Professional Documents
Culture Documents
Electrolytes
Uploaded by
Venus Amoroso BaguiosoOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Electrolytes
Uploaded by
Venus Amoroso BaguiosoCopyright:
Available Formats
Electrolytes Clinical Significance Causes
Sodium Hyponatremia Depletional hyponatremia – losing Dilutional hyponatremia – gaining sodium
<135 mmol/L water than sodium than water
diuretics, hypoaldosteronism overhydration
(Addison disease), diarrhea, or syndrome of inappropriate
vomiting, and severe burns or antidiuretic hormone (SIADH),
trauma congestive heart failure
cirrhosis
nephrotic syndrome.
Hypernatremia >145 Water is lost Sodium is retained
mmol/L diarrhea acute ingestion
excessive sweating hyperaldosteronism
diabetes insipidus infusion of hypertonic solutions
during dialysis
Potassium Hypokalemia <3.0 Decreased dietary intake diarrhea
mmol/L hyperaldosteronism laxative abuse
diuretics excess insulin which causes
vomiting increased cellular uptake of
potassium
Hyperkalemia >5.0 Increased intake increased red blood cell lysis
mmol/ renal failure leukemia chemotherapy
hypoaldosteronism
metabolic acidosis
Chloride Hypochloremia <98 excessive vomiting burns
mmol/L use of diuretics aldosterone deficiency
Hyperchloremia > 107 prolonged diarrhea dehydration
mmol/L renal tubular disease excess loss of bicarbonate
Bicarbonate Decreased ctCO2 metabolic acidosis salicylate toxicity
diabetic ketoacidosis
Increased ctCO2 metabolic alkalosis severe vomiting
emphysema
Calcium Hypocalcemia Hypoparathyroidism magnesium deficiency
hypoalbuminemia vitamin D deficiency
chronic renal failure
Hypercalcemia Hyperparathyroidism malignancy involving bone
hypothyroidism renal failure
acute adrenal insufficiency
Phosphorus Hypophosphatemia renal failure lymphoblastic leukemia
hypoparathyroidism intense exercise
neoplastic diseases
Hyperphosphatemia diabetic ketoacidosis alcoholism
hyperparathyroidism malabsorption syndrome
asthma
Magnesium Hypomagnesemia renal failure
excess antacids
Hypermagnesemia gastrointestinal disorders drugs (e.g., diuretic therapy, cardiac
renal diseases glycosides, cisplatin, cyclosporine)
hyperparathyroidism diabetes mellitus with glycosuria
(hypercalcemia alcoholism due to dietary deficiency
Anion gap Decreased anion gap hypoalbuminemia
hypercalcemia.
Increased anion gap uremia hypernatremia
lactic acidosis, ketoacidosis ingestion of methanol, ethylene
glycol, or salicylate
pH disorders ctCO2 PCO2 pH Associated disease
diabetic ketoacidosis due to the production of acetoacetic
acid and p-hydroxybutyric acid
lactic acidosis due to the production of lactic acid
poisonings such as salicylate, ethylene glycol, and methyl
Acidosis ↓ N ↓ alcohol
reduced acid excretion due to renal failure or tubular
acidosis
loss of bicarbonate due to diarrhea or excessive renal
excretion.
Metabolic
ingestion of excess alkali (antacids)
intravenous administration of bicarbonate
renal bicarbonate retention
Alkalosis ↑ N ↑ prolonged diuretic use
loss of hydrochloric acid from the stomach after vomiting,
intestinal obstruction, or gastric suction
glucocorticoid excess as in dishing syndrome
mineralocorticoid excess as in hyperaldosteronism.
chronic obstructive pulmonary disease, such as chronic
bronchitis and emphysema
Acidosis N ↑ ↓ ingestion of narcotics and barbiturates, and
severe infections of the central nervous system such as
meningitis.
Respirator hypoxia
y anxiety
nervousness
Alkalosis N ↓ ↑ excessive crying
pulmonary embolism
pneumonia
congestive heart failure
salicylate overdose
Process ctCO2 PCO2 pH
Respiratory Metabolic ↓pH →Hyperventilation → ↓PCO2 → ↑pH ↓ ↓ N
Compensator acidosis
y Mechanism
Metabolic ↑pH →Hypoventilation → ↑CO2 → ↑H2CO → ↑cdCO2 →↓pH ↑ ↑ N
alkalosis
Renal Resipratory Kidney→ ↑CHCO3 → ↑ cHCO3:cdCO2 → ↑pH ↑ ↑ N
Compensator acidosis
y Mechanism
Respiratory excreting bicarbonate = corrects respiratory alkalosis ↓ ↓ N
alkalosis
You might also like
- Hypermagnesemia Handouts Group 9Document3 pagesHypermagnesemia Handouts Group 9Risha Ethel BerondoNo ratings yet
- FBCA Biomarkers and ConditionsDocument8 pagesFBCA Biomarkers and Conditionsmet50% (2)
- Understanding ElectrolytesDocument2 pagesUnderstanding Electrolytessurviving nursing schoolNo ratings yet
- Clinical Chemistry 2 LAB MT305 Rlh3: ElectrolytesDocument2 pagesClinical Chemistry 2 LAB MT305 Rlh3: ElectrolytesEmiaj Francinne Mendoza100% (1)
- Electrolytes TableDocument4 pagesElectrolytes TableMeg NoriegaNo ratings yet
- Everything You Need To Know About ZappersDocument6 pagesEverything You Need To Know About ZappersArgiris Karavoulias100% (1)
- Diabetic Ketoacidosis Is An Extreme Metabolic Hyperosmotiic Hyperglycemic State Is A LifeDocument2 pagesDiabetic Ketoacidosis Is An Extreme Metabolic Hyperosmotiic Hyperglycemic State Is A LifeLyod BalagasayNo ratings yet
- PathophysiologyDocument7 pagesPathophysiologyJerica Mae VenoyaNo ratings yet
- ABNORMAL Drill Week2Document8 pagesABNORMAL Drill Week2MS Zhou Si ViolonNo ratings yet
- Hyponatremia: Presenter: DR Arun Karmakar Moderator: Prof. N. SharatkumarDocument50 pagesHyponatremia: Presenter: DR Arun Karmakar Moderator: Prof. N. SharatkumarLyra FebriandaNo ratings yet
- Interventional Cardiac Electrophysiology - A Multidisciplinary Approach Section 1, Technology and Therapeutic Techniques - PDF RoomDocument306 pagesInterventional Cardiac Electrophysiology - A Multidisciplinary Approach Section 1, Technology and Therapeutic Techniques - PDF RoomVeronica JanethNo ratings yet
- Neonatal Intestinal ObstructionDocument21 pagesNeonatal Intestinal ObstructionShahzad Bashir ShamsNo ratings yet
- Primary Skin LesionDocument7 pagesPrimary Skin Lesion_carido_No ratings yet
- Electrolyte AbnormalitiesDocument74 pagesElectrolyte Abnormalitiesbluecrush1No ratings yet
- Transfusion ReactionsDocument28 pagesTransfusion ReactionsRovefrances ErpeluaNo ratings yet
- Pa Tho Physiology Final DMDocument6 pagesPa Tho Physiology Final DMJamil LorcaNo ratings yet
- Test Normal Values Higher Value Lower Value NotesDocument6 pagesTest Normal Values Higher Value Lower Value Notesjetri0905No ratings yet
- Diuretic Drugs For Nursing PharmacologyDocument1 pageDiuretic Drugs For Nursing Pharmacologylhayes1234100% (7)
- Fluid and Electrolyte Imbalances Part 2Document46 pagesFluid and Electrolyte Imbalances Part 2Gabrielle Frances FernandezNo ratings yet
- Blok 24 Skenario 1 - Analisa Gas Darah Akibat Ketidakseimbangan ElektrolitDocument15 pagesBlok 24 Skenario 1 - Analisa Gas Darah Akibat Ketidakseimbangan ElektrolitGogmaFirmansyahSiraitNo ratings yet
- Pemeriksaan Lab 1 Nilai NormalDocument3 pagesPemeriksaan Lab 1 Nilai NormalSivasangkari AnbalaganNo ratings yet
- Fluid Therapy Minilecture - Kelompok Mugi N.H PDFDocument35 pagesFluid Therapy Minilecture - Kelompok Mugi N.H PDFMugi NurhudaNo ratings yet
- Week 2Document3 pagesWeek 2api-530814583No ratings yet
- Electrolyte Imbalances Causes: Signs & Symptoms:: Physical Exam: Lab FindingsDocument4 pagesElectrolyte Imbalances Causes: Signs & Symptoms:: Physical Exam: Lab Findingsworleyb83No ratings yet
- 1 ElectrolytesDocument8 pages1 ElectrolytesJessa MayNo ratings yet
- Hypokalemia 180813073624Document26 pagesHypokalemia 180813073624korotkofNo ratings yet
- Fluids and Electrolytes (Concentration and Composition Changes)Document6 pagesFluids and Electrolytes (Concentration and Composition Changes)Kristin SaberonNo ratings yet
- 2-Liver DiseasesDocument28 pages2-Liver DiseasesAhmed IsmaillNo ratings yet
- KIDNEY DISEASES and LIVER DISEASES CHARTDocument16 pagesKIDNEY DISEASES and LIVER DISEASES CHARThira khatriNo ratings yet
- Electrolyte SummaryDocument3 pagesElectrolyte SummaryDeanne Morris-DeveauxNo ratings yet
- Water & Electrolyte BalanceDocument27 pagesWater & Electrolyte Balanceanisa rachmitaNo ratings yet
- Lab Normal Value Comments: AlbuminDocument4 pagesLab Normal Value Comments: AlbumindelantarzNo ratings yet
- Fluid and Electrolytes Cram SheetDocument8 pagesFluid and Electrolytes Cram SheetChrizley Shawn DeroniaNo ratings yet
- Dks HhsDocument16 pagesDks HhsDebora Putri Fernanda SaragihNo ratings yet
- ElectrolytesDocument3 pagesElectrolytesgheannieveleen26No ratings yet
- ELECTROLYTES Edited Semi Finals XDDocument52 pagesELECTROLYTES Edited Semi Finals XDzerachiel zephyrNo ratings yet
- Principles of Fluid & Electrolyte Balance in Surgical PatientsDocument15 pagesPrinciples of Fluid & Electrolyte Balance in Surgical PatientsQuratulain FarooqNo ratings yet
- Lecture 3 CKDDocument53 pagesLecture 3 CKDPharmswipe KenyaNo ratings yet
- Fluid PDFDocument93 pagesFluid PDFSandeep VermaNo ratings yet
- Ipd - Kelas Ac - Kad Dan Hhs - DR - DR.K Heri Nugroho HS, SP - PD, K-EmdDocument51 pagesIpd - Kelas Ac - Kad Dan Hhs - DR - DR.K Heri Nugroho HS, SP - PD, K-EmdTeresia MaharaniNo ratings yet
- Chronic Renal Failure and Renal Disorders - 123159Document25 pagesChronic Renal Failure and Renal Disorders - 123159Syed Yusuf SyedNo ratings yet
- Diabetic Ketoacidosis Hyperglycemic Hyperosmolar State: Dka Dan HhsDocument20 pagesDiabetic Ketoacidosis Hyperglycemic Hyperosmolar State: Dka Dan HhsRashellya RasyidaNo ratings yet
- MNT Penyakit GinjalDocument41 pagesMNT Penyakit GinjalNurfitriana DwiNo ratings yet
- 2 5463111801086427966Document13 pages2 5463111801086427966haidernadhem57No ratings yet
- Hypokalemia 2Document32 pagesHypokalemia 2aqilasafikaNo ratings yet
- Renal Diseases: Dr. Nidhi SharmaDocument36 pagesRenal Diseases: Dr. Nidhi Sharmanidhi261987No ratings yet
- Drug Index Updated2 2Document104 pagesDrug Index Updated2 2docaliNo ratings yet
- Fluids & Electrolytes 5Document14 pagesFluids & Electrolytes 5Justin Angelo SildoraNo ratings yet
- ELECTROLYTES Clinica SignificanceDocument6 pagesELECTROLYTES Clinica SignificanceKim Mae ComendadorNo ratings yet
- Drug Index Updated2 2Document104 pagesDrug Index Updated2 2Sarah RonquilloNo ratings yet
- NCM 112 Fluid and Electrolytes: Hyperkalemia or Potassium ExcessDocument2 pagesNCM 112 Fluid and Electrolytes: Hyperkalemia or Potassium ExcessAngeline NavarroNo ratings yet
- Bagi DIURETIK 1804Document31 pagesBagi DIURETIK 1804Bayyin NuhaNo ratings yet
- Electrolyte Disorders: Crisbert I. Cualteros, MD S.page - TLDocument45 pagesElectrolyte Disorders: Crisbert I. Cualteros, MD S.page - TLm_arianne268932No ratings yet
- Fluid and Electrolyte ImbalanceDocument29 pagesFluid and Electrolyte ImbalancePrincewill SeiyefaNo ratings yet
- محمود جابرDocument2 pagesمحمود جابرAya Eid 7asanNo ratings yet
- Chronic Kidney DiseaseDocument26 pagesChronic Kidney DiseaseAimi ZulkipliNo ratings yet
- Chronic Kidney DiseaseDocument4 pagesChronic Kidney DiseaseImnot YouNo ratings yet
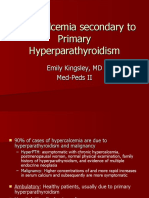
- Hypercalcemia Secondary To Primary HyperparathyroidismDocument26 pagesHypercalcemia Secondary To Primary HyperparathyroidismClaudia IrimieNo ratings yet
- Fluid & Electrolyte Management & Acid Base Disorders: Alice Augustin Amina S Anagha P RDocument47 pagesFluid & Electrolyte Management & Acid Base Disorders: Alice Augustin Amina S Anagha P RAsif AbbasNo ratings yet
- SodiumDocument3 pagesSodiumEmily FernandezNo ratings yet
- A Presentation On: Diabetes MellitusDocument17 pagesA Presentation On: Diabetes MellitusAnil YadavNo ratings yet
- Bhatia ElectrolytesDocument5 pagesBhatia Electrolytesnaga tanoojNo ratings yet
- PEDIA2 2.01b Fluids Electrolytes Summary TablesDocument4 pagesPEDIA2 2.01b Fluids Electrolytes Summary TablesVon HippoNo ratings yet
- Electrolytes, Trace Elements and VitaminsDocument67 pagesElectrolytes, Trace Elements and VitaminsFatima MendozaNo ratings yet
- Fluid and Electrolytes: Dr. Nupur SarkarDocument24 pagesFluid and Electrolytes: Dr. Nupur SarkarNupurshinjiniNo ratings yet
- Angelam - LTC Case StudiesDocument6 pagesAngelam - LTC Case Studiesapi-257604563No ratings yet
- Tenecteplase Thrombolysis For Acute IschemicDocument12 pagesTenecteplase Thrombolysis For Acute IschemicRicardo AcostaNo ratings yet
- 5 Cover Letter Samples For Your Scientific ManuscriptDocument11 pages5 Cover Letter Samples For Your Scientific ManuscriptAlejandra J. Troncoso100% (2)
- Efficacy of Dialectical Behavior Therapy For Adolescents at High Risk For Suicide: A Randomized Clinical TrialDocument11 pagesEfficacy of Dialectical Behavior Therapy For Adolescents at High Risk For Suicide: A Randomized Clinical TrialLia Marcela Rivera HernandezNo ratings yet
- Neacsu Aurelia EssayDocument3 pagesNeacsu Aurelia EssaySimona NeacsuNo ratings yet
- SahodayaQP Psychology Set1 Term2Document3 pagesSahodayaQP Psychology Set1 Term2Nishtha JainNo ratings yet
- Update On Antimicrobial Therapy in Management of Acute Odontogenic Infection in Oral and Maxillofacial SurgeryDocument9 pagesUpdate On Antimicrobial Therapy in Management of Acute Odontogenic Infection in Oral and Maxillofacial SurgeryMARISOL GALLEGO DUQUENo ratings yet
- Management of Portal Hypertension in Children: Ahmed Mahmoud El-Tawil, MSC, MRCS, PHDDocument9 pagesManagement of Portal Hypertension in Children: Ahmed Mahmoud El-Tawil, MSC, MRCS, PHDNulul Ci LoolyNo ratings yet
- Narazo v. ECC, February 6, 1990Document6 pagesNarazo v. ECC, February 6, 1990bentley CobyNo ratings yet
- Do Vaccinations Cause Autism?Document3 pagesDo Vaccinations Cause Autism?Josh BarberaNo ratings yet
- Blue FrontDocument18 pagesBlue FrontArshmeet Singh PanesarNo ratings yet
- GrieDocument410 pagesGrieamravati_hospital8No ratings yet
- Charlie Gard Ethics, Conflict and Medical Treatment For ChildrenDocument15 pagesCharlie Gard Ethics, Conflict and Medical Treatment For ChildrenNurudeen AdesinaNo ratings yet
- IvpDocument18 pagesIvpFranz SalazarNo ratings yet
- History of Arbovirology: Memories From The Field: Nikos Vasilakis Laura D. Kramer EditorsDocument552 pagesHistory of Arbovirology: Memories From The Field: Nikos Vasilakis Laura D. Kramer Editorsjulio castilloNo ratings yet
- Trimethylamine N-Oxide: The Good, The Bad and The Unknown: Health Sciences Research CommonsDocument12 pagesTrimethylamine N-Oxide: The Good, The Bad and The Unknown: Health Sciences Research CommonsVeneta GizdakovaNo ratings yet
- Early Initiation MV 2017 - DR - TrisnaDocument34 pagesEarly Initiation MV 2017 - DR - TrisnaHappy ShalalaNo ratings yet
- Kode ICD 10 THTDocument11 pagesKode ICD 10 THTFirman ZakyNo ratings yet
- s40880 018 0280 5 PDFDocument7 pagess40880 018 0280 5 PDFzoehdiismailNo ratings yet
- Science Wonders: Grade 3Document97 pagesScience Wonders: Grade 3sam efraim LegnisNo ratings yet
- Logbook GIDocument15 pagesLogbook GIAna BorodinaNo ratings yet
- Difference Between Bacteria and VirusDocument11 pagesDifference Between Bacteria and VirusSakib Rahman DiptoNo ratings yet
- Get The Facts About COVID-19 Vaccines - Mayo ClinicDocument10 pagesGet The Facts About COVID-19 Vaccines - Mayo ClinicLuna BellatrixNo ratings yet
- Vet Radiology Ultrasound - 2023 - MacLeod - Ultrasonographic Appearance of Gallbladder Neoplasia in 14 Dogs and 1 CatDocument9 pagesVet Radiology Ultrasound - 2023 - MacLeod - Ultrasonographic Appearance of Gallbladder Neoplasia in 14 Dogs and 1 CatnerakyokNo ratings yet