Professional Documents
Culture Documents
Infectious Diseases USMLE Notes (Free Trial)
Infectious Diseases USMLE Notes (Free Trial)
Uploaded by
Shoaib MughalOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Infectious Diseases USMLE Notes (Free Trial)
Infectious Diseases USMLE Notes (Free Trial)
Uploaded by
Shoaib MughalCopyright:
Available Formats
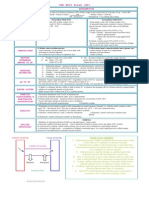
Infectious diseases
Tick-Borne Diseases
Disease Description Clinical Features Diagnosis & Treatment
- Is a protozoal disease caused by the genus plasmodium, - Hallmark is cyclical fever (which it coincides with RBC lyses by parasites) Dx is made from :
(which is a RBC parasite) . Fever patter : Giemsa-stained peripheral blood smear
Fever occurs every 48 hours with vivax & ovale. TTT:
- Transmitted by tick bite of infected: anopheles mosquitoes. every 72 hours with malarieae, A) Treatment:
Periodicity is NOT seen with falciparum (constant fever) - Chloroquine (safe in pregnancy) If chloroquine resistance :
- You have 4 species: a- Quinine & Tetracycline or
Falciparum: Most deaths are due to falciparum (P. falciparum IV Quinidine & Doxycycline)
Malaria vivax, ovale: are responsible for several relapse.
- The typical episode consists of 3 stages :
1- Cold stage: chills & shivering followed by b- & Mefloquine & Atovaquone–proguanil # in Pregnancy & CRD
malariae. 2- Hot stage: high grade fever 2-6 hours later B) Prophylaxis : to all travels to malarious regions
3- Sweating stage: diaphoresis & resolution of the fever.
1- Mefloquine :is the DOC for chemoprophylaxis against
Contraindicated in Seizures & Psych. chloroquine-resistant malaria.
Add a 2-week regimen of : Primaquine
- Started 1 week before travel continued until 4 weeks after
departure from an endemic area.
Contraindicated in patients with G6PD deficiency
2- Primaquine (both for prophylaxis & ttt ) is indicated against:
p. vivax or p. ovale, (which can cause persistence in the liver).
- Parasite enters the patient’s RBC and causes hemolysis.
Babesiosis - Is a protozoal disease caused by the genus babesia . - Clinical manifestations vary from : Definitive dx is made from :
Giemsa-stained thick & thin blood smear.
Asymptomatic infection to
- Transmitted by tick bite of infected: ixodes tick , in
Clinically significant illness Hemolytic anemia associated with:
usually occurs in people: endemic area: TTT:
jaundice, hemoglobinuria, renal failure, and death.
1- Over age 40, pts Etiology: B. microti in the northern & midwestern of US. 1- Quinine-Clindamycin or
Unlike other tick-borne illnesses, rash is NOT a feature of babesiosis,
2- Without a spleen, or 2- Atovaquone-Azithromycin.
except in severe infection where thrombocytopenia may cause a
3- Immunocompromised. secondary petechial or purpuric rash.
1- Early localized stage: Dignosis clinical / +ve (ELISA) & Western Blot tests for antibodies.
- Is a tick-borne illness caused by the spirochete Borrelia - Skin: erythema chronicum migrans (Bull's eye) at site of tick
Burgdorferi . 2- Early disseminated stage: (days to weeks to months after skin rash) TTT:
- Fever + Chills, fatigue, arthralgias, headache
- Transmitted by tick bite of infected: ixodes scapularis - Early Lyme Disease (Rash / Joint / Bell's palsy) :
- Neuro : -- Bell palsy (Cranial neuritis)
Lyme disease - History of: Outdoor activities (e.g., hiking, camping). -- sensory-motor neuropathies 1- Doxycycline (Oral) for 21 days
Contraindicated in: Pregnant / Child <8 y Amoxicillin
-- Aseptic meningitis (Brudzinski & Kernig signs negative).
-- Encephalitis Allergy: Erythromycin
- Cardiac: AV block / Myocarditis / Pericarditis 2- Amoxicillin / Cefuroxime
3- Late disseminated stage: (few months to years later) :
- For Cardiac & CNS (other than Bell's palsy) :
- Joint: Monoarthritis(Large especially knee) / chronic synovitis
Ceftriaxone (IV)
- Neuro: Encephalitis / Transverse myelitis
Typically 1 week after the tick bite. Dx requires a high index of clinical suspicion
- Is a tick-borne illness caused by the intracellular bacteria
Rickettsia Rickettsii - In the first 3 days: TTT:
Rocky - Transmitted by tick bite of ticks feeding on animals
Indistinguishable from a self-limiting viral illness
FAHM: Fever, Anorexia, Headache, Myalgias / Nausea, vomiting
ABC’s should always come first when treating any pt. check vitals
to make sure that the pt is stable.
mountain - History of: Outdoor activities - After 3 days of fever Rash : - If signs of shock (hypotensive) :
1- Maculopapular rash: The best NEXT best step is: IV fluids to replete intravascular volume.
spotted fever Organisms enter the host cells via tick bites multiply in the Starts peripherally (palms & soles) Spread centrally (limbs/trunk/face) - After he is stable: DOC :
vascular endotheliumDamage to the vascular endothelium Doxycycline (Oral/IV) for both adults & children.
2- then petechiae:
- The most serious tick- results in : microhemorrhages, and microinfarcts.
Micro vascular damage as disease progress : - In pregnant:
borne disease in the US
- Petechiate + Hypotension & Non-cardiogenic pulmonary edema Chloramphenicol
- Is a tick-borne illness caused by one of 3 different Incubation period varies from 1 to 3 weeks.
Dx : Confirm by serology
Ehrlichiosis intracellular gram -ve bacteria , genus Ehrlichia - FAHM
- Transmitted by tick bite. - No Rash its description as : “spotless rocky mountain spotted fever.” TTT:
- Complications: Renal Failure / GIT bleeding
It infects and kills WBCs show - Doxycyline (for 1 week)
intracellular inclusions (morulae) LABS:
leucopenia / thrombocytopenia aminotransferases.
Cestode
- Is a parasitic disease caused by larval stage of the pork If a person (rather than a pig"intermediate host") consumes the T. solium
tapeworm: Taenia solium eggs excreted in human feces Cysticercosis results.
Normal Life cycle of Taenia Solium: - After ingestion, the embryos are released in the intestine larvae
Cysticercosis * Definitive Host: Humans (only) invade the intestinal wall disseminate hematogenously to encyst in:
1- Brain: Neurocysticercosis
TTT:
* Intermediate host: pig Treatment of Neurocysticercosis :
* Infective stage: larva -- multiple, small (usually <1cm ) , fluid-filled cysts in the brain
* Mode of infection: humans eat larvae in meat such as … parenchyma and have a membranous wall Albendazole
NCC is the most common
infected, undercooked pork. -- On neuroimaging: invaginated scolex
parasitic infection of brain
* Habitat: adult in upper jejunumexcretes its eggs into feces 2- Skeletal muscle
If a pig consumes these eggs, it becomes an 3- Subcutaneous tissue
intermediate host, with larvae encysting in its tissues. 4- Eye
- Echinococcus tape worm has two main species: - If a human (rather than sheep) consumes infectious eggs excreted by Both be diagnosed with a combination of imaging and serology
1- E.Granulosus causes: cystic echinococcosis (CE) dogs in the feces Echinococcosis results. In the absence of a positive serologic test: percutaneous aspiration
Echinococcosis 2- E. multilocularis causes: alveolar echinococcosis (AE) or biopsy (may be required to confirm the diagnosis).
- After ingestion, the oncospheres are hatched in the intestine
Hydatid cyst is a fluid filled Normal Life cycle of E.Granlosus: penetrate the bowel wall disseminate hematogenously to various
* Definitive Host: Dogs (& other canines) visceral organs Formation Hydatid Cyst, mostly in : TTT:
cyst with an inner germinal
1- Liver : RUQ pain, rupture to peritoneal cavity anaphylaxis 1- Surgical resection as in liver cycts.
layer and an outer acellular * Intermediate host: Cattle / Sheep
2- Lung: cough / chest pain / dyspnea / hemoptosis 2- Percutaneous management
laminated membrane * Infective stage: Embryonated Eggs in feces.
* Mode of infection: Eating food contaminated with egg. 3- Medical:
* Habitat: Small intestine Germinal layer gives rise to numerous secondary daughter cysts. Albendazole: 1 week prior to surgery/ 4 weeks postoperatively
Nematode
- It is caused by the roundworm trichinella spiralis 3 phases + Eosinophilia. Dx: Triad clinical symptoms confirmed by serology.
- It is acquired by eating undercooked pork that contains • Initial phase: in 1st week larvae invade the intestinal wall.
GIT symptoms: abdominal pain, nausea, vomiting, diarrhea. TTT:
Trichinosis encysted trichenella larva
Triad :
• 2nd phase: in 2nd week of infection larval migration : 1- mild infection : No Antiparasitics
Local & Systemic hypersensitivity reaction Symptomatic treatment with analgesia & Antipyretics
(trichinellosis)
1- Muscle pain (myositis) Nail : “splinter” hemorrhages, 2- In Systemic Symptoms :
2- Periorbital edema Eye: conjunctival & retinal hemorrhages/per orbital edema/chemosis. - Albendazole / Mebendazole
3- Eosinophilia • 3rd phase: larvae enter the pt’s skeletal muscle: - together with corticosteroids
after eating raw meat = Trichinella spiralis (trichinosis) Muscle symptoms: muscle pain, tenderness, swelling, weakness.
- It is caused by the roundworm Ascaris Lumbricoides Ascariasis often presents as : Dx : Egg seen in stool examination.
- It is acquired by eating food that contains Embryonated egg 1- Lung phase with non productive cough followed by : TTT:
(containing 2nd stage rhabditiform larva)
Ascariasis Notes :
2- Asymptomatic intestinal phase 1- First line: Albendazole / Mebendazole
Contraindicated in: Pregnant Pyrantel Pamoate
Symptoms result from obstruction caused by the organisms, as:
Ascariasis can also present with GIT symptoms + eosinophilia 2- Alternative: Ivermectin / Nitazoxanide
small bowel or biliary obstruction.
- It is caused by the pinworm Enterobius Vermicularais. At night, females migrate out through the rectum onto the perianal skin Dx is by the “scotch tape test” demonstrates presence of eggs.
Enterobiasis - Adult parasite thrives in the Cecum / appendix. to deposit eggs Nocturnal Perianal Pruritis. TTT: Albendazole or Mebendazole
- It is caused by dog & cat hookworm ancylostoma braziliense. - Initially : Dx is clinical in cutaneous disease/ & pulmonary disease : dry cough
Cutaneous - It's acquired after skin contact with soil/sand contaminated multiple pruritic, erythematous papules at the site of larval entry TTT:
- Followed by: Migration 1- Preferred : Ivermectin
larva migrans with dog or cat feces containing the infective larvae
Notes :
Severely pruritic, elevated, serpiginous, reddish brown lesions on 2- Alternative: Albendazole
(creeping eruption) the skin, which elongate at the rate of several millimeters per day as
Most common seen in the LE / but the UE can also be involved. No Antiparasites in Pulmonary disease since illness is mild & self-limited
the larvae migrate in the epidermis.
To download the full file and the other USMLE files, please click here to SUBSCRIBE and get a lifetime membership
You might also like
- Cranial Nerves - Function and Dysfunctions, 3E (2010) (PDF) (UnitedVRG)Document262 pagesCranial Nerves - Function and Dysfunctions, 3E (2010) (PDF) (UnitedVRG)Alvaro RivCalle87% (15)
- My Notes For USMLEDocument1 pageMy Notes For USMLEmonica ortizNo ratings yet
- Parasitology Table Review 2Document8 pagesParasitology Table Review 2Sarah Lim100% (2)
- Embryology: Lung DevelopmentDocument91 pagesEmbryology: Lung DevelopmentPrarthanaNo ratings yet
- UW Infectious Diseases + Microbiology Educational Objectives PDFDocument75 pagesUW Infectious Diseases + Microbiology Educational Objectives PDFDrbee10No ratings yet
- Cases in Primary Care - NEJMGroup - CollectionDocument146 pagesCases in Primary Care - NEJMGroup - CollectionPanayiotis Stavroulakis100% (2)
- UW (Step 1) Dermatology - Educational Objectives PDFDocument28 pagesUW (Step 1) Dermatology - Educational Objectives PDFUsama BilalNo ratings yet
- 7sgdfgf PDFDocument438 pages7sgdfgf PDFPratik JadhavNo ratings yet
- Differential Diagnosis of Glomerular DiseasesDocument2 pagesDifferential Diagnosis of Glomerular DiseasesMaryam Fadah100% (1)
- Hemolytic Anemias: Common Findings in AllDocument4 pagesHemolytic Anemias: Common Findings in AllSamah KhanNo ratings yet
- 100 Concepts - MCBDocument316 pages100 Concepts - MCBNisreen SalameNo ratings yet
- Poliomyelitis Haemophilus Influenzae Type B VariecellaDocument4 pagesPoliomyelitis Haemophilus Influenzae Type B VariecellaJeanna Chong100% (1)
- Infectious Diseases USMLE Notes (Free Trial)Document1 pageInfectious Diseases USMLE Notes (Free Trial)Laura Tapia100% (1)
- Normal Lab Values (USMLE Step 1)Document12 pagesNormal Lab Values (USMLE Step 1)nmp274No ratings yet
- Nephrotic Nephritic SyndromsDocument4 pagesNephrotic Nephritic SyndromsKimiwari100% (2)
- Microbiology Key WordsDocument5 pagesMicrobiology Key Wordsmoilo86020% (1)
- HY DermatologyDocument68 pagesHY DermatologyDiegoNo ratings yet
- Micro NotesDocument29 pagesMicro NotesRoberto Christian Cerrud RodríguezNo ratings yet
- Mtap Batch 2 MidtermsDocument75 pagesMtap Batch 2 MidtermsLea JuanNo ratings yet
- Parathyroid Hormone PDFDocument120 pagesParathyroid Hormone PDFLaura TapiaNo ratings yet
- Goljan - Integrated Pathology Notes PDFDocument60 pagesGoljan - Integrated Pathology Notes PDFIsaac JacksNo ratings yet
- MOST IMPORATANT ONE LINERS Compiled by Medicinosis Magnus 2Document18 pagesMOST IMPORATANT ONE LINERS Compiled by Medicinosis Magnus 2VAIBHAV SHARMA- 122No ratings yet
- Infectious DiseaseDocument28 pagesInfectious DiseaseAnukriti MamgainNo ratings yet
- El Husseinys Essentials of General PrinciplesDocument92 pagesEl Husseinys Essentials of General PrinciplesSara Alsubaie100% (1)
- Disorders of Primary Hemostasis Quantitative Disorders of Secondary HemostasisDocument23 pagesDisorders of Primary Hemostasis Quantitative Disorders of Secondary Hemostasisasda201487100% (1)
- 2015 Usmle Review Lecture Histology and Cell Biology I Rhys BrooksDocument25 pages2015 Usmle Review Lecture Histology and Cell Biology I Rhys BrooksRushi ShahNo ratings yet
- Herpes, Pox, Rhabdo, Arena VIRUSDocument7 pagesHerpes, Pox, Rhabdo, Arena VIRUSErnie G. Bautista II, RN, MDNo ratings yet
- HaematinicsDocument2 pagesHaematinicsGerardLum100% (2)
- International Medical Graduate and the United States Medical Residency Application: A Guide to Achieving SuccessFrom EverandInternational Medical Graduate and the United States Medical Residency Application: A Guide to Achieving SuccessRaghav GovindarajanNo ratings yet
- My Notes For USMLEDocument48 pagesMy Notes For USMLEaesfafafaNo ratings yet
- Virology - Study GuideDocument5 pagesVirology - Study GuideMatt McGlothlinNo ratings yet
- Parasite QuizDocument7 pagesParasite QuizNur Liyana100% (1)
- PATH All TA Reviews Answers and Notes11Document718 pagesPATH All TA Reviews Answers and Notes11Andleeb Imran100% (1)
- Most CommonDocument24 pagesMost CommonTarek TarekNo ratings yet
- 500 Nuggets CK CourseDocument36 pages500 Nuggets CK Coursepangea80No ratings yet
- Diseases Study Guide 2007Document6 pagesDiseases Study Guide 2007Bahaa Ibrahim HelmiNo ratings yet
- InfectionDocument42 pagesInfectionAhmad SobihNo ratings yet
- Cns PathologyDocument18 pagesCns Pathologysunnyorange8No ratings yet
- Microbiology TablesDocument19 pagesMicrobiology TablesRebecca MarshallNo ratings yet
- Structural Biology of HIVDocument31 pagesStructural Biology of HIVLaura TapiaNo ratings yet
- Gastrointestinal & NutritionBlock3 PDFDocument170 pagesGastrointestinal & NutritionBlock3 PDFTed DoyleNo ratings yet
- Rapid Review From Usmle ... Spotters and OnelinersDocument120 pagesRapid Review From Usmle ... Spotters and OnelinersViroop ReddyNo ratings yet
- Micro Buzz Words - KEY WordsDocument8 pagesMicro Buzz Words - KEY WordsKris GulleyNo ratings yet
- First Aid Pharmacology AntimicrobialsDocument23 pagesFirst Aid Pharmacology AntimicrobialsLaura Lopez RocaNo ratings yet
- Major Bacterial Genera Table For ReviewDocument12 pagesMajor Bacterial Genera Table For ReviewmojdaNo ratings yet
- Malassezia Furfur An-An Ap-Ap Naturally Found On The SkinDocument48 pagesMalassezia Furfur An-An Ap-Ap Naturally Found On The SkinNikki ValerioNo ratings yet
- Medical Mnemonics For MicroorgDocument4 pagesMedical Mnemonics For Microorgkenz18096No ratings yet
- Taenia SoliumDocument48 pagesTaenia Soliumniki100% (1)
- NO Hazard Slight Moderate Serious Extreme: Hazard Hazard Hazard HazardDocument74 pagesNO Hazard Slight Moderate Serious Extreme: Hazard Hazard Hazard HazardCristy Jean100% (1)
- Parasitology Chart 211Document20 pagesParasitology Chart 211Sanjay Kumar100% (1)
- Microbiology: Presented by Alyazeed Hussein, BSCDocument64 pagesMicrobiology: Presented by Alyazeed Hussein, BSCT N100% (1)
- DRTPAnnouncementEN PDFDocument1 pageDRTPAnnouncementEN PDFSinaShafaatiNo ratings yet
- The Craming MDDocument132 pagesThe Craming MDRosalie Catalan EslabraNo ratings yet
- 'Aliah's Physio NotesDocument30 pages'Aliah's Physio NotesLuqman Al-Bashir FauziNo ratings yet
- Block 13 Patho SlidesDocument62 pagesBlock 13 Patho SlidesLennon Ponta-oyNo ratings yet
- Rashes and FeversDocument36 pagesRashes and FeversLucykeshNo ratings yet
- Fmge June 2021 Reacall Questions by Saunil ShahDocument12 pagesFmge June 2021 Reacall Questions by Saunil ShahTamilmani n.mNo ratings yet
- Set 3048993Document64 pagesSet 3048993dammytemiNo ratings yet
- Bacteriology SummaryDocument38 pagesBacteriology SummaryMohsen HaleemNo ratings yet
- Harrisons: Introduction To Infectious DiseasesDocument3 pagesHarrisons: Introduction To Infectious Diseasesapi-3704562No ratings yet
- Microbiology Nca-Cls: Terms in This SetDocument18 pagesMicrobiology Nca-Cls: Terms in This SetjustinNo ratings yet
- CLINPATH Finals ReviewerDocument28 pagesCLINPATH Finals ReviewerVon HippoNo ratings yet
- Gram Positive Cocci Reviewer 1Document6 pagesGram Positive Cocci Reviewer 1alianaNo ratings yet
- Medical MnemonicsDocument65 pagesMedical MnemonicsMIRZA MUHAMMAD ADNAN100% (1)
- LOOK! Neuroscience Brainstorm 2010Document32 pagesLOOK! Neuroscience Brainstorm 2010genome12345No ratings yet
- Mnemonics Step 1Document4 pagesMnemonics Step 1Raji NaamaniNo ratings yet
- QuizletDocument104 pagesQuizletS.No ratings yet
- Vector Borne Diseases: Malaria (Ague)Document20 pagesVector Borne Diseases: Malaria (Ague)Nina OaipNo ratings yet
- Lang Holz Kristen Sen 2013Document3 pagesLang Holz Kristen Sen 2013bamhoi07No ratings yet
- Worksheet 2016Document6 pagesWorksheet 2016Laura TapiaNo ratings yet
- Infectious DemoDocument42 pagesInfectious DemoLaura TapiaNo ratings yet
- Pathology Test IIDocument51 pagesPathology Test IILaura TapiaNo ratings yet
- Learning Objectives: The Shoulder JointDocument7 pagesLearning Objectives: The Shoulder JointLaura TapiaNo ratings yet
- Somatic Recombination and Hypermutation in The Immune SystemDocument62 pagesSomatic Recombination and Hypermutation in The Immune SystemLaura TapiaNo ratings yet
- Patterns of Nerve Injury and Neuropathies: The Motor UnitDocument6 pagesPatterns of Nerve Injury and Neuropathies: The Motor UnitLaura TapiaNo ratings yet
- Guia Pequeños ArtesanalesDocument20 pagesGuia Pequeños ArtesanalesLaura TapiaNo ratings yet
- Braquial PlexusDocument9 pagesBraquial PlexusLaura TapiaNo ratings yet
- Today : Please Be Sure To Turn in Your First Problem Set Assignment Today, and Also Pick Up The Second Problem SetDocument51 pagesToday : Please Be Sure To Turn in Your First Problem Set Assignment Today, and Also Pick Up The Second Problem SetLaura TapiaNo ratings yet
- Parathyroid HormoneDocument32 pagesParathyroid HormoneLaura TapiaNo ratings yet
- BiasDocument111 pagesBiasLaura TapiaNo ratings yet
- TaeniaDocument2 pagesTaeniaMuhammad Fuad JaafarNo ratings yet
- NCC Vs Cns TuberculomaDocument28 pagesNCC Vs Cns TuberculomaAbhinav AggarwalNo ratings yet
- Parasitology Midterms ReviewerDocument7 pagesParasitology Midterms ReviewerRam RamNo ratings yet
- Chapter 53: Antihelminthic Drugs: Drugs That Act Against NematodesDocument4 pagesChapter 53: Antihelminthic Drugs: Drugs That Act Against NematodesChristian DeeNo ratings yet
- Neurocysticercosis An Update On Diagnosis,.10Document9 pagesNeurocysticercosis An Update On Diagnosis,.10RENZO ALEJANDRO ACUÑA FLORESNo ratings yet
- Post-Lecture Exam - Parasitology Answer KeyDocument87 pagesPost-Lecture Exam - Parasitology Answer KeylenvycahpdelusaNo ratings yet
- MBP Lab ReviewerDocument9 pagesMBP Lab ReviewerTrisha PaolaNo ratings yet
- A. Classification: Taenia Solium and Taenia SaginataDocument8 pagesA. Classification: Taenia Solium and Taenia SaginataadhiNo ratings yet
- Learning Guide 14: Animal Health Care Service NTQF Level-IVDocument41 pagesLearning Guide 14: Animal Health Care Service NTQF Level-IVRafez JoneNo ratings yet
- GIDocument196 pagesGIswagmasterNo ratings yet
- TM2 - K37 - Eye Disorders Due To Tropical DiseasesDocument86 pagesTM2 - K37 - Eye Disorders Due To Tropical DiseasesedelinNo ratings yet
- T SoliumDocument17 pagesT SoliumKanchan LalwaniNo ratings yet
- 39 HelminthiasisDocument87 pages39 HelminthiasisArlini Nurul YuliantiNo ratings yet
- Other CestodesDocument9 pagesOther CestodesChristine BuenNo ratings yet
- Antiparasitic DrugsDocument8 pagesAntiparasitic DrugsAdelina MariaNo ratings yet
- Dipiro 8 ParasitDocument12 pagesDipiro 8 ParasitErik Firman RusdiantoNo ratings yet
- Common Worm Infestations in Children: DR Nishant Verma Department of PediatricsDocument25 pagesCommon Worm Infestations in Children: DR Nishant Verma Department of PediatricsJosephine TungoeNo ratings yet
- TaeniasisDocument4 pagesTaeniasisSigrid MNo ratings yet
- Animal ScienceDocument59 pagesAnimal ScienceMounicaNo ratings yet
- Calcific Neurocysticercosis and EpileptogenesisDocument7 pagesCalcific Neurocysticercosis and EpileptogenesiskreizztelNo ratings yet
- Taenia Saginata :)Document20 pagesTaenia Saginata :)faradillaNo ratings yet
- HelmenthsDocument38 pagesHelmenthsKarwanNo ratings yet
- Zoonotic DiseasesDocument96 pagesZoonotic DiseasesWakjira GemedaNo ratings yet
- Cestoda: Dr. Hendra (Tropmed) Parasitology Department Medical Faculty of UnpriDocument42 pagesCestoda: Dr. Hendra (Tropmed) Parasitology Department Medical Faculty of UnpriElvy ShaluNo ratings yet