Professional Documents
Culture Documents
Blood Transfusion: Etiology of Blood Cell
Blood Transfusion: Etiology of Blood Cell
Uploaded by
bunso padillaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Blood Transfusion: Etiology of Blood Cell
Blood Transfusion: Etiology of Blood Cell
Uploaded by
bunso padillaCopyright:
Available Formats
to stimulate the production of mature red blood cells, to
BLOOD TRANSFUSION maintain healthy oxygen levels in our tissues.
Course Outline
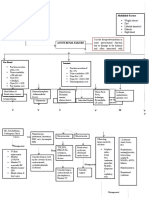
ETIOLOGY OF BLOOD CELL
DEFINITION OF BLOOD Blood cells do not originate in the bloodstream itself but in
PORTIONS OF THE BLOOD specific blood-forming organs, notably the marrow of certain
ETIOLOGY OF BLOOD CELL
bones. In the human adult, the bone marrow produces all the
UNDERSTANDING BLOOD TRANSFUSION THERAPY
ELIGIBLE & INELIGIBLE TO BLOOD DONATION red blood cells.
BLOOD CLOTTING FACTORS
NURSE’S RESPONSIBILITY The lymphatic tissues, particularly the thymus, the spleen, and
TRANSFUSION PRECAUTIONS the lymph nodes, produce the lymphocytes. And then, the
DOCUMENTATION reticuloendothelial tissues of the spleen, liver, lymph nodes,
BLOOD PRODUCTS and other organs produce the monocytes.
BLOOD TRANSFUSION
TRANSFUSION REACTIONS UNDERSTANDING BLOOD TRANSFUSION THERAPY
BLOOD is a mixture of cells and a complex TRANSPORT BLOOD TRANSFUSION
mechanism
▪ The infusion of whole blood or blood component into
T – transports hormones the patient’s venous circulation.
▪ Lifesaving therapy for patients with medical or surgical
R – removes waste products conditions that need blood.
▪ RA 7719 [National Blood Services Act of 1994] – an act
R – regulates body temperature of promoting voluntary blood donation.
▪ The volume of fluids will adjust within a few hours
P – protects the body
after your donation. The RBC will be replaced within a
P – promotes hemostasis few weeks.
▪ The minimum interval between 2 donations is 12
S – supplies oxygen weeks or 3 months.
PORTIONS OF THE BLOOD Indications of blood transfusion:
Blood is composed of 55% of plasma and 45% cellular (a) Hemorrhage caused by trauma
components. The body contains 10-12 pints (5-6 L) of blood, (b) High blood loss surgery
your whole blood donation approximately 1 pint or equivalent (c) Hemolysis
to 450-500 ml. (d) Anemia
Plasma is the main component of blood and consists mostly of Purposes:
water with CHON, ions, nutrients, lipids, glucose, and salt mixed
in. To restore and maintain blood volume.
To improve the oxygen-carrying capacity of the blood.
Platelets is a blood cell that is responsible for blood clotting. It To replace deficient blood components.
stops the bleeding and promote blood clotting.
WHO CAN & WHO CAN’T GIVE BLOOD
White blood cells are cells that play a major role in defense in
microorganisms, so they fight viruses, bacteria, and other ▪ Eligible donors must:
foreign invaders that threaten your health. 18 and above
Weigh at least 110lb
Red blood cells are responsible for carrying and transportation Skin disease free
of oxygen and carbon dioxide. Not donated in the past 56 days
Hgb level is at least 12.5g/dl [women] or
Erythropoietin is a hormone that is produced by the kidneys
13.5g/dl [men]
when oxygen levels in the blood are low. It acts in bone marrow
Normal VS
Blood volume collected will depend mainly on Gently suspend the RBC within the plasma
your body weight. Observe signs of hemolytic reaction that generally
▪ Ineligible donors include: occurs within first 10-15 minutes.
HIV, AIDS, STD
Took illegal drugs Shivering, headache, low back pain, increased RR & PR,
hemoglobinuria, oliguria, and hypotension
Had sex with prostitutes in the past 12
months Observe signs of febrile reaction that usually occurs
Had sex with anyone above categories withing 30 minutes
Pregnant
Shaking, headache, elevated temperature, back pain,
Hepatitis B/C
confusion, and hematemesis.
Certain types of cancer
Hemophilia Act promptly if the patient develops bronchospasm
Who have receive clotting factor and wheezing. This may indicate allergic reaction or
concentration anaphylaxis.
Chronic alcoholism
INTERVENTIONS PRIOR BLOOD TRANSFUSION
Body piercing and tattooing
✓ Proper cross-matching of donor’s and recipient’s blood
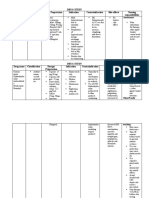
BLOOD CLOTTING FACTORS to assure compatibility.
I Fibrinogen ✓ After receiving delivery from blood bank, check if you
II Prothrombin receive both the product and the transfusion record
III Thromboplastin that corresponds to it.
IV Calcium ✓ Inspect the label, integrity of unit, and the appearance.
V Proaccelerin
VII Proconvertin (stable factor) SAFETY PRECAUTIONS
VIII Antihemophilic Factor A
IX Antihemophilic Factor B ❖ PPE
X Stuart-Prower Factor ❖ Hand hygiene or hand washing.
XI Plasma thromblastin antecedent ❖ If possible, use needleless system.
XII Hageman factor ❖ Do not recap the needle.
XIII Fibrin stabilizing factor
❖ Observe proper waste disposal.
NURSE’S RESPONSIBILITY ❖ Don’t touch blood with bare hands.
❖ Secure blood bag.
NURSES MUST: ❖ Always double or triple check.
❖ Perform disinfection technique.
Assure that informed consent has been obtained prior
starting transfusion.
TRANSFUSION PRECAUTIONS
Patient education regarding benefits, risks,
alternatives to transfusion [iron/ ESAs] 1 Don’t add medications to the blood.
2 Don’t transfuse if you suspect or discover discrepancy
RESPONSIBILITIES:
in blood number, blood type or pt identification
Check blood or blood components have been typed & number.
cross-matched for compatibility. Two nurses verify the 3 Don’t piggyback blood into the port of an existing
blood type, Rh factor, serial number, extraction date infusion set.
and expiration date.
Don’t administer blood without warming it. DOCUMENTATION
Obtain VS before and 15 minutes after transfusion. □ Date and time of transfusion was started and
Always have an isotonic solution set up as a primary completed.
line along with the transfusion.
□ Name of HCW who verified information of the patient
Maintain standard precaution in handling blood or IV
and the blood.
equipment
□ Type of catheter and gauge.
Inform the client or assure them that risk for AIDS is
□ Total amount of transfusion.
minimal because the blood is screened.
□ Pt vital signs before and after transfusion
□ Infusion device It is made from 1 unit partially thawed FFP and the amount is
□ Flow rate and blood warmer if used 15mL. It is very rich in fibrinogen and Factor VIII.
□ Name of component, unit number Indications: it helps control bleeding or immediately prior to an
□ Evidence of possible transfusion reaction and the invasive procedure in patients with significant
interventions done. hypofibrinogenemia. It contains specific proteins for clotting.
□ Patient’s outcome. Indicated clients with missing factor VIII and factor XIII this
helps platelets stick together.
RISKS OF BLOOD TRANSFUSION Nursing Considerations: crossmatching is not required but it
should be ABO compatible. It must not store in ward fridges if
(1) HIV stored in fridge, require re-thawing by blood bank.
(2) Hepatitis B Administered at a rate of 5-10 minutes per unit. Faster
(3) Hepatitis C administration is for acute bleeding situations only.
(4) BT reactions
BLOOD TRANSFUSION
BLOOD PRODUCTS
EQUIPMENT NEEDED FOR BLOOD TRANSFUSION
WHOLE BLOOD
1) Blood product
Indications: to restore blood volume from hemorrhaging, 2) Blood transfusion set
trauma, or burn patients. One unit is given over 2-3 hours or 4- 3) IVF = 0.9 NaCl
6 hours. The total volume is approximately 450-500mL.
4) IV pole
Nursing Considerations: do not infuse more than 4 hours, warm 5) IV catheter
the blood if giving large quantity, and stop when the patient 6) Disposable gloves
can’t tolerate the circulating volume. 7) Micropore tape
PACKED RED BLOOD CELL (PRBC) PRE-ASSESSMENT
Indications: to restore or maintain the oxygen-carrying ▪ Secure BT consent
capacity, correct anemia or surgical blood loss and the total
▪ Obtain baseline vital signs, lung sounds, and urinary
volume of blood is 250mL.
output.
Nursing Considerations: do not infuse for more than 6 hours. ▪ Review recent laboratory values.
RBCs have the same oxygen-carrying capacity as whole blood, ▪ Ask for previous transfusion reactions.
minimizing the hazard of volume overload. ▪ Inspect IV insertion site and check type of solution.
PLATELETS
DOING BLOOD TRANSFUSION
Indications: to treat thrombocytopenia, acute leukemia, and
1) Determine whether patient knows reason for
marrow aplasia. The total volume is approximately 50mL.
transfusion.
Nursing Considerations: RH type matching is compared to ABO 2) Explain to patient what will happen. Check for signed
compatibility is preferable with repeated platelet transfusions. consent. Advise the patient to report any hemolytic or
100mL is infuse over 15 minutes. Administer at 150 to 200mL febrile reactions.
per hour or as rapidly as the pt can tolerate and don’t exceed to
3) Give pre-medications, if ordered by the physician.
4 hours. Avoid administering platelets to febrile patients.
4) Hang container of NSS with blood transfusion. Initiate
FRESH FROZEN PLASMA (FFP) infusion.
5) Start IV with gauge 18 or 19. Run normal saline at KVO.
Indications: one unit is 200-250mL and this can treat
6) Obtain the blood product.
postsurgical hemorrhage/shock and correct an undetermined
coagulation factor deficiency. 7) Complete identification and checks.
8) Take baseline VS.
Nursing Considerations: RH type matching is compared to ABO 9) Start infusion of blood [thawed].
compatibility is preferable with repeated platelet transfusions. ✓ Prime in-line filter with blood.
Large volume of FFP may require correction for hypocalcemia. ✓ Start administration slowly.
Citric acid in FFP binds in calcium.
✓ Stay with the patient for the first 5 to 15
CRYOPRECIPITATE minutes of transfusion.
✓ Check vital signs q15 for the first hour
✓ Observe for blood transfusion reactions. Nursing Interventions: administer antihistamines
10) Consume blood within 6 hours. Prevention: premedicate with antihistamine if pt has hx of
11) Assess frequently for transfusion reactions. allergic reactions. Observe pt closely for the first 30 minutes
of the transfusion.
TERMINATING THE TRANSFUSION (iv) Plasma Protein Incompatibility
Nursing Interventions: treat shock by administering O2,
➢ Flush the blood tubing with an adequate amount of
fluids, epinephrine, or steroid as ordered.
NSS according to patient’s condition.
Prevention: transfuse only IgA-deficient blood or well
➢ On a Y-type set, close the clamp on the bloodline and
washed RBCs.
open the clamp on the saline solution line.
(v) Bacterial Contamination
➢ Discard tubing, filter, and blood bag according to
Nursing Interventions: broad-spectrum antibiotics and
policy of institution.
steroids treatment.
➢ Reassess the patient’s condition and vital signs.
Prevention: inspect blood prior transfusion for gas, clot, &
dark purple color. Use air free, touch-free methods to draw
TRANSFUSION REACTIONS
& deliver blood. Maintain strict storage control. Change the
DEFINITION blood tubing and filter q4h. Infuse each unit of blood over2-
4hrs; terminate the infusion if the time period exceeds
➢ Reaction of the body to transfusion of blood that’s not 4hours. Maintain sterile technique when administering
compatible with its own blood. blood products.
➢ Usually attributed to major antigen-antibody (vi) Circulation Overload
reactions. Nursing Interventions: stop infusion and maintain IV with
➢ Acute transfusion reactions usually appear within the NSS. Administer O2 while the head is elevated. Administer
first 5 to 15 minutes after transfusion started. diuretics as ordered by the physician.
Prevention: transfuse blood slowly. Don’t exceed 2 units in
WHEN BT REACTION OCCURS… SPIN
4 hours; less for elderly, infants or pt with cardiac
S – stop the infusion conditions.
P- pulse and other vital signs assessment
I – infuse NSS
N – notify the physician
TRANSFUSION REACTION MANAGEMENT
(i) Hemolytic
Nursing Interventions: keep track BP, treat shock as
indicated [IVF, O2, epinephrine, diuretic, and vasopressor].
Obtain post transfusion reaction, blood and urine sample
for evaluation. Observe signs of hemorrhage resulting from
DIC
Prevention: Before transfusion, check donor & recipient
blood types to ensure compatibility. Identify pt with
another nurse or doctor present. Transfuse the blood slowly
for the first 15 to 20 minutes closely observe the patient for
the first 30 minutes of the transfusion.
(ii) Febrile
Nursing Interventions: Administer antipyretic, antihistamine
or meperidine.
Prevention: premedicate with an antipyretic, antihistamine
or steroid. Use leukocyte-poor or washed RBCs. Use
leukocyte-poor removal filter specific to the component.
(iii) Allergic Reaction
You might also like
- BMT Flow Chart - 2018 PDFDocument1 pageBMT Flow Chart - 2018 PDFMisty Long NgenuyenNo ratings yet
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Nursing Care of Stroke - NewDocument4 pagesNursing Care of Stroke - Newninda saputriNo ratings yet
- C191W003 Control Bleeding and Hypovolemic ShockDocument51 pagesC191W003 Control Bleeding and Hypovolemic ShockEmad Hussien Haj-AbdullaNo ratings yet
- Stroke and Cerebrovascular DiseaseDocument14 pagesStroke and Cerebrovascular DiseaseMarwan M.No ratings yet
- Drug Study Drug Name Classificatio N Dosage/ Prepatarion Indication Contraindication Side Effects Nursing ResponsibilitiesDocument4 pagesDrug Study Drug Name Classificatio N Dosage/ Prepatarion Indication Contraindication Side Effects Nursing ResponsibilitiesTheresa AbrilloNo ratings yet
- Congestive Heart FailureDocument14 pagesCongestive Heart FailureBella Trix PagdangananNo ratings yet
- Head Injury: Manali H. Solanki F.Y. M.Sc. Nursing J G College of NursingDocument31 pagesHead Injury: Manali H. Solanki F.Y. M.Sc. Nursing J G College of NursingWaqar AhmedNo ratings yet
- Cushings SyndromeDocument51 pagesCushings SyndromeTina TalmadgeNo ratings yet
- Case Presentation - NSTEMIDocument18 pagesCase Presentation - NSTEMIZNo ratings yet
- Management of Hypovolemic Shock FinalDocument13 pagesManagement of Hypovolemic Shock FinalDrGarikipati Krishna VenuNo ratings yet
- Management of Sepsis and Septic ShockDocument29 pagesManagement of Sepsis and Septic ShockWildan Ibnu AdrianNo ratings yet
- Brain DeathDocument6 pagesBrain DeathKabelo MaruvaNo ratings yet
- Nutritional Support of Stroke Patients: ESPEN Congress Lisbon 2015Document40 pagesNutritional Support of Stroke Patients: ESPEN Congress Lisbon 2015Risma SaroyaNo ratings yet
- Pulmonary EdemaDocument14 pagesPulmonary EdemaRizzamwah Catague100% (1)
- Gastrointestinal Bleeding: Prepared By: DR Gloria Lyimo Facilitated By: DR MbeleDocument43 pagesGastrointestinal Bleeding: Prepared By: DR Gloria Lyimo Facilitated By: DR MbeleSamar AhmadNo ratings yet
- DVT & PeDocument57 pagesDVT & PeRashed ShatnawiNo ratings yet
- Elevated Arterial Pressure Is Called HypertensionDocument27 pagesElevated Arterial Pressure Is Called Hypertensionsaurabhv89No ratings yet
- Diagnosis and Management of Shock PIPODocument25 pagesDiagnosis and Management of Shock PIPOFitri NurullahNo ratings yet
- Cerebrovascular AccidentDocument62 pagesCerebrovascular AccidentJaydee DalayNo ratings yet
- Pathophysiology of Atrial FibrillationDocument12 pagesPathophysiology of Atrial FibrillationAndrew Surya Putra SccNo ratings yet
- Indication Specific Action Side Effects/ Adverse Effects Nursing Consideration/ Patient TeachingDocument6 pagesIndication Specific Action Side Effects/ Adverse Effects Nursing Consideration/ Patient TeachingKrista Madranca CastroNo ratings yet
- How Stroke Affects Speech and LanguageDocument5 pagesHow Stroke Affects Speech and Languagemino songNo ratings yet
- Cerebrovascular Accident (CVA)Document71 pagesCerebrovascular Accident (CVA)nur muizzah afifah hussinNo ratings yet
- CvaDocument42 pagesCvad_94No ratings yet
- Cerebrovascular Accident: "A Case Study Presentation"Document38 pagesCerebrovascular Accident: "A Case Study Presentation"Kristine YoungNo ratings yet
- ResumeDocument5 pagesResumeMal Di TaNo ratings yet
- Nursing Education Department: Patient AssessmentDocument34 pagesNursing Education Department: Patient AssessmentSitti Mardiya SariolNo ratings yet
- Pleural Fluid AnalysisDocument15 pagesPleural Fluid AnalysisNatalie Sarah MoonNo ratings yet
- Tracheostomy Care: PhysiologyDocument2 pagesTracheostomy Care: PhysiologyrajirajeshNo ratings yet
- Mitral Valve ProlapseDocument3 pagesMitral Valve ProlapseKristine CastilloNo ratings yet
- ARF PathoDocument3 pagesARF PathoNikki RodrigoNo ratings yet
- National Guideline For Dengue 2018 PDFDocument96 pagesNational Guideline For Dengue 2018 PDFTapash GopeNo ratings yet
- CHF Left SidedDocument21 pagesCHF Left SidedSandie Daniel GabalunosNo ratings yet
- I. A. Brief Description: Chakinala, 2015)Document54 pagesI. A. Brief Description: Chakinala, 2015)Kacelyn QuibanNo ratings yet
- Renal Failure PresentationDocument65 pagesRenal Failure PresentationBhawna Joshi100% (1)
- Concept Map MI 2Document1 pageConcept Map MI 2nicole barcenaNo ratings yet
- Lumbar Puncture (Spinal Tap)Document35 pagesLumbar Puncture (Spinal Tap)Joisy AloorNo ratings yet
- Coronary Artery Bypass SurgeryDocument12 pagesCoronary Artery Bypass SurgeryCarlos Eduardo Quisse SánchezNo ratings yet
- Blood TransfusionDocument25 pagesBlood Transfusionpriya9balan-863873No ratings yet
- Cardiogenic ShockDocument82 pagesCardiogenic ShockLenin Zavaleta RodriguezNo ratings yet
- NCP SPH 5Document3 pagesNCP SPH 5jay5ar5jamorabon5torNo ratings yet
- Nstemi: How To Risk Stratify?Document32 pagesNstemi: How To Risk Stratify?dhannibernadetNo ratings yet
- 22 Manuscript Intestinal ObstructionDocument8 pages22 Manuscript Intestinal Obstructionkint manlangitNo ratings yet
- Week 4 Ethics Decision MakingDocument59 pagesWeek 4 Ethics Decision Makingmaha abdallahNo ratings yet
- Evaluation and Management of Suspected Sepsis and Septic Shock in Adults - UpToDateDocument37 pagesEvaluation and Management of Suspected Sepsis and Septic Shock in Adults - UpToDatebarcanbiancaNo ratings yet
- Dialysis Round Work Plan 2022 - للطلابDocument16 pagesDialysis Round Work Plan 2022 - للطلابAhmed SalahNo ratings yet
- Overview of Fluid and Electrolyte MaintenanceDocument54 pagesOverview of Fluid and Electrolyte MaintenanceIan WongNo ratings yet
- What Is Acute Glomerulonephritis?: Acute Glomerulonephritis (GN) Comprises A Specific Set of Renal Diseases inDocument6 pagesWhat Is Acute Glomerulonephritis?: Acute Glomerulonephritis (GN) Comprises A Specific Set of Renal Diseases inAnnapoorna SHNo ratings yet
- Chapter 067 Sirs ModsDocument25 pagesChapter 067 Sirs Modsapi-232466940No ratings yet
- Cost EffectivenessDocument22 pagesCost EffectivenessEdalyn CapiliNo ratings yet
- Managing Coagulopathy ICUDocument38 pagesManaging Coagulopathy ICUMirabela Colac100% (1)
- Diabetes ComplicationsDocument29 pagesDiabetes ComplicationsTom ThomasNo ratings yet
- Coronary Artery Bypass Graft Report NCM 118Document23 pagesCoronary Artery Bypass Graft Report NCM 118Vhince Norben PiscoNo ratings yet
- Cardiac TestsDocument17 pagesCardiac TestsGiorgiana pNo ratings yet
- Dka Vs Hhs Edit 1Document25 pagesDka Vs Hhs Edit 1Razeen RiyasatNo ratings yet
- West Visayas State University: Nursing ProcessDocument4 pagesWest Visayas State University: Nursing ProcessPhylum Chordata100% (1)
- Heart FailureDocument10 pagesHeart Failureurmila prajapatiNo ratings yet
- Pneumonia Management ProtocolDocument2 pagesPneumonia Management Protocolsky nuts100% (1)
- Acute Kidney FailureDocument8 pagesAcute Kidney Failureanimesh pandaNo ratings yet
- Vascular Responses to PathogensFrom EverandVascular Responses to PathogensFelicity N.E. GavinsNo ratings yet
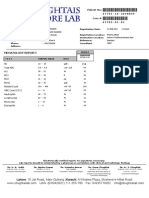
- SN FormsDocument6 pagesSN Formsbunso padillaNo ratings yet
- RRLDocument2 pagesRRLbunso padillaNo ratings yet
- Nursing Care For Child With Autoimmune Diseases & GI DisordersDocument4 pagesNursing Care For Child With Autoimmune Diseases & GI Disordersbunso padillaNo ratings yet
- Schematic DiagramDocument3 pagesSchematic Diagrambunso padillaNo ratings yet
- 04 OxygenationDocument4 pages04 Oxygenationbunso padillaNo ratings yet
- 04 Pediatric Basic Life SupportDocument2 pages04 Pediatric Basic Life Supportbunso padillaNo ratings yet
- 03 Foreign Body ObstructionDocument2 pages03 Foreign Body Obstructionbunso padillaNo ratings yet
- 05 Integrated Management of Childhood IlnessessDocument4 pages05 Integrated Management of Childhood Ilnessessbunso padillaNo ratings yet
- 1.sphingolipids: Nonglyceride LipidsDocument2 pages1.sphingolipids: Nonglyceride Lipidsbunso padillaNo ratings yet
- 02 IV TherapyDocument3 pages02 IV Therapybunso padillaNo ratings yet
- Nucleic AcidsDocument2 pagesNucleic Acidsbunso padillaNo ratings yet
- Preliminary Steps: Dna ReplicationDocument2 pagesPreliminary Steps: Dna Replicationbunso padillaNo ratings yet
- 03 Perioperative NursingDocument2 pages03 Perioperative Nursingbunso padillaNo ratings yet
- Blood Transfusion, Complications and ManagementDocument14 pagesBlood Transfusion, Complications and ManagementRubini Devi100% (1)
- Guidelines and Toolkit For Massive Transfusion in Nova ScotiaDocument64 pagesGuidelines and Toolkit For Massive Transfusion in Nova Scotiagasparsoriano3371No ratings yet
- Blood: Blood Transports Everything That Must Be Carried From One Place To Another, Such AsDocument71 pagesBlood: Blood Transports Everything That Must Be Carried From One Place To Another, Such AsAudrie Allyson GabalesNo ratings yet
- Chapter 39: Hematologic Disorders Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionDocument5 pagesChapter 39: Hematologic Disorders Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionHelen UgochukwuNo ratings yet
- Anemia: Prof. Dr. Rafita Ramayati, Spa (K) Prof. Dr..Rusdidjas, Spa (K) Dr. Oke Rina Ramayani, Spa BGN Ilmu Kes. Anak Fk-UsuDocument44 pagesAnemia: Prof. Dr. Rafita Ramayati, Spa (K) Prof. Dr..Rusdidjas, Spa (K) Dr. Oke Rina Ramayani, Spa BGN Ilmu Kes. Anak Fk-UsuleniNo ratings yet
- Bleeding DisordersDocument27 pagesBleeding DisordersIliana América AlarcónNo ratings yet
- Tests Modul 2Document99 pagesTests Modul 2yasserzeddou3000No ratings yet
- Hema OmgDocument82 pagesHema OmgBernadeth BaduaNo ratings yet
- Fluid Management & Blood Component TherapyDocument48 pagesFluid Management & Blood Component TherapySinta AgustinaNo ratings yet
- BC-6800 BrochureDocument17 pagesBC-6800 BrochureDwiyan FitraNo ratings yet
- Haemogram: Blood CountsDocument3 pagesHaemogram: Blood CountsAbhi PrajapatiNo ratings yet
- Ahg NotesDocument5 pagesAhg NotesRonron GarciaNo ratings yet
- Bombay Blood Group - Case ReportDocument3 pagesBombay Blood Group - Case ReportPremier PublishersNo ratings yet
- XN-L Series: Leading Haematology For Better Patient CareDocument12 pagesXN-L Series: Leading Haematology For Better Patient Care郑伟健No ratings yet
- RH Incompatibility - RupeshDocument4 pagesRH Incompatibility - Rupeshrupesh_mamidi100% (2)
- Blood and Blood Components-LectureDocument13 pagesBlood and Blood Components-LectureMelissa GinesNo ratings yet
- Blood Bank QuizDocument13 pagesBlood Bank Quizdimalawang.af100% (1)
- Blood Dyscrasia SDocument24 pagesBlood Dyscrasia SMasha FloreaNo ratings yet
- Guillette - Blood Typing Worksheet - Answer SheetDocument2 pagesGuillette - Blood Typing Worksheet - Answer SheetNOVA LESLIE AGAPAYNo ratings yet
- Work Process and SOP For Taking Blood CultureDocument5 pagesWork Process and SOP For Taking Blood CultureKhor Kee GuanNo ratings yet
- Blood and LymphaticDocument4 pagesBlood and LymphaticCKNo ratings yet
- 16/09/2015 1 Mujtaba AshrafDocument44 pages16/09/2015 1 Mujtaba Ashrafதீரன் சக்திவேல்No ratings yet
- MCqs On Hematological Disorder Provided by MirhaDocument4 pagesMCqs On Hematological Disorder Provided by MirhaAkml KhanNo ratings yet
- Haematology Diagnosis-Army USADocument205 pagesHaematology Diagnosis-Army USAManuela BotisNo ratings yet
- ReportViewer3 CBCDocument1 pageReportViewer3 CBCMuhammad Munawar BuzdarNo ratings yet
- A Clinicohematological Profile of SplenomegalyDocument6 pagesA Clinicohematological Profile of SplenomegalyIvan Louis ToledoNo ratings yet
- Magnesium Sulfate As An Alternative in VitroDocument9 pagesMagnesium Sulfate As An Alternative in Vitrorince noveliaNo ratings yet
- RBC Indices and Extended RBC Parameters: Learning GuideDocument39 pagesRBC Indices and Extended RBC Parameters: Learning GuideYaser MNo ratings yet
- Blood Bank Visit ReportDocument13 pagesBlood Bank Visit ReportsysiddhiyadavNo ratings yet