Professional Documents
Culture Documents
Dispensing2 Lab - Therapeutic Incompatibilities
Uploaded by
Alyssa Erika AzoresOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Dispensing2 Lab - Therapeutic Incompatibilities
Uploaded by
Alyssa Erika AzoresCopyright:
Available Formats
Dispensing II
PHA 6130 | BATCH 2022
FACULTY OF PHARMACY – UNIVERSITY OF SANTO TOMAS
LECTURERS: Ms. Marri Jmelou Roldan, RPh, MSc.
Ms. Michaella Odonio, RPh, MSc.
TRANSRIBED BY: Azores, 3FPH
Therapeutic Incompatibilities
REFERENCES: PPT, Lecture Video
THERAPEUTIC INCOMPATIBILITIES
• Includes drug interactions which occur at the site of
action Degree of dilution i
• Potentiation of therapeutic interactions between 2 or • generally, the more diluted the drugs are in a
more ingredients. solution, the less chance there is for an ion
• Destruction of effectiveness of one or more interaction leading to incompatibility.
ingredients. • In administering LVPs, hindi pa dapat siya puno. You
o Counteracts or cancels the effect of another have to observe if the drug is somehow consumed
drug/ingredient already, before refilling it to prevent over dilution.
• Occurrence of toxic manifestations within the
patient. (worst condition, can lead to toxicity) Length of time in solution i
• • incompatibility increases with the length of time that
drugs are in contact with each other.
IV DRUG COMPATIBILITY
• Physicochemical incompatibility (PCI) between drugs Order of mixing i
infused together is frequent, but under-recognized. • Ex.: Calcium phosphate, should not be added
• PCI can lead to consecutively when an IV admixture is being
o drug inactivity (therapeutic failure) prepared.
o catheter occlusion • This keeps these substances from pooling or forming
▪ usually occurs in the bloodstream due to a layer on top of the IV fluid, decreasing the chance
crystallization of incomp.
o embolism due to crystallization and separation • Thorough mixing after each addition is essential
o inflammatory reactions
o Tissue irritation due to pH change Other Examples i
o Damage from toxic products 1. Amphotericin B, cisplatin and metronidazole must be
o Death protected from light.
▪ Some tend to neglect the possibility of o Dextrose bottles are not light resistant. In some
precipitation when preparing IV admixtures patients receiving LVP, it is wrapped in
and that can actually lead to embolism aluminum foil.
which is fatal to the patient 2. Cefazolin is stable at room temperature for 24 hours
• Tools proposed to reduce the frequency of PCI and 14 days if refrigerated.
include: 3. Up to 10 mEq of Calcium can be added to each lite of
o compatibility cross-tables TPN containing 20 mEq of PO4
o labeling of drugs with extreme pH 4. Bactrim 5mL/75mL D5W stable for 2 hours, whereas
o optimized administration schedules. 5mL/125mL D5W is stable for 6 hours.
▪ Excessive contact time with the drug (e.g., 5. Amino acid composition and concentration in TPN
Large volume parenterals [LVP]) can lead to
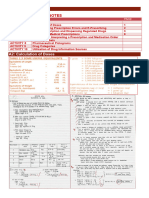
incompatibility EXAMPLE OF A COMPATIBILITY TABLE
FACTORS AFFECTING IV COMPATIBILITY
pH i
• incompatibility is more likely to occur when the
components of an IV solution differ significantly in pH.
Explained by chemical reaction between an acid and
a base, which yields a salt and water; the salt may
form an insoluble ppt.
• can also indicate stability of drug
• most drugs are only stable at a certain pH, once there
is a change in pH problems may occur (e.g.,
insolubility and instability)
Temperature i
• increased storage temperature speeds up drug
degradation. To preserve drug stability, drugs should
be stored in a refrigerator or freezer as appropriate.
DISPENSING2 LAB| THERAPEUTIC INCOMPATIBILITIES 1|AZORES
WAYS TO MINIMIZE OR PREVENT IV INCOMPATIBILITIES CORRECTION OF INCOMPATIBILITIES
1. Mix thoroughly when a drug is added to the • consult the physician
preparation. o Regarding modification / alteration of the
o Ex. Dissolve in the solution completely prescription
2. Minimize the number of drugs mixed together in an IV o Whenever you call the attention of the doctor,
solution. you should also have an evidence about the
o The lesser the number of drugs mixed in IV fluid, problems in the prescription and a
the lesser the chance of having an recommendation which is evidence-based as
incompatibility well.
3. Use freshly prepared solutions for compounding. • use pharmaceutical knowledge
4. Always verify correct diluent, IV fluid. Drug, and final • add an ingredient
concentration before compounding. o e.g., using superimposition, +inert ingredient to
5. Order of mixing additives affects the compatibility absorb the water
(e.g. add PO4 last to TPN). • remove an ingredient
6. Solutions should be administered promptly after o Act of omission; If the ingredient does not have
mixing or within the stability window so that the any or has less therapeutic value in the
occurrence of potential reaction can be minimized. prescription
7. Always refer to compatibility references. • change the vehicle
8. Always visually inspect final product after o If you notice that the active ingredient is organic
compounding for integrity, leaks, solution, and the vehicle is inorganic/aqueous in nature
cloudiness, particulates, color, and proper then we can change the vehicle or do post-
preparation. solvency system
o Check for clarity • change an ingredient
9. Ensure proper labeling of final IV product with beyond o Ex. If your vehicle is water and you are using an
use date and time. alkaloid, you can change the free form of the
alkaloid to its salt form to increase its solubility.
PARENTERAL NUTRITION (PN) • change the dosage form
FACTORS FOR INCOMPATIBILITIES WITH PARENTERAL o We usually change the solution into a suspension,
NUTRITION because solutions tend to precipitate unlike
1. Precipitation of Calcium and Phosphate suspensions
2. Creaming/ cracking of the liquid emulsion
• read the literature
3. Addition/ simultaneous application of drugs to/ with
PN.
PREVENTING OR MINIMIZING INCOMPATIBILITIES
• Each drug should be mixed thoroughly after it is added
CRITERIA FOR DRUG COMMONLY ADDED TO PN to the preparation
ADMIXTURES (e.g., INSULIN, HEPARIN, AND FAMOTIDINE)
• Solutions should be administered promptly after they
1. Stable dosage regimen over 24 hours
are mixed to minimize the time available for a
o PN & IVF are usually given for 24 hours
potential reaction to occur
2. Pharmacokinetic profile supporting 24-hour infusion
o Especially if the product has a delayed
3. Stable PN solution infusion rate
incompatibility
4. Documented chemical and physical stability over 24
hours • The number of drugs mixed together in an IV solution
should be kept to a minimum
HOW TO AVOID INCOMPATIBILITIES WITH PN? • If a Rx calls for unfamiliar drugs or IV fluids,
1. Never use PN for electrolyte therapy compatibility references should be consulted
o Remember that PN is different from IVF o Drugs.com - to check for drug incompatibilities
2. Be familiar with manufacturer’s recommendation
o Read manual / insert
3. Add divalent cations (calcium and magnesium) and
phosphate as organic bound salts (e.g. gluconate)
4. Do not add drugs or Iron to PN
5. May piggy back lipids separately
o In administering lipids, use piggy back
6. Avoid Y-site administration of drugs with PN
DISPENSING2 LAB | THERAPEUTIC INCOMPATIBILITIES 2|AZORES
You might also like
- Dispensing TechniquesDocument31 pagesDispensing TechniquesCesly Jewel Acosta AvilesNo ratings yet
- Lesson 1 Prescription and Medication OrderDocument30 pagesLesson 1 Prescription and Medication OrderAngelica GomezNo ratings yet
- Dispensing Lecture Reviewer - MidtermDocument26 pagesDispensing Lecture Reviewer - Midtermapi-306968266No ratings yet
- C-6 Powders and GranulesDocument6 pagesC-6 Powders and GranulesAli Uy50% (2)
- Activity 1 DDS LABDocument96 pagesActivity 1 DDS LABChristine RanoaNo ratings yet
- Monophasic Liquid Formulation OptimizationDocument25 pagesMonophasic Liquid Formulation OptimizationAamir KhanNo ratings yet
- Standard Patient Counseling ScriptDocument22 pagesStandard Patient Counseling ScriptElleason Joshua G. FranciscoNo ratings yet
- SolderDocument11 pagesSolderahmedNo ratings yet
- IncompatibilitiesDocument59 pagesIncompatibilitiesabdullah2020No ratings yet
- RPh's Guide to Drug IncompatibilitiesDocument27 pagesRPh's Guide to Drug IncompatibilitiesArk Olfato Parojinog100% (1)
- Prescription and Medication SafetyDocument156 pagesPrescription and Medication SafetyJonille EchevarriaNo ratings yet
- Pharmaceutical Labeling RequirementsDocument31 pagesPharmaceutical Labeling RequirementsJosa Camille BungayNo ratings yet
- Dispensing2 Lab - RX 7-12Document3 pagesDispensing2 Lab - RX 7-12Alyssa Erika AzoresNo ratings yet
- Effervescent Granules Lab ManualDocument2 pagesEffervescent Granules Lab Manuallalag yanNo ratings yet
- 03 Solutions PDFDocument77 pages03 Solutions PDFIra MoranteNo ratings yet
- Dispensing and Medication CounselingDocument12 pagesDispensing and Medication CounselingLei100% (3)
- Clinical Toxicology GuideDocument70 pagesClinical Toxicology GuideJerson Aizpuro SuplementoNo ratings yet
- Preparation # I. Objectives:: Pharmaceutical Dosage Forms Laboratory ManualDocument2 pagesPreparation # I. Objectives:: Pharmaceutical Dosage Forms Laboratory Manuallalag yanNo ratings yet
- Dosage - Chapter 14Document57 pagesDosage - Chapter 14Kim Manlangit100% (1)
- Pharmaceutical Analysis 2 - Introduction RevisedDocument78 pagesPharmaceutical Analysis 2 - Introduction RevisedJesse'Lee CardosoNo ratings yet
- IV Drug IncompatibilitiesDocument29 pagesIV Drug IncompatibilitiesMichael Freudiger100% (2)
- Drug incompatibilities guide for pharmacistsDocument45 pagesDrug incompatibilities guide for pharmacistsANKUR JAIN100% (1)
- The PrescriptionDocument86 pagesThe PrescriptionChristine Arrabis100% (3)
- Dispensing Post LabDocument3 pagesDispensing Post LabYanni Bryan RegaladoNo ratings yet
- Dr. Derm CatalogDocument20 pagesDr. Derm CatalogCosmetics Bulgaria100% (1)
- DDS FINALS Compiled ReviewerDocument21 pagesDDS FINALS Compiled ReviewerChantelle Mea100% (1)
- Social and Administrative PharmacyDocument5 pagesSocial and Administrative PharmacyGrace Marino100% (1)
- 4-Drug Delivery Systems (Autosaved)Document41 pages4-Drug Delivery Systems (Autosaved)Chelle PaloNo ratings yet
- Cs & Las Impact Req - Asme Sec Viii Div 2Document16 pagesCs & Las Impact Req - Asme Sec Viii Div 2AmitNarayanNitnawareNo ratings yet
- Drug Delivery System - AnswerDocument14 pagesDrug Delivery System - AnswerFred100% (1)
- Boiler Water Treatment: Thermax Limited Chemical DivisionDocument53 pagesBoiler Water Treatment: Thermax Limited Chemical Divisionkcp1986100% (2)
- Slide 9 Patient Counseling and Other Special Considerations in CounselingDocument22 pagesSlide 9 Patient Counseling and Other Special Considerations in CounselingJean GanubNo ratings yet
- Post Lab Qc1 2019Document42 pagesPost Lab Qc1 2019Frances SaludNo ratings yet
- (Dispensing 1 Laboratory) Review NotesDocument12 pages(Dispensing 1 Laboratory) Review NotesZen HeartNo ratings yet
- Chapter 3: Atomic and Ionic Arrangements: 3-1 SolutionDocument52 pagesChapter 3: Atomic and Ionic Arrangements: 3-1 SolutionMarcos Jose100% (1)
- Pha6111 Dispensing Lab Customer Service PDFDocument5 pagesPha6111 Dispensing Lab Customer Service PDFKATHLEEN CALALANGNo ratings yet
- Magnetic PropertiesDocument29 pagesMagnetic PropertiesSiyan ShivaNo ratings yet
- PH-PHR212 Lecture 2 FS2021 PDFDocument57 pagesPH-PHR212 Lecture 2 FS2021 PDFIra MoranteNo ratings yet
- Pharmaceutical Care Principles for Improving Patient HealthDocument9 pagesPharmaceutical Care Principles for Improving Patient HealthJesza IgnacioNo ratings yet
- UST Hospital Prescriptions SummaryDocument5 pagesUST Hospital Prescriptions SummaryMich Tolentino100% (1)
- Pharmacy Informatics Laboratory Activity 14Document1 pagePharmacy Informatics Laboratory Activity 14April Mergelle LapuzNo ratings yet
- DISPLABPreps1 20 2Document21 pagesDISPLABPreps1 20 2Alexa Joy C. InguilloNo ratings yet
- In Komp A Tibi LitasDocument54 pagesIn Komp A Tibi LitasHifi Rizki.RNo ratings yet
- DISPENSING 1 - Module 1Document68 pagesDISPENSING 1 - Module 1Precious Faith SabalaNo ratings yet
- Activity 7 DISPENSING PRICE With AnswersDocument3 pagesActivity 7 DISPENSING PRICE With AnswersChristine DelmendoNo ratings yet
- Internship 5 7 BSPHDocument59 pagesInternship 5 7 BSPHJaica Mangurali TumulakNo ratings yet
- Physicochemical IncompatibilitiesDocument20 pagesPhysicochemical Incompatibilitiesvicbart11No ratings yet
- Understanding Dispensing PharmacyDocument67 pagesUnderstanding Dispensing Pharmacyneha_dand15910% (1)
- Pharm. Chem. - 2 Lab Exp No 5Document3 pagesPharm. Chem. - 2 Lab Exp No 5davenNo ratings yet
- Prelim HospiDocument63 pagesPrelim Hospi;'SiLeNt';No ratings yet
- Preparation No. "17" "Liquid Petrolatum Emulsion" A. Wrap-Up Guide QuestionsDocument5 pagesPreparation No. "17" "Liquid Petrolatum Emulsion" A. Wrap-Up Guide QuestionsMEDELYN KEITH ESTANISLAONo ratings yet
- Chocolate Syrup GuideDocument3 pagesChocolate Syrup GuideMikaela LaoNo ratings yet
- GROUP 1 Prep-14 Data SheetDocument2 pagesGROUP 1 Prep-14 Data SheetTrisha ArgaoNo ratings yet
- Preventing Dispensing ErrorsDocument39 pagesPreventing Dispensing ErrorsMark RevertNo ratings yet
- Pharmaceutical Dosage Froms and Drug Delivery SystemsDocument14 pagesPharmaceutical Dosage Froms and Drug Delivery SystemsChantelle MeaNo ratings yet
- 14 Disperse Systems With AnswersDocument5 pages14 Disperse Systems With AnswersPatricia Camryne Ambida100% (2)
- Chapter 6 QC2 PDFDocument5 pagesChapter 6 QC2 PDFAnalizaNo ratings yet
- DdsDocument9 pagesDdsClaudette JunioNo ratings yet
- 25 Rodriguez - Chapter 15-17Document9 pages25 Rodriguez - Chapter 15-17JANNIE BELLE RODRIGUEZNo ratings yet
- 1 Herbs and Health ProductsDocument29 pages1 Herbs and Health ProductsanavyaledzurcNo ratings yet
- FormularyDocument32 pagesFormularyAnonymous U4JLHU9e3100% (1)
- Community Pharmacy Intern Exercises5-9Document6 pagesCommunity Pharmacy Intern Exercises5-9Joslin RozNo ratings yet
- Data 568320Document1 pageData 568320Waqas AhmadNo ratings yet
- Shishuvan - STD 7 (2021-22) - IntegersDocument10 pagesShishuvan - STD 7 (2021-22) - IntegersHardik ViraNo ratings yet
- Material Test CertificateDocument2 pagesMaterial Test CertificatesatishNo ratings yet
- Carbonyls, Carboxylic Acid and ChiralityDocument23 pagesCarbonyls, Carboxylic Acid and ChiralityAyshath MaaishaNo ratings yet
- Us3479310 PDFDocument7 pagesUs3479310 PDFKhoi Nguyen DangNo ratings yet
- Sop of Aqu - ExtractionDocument5 pagesSop of Aqu - ExtractioneyobNo ratings yet
- App3Document2 pagesApp3hamidrezaee008No ratings yet
- RRLDocument3 pagesRRLArianne Rose TalledoNo ratings yet
- Module 1 Unit 1Document12 pagesModule 1 Unit 1Mia Lorena JandocNo ratings yet
- Guide To Detergents and Removal PropertiesDocument20 pagesGuide To Detergents and Removal PropertiesalexNo ratings yet
- SS - AIATS - 01 (Adv) - P - 1 - A - 2020-06-21 - 2020 - QDocument23 pagesSS - AIATS - 01 (Adv) - P - 1 - A - 2020-06-21 - 2020 - Qyash chawliyaNo ratings yet
- Mathematical Modeling of Corrosion Phenomenon in Pipelines-1553491748Document10 pagesMathematical Modeling of Corrosion Phenomenon in Pipelines-1553491748Jorge LunaNo ratings yet
- Numerical Analysis of Reinforced Concrete Beam Column Joint Retrofitted Using Carbon Fiber Reinforced Polymer SheetsDocument10 pagesNumerical Analysis of Reinforced Concrete Beam Column Joint Retrofitted Using Carbon Fiber Reinforced Polymer Sheetsseena jalalNo ratings yet
- Sizing and Design of Utilities For Chemical ProcessDocument13 pagesSizing and Design of Utilities For Chemical Processpavanchem610% (1)
- Organic Chemistry Test QuestionsDocument4 pagesOrganic Chemistry Test QuestionsAbaring KathrynaNo ratings yet
- NCERT Solutions For Class 12 Chemistry Chapter 4 Chemical KineticsDocument31 pagesNCERT Solutions For Class 12 Chemistry Chapter 4 Chemical KineticsGourav ARNo ratings yet
- Gear Beam and Wear StrengthDocument46 pagesGear Beam and Wear StrengthNisarg MistryNo ratings yet
- Ideal Gas and Rankine CycleDocument12 pagesIdeal Gas and Rankine CycleAkshay A KumarNo ratings yet
- Study Rate: Chemistry Notes For Class 12 Chapter 14 BiomoleculesDocument21 pagesStudy Rate: Chemistry Notes For Class 12 Chapter 14 BiomoleculesYASH SONARNo ratings yet
- Chem 59-250: Molecular Orbital TheoryDocument25 pagesChem 59-250: Molecular Orbital TheoryNuansak3No ratings yet
- A Type-Curve Matching Procedure For Material Balance Analysis of Production Data From Geopressured Gas Reservoirs A.K. AmbasthaDocument6 pagesA Type-Curve Matching Procedure For Material Balance Analysis of Production Data From Geopressured Gas Reservoirs A.K. AmbasthaAnderson JimenezNo ratings yet
- Science: Quarter 3 - Module 1: The Particle Nature of MatterDocument20 pagesScience: Quarter 3 - Module 1: The Particle Nature of MatterFernadez RodisonNo ratings yet
- Super Kit ManualDocument22 pagesSuper Kit ManualFabiana ChusitNo ratings yet
- Microscopy REMOTE Quiz QuestionsDocument2 pagesMicroscopy REMOTE Quiz QuestionsadamNo ratings yet