Professional Documents
Culture Documents
Thalassemia Nursing Diagnosis and Care
Thalassemia Nursing Diagnosis and Care
Uploaded by
Hannah Clarisse Monge IgniCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Thalassemia Nursing Diagnosis and Care
Thalassemia Nursing Diagnosis and Care
Uploaded by
Hannah Clarisse Monge IgniCopyright:
Available Formats
Activity intolerance r/t imbalance between oxygen supply and
demand secondary to anemia AEB lethargy and weakness
1. Discuss with patient the need for activity to communicate to patient that
activity will improve physical and psychosocial well-being.
2. Identify and minimize factors that decrease the patient’s exercise tolerance to
help increase the activity level.
3. Support and encourage activity to patient’s level of tolerance to help patient
develop independence.
Fear r/t ability to live with serious disease secondary to thalassemia AEB
verbalizing worry of his condition--"baka mamatay ako agad, paano na sila mama?"
1. Open up about your awareness of the patient’s fear. This approach validates the
feelings the patient is holding and demonstrates recognition of those feelings.
2. Tell patient that fear is a normal and appropriate response to circumstances in
which pain, danger, or loss of control is anticipated or felt. This reassurance
places fear within the field of normal human experiences.
3. If patient’s fear is a reasonable response, empathize with him or her. Avoid
false reassurances and be truthful. Reassure patients that asking for help is both
a sign of strength and a step toward resolution of the problem.
Risk for Infection r/t inadequate secondary defenses: immunosuppression secondary
to thalassemia
1. Monitor white blood count (WBC). Rising WBC indicates body's efforts to combat
pathogens; normal values: 4000 to 11,000.
2. Assess nutritional status, including weight, history of weight loss, and serum
albumin. Patients with poor nutritional status may be anergic, or unable to muster
a cellular immune response to pathogens and are therefore more susceptible to
infection.
3. Limit visitors. To reduce the number of organisms in patient's environment and
restrict visitation by individuals with any type of infection to reduce the
transmission of pathogens to the patient at risk for infection.
IRON CHELATION:
A cardinal rule of iron chelation therapy was established by Modell and her
colleagues in the 1970s and reiterated in the 1990s. (source:
https://ashpublications.org/blood/article/111/2/483/103696/Oral-iron-chelation-new-
drug-old-rules)
In the 1950s, Norman Clarke, Sr. was treating workers at a battery factory for lead
poisoning when he noticed that some of his patients had improved angina pectoris
following chelation therapy.[18] Clarke subsequently administered chelation therapy
to patients with angina pectoris and other occlusive vascular disease and published
his findings in The American Journal of the Medical Sciences in December 1956.
(source: https://en.wikipedia.org/wiki/Chelation_therapy#History)
You might also like
- Code Blue PDFDocument9 pagesCode Blue PDFanggristyanugrohoNo ratings yet
- Dental MaterialDocument2 pagesDental MaterialDela martha0% (1)
- Kause and Effect MOT Intake Form Carrie KauseDocument4 pagesKause and Effect MOT Intake Form Carrie KauseCarrie KauseNo ratings yet
- Lesson PlanDocument8 pagesLesson PlanUpendra Nayka50% (2)
- Management of Tuberculosis: A guide for clinicians (eBook edition)From EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)No ratings yet
- Hepatocellular CarcinomaDocument24 pagesHepatocellular CarcinomaEthan Matthew HuntNo ratings yet
- New Perio ClassificationDocument8 pagesNew Perio ClassificationLauraNo ratings yet
- Bibliotherapy Self Harm 2011Document6 pagesBibliotherapy Self Harm 2011Adina DanciuNo ratings yet
- Exercise After Stroke GuidelinesDocument67 pagesExercise After Stroke GuidelinesMTEMEINo ratings yet
- PRIORITIZATION-NCP Acute Myelogenous LeukemiaDocument2 pagesPRIORITIZATION-NCP Acute Myelogenous LeukemiaAllan Macacapagal50% (2)
- Learning Packet in Level 2 RLE - RED: College of Nursing School Year 2020-2021Document28 pagesLearning Packet in Level 2 RLE - RED: College of Nursing School Year 2020-2021Nur SetsuNo ratings yet
- Intrusión OrtodónticaDocument4 pagesIntrusión OrtodónticaLisbethNo ratings yet
- Actual NCPDocument2 pagesActual NCPbaki0146No ratings yet
- Specialized Community Health NursingDocument45 pagesSpecialized Community Health NursingdaveNo ratings yet
- Case Report On Bipolar Affective Disorder: Mania With Psychotic SymptomsDocument2 pagesCase Report On Bipolar Affective Disorder: Mania With Psychotic SymptomskslhfwoiebvNo ratings yet
- KamanJan ChloroquineDocument3 pagesKamanJan Chloroquinekimberly_caberteNo ratings yet
- Example of Drug StudyDocument2 pagesExample of Drug Studydonna mae junioNo ratings yet
- Physical Exam - AppendectomyDocument8 pagesPhysical Exam - Appendectomyirish felixNo ratings yet
- Nursing Care Plan On SepsisDocument6 pagesNursing Care Plan On SepsisleoNo ratings yet
- Assessment Diagnosis Rationale Planning Implementation Rationale EvaluationDocument2 pagesAssessment Diagnosis Rationale Planning Implementation Rationale Evaluationkristel_nicole18yahoNo ratings yet
- Reflection On MCN LECDocument12 pagesReflection On MCN LECLecery Sophia WongNo ratings yet
- PantoprazoleDocument1 pagePantoprazolehahahahaaaaaaaNo ratings yet
- AmbroxolDocument1 pageAmbroxolPrecious CarmelaNo ratings yet
- Gastroschisis & OmphaloceleDocument1 pageGastroschisis & OmphaloceleMaecy PasionNo ratings yet
- CELINDocument9 pagesCELINaikoestrellaNo ratings yet
- Tamsulosin - Drug Information - UpToDateDocument23 pagesTamsulosin - Drug Information - UpToDateGénesis GabrielaNo ratings yet
- NCP2 - DengueDocument4 pagesNCP2 - DengueSummer SuarezNo ratings yet
- A Client With Cushing's Syndrome: Nursing Care PlanDocument1 pageA Client With Cushing's Syndrome: Nursing Care PlanJulius Caesar ColladoNo ratings yet
- Health Teaching PlanDocument10 pagesHealth Teaching PlanPaolo Vittorio Perdigueros GonzalesNo ratings yet
- AspirinDocument1 pageAspirinAmanda CoadNo ratings yet
- Health-Perception-Health-Management PatternDocument3 pagesHealth-Perception-Health-Management PatternBela MillenaNo ratings yet
- MetronidazoleDocument4 pagesMetronidazoleapi-3797941100% (4)
- Discharge Plan Post SeizureDocument2 pagesDischarge Plan Post SeizureVecky TolentinoNo ratings yet
- Baiae NCPDocument1 pageBaiae NCPreignyfayeNo ratings yet
- Nursing Care Plan On HypertensionDocument5 pagesNursing Care Plan On Hypertensionbhavana100% (1)
- Common Side Effects of Oxytocin Include:: CNS: Maternal: COMADocument3 pagesCommon Side Effects of Oxytocin Include:: CNS: Maternal: COMAann camposNo ratings yet
- Nursing Care Plan - EVALUATION PHASEDocument3 pagesNursing Care Plan - EVALUATION PHASEChezka Orton Swift BolintiamNo ratings yet
- Tetracycline Drug StudyDocument5 pagesTetracycline Drug StudyEmagra AzilNo ratings yet
- As Needed.: Environmental Stimuli 6Document4 pagesAs Needed.: Environmental Stimuli 6Nicole GumolonNo ratings yet
- The Difference Between Community Health and Public Health NursingDocument1 pageThe Difference Between Community Health and Public Health NursingMelissa Briggs100% (1)
- Criteria Good Fair Poor Rationale Justification XDocument3 pagesCriteria Good Fair Poor Rationale Justification XJaye DangoNo ratings yet
- Group1 HTP Dengue-FinalDocument9 pagesGroup1 HTP Dengue-FinalCHRISTINE GRACE ELLONo ratings yet
- Virtual Clinical Duty Daily RequirementsDocument7 pagesVirtual Clinical Duty Daily RequirementsEdgie FabreNo ratings yet
- Atrial Septal Defect - 7 Year OldDocument1 pageAtrial Septal Defect - 7 Year OldMSNo ratings yet
- Drug StudyDocument2 pagesDrug Studypopoyoio100% (2)
- Nursing Care Plan: Cues Objectives Interventions Rationale EvaluationDocument2 pagesNursing Care Plan: Cues Objectives Interventions Rationale EvaluationJP2001100% (1)
- Case CHFDocument10 pagesCase CHFAgnes Erlita Distriani Patade50% (2)
- Assessment Nursing Diagnosis Planning Interventions EvaluationsDocument4 pagesAssessment Nursing Diagnosis Planning Interventions EvaluationsAjay SupanNo ratings yet
- FNCPDocument5 pagesFNCPCarina QuibinitNo ratings yet
- Rufino, Leslie Kriztel S. BSN 3-2 Group 1Document6 pagesRufino, Leslie Kriztel S. BSN 3-2 Group 1Deinielle Magdangal RomeroNo ratings yet
- NPI Inference Remark/AnalysisDocument1 pageNPI Inference Remark/AnalysisAziil LiizaNo ratings yet
- Ppe4 Reflection AssignmentDocument11 pagesPpe4 Reflection Assignmentapi-318846856100% (1)
- Novilyn C. Pataray BSN - Ii Impetigo: St. Paul College of Ilocos SurDocument1 pageNovilyn C. Pataray BSN - Ii Impetigo: St. Paul College of Ilocos SurCharina AubreyNo ratings yet
- Generic Name & Brand Name Mechanism of Action Indications and Drug Rationale Contraindications Common Side Effects Nursing ConsiderationsDocument2 pagesGeneric Name & Brand Name Mechanism of Action Indications and Drug Rationale Contraindications Common Side Effects Nursing ConsiderationsMary Shine GonidaNo ratings yet
- Hypertension CASE REPORTDocument57 pagesHypertension CASE REPORTJulienne Sanchez-SalazarNo ratings yet
- ANATOMY AND PHYSIOLOGY of RabiesDocument5 pagesANATOMY AND PHYSIOLOGY of RabiesDavid CalaloNo ratings yet
- NCP Cough PneumoniaDocument2 pagesNCP Cough PneumoniaAirme Raz AlejandroNo ratings yet
- Drug StudyDocument2 pagesDrug Studymegreen GamingNo ratings yet
- NCP - ERDocument5 pagesNCP - ERAnnelore ArcayNo ratings yet
- Valacyclovir HydrochlorideDocument3 pagesValacyclovir HydrochlorideAndrea Huecas TriaNo ratings yet
- Ceftriaxone Sodium Drug StudyDocument1 pageCeftriaxone Sodium Drug StudyMelissa Marie CustodioNo ratings yet
- RRLDocument4 pagesRRLAnnalyn MantillaNo ratings yet
- Therapeutic Communication: Department of Health, PhilippinesDocument35 pagesTherapeutic Communication: Department of Health, PhilippinesKeith Clarence BunaganNo ratings yet
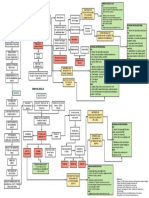
- 4 Flow Chart PretermDocument4 pages4 Flow Chart PretermYeni PuspitaNo ratings yet
- Nursing Care Plan: Subjective DataDocument4 pagesNursing Care Plan: Subjective DataAbdallah AlasalNo ratings yet
- Sample Letter Templates (4th Year)Document49 pagesSample Letter Templates (4th Year)Yna LafuenteNo ratings yet
- GC COURSEWORK (Maternal April 13, 2020) - VARGASDocument5 pagesGC COURSEWORK (Maternal April 13, 2020) - VARGASKathleen VargasNo ratings yet
- HEMATOLOGICAL CONDITIONS Answers Theory 2Document14 pagesHEMATOLOGICAL CONDITIONS Answers Theory 2CJ RelleveNo ratings yet
- Sample Family Nursing Care PlanDocument1 pageSample Family Nursing Care PlanHannah Clarisse Monge IgniNo ratings yet
- Herpes Zoster (Shingles Acute Posterior Ganglionitis)Document2 pagesHerpes Zoster (Shingles Acute Posterior Ganglionitis)Hannah Clarisse Monge IgniNo ratings yet
- Herpes Zoster: Shingles Acute Posterior GanglionitisDocument23 pagesHerpes Zoster: Shingles Acute Posterior GanglionitisHannah Clarisse Monge IgniNo ratings yet
- Rabies: A Case Study by Hannah IgniDocument15 pagesRabies: A Case Study by Hannah IgniHannah Clarisse Monge IgniNo ratings yet
- ENDOCRINODocument14 pagesENDOCRINOreogomezNo ratings yet
- Dilg Reportorial 2019116 - Fc16750a06Document150 pagesDilg Reportorial 2019116 - Fc16750a06Lowela Abogadie100% (1)
- Scope and Standards of Nursing PracticeDocument12 pagesScope and Standards of Nursing Practiceapi-251834934No ratings yet
- Delay Tooth EruptionDocument4 pagesDelay Tooth EruptionSyifa IKNo ratings yet
- Salivary Gland RadiologyDocument17 pagesSalivary Gland RadiologyAbdillah Adipatria Budi AzharNo ratings yet
- jpsr09021729 PDFDocument6 pagesjpsr09021729 PDFirsyad tsaniNo ratings yet
- Seldinger ModifiedseldingerDocument6 pagesSeldinger ModifiedseldingerThiago BañosNo ratings yet
- Case Study Presentation KPJ JohorDocument131 pagesCase Study Presentation KPJ JohorAmar Nur Arif ZazuliNo ratings yet
- Chromogenic Bacteria in The Oral Cavity and Social Impact in Pediatric Dentistry A Systematic ReviewDocument20 pagesChromogenic Bacteria in The Oral Cavity and Social Impact in Pediatric Dentistry A Systematic ReviewAthenaeum Scientific PublishersNo ratings yet
- CMHNDocument44 pagesCMHNKumaidi Potter100% (1)
- SJ Flyer BigDocument1 pageSJ Flyer Bigapi-261038003No ratings yet
- Module Date List 2020 2021 For Website 21 01 21Document1 pageModule Date List 2020 2021 For Website 21 01 21SKNo ratings yet
- Equinox Permission FormDocument2 pagesEquinox Permission FormBebington ExplorersNo ratings yet
- Health Teaching Plan To A Mother in A Pre-Natal Setting: Mercy Anne EcatDocument19 pagesHealth Teaching Plan To A Mother in A Pre-Natal Setting: Mercy Anne EcatMercy Anne EcatNo ratings yet
- IELTS Listening - Section 1Document8 pagesIELTS Listening - Section 1Xiomara MendozaNo ratings yet
- Faculy of Computer Science and Engineering Project Registration Form Final Year Project YEARDocument1 pageFaculy of Computer Science and Engineering Project Registration Form Final Year Project YEARSadiq Shah Yushi BazukayNo ratings yet
- Ncm-106-Nursing-Process - Part3w1Document5 pagesNcm-106-Nursing-Process - Part3w1Marielle ChuaNo ratings yet
- Cad Cam International2 2016all PDFDocument52 pagesCad Cam International2 2016all PDFDragoş Şerban PopNo ratings yet
- Role of The Nurse in Disaster PDFDocument44 pagesRole of The Nurse in Disaster PDFDanielle OnaNo ratings yet
- Final Proposal Dr. JahangirDocument21 pagesFinal Proposal Dr. JahangirJahangir GibranNo ratings yet