajNo ratings yet
- Electrochemistry NotesDocument19 pagesElectrochemistry NotesLinaNo ratings yet
- 2021-11-17 CATF Report Electrolysis FinalDocument79 pages2021-11-17 CATF Report Electrolysis Finalle hoai NamNo ratings yet
- Chemistry 2810 A Answers To The First AssignmentDocument11 pagesChemistry 2810 A Answers To The First Assignmenthodaps.ggsNo ratings yet
- R18B Tech CivilEngg SyllabusDocument119 pagesR18B Tech CivilEngg SyllabusKishore Naik MalothNo ratings yet
- As 4036-2006 Corrosion of Metals - Dissimilar Metals in Contact in SeawaterDocument8 pagesAs 4036-2006 Corrosion of Metals - Dissimilar Metals in Contact in SeawaterSAI Global - APACNo ratings yet
- Lecture 3 Kinetics PDFDocument69 pagesLecture 3 Kinetics PDFmanishtubNo ratings yet
- Saudi Aramco Test Report: Galvanic CP Testing SATR-X-3101 3-Jul-18 CPDocument2 pagesSaudi Aramco Test Report: Galvanic CP Testing SATR-X-3101 3-Jul-18 CPkarthi51289No ratings yet
- 6.9 Exercises On ElectrochemistryDocument35 pages6.9 Exercises On ElectrochemistrySphoorti NipanikarNo ratings yet
- ICAO TI Lithium Battery Summary ChartDocument2 pagesICAO TI Lithium Battery Summary Chartzubeen RIZVINo ratings yet
- 11S Chemistry: TR: Ms Cavieta Persaud Ram KishoreDocument8 pages11S Chemistry: TR: Ms Cavieta Persaud Ram KishoreManisha PersaudNo ratings yet
- CP PresentationDocument24 pagesCP PresentationCương Lê VănNo ratings yet
- Electrochemistry and Chemical Sensors: Prasad V.A. PamidiDocument32 pagesElectrochemistry and Chemical Sensors: Prasad V.A. PamidiRiskullah MakmurNo ratings yet
- Li!IllDocument11 pagesLi!IllHira FiazNo ratings yet
- Astm A630Document8 pagesAstm A630AlbertoNo ratings yet