Professional Documents
Culture Documents
Acute Compartment Syndrome in Lower Extremity JAAOS
Uploaded by
Azmi FarhadiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Acute Compartment Syndrome in Lower Extremity JAAOS
Uploaded by
Azmi FarhadiCopyright:
Available Formats
Acute Compartment
Syndrome in Lower
Extremity Musculoskeletal
Trauma
Steven A. Olson, MD, and Abstract
Downloaded from http://journals.lww.com/jaaos by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC1y0abggQZXdtwnfKZBYtws= on 01/28/2022
Robert R. Glasgow, MD Acute compartment syndrome is a potentially devastating
condition in which the pressure within an osseofascial
compartment rises to a level that decreases the perfusion gradient
across tissue capillary beds, leading to cellular anoxia, muscle
ischemia, and death. A variety of injuries and medical conditions
may initiate acute compartment syndrome, including fractures,
contusions, bleeding disorders, burns, trauma, postischemic
swelling, and gunshot wounds. Diagnosis is primarily clinical,
supplemented by compartment pressure measurements. Certain
anesthetic techniques, such as nerve blocks and other forms of
regional and epidural anesthesia, reportedly contribute to a delay in
diagnosis. Basic science data suggest that the ischemic threshold of
normal muscle is reached when pressure within the compartment
is elevated to 20 mm Hg below the diastolic pressure or 30 mm Hg
below the mean arterial blood pressure. On diagnosis of impending
or true compartment syndrome, immediate measures must be
Dr. Olson is Associate Professor,
Division of Orthopaedic Surgery, Duke
taken. Complete fasciotomy of all compartments involved is
University, Durham, NC. Dr. Glasgow is required to reliably normalize compartment pressures and restore
Orthopaedic Surgeon, Division of perfusion to the affected tissues. Recognizing compartment
Orthopaedic Surgery, Royal Alexander
syndromes requires having and maintaining a high index of
Hospital, Edmonton, AB, Canada.
suspicion, performing serial examinations in patients at risk, and
None of the following authors or the
departments with which they are
carefully documenting changes over time.
affiliated has received anything of value
from or owns stock in a commercial
T
company or institution related directly or he importance of timely diagno- most common cause of acute com-
indirectly to the subject of this article: sis and management of compart- partment syndrome in this series was
Dr. Olson and Dr. Glasgow.
ment syndrome was recently empha- fracture (69%); fracture of the tibial
Reprint requests: Dr. Olson, Duke sized in a review of the medical-legal diaphysis was most frequent (36%),
University, Box 3389, Durham, NC aspects of this condition.1 McQueen followed by distal radius fractures
27710. et al2 studied 164 patients (149 men, (9.8%). Soft-tissue injury without
15 women) with acute traumatic fracture was the second most com-
J Am Acad Orthop Surg 2005;13:436-
compartment syndrome. The inci- mon cause (23.2%), with 10% of
444
dence of compartment syndrome was these occurring in patients taking an-
Copyright 2005 by the American 7.3 per 100,000 in men (average age, ticoagulants or with a bleeding disor-
Academy of Orthopaedic Surgeons. 30 years) and 0.7 per 100,000 in der. The incidence of compartment
women (average age, 44 years).2 The syndrome associated with high- and
436 Journal of the American Academy of Orthopaedic Surgeons
Steven A. Olson, MD, and Robert R. Glasgow, MD
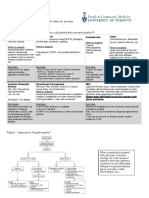
Table 1 Figure 1
Causes of Compartment Syndrome
Fracture
Soft-tissue trauma without fracture
Intracompartmental bleeding
Tight casts, dressings, or external
wrappings
Thermal injury, burn eschar
Extravasation of intravenous infusion
Venous obstruction
Reperfusion injury following
prolonged ischemia
Penetrating trauma
low-energy injuries is nearly equal.
The presence of open wounds does
not mean that compartments are de-
compressed; compartment syndrome Change in compartment pressure (percent) with increasing calcaneal pin traction
is seen after open fractures.2-4 (kg) in patients with tibial shaft fractures. (Adapted with permission from
Shakespeare DT, Henderson NJ: Compartmental pressure changes during
Etiology calcaneal traction in tibial fractures. J Bone Joint Surg Br 1982;64:498-499.)
A variety of injuries and medical
conditions may initiate acute com- material results in a marked decrease ly with increasing traction, up to 9.1
partment syndrome (Table 1). Frac- in intracompartmental pressure. kg (Figure 1). The pressure did not
tures; contusions; bleeding disor- Pneumatic antishock garments fall during the time the traction was
ders; burns; trauma; postischemic have been associated with lower ex- applied. For each increase of 1 kg in
swelling; tight casts, dressings, or tremity compartment syndromes. longitudinal traction, the compart-
external wrappings; and gunshot Templeman et al9 reported on a pa- ment pressure within the deep pos-
wounds are some of the most fre- tient who developed bilateral com- terior compartment increased by
quent causes.2-12 Anatomic struc- partment syndromes in uninjured more than 5%; pressure in the ante-
tures, including epimysium, fascia, extremities after wearing a pneu- rior compartment increased by <2%.
and skin, may limit the potential matic antishock garment. However, Intramuscular pressure is lowest in
size of a compartment. Therefore, inflation pressures <50 mm Hg in the anterior compartment with the
closure of incisions or defects in these garments have been used for ankle in the neutral to dorsiflexed
these structures should not be done long periods of time (eg, 48 hours for position; it is lowest in the deep pos-
acutely when the patient is at risk pelvic fractures) without adverse se- terior compartment when the ankle
for compartment syndrome. Ther- quelae.9 is in the plantarflexed position.13
mal injuries, especially circumferen- Traction, ankle joint position, and Longitudinal calcaneal traction
tial third-degree burns, can cause an limb positioning have been shown to tends to dorsiflex the ankle and in-
acute compartment syndrome by affect compartment volume and crease the pressure in the deep pos-
forming inelastic constrictions, es- pressure and to contribute to the terior compartment more than in
chars, and massive edema which, in formation of compartment syn- the anterior compartment. After cast
combination, result in ischemia to dromes.3,8,10,11,13,15,16 Traction causes application, the pressure in both the
neurovascular and muscular struc- the fascia to tighten and constrict anterior and deep posterior compart-
tures.2,5,7,13 Circumferential wraps, the limb, decreasing the compart- ments increases three- to seven-fold,
such as casting material or cast pad- ment volume. Shakespeare and depending on the position of the an-
ding, can lead to restriction of com- Henderson15 described compartmen- kle.13 Ankle plantar flexion of 0° to
partment expansion and increased tal pressure changes during calca- 37° is the most protective position
compartmental pressure.8,13,14 Re- neal traction for tibial fractures. for minimizing the combined risks
leasing all circumferential dressings, Pressure in the anterior and deep of anterior and posterior compart-
splitting casts, and cutting casting posterior compartments rose linear- ment syndromes.13
Volume 13, Number 7, November 2005 437
Acute Compartment Syndrome in Lower Extremity Musculoskeletal Trauma
Compartment syndromes have pressure elevation ≥40 mm Hg (max- to a decrease in the arteriovenous
been described with prolonged use imum, 58 mm Hg); all pressures gradient.7 Change in the local vascu-
of the Lloyd-Davies (lithotomy) po- returned to below 20 mm Hg by the lar resistance can accommodate for
sition with flexion, elevation, and end of the procedure. The authors some of the reduction in the arterio-
abduction of the well leg during in- concluded that patients with a tibial venous gradient; however, this
tramedullary nailing of femoral frac- fracture who demonstrate signs and change becomes ineffective with in-
tures.11,13 The combined effects of symptoms of an acute compartment creasing tissue pressure. Compart-
direct compression on the leg, com- syndrome on presentation should ment syndrome occurs when the lo-
pressive circumferential bindings or undergo a four-compartment fasci- cal arteriovenous gradient does not
stockings, sequential inflatable de- otomy before intramedullary nail- allow sufficient blood flow to meet
vices, and relative elevation of the ing, and that pressure elevations the metabolic demands of the tis-
limb contribute to increased com- during nailing should be minimized sue.7 Vascular tone, blood pressure,
partment pressure, decreased com- by avoiding prolonged traction. duration of pressure elevation, and
partment volume, and decreased McQueen and Court-Brown4 used metabolic demands of the tissue are
blood flow, leading to the formation continuous compartment pressure important in determining whether a
of compartment syndromes.11 monitoring during tibial nailing in a compartment syndrome will oc-
Many authors have discussed ele- prospective study of 116 patients. cur.7
vated compartment pressures asso- Use of reamed versus unreamed nail- Muscle ischemia can lead to re-
ciated with intramedullary nailing ing had no effect on the incidence of lease of myoglobin from damaged
of tibial fractures.4,16-20 The etiology compartment syndrome. Tibial nail- muscle cells. During reperfusion,
of acute compartment syndrome as- ing with or without prior canal ream- myoglobin is released into the cir-
sociated with intramedullary fixa- ing is a safe method of managing culation with other inflammatory
tion is multifactorial: tissue damage tibial shaft fractures at risk for com- and toxic metabolites. Myoglobin-
secondary to the injury causes swell- partment syndrome. Prolonged fixed uria, metabolic acidosis, and hyper-
ing, traction decreases the volume of traction should be avoided to the ex- kalemia can lead to renal failure,
the compartments, reaming forces tent possible. shock, hypothermia, and cardiac
blood and marrow into the compart- arrhythmias and/or failure. The de-
ments, and limb supports may cause velopment and extent of these sys-
Pathophysiology of
outflow constriction.16 Moed and temic effects depends on the sever-
Ischemia
Strom,18 using a canine model, found ity and duration of compromised
that pressure changes during ream- The pathophysiologic mechanism tissue perfusion and the size and
ing were transient, returning to base- that causes compartment syn- number of muscle compartments
line or lower after the reamer was dromes is increased tissue pressure involved.7
removed from the intramedullary and the resulting development of is- By using objective, noninvasive
canal. After nail insertion, the pres- chemia, which leads to irreversible techniques, experimental and clini-
sure remained elevated in the an- muscle damage. Cellular anoxia is cal investigators have determined
terolateral compartment and was the final common pathway of all of the changes in muscle blood flow
transiently elevated in the posterior the varieties of compartment syn- that occur during compartment syn-
compartment. Mawhinney et al20 drome. However, the interaction be- drome.24 Induced compartment syn-
showed that peak pressures were tween increased compartment pres- dromes in dogs revealed three histo-
reached after the first two reaming sure, blood pressure, and blood flow logic regions of muscle injury.24 In
cycles. are incompletely understood. It was skeletal muscle, the central portion
Several authors have recom- originally suggested that there was a of the muscle becomes ischemic
mended using an unreamed nail in threshold compartment pressure first. The surrounding zone of mus-
tibial fractures with associated above which irreversible changes cle tissue then shows evidence of
compartment syndrome, or in pa- would occur.21 More recent evidence partial ischemic injury with in-
tients without compartment syn- indicates that the absolute differ- creased tissue edema and swelling.
drome who have elevated compart- ence between compartment pressure The peripheral layers of muscle are
ment pressures, in order to minimize and blood pressure is the critical the last to be affected, often remain-
pressure elevation during the pro- variable.21-26 To avoid collapsing of ing normal in incomplete compart-
cedure.16-19 Tornetta and French16 the veins, the pressure inside the ment syndromes. Microangiograms
reported on anterior compartment veins cannot be less than that of the showed an abundance of epimysial
pressures during unreamed tibial surrounding tissue.7,27 An increase in vessels with occlusion of central
nailing without traction. Eight of 20 compartment pressure results in an penetrating branches in specimens
patients had transient compartment increase in venous pressure, leading from severe cases.24
438 Journal of the American Academy of Orthopaedic Surgeons
Steven A. Olson, MD, and Robert R. Glasgow, MD
Using autologous plasma infusion value diminished toward a value of neural deficit. However, McQueen
in a canine compartment syndrome 10 mm Hg. Normal limbs did not and Court-Brown4 reported a patient
model, Heckman et al21 studied the become metabolically compromised in whom a compartment syndrome
ischemic threshold of muscle by in- until the ∆P value declined to <30 was diagnosed by increased compart-
ducing elevated pressures for 8 mm Hg. Postischemic muscle is ment pressures before the onset of
hours. Irreversible histologic chang- more easily and much more rapidly signs or symptoms.
es, including focal muscle infarction compromised metabolically by in- Pressure or firmness in the com-
and fibrosis, were documented in all creased interstitial pressure than is partment, a direct manifestation of
compartments subjected to tissue normal muscle.25 increased intracompartmental pres-
pressures within 10 mm Hg of dia- Vollmar et al26 used a skinfold sure, is the earliest and may be the
stolic pressure. None of the animals chamber to examine vessel response only objective finding of early com-
with a difference in perfusion pres- to increased pressure in hamsters. partment syndrome. Peripheral puls-
sure >30 mm Hg from mean arterial Venules exhibited early reduction in es are palpable and, unless a major
and >20 mm Hg from diastolic pres- size proportional to external pres- arterial injury is present, capillary
sure demonstrated any evidence of sure. No similar change was observed refill is routinely present. Only rare-
irreversible changes, although occa- in arterioles. This study suggests that ly is the compartment pressure ele-
sional cells underwent myofibrillar impaired venous drainage with cap- vated sufficiently to occlude arterial
degeneration. Mean compartment illary stasis but without arteriolar pressure.7
pressures of 59 mm Hg with ade- constriction is a significant patho- Paresis is difficult to interpret and
quate perfusion pressure were toler- physiologic component in the devel- may be caused by muscle ischemia,
ated for 8 hours without evidence of opment of compartment syndrome. nerve ischemia, guarding secondary
infarction. The authors concluded to pain, or a combination of all three.
that the ischemic threshold of skel- True paralysis is a late finding that is
Diagnosis
etal muscle, beyond which irrevers- caused by prolonged nerve compres-
ible tissue damage occurs after 8 History and Physical sion or irreversible muscle damage.
hours, is directly related to the dif- Examination Paresthesia is an early sign of com-
ference between the compartment Critical to recognizing compart- partment syndrome that, without
and mean arterial or diastolic pres- ment syndrome is having and main- treatment, progresses to hypesthesia
sures. The critical tissue pressure taining a high index of suspicion and and anesthesia. Sensory symptoms
differentials were ≤30 mm Hg from performing serial examinations in and signs are often the first indica-
mean arterial pressure and ≤20 mm patients at risk to document chang- tion of nerve ischemia.3 Matava et
Hg from diastolic blood pressure.21 es over time.2,5-7,12 Patient history is al22 have shown that peripheral
Matava et al22 performed a similar important for determining the me- nerve tissue is actually more sensi-
study in canines and also found that chanism of injury and whether there tive to an ischemic event than mus-
the threshold for muscle necrosis are associated risk factors for devel- cle, with nerve function ceasing af-
was 20 mm Hg less than the diastol- oping compartment syndrome.6 The ter 75 minutes of total ischemia.
ic pressure. These findings support classic clinical diagnosis encompass- The duration and degree of pressure
the hypothesis that tissue damage is es the six Ps: pain, pressure, pulse- elevation leading to irreversible
directly related to absolute differ- lessness, paralysis, paresthesia, and nerve injury secondary to compres-
ence between compartment pressure pallor.12 sion is uncertain.22 Typically, abnor-
and blood pressure and that this dif- Pain out of proportion to the in- mal neurologic findings are associat-
ference is a variable that affects not jury, aggravated by passive stretching ed with nerves that course through
only microvascular perfusion but of muscle groups in the correspond- affected compartments. The isolated
also the onset of tissue damage. ing compartment, is one of the earli- finding of paresthesia is frequently
Bernot et al25 observed that mus- est and most sensitive clinical signs resolved with the release of con-
cle subjected to ischemia before of compartment syndrome. However, stricting wraps or bandages alone.
compartment pressurization had a pain may be an unreliable indicator Although frequently listed as one of
lower threshold for metabolic deteri- and may be absent in an established the “P’s,” pallor is uncommon. It oc-
oration than did nontraumatized compartment syndrome.3 Pain per- curs in the rare circumstance in
muscle. Hypoxic metabolic changes ception may be diminished or absent which arterial inflow is severely di-
occurred in the postischemic limbs in the obtunded patient, thus requir- minished.
in all compartments with a perfu- ing additional diagnostic methods.7 McQueen et al3 reported a mean
sion pressure (∆P) <40 mm Hg. The The absence of pain in a compart- of 7 hours from fracture manipula-
metabolic deterioration observed ment syndrome is often caused by a tion and fixation to the development
was more rapid and severe as the ∆P superimposed central or peripheral of a compartment syndrome in 13
Volume 13, Number 7, November 2005 439
Acute Compartment Syndrome in Lower Extremity Musculoskeletal Trauma
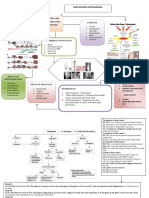
fracture patients undergoing com- Figure 2
partment pressure monitoring. Four
patients had delayed onset of com-
partment syndrome at 14 to 24
hours after fracture manipulation
and fixation.3 However, compart-
ment syndrome occasionally occurs
2 to 4 days after the precipitating
event; therefore, late onset must be
considered.27
Associated conditions can affect
susceptibility to compartment syn-
drome or contribute to missed diag-
nosis. The perfusion gradient may
be inadequate in the presence of
systemic hypotension, even with
compartments that are supple to
physical examination. Anesthetic
techniques have been reported to The mean compartment tissue pressure measurement in a series of tibial shaft
contribute to a delay in diagnosis. fractures. The pressures are presented by location relative to the tibial fracture site.
Compartment syndromes after sur- Data suggest that the highest pressures occur within 5 cm of the fracture. (Adapted
gery done to manage fractures have with permission from Heckman MM, Whitesides TE Jr, Grewe SR, Rooks MD:
been associated with the use of local Compartment pressure in association with closed tibial fractures: The relationship
nerve blocks, epidural anesthesia, between tissue pressure, compartment, and the distance from the site of the
and other forms of regional ane- fracture. J Bone Joint Surg Am 1994;76:1285-1292.)
sthesia.28-32 Patients receiving epi-
dural anesthesia have been reported ment pressure and diastolic blood partments, have gained widespread
to be four times as likely to have a pressure ≥30 mm Hg was main- popularity. Moed and Thorderson35
neurologic complication than those tained and compartments were not reported that no statistically signif-
receiving systemic narcotics.32 Epi- released, patients had normal mus- icant difference was found between
dural anesthesia increases local cle function at the time of follow-up. the measurements obtained with the
blood flow secondary to sympa- Data from preclinical research stud- slit catheter and the side port needle.
thetic blockade, thereby potentially ies suggest that the ischemic thresh- However, measurements with a
exacerbating swelling of an injured old of muscle is a perfusion pressure standard 18-gauge needle were high-
extremity.32 The use of local anes- of at least 20 mm Hg between the er than both the slit catheter and
thetics combined with narcotics compartment pressure and the dia- side port needle by nearly 20 mm
during epidural anesthesia has been stolic pressure.21 In a fracture at risk, Hg. Therefore, a standard 18-gauge
shown to increase the likelihood of measuring compartment pressures needle is less accurate and cannot be
missed compartment syndromes early in the course of treatment can recommended. Several commercial-
and is not recommended in the at- provide a reference point to detect a ly available pressure measurement
risk patient.31,33 trend if later compartment pressure devices are available for determining
measurements are needed. intracompartmental pressures.
Compartment Pressure Various methods of measuring The location in the compartment
Measurement compartment pressures have been from which the measurement is
Sometimes the clinical picture described.34-39 The two most com- taken is important for accuracy.
may be borderline or the patient ex- mon techniques are a slit catheter Seiler et al37 determined that unin-
amination may be equivocal, unreli- and the side port needle. The slit jured compartments exhibited clin-
able, or unobtainable. In such in- catheter is a low-volume infusion ically significant intracompartmen-
stances, measuring compartment technique.34 The measurement cath- tal pressure measurement variability
pressures is recommended to aid the eter may be left in situ within the in the forearm. In their study of 25
decision-making process. McQueen compartment for repeated or contin- patients with closed tibial fracture,
and Court-Brown4 reported a pro- uous compartment pressure mea- Heckman et al23 reported a relation-
spective clinical series using con- surements over a period of hours. ship between compartmental tissue
tinuous compartment monitoring. Side port needles, which were de- pressure and the distance from the
When a difference between compart- veloped to measure multiple com- site of the fracture (Figure 2). Pres-
440 Journal of the American Academy of Orthopaedic Surgeons
Steven A. Olson, MD, and Robert R. Glasgow, MD
sure was measured at the fracture science data suggest that a ∆P value Table 2
site and in 5-cm increments distal of 20 mm Hg is safe. (2) In the inves-
and proximal. The highest pressure tigations of McQueen and Court- Indications for Compartment
recorded was in the deep posterior Brown,4 fasciotomies were per- Pressure Measurement
or anterior compartment, or both. formed for a ∆P value of 30 mm Hg
One or more symptoms of
Eighty-nine percent of compart- and did not identify an absolute min-
compartment syndrome with
ments had the highest pressure mea- imal ∆P threshold. (3) In our experi- confounding factors (eg, neurologic
surement at the fracture site: 5% at ence, many patients in the operating injury, regional anesthesia,
5 cm distal and 2% at 5 cm proxi- room have vasodilatory effects of an- undermedication)
mal. The mean difference in pressure esthesia, leading to transiently low No symptoms other than increased
5 cm from the highest level recorded diastolic blood pressure with normo- firmness or swelling in the limb in an
was 10 mm Hg. These data indicate tensive systolic pressures. In the lat- awake, alert patient receiving
that pressure measurements should ter situation, a patient with com- regional anesthesia for
be performed within all compart- partment pressures in the mid 20s postoperative pain control
ments and at multiple sites, particu- with a supple limb may have a ∆P Unreliable or unobtainable
larly within 5 cm of the level of in- value <30 mm Hg with the diastolic examination with firmness or
jury.23 blood pressure. swelling in the injured extremity
Compartment pressure measure- Prolonged hypotension and a swollen
ment is indicated whenever the diag- Laboratory Tests extremity with equivocal firmness
nosis is uncertain in a patient at risk. Serum creatine phosphokinase, Spontaneous increase in pain in the
Several clinical scenarios fall into which reflects muscle necrosis, has limb after receiving adequate pain
this category (Table 2). One of the been used as an indicator of compart- control
most beneficial uses of compart- ment syndrome.12 Decompression
ment pressure measurement is for should result in a downward trend of
distinguishing an undermedicated creatine phosphokinase levels. Per- sion while minimizing swelling.7
patient from one who is developing sistently high levels or progression When, despite these steps, the clin-
compartment syndrome. This di- indicates inadequate decompression ical diagnosis of compartment syn-
lemma can occur when a long-acting and ongoing muscle necrosis. Myo- drome remains clear, emergent and
anesthetic block wears off without globin, a breakdown product of mus- complete fasciotomy of all compart-
appropriate systemic pain medica- cle cell lysis, is evidenced by myo- ments with elevated pressures is
tion. In this scenario, the pain can be globinuria. It can be misinterpreted necessary to reliably normalize com-
severely increased with passive as hematuria; a definitive diagnosis partment pressures and restore per-
range of motion, and residual pares- is indicated by a positive urine ben- fusion to the affected tissues.
thesias can remain from a nerve zidine test for occult blood in the ab- The length of skin incision has an
block. It is often helpful to obtain a sence of red blood cells. Myoglobin is effect on fascial decompression in
baseline set of pressure measure- toxic to glomeruli of the kidney and the leg associated with an acute
ments in at-risk compartments in a leads to renal failure when the com- compartment syndrome. Some au-
patient who cannot be examined for partment syndrome is not ade- thors favor limited incisions, claim-
an extended period. When subse- quately treated.12 ing low morbidity, while others
quent physical examination findings recommend long incisions, em-
are of concern (eg, increased swell- phasizing that these are required to
Treatment
ing, firmness in the limb), a second decompress affected compartments
set of compartment pressures can Following the diagnosis of impend- adequately.40-42 Several instances
provide evidence of a trend, in addi- ing or true compartment syndrome, have been reported in which the
tion to the actual ∆P value at the immediate measures are necessary skin continued to cause compres-
time of pressure measurement. Ob- to ensure that the deleterious se- sion after fasciotomy through short
tunded patients with an increasing quelae of compartment syndrome incisions.40 Cohen et al40 deter-
trend in pressure should be moni- do not occur. First, casts or occlu- mined the effect of the length of
tored closely. sive dressings should be split com- the skin incision in posttraumatic
At our institution, a ∆P value of pletely. Cast padding or circumfer- compartment syndromes of the
20 mm Hg from measured compart- ential dressings should be released lower extremity treated with fascial
ment pressure to diastolic blood around their entire circumference. decompression using a two-incis-
pressure is an absolute indicator for The affected limb should not be ion technique. The affected com-
fasciotomy. This approach was elevated higher than the patient’s partments initially were released
adopted for three reasons. (1) Basic heart in order to maximize perfu- through 8-cm incisions and the pres-
Volume 13, Number 7, November 2005 441
Acute Compartment Syndrome in Lower Extremity Musculoskeletal Trauma
sures recorded. The skin incisions access to the lateral portion of the At our institution, the fasciotomy
were enlarged by 2-cm increments superficial posterior compartment. site is typically dressed with a
until readings showed no further de- The superficial compartment is mo- wound vac sponge. The patient is re-
crease. The final length of the ex- bilized posteriorly to give access to turned to the operating room 3 to 5
tended incisions averaged 16 cm ± 4 the deep posterior compartment in days later to attempt closure. When
cm. Mean final pressure in the com- order to perform the fasciotomy. muscle necrosis is a possibility, the
partments, which required exten- In the two-incision technique, the patient must return to surgery after
sion of the incisions, was 13 mm Hg, location of the medial skin incision 24 to 48 hours for débridement.
notably less than pre-extension re- is important. The bulk of the mus- Wound closure should not be at-
cordings. Long incisions add little to culature in the superficial posterior tempted until all necrotic tissue is
morbidity and influence neither the compartment is proximal and re- débrided. Direct closure can be at-
complication rate nor the late func- quires a proximal extent to the inci- tempted when the wound approxi-
tional result. Long incisions also sion to adequately decompress the mates without excess tension. When
eliminate the risk of the skin acting region. However, the bulk of the the wound edges will not oppose
as an unrecognized compartment deep posterior musculature is locat- easily, split-thickness skin graft is
envelope, which is especially impor- ed in the distal half of the limb. Ad- indicated.
tant during the hyperemic period equate decompression requires de-
following decompression of an is- taching the soleus origin from the
Outcomes and
chemic compartment.40,42 medial aspect of the tibial shaft.
Complications
Compartment syndromes can oc- Therefore, to adequately decompress
cur in a variety of locations in the all four compartments through two Sheridan and Matsen44 reported the
lower extremity, such as the gluteal incisions, long medial and lateral in- clinical outcome of 44 patients who
musculature, thigh, lower leg, and cisions are required. Foot compart- underwent decompressive fasciot-
foot. Regardless of location, the key ment syndrome is typically treated omy. Twenty-two patients were
in treatment is to adequately decom- with two longitudinal incisions in treated with fasciotomy before 12
press the muscles involved. In the the dorsum of the foot, one centered hours and 22 after 12 hours. In the
gluteal region, a posterior incision over the fourth metatarsal and one first group, 68% of patients had nor-
that provides access to the gluteus over the space between the first and mal lower extremity function at the
maximus and the abductor muscula- second metatarsals. Adequate de- time of final follow-up, compared
ture is adequate. In the thigh, a long compression requires release of the with only 8% in the delayed-
single lateral incision can adequate- fascia of the intrinsic foot muscles treatment group.44
ly decompress the anterior and pos- attaching to the metatarsals. Finkelstein et al45 reported on five
terior compartments. Occasionally, In their study of secondary clo- patients who underwent fasciotomy
a medial adductor incision is re- sure of the skin following fascioto- later than 35 hours after the estab-
quired, as well. A one- or two- my for acute compartment syn- lished diagnosis of lower extremity
incision approach can be used in the drome, Wiger et al43 noted that tight compartment syndrome. In this ret-
lower leg. Generally, a long single closures may increase intramuscular rospective review, one patient died
lateral incision is sufficient for a pressure to dangerous levels. To pre- of multisystem organ failure direct-
four-compartment fasciotomy. vent this, limb swelling must be re- ly related to complications from the
The one-incision procedure duced before secondary closure. Pa- fasciotomy. The remaining four pa-
should be performed through a long tients were encouraged to perform tients required amputation.
incision based over the anterolateral concentric muscular activity and Fitzgerald et al41 reported on
calf. The extended incision is made weight-bearing exercises to assist in long-term sequelae of fasciotomy
from within 5 cm of either end of the reducing elevated intramuscular wounds in 60 patients and demon-
fibula. The basic technique involves pressures of the swollen extremities. strated that the patients frequently
identifying the septum between the Active contraction of muscle en- had complaints at the fasciotomy
anterior and lateral compartments, hances lymph flow, and the normal site. Seventy-seven percent reported
then performing a fasciotomy on increase of hydrostatic pressure is a decreased sensibility, 7% had teth-
each of these compartments. Care powerful edema-reducing mecha- ered tendons, and 13% had recur-
should be taken to avoid injury to nism. At follow-up, there were no rent ulcerations within the wound
the superficial peroneal nerve distal- signs of ischemic muscular contrac- closure area.41 Although a fasciot-
ly. Lateral compartment muscula- ture when intramuscular pressure omy incision does result in some
ture is then elevated off the posteri- did not exceed 30 mm Hg during sec- morbidity to the patient, the mor-
or intramuscular septum. Incision of ondary closure in a normotensive bidity of an incompletely released
this intramuscular septum provides patient.43 compartment, delayed diagnosis,
442 Journal of the American Academy of Orthopaedic Surgeons
Steven A. Olson, MD, and Robert R. Glasgow, MD
or unrecognized compartment syn- patient morbidity. The diagnosis of matic antishock garments. J Trauma
drome is substantially worse. compartment syndrome is usually 1987;27:79-81.
10. Slater RR Jr, Weiner TM, Koruda MJ:
It is not possible to determine the made based on clinical factors, such
Bilateral leg compartment syndrome
precise time a compartment syn- as pain, pressure, paresthesia, paral- complicating prolonged lithotomy
drome begins. Therefore, it is not ysis, and pulselessness. Adjunctive position. Orthopedics 1994;17:954-
possible to know how long a com- use of compartment pressure mea- 959.
partment syndrome has been estab- surements is warranted in the ma- 11. Goldsmith AL, McCallum MI: Com-
lished. Anecdotal reports suggest jority of patients. partment syndrome as a complication
that performing a fasciotomy in the of the prolonged use of the Lloyd-
Davies position. Anaesthesia 1996;
setting of a delayed diagnosis can be References 51:1048-1052.
harmful to the patient and often re-
12. Velmahos GC, Toutouzas KG: Vascu-
sults in amputation. Evidence-based Medicine: Moed and lar trauma and compartment syn-
The dilemma is determining how Thorderson (reference 35) report a dromes. Surg Clin North Am 2002;82:
late a presentation is too late for a comparison study of measurements 125-141.
fasciotomy. In general, clinical as- of intracompartmental pressures 13. Weiner G, Styf J, Nakhostine M, Ger-
sessment of the limb helps with (level II study), and Shakespeare et shuni DH: Effect of ankle position and
a plaster cast on intramuscular pres-
decision-making. The patient with al (reference 34) compared the slit
sure in the human leg. J Bone Joint
clinical evidence of compartment catheter with the wick catheter Surg Am 1994;76:1476-1481.
syndrome who has the ability to vol- (level II study). Younger et al (refer- 14. Younger AS, Curran P, McQueen
untarily contract muscles within the ence 14) compared prospectively MM: Backslabs and plaster casts:
compartment has some viable mus- plaster backslabs and plaster cast in Which will best accommodate in-
creasing intracompartmental pres-
cle; therefore, fasciotomy is indicat- a prospective cohort study (level II
sures? Injury 1990;21:179-181.
ed regardless of the delay. Fascioto- study). 15. Shakespeare DT, Henderson NJ:
my is not performed when a patient Compartmental pressure changes
has clinical evidence of compart- 1. Bhattacharyya T, Vrahas MS: The during calcaneal traction in tibial
ment syndrome with a suspected du- medical-legal aspects of compart- fractures. J Bone Joint Surg Br 1982;
ment syndrome. J Bone Joint Surg Am 64:498-499.
ration ≥8 hours, has neither a nerve
2004;86:864-868. 16. Tornetta P III, French BG: Compart-
injury nor a nerve block that could 2. McQueen MM, Gaston P, Court- ment pressures during nonreamed tib-
potentially alter the clinical exami- Brown CM: Acute compartment syn- ial nailing without traction. J Orthop
nation, and has no demonstrable drome: Who is at risk? J Bone Joint Trauma 1997;11:24-27.
muscle function in any segment of Surg Br 2000;82:200-203. 17. Hak DJ, Johnson EE: The use of the
3. McQueen MM, Christie J, Court- unreamed nail in tibial fractures with
the involved limb. Instead, the limb
Brown CM: Acute compartment syn- concomitant preoperative or intraop-
is aggressively splinted to maintain drome in tibial diaphyseal fractures. erative elevated compartment pres-
a functional position as the muscle J Bone Joint Surg Br 1996;78:95-98. sure or compartment syndrome. J Or-
develops fibrosis and contracture. 4. McQueen MM, Court-Brown CM: thop Trauma 1994;8:203-211.
Supportive care should be given for Compartment monitoring in tibial 18. Moed BR, Strom DE: Compartment
fractures: The pressure threshold for syndrome after closed intramedullary
the potential risk of myoglobinuria,
decompression. J Bone Joint Surg Br nailing of the tibia: A canine model
which may occur in this scenario. 1996;78:99-104. and report of two cases. J Orthop Trau-
5. Mubarak SJ: Technique of diagnosis ma 1991;5:71-77.
and treatment of the lower extremity 19. Georgiadis GM: Tibial shaft fractures
Summary compartment syndromes in children. complicated by compartment syn-
Acute compartment syndrome is Operative Techniques in Ortho- drome: Treatment with immediate
paedics 1995;5:178-189. fasciotomy and locked unreamed
a potentially devastating condition 6. Gulli B, Templeman D: Compart- nailing. J Trauma 1995;38:448-452.
associated with musculoskeletal ment syndrome of the lower extrem- 20. Mawhinney IN, Maginn P, McCoy
trauma. The final common path- ity. Orthop Clin North Am 1994;25: GF: Tibial compartment syndromes
way is cellular ischemia resulting 677-684. after tibial nailing. J Orthop Trauma
7. Ouellette EA: Compartment syn- 1994;8:212-214.
from increased tissue pressure
dromes in obtunded patients. Hand 21. Heckman MM, Whitesides TE Jr,
within an osseofascial compart- Clin 1998;14:431-450. Grewe SR, Judd RL, Miller M,
ment. Compartment syndrome can 8. Janzing H, Broos P, Rommens P: Com- Lawrence JH III: Histologic determi-
occur as a result of many different partment syndrome as a complication nation of the ischemic threshold of
causes, such as fractures, contu- of skin traction in children with fem- muscle in the canine compartment
oral fractures. J Trauma 1996;41:156- syndrome model. J Orthop Trauma
sions, bleeding disorders, burns,
158. 1993;7:199-210.
trauma, postischemic swelling, and 9. Templeman D, Lange R, Harms B: 22. Matava MJ, Whitesides TE Jr, Seiler
gunshot wounds. Prompt diagnosis Lower-extremity compartment syn- JG III, Hewan-Lowe K, Hutton WC:
and treatment are key in limiting dromes associated with use of pneu- Determination of the compartment
Volume 13, Number 7, November 2005 443
Acute Compartment Syndrome in Lower Extremity Musculoskeletal Trauma
pressure threshold of muscle is- anesthesia. Can J Anesth 2000;47: ments in the normal forearm. J Or-
chemia in a canine model. J Trauma 1094-1098. thop Trauma 1993;7:414-416.
1994;37:50-58. 30. Strecker WB, Wood MB, Bieber EJ: 38. Abraham P, Leftheriotis G, Saumet
23. Heckman MM, Whitesides TE Jr, Compartment syndrome masked by JL: Laser Doppler flowmetry in the di-
Grewe SR, Rooks MD: Compartment epidural anesthesia for postoperative agnosis of chronic compartment syn-
pressure in association with closed pain. J Bone Joint Surg Am 1986;68: drome. J Bone Joint Surg Br 1998;80:
tibial fractures: The relationship be- 1447-1448. 365-369.
tween tissue pressure, compartment, 31. Dunwoody JM, Reichert CC, Brown 39. Willy C, Gerngross H, Sterk J: Mea-
and the distance from the site of the KL: Compartment syndrome associ-
surement of intracompartmental
fracture. J Bone Joint Surg Am 1994; ated with bupivacaine and fentanyl
pressure with use of a new electronic
76:1285-1292. epidural analgesia in pediatric ortho-
transducer-tipped catheter system.
24. Har-Shai Y, Silbermann M, Reis ND, paedics. J Pediatr Orthop 1997;17:
J Bone Joint Surg Am 1999;81:158-
et al: Muscle microcirculatory im- 285-288.
168.
pairment following acute compart- 32. Iaquinto JM, Pienkowski D, Thorns-
ment syndrome in the dog. Plast Re- berry R, Grant S, Stevens DB: In- 40. Cohen MS, Garfin SR, Hargens AR,
constr Surg 1992;89:283-289. creased neurologic complications as- Mubarak SJ: Acute compartment syn-
25. Bernot M, Gupta R, Dobrasz J, Chance sociated with postoperative epidural drome: Effect of dermotomy on fascial
B, Heppenstall RB, Sapega A: The ef- analgesia after tibial fracture fixation. decompression in the leg. J Bone Joint
fect of antecedent ischemia on the tol- Am J Orthop 1997;26:604-608. Surg Br 1991;73:287-290.
erance of skeletal muscle to increased 33. Mubarak SJ, Wilton NC: Compart- 41. Fitzgerald AM, Gaston P, Wilson Y,
interstitial pressure. J Orthop Trauma ment syndromes and epidural analge- Quaba A, McQueen MM: Long-term
1996;10:555-559. sia. J Pediatr Orthop 1997;17:282-284. sequelae of fasciotomy wounds. Br J
26. Vollmar B, Westermann S, Menger 34. Shakespeare DT, Henderson NJ, Plast Surg 2000;53:690-693.
MD: Microvascular response to com- Clough G: The slit catheter: A com- 42. Rush DS, Frame SB, Bell RM, Berg EE,
partment syndrome-like external parison with the wick catheter in the Kerstein MD, Haynes JL: Does open
pressure elevation: An in vivo fluores- measurement of compartment pres- fasciotomy contribute to morbidity
cence microscopic study in the ham- sure. Injury 1982;13:404-408. and mortality after acute lower ex-
ster striated muscle. J Trauma 1999; 35. Moed BR, Thorderson PK: Measure- tremity ischemia and revasculariza-
46:91-96. ment of intracompartmental pres- tion? J Vasc Surg 1989;10:343-350.
27. Matsen FA III, Winquist RA, Krug- sure: A comparison of the slit cathe- 43. Wiger P, Tkaczuk P, Styf J: Secondary
mire RB Jr: Diagnosis and manage- ter, side-ported needle, and simple wound closure following fasciotomy
ment of compartmental syndromes. needle. J Bone Joint Surg Am 1993;75: for acute compartment syndrome in-
J Bone Joint Surg Am 1980;62:286- 231-235. creases intramuscular pressure. J Or-
291. 36. Uppal GS, Smith RC, Sherk HH, thop Trauma 1998;12:117-121.
28. Hyder N, Kessler S, Jennings AG, De Mooar P: Accurate compartment 44. Sheridan GW, Matsen FA III: Fasciot-
Boer PG: Compartment syndrome in pressure measurement using the In- omy in the treatment of the acute
tibial shaft fracture missed because of tervenous Alarm Control (IVAC) compartment syndrome. J Bone Joint
a local nerve block. J Bone Joint Surg Pump: Report of a technique. J Orthop Surg Am 1976;58:112-115.
Br 1996;78:499-500. Trauma 1992;6:87-89. 45. Finkelstein JA, Hunter GA, Hu RW:
29. Ananthanarayan C, Castro C, McKee 37. Seiler JG III, Womack S, De L’Aune Lower limb compartment syndrome:
N, Sakotic G: Compartment syn- WR, Whitesides TE, Hutton WC: In- Course after delayed fasciotomy.
drome following intravenous regional tracompartmental pressure measure- J Trauma 1996;40:342-344.
444 Journal of the American Academy of Orthopaedic Surgeons
You might also like
- Acute Compartment Syndrome in Lower Extremity.3Document9 pagesAcute Compartment Syndrome in Lower Extremity.3marsss.medNo ratings yet
- Imágenes de RM de Trauma MuscularDocument23 pagesImágenes de RM de Trauma Muscularmicamart.94No ratings yet
- Fasciotomy in The Treatment of The AcutDocument4 pagesFasciotomy in The Treatment of The AcutWarut BoonamnuaykitNo ratings yet
- Myofascial Genesis of PainDocument11 pagesMyofascial Genesis of PainMarita PalacoNo ratings yet
- SD Compartimental Cordón de Zapato + VacDocument4 pagesSD Compartimental Cordón de Zapato + Vacyerec51683No ratings yet
- 1091 FullDocument9 pages1091 FulldrsubramanianNo ratings yet
- Sd. Compartimental y AR A CL 2022Document19 pagesSd. Compartimental y AR A CL 2022Alejandra SanchezNo ratings yet
- MED-SURG NURSING: CARE OF CLIENTS WITH PAINDocument6 pagesMED-SURG NURSING: CARE OF CLIENTS WITH PAINELAGNE MEDINANo ratings yet
- Bowyer2015 Article LowerExtremityFasciotomyIndicaDocument16 pagesBowyer2015 Article LowerExtremityFasciotomyIndicaFaridatul IsniyahNo ratings yet
- Burnout, Compassion Fatigue, Compassion Satisfaction, and Secondary Traumatic Stress in Trauma NursesDocument10 pagesBurnout, Compassion Fatigue, Compassion Satisfaction, and Secondary Traumatic Stress in Trauma NursesambreenNo ratings yet
- Copaxone - Ms Drug StudyDocument1 pageCopaxone - Ms Drug StudygraceNo ratings yet
- Acute Subdural Hematoma Because of Boxing.2Document6 pagesAcute Subdural Hematoma Because of Boxing.2Mon ChávezNo ratings yet
- CrossDocument10 pagesCrossvalentinaro73No ratings yet
- Compartment Syndrome: It Occurs When Excessive Pressure Builds Up Inside An Enclosed Muscle Space in The BodyDocument1 pageCompartment Syndrome: It Occurs When Excessive Pressure Builds Up Inside An Enclosed Muscle Space in The BodyRachelle Ann CarilloNo ratings yet
- Vascular Cognitive Impairment: Mechanisms EpidemiologyDocument1 pageVascular Cognitive Impairment: Mechanisms EpidemiologyRaúl ChoqueNo ratings yet
- Joint Pain One PagerDocument3 pagesJoint Pain One PagermustafaNo ratings yet
- Critical Care Cardiovascular Disease Chapter 22: Classification, Pathophysiology, and Management of ShockDocument44 pagesCritical Care Cardiovascular Disease Chapter 22: Classification, Pathophysiology, and Management of Shockismi latifahNo ratings yet
- Aspectos Neurológicos Del Trauma Craneoencefálico IRPDocument10 pagesAspectos Neurológicos Del Trauma Craneoencefálico IRPAndres FierroNo ratings yet
- 10.1038@s41572 019 0088 XDocument1 page10.1038@s41572 019 0088 XPierrotNo ratings yet
- Josptcases 2021 9976Document4 pagesJosptcases 2021 9976Ludmila PirtacNo ratings yet
- Lesiones SindesmalesDocument9 pagesLesiones SindesmalesDaniel Cancino CallirgosNo ratings yet
- Impact of Varying Degrees of Peripheral Nerve BlockadeDocument7 pagesImpact of Varying Degrees of Peripheral Nerve BlockadeAlejandra SanchezNo ratings yet
- Myasthenia Gravis: Immunopathogenesis, Diagnosis, and ManagementDocument28 pagesMyasthenia Gravis: Immunopathogenesis, Diagnosis, and ManagementAllan SalmeronNo ratings yet
- Peripheral Nerve.10Document27 pagesPeripheral Nerve.10Novanda RizkyNo ratings yet
- DEEP TISSUE PRESSURE INJURY: A CLINICAL REVIEW OF BEST NURSING PRACTICESDocument8 pagesDEEP TISSUE PRESSURE INJURY: A CLINICAL REVIEW OF BEST NURSING PRACTICESwennyNo ratings yet
- Regeneration of Injured Skeletal Muscle After The Injury: Review ArticleDocument9 pagesRegeneration of Injured Skeletal Muscle After The Injury: Review ArticleSahira Rivera DroguettNo ratings yet
- Thoracic Outlet SyndromeDocument11 pagesThoracic Outlet SyndromeTan Zhen XinNo ratings yet
- POSITION EMS Spinal Precautions and The Use of The Long BackboardDocument2 pagesPOSITION EMS Spinal Precautions and The Use of The Long BackboardJade OttoniNo ratings yet
- CURS 15, 16-Sd Coronariene Acute Si ICDocument73 pagesCURS 15, 16-Sd Coronariene Acute Si ICCristian Banarie100% (1)
- Clarissa Maharani Gandi LP IGD Sem.6 Kelas ADocument8 pagesClarissa Maharani Gandi LP IGD Sem.6 Kelas ARisa RissaNo ratings yet
- Amputations in Natural Disasters and Mass Casualties Staged ApproachDocument6 pagesAmputations in Natural Disasters and Mass Casualties Staged ApproachIcha YulianiNo ratings yet
- Fneur 14 1104817Document6 pagesFneur 14 1104817geowalker7092No ratings yet
- Dr. Kiki - Pengantar Trauma UpdateDocument20 pagesDr. Kiki - Pengantar Trauma UpdateRsud Malinau Ppk BludNo ratings yet
- Shock: Classification, Pathophysiology, and Approach To ManagementDocument45 pagesShock: Classification, Pathophysiology, and Approach To ManagementClaudia IsabelNo ratings yet
- PBL - NervousDocument2 pagesPBL - Nervousgie sarcedaNo ratings yet
- Soft tissue healing techniquesDocument6 pagesSoft tissue healing techniquesPamela CoralNo ratings yet
- Johnson Et Al 2007 The Effect of Anterior Versus Posterior Glide Joint Mobilization On External Rotation Range ofDocument12 pagesJohnson Et Al 2007 The Effect of Anterior Versus Posterior Glide Joint Mobilization On External Rotation Range ofAhmed SamirNo ratings yet
- OsteosarkomaDocument2 pagesOsteosarkomaLinawati DLNo ratings yet
- 2019 Role of The Extracellular Matrix in Muscle InjuriesDocument3 pages2019 Role of The Extracellular Matrix in Muscle InjuriesPhysio AcademyNo ratings yet
- Bone FractureDocument20 pagesBone Fracturemb5bariyaNo ratings yet
- Compartment Syndrome Hand and ForearmDocument33 pagesCompartment Syndrome Hand and ForearmProfesseur Christian Dumontier100% (2)
- Fneur 13 821097Document4 pagesFneur 13 821097Jeremi SetiawanNo ratings yet
- Pain Science in PracticeDocument4 pagesPain Science in PracticeIan PeroniNo ratings yet
- Compartment SyndromeDocument10 pagesCompartment SyndromerobbyNo ratings yet
- Muscle Strain Injuries: Tero A.H. Järvinen, Minna Kääriäinen, Markku Järvinen,,, and Hannu KalimoDocument7 pagesMuscle Strain Injuries: Tero A.H. Järvinen, Minna Kääriäinen, Markku Järvinen,,, and Hannu Kalimonnick0No ratings yet
- Emergency Surgery 3: Diagnosis and Treatment of Acute Extremity Compartment SyndromeDocument12 pagesEmergency Surgery 3: Diagnosis and Treatment of Acute Extremity Compartment SyndromeIlham RamadhanNo ratings yet
- CXZZXDocument7 pagesCXZZXLeonardo SanchezNo ratings yet
- Head Neck Spine Conditions SummaryDocument5 pagesHead Neck Spine Conditions SummaryDominic c. CastañedaNo ratings yet
- Sindrome Corazon RotoDocument6 pagesSindrome Corazon RotoDiana Milena Luna PinzonNo ratings yet
- Pcu 2015 04 2Document7 pagesPcu 2015 04 2Nurdiana Desyy LylaNo ratings yet
- Blue 3D Illustration Guess The Word Game Fun Presentation 2 PDFDocument13 pagesBlue 3D Illustration Guess The Word Game Fun Presentation 2 PDFAESTHETIC PHOTONo ratings yet
- Circulatory Responses To Voluntary and Electrically Induced Muscle Contractions in HumansDocument8 pagesCirculatory Responses To Voluntary and Electrically Induced Muscle Contractions in HumansLuis Fernando OsorioNo ratings yet
- TBICossu GDocument13 pagesTBICossu GKapil LakhwaraNo ratings yet
- Anesthesia Regional y Sindrome Compartamental Nov 21Document5 pagesAnesthesia Regional y Sindrome Compartamental Nov 21ema moralesNo ratings yet
- Jurnal RadiologiDocument12 pagesJurnal Radiologiimamlutfi13No ratings yet
- C S: O E: Ompartment Yndrome AN Rthopedic MergencyDocument5 pagesC S: O E: Ompartment Yndrome AN Rthopedic MergencyAndreew SoscueNo ratings yet
- Pleurisy: Risk Factors/ Causes DX Test ManagementDocument6 pagesPleurisy: Risk Factors/ Causes DX Test ManagementiluvmunicamuchNo ratings yet
- Athletic Injuries of The ThoracicDocument20 pagesAthletic Injuries of The ThoracicGrado CristianNo ratings yet
- Facial Nerve Trauma Clinical Evaluation And.41Document15 pagesFacial Nerve Trauma Clinical Evaluation And.41Razaria DailyneNo ratings yet
- Articulo Clavicula 1Document9 pagesArticulo Clavicula 1Emmy LiraNo ratings yet
- Subaidah 7/1/1958 362516 Ods Glaukoma Os Pe + Iol FD WA GA 2Document1 pageSubaidah 7/1/1958 362516 Ods Glaukoma Os Pe + Iol FD WA GA 2Azmi FarhadiNo ratings yet
- Marfan Syndrome A Clinical Update JAAOSDocument7 pagesMarfan Syndrome A Clinical Update JAAOSAzmi FarhadiNo ratings yet
- NexusDocument6 pagesNexusAzmi FarhadiNo ratings yet
- The Governance of Islamic Boarding Schools in IndonesiaDocument17 pagesThe Governance of Islamic Boarding Schools in IndonesiaAzmi FarhadiNo ratings yet
- Agricultural InjuryDocument21 pagesAgricultural InjuryAzmi FarhadiNo ratings yet
- Subaxial Cervical Spine Trauma JAAOSDocument12 pagesSubaxial Cervical Spine Trauma JAAOSAzmi FarhadiNo ratings yet
- Thoracolumbar Spine Trauma I Evaluation and Classification JAAOSDocument8 pagesThoracolumbar Spine Trauma I Evaluation and Classification JAAOSAzmi FarhadiNo ratings yet
- Extensor Tendon Injuries in The Hand JAAOSDocument8 pagesExtensor Tendon Injuries in The Hand JAAOSAzmi FarhadiNo ratings yet
- Hannover Polytrauma Score AssessmentDocument2 pagesHannover Polytrauma Score AssessmentAzmi FarhadiNo ratings yet
- Idiopathic Congenital Talipes Equinovarus PDFDocument10 pagesIdiopathic Congenital Talipes Equinovarus PDFEric RothNo ratings yet
- Damage Control Orthopaedics in Spinal Trauma JAAOSDocument12 pagesDamage Control Orthopaedics in Spinal Trauma JAAOSAzmi FarhadiNo ratings yet
- The Orthopaedic Implications of Diphosphonate Therapy: Review ArticleDocument8 pagesThe Orthopaedic Implications of Diphosphonate Therapy: Review ArticleroyNo ratings yet
- ASIA ISCOS IntlWorksheet 2019Document2 pagesASIA ISCOS IntlWorksheet 2019Anastasia CanahuateNo ratings yet
- Malignant Bone Pain Pathophysiology and TreatmentDocument18 pagesMalignant Bone Pain Pathophysiology and TreatmentAzmi FarhadiNo ratings yet
- Treatment of Blast Injuries of The Extremity JAAOSDocument5 pagesTreatment of Blast Injuries of The Extremity JAAOSAzmi FarhadiNo ratings yet
- A Systematic Summary of Systematic Reviews On The Topic of The Anterior Cruciate LigamentDocument23 pagesA Systematic Summary of Systematic Reviews On The Topic of The Anterior Cruciate LigamentAzmi FarhadiNo ratings yet
- 10.1097@00124635 199701000 00001Document10 pages10.1097@00124635 199701000 00001Azmi FarhadiNo ratings yet
- Primary Osteoporosis in Postmenopausal WomenDocument5 pagesPrimary Osteoporosis in Postmenopausal WomenAzmi FarhadiNo ratings yet
- Spondylolysis and Spondylolisthesis in Children and Adolescents JAAOSDocument8 pagesSpondylolysis and Spondylolisthesis in Children and Adolescents JAAOSAzmi FarhadiNo ratings yet
- Wear and Osteolysis Around Total Knee Arthroplasty JAAOSDocument12 pagesWear and Osteolysis Around Total Knee Arthroplasty JAAOSAzmi FarhadiNo ratings yet
- Safe Tourniquet Use A Review of The Evidence JAAOSDocument10 pagesSafe Tourniquet Use A Review of The Evidence JAAOSAzmi FarhadiNo ratings yet
- Fat EmbolismDocument10 pagesFat EmbolismAzmi FarhadiNo ratings yet
- TB Arthritis Ankle Mimicking SynovitisDocument8 pagesTB Arthritis Ankle Mimicking SynovitisAzmi FarhadiNo ratings yet
- Supracondylar Fractures of The Humerus in Children.3Document8 pagesSupracondylar Fractures of The Humerus in Children.3Azmi FarhadiNo ratings yet
- True Ponte Osteotomy Ponte 2018Document10 pagesTrue Ponte Osteotomy Ponte 2018Azmi FarhadiNo ratings yet
- Venous Thromboembolism in MalignancyDocument3 pagesVenous Thromboembolism in MalignancyAzmi FarhadiNo ratings yet
- USS Universal Spine SystemDocument32 pagesUSS Universal Spine SystemAzmi Farhadi100% (1)
- Varus Osteotomy French 1959Document3 pagesVarus Osteotomy French 1959Azmi FarhadiNo ratings yet
- Water Vascular System of AsteriasDocument3 pagesWater Vascular System of AsteriasCyanDes50% (2)
- Chemical Classification of HormonesDocument65 pagesChemical Classification of HormonesetNo ratings yet
- Cfasmsumain Fplereview2022 PhycologyDocument149 pagesCfasmsumain Fplereview2022 PhycologyPilihp Elessej Yaj NiuqidcidNo ratings yet
- BIOCHEMISTRY AND METABOLISMDocument63 pagesBIOCHEMISTRY AND METABOLISMdeepakNo ratings yet
- DigestionDocument5 pagesDigestionRashri SharmaNo ratings yet
- Serum Protein Multi-Calibrator InsertDocument6 pagesSerum Protein Multi-Calibrator InsertDaniel VargasNo ratings yet
- Animal Kingdom Digital NotesDocument20 pagesAnimal Kingdom Digital NotesKshreeNo ratings yet
- Animal and Plant Cell ComparisonDocument4 pagesAnimal and Plant Cell ComparisonMd A RAZZAKNo ratings yet
- ANAT.301 3 (1-2) : Veterinary Anatomy - I Theory One Class/ Week 20 Mrks Practical Two Classes/ WeekDocument34 pagesANAT.301 3 (1-2) : Veterinary Anatomy - I Theory One Class/ Week 20 Mrks Practical Two Classes/ WeekIftikhar hussainNo ratings yet
- Friedman 2018Document7 pagesFriedman 2018Genshin SatuNo ratings yet
- Breastfeeding Challenges and The Preterm Mother-Infant Dyad A Conceptual ModelDocument10 pagesBreastfeeding Challenges and The Preterm Mother-Infant Dyad A Conceptual Modelunisa magisterNo ratings yet
- Chest TraumaDocument47 pagesChest Traumafrenee aradanasNo ratings yet
- Learning Activity Sheet Biotechnology 8Document11 pagesLearning Activity Sheet Biotechnology 8Jaeda BaltazarNo ratings yet
- Veterinary Anatomy of Domestic Mammals (PDFDrive)Document646 pagesVeterinary Anatomy of Domestic Mammals (PDFDrive)Misaaaki CristinaNo ratings yet
- 1.question Bank - IGMCRI (Biochemistry)Document11 pages1.question Bank - IGMCRI (Biochemistry)Anirudh BNo ratings yet
- Glycogen MetabolismDocument11 pagesGlycogen MetabolismShruti MishraNo ratings yet
- Gas Exchange Self StudyDocument5 pagesGas Exchange Self Study4E-27 Tsoi Cheuk Ying (Ada)No ratings yet
- Parasitology Lect. (4) : Preparation of Solutions For Wet MountDocument5 pagesParasitology Lect. (4) : Preparation of Solutions For Wet MountAbdul hadiNo ratings yet
- Darlene Krizian G. Dayuha: Bio100 - General BotanyDocument2 pagesDarlene Krizian G. Dayuha: Bio100 - General BotanyDarlene KrizianNo ratings yet
- Metabolic Effects of 3,5-Diiodo-L-Thyronine Giammanco M Et AlDocument11 pagesMetabolic Effects of 3,5-Diiodo-L-Thyronine Giammanco M Et AlMarco GiammancoNo ratings yet
- Capítulo 2 The Structure of Unconditioned BehaviorDocument14 pagesCapítulo 2 The Structure of Unconditioned BehaviorAngela JordáNo ratings yet
- Nutrition: Mark J. Burkitt D.PhilDocument4 pagesNutrition: Mark J. Burkitt D.PhilAnis RanisNo ratings yet
- DehydrationDocument16 pagesDehydrationBenben LookitandI'mNo ratings yet
- 13 The Respiratory SystemDocument5 pages13 The Respiratory SystemCristina AdolfoNo ratings yet
- Animal KingdomDocument13 pagesAnimal KingdomAanchal Pandey100% (2)
- Introduction To Urine Analysis: General VeiwDocument8 pagesIntroduction To Urine Analysis: General Veiwبلسم محمود شاكرNo ratings yet
- Animal Genetics and Breeding (PDFDrive)Document208 pagesAnimal Genetics and Breeding (PDFDrive)Hồng Quân DươngNo ratings yet
- Antiarrhythmic Drug GuideDocument42 pagesAntiarrhythmic Drug GuideRamadi PrameelaNo ratings yet
- Resistance of The Body To Infection: Maria Verena R. Remudaro, MDDocument69 pagesResistance of The Body To Infection: Maria Verena R. Remudaro, MDRen AlvNo ratings yet
- The Octopus 2Document29 pagesThe Octopus 2Carlos AlejandroNo ratings yet