Professional Documents
Culture Documents
Supracondylar Fractures of The Humerus in Children.3
Uploaded by
Azmi FarhadiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Supracondylar Fractures of The Humerus in Children.3
Uploaded by
Azmi FarhadiCopyright:
Available Formats
Supracondylar Fractures of the Humerus in Children
Norman Y. Otsuka, MD, and James R. Kasser, MD
Abstract
The treatment of type II and type III supracondylar fractures of the humerus in medial displacement of the distal
Downloaded from http://journals.lww.com/jaaos by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC4/OAVpDDa8KKGKV0Ymy+78= on 08/21/2021
children with closed reduction and percutaneous pinning has dramatically low- humerus; a lateral periosteal hinge
ered the rate of complications from this injury. The incidence rates of malunion is intact with lateral displacement.
(cubitus varus) and compartment syndrome have both decreased. Nerve injury
accompanying this type of fracture (prevalence, 5% to 19%) is usually a neura-
praxia, which should be managed conservatively. Vascular insufficiency at pre- Physical Examination
sentation (prevalence, 5% to 17%) should be managed initially by rapid closed
reduction and pinning without arteriography. Persistent vascular insufficiency The initial evaluation of the child
necessitates exploration and vascular reconstruction. with an elbow injury must include
J Am Acad Orthop Surg 1997;5:19-26 an overall assessment to rule out
associated trauma. Fractures of the
midshaft of the ipsilateral humerus
are uncommon, but distal forearm
Supracondylar fracture of the sion or flexion injuries. The exten- fractures are common; both injuries
humerus is a common elbow injury sion type is the most common, may be overlooked if attention is
in children. Two thirds of all hospi- accounting for 90% to 98% of cases. focused solely on the elbow.
talizations for elbow injuries in chil- It is caused by a fall on an out- The elbow with a supracondylar
dren are for supracondylar frac- stretched hand with the elbow fracture is characterized by swell-
tures,1 but the incidence of supra- hyperextended.6 The characteristic ing and deformity. With type III
condylar fractures has yet to be docu- displacement of the distal humeral fractures, an S-shaped deformity of
mented. In his review of 8,672 pedi- fragment in extension-type injuries the elbow develops due to angula-
atric fractures, Landin2 found that has been reported to be posterome- tion and translation of the fracture
supracondylar fractures accounted dial in 90% of cases and posterolat- fragments. A thorough neurovas-
for only 3.3%. Supracondylar frac- eral in 10%.7 In our study,8 49% of cular examination of the involved
tures are most common in children the supracondylar fractures were
aged less than 10 years, with a peak displaced posterolaterally. The
incidence between ages 5 and 8 flexion-type fracture, which is
years.3 These fractures often require caused by falling on a flexed Dr. Otsuka is Assistant Professor of
surgery and historically are associat- elbow, is a rare occurrence. Orthopaedic Surgery, University of California,
ed with significant morbidity due to There have been numerous San Francisco (UCSF), and Chief, Pediatric
Orthopaedic Service, UCSF Medical Center.
malunion, neurovascular complica- attempts in the literature to classify
Dr. Kasser is Associate Professor of
tions, and compartment syndrome.4,5 supracondylar fractures. Gartland’s Orthopaedic Surgery, Harvard Medical School,
As a result, controversy still exists as classification9 is simple and widely and Orthopaedic Surgeon-in-Chief, Depart-
to what constitutes optimal manage- used. In that system, type I frac- ment of Orthopaedic Surgery, Children’s
ment of this type of fracture and its tures are nondisplaced. Type II Hospital, Boston.
complications. fractures are displaced with a vari-
Reprint requests: Dr. Kasser, Department of
able amount of angulation, but the
Orthopaedic Surgery, Children’s Hospital, 300
posterior cortex of the humerus is Longwood Avenue, Boston, MA 02115.
Classification intact. Type III fractures are com-
pletely displaced with no cortical Copyright 1997 by the American Academy of
Supracondylar fractures of the contact. A medial periosteal hinge Orthopaedic Surgeons.
humerus are categorized as exten- is intact in type III fractures with
Vol 5, No 1, January/February 1997 19
Supracondylar Fractures of the Humerus in Children
upper extremity is mandatory view. Oblique views may be neces-
because this fracture is associated sary to visualize minimally dis- A
with neurovascular injuries, with a placed fractures. The fat-pad sign,
reported incidence of 11% to 49%.8 which is representative of an intra-
In the initial assessment, particu- articular effusion, will be seen on
lar attention should be paid to radial the lateral view of a minimally dis-
nerve function. Posteromedial dis- placed supracondylar fracture.
α
placement of the fracture is associ- On the lateral view of a normal
ated with median and anterior elbow, the ossification center of the
interosseous nerve dysfunction; capitellum is partially transected
posterolateral displacement is asso- by a line drawn along the anterior B
90°-α
ciated with brachial artery injury.8 aspect of the humerus (the “anteri-
It is important to document the ini- or humeral line”). In a type I frac-
tial neurovascular examination as a ture, this relationship persists, as
baseline for comparison before any neither significant translation nor
treatment is instituted and to iden- angulation exists (Fig. 1, A). The
tify any subsequent deterioration of lateral view of a type II fracture
the neurovascular status. shows an anterior humeral line that
At the end of the clinical assess- does not transect the capitellum, Fig. 2 Baumann’s angle is a radiographic
ment, the injured elbow should be and there is an intact but plastically angle demonstrated on an anteroposterior
immobilized with a splint in a posi- deformed posterior cortex (Fig. 1, view of the elbow. This angle is created by
the intersection of a line drawn down the
tion of 20 to 30 degrees of flexion to B). In a type III fracture, the distal humeral axis (A) and a line drawn along
prevent further displacement of the fragment is totally displaced, and the growth plate of the lateral condyle of
fracture and additional neurovas- the proximal fragment may be seen the elbow (B). This angle is useful in deter-
mining the adequacy of reduction.
cular damage. Splinting in full to penetrate through the brachialis
elbow extension is to be avoided muscle (Fig. 1, C).
because it stretches the neurovas- On the AP view, Baumann’s
cular bundle over the distal tip of angle is an important landmark for the contralateral elbow should be
the proximal fragment. the assessment of supracondylar used for comparison. The distal
fractures. This angle, created by the fracture fragment is often rotated
intersection of a line drawn down medially or internally and into
Radiographic Examination the humeral axis and a line drawn varus deviation in relation to the
along the growth plate of the lateral proximal humerus, which produces
The radiographic examination of condyle of the elbow, maintains a an increase in Baumann’s angle.10
the injured elbow must include an constant relation with the carrying Some authors do not advocate
anteroposterior (AP) and a lateral angle (Fig. 2). Baumann’s angle of use of Baumann’s angle because of
A B C
Fig. 1 A, Type I supracondylar humeral fracture. Solid arrow defines the fracture line. The anterior humeral line partially transects the
capitellum, and there is a posterior fat-pad sign (open arrow). B, Type II supracondylar fracture with an intact posterior cortex (arrow).
C, Type III supracondylar fracture with a totally displaced distal humeral fragment.
20 Journal of the American Academy of Orthopaedic Surgeons
Norman Y. Otsuka, MD, and James R. Kasser, MD
the difficulty of identifying the degree of soft-tissue swelling, but required to maintain reduction.
capitellar growth plate. An alter- this usually is not necessary. A radio- After reduction and immobiliza-
native to Baumann’s angle, the graph should be taken 1 week after tion, patients should be observed in
medial epicondylar epiphyseal injury to be sure that displacement the hospital overnight for swelling
angle, has recently been described has not occurred, which usually is and circulatory changes. Casting
as a means of evaluating supra- evidenced by an increase in varus should be maintained for 3 weeks,
condylar fractures.11 This angle is angulation. After 3 weeks of immo- after which protected active range-
created by the intersection of a line bilization, protected active range-of- of-motion exercises can be begun.
drawn down the humeral axis and motion elbow exercises may be Maintenance of hyperflexion in a
a line drawn along the medial epi- started. Usually, no further treat- circular cast carries a high risk of
condylar epiphyseal plate. ment or observation is necessary for compartment syndrome. Therefore,
Both Baumann’s angle and the these nondisplaced fractures. we believe these fractures should be
medial epicondylar epiphyseal pinned percutaneously if there is
angle are also useful in determin- Type II Fractures significant swelling, if there is inad-
ing the adequacy of reduction of Type II fractures are angulated equate circulation when the elbow
supracondylar fractures. In prac- but not translated, because the pos- is flexed, or if the fracture might
tice, we use three criteria to deter- terior cortex remains intact. Reduc- become unstable. Potentially unsta-
mine the adequacy of reduction: tion can be achieved by flexion of ble type II fractures are those with a
(1) Baumann’s angle, (2) the rela- the elbow and pronation of the possible fracture of the posterior
tionship of the capitellum to the forearm with the patient under cortex, especially when rotational
anterior humeral line, and (3) anesthesia. Rang described the use deformity is present. Two lateral
restoration of the anatomy of the of a figure-of-eight cast for immo- pins, rather than crossed pins, may
olecranon fossa. In radiographic bilization in hyperflexion and be used to decrease the risk of ulnar
evaluation of type I fractures treat- pronation without encircling the nerve injury by the medial pin (Fig.
ed in a cast, we have found that the elbow in plaster. 1 Millis et al 12 3). The use of two lateral pins is less
best films are obtained by using a showed that flexion of the elbow secure than the use of two crossed
fiberglass cast and ordering an AP by more than 120 degrees was pins.13 If two lateral pins are used,
view of the distal humerus rather
than an AP view of the elbow.
Treatment
We believe the treatment of choice
for displaced supracondylar frac-
tures is closed reduction and percu-
taneous pinning. Nondisplaced
(type I) fractures may be managed
in a cast or splint. Traction is useful
when supracondylar comminution
is present.
Type I Fractures
Type I fractures are nondisplaced
and are not associated with neu-
rovascular injury. These fractures
can be treated with immobilization
in a splint or circular cast with the
elbow flexed to 90 degrees and the
forearm in neutral position. A B
Children may be admitted to the Fig. 3 Anteroposterior (A) and lateral (B) views of a supracondylar humeral fracture
hospital for observation and eleva- pinned with two lateral percutaneous Kirschner wires placed parallel to each other.
tion of the arm, depending on the
Vol 5, No 1, January/February 1997 21
Supracondylar Fractures of the Humerus in Children
they should be placed either parallel ing this fracture. Patients should be
to each other or crossing well above observed in the hospital after this
the fracture line. If swelling of the injury to monitor neurovascular sta-
elbow does not allow reduction, tus.
traction can be used until swelling
has decreased enough that reduc- Closed Reduction
tion can be attempted. In general, Accurate reduction of the frac-
traction is not required. ture is important in the prevention
of cubitus varus deformity. Under
Type III Fractures fluoroscopic control, traction is first
Type III fractures are the result of applied to disengage the proximal
more severe injuries and are associ- fragment from the brachialis mus-
ated with greater soft-tissue damage cle. The distal fragment must then
and swelling, difficult reduction, be translated into proper medial-to-
compartment syndromes, and neu- lateral orientation relative to the
rovascular injuries. These fractures shaft. The internal rotation deformi-
are completely displaced with most ty is then corrected. Next, with the
of the periosteum torn, and there is examiner’s thumb over the olecra-
significant risk of injury to the non, the distal fragment is pushed
brachialis muscle and neurovascu- forward while flexing the patient’s
lar bundle. Residual deformity is elbow to 120 degrees and pronating
Fig. 5 After traction and centralization,
also a potential problem. The inci- the wrist to tighten the periosteal the distal fragment is reduced by direct
dence of cubitus varus (Fig. 4) has hinge (Fig. 5). In the posterolateral pressure over the olecranon as the elbow is
been reported to be as high as 58%.7 fracture, the wrist is supinated to flexed.
Closed reduction and cast immobi- tighten the lateral periosteal hinge.
lization should not be used in treat- The reduction is then checked on
AP and lateral views with the use of
fluoroscopy. The fracture is gener- down the ulna) is a more accurate
ally stable in external rotation, means of assessing the adequacy of
which allows a lateral view of the reduction. Because the position of
elbow to be obtained by externally the reduced distal humerus is usu-
rotating the shoulder while holding ally evaluated with the elbow
the elbow in hyperflexion. flexed, we have not found this
The adequacy of reduction in view to be particularly helpful.
the coronal plane can be assessed Lagrange and Rigault15 and Conn
with Jones views of the distal and Wade16 described the “crescent
humerus with the hyperflexed sign” (overlapping of the ossifica-
elbow in slight internal and exter- tion centers of the lateral condyle
nal rotation. These views can be and the olecranon) on the lateral
difficult to evaluate, however, view as an indicator of inadequate
because of imposition of the proxi- reduction, but we have found that
mal radius and ulna. As described Baumann’s angle, the relationship
previously, Baumann’s angle and of the capitellum to the anterior
the medial epicondylar epiphyseal humeral line, and restoration of the
angle are useful ways to assess normal anatomy of the olecranon
reduction. A deviation of more fossa are the best indicators of an
than 5 degrees relative to the acceptable reduction.
Baumann’s angle measured in the
noninjured extremity represents an Percutaneous Pinning
inadequate reduction.1 Webb and After anatomic reduction, percu-
Fig. 4 Child with cubitus varus deformity
of the elbow after a supracondylar humeral
Sherman14 report that the humero- taneous pinning of the elbow can
fracture. ulnar angle (the angle between the be performed with use of the ster-
midhumeral line and a line drawn ilely draped screen of the fluo-
22 Journal of the American Academy of Orthopaedic Surgeons
Norman Y. Otsuka, MD, and James R. Kasser, MD
roscopy (C-arm) unit as the operat- the distal humeral physis. The posi- Traction
ing surface. The distal fracture tion of the wire should be checked Traction has lost popularity as
fragment is usually stable in 120 fluoroscopically on AP and lateral percutaneous pinning of supra-
degrees of flexion in pronation, and views. For the lateral view, the arm condylar fractures has gained
the arm can be moved from neutral can be externally rotated at the broad acceptance. However, trac-
to external rotation so that imaging shoulder while flexion and prona- tion is a treatment option for the
of the elbow can be done in differ- tion of the elbow is maintained. severely swollen arm, the irre-
ent planes without moving the C The medial wire is placed with ducible or comminuted fracture,
arm. Slight internal and external the arm in 80 to 90 degrees of flex- and the fracture that cannot be
rotation of the arm will allow the ion; additional elbow flexion may pinned because of an associated
medial and lateral columns of the cause the ulnar nerve to subluxate skin disorder or a life-threatening
distal humerus to be visualized. volarward into the path of the condition. Traction necessitates
For comminuted fractures or frac- Kirschner wire. Because the lateral constant supervision and adjust-
tures that are unstable, crossed pin- wire provides sufficient stability, ment to prevent varus deformity.
ning with one lateral and one hyperflexion is no longer necessary. Our primary indication for trac-
medial pin is advised (Fig. 6). Two A medial incision is then made over tion is supracondylar comminution
lateral pins may be satisfactory if a the medial epicondyle. A hemostat (Fig. 7). Dunlop’s skin traction17 or
stable reduction has been achieved. is used to separate tissues down to modifications involving skeletal
Percutaneous pinning is per- the medial epicondyle to ensure traction have been described. A
formed with the maximally flexed that the ulnar nerve is not injured. variation of skeletal traction
and pronated arm resting on the An AO tissue protector can be used involves insertion of the Ormandy
sterile C-arm screen. The lateral to protect soft tissues. The position screw 18 or the Palmer winged
side is approached first. A smooth of the Kirschner wire should be screw19 into the ulna. Traction can
Kirschner wire is inserted through checked with the C arm before be applied overhead or in a side-
the lateral condyle, crossing just lat- insertion to ensure that it is piercing arm manner. We find that over-
eral to the olecranon fossa and the medial epicondyle and not the head traction with use of an olecra-
engaging the medial humeral cor- ulnar groove. The wire is then driv- non screw is the easiest to manage.
tex. A 0.062-mm wire is appropri- en up the medial column so that it Traction can be used with a short
ate for a small child aged less than 4 crosses the lateral wire proximal to arm cast if there is also a forearm
years; a 5/64-inch wire is appropri- the olecranon fossa. The medial fracture. Once swelling has re-
ate for an older child. The wire is wire is usually more transverse solved, the elbow can be placed in
passed through the capitellum and than the lateral wire. plaster, remanipulated, or pinned
The reduction and wire place- percutaneously.
ment should then be checked again Pirone et al 20 compared three
with the C arm. The wires are bent methods for treatment of supra-
and generally left protruding from condylar fractures: closed reduc-
the skin for easy removal in 3 tion with casting, skeletal traction,
weeks. Before the drapes are and closed reduction with percuta-
removed, the vascular status of the neous pin fixation. They found
arm should be checked. The elbow that the results for patients treated
is splinted in 60 to 90 degrees of with skeletal traction were equal to
flexion with the forearm in neutral those for patients treated with
rotation. A bivalve cast or splint is closed reduction with percuta-
applied, and the patient is admit- neous pinning.
ted for observation overnight.
The Kirschner wires are re- Indications for Open Reduction
moved without anesthesia in the The indications for open reduc-
office 3 to 4 weeks postoperatively tion of supracondylar fractures
Fig. 6 Supracondylar humeral fracture after healing of the fracture. include (1) a fracture that is irre-
that has been pinned with lateral and Physical therapy is generally not ducible by closed methods, (2) vas-
medial Kirschner wires. Note that the
medial wire enters through the medial epi-
required, as the child will regain cular compromise necessitating
condyle above the ulnar groove. full use of the elbow over the ensu- exploration and repair of the
ing 3 weeks. brachial artery, and (3) an open
Vol 5, No 1, January/February 1997 23
Supracondylar Fractures of the Humerus in Children
for a posterolaterally displaced lar fractures, Campbell et al8 found
fracture associated with vascular a median nerve deficit in 52% of
compromise or a median nerve cases and a radial nerve deficit in
deficit. In general, the most versa- 28%. A high frequency of median
tile approach is through an anterior nerve palsy was associated with
transverse incision over the antecu- posteromedial displacement of the
bital fossa, with extension of the distal fragment. Fortunately, most
medial side proximally and the lat- deficits that occur at the time of
eral side distally as needed. It is injury are neurapraxias.23 Motor
often the case that only the trans- function can take from 7 to 12 weeks
verse part of the incision is re- to return, but sensory recovery may
quired. Once reduction has been take more than 6 months.24 Culp et
achieved, fixation with crossed al25 found that if there was no clini-
Kirschner wires is recommended. cal or electromyographic evidence
A posterior approach may jeopar- of return of neural function 5
dize the blood supply to the distal months after injury, exploration and
humerus and is not indicated. neurolysis were indicated. If the
nerve was seen to be in continuity
Flexion-type Fractures intraoperatively, the prognosis for
Flexion-type supracondylar frac- neurolysis was excellent.
tures are very uncommon, reported- Early exploration is indicated
ly occurring in only 1% to 10% of all when there is an open injury over a
Fig. 7 Traction applied through an olecra- supracondylar injuries 1 (Fig. 8). nerve that is not functioning.
non wing screw can be valuable when
supracondylar comminution is present. Flexion-type fractures can be classi- Exploration is also indicated if
fied like extension-type fractures on nerve function becomes compro-
the basis of the degree of displace- mised after closed reduction of the
ment. The reduction maneuver for fracture.26
fracture requiring irrigation and type II and type III flexion fractures Nerve injury can also occur dur-
debridement. is opposite to that used for exten- ing pinning of supracondylar frac-
It is uncommon for a supra- sion-type fractures, and reduction is tures. In a retrospective review of
condylar fracture to be irreducible done in extension. The medial 143 supracondylar fractures, four
by closed methods. Elstrom et al21 periosteum may be disrupted, with cases of nerve palsy were identified
reported that in cases of entrapment a valgus component that requires a after percutaneous fixation.27 All
of the brachial artery and median varus moment to gain reduction. four nerve palsies were associated
nerve between the fracture frag- Pinning is necessary for most with a medial pin. Royce et al27
ments, attempts at closed reduction flexion-type fractures that require
resulted in vascular compromise. reduction, because casting the
Wilkins22 reported that buttonhol- elbow in extension is awkward.
ing of the proximal fracture frag- Pinning a flexion-type fracture
ment through the brachialis muscle must be done in extension. The C
can block reduction. When reduc- arm is rotated about the distal
tion cannot be obtained, one must humerus because the fracture will
always beware of entrapped neural not be stable in flexion.
or vascular structures. This occurs
most frequently in posterolaterally
displaced fractures. Complications
In general, the surgical approach
should be through the area of dis- Nerve Injuries
rupted periosteum. The neurovas- Nerve injuries associated with
cular deficit present should also be displaced supracondylar fractures
Fig. 8 In a flexion-type supracondylar
considered in planning the surgical are common, with reported preva- fracture, the distal fragment is displaced
approach. An anterior or antero- lences ranging from 5% to 19%. In a anteriorly.
medial approach should be used 1995 review of type III supracondy-
24 Journal of the American Academy of Orthopaedic Surgeons
Norman Y. Otsuka, MD, and James R. Kasser, MD
found that the rate of iatrogenic tracture is necessary. It should be recurrent deformity. Corrective
nerve injury after percutaneous recognized that the pain and signs osteotomy provided permanent
pinning was 2% to 3%. Nerve of compartment syndrome may be correction of the deformity in the
palsies without transection of the absent if the median nerve has been absence of growth arrest. A correc-
nerve should be treated conserva- injured, resulting in an anesthetic tive osteotomy for cubitus varus
tively; resolution will generally hand. 30 Mubarak and Carroll 31 deformity should be delayed until
occur within 6 months. have recommended that forearm at least 1 year after injury to evalu-
fasciotomy be performed if there ate the possible presence of medial
Arterial Injuries are clinical signs of compartment growth arrest.
The prevalence of vascular syndrome or if intracompartmental Cubitus valgus deformity does
insufficiency accompanying supra- pressure measurements are greater not occur as commonly as cubitus
condylar fractures has been report- than 30 mm Hg. varus and is not as well document-
ed to range from 5% to 12%. 28,29 ed in the literature. This deformity
Shaw et al29 recommend immediate Deformity causes functional loss of extension
closed reduction and Kirschner- Angular deformities of the distal and the development of a tardy
wire stabilization of fractures ac- humerus are common after supra- ulnar nerve paralysis.
companied by vascular insufficien- condylar fractures. The remodel-
cy. This treatment protocol result- ing potential of the distal humerus Stiffness and Myositis Ossificans
ed in restoration of pulse in 13 of is limited because the distal physis Loss of motion in the anatomi-
their 17 patients (12% of 143 type contributes only 20% of the growth cally reduced supracondylar frac-
III fractures). Arterial exploration of the humerus. Although remod- ture is uncommon. Significant loss
was performed in 3 patients who eling of posterior angulation can of flexion can occur after fractures
had an intact pulse preoperatively occur, angular deformities in the with posterior angulation of the
but no pulse after reduction; in coronal plane will not remodel, distal fragment. In a review of
each case, there was a discrete arte- resulting in a cubitus varus or cubi- supracondylar fractures in chil-
rial lesion at the level of the frac- tus valgus deformity. dren, Henrikson 3 reported that
ture. Shaw et al concluded that Cubitus varus deformity is pri- fewer than 5% were ultimately
preoperative arteriography would marily a cosmetic, rather than a associated with flexion or extension
not have contributed to the man- functional, disability. The deformi- loss exceeding 5 degrees as com-
agement of these injuries with ty is most apparent with full exten- pared with the noninjured side.
strong clinical signs suggestive of sion of the elbow. The primary in- Although extensive manipulation
vascular compromise. Their indi- dication for surgical correction is and physical therapy have been
cations for arterial exploration also cosmetic. The techniques for noted to incite myositis ossificans,
were (1) the absence of a palpable corrective osteotomy include lateral this complication is extremely rare.
pulse after reduction with any sug- closing-wedge osteotomy, dome
gestion of decreased capillary refill, rotational osteotomy, and step-cut
increased compartment pressure, lateral closing-wedge osteotomy. 1 Summary
or pallor, and (2) the total absence However, these osteotomies are
on Doppler imaging of a pulse in a associated with a significant com- Although supracondylar fractures
nonischemic extremity. They also plication rate. Labelle et al32 report- of the humerus are common in
asserted that delaying treatment of ed a loss of correction and/or nerve children, management of the injury
a pulseless extremity to obtain an injuries in 33% of their patients. and treatment of complications are
arteriogram before reduction and In a 1994 study, Voss et al 33 still controversial. Expedient man-
pinning is not warranted. found that the cubitus varus defor- agement of the fracture with reduc-
A dreaded complication of vas- mity was generally the result of tion and stabilization markedly
cular compromise or injury is malreduction, but disruption of decreases the incidence of neuro-
Volkmann’s ischemic contracture. medial growth was the cause in vascular complications. Anatomic
Ottolenghi 28 reported that this 11% of their patients with progres- reduction and Kirschner-wire fixa-
complication occurred in fewer sive deformity. If medial growth tion with special attention given to
than 1% of his 830 patients with arrest was present, these authors soft tissues and careful monitoring
supracondylar fractures. An suggested that a lateral epiphysi- of neurovascular function are key
aggressive surgical approach to odesis should accompany the to management of this injury in
prevent Volkmann’s ischemic con- osteotomy to reduce the risk of children.
Vol 5, No 1, January/February 1997 25
Supracondylar Fractures of the Humerus in Children
References
1. Wilkins KE: Fractures and disloca- Determination of medial epicondylar maturity of fifty-three patients treated
tions of the elbow region, in epiphyseal angle for supracondylar conservatively. J Bone Joint Surg Am
Rockwood CA Jr, Wilkins KE, King RE humeral fractures in children. J Pediatr 1986;68:333-344.
(eds): Fractures in Children, 3rd ed. Orthop 1993;13:94-97. 24. McGraw JJ, Akbarnia BA, Hanel DP, et
Philadelphia: JB Lippincott, 1991, vol 12. Millis MB, Singer IJ, Hall JE: al: Neurological complications result-
3, pp 526-617. Supracondylar fracture of the ing from supracondylar fractures of
2. Landin LA: Fracture patterns in chil- humerus in children: Further experi- the humerus in children. J Pediatr
dren: Analysis of 8,682 fractures with ence with a study in orthopaedic deci- Orthop 1986;6:647-650.
special reference to incidence, etiology sion-making. Clin Orthop 1984;188: 25. Culp RW, Osterman AL, Davidson RS,
and secular changes in a Swedish 90-97. et al: Neural injuries associated with
urban population, 1950–1979. Acta 13. Herzenberg JE, Koreska J, Carroll NC, supracondylar fractures of the
Orthop Scand Suppl 1983;202:1-109. et al: Biomechanical testing of pin fix- humerus in children. J Bone Joint Surg
3. Henrikson B: Supracondylar fracture ation techniques for pediatric supra- Am 1990;72:1211-1215.
of the humerus in children: A late condylar elbow fractures. Orthop 26. Martin DF, Tolo VT, Sellers DS, et al:
review of end-results with special ref- Trans 1988;12:678-679. Radial nerve laceration and retraction
erence to the cause of deformity, dis- 14. Webb AJ, Sherman FC: Supracondylar associated with a supracondylar frac-
ability and complications. Acta Chir fractures of the humerus in children. J ture of the humerus. J Hand Surg [Am]
Scand Suppl 1966;369:1-72. Pediatr Orthop 1989;9:315-325. 1989;14:542-545.
4. Hanlon CR, Estes WL Jr: Fractures in 15. Lagrange J, Rigault P: Fractures 27. Royce RO, Dutkowsky JP, Kasser JR,
childhood: A statistical analysis. Am J supra-condyliennes. Rev Chir Orthop et al: Neurologic complications after
Surg 1954;87:312-323. 1962:48:337-414. K-wire fixation of supracondylar
5. Arnold JA, Nasca RJ, Nelson CL: 16. Conn J Jr, Wade PA: Injuries of the humerus fractures in children. J
Supracondylar fractures of the elbow: A ten-year review. J Trauma Pediatr Orthop 1991;11:191-194.
humerus: The role of dynamic factors 1961;1:248-268. 28. Ottolenghi CE: Prophylaxie du syn-
in prevention of deformity. J Bone 17. Dunlop J: Transcondylar fractures of drome de Volkmann dans les fractures
Joint Surg Am 1977;59:589-595. the humerus in childhood. J Bone Joint supra-condyliennes du coude chez
6. Minkowitz B, Busch MT: Supra- Surg 1939;21:59-73. 1’enfant. Rev Chir Orthop 1971;57:517-
condylar humerus fractures: Current 18. Ormandy L: Olecranon screw for 525.
trends and controversies. Orthop Clin skeletal traction of the humerus. Am J 29. Shaw BA, Kasser JR, Emans JB, et al:
North Am 1994;25:581-594. Surg 1974;127:615-616. Management of vascular injuries in
7. Kasser JR: Percutaneous pinning of 19. Palmer EE, Niemann KMW, Vesely D, displaced supracondylar humerus
supracondylar fractures of the et al: Supracondylar fracture of the fractures without arteriography. J
humerus. Instr Course Lect 1992;41: humerus in children. J Bone Joint Surg Orthop Trauma 1990:4:25-29.
385-390. Am 1978;60:653-656. 30. Harris IE: Supracondylar fractures of
8. Campbell CC, Waters PM, Emans JB, 20. Pirone AM, Graham HK, Krajbich JI: the humerus in children. Orthopedics
et al: Neurovascular injury and dis- Management of displaced extension- 1992;15:811-817.
placement in type III supracondylar type supracondylar fractures of the 31. Mubarak SJ, Carroll NC: Volkmann’s
humerus fractures. J Pediatr Orthop humerus in children. J Bone Joint Surg contracture in children: Aetiology and
1995;15:47-52. Am 1988;70:641-650. prevention. J Bone Joint Surg Br
9. Gartland JJ: Management of supra- 21. Elstrom JA, Pankovich AM, Kassab 1979;61:285-293.
condylar fractures of the humerus in MT: Irreducible supracondylar frac- 32. Labelle H, Bunnell WP, Duhaime M, et
children. Surg Gynecol Obstet 1959;109: ture of the humerus in children: A al: Cubitus varus deformity following
145-154. report of two cases. J Bone Joint Surg supracondylar fractures of the
10. Camp J, Ishizue K, Gomez M, et al: Am 1975;57:680-681. humerus in children. J Pediatr Orthop
Alteration of Baumann’s angle by 22. Wilkins KE: The operative manage- 1982;2:539-546.
humeral position: Implications for ment of supracondylar fractures. 33. Voss FR, Kasser JR, Trepman E, et al:
treatment of supracondylar humerus Orthop Clin North Am 1990;21:269-289. Uniplanar supracondylar humeral
fractures. J Pediatr Orthop 1993;13: 23. Ippolito E, Caterini R, Scola E: osteotomy with preset Kirschner wires
94-97. Supracondylar fractures of the for posttraumatic cubitus varus. J
11. Biyani A, Gupta SP, Sharma JC: humerus in children: Analysis at Pediatr Orthop 1994;14:471-478.
26 Journal of the American Academy of Orthopaedic Surgeons
You might also like
- Bone Marrow Aspirate Concentrate and Expanded Stem Cell Applications in OrthopaedicsFrom EverandBone Marrow Aspirate Concentrate and Expanded Stem Cell Applications in OrthopaedicsNo ratings yet
- Current Challenges with their Evolving Solutions in Surgical Practice in West Africa: A ReaderFrom EverandCurrent Challenges with their Evolving Solutions in Surgical Practice in West Africa: A ReaderNo ratings yet
- Fractures and Dislocations About The Elbow in The Pediatric PatientDocument65 pagesFractures and Dislocations About The Elbow in The Pediatric PatientPeter HubkaNo ratings yet
- SC - Fracture ZMHDocument51 pagesSC - Fracture ZMHMis StromNo ratings yet
- Actures - In.adults.8e Booksmedicos - Org Parte4 PDFDocument1 pageActures - In.adults.8e Booksmedicos - Org Parte4 PDFeladioNo ratings yet
- Fractures in ChildrenDocument5 pagesFractures in ChildrenAbigaille ChuaNo ratings yet
- Leg Compartment Syndrome - Trauma - OrthobulletsDocument1 pageLeg Compartment Syndrome - Trauma - OrthobulletsArief AbidinNo ratings yet
- Surgical Antibiotic Prophylaxis GuidelineDocument7 pagesSurgical Antibiotic Prophylaxis GuidelineConstantin BudinNo ratings yet
- Intramedullary Nailing of The Lower Extremity. Biomechanics and BiologyDocument10 pagesIntramedullary Nailing of The Lower Extremity. Biomechanics and Biologyorthopod_idreesNo ratings yet
- Bone Tumour Staging - PathologyDocument2 pagesBone Tumour Staging - Pathologyo7113No ratings yet
- Bone Remodeling - Basic Science - OrthobulletsDocument4 pagesBone Remodeling - Basic Science - OrthobulletsCindy Julia AmandaNo ratings yet
- Fracture Classifications in OrthopaedicsDocument34 pagesFracture Classifications in Orthopaedicshaswal fazry AwalNo ratings yet
- M.S. Orthopaedic Surgery SyllabusDocument8 pagesM.S. Orthopaedic Surgery SyllabusMuthu KumarNo ratings yet
- Adult Pyogenic Vertebral Osteomyelitis - SpineDocument6 pagesAdult Pyogenic Vertebral Osteomyelitis - SpineL Yudhantoro YudhaNo ratings yet
- Modified French OsteotomyDocument5 pagesModified French OsteotomyKaustubh KeskarNo ratings yet
- 7 Xray Questions Handout793266145Document3 pages7 Xray Questions Handout793266145jojoNo ratings yet
- Clinical Examination of The Wrist PDFDocument11 pagesClinical Examination of The Wrist PDFAdosotoNo ratings yet
- Fixation Methods in OrthopaedicsDocument40 pagesFixation Methods in OrthopaedicsBhaskar BorgohainNo ratings yet
- Orthopaedic Instruments ImagesDocument40 pagesOrthopaedic Instruments ImagesKannan KannanNo ratings yet
- 1.26 (Surgery) Orthopedic Pathology - OncologyDocument7 pages1.26 (Surgery) Orthopedic Pathology - OncologyLeo Mari Go LimNo ratings yet
- PreviewDocument24 pagesPreviewSabryNo ratings yet
- Acetabular Fracture PostgraduateDocument47 pagesAcetabular Fracture Postgraduatekhalidelsir5100% (1)
- New Trends and Techniques in Open Reduction and Internal Fixation of Fractures of The Tibial PlateauDocument8 pagesNew Trends and Techniques in Open Reduction and Internal Fixation of Fractures of The Tibial PlateauCosmina BribanNo ratings yet
- FRCS (Tr & Orth) Examination Questions: MCQs, Vivas and Clinical Examination SectionsDocument2 pagesFRCS (Tr & Orth) Examination Questions: MCQs, Vivas and Clinical Examination SectionsNishil ModiNo ratings yet
- Hamstring Tendon Autograft For Anterior Cruciate Ligament ReconstructionDocument22 pagesHamstring Tendon Autograft For Anterior Cruciate Ligament ReconstructionJaime Vázquez ZárateNo ratings yet
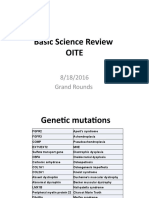
- Basic Science OITE ReviewDocument91 pagesBasic Science OITE ReviewICH KhuyNo ratings yet
- Osteopetrosis - PediatricsDocument3 pagesOsteopetrosis - PediatricstaufiqtopNo ratings yet
- Ficat and Arlet staging of hip AVNDocument6 pagesFicat and Arlet staging of hip AVNFernando Sugiarto0% (1)
- Orthopedics: Notes, 1/eDocument26 pagesOrthopedics: Notes, 1/evkNo ratings yet
- Posterior Tibial Tendon Insufficiency (PTTI) - Foot & Ankle - OrthobulletsDocument5 pagesPosterior Tibial Tendon Insufficiency (PTTI) - Foot & Ankle - OrthobulletsguriakkNo ratings yet
- MILLER Testable ConceptsDocument109 pagesMILLER Testable ConceptsMohammedGooda100% (1)
- Orthopedic Exam Notes Apu PDFDocument6 pagesOrthopedic Exam Notes Apu PDFabiramirajalaksmiNo ratings yet
- Acute Distal Radioulnar Joint InstabilityDocument13 pagesAcute Distal Radioulnar Joint Instabilityyerson fernando tarazona tolozaNo ratings yet
- DR - O. K. A. SamuelsDocument76 pagesDR - O. K. A. Samuelsgdudex118811No ratings yet
- Approach To FractureDocument17 pagesApproach To FractureRebecca WongNo ratings yet
- DRUJinstabilityreview - PDF 034407Document15 pagesDRUJinstabilityreview - PDF 034407Oscar Cayetano Herrera RodríguezNo ratings yet
- Chemical Hip Denervation For Inoperable Hip FractureDocument6 pagesChemical Hip Denervation For Inoperable Hip Fracturemanuel torresNo ratings yet
- Hand OITE Questions for NYSSH Update Course 2007Document35 pagesHand OITE Questions for NYSSH Update Course 2007ICH KhuyNo ratings yet
- Acetabular Fractures: Dr. Roshan DDocument65 pagesAcetabular Fractures: Dr. Roshan DKaizar EnnisNo ratings yet
- AAOS Orthopaedic Knowledge Update 8Document763 pagesAAOS Orthopaedic Knowledge Update 8Hiohi LianaNo ratings yet
- Genu ValgoDocument9 pagesGenu Valgoazulqaidah95No ratings yet
- Aaos PDFDocument4 pagesAaos PDFWisnu CahyoNo ratings yet
- External Fixation Principles and Applications.5Document8 pagesExternal Fixation Principles and Applications.5Leonardo Rocha100% (1)
- 1ry & 2ry Lesions DermatologyDocument9 pages1ry & 2ry Lesions DermatologyHassan.shehriNo ratings yet
- Gpe - 017.1 - Orthopaedic ExaminationDocument3 pagesGpe - 017.1 - Orthopaedic ExaminationImiey Eleena HanumNo ratings yet
- Ortho AIIMSDocument15 pagesOrtho AIIMSvkNo ratings yet
- Lateral Condyle Fracture Tips and TricksDocument33 pagesLateral Condyle Fracture Tips and TricksPurushotham NalamatiNo ratings yet
- Malunions of the Distal Radius: Evaluation and TreatmentDocument14 pagesMalunions of the Distal Radius: Evaluation and TreatmentSivaprasath JaganathanNo ratings yet
- Sheety PDFDocument378 pagesSheety PDFLakshita PrajapatiNo ratings yet
- Classification AO PediatricDocument36 pagesClassification AO PediatricdvcmartinsNo ratings yet
- Open Reduction and Internal Fixation of Fractures of The Radial HeadDocument5 pagesOpen Reduction and Internal Fixation of Fractures of The Radial Headjeremy1roseNo ratings yet
- AAOS Mini Open Rotator Cuff RepairDocument10 pagesAAOS Mini Open Rotator Cuff RepairHannah CoNo ratings yet
- CHAPTER 14 - Treatment of Bone Def - 2008 - Surgical Techniques of The ShoulderDocument11 pagesCHAPTER 14 - Treatment of Bone Def - 2008 - Surgical Techniques of The ShoulderJaime Vázquez ZárateNo ratings yet
- OKU Referat Bedah PDFDocument469 pagesOKU Referat Bedah PDFAde ZulfiahNo ratings yet
- Hand OITE - 2012 2013 2014Document209 pagesHand OITE - 2012 2013 2014Sadiq AliNo ratings yet
- Traumatology Orthopaedic EXAMDocument219 pagesTraumatology Orthopaedic EXAMElo GonçalvesNo ratings yet
- Transtibial Tunnel Posterior Cruciate Ligament ReconstructionDocument9 pagesTranstibial Tunnel Posterior Cruciate Ligament ReconstructionJaime Vázquez ZárateNo ratings yet
- 829 FullDocument3 pages829 FullRakesh KumarNo ratings yet
- Fragment-Specific Fixation in Distal Radius Fractures: AnatomyDocument8 pagesFragment-Specific Fixation in Distal Radius Fractures: Anatomyosman gorkemNo ratings yet
- Marfan Syndrome A Clinical Update JAAOSDocument7 pagesMarfan Syndrome A Clinical Update JAAOSAzmi FarhadiNo ratings yet
- NexusDocument6 pagesNexusAzmi FarhadiNo ratings yet
- The Governance of Islamic Boarding Schools in IndonesiaDocument17 pagesThe Governance of Islamic Boarding Schools in IndonesiaAzmi FarhadiNo ratings yet
- Articulo Clavicula 1Document9 pagesArticulo Clavicula 1Emmy LiraNo ratings yet
- Subaidah 7/1/1958 362516 Ods Glaukoma Os Pe + Iol FD WA GA 2Document1 pageSubaidah 7/1/1958 362516 Ods Glaukoma Os Pe + Iol FD WA GA 2Azmi FarhadiNo ratings yet
- Acute Compartment Syndrome in Lower Extremity JAAOSDocument9 pagesAcute Compartment Syndrome in Lower Extremity JAAOSAzmi FarhadiNo ratings yet
- Subaxial Cervical Spine Trauma JAAOSDocument12 pagesSubaxial Cervical Spine Trauma JAAOSAzmi FarhadiNo ratings yet
- Agricultural InjuryDocument21 pagesAgricultural InjuryAzmi FarhadiNo ratings yet
- The Orthopaedic Implications of Diphosphonate Therapy: Review ArticleDocument8 pagesThe Orthopaedic Implications of Diphosphonate Therapy: Review ArticleroyNo ratings yet
- Spondylolysis and Spondylolisthesis in Children and Adolescents JAAOSDocument8 pagesSpondylolysis and Spondylolisthesis in Children and Adolescents JAAOSAzmi FarhadiNo ratings yet
- ASIA ISCOS IntlWorksheet 2019Document2 pagesASIA ISCOS IntlWorksheet 2019Anastasia CanahuateNo ratings yet
- Thoracolumbar Spine Trauma I Evaluation and Classification JAAOSDocument8 pagesThoracolumbar Spine Trauma I Evaluation and Classification JAAOSAzmi FarhadiNo ratings yet
- Treatment of Blast Injuries of The Extremity JAAOSDocument5 pagesTreatment of Blast Injuries of The Extremity JAAOSAzmi FarhadiNo ratings yet
- Hannover Polytrauma Score AssessmentDocument2 pagesHannover Polytrauma Score AssessmentAzmi FarhadiNo ratings yet
- Extensor Tendon Injuries in The Hand JAAOSDocument8 pagesExtensor Tendon Injuries in The Hand JAAOSAzmi FarhadiNo ratings yet
- Damage Control Orthopaedics in Spinal Trauma JAAOSDocument12 pagesDamage Control Orthopaedics in Spinal Trauma JAAOSAzmi FarhadiNo ratings yet
- Idiopathic Congenital Talipes Equinovarus PDFDocument10 pagesIdiopathic Congenital Talipes Equinovarus PDFEric RothNo ratings yet
- Fat EmbolismDocument10 pagesFat EmbolismAzmi FarhadiNo ratings yet
- A Systematic Summary of Systematic Reviews On The Topic of The Anterior Cruciate LigamentDocument23 pagesA Systematic Summary of Systematic Reviews On The Topic of The Anterior Cruciate LigamentAzmi FarhadiNo ratings yet
- Wear and Osteolysis Around Total Knee Arthroplasty JAAOSDocument12 pagesWear and Osteolysis Around Total Knee Arthroplasty JAAOSAzmi FarhadiNo ratings yet
- 10.1097@00124635 199701000 00001Document10 pages10.1097@00124635 199701000 00001Azmi FarhadiNo ratings yet
- Malignant Bone Pain Pathophysiology and TreatmentDocument18 pagesMalignant Bone Pain Pathophysiology and TreatmentAzmi FarhadiNo ratings yet
- Safe Tourniquet Use A Review of The Evidence JAAOSDocument10 pagesSafe Tourniquet Use A Review of The Evidence JAAOSAzmi FarhadiNo ratings yet
- Primary Osteoporosis in Postmenopausal WomenDocument5 pagesPrimary Osteoporosis in Postmenopausal WomenAzmi FarhadiNo ratings yet
- TB Arthritis Ankle Mimicking SynovitisDocument8 pagesTB Arthritis Ankle Mimicking SynovitisAzmi FarhadiNo ratings yet
- Venous Thromboembolism in MalignancyDocument3 pagesVenous Thromboembolism in MalignancyAzmi FarhadiNo ratings yet
- True Ponte Osteotomy Ponte 2018Document10 pagesTrue Ponte Osteotomy Ponte 2018Azmi FarhadiNo ratings yet
- USS Universal Spine SystemDocument32 pagesUSS Universal Spine SystemAzmi Farhadi100% (1)
- Varus Osteotomy French 1959Document3 pagesVarus Osteotomy French 1959Azmi FarhadiNo ratings yet
- LEG. MED-Case DigestDocument19 pagesLEG. MED-Case DigestAubrey BalindanNo ratings yet
- Master of Business Administration: Summer Internship Programm Report ONDocument18 pagesMaster of Business Administration: Summer Internship Programm Report ONshubham moonNo ratings yet
- Physician CatalogDocument573 pagesPhysician CatalogIfan RizkyNo ratings yet
- MURMURDocument21 pagesMURMURtoyyibNo ratings yet
- 862 1894 1 PBDocument5 pages862 1894 1 PBChristo LimbongNo ratings yet
- PocketCPR 2010 Guidelines 102510Document1 pagePocketCPR 2010 Guidelines 102510Adiyanto DidietNo ratings yet
- Auto PeepDocument6 pagesAuto PeepVadelain GaldamesNo ratings yet
- Mechanical Ventilator GuideDocument3 pagesMechanical Ventilator GuideDivine Mercy De JulianNo ratings yet
- Sdcep Management of Dental Patients Taking Anticoagulants or Antiplatelet Drugs 2nd EditionDocument58 pagesSdcep Management of Dental Patients Taking Anticoagulants or Antiplatelet Drugs 2nd EditionMeryem LahlouNo ratings yet
- Vital Pulp Therapy TechniquesDocument11 pagesVital Pulp Therapy TechniquesZeinab Mohamed MorsyNo ratings yet
- Our Purpose Our Mission Our Solid Strategic Platform: An Emphasis OnDocument2 pagesOur Purpose Our Mission Our Solid Strategic Platform: An Emphasis Onwmturner72No ratings yet
- Unstable Angina: DR Abdul Mateen Ansari, MD Professor and HOD General Medicine, Cimsh, LucknowDocument27 pagesUnstable Angina: DR Abdul Mateen Ansari, MD Professor and HOD General Medicine, Cimsh, LucknowCyntia KhairaniNo ratings yet
- Gracey's CurettesDocument29 pagesGracey's CurettesEma RaduNo ratings yet
- Inguinal Hernias: BMJ (Online) March 2008Document5 pagesInguinal Hernias: BMJ (Online) March 2008Karl PinedaNo ratings yet
- Perioperative Nursing - 50 ItemsDocument6 pagesPerioperative Nursing - 50 Itemsapi-371817496% (26)
- SocivoDocument16 pagesSocivoSlobodan MilovanovicNo ratings yet
- Uptodate: Chronic Kidney DiseaseDocument13 pagesUptodate: Chronic Kidney DiseaseAtiqah ShahNo ratings yet
- Hepatic PackingDocument4 pagesHepatic PackingRESIDENTES CIRUGIA IMSSNo ratings yet
- Transport of Critically Ill PatientsDocument13 pagesTransport of Critically Ill Patientsansuh22100% (1)
- 7 RotDocument17 pages7 RotsnowyfingersNo ratings yet
- Forwarding LetterDocument3 pagesForwarding LetterGurudatt RamNo ratings yet
- جذومن -سويرولاكبلا ةلمحل يعاعشلإا ريوصتلا ناحتما A) ) Radiography Technology Bachelor Degree) Bsc Exam Number:) Bsc-A)Document9 pagesجذومن -سويرولاكبلا ةلمحل يعاعشلإا ريوصتلا ناحتما A) ) Radiography Technology Bachelor Degree) Bsc Exam Number:) Bsc-A)Nuhad Bou MoslehNo ratings yet
- MRI ReportDocument47 pagesMRI ReportRizell MangubatNo ratings yet
- Primarya Angle Closure Glaucoma 2021Document147 pagesPrimarya Angle Closure Glaucoma 2021robeyeNo ratings yet
- HELDMANN 1999 The Association of Propofol Usage With Posoperatve Wound Infection Rate in Clean Wounds PDFDocument4 pagesHELDMANN 1999 The Association of Propofol Usage With Posoperatve Wound Infection Rate in Clean Wounds PDFAntonio PG´sNo ratings yet
- Catheterisation - Suprapubic Catheter ProcedureNewDocument12 pagesCatheterisation - Suprapubic Catheter ProcedureNewAmit KapuriaNo ratings yet
- Quick medical specialists referenceDocument2 pagesQuick medical specialists referenceAdnan ADIGÜZELNo ratings yet
- ASGE 2013 Endoscopic Practice in ElderlyDocument7 pagesASGE 2013 Endoscopic Practice in ElderlyjordanNo ratings yet
- Open FractureDocument20 pagesOpen FracturegraceswanNo ratings yet
- Focus On Adult Health Medical Surgical Nursing Pellico Edition Test BankDocument8 pagesFocus On Adult Health Medical Surgical Nursing Pellico Edition Test BankCarolineAndersoneacmg100% (33)