Professional Documents
Culture Documents
Dementia NCP
Uploaded by
Donnalyn Millares0 ratings0% found this document useful (0 votes)
268 views3 pagesAfter 1 day of nursing intervention, the patient will have preserved sensory and communication abilities and controlled effects of deficits. The nursing intervention included assessing the patient's cognitive, sensory, and communication functions and making appropriate environmental modifications to enhance the patient's abilities and promote safety. Evaluation after 1 day found the patient was able to respond and communicate appropriately within the limits of their disease process.
Original Description:
Original Title
DEMENTIA-NCP-
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentAfter 1 day of nursing intervention, the patient will have preserved sensory and communication abilities and controlled effects of deficits. The nursing intervention included assessing the patient's cognitive, sensory, and communication functions and making appropriate environmental modifications to enhance the patient's abilities and promote safety. Evaluation after 1 day found the patient was able to respond and communicate appropriately within the limits of their disease process.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
268 views3 pagesDementia NCP
Uploaded by
Donnalyn MillaresAfter 1 day of nursing intervention, the patient will have preserved sensory and communication abilities and controlled effects of deficits. The nursing intervention included assessing the patient's cognitive, sensory, and communication functions and making appropriate environmental modifications to enhance the patient's abilities and promote safety. Evaluation after 1 day found the patient was able to respond and communicate appropriately within the limits of their disease process.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 3
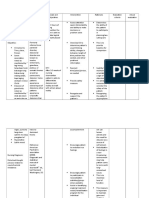
Assessment Nursing Dx.
Planning Intervention Rationale Evaluation
Subjective Disturbed After 1 day of Independent: Identify factors After 1 day of
Data: thought nursing Identify factors present (e.g., present that is nursing
“I’ve been processes intervention, the acute/chronic brain important to know intervention, the
forgetting related to patient will syndrome, stroke, the patient
things. physiologic maintain reality Alzheimer’s disease), brain causative/contributi maintained
Yesterday, I al changes orientation and injury or increased ng factor. reality orientation
couldn’t such as recognizes intracranial pressure, anoxic and recognizes
remember aging (66 changes in changes in
event, acute infections,
my dog’s y/o), and thinking/behavio thinking/behavio
malnutrition, sleep or
name. I was disorientatio ur. ur.
trying to n AEB sensory deprivation, chronic
call her to patient mental illness.
come in and reported
I just stood that she Review laboratory values for Monitoring
there sometimes abnormalities such as laboratory values
staring at has metabolic aids in identifying
her for a difficulty alkalosis, hypokalemia, ane contributing
good long thinking of mia, elevated ammonia factors.
time. It was the words levels, and signs of infection.
very scary.” she needs to
As express Assess attention
verbalized herself and span/distractibility and This determines the
by the concerned ability to make decisions or
patient. of being ability of the
problem solve. patient to
forgetful,
Objective frequently participate in
Data: misplacing planning/executing
Mini objects or Assist with testing/review care.
Mental forgetting results evaluating mental
State Exam what she status according to age and This is to assess the
score: was doing. developmental capacity. degree of
24/30 impairment.
Age: 66 y/o Interview SO or caregiver to
Temperatur determine patient’s usual
e: 37.2 ̊C thinking ability, changes in
HR: 85 behavior, length of time This is to provide
bpm problem has existed, and baseline for
BP: 142/76 other pertinent information. comparison.
Respiratory
rate: 17, Reorient to
unlabored
time/place/persin, as
needed. Have patient write Inability to
name periodically; keep this maintain
record for comparison and orientation is a sign
report differences. of deterioration.
These are
important
measures to
prevent further
deterioration and
maximize level of
function.
Assessment Nursing Dx. Planning Intervention Rationale Evaluation
Subjective Data: Disturbed After 1 day of Independent: Cognitive After 1 day of
“I just seem to sensory nursing Assess for dysfunction nursing
get frustrated or perception intervention, the confusional behavior changes intervention, the
irritated easily.” related to Patient will have state, may result from Patient had
As verbalized by inability to preservation of disorientation, sensory preservation of
the patient. communicate, sensory/perceptual difficulty and deficits/deprivation sensory/perceptual
understand, and function and slowing of caused by function and
Objective Data: speak/respond controlled effects mental ability, physiologic, controlled effects of
Mini Mental AEB rapid mood of deficits within changes in psychological, deficits within limits
State Exam swings and limits of disease behavior and and/or of disease process,
score: 24/30 irritability. process, and emotional environmental and patient is now
Age: 66 y/o patient will be able responses factors. able to respond and
Temperature: to respond and communicate to
37.2 ̊C communicate to the discussion
HR: 85 bpm the discussion Assess visual Presbyopia is appropriately.
BP: 142/76
appropriately. acuity, visual common among
Respiratory rate:
difficulties or elderly, other
17, unlabored
loss and its visual changes
effect from these caused by
changes; physiologic
presence changes require
of cataract, correction
glaucoma, and by surgery or with
status of eye glasses. Visual
remaining vision. deficits create
mobility and
socialization
changes.
Assess auditory Presbycusis is
acuity, cerumen common in the
in ears, elderly. Conductive
responses to hearing loss results
noises and effect in false
on hearing, interpretation of
ability to words and creates
communicate, poor
amount of loss communication,
and effect, and isolation and
difficulty in depression.
locating and
identifying
sounds. Enhances
Face the patient, communication if
use eye contact hearing is impaired
and speak loud and promotes
enough to be feeling of warmth
heard, speak and caring.
slowly and
clearly with
proper pitch, use
short clear
sentences and
gestures,
maintain
position even
with patient to
allow view of
lips, and use
touch to hold
attention.
Provides for
Instruct family in patient safety by
environmental preventing injury in
modifications to the presence of
enhance vision, sensory
hearing, taste, impairment.
smell, and touch
as appropriate.
You might also like
- Disturbed Thought Process NCP Gallano May 22 2018Document3 pagesDisturbed Thought Process NCP Gallano May 22 2018Charles Mallari ValdezNo ratings yet
- Nursing Care Plan For Impaired Environmental Interpretaion NCPDocument4 pagesNursing Care Plan For Impaired Environmental Interpretaion NCPderic100% (2)
- Everyone Would Be Better Off Without Me" As Verbalized by The PatientDocument4 pagesEveryone Would Be Better Off Without Me" As Verbalized by The PatientDanica Kate GalleonNo ratings yet
- NCP 2Document2 pagesNCP 2ampalNo ratings yet
- NCP PsychosisDocument3 pagesNCP PsychosisKristian Karl Bautista Kiw-is100% (1)
- NCP For FractureDocument4 pagesNCP For FracturejpNo ratings yet
- NCP FormatDocument3 pagesNCP FormatAl Bhert Timbal MagbalotNo ratings yet
- Nursing Diagnosis: Impaired Physical Mobility Assessment Planning Intervention Rationale EvaluationDocument3 pagesNursing Diagnosis: Impaired Physical Mobility Assessment Planning Intervention Rationale EvaluationSheril Sularte CasanesNo ratings yet
- Working Phase (Psych Nursing) Progress Report Process ReportingDocument5 pagesWorking Phase (Psych Nursing) Progress Report Process ReportingCalimlim KimNo ratings yet
- Impaired MobilityDocument3 pagesImpaired MobilityYeana AlonNo ratings yet
- Jerome Andres - Silver Lining Playbook, Movie Reaction1Document3 pagesJerome Andres - Silver Lining Playbook, Movie Reaction1Jerome AndresNo ratings yet
- Quiz Process RecordingDocument7 pagesQuiz Process RecordingDewley Guevarra MontenegroNo ratings yet
- Risk For SuicideDocument3 pagesRisk For SuicidepamfiestaNo ratings yet
- Decreased Cardiac OutputDocument5 pagesDecreased Cardiac Outputshuang81No ratings yet
- Nursing Care Plan: Assessment Nursing Diagnosis Planning Implementio N EvaluationDocument3 pagesNursing Care Plan: Assessment Nursing Diagnosis Planning Implementio N EvaluationAndrew James Javier Quidez100% (1)
- Disturbed Sleeping Pattern NCPDocument4 pagesDisturbed Sleeping Pattern NCPSamVelascoNo ratings yet
- NCA2 PosttestsDocument20 pagesNCA2 PosttestsCzarena Ysabelle PayotNo ratings yet
- Drug Study HaldolDocument2 pagesDrug Study HaldolGracia EvangelistaNo ratings yet
- Drug StudyDocument8 pagesDrug StudyzenNo ratings yet
- NCP DepressionDocument2 pagesNCP Depressionhollymadison80% (5)
- Case Study Scenario # 1 Congestive Heart Failure (Mojica)Document10 pagesCase Study Scenario # 1 Congestive Heart Failure (Mojica)Noah Kent MojicaNo ratings yet
- Nursing Care PlanDocument2 pagesNursing Care PlanCaracel Cabrera SobionoNo ratings yet
- X. Nursing Care Plan: ObjectiveDocument6 pagesX. Nursing Care Plan: ObjectiveRenea Joy ArruejoNo ratings yet
- Nursing Care Plan: Subjective CuesDocument6 pagesNursing Care Plan: Subjective CuesRYAN SAPLADNo ratings yet
- DS BiperidenDocument3 pagesDS BiperidenbillyktoubattsNo ratings yet
- NCP Systemic Viral Infection SVIDocument4 pagesNCP Systemic Viral Infection SVIPavel Kolesnikov100% (1)
- FlupentixolDocument1 pageFlupentixolArnzz AgbulosNo ratings yet
- XIII. Process Recording: Nurse Patient InteractionDocument9 pagesXIII. Process Recording: Nurse Patient InteractionJaka Carina CalicaNo ratings yet
- NCP Gouty ArthritisDocument21 pagesNCP Gouty ArthritisSeanmarie CabralesNo ratings yet
- Social IsolationDocument2 pagesSocial IsolationFlos Carmeli MontanaNo ratings yet
- NoncomplianceDocument3 pagesNoncomplianceChristy Berry100% (1)
- NCP Severe HypocalcemiaDocument4 pagesNCP Severe HypocalcemiaMark Zedrix MediarioNo ratings yet
- Therapeutic Communication: Department of Health, PhilippinesDocument35 pagesTherapeutic Communication: Department of Health, PhilippinesKeith Clarence BunaganNo ratings yet
- HoplessnessDocument16 pagesHoplessnessHamza IshtiaqNo ratings yet
- 5 NCPDocument3 pages5 NCPAllord Lacanilao Bungay0% (1)
- NCPDocument2 pagesNCPsphinx809100% (2)
- Process RecordingDocument12 pagesProcess Recordingchristian_cayle100% (1)
- NCPDocument1 pageNCPTalTal Balcera Beniten100% (1)
- Psych NCP SchizopreniaDocument5 pagesPsych NCP SchizopreniaPatricia Lae Retonda DeLazoNo ratings yet
- NCP ImmobiltyDocument4 pagesNCP ImmobiltyAlizza Therese Severo AnzanoNo ratings yet
- Nursing Care Plan: Assessment Diagnosis Planning Interventions Rationale EvaluationDocument11 pagesNursing Care Plan: Assessment Diagnosis Planning Interventions Rationale EvaluationDa NicaNo ratings yet
- Activity IntoleranceDocument3 pagesActivity Intolerancelouie roderosNo ratings yet
- High Percentage of Sleep Disturbances Can Affect The Recovery of The PatientDocument1 pageHigh Percentage of Sleep Disturbances Can Affect The Recovery of The PatientMatt SinnungNo ratings yet
- Assessment Diagnosis Background Knowledge Planning Intervention Rationale Evaluation SubjectiveDocument3 pagesAssessment Diagnosis Background Knowledge Planning Intervention Rationale Evaluation SubjectiveAngelaNo ratings yet
- WHOQOL 100 InglesDocument30 pagesWHOQOL 100 Inglescristhianibo777No ratings yet
- Cutaneous Anthrax Nursing Care PlanDocument2 pagesCutaneous Anthrax Nursing Care PlanYayin Pestaño100% (1)
- Potential Nursing Care Plan SchizopremiaDocument1 pagePotential Nursing Care Plan SchizopremiaopxNo ratings yet
- Impaired Physical MobilityDocument3 pagesImpaired Physical MobilityCalimlim Kim100% (1)
- Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective Short Term Short TermDocument2 pagesAssessment Diagnosis Planning Intervention Rationale Evaluation Subjective Short Term Short TermFrancis Xavier S. MendezNo ratings yet
- Cognitive TherapyDocument7 pagesCognitive Therapyshivani singhNo ratings yet
- NCP Alzheimers DiseaseDocument2 pagesNCP Alzheimers DiseaseShawn TejanoNo ratings yet
- Acute Pain Related To Tissue Trauma and InjuryDocument4 pagesAcute Pain Related To Tissue Trauma and Injuryprickybiik50% (2)
- Novilyn C. Pataray Bsn-Ii Retinophathy: St. Paul College of Ilocos SurDocument1 pageNovilyn C. Pataray Bsn-Ii Retinophathy: St. Paul College of Ilocos SurCharina AubreyNo ratings yet
- NCP-Septic Shock (Acute Pain)Document3 pagesNCP-Septic Shock (Acute Pain)Ted anadiloNo ratings yet
- Fdar - Schizophrenia Jan 11-13Document2 pagesFdar - Schizophrenia Jan 11-13Grape Juice100% (1)
- Alzheimers Disease Nursing Care PlanDocument6 pagesAlzheimers Disease Nursing Care PlanMary Josette NavarraNo ratings yet
- NSG Care Plan - BipolarDocument17 pagesNSG Care Plan - BipolaraijelethdaldeavilaNo ratings yet
- Nursing Care Plan: Phinma University of IloiloDocument2 pagesNursing Care Plan: Phinma University of IloiloBeatrice ManingasNo ratings yet
- Altered Thought ProcessDocument17 pagesAltered Thought Processbinteazhar50% (2)
- NCPDocument3 pagesNCPCharles Mallari Valdez100% (1)
- Memory:: EncodingDocument4 pagesMemory:: EncodingNoor Ul Ain ZareefNo ratings yet
- Metacoqnitive in Language TeachingDocument8 pagesMetacoqnitive in Language TeachingbilaNo ratings yet
- Jerome Bruner (Cognitive Development & Constructivist Theory)Document10 pagesJerome Bruner (Cognitive Development & Constructivist Theory)Gie Marie Francisco UmaliNo ratings yet
- Vaster Than Sky Greater Than Space - Mooji - SampleDocument18 pagesVaster Than Sky Greater Than Space - Mooji - SampleglennkenobiNo ratings yet
- Literary DevicesDocument8 pagesLiterary DevicesShiela Mae CruzNo ratings yet
- Creative Arts Music and Drama in The CurriculumDocument12 pagesCreative Arts Music and Drama in The CurriculumRobin Escoses MallariNo ratings yet
- Pepperberg - Parrot Learning: Issues and DebatesDocument7 pagesPepperberg - Parrot Learning: Issues and DebatesNadeen KhalilNo ratings yet
- Piaget StagesDocument6 pagesPiaget StagesleyliliNo ratings yet
- Schemas: Cultural Differences in Social CognitionDocument2 pagesSchemas: Cultural Differences in Social Cognitionnguyễnthùy dươngNo ratings yet
- Structured Learning ExperienceDocument4 pagesStructured Learning ExperienceKun AoiNo ratings yet
- Kimchi-The Perception of Hierarchical StructureDocument24 pagesKimchi-The Perception of Hierarchical StructureIntunericulNo ratings yet
- Can Dogs Sense EmotionDocument2 pagesCan Dogs Sense EmotionArelys Ariana PEREZ FLORESNo ratings yet
- Rano - The Effect of MusicDocument6 pagesRano - The Effect of MusicAbner Harryndra Naiara SiregarNo ratings yet
- Media BiasDocument25 pagesMedia BiasgefrancaNo ratings yet
- ORGANISATIONAL BEHAVIOUR CHAPTER 3,5 Shiv DasDocument16 pagesORGANISATIONAL BEHAVIOUR CHAPTER 3,5 Shiv Dasjatin12335jatinNo ratings yet
- Eisen, Mitchell L. - Memory and Suggestibility in The Forensic Interview (Personality and Clinical Psychology) (2001) PDFDocument496 pagesEisen, Mitchell L. - Memory and Suggestibility in The Forensic Interview (Personality and Clinical Psychology) (2001) PDFchampang supernova100% (1)
- Cis - Pec - Thinking SkillsDocument4 pagesCis - Pec - Thinking SkillsTineswaran SehgarNo ratings yet
- English For Social CommunicationDocument2 pagesEnglish For Social CommunicationnursaidaNo ratings yet
- Behaviorism Cognitivism ConstructivismDocument2 pagesBehaviorism Cognitivism Constructivism1005 Siti Ainunnisa Lingga WinariNo ratings yet
- Super Reading: Week 3 WorkbookDocument20 pagesSuper Reading: Week 3 WorkbookAnteNo ratings yet
- C9 - BPSY1113 BehaviorismDocument45 pagesC9 - BPSY1113 BehaviorismAsia AbduNo ratings yet
- David Carr - The Fifth Meditation and Husserls CartesianismDocument23 pagesDavid Carr - The Fifth Meditation and Husserls CartesianismMarina LilásNo ratings yet
- Collective Memory PhenomenaDocument2 pagesCollective Memory PhenomenaAndrey GerstNo ratings yet
- Academic Vocabulary Set 01 Unit1:Learn To Succeed: Words IPA Meaning and Example AdolescenceDocument4 pagesAcademic Vocabulary Set 01 Unit1:Learn To Succeed: Words IPA Meaning and Example AdolescenceTrung TrầnNo ratings yet
- UCU103 Case Study 2 Thinking For OneselfDocument6 pagesUCU103 Case Study 2 Thinking For OneselfAvuh AtsienoNo ratings yet
- Developing The Whole Person Lesson 2Document36 pagesDeveloping The Whole Person Lesson 2AngelaNo ratings yet
- Ericsson Verbal ProtocolDocument67 pagesEricsson Verbal Protocolkrupicevadora100% (1)
- Dream ProgramingDocument15 pagesDream ProgramingMohanavelu Ramasamy100% (1)
- Blooms Taxonomy and Verbs For Assessment CriteriaDocument2 pagesBlooms Taxonomy and Verbs For Assessment CriteriaTomNo ratings yet
- Human Memory Don't Ask Too Much of Mere Mortals: Material Mainly From Dix Et Al Chapter 1Document22 pagesHuman Memory Don't Ask Too Much of Mere Mortals: Material Mainly From Dix Et Al Chapter 1Naman LadhaNo ratings yet