Professional Documents
Culture Documents
Pedia Meningitis
Uploaded by
iSmayli (smyle-smayl)Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pedia Meningitis
Uploaded by
iSmayli (smyle-smayl)Copyright:
Available Formats
CNS
INFECTIONS
EPIDEMIOLOGY
• Significant cause of mortality and morbisity in children
• Viral is the most common in children
COMMON SIGNS AND SYMPTOMS
• Symptoms: headache, nausea, vomiting, anorexia, photophobia, restlessness, altered consciousness and irritability
• Signs: fever, neck pain and rigidity (12-18 months: absent Kernig and Brudzinski), focal neurologic deficits, seizures, obtundation and coma.
DIAGNOSTICS
• CSF analysis, PCR and imaging
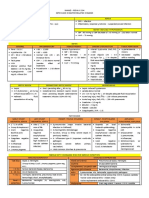
Bacterial Meningitis Viral Meningitis Tuberculous Meningitis
Etiology First 2 months: GBS, G(-) enteric bacilli, L. Enterovirus (most common) Metastatic caseous lesion from primary TB
monocytogenes Parechovirus (cause of aseptic infection
2 months to 12 years: S. pneumonia, H. meningitis/encephalitis in infants)
influenza, N. meninigitidis HSV, VZV, Mumps
Manifestations Common signs and symptoms (see above) More benign course than bacterial cause More rapid progression in infants and
VZV (cerebellar ataxia) children.
Mumps (may cause deafness from CN8 Acute onset of hydrocephalus, seizures and
damage) cerebral edema.
Diagnostic Blood Culture EEG: diffuse slow wave activity Acid fast almost never seen on smear
(see CSF High CRP, ESR Procalcitonin (diff from Viral) Imaging: swelling of the brain parenchyma Ground glass appearance of CSF fluid
analysis Ancillary: PCR, ELISA, Latex Agglutination
below) Cranial Imaging:
• Basilar enhancement,
• Communicating Hydrocephalus
• Cerebral Edema
• Focal Ischemia
Management Antibiotics (see table below) Supportive Anti Koch’s
Dexamethasone (IV) 0.15 mg/kg q 6hr for 2 • IV fluid • Newly diagnosed: 2 HRZE+10HR
days • NSAID for relief of headache • Previously treated DS:
• H.influenza: 1-2 hrs before antibiotics HSV: Acyclovir 2HRZES+1HRZE+9HRE
• Less fever lower CSF protein, reduced Corticosteroid
auditory nerve damage - Improves survival but not severe
disability
Prognosis Appropriate antibiotic therapy and supportive Recovery depends on severity, specific
care reduced the mortality beyond neonatal causative agent and age
period to <10%
Prevention Vaccination and Antibitiotic Prophylaxis Vaccination
PCV, Hib/ Penta (6,10,14 weeks) • Polio (6-10-14)
• MMR (12 months)
• Varicella (12 months)
• JapEn (9 months)
• Vector control (arbovirus)
CSF ANALYSIS
Condition Pressure (cmH2O) Leukocytes (mm3) Protein (mg/dL) Glucose (mg/dL)
Normal <28 cm H20 / 50- 80 mmH20 <5, >75% lymphocytes 20-45 >50 (>75% serum
In neonates: <20 glucose)
Acute Bacterial Usually elevated (100mmH2O) 10-10,000 or more 100-500 Decreased <40 mg/dL
Meninigitis Usually 300-2000 <50% of serum glucose)
PMNs predominance
Partially Treated Normal or elevated 5-10,000 100-500 Normal or decreased
BacMen PMN
Mononuclear cells if pretreated for extended
period of time
Viral Meningitis Normal to slightly elevated Rarely >1000 mm3 50-200 Generally normal
(80-150 mmH2O) PMNs early May be decreased
Mononuclear in most of the course (<40mg/dL) in mumps
Tuberculous Usually elevated 10-500 100-3000 <50 in most cases
Meningitis PMNs early Higher I the
Lymphocytes in most of the course presence of block
ANTIBIOTICS
Empiric Ceftriaxone or Cefatoxime
Vancomycin if PR L. monocytogenes Ampicillin
Chloramphenicol for >1 month old (Pen allergic) Alternative: IV TMP-SMX
Alternative: Vancomycin +rifampin Hib Ampicillin 7-10 days
N meningitides Pen G IV for 5-7days E.coli Cefotaxime or Ceftriaxone for 3 weeks OR at least
Pen Allergic: Meropenem or Vancomycin 2 weeks after CSF sterilization
S pneumonia Vancomycin + 3rd gen Ceph or Pen IV for 10-14 PAe Ceftazidime for 3 weeks OR at least 3 weeks after
days CSF sterilization
Vancomycin is added due to risk of resistance with Partially treated Ceftriaxone or Cefotaxime for 7-10 days
the other antibiotics
Penicillin resistant isolates Vancomycin
You might also like
- Meningitis PDFDocument10 pagesMeningitis PDFAlfatahadi SNo ratings yet
- Bacterial MeningitisDocument2 pagesBacterial Meningitisjennielunay00No ratings yet
- CNS InfectionDocument36 pagesCNS InfectionIkaDian PuspitanzaNo ratings yet
- CNS Infection: Nurcahaya Sinaga Haji Pemprovsu Hospital, Faculty of Medicine Universitas Muhammadiyah Sumatera UtaraDocument34 pagesCNS Infection: Nurcahaya Sinaga Haji Pemprovsu Hospital, Faculty of Medicine Universitas Muhammadiyah Sumatera Utaramuhammad alqoriNo ratings yet
- SEPSIS Early DetectionDocument35 pagesSEPSIS Early DetectionKomang_JananuragaNo ratings yet
- Dengue: History Physical Examination InvestigationDocument4 pagesDengue: History Physical Examination InvestigationNik Hanisah Zuraidi AfandiNo ratings yet
- Shanz - Pedia Ii 2.04Document4 pagesShanz - Pedia Ii 2.04Petrina XuNo ratings yet
- Meningitis-Malaria E PDFDocument44 pagesMeningitis-Malaria E PDFSana ShafeeqNo ratings yet
- Meningitis and Encephalitis: PGI Roddame Angelo ErispeDocument100 pagesMeningitis and Encephalitis: PGI Roddame Angelo ErispeAngelo ErispeNo ratings yet
- Meningitis Beyond The Neonatal AgeDocument51 pagesMeningitis Beyond The Neonatal AgeBeamlak Getachew WoldeselassieNo ratings yet
- PATHOPISIOLOGYDocument2 pagesPATHOPISIOLOGYjennielunay00No ratings yet
- Kang Mamat MaraisDocument2 pagesKang Mamat MaraisMuhammad Amri KautsarNo ratings yet
- NC InfeksiAndi Asriel DBDDocument20 pagesNC InfeksiAndi Asriel DBDeunike jaequelineNo ratings yet
- AKI FlowchartDocument1 pageAKI FlowchartTush RameNo ratings yet
- Mis C Clinical GuidelineDocument9 pagesMis C Clinical GuidelineasyqarNo ratings yet
- Mis C Clinical GuidelineDocument8 pagesMis C Clinical GuidelineClamargav aNo ratings yet
- Meningitis - 2018Document55 pagesMeningitis - 2018Abraham Anaely100% (1)
- CNS InfectionDocument18 pagesCNS InfectionJason LinNo ratings yet
- Bsn-Rs-Careplan 3-2Document12 pagesBsn-Rs-Careplan 3-2api-509646698No ratings yet
- Acute Bacterial Meningitis in ChildrenDocument48 pagesAcute Bacterial Meningitis in ChildrenRadhika BatraNo ratings yet
- Thromboprophylaxis in Sepsis Case BasedDocument32 pagesThromboprophylaxis in Sepsis Case BasedVasantha KumarNo ratings yet
- Paediatrics Notes CreatedDocument28 pagesPaediatrics Notes CreatedAbraham AnaelyNo ratings yet
- Cerebrospinal FluidDocument33 pagesCerebrospinal FluidSolomon Fallah Foa SandyNo ratings yet
- Acquired Heart DiseaseDocument44 pagesAcquired Heart DiseaseMedisina101No ratings yet
- Acute Bacterial Meningitis and Anti Microbials in Neuro SurgeryRepairedDocument35 pagesAcute Bacterial Meningitis and Anti Microbials in Neuro SurgeryRepairedCalicut NeurosurgeryNo ratings yet
- Bacterial MeningitisDocument2 pagesBacterial Meningitisjennielunay00No ratings yet
- All About Fever 6Document42 pagesAll About Fever 6brajendra singhNo ratings yet
- Internal Medicine II - NEUROLOGY CASESDocument33 pagesInternal Medicine II - NEUROLOGY CASESAhmad SobihNo ratings yet
- PSGNDocument23 pagesPSGNalpha mae beltranNo ratings yet
- Case Scenario:: Is An Eye Finding Occurring Early inDocument5 pagesCase Scenario:: Is An Eye Finding Occurring Early inDenice Tamayo De GuzmanNo ratings yet
- Sepsis in The Setting of AspleniaDocument30 pagesSepsis in The Setting of Aspleniaapi-740273867No ratings yet
- Bacterial Meningitis in Over 1 Month Old: Tehmas Ahmad Khan PGY-1 Pediatrics, KRL Hospital, IslamabadDocument52 pagesBacterial Meningitis in Over 1 Month Old: Tehmas Ahmad Khan PGY-1 Pediatrics, KRL Hospital, IslamabadTabada NickyNo ratings yet
- 20 - Neonatal InfectionsDocument4 pages20 - Neonatal InfectionsYassboy MsdNo ratings yet
- Paralisis FacialDocument25 pagesParalisis FacialItzel Estephany ANo ratings yet
- Kawasaki DiseaseDocument7 pagesKawasaki DiseaseRitamariaNo ratings yet
- Model Test-1 SolveDocument20 pagesModel Test-1 SolveRaihanShaheedNo ratings yet
- Meningitis SVDocument15 pagesMeningitis SVLydia Lopz MsnrncdNo ratings yet
- Acute Meningitis: DR K. Saroj Novel Jr-1 General Medicine Moderator:Dr - Sushanth MD Assistant ProfessorDocument28 pagesAcute Meningitis: DR K. Saroj Novel Jr-1 General Medicine Moderator:Dr - Sushanth MD Assistant ProfessorSaikiran GundaboynaNo ratings yet
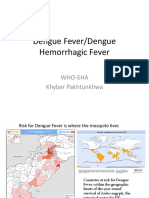
- Presentation On Dengue FeverDocument31 pagesPresentation On Dengue FeverDrMuhammad Ishfaq HabibNo ratings yet
- Dengue Hemorrhagic Fever: Dr. Dwi Lingga Utama, Spa (K)Document31 pagesDengue Hemorrhagic Fever: Dr. Dwi Lingga Utama, Spa (K)Sheryl ElitaNo ratings yet
- Training HD GgaDocument31 pagesTraining HD Ggawulan ulfah nurrohmahNo ratings yet
- Massa Kat 2019Document17 pagesMassa Kat 2019nayyarNo ratings yet
- Opening Pressure Color Presence of Rbcs WBC Count: Neurosciences 251Document3 pagesOpening Pressure Color Presence of Rbcs WBC Count: Neurosciences 251Bea ConstantinoNo ratings yet
- Meningitis 2005Document87 pagesMeningitis 2005nafisyarifahNo ratings yet
- CNSInfections 2Document39 pagesCNSInfections 2Nica BalaresNo ratings yet
- 06NTD 2022 - Managing Dengue in Children: An UpdateDocument40 pages06NTD 2022 - Managing Dengue in Children: An UpdateInstitute for Clinical ResearchNo ratings yet
- Encephalitis Workup - Approach Considerations, Blood and Urine Tests, Studies To Identify Infectious AgentDocument5 pagesEncephalitis Workup - Approach Considerations, Blood and Urine Tests, Studies To Identify Infectious AgentdilaNo ratings yet
- Enumerate The Aetiological Agents of Meningeal Involvement in ChildrenDocument21 pagesEnumerate The Aetiological Agents of Meningeal Involvement in ChildrenAbhirup BoseNo ratings yet
- Meningitis and Fractures Concept MapDocument4 pagesMeningitis and Fractures Concept MapNamayanja SumayiyahNo ratings yet
- Acute Chest SyndromeDocument28 pagesAcute Chest SyndromeJohn OkidiNo ratings yet
- 5 Neurological ManifestationsDocument30 pages5 Neurological ManifestationsCalvin ChisangoNo ratings yet
- Death Case Report Februari 25 2021 A 1 Year 6 Months Old Girl With Langerhans Cell Hystiocytosis and Its ComplicationDocument11 pagesDeath Case Report Februari 25 2021 A 1 Year 6 Months Old Girl With Langerhans Cell Hystiocytosis and Its ComplicationVianNo ratings yet
- SepsisDocument26 pagesSepsisWulan MulyaniNo ratings yet
- 2011 CNS Bacterial InfectionDocument47 pages2011 CNS Bacterial InfectionZEMENAY TRUNEHNo ratings yet
- 17 MedsurgDocument3 pages17 MedsurgLomocso Baron JudyNo ratings yet
- Neonatal SeizuresDocument4 pagesNeonatal SeizuresSerag EdeenNo ratings yet
- Infeksi Susunan Saraf PusatDocument37 pagesInfeksi Susunan Saraf PusatBinot's TogamaNo ratings yet
- DengueDocument32 pagesDengueUsamaNo ratings yet
- Asuhan Keperawatan Pada Klien Dengan Meningitis: Retno LestariDocument57 pagesAsuhan Keperawatan Pada Klien Dengan Meningitis: Retno Lestariaha ehe ohoNo ratings yet
- Asthma: Bronchospasm, Airway Edema, Mucus ProductionDocument2 pagesAsthma: Bronchospasm, Airway Edema, Mucus ProductioniSmayli (smyle-smayl)No ratings yet
- Case For RCPCC 2Document4 pagesCase For RCPCC 2iSmayli (smyle-smayl)No ratings yet
- Systemic Lupus Erythematosus-Pedia: 4 Criteria (Including at Least 1 Clinical and 1 Immunologic Criterion)Document1 pageSystemic Lupus Erythematosus-Pedia: 4 Criteria (Including at Least 1 Clinical and 1 Immunologic Criterion)iSmayli (smyle-smayl)No ratings yet
- PEDIA aPSGNDocument2 pagesPEDIA aPSGNiSmayli (smyle-smayl)No ratings yet
- PEDIA Typhoid-FeverDocument1 pagePEDIA Typhoid-FeveriSmayli (smyle-smayl)No ratings yet
- Clinical Practice Guidelines PSOHNS2016Document45 pagesClinical Practice Guidelines PSOHNS2016Jan Marvin Lichauco MendozaNo ratings yet
- Home Care For CovidDocument18 pagesHome Care For CovidiSmayli (smyle-smayl)No ratings yet
- Pathophy Miliary TBDocument5 pagesPathophy Miliary TBiSmayli (smyle-smayl)No ratings yet
- PMA Code of EthicsDocument7 pagesPMA Code of EthicskaliyasaNo ratings yet
- Research - Rev Lit BseDocument7 pagesResearch - Rev Lit BseiSmayli (smyle-smayl)No ratings yet
- Eye Chart Template 17Document2 pagesEye Chart Template 17iSmayli (smyle-smayl)No ratings yet
- PMA Code of EthicsDocument7 pagesPMA Code of EthicskaliyasaNo ratings yet
- Ob BioethicsDocument1 pageOb BioethicsiSmayli (smyle-smayl)No ratings yet
- LECTURER: Alizza Love F. Velasco, MD, FPAFP, FPSHPM: WellnessDocument6 pagesLECTURER: Alizza Love F. Velasco, MD, FPAFP, FPSHPM: WellnessiSmayli (smyle-smayl)No ratings yet
- Note To SelfDocument1 pageNote To SelfiSmayli (smyle-smayl)No ratings yet
- YohimbimeDocument13 pagesYohimbimeiSmayli (smyle-smayl)No ratings yet
- Para Cestode TableDocument3 pagesPara Cestode TableiSmayli (smyle-smayl)100% (1)
- Chemotherapy For MalariaDocument5 pagesChemotherapy For MalariaiSmayli (smyle-smayl)No ratings yet
- PemphigusDocument1 pagePemphigusiSmayli (smyle-smayl)No ratings yet
- Epidemiology Distribution of Diseases Caused by AnimalDocument1 pageEpidemiology Distribution of Diseases Caused by AnimaliSmayli (smyle-smayl)No ratings yet
- Valgancyclovir MOA: Uses Pharmacokinetics Dosage Side Effects ContraindicationsDocument2 pagesValgancyclovir MOA: Uses Pharmacokinetics Dosage Side Effects ContraindicationsiSmayli (smyle-smayl)No ratings yet
- Superficial MycosesDocument2 pagesSuperficial MycosesiSmayli (smyle-smayl)No ratings yet
- In The EastDocument2 pagesIn The EastiSmayli (smyle-smayl)No ratings yet
- Real-World Examples: Data AnalysisDocument6 pagesReal-World Examples: Data AnalysisiSmayli (smyle-smayl)No ratings yet
- Nelson Tools For Space Analysis and Design 050211Document11 pagesNelson Tools For Space Analysis and Design 050211iSmayli (smyle-smayl)No ratings yet
- Maricris Joy L. CaoileDocument1 pageMaricris Joy L. CaoileiSmayli (smyle-smayl)No ratings yet
- Who Diagnostic Criteria MyelofibrosisDocument2 pagesWho Diagnostic Criteria MyelofibrosisaymenNo ratings yet
- Biology - Practice Questions PDFDocument12 pagesBiology - Practice Questions PDFzahra giyoriNo ratings yet
- Bacterial Cell Structure, Physiology, Metabolism, and GeneticsDocument91 pagesBacterial Cell Structure, Physiology, Metabolism, and GeneticsLindsay OttoNo ratings yet
- Mutagenesis: Site-Specific: September 2005Document13 pagesMutagenesis: Site-Specific: September 2005Sarnam SinghNo ratings yet
- Topic 6 Gene Control: Suggested ActivitiesDocument2 pagesTopic 6 Gene Control: Suggested ActivitiesSemwezi EnockNo ratings yet
- Rationale PQ 1Document12 pagesRationale PQ 1ChaNo ratings yet
- Essays On Heart of DarknessDocument5 pagesEssays On Heart of DarknessafiboeolrhismkNo ratings yet
- Identification of Pathogenic Bacteria in Clinical Microbiology LaboratoryDocument70 pagesIdentification of Pathogenic Bacteria in Clinical Microbiology Laboratoryamare100% (4)
- Tannic Acid Specific Form of Tannins in Cancer CheDocument11 pagesTannic Acid Specific Form of Tannins in Cancer Cheuci kinaseNo ratings yet
- Bte 102 FinalDocument2 pagesBte 102 FinalSadman RashidNo ratings yet
- Plasmodium SP: Sitti Wahyuni, MD, PHDDocument29 pagesPlasmodium SP: Sitti Wahyuni, MD, PHDAhmad Al MuhtadiNo ratings yet
- Types of MutationsDocument4 pagesTypes of MutationsJestoni BigaelNo ratings yet
- VIII CPP Cell Structure and Functions 19.09.2022Document1 pageVIII CPP Cell Structure and Functions 19.09.2022Rajeswari SareddyNo ratings yet
- Sciencedirect Food Fermentations For Improved Digestibility of Plant Foods - An Essential Ex Situ Digestion Step in Agricultural Societies?Document8 pagesSciencedirect Food Fermentations For Improved Digestibility of Plant Foods - An Essential Ex Situ Digestion Step in Agricultural Societies?arNo ratings yet
- General Science NotesDocument93 pagesGeneral Science Notesvijayiitkgp2008968350% (2)
- Bone Marrow Film Examination For Platelet Maturation Series: Activity No. 1Document43 pagesBone Marrow Film Examination For Platelet Maturation Series: Activity No. 1pixiedustNo ratings yet
- Department of Haematology: Test Name Result Unit Bio. Ref. Range MethodDocument4 pagesDepartment of Haematology: Test Name Result Unit Bio. Ref. Range MethodSiva JabilliNo ratings yet
- Agar-Gel Immunodiffusion (AGID) : EquipmentDocument6 pagesAgar-Gel Immunodiffusion (AGID) : Equipmenta教授No ratings yet
- Lecture-1, Introductio To MicrobiologyDocument35 pagesLecture-1, Introductio To MicrobiologyWaleed 1100% (1)
- Xi STD Reduced Syllabus - 2021-22 by AmDocument52 pagesXi STD Reduced Syllabus - 2021-22 by AmTwelegyNo ratings yet
- Biorisk Mitigation Strategies - PASMETH - PhBBA - DTRADocument66 pagesBiorisk Mitigation Strategies - PASMETH - PhBBA - DTRARyan Marañon PedregosaNo ratings yet
- EUCAST V - 9.0 - Breakpoint - Tables PDFDocument100 pagesEUCAST V - 9.0 - Breakpoint - Tables PDFRicardo Ariel GianeciniNo ratings yet
- HLA Sensitisation - Can It Be PreventedDocument11 pagesHLA Sensitisation - Can It Be PreventedPatriciaNo ratings yet
- Population Genetics Lecture NotesDocument23 pagesPopulation Genetics Lecture NotesMaryam AmiruNo ratings yet
- 10 1016@j Biopha 2019 109142Document13 pages10 1016@j Biopha 2019 109142CoNo ratings yet
- MHC MoleculeDocument45 pagesMHC MoleculeShah NAWAZNo ratings yet
- BIO G10 Q3 W5 D1 RevDocument4 pagesBIO G10 Q3 W5 D1 RevGu Jun PyoNo ratings yet
- Recent Research Papers in Animal BiotechnologyDocument5 pagesRecent Research Papers in Animal Biotechnologys1bivapilyn2100% (1)
- Anti-Inflammatory, Anti-Arthritis, and Related AgentsDocument22 pagesAnti-Inflammatory, Anti-Arthritis, and Related AgentsMarjolene PudaderaNo ratings yet
- Expository Essay - GunjanDocument3 pagesExpository Essay - GunjanRaghav LaddhaNo ratings yet