Professional Documents
Culture Documents
Bacterial Meningitis
Uploaded by
jennielunay000 ratings0% found this document useful (0 votes)
3 views2 pagesCopyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
3 views2 pagesBacterial Meningitis
Uploaded by
jennielunay00Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 2
Bacterial Meningitis
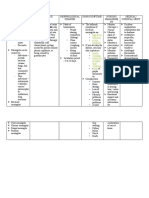
Modifiable Factors: Non-Modifiable Factors:
• Vaccination Status • Age
• Hygiene • Medical Condition (Congenital abnormalities)
• Avoiding close contact • Premature birth
• Genetics
Streptococcus Pneumonia
Neisseria meningitidis
Organisms gain entry into CNS through Inflammatory response
upper respiratory tract via blood stream
• Increase cerebrospinal fluid
• Increased intracranial pressure
May enter through penetrating wounds of
the skull or fractured sinuses in basilar skull
fractures Increased ICP early signs
• Altered LOC, restless, irritability,
Purulent secretions spread throughout agitation, decreased mental
brain through the cerebrospinal fluid and status
cover cranial nerves and other intercranial
structures
If extends to brain parenchyma or if Observe for signs of increased ICP, it can
concurrent encephalitis is present, cerebral be increased from swelling and increased
edema and increased intracranial pressure cerebrospinal fluid volume
become a problem
SIGNS AND SYMPTOMS:
• High pitch cry LABS & DIAGNOSTIC PROCEDURE:
• Bulging fontanels
Cranial UTZ: (benign enlargement of the
• Hard stiff neck (nuchal rigidity)
subarachnoid space hydrocephalus)
• High temp (fever)
• Photophobia Hematology: (low HCT, low RBC, low EO, high MCH)
• Increased intracranial pressure (could lead to seizure, CT scan
coma, death)
• Agitation
• Altered/decrease Level of Consciousness
• Severe headache
• Nausea
• vomiting
If Yes Management If No
Persistent or recurrent infections
Nursing Management: Medical Management:
• Monitor vital signs closely, including • Initiate empiric antibiotic therapy
temperature, heart rate, respiratory immediately upon suspicion of Enlargement of ventricles and increased ICP
rate, and blood pressure. bacterial meningitis, based on
local antimicrobial resistance
• Assess neurological status regularly, patterns.
including level of consciousness, Neurologic complications (motor
• Perform lumbar puncture for
pupillary response, and motor cerebrospinal fluid (CSF) analysis impairments, sensory deficits, cognitive
function. to confirm the diagnosis of dysfunction, damage to cerebral cortex or
• Implement strict infection control bacterial meningitis and guide basal ganglia)
measures to prevent the spread of antibiotic selection.
bacterial meningitis to other patients • Administer appropriate antibiotics
Neurologic complications (motor
and healthcare workers. intravenously for a duration
determined by the specific impairments, sensory deficits, cognitive
• Provide comfort measures, such as organism and clinical response. dysfunction)
positioning the infant for optimal • intensive care teams to optimize
comfort and administering pain relief management and outcomes.
as needed.
Vision and hearing impairments
• Educate parents or caregivers about
• Consider placement of an external
the signs and symptoms of bacterial Developmental delays and disabilities
ventricular drain (EVD) or
meningitis and hydrocephalus, as
ventriculoperitoneal shunt (VP
well as the importance of follow-up
shunt) for management of
care.
hydrocephalus if indicated by
• Provide emotional support to parents
imaging studies or clinical
or caregivers during this challenging Recurrent seizure and epilepsy
symptoms.
time, offering reassurance and
• Provide supportive care for
information as needed.
complications such as seizures,
• Ensure adequate hydration and respiratory distress, or
nutrition, possibly through disseminated intravascular
nasogastric or intravenous routes if coagulation (DIC). Chronic health conditions
necessary. • Perform regular neurologic
assessments to monitor for
• Monitor for signs of increased
changes in status and response to
intracranial pressure (ICP), such as
treatment.
irritability, bulging fontanelle, or
• Coordinate multidisciplinary care Mortality
changes in level of consciousness.
involving neurology, neurosurgery,
• infectious disease, and pediatric
intensive care teams to optimize
management and outcomes.
You might also like
- Bacterial MeningitisDocument2 pagesBacterial Meningitisjennielunay00No ratings yet
- Unconscious and Comatose Patients DR Moses KazevuDocument17 pagesUnconscious and Comatose Patients DR Moses KazevuMoses Jr KazevuNo ratings yet
- Neuro NotesDocument15 pagesNeuro NotesClyde CapapasNo ratings yet
- High Fever Stiff Neck Severe HeadacheDocument3 pagesHigh Fever Stiff Neck Severe HeadacheDiana Jane LauretaNo ratings yet
- Guarin - Inflammatory Disturbances NotesDocument6 pagesGuarin - Inflammatory Disturbances NotesMary Joy Anne LucasNo ratings yet
- PyomeningitisDocument54 pagesPyomeningitisRiya BagdiNo ratings yet
- Pathogenesis of MENINGITISDocument30 pagesPathogenesis of MENINGITISPrachi TeteNo ratings yet
- Meningitis SVDocument15 pagesMeningitis SVLydia Lopz MsnrncdNo ratings yet
- NURSING CARE PLAN - HydrocephalusDocument3 pagesNURSING CARE PLAN - Hydrocephalusderic98% (41)
- Nursing Care Plan HydrocephalusDocument3 pagesNursing Care Plan Hydrocephalusstar7707100% (1)
- Supratentorial: Common Neuro Surgeries Common Drugs Administered PreopDocument4 pagesSupratentorial: Common Neuro Surgeries Common Drugs Administered PreopMarissa AsimNo ratings yet
- Meningitis and Fractures Concept MapDocument4 pagesMeningitis and Fractures Concept MapNamayanja SumayiyahNo ratings yet
- Bacterial MeningitisDocument37 pagesBacterial MeningitisMission JupiterNo ratings yet
- Group 3: Clinicopathological ConferenceDocument31 pagesGroup 3: Clinicopathological ConferenceNathanielTalibongNo ratings yet
- MeningitisDocument17 pagesMeningitisKyla Marie TejadaNo ratings yet
- Pathophysiology FinalDocument3 pagesPathophysiology Finaljustineneri324No ratings yet
- The Child With A Neurologic DisorderDocument42 pagesThe Child With A Neurologic DisorderLeilani FullerNo ratings yet
- Brain Abscess: Zarqa Wahid BuxDocument9 pagesBrain Abscess: Zarqa Wahid Buxzarka wahid buxNo ratings yet
- Possible Mechanisms of Pathogenesis For The Neuropsychiatric Manifestations of COVIDDocument3 pagesPossible Mechanisms of Pathogenesis For The Neuropsychiatric Manifestations of COVIDHyacinth ManoodNo ratings yet
- Medsurg Finals TheoryDocument27 pagesMedsurg Finals TheoryKAYE PAULINE SERVIDADNo ratings yet
- 3 Problem Emergency Medicine Block: 8 October 2019 Group 15Document60 pages3 Problem Emergency Medicine Block: 8 October 2019 Group 15RioNo ratings yet
- NCM 116: Neurologic Dysfunctions: Joyce Bernadette P. Andot - Anna Delle Nicole P. Aranding, BSN-IIIDocument46 pagesNCM 116: Neurologic Dysfunctions: Joyce Bernadette P. Andot - Anna Delle Nicole P. Aranding, BSN-IIIMercy Anne EcatNo ratings yet
- PATHOPISIOLOGYDocument2 pagesPATHOPISIOLOGYjennielunay00No ratings yet
- PHCP - Unit 5 - NEUROLOGIC NERVOUS SYSTEM DISORDERDocument10 pagesPHCP - Unit 5 - NEUROLOGIC NERVOUS SYSTEM DISORDERDuh realNo ratings yet
- Subarachnoid HemorrhageDocument16 pagesSubarachnoid HemorrhageErika NaingNo ratings yet
- Sepsis and MODS 2Document12 pagesSepsis and MODS 2Alex ChiuNo ratings yet
- Acute Meningitis: DR K. Saroj Novel Jr-1 General Medicine Moderator:Dr - Sushanth MD Assistant ProfessorDocument28 pagesAcute Meningitis: DR K. Saroj Novel Jr-1 General Medicine Moderator:Dr - Sushanth MD Assistant ProfessorSaikiran GundaboynaNo ratings yet
- Central Nervous System Infection (Infeksi Susunan Saraf Pusat)Document92 pagesCentral Nervous System Infection (Infeksi Susunan Saraf Pusat)Farihatun NisaNo ratings yet
- Dizziness and VertigoDocument6 pagesDizziness and VertigoJose Luis De GuzmanNo ratings yet
- Encephalitis Brain Abscess: Reşat Özaras, MD, Prof. Infection DeptDocument45 pagesEncephalitis Brain Abscess: Reşat Özaras, MD, Prof. Infection DeptChristian KennethNo ratings yet
- Benign Febrile Seizure: PediatricsDocument2 pagesBenign Febrile Seizure: PediatricsKrista P. AguinaldoNo ratings yet
- Febrile Seizures 12 - 1 - 2019 3Document12 pagesFebrile Seizures 12 - 1 - 2019 3ninta karinaNo ratings yet
- Pedia2 Sepsis (Dr. Seng)Document3 pagesPedia2 Sepsis (Dr. Seng)Tony DawaNo ratings yet
- Ii - Pedia-Rn DisordersDocument15 pagesIi - Pedia-Rn DisordersAnnie Rose Dorothy MamingNo ratings yet
- EncephalitisDocument23 pagesEncephalitisCHARLOTTE DU PREEZNo ratings yet
- Nyeri Pada NeonatusDocument38 pagesNyeri Pada NeonatusRey AlwiwikhNo ratings yet
- AAAA2Document142 pagesAAAA2Sruthi SruthiNo ratings yet
- Neuroscience Ii: Summary: Nationality (Will Tell You Incidence, For Example, AsiansDocument29 pagesNeuroscience Ii: Summary: Nationality (Will Tell You Incidence, For Example, AsiansAngelaTrinidad100% (2)
- Meningococcemia: Regati Meenakshi ROLL: B30Document16 pagesMeningococcemia: Regati Meenakshi ROLL: B30Meena RajNo ratings yet
- Increased Intracranial Pressure (Iicp)Document3 pagesIncreased Intracranial Pressure (Iicp)رجمه ديوانNo ratings yet
- Infectious Diseases - Nervous System: Fcnlxa - St. Luke's College of NursingDocument5 pagesInfectious Diseases - Nervous System: Fcnlxa - St. Luke's College of NursingLAXA FRANCINENo ratings yet
- Tuberculoma: Case ReportDocument34 pagesTuberculoma: Case ReportitaNo ratings yet
- GYLLE Meningitis Otitis Media Pertussis Pneumonia Rotavirus 1Document37 pagesGYLLE Meningitis Otitis Media Pertussis Pneumonia Rotavirus 1Marie Ashley CasiaNo ratings yet
- Pappagallo 01Document27 pagesPappagallo 01Steven GodelmanNo ratings yet
- Metabolic EncephalopathyDocument22 pagesMetabolic Encephalopathytricia isabellaNo ratings yet
- Common Pediatric DiseasesDocument16 pagesCommon Pediatric Diseasesboxed juiceNo ratings yet
- Pedia MeningitisDocument1 pagePedia MeningitisiSmayli (smyle-smayl)No ratings yet
- 4 - Management of Patients With Neurologic Dysfunction Origenal K.Document21 pages4 - Management of Patients With Neurologic Dysfunction Origenal K.Taif SalimNo ratings yet
- 20 Bacterial MeningitisDocument35 pages20 Bacterial MeningitisBhakti WashilkarNo ratings yet
- The Severely Ill Patient - September 2010Document11 pagesThe Severely Ill Patient - September 2010Nor Haryanti HashimNo ratings yet
- TB Paa Nervous SystemDocument39 pagesTB Paa Nervous SystemRivan DanuajiNo ratings yet
- Approach To Comatose Child: DR G.VenkateshDocument83 pagesApproach To Comatose Child: DR G.VenkateshG VenkateshNo ratings yet
- Requirement in PathophysiologyDocument38 pagesRequirement in PathophysiologyckathreenahNo ratings yet
- Neuro ICUDocument11 pagesNeuro ICUBatch V Med 2 SY 21-22No ratings yet
- Vascular Considerations: (I) Cervical Arterial Dissection (CAD)Document2 pagesVascular Considerations: (I) Cervical Arterial Dissection (CAD)BhargavaNo ratings yet
- Bacterial MeningitisDocument40 pagesBacterial MeningitisDinesh ReddyNo ratings yet
- Group 1.2 Case StudyDocument19 pagesGroup 1.2 Case Studychandria0026No ratings yet
- Encephalitis, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandEncephalitis, A Simple Guide To The Condition, Treatment And Related ConditionsRating: 5 out of 5 stars5/5 (16)
- The Perfect Ic Diet Cookbook The Complete Nutrition Guide To Healing Chronic Pelvic Pain And Managing Symptoms Of Interstitial Cystitis With Delectable And Nourishing RecipesFrom EverandThe Perfect Ic Diet Cookbook The Complete Nutrition Guide To Healing Chronic Pelvic Pain And Managing Symptoms Of Interstitial Cystitis With Delectable And Nourishing RecipesNo ratings yet
- The Perfect Parkinson Diet Cookbook; The Complete Nutrition Guide To Managing And Healing Parkinson's Disease With Delectable And Nourishing RecipesFrom EverandThe Perfect Parkinson Diet Cookbook; The Complete Nutrition Guide To Managing And Healing Parkinson's Disease With Delectable And Nourishing RecipesNo ratings yet
- Course Hero 1Document2 pagesCourse Hero 1jennielunay00No ratings yet
- Perilight-Exposure (AutoRecovered)Document1 pagePerilight-Exposure (AutoRecovered)jennielunay00No ratings yet
- 1Document1 page1jennielunay00No ratings yet
- 5Document1 page5jennielunay00No ratings yet
- Module 4 Assignment Cortez and Salalila PDFDocument7 pagesModule 4 Assignment Cortez and Salalila PDFjennielunay00No ratings yet
- Trauma 1Document45 pagesTrauma 1Abdul HaiNo ratings yet
- 2023 ASF Walk Press ReleaseDocument1 page2023 ASF Walk Press ReleaseNBC MontanaNo ratings yet
- Faith Mental Health GuideDocument26 pagesFaith Mental Health GuideRJ MagoNo ratings yet
- Maladaptive Behavior by ShrkydnlDocument7 pagesMaladaptive Behavior by ShrkydnlPizza MozzarellaNo ratings yet
- Psychometrics of The Child PTSD Symptom Scale For DSM-5 For Trauma-Exposed Children and AdolescentsDocument10 pagesPsychometrics of The Child PTSD Symptom Scale For DSM-5 For Trauma-Exposed Children and AdolescentsRodolfo Preciado FabiánNo ratings yet
- Post-Falls Assessment Form FCG FinalDocument2 pagesPost-Falls Assessment Form FCG Finalbernie hewsonNo ratings yet
- Sam 093 FDocument8 pagesSam 093 FVerenice Henostroza LopezNo ratings yet
- Acidosis: Acid-Base Control SystemsDocument4 pagesAcidosis: Acid-Base Control SystemsAnila zafarNo ratings yet
- Hypernatremia: Done By:areen TarawnehDocument10 pagesHypernatremia: Done By:areen Tarawnehraed faisalNo ratings yet
- MOST IMPORATANT ONE LINERS Compiled by Medicinosis Magnus 2Document18 pagesMOST IMPORATANT ONE LINERS Compiled by Medicinosis Magnus 2VAIBHAV SHARMA- 122No ratings yet
- Body Dysmorphic Disorder: A Screening Guide For OrthodontistsDocument4 pagesBody Dysmorphic Disorder: A Screening Guide For Orthodontistsdruzair007No ratings yet
- Congenital Muscular TorticollisDocument15 pagesCongenital Muscular TorticollisAhmedAbdelZaherNo ratings yet
- Delusional DisorderDocument12 pagesDelusional Disorderayyappan.ashok6713100% (2)
- Psychiatric Disorders in Medical Practice: Specific SyndromesDocument14 pagesPsychiatric Disorders in Medical Practice: Specific SyndromesEduard TomițaNo ratings yet
- Factitious Disorder Imposed On Another IIIDocument4 pagesFactitious Disorder Imposed On Another IIIirsan_unhaluNo ratings yet
- VP Shunt Pada NPHDocument1 pageVP Shunt Pada NPHmiranti fauziNo ratings yet
- 3567 7418 1 PBDocument8 pages3567 7418 1 PBQuynh Anh TranNo ratings yet
- Psychiatry's New Brain-Mind and The Legend of The "Chemical Imbalance"Document1 pagePsychiatry's New Brain-Mind and The Legend of The "Chemical Imbalance"alloNo ratings yet
- Dissociative Identity DisorderDocument1 pageDissociative Identity DisorderMary Belle OrtegaNo ratings yet
- Levels of PreventionDocument12 pagesLevels of PreventionRuth EkanemNo ratings yet
- Eating DisordersDocument3 pagesEating DisordersSawera KhadimNo ratings yet
- Ian Caplar - Depressive Disorders Powerpoint 1Document23 pagesIan Caplar - Depressive Disorders Powerpoint 1api-314113064No ratings yet
- Trauma and Stressor-Related DisordersDocument32 pagesTrauma and Stressor-Related DisordersRay Anne Labra-PepitoNo ratings yet
- Physical Therapy Initial Evaluation: Subjective FindingsDocument12 pagesPhysical Therapy Initial Evaluation: Subjective FindingsAdrian LacsonNo ratings yet
- Multiple Organ Dysfunction Syndrome (MODS)Document1 pageMultiple Organ Dysfunction Syndrome (MODS)mikErlh50% (2)
- Sensus Harian TGL 12 Maret 2022......Document96 pagesSensus Harian TGL 12 Maret 2022......Ruhut Putra SinuratNo ratings yet
- (ARTIGO) ARCELUS, Et Al. - Prevalence of Eating Disorders Amongst Dancers. A Systemic Review and Meta-Analysis (2013) - PUBMEDDocument28 pages(ARTIGO) ARCELUS, Et Al. - Prevalence of Eating Disorders Amongst Dancers. A Systemic Review and Meta-Analysis (2013) - PUBMEDGuido BrustNo ratings yet
- Retinal Vascular Diseas E: Christine Anne D. EspejaDocument25 pagesRetinal Vascular Diseas E: Christine Anne D. EspejaPaolo QuezonNo ratings yet
- Adult Development and Aging The Canadian Experience 1st Edition Harper Test BankDocument17 pagesAdult Development and Aging The Canadian Experience 1st Edition Harper Test Bankalexanderariellpu9q100% (26)
- Depression: Depression Is Different From Sadness or Grief/BereavementDocument3 pagesDepression: Depression Is Different From Sadness or Grief/BereavementSalinaMaydinNo ratings yet