Professional Documents
Culture Documents
Answers, Rationales, and Test Taking Strategies: Managing Care Quality and Safety
Uploaded by
NursyNurseOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Answers, Rationales, and Test Taking Strategies: Managing Care Quality and Safety
Uploaded by
NursyNurseCopyright:
Available Formats
The Client with Endocrine Health Problems 487
110. Which of the following therapeutic classes 113. Glulisine (Apidra) insulin is ordered to be
of drugs is used to treat tachycardia and angina in a administered to a client before each meal. To assist
client with pheochromocytoma? the day-shift nurse who is receiving the report, the
■ 1. Angiotensin-converting enzyme (ACE) night-shift nurse gives the morning dose of glulisine.
inhibitors. When the day-shift nurse goes to the room of the
■ 2. Calcium channel blockers. client who requires glulisine, the nurse finds that
■ 3. Beta blockers. the client is not in the room. The client’s roommate
■ 4. Diuretics. tells the nurse that the client “went for a test.” What
should the nurse do next?
■ 1. Bring a small glass of juice, and locate the
Managing Care Quality and Safety client.
■ 2. Call the client’s physician.
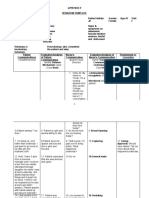
111. The nurse is reviewing the postoperative ■ 3. Check the computerized care plan to deter-
orders (see chart) just written by a physician for mine what test was scheduled.
a client with insulin-dependent diabetes who has ■ 4. Send the nurse’s assistant to the X-ray depart-
returned to the surgery floor from the recovery room ment to bring the client back to his room.
following surgery for a left hip replacement. The cli- 114. A young adult client has been diagnosed with
ent has pain of 5 on a scale of 1 to 10. The hand-off type 1 diabetes. He has an insulin drip to aid in low-
report from the nurse in the recovery room indicated ering the serum blood glucose level of 600 mg/dL.
that the vital signs have been stable for the last 30 He is also receiving ciprofloxacin (Cipro) I.V. The
minutes. After obtaining the client’s glucose level, physician orders discontinuation of the insulin drip.
the nurse should do which of the following first? The nurse should next?
■ 1. Administer the morphine. ■ 1. Discontinue the insulin drip, as ordered.
■ 2. Contact the physician to report the glucose ■ 2. Hang the next I.V. dose of antibiotic before
level and rewrite the insulin order. discontinuing the insulin drip.
■ 3. Administer oxygen per nasal canula at 2 L/ ■ 3. Inform the physician that the client has not
minute. received any subcutaneous insulin yet.
■ 4. Take the vital signs. ■ 4. Add glargine (Lantus) to the insulin drip
before discontinuing it.
Physician Order
Vital signs every 15 minutes for 4 hours, then every
hour for 8 hours. Answers, Rationales, and Test
Oxygen 2 L/minute per nasal canula.
1000 mL NS every 8 hours. Taking Strategies
10 mg morphine intramuscularly every 4 hours as
needed.
10 u regular insulin stat. The answers and rationales for each question follow
below, along with keys ( ) to the client need
(CN) and cognitive level (CL) for each question. Use
these keys to further develop your test-taking skills.
For additional information about test-taking skills
112. A client with type 1 diabetes is admitted to and strategies for answering questions, refer to pages
the emergency department with dehydration follow-
10–21, and pages 25–26 in Part 1 of this book.
ing the flu. The client has a blood glucose level of
325 mg/dL and a serum potassium level of 3.5 mEq.
The physician has ordered 1,000 mL 5% dextrose
in water to be infused every 8 hours. Prior to imple- The Client with Thyrotoxicosis
menting the physician orders, the nurse should
contact the physician, explain the situation, provide 1. 2. Graves’ disease, the most common type
background information, report the current assess- of thyrotoxicosis, is a state of hypermetabolism.
ment of the client, and: The increased metabolic rate generates heat and
■ 1. Suggest adding potassium to the fluids. produces tachycardia and fine muscle tremors.
■ 2. Request an increase in the volume of intrave- Anorexia is associated with hypothyroidism. Loss of
nous fluids. weight, despite a good appetite and adequate caloric
■ 3. Verify the order for 5% dextrose in water. intake, is a common feature of hyperthyroidism.
■ 4. Determine if the client should be placed in Cold skin is associated with hypothyroidism.
isolation. CN: Physiological adaptation;
CL: Analyze
Billings_Part 2_Chap 3_Test 08.indd 487 8/7/2010 10:17:05 AM
488 The Nursing Care of Adults with Medical and Surgical Health Problems
2. 3. A change in the menstrual interval, dimin- 7. 3. Treatment of mild ophthalmopathy that
ished menstrual flow (oligomenorrhea), or even the may accompany thyrotoxicosis includes measures
absence of menstruation (amenorrhea) may result such as wearing sunglasses to protect the eyes from
from the hormonal imbalances of thyrotoxicosis. corneal irritation. Treatment of ophthalmopathy
Oligomenorrhea in women and decreased libido and should be performed in consultation with an oph-
impotence in men are common features of thyro- thalmologist. Massaging the eyes will not help to
toxicosis. Dysmenorrhea is painful menstruation. protect the cornea. An ophthalmic anesthetic is
Metrorrhagia, blood loss between menstrual peri- used to examine and possibly treat a painful eye,
ods, is a symptom of hypothyroidism. Menorrhagia, not protect the cornea. Covering the eyes with moist
excessive bleeding during menstrual periods, is a gauze pads is not a satisfactory nursing measure
symptom of hypothyroidism. to protect the eyes of a client with exophthalmos
because treatment is not focused on moisture to the
CN: Physiological adaptation;
eye but rather on protecting the cornea and optic
CL: Analyze
nerve. In exophthalmos, the retrobulbar connec-
3. 2, 3, 5, 6. Clients with hypothyroidism tive tissues and extraocular muscle volume are
exhibit symptoms indicating a lack of thyroid hor- expanded because of fluid retention. The pressure is
mone. Bradycardia, decreased energy and lethargy, also increased.
memory problems, weight gain, coarse hair, con-
CN: Reduction of risk potential;
stipation, and menorrhagia are common signs and
CL: Synthesize
symptoms of hypothyroidism.
CN: Physiological adaptation;
8. 4. Sodium iodide 131I destroys the thyroid
follicular cells, and thyroid hormones are no longer
CL: Analyze
produced. RAI is commonly recommended for cli-
4. 1. The most serious adverse effects of PTU are ents with Graves’ disease, especially the elderly. The
leukopenia and agranulocytosis, which usually occur treatment results in a “medical thyroidectomy.” RAI
within the first 3 months of treatment. The client is given in lieu of surgery, not before surgery. RAI
should be taught to promptly report to the health care does not reduce uptake of thyroxine. The outcome
provider signs and symptoms of infection, such as a of giving RAI is the destruction of the thyroid fol-
sore throat and fever. Clients complaining of a sore licular cells. It is possible to slow the production of
throat and fever should have an immediate white thyroid hormones with RAI.
blood cell count and differential performed, and the
CN: Pharmacological and parenteral
drug must be withheld until the results are obtained.
therapies; CL: Synthesize
Painful menstruation, constipation, and increased
urine output are not associated with PTU therapy. 9. 3. The client needs to be educated about the
need for lifelong thyroid hormone replacement. Per-
CN: Pharmacological and parenteral
manent hypothyroidism is the major complication
therapies; CL: Synthesize
of RAI 131I treatment. Lifelong medical follow-up
5. 2. A typical sign of thyrotoxicosis is irritabil- and thyroid replacement are warranted. The client
ity caused by the high levels of circulating thyroid needs to monitor for signs and symptoms of hypo-
hormones in the body. This symptom decreases thyroidism, not hyperthyroidism. Resting for 1 week
as the client responds to therapy. Thyrotoxicosis is not necessary. Hypertension and tachycardia are
does not cause confusion. The client may be wor- signs of hyperthyroidism, not hypothyroidism.
ried about her illness, and stress may influence her
CN: Pharmacological and parenteral
mood; however, irritability is a common symptom of
therapies; CL: Synthesize
thyrotoxicosis and the client should be informed of
that fact rather than blamed. 10. 2. SSKI is frequently administered before
a thyroidectomy because it helps decrease the
CN: Psychosocial adaptation;
vascularity of the thyroid gland. A highly vascu-
CL: Synthesize
lar thyroid gland is very friable, a condition that
6. 4. Elevated serum concentrations of thyroid presents a hazard during surgery. Preparation of the
hormones and suppressed serum TSH are the fea- client for surgery includes depleting the gland of
tures of thyrotoxicosis. Decreased or absent serum thyroid hormone and decreasing vascularity. SSKI
TSH is a very accurate indicator of thyrotoxicosis. does not decrease the progression of exophthalmos,
Increased levels of circulating thyroid hormones and it does not decrease the body’s ability to store
cause the feedback mechanism to the brain to sup- thyroxine or increase the body’s ability to excrete
press TSH secretion. thyroxine.
CN: Physiological adaptation; CN: Pharmacological and parenteral
CL: Analyze therapies; CL: Apply
Billings_Part 2_Chap 3_Test 08.indd 488 8/7/2010 10:17:06 AM
The Client with Endocrine Health Problems 489
11. 3. SSKI should be diluted well in milk, of tetany. Bleeding on the back of the dressing is
water, juice, or a carbonated beverage before admin- related to possible incisional complications. Ten-
istration to help disguise the strong, bitter taste. sion on the suture line may indicate swelling,
Also, this drug is irritating to mucosa if taken undi- infection, or internal bleeding, but it is not related
luted. The client should sip the diluted preparation to tetany.
through a drinking straw to help prevent staining of CN: Physiological adaptation;
the teeth. Pouring the solution over ice chips will CL: Analyze
not sufficiently dilute the SSKI or cover the taste.
Antacids are not used to dilute or cover the taste 15. 2. The client with tetany is suffering from
of SSKI. Mixing in a puree would put the SSKI in hypocalcemia, which is treated by administering an
contact with the teeth. I.V. preparation of calcium, such as calcium glucon-
ate or calcium chloride. Oral calcium is then nec-
CN: Pharmacological and parenteral essary until normal parathyroid function returns.
therapies; CL: Apply Sodium phosphate is a laxative. Echothiophate
12. 3. Laryngeal nerve damage is a potential iodide is an eye preparation used as a miotic for an
complication of thyroid surgery because of the antiglaucoma effect. Sodium bicarbonate is a potent
proximity of the thyroid gland to the recurrent systemic antacid.
laryngeal nerve. Asking the client to speak helps CN: Pharmacological and parenteral
assess for signs of laryngeal nerve damage. Per- therapies; CL: Apply
sistent or worsening hoarseness and weak voice
are signs of laryngeal nerve damage and should 16. 2. Typical signs and symptoms of hypothy-
be reported to the physician immediately. Internal roidism include weight gain, fatigue, decreased
hemorrhage is detected by changes in vital signs. energy, apathy, brittle nails, dry skin, cold intoler-
The client’s level of consciousness can be partially ance, hair loss, constipation, and numbness and
assessed by asking her to speak, but that is not the tingling in the fingers. Tachycardia is a sign of
primary reason for doing so in this situation. Upper hyperthyroidism, not hypothyroidism. Diarrhea and
airway obstruction is detected by color and respira- nausea are not symptoms of hypothyroidism.
tory rate and pattern. CN: Physiological adaptation;
CN: Reduction of risk potential; CL: Analyze
CL: Analyze 17. 4. A major problem for the person with
13. 4. Equipment for an emergency tracheotomy hypothyroidism is fatigue. Other signs and symp-
should be kept in the room, in case tracheal edema toms include lethargy, personality changes, general-
and airway occlusion occur. Laryngeal nerve dam- ized edema, impaired memory, slowed speech, cold
age can result in vocal cord spasm and respiratory intolerance, dry skin, muscle weakness, constipa-
obstruction. A tracheostomy set, oxygen and suction tion, weight gain, and hair loss. Incomplete closure
equipment, and a suture removal set (for respiratory of the eyelids, hypermetabolism, and diarrhea are
distress from hemorrhage) make up the emergency associated with hyperthyroidism.
equipment that should be readily available. Total CN: Basic care and comfort;
parenteral nutrition is not anticipated for the client CL: Analyze
undergoing thyroidectomy. Intravenous infusion
via a cutdown is not an expected possible treatment 18. 4. Hypothyroidism may contribute to
after thyroidectomy. Tube feedings are not antici- sadness and depression. It is good practice for
pated emergency care. clients with newly diagnosed depression to
be monitored for hypothyroidism by checking
CN: Reduction of risk potential; serum thyroid hormone and thyroid-stimulating
CL: Synthesize hormone levels. This client needs to know that
14. 2. Tetany may occur after thyroidectomy if these feelings may be related to her low thyroid
the parathyroid glands are accidentally injured or hormone levels and may improve with treatment.
removed during surgery. This would cause a dis- Replacement therapy does not cause depression.
turbance in serum calcium levels. An early sign of Depression may accompany chronic illness, but
tetany is numbness and tingling of the fingers or it is not “normal.”
toes and in the circumoral region. Tetany may occur CN: Psychosocial adaptation;
from 1 to 7 days postoperatively. Late signs and CL: Analyze
symptoms of tetany include seizures, contraction of
the glottis, and respiratory obstruction. Pains in the
joints of the hands and feet are not early symptoms
Billings_Part 2_Chap 3_Test 08.indd 489 8/7/2010 10:17:07 AM
490 The Nursing Care of Adults with Medical and Surgical Health Problems
The Client with Diabetes Mellitus Decreased serum potassium level has no effect
on insensible fluid loss. Hypotension occurs due
19. 3. Empowerment is an approach to clinical to polyurea and inadequate fluid intake. It may
practice that emphasizes helping people discover decrease the flow of blood to the skin, causing skin
and use their innate abilities to gain mastery over to be warm and dry.
their own condition. Empowerment means that indi- CN: Reduction of risk potential;
viduals with a health problem have the tools, such CL: Analyze
as knowledge, control, resources, and experience,
to implement and evaluate their self-management 24. 4. Glargine (Lantus) is a long-acting recom-
practices. Involvement of others, such as asking the binant human insulin analog. Glargine should not
client about family involvement, implies that the be mixed with any other insulin product. Insu-
others will provide the direct care needed rather lins should not be shaken; instead, if the insulin
than the client. Asking the client what the client is cloudy, roll the vial or insulin pen between the
needs to know implies that the nurse will be the one palms of the hands.
to provide the information. Telling the client what is CN: Pharmacological and parenteral
required does not provide the client with options or therapies; CL: Synthesize
lead to empowerment.
25. 1. A rare but serious adverse effect of met-
CN: Health promotion and maintenance; formin (Glucophage) is lactic acidosis; half the
CL: Synthesize cases are fatal. Ideally, one should stop metformin
20. 1, 2, 4, 5. The risk factors for developing type for 2 days before and 2 days after drinking alcohol.
2 diabetes include giving birth to an infant weigh- Signs and symptoms of lactic acidosis are weakness,
ing more than 9 lb; obesity (BMI over 30); ethnicity fatigue, unusual muscle pain, dyspnea, unusual
of Asian, African American, or Native American stomach discomfort, dizziness or light-headedness,
Indian; age greater than 45 years; hypertension; and bradycardia or cardiac arrhythmias. Bloating is
and family history in parents or siblings. Child- not an adverse effect of metformin.
hood obesity is also a risk factor for type 2 diabetes. CN: Pharmacological and parenteral
Maintaining an ideal weight, eating a low-fat diet, therapies; CL: Evaluate
and exercising regularly decrease the risk of type 2
diabetes. 26. 3. Oral hypoglycemic agents of the sulfonylu-
rea group, such as tolbutamide (Orinase), lower the
CN: Reduction of risk potential; blood glucose level by stimulating functioning beta
CL: Analyze cells in the pancreas to release insulin. These agents
21. 2. Diabetes insipidus is caused by a defi- also increase insulin’s ability to bind to the body’s
ciency of antidiuretic hormone, which results in cells. They may also act to increase the number of
excretion of a large volume of dilute urine. There- insulin receptors in the body. Tolbutamide does not
fore, a urine specific gravity of less than 1.005 potentiate the action of insulin. Tolbutamide does
should be reported. Urine output should be 30 to not lower the renal threshold of glucose, which
50 mL/hour; thus, 350 mL is a normal urinary would not be a factor in the treatment of diabetes
output over 8 hours. The potassium level is normal. in any case. Tolbutamide does not combine with
Weight loss, not weight gain, should be monitored glucose to render it inert.
as a sign of dehydration. CN: Pharmacological and parenteral
CN: Reduction of risk potential; therapies; CL: Apply
CL: Synthesize 27. 1, 5. Being overweight and having a large
22. 1. The elevated blood glucose level indi- waist-hip ratio (central abdominal obesity) increase
cates hyperglycemia. The hemoglobin is normal. insulin resistance, making control of diabetes more
The client’s cholesterol and LDL levels are both difficult. The ADA recommends a yearly referral
normal. The nurse should determine if there are to an ophthalmologist and podiatrist. Exercise and
standing orders for the hyperglycemia or notify the weight management decrease insulin resistance.
physician. Insulin is not always needed for type 2 diabetes;
diet, exercise, and oral medications are the first-line
CN: Reduction of risk potential; treatment. The client must monitor all nutritional
CL: Analyze sources for a balanced diet–fats, carbohydrates, and
23. 3. Due to the rapid, deep respirations, the cli- protein.
ent is losing fluid from vaporization from the lungs CN: Reduction of risk potential;
and skin (insensible fluid loss). Normally, about CL: Create
900 mL of fluid is lost per day through vaporization.
Billings_Part 2_Chap 3_Test 08.indd 490 8/7/2010 10:17:08 AM
The Client with Endocrine Health Problems 491
28. 1. The client with diabetes is prone to serious 33. 1, 2, 3, 4, 5. The client with unstable diabetes
foot injuries secondary to peripheral neuropathy mellitus is at risk for many microvascular and mac-
and decreased circulation. The client should be rovascular complications. Heart disease is the lead-
taught to avoid going barefoot to prevent injury. ing cause of mortality in clients with diabetes. The
Shoes that do not fit properly should not be worn goal blood pressure for diabetics is less than 130/80
because they will cause blisters that can become mm Hg. Therefore, the nurse would need to report
nonhealing, serious wounds for the diabetic client. any findings greater than 130/80 mm Hg. The goal of
Toenails should be cut straight across. A heating pad HbA1c is less than 7%; thus, a level of 10.2% must
should not be used because of the risk of burns due be reported. HDL less than 40 mg/dL and triglycer-
to insensitivity to temperature. ides greater than 150 mg/dL are risk factors for heart
disease. The nurse would need to report the client’s
CN: Reduction of risk potential;
HDL and triglyceride levels. The urine ketones are
CL: Synthesize
negative, but this is a late sign of complications when
29. 2. A client with diabetes should be advised there is a profound insulin deficiency.
to consult a physician or podiatrist for corn removal
CN: Reduction of risk potential;
because of the danger of traumatizing the foot tissue
CL: Analyze
and potential development of ulcers. The diabetic
client should never self-treat foot problems but 34. 4. A client with diabetes who takes any
should consult a physician or podiatrist. first- or second-generation sulfonylurea should be
advised to avoid alcohol intake. Sulfonylureas in
CN: Reduction of risk potential;
combination with alcohol can cause serious disul-
CL: Synthesize
firam (Antabuse)–like reactions, including flushing,
30. 2. Proper and careful first-aid treatment is angina, palpitations, and vertigo. Serious reactions,
important when a client with diabetes has a skin cut such as seizures and possibly death, may also occur.
or laceration. The skin should be kept supple and as Hypokalemia, hyperkalemia, and hypocalcemia do
free of organisms as possible. Washing and bandag- not result from taking sulfonylureas in combination
ing the cut will accomplish this. Washing wounds with alcohol.
with alcohol is too caustic and drying to the skin.
CN: Physiological adaptation; CL: Apply
Having the children help is an unrealistic sugges-
tion and does not educate the client about proper 35. 3. The most important factor predisposing
care of wounds. Tight control of blood glucose levels to the development of type 2 diabetes mellitus is
through adherence to the medication regimen is obesity. Insulin resistance increases with obesity.
vitally important; however, it does not mean that Cigarette smoking is not a predisposing factor, but
careful attention to cuts can be ignored. it is a risk factor that increases complications of
diabetes mellitus. A high-cholesterol diet does not
CN: Reduction of risk potential;
necessarily predispose to diabetes mellitus, but
CL: Synthesize
it may contribute to obesity and hyperlipidemia.
31. 4. Diabetes mellitus is a multifactorial, Hypertension is not a predisposing factor, but it is a
systemic disease associated with problems in the risk factor for developing complications of diabetes
metabolism of all food types. The client’s diet mellitus.
should contain appropriate amounts of all three
CN: Health promotion and maintenance;
nutrients, plus adequate minerals and vitamins.
CL: Apply
CN: Basic care and comfort; CL: Apply
36. 2. The client with diabetes mellitus is espe-
32. 1. Deep, rapid respirations with long expi- cially prone to hypertension due to atherosclerotic
rations is indicative of Kussmaul’s respirations, changes, which leads to problems of the microvas-
which occur in metabolic acidosis. The respirations cular and macrovascular systems. This can result
increase in rate and depth, and the breath has a in complications in the heart, brain, and kidneys.
“fruity” or acetone-like odor. This breathing pat- Heart disease and stroke are twice as common
tern is the body’s attempt to blow off carbon dioxide among people with diabetes mellitus than among
and acetone, thus compensating for the acidosis. people without the disease. Painful, inflamed joints
The other breathing patterns listed are not related accompany rheumatoid arthritis. A stooped appear-
to ketoacidosis and would not compensate for the ance accompanies osteoporosis with narrowing of
acidosis. the vertebral column. A low hemoglobin concentra-
tion accompanies anemia, especially iron deficiency
CN: Physiological adaptation;
anemia and anemia of chronic disease.
CL: Analyze
CN: Reduction of risk potential;
CL: Analyze
Billings_Part 2_Chap 3_Test 08.indd 491 8/7/2010 10:17:08 AM
492 The Nursing Care of Adults with Medical and Surgical Health Problems
37. 1. Although some individual variation exists, 42. 1. The nurse should judge that learning has
when the blood glucose level decreases to less than occurred from evidence of a change in the client’s
70 mg/dL, the client experiences or is at risk for behavior. A client who performs a procedure safely
hypoglycemia. Hypoglycemia can occur in both and correctly demonstrates that he has acquired a
type 1 and type 2 diabetes mellitus, although it is skill. Evaluation of this skill acquisition requires
more common when the client is taking insulin. The performance of that skill by the client with observa-
nurse should instruct the client on the prevention, tion by the nurse. The client must also demonstrate
detection, and treatment of hypoglycemia. cognitive understanding, as shown by the ability
to critique the nurse’s performance. Explaining the
CN: Physiological adaptation;
steps demonstrates acquisition of knowledge at the
CL: Analyze
cognitive level only. A posttest does not indicate the
38. 4. Diabetic retinopathy, cataracts, and glau- degree to which the client has learned a psychomo-
coma are common complications in diabetics, neces- tor skill.
sitating eye assessment and examination. The feet
CN: Pharmacological and parenteral
should also be examined at each client encounter,
therapies; CL: Evaluate
monitoring for thickening, fissures, or breaks in the
skin; ulcers; and thickened nails. Although assess- 43. 32 units
ments of the abdomen, pharynx, and lymph glands Clients commonly need to mix insulin, requiring
are included in a thorough examination, they are careful mixing and calculation. The total dosage is
not pertinent to common diabetic complications. 10 units plus 22 units, for a total of 32 units.
CN: Reduction of risk potential; CN: Pharmacological and parenteral
CL: Analyze therapies; CL: Apply
39. 4. The client with diabetes mellitus who is 44. 3. Renal failure frequently results from the
taking NPH insulin (Humulin N) in the evening is vascular changes associated with diabetes melli-
most likely to become hypoglycemic shortly after tus. ACE inhibitors increase renal blood flow and
midnight because this insulin peaks in 6 to 8 hours. are effective in decreasing diabetic nephropathy.
The client should eat a bedtime snack to help pre- Chronic obstructive pulmonary disease is not a
vent hypoglycemia while sleeping. complication of diabetes, nor is it prevented by ACE
inhibitors. Pancreatic cancer is neither prevented
CN: Pharmacological and parenteral
by ACE inhibitors nor considered a complication of
therapies; CL: Apply
diabetes. Cerebrovascular accident is not directly
40. 3. If the client engages in an activity or prevented by ACE inhibitors, although management
exercise that focuses on one area of the body, that of hypertension will decrease vascular disease.
area may cause inconsistent absorption of insulin.
CN: Pharmacological and parenteral
A good regimen for a jogger is to inject the abdomen
therapies; CL: Apply
for 1 week and then rotate to the buttock. A jog-
ger may have inconsistent absorption in the legs or 45. 1. The four most commonly reported signs
arms with strenuous running. The iliac crest is not and symptoms of hypoglycemia are nervousness,
an appropriate site due to a lack of loose skin and weakness, perspiration, and confusion. Other signs
subcutaneous tissue in that area. and symptoms include hunger, incoherent speech,
tachycardia, and blurred vision. Anorexia and
CN: Pharmacological and parenteral
Kussmaul’s respirations are clinical manifestations
therapies; CL: Apply
of hyperglycemia or ketoacidosis. Bradycardia is not
41. 1. Insulin lispro (Humalog) begins to act associated with hypoglycemia; tachycardia is.
within 10 to 15 minutes and lasts approximately
CN: Reduction of risk potential;
4 hours. A major advantage of Humalog is that the
CL: Apply
client can eat almost immediately after the insulin
is administered. The client needs to be instructed 46. 2. Steroids can cause hyperglycemia because
regarding the onset, peak, and duration of all insu- of their effects on carbohydrate metabolism, making
lin, as meals need to be timed with these param- diabetic control more difficult. Aspirin is not known
eters. Waiting 1 hour to eat may precipitate hypogly- to affect glucose metabolism. Sulfonylureas are oral
cemia. Eating 2 hours before the insulin lispro could hypoglycemic agents used in the treatment of diabe-
cause hyperglycemia if the client does not have cir- tes mellitus. ACE inhibitors are not known to affect
culating insulin to metabolize the carbohydrate. glucose metabolism.
CN: Pharmacological and parenteral CN: Pharmacological and parenteral
therapies; CL: Synthesize therapies; CL: Apply
Billings_Part 2_Chap 3_Test 08.indd 492 8/7/2010 10:17:09 AM
The Client with Endocrine Health Problems 493
47. 1. Colds and influenza present special chal- 51. 2. Excessive prolactin secretion in men
lenges to the client with diabetes mellitus because results in decreased libido and impotence; these
the body’s need for insulin increases during illness. are often the only significant signs and symptoms
Therefore, the client must take the prescribed insu- until the tumor becomes large. Signs and symp-
lin dose, increase the frequency of blood glucose toms of pituitary tumors result from both the
testing, and maintain an adequate fluid intake to presence of a space-occupying mass in the cranium
counteract the dehydrating effect of hyperglyce- and the excess secretion of hormones. Lethargy
mia. Clear fluids, juices, and Gatorade are encour- and fatigue are associated with hypothyroidism or
aged. Not taking insulin when sick, or taking half Addisonian crisis. Bony proliferation and voice
the normal dose, may cause the client to develop changes are associated with excessive growth
ketoacidosis. hormone.
CN: Reduction of risk potential; CN: Physiological adaptation;
CL: Synthesize CL: Analyze
48. 1. Imbalanced nutrition: Less than body 52. 4. With transsphenoidal hypophysectomy,
requirements is a priority nursing diagnosis for the the sella turcica is entered from below, through the
client with diabetes mellitus who is experiencing sphenoid sinus. There is no external incision; the
vomiting with influenza. The diabetic client should incision is made between the upper lip and gums.
eat small, frequent meals of 50 g of carbohydrate or
CN: Reduction of risk potential;
food equal to 200 calories every 3 to 4 hours. If the
CL: Apply
client cannot eat the carbohydrates or take fluids,
the health care provider should be called or the 53. 3. Deep breathing is the best choice for help-
client should go to the emergency department. The ing prevent atelectasis. The client should be placed
diabetic client is in danger of complications with in the semi-Fowler’s position (or as ordered) and
dehydration, electrolyte imbalance, and ketoacido- taught deep breathing, sighing, mouth breathing,
sis. Increasing the client’s coping skills is important and how to avoid coughing. Blow bottles are not
to lifestyle behaviors, but it is not a priority during effective in preventing atelectasis because they do
this acute illness of influenza. Pain relief may be a not promote sustained alveolar inflation to maxi-
need for this client, but it is not the priority at this mal lung capacity. Frequent position changes help
time; neither is intolerance for activity. loosen lung secretions, but deep breathing is most
important in preventing atelectasis. Coughing is
CN: Basic care and comfort;
contraindicated because it increases intracranial
CL: Analyze
pressure and can cause cerebrospinal fluid to
49. 4. The best response is to allow the client to leak from the point at which the sella turcica was
verbalize her fears about giving herself a shot each entered.
day. Tactics that increase fear are not effective in
CN: Reduction of risk potential;
changing behavior. If possible, the client needs to be
CL: Synthesize
responsible for her own care, including giving self-
injections. It is unlikely that the client’s insurance 54. 1. A major focus of nursing care after trans-
company will pay for home-care visits if the client sphenoidal hypophysectomy is prevention of and
is capable of self-administration. monitoring for a CSF leak. CSF leakage can occur
if the patch or incision is disrupted. The nurse
CN: Psychosocial adaptation;
should monitor for signs of infection, including
CL: Synthesize
elevated temperature, increased white blood cell
count, rhinorrhea, nuchal rigidity, and persis-
tent headache. Hypoglycemia and adrenocortical
The Client with Pituitary Adenoma insufficiency may occur. Monitoring for fluctuat-
ing blood glucose levels is not related specifically
50. 1. Galactorrhea, or abnormal flow of breast to transsphenoidal hypophysectomy. The client
milk, results from overproduction of prolactin. Pitu- will be given I.V. fluids postoperatively to supply
itary tumors are almost always secreting tumors, and carbohydrates. Cushing’s disease results from adre-
they are classified by the specific hormone secreted. nocortical excess, not insufficiency. Monitoring for
Pituitary tumors can cause oversecretion of ACTH, cardiac arrtyhmias is important, but arrtythimias
GH, or TSH. Overproduction of ACTH results in are not anticipated following a transsphenoidal
Cushing’s disease. Overproduction of GH results in hypophysectomy.
gigantism. Overproduction of TSH results in hyper-
thyroidism. CN: Reduction of risk potential;
CL: Analyze
CN: Physiological adaptation; CL: Apply
Billings_Part 2_Chap 3_Test 08.indd 493 8/7/2010 10:17:10 AM
494 The Nursing Care of Adults with Medical and Surgical Health Problems
55. 1. The client’s sexual problems are directly status, energy level, muscle strength, and cognitive
related to the excessive prolactin level. Removing function. In adults, changes in sexual function,
the source of excessive hormone secretion should impotence, or decreased libido should be reported.
allow the client to return gradually to a normal Acromegaly and Cushing’s disease are conditions of
physiologic pattern. Fertility will return, and erec- hypersecretion. Diabetes mellitus is related to the
tile function and sexual desire will return to base- function of the pancreas and is not directly related
line as hormone levels return to normal. to the function of the pituitary.
CN: Physiological adaptation; CN: Reduction of risk potential;
CL: Apply CL: Analyze
56. 3. The dural opening is typically repaired 60. 1. Pituitary diabetes insipidus is a poten-
with a patch of muscle or fascia taken from the tial complication after pituitary surgery because of
abdomen or thigh. The client should be prepared possible interference with the production of antidi-
preoperatively for the presence of this additional uretic hormone (ADH). One major manifestation of
incision in the abdomen or thigh. The client will diabetes insipidus is polyuria because lack of ADH
need the patch of muscle or fascia to replace the results in insufficient water reabsorption by the
dura. Disposable sutures alone will not provide an kidneys. The polyuria leads to a decreased urine
intact suture line. Nasal packing will not provide specific gravity (between 1.001 and 1.010). The cli-
closure for the dural opening. A synthetic mesh is ent may drink and excrete 5 to 40 L of fluid daily.
not the tissue of choice for surgical repair of the Diabetes insipidus does not affect metabolism. A
dura. blood glucose level higher than 300 mg/dL is associ-
ated with impaired glucose metabolism or diabetes
CN: Reduction of risk potential; mellitus. Urine negative for sugar and ketones is
CL: Apply normal.
57. 3. If CSF leakage is suspected or confirmed, CN: Reduction of risk potential;
the client is treated initially with bed rest with the CL: Analyze
head of the bed elevated to decrease pressure on
the graft site. Most leaks heal spontaneously, but 61. 2. The major characteristic of diabetes insipi-
occasionally surgical repair of the site in the sella dus is decreased tubular reabsorption of water due
turcica is needed. Repacking the nose will not heal to insufficient amounts of antidiuretic hormone
the leak at the graft site in the dura. The client will (ADH). Vasopressin (Pitressin) is administered to the
not be returned to surgery immediately because client with diabetes insipidus because it has pressor
most leaks heal spontaneously. High-dose corti- and ADH activities. Vasopressin works to increase
costeroid therapy is not effective in healing a CSF the concentration of the urine by increasing tubu-
leak. lar reabsorption, thus preserving up to 90% water.
Vasopressin is administered to the client with dia-
CN: Physiological adaptation; betes insipidus because it is a synthetic ADH. The
CL: Apply administration of vasopressin results in increased
58. 1. After transsphenoidal surgery, the client tubular reabsorption of water, and it is effective for
must be careful not to disturb the suture line while emergency treatment or daily maintenance of mild
healing occurs. Frequent oral care should be pro- diabetes insipidus. Vasopressin does not decrease
vided with rinses of saline, and the teeth may be blood pressure or affect insulin production or glu-
gently cleaned with Toothettes. Frequent or vigor- cose metabolism, nor is insulin production a factor
ous toothbrushing or flossing is contraindicated in diabetes insipidus.
because it may disturb or cause tension on the CN: Pharmacological and parenteral
suture line. therapies; CL: Apply
CN: Physiological adaptation; 62. 1. Because diabetes insipidus involves excre-
CL: Synthesize tion of large amounts of fluid, maintaining normal
59. 4. Most clients who undergo adenoma fluid and electrolyte balance is a priority for this cli-
removal experience a gradual return of normal pitu- ent. Special dietary programs or restrictions are not
itary secretion and do not experience complications. indicated in treatment of diabetes insipidus. Serum
However, hypopituitarism can cause growth hor- glucose levels are priorities in diabetes mellitus but
mone, gonadotropin, thyroid-stimulating hormone, not in diabetes insipidus.
and adrenocorticotropic hormone deficits. The cli- CN: Physiological adaptation;
ent should be taught to monitor for change in mental CL: Evaluate
Billings_Part 2_Chap 3_Test 08.indd 494 8/7/2010 10:17:11 AM
The Client with Endocrine Health Problems 495
The Client with Addison’s Disease 67. 1. Each liter of 5% dextrose in normal saline
solution contains 170 calories. The nurse should
63. 4. Adrenal crisis can occur with physi- consult with the physician and dietitian when a
cal stress, such as surgery, dental work, infection, client is on I.V. therapy or is on nothing-by-mouth
flu, trauma, and pregnancy. In these situations, status for an extended period because further elec-
glucocorticoid and mineralocorticoid dosages are trolyte supplementation or alimentation therapy
increased. Weight loss, not gain, occurs with adrenal may be needed.
insufficiency. Psychological stress has less effect on
CN: Pharmacological and parenteral
corticosteroid need than physical stress.
therapies; CL: Apply
CN: Reduction of risk potential;
CL: Synthesize
68. 3. Electrolyte imbalances associated with
Addison’s disease include hypoglycemia, hypona-
64. 2. Addison’s disease is caused by a deficiency tremia, and hyperkalemia. Salted bouillon and
of adrenal corticosteroids and can result in severe fruit juices provide glucose and sodium to replen-
hypotension and shock because of uncontrolled loss ish these deficits. Diet soda does not contain sugar.
of sodium in the urine and impaired mineralocor- Water could cause further sodium dilution. Coffee’s
ticoid function. This results in loss of extracellular diuretic effect would aggravate the fluid deficit. Milk
fluid and dangerously low blood volume. Glucocor- contains potassium and sodium.
ticoids must be administered to reverse hypoten-
CN: Basic care and comfort; CL: Apply
sion. Preventing infection is not an appropriate goal
of care in this life-threatening situation. Relieving 69. 2. Finding alternative methods of deal-
anxiety is appropriate when the client’s condition is ing with stress, such as relaxation techniques, is a
stabilized, but the calm, competent demeanor of cornerstone of stress management. Removing all
the emergency department staff will be initially sources of stress from one’s life is not possible. Anti-
reassuring. anxiety drugs are prescribed for temporary manage-
ment during periods of major stress, and they are
CN: Physiological adaptation;
not an intervention in stress management classes.
CL: Synthesize
Avoiding discussion of stressful situations will not
65. 2. Adrenal hormone deficiency can cause necessarily reduce stress.
profound physiologic changes. The client may
CN: Psychosocial adaptation;
experience severe pain (headache, abdominal pain,
CL: Synthesize
back pain, or pain in the extremities). Inhibited
gluconeogenesis commonly produces hypoglycemia, 70. 3. Primary Addison’s disease refers to a prob-
and impaired sodium retention causes decreased, lem in the gland itself that results from idiopathic
not increased, fluid volume. Edema would not be atrophy of the glands. The process is believed to be
expected. Gastrointestinal disturbances, including autoimmune in nature. The most common causes of
nausea and vomiting, are expected findings in Addi- primary adrenocortical insufficiency are autoimmune
son’s disease, not hunger. destruction (70%) and tuberculosis (20%). Insuf-
ficient secretion of GH causes dwarfism or growth
CN: Physiological adaptation;
delay. Hyposecretion of glucocorticoids, aldosterone,
CL: Analyze
and androgens occur with Addison’s disease. Pitu-
66. 1. Signs of infiltration include slowing of the itary dysfunction can cause Addison’s disease, but
infusion and swelling, pain, hardness, pallor, and this is not a primary disease process. Oversecretion of
coolness of the skin at the site. If these signs occur, the adrenal medulla causes pheochromocytoma.
the I.V. line should be discontinued and restarted at
CN: Physiological adaptation; CL: Apply
another infusion site. The new anatomic site, time,
and type of cannula used should be documented. 71. 2, 3, 4, 5, 6. Addison’s disease occurs when
The nurse may apply a warm soak to the site, but the client does not produce enough steroids from
only after the I.V. line is discontinued. Parenteral the adrenal cortex. Lifetime steroid replacement is
administration of fluids should not be stopped needed. The client should be taught lifestyle man-
intermittently. Stopping the flow does not treat the agement techniques to avoid stress and maintain rest
problem, nor does it address the client’s needs for periods. A medical identification bracelet should
fluid replacement. Infiltrated I.V. sites should not be worn and the family should be taught signs
be irrigated; doing so will only cause more swelling and symptoms that indicate an impending adrenal
and pain. crisis, such as fatigue, weakness, dizziness, or mood
changes. Dental work, infections, and surgery com-
CN: Pharmacological and parenteral
monly require an adjusted dosage of steroids.
therapies; CL: Synthesize
CN: Physiological adaptation; CL: Create
Billings_Part 2_Chap 3_Test 08.indd 495 8/7/2010 10:17:12 AM
496 The Nursing Care of Adults with Medical and Surgical Health Problems
72. 3. Although many of the disease signs and instructing the client to take the medication with a
symptoms are vague and nonspecific, most clients full glass of water will not help prevent gastric com-
experience lethargy and depression as early symp- plications from steroids. Steroids should never be
toms. Other early signs and symptoms include mood taken on an empty stomach. Glucocorticoids should
changes, emotional lability, irritability, weight loss, be taken in the morning, not at bedtime.
muscle weakness, fatigue, nausea, and vomiting. CN: Pharmacological and parenteral
Most clients experience a loss of appetite. Muscles therapies; CL: Apply
become weak, not spastic, because of adrenocortical
insufficiency. 77. 4. Measuring daily weight is a reliable, objec-
tive way to monitor fluid balance. Rapid variations
CN: Physiological adaptation; in weight reflect changes in fluid volume, which
CL: Analyze suggests insufficient control of the disease and the
73. 3. Decreased hepatic gluconeogenesis and need for more glucocorticoids in the client with
increased tissue glucose uptake cause hypoglycemia Addison’s disease. Nurses should instruct clients
in clients with Addison’s disease. Hyperkalemia and taking oral steroids to weigh themselves daily and
hyponatremia are characteristic of Addison’s dis- to report any unusual weight loss or gain. Skin
ease. There is decreased renal perfusion and excre- turgor testing does supply information about fluid
tion of waste products, which causes an elevated status, but daily weight monitoring is more reliable.
BUN level. Temperature is not a direct measurement of fluid
balance. Thirst is a nonspecific and very late sign of
CN: Reduction of risk potential; weight loss.
CL: Analyze
CN: Pharmacological and parenteral
74. 1. The need for glucocorticoids changes therapies; CL: Evaluate
with circumstances. The basal dose is established
when the client is discharged, but this dose covers 78. 3. Rapid weight gain, because it reflects
only normal daily needs and does not provide for excess fluids, is a warning sign that the client is
additional stressors. As the manager of the medica- receiving too much hormone replacement. It may
tion schedule, the client needs to know signs and be difficult to individualize the correct dosage for
symptoms of excessive and insufficient dosages. a client taking glucocorticoids, and the therapeutic
Glucocorticoid needs fluctuate. Glucocorticoids are range between underdosage and overdosage is nar-
not cumulative and must be taken daily. They must row. Maintaining the client on the lowest dose that
never be discontinued suddenly; in the absence of provides satisfactory clinical response is always
endogenous production, addisonian crisis could the goal of pharmacotherapeutics. Fluid balance is
result. Two-thirds of the daily dose should be taken an important indicator of the adequacy of hormone
at about 8 a.m. and the remainder at about 4 p.m. replacement. Anorexia is not present with gluco-
This schedule approximates the diurnal pattern of corticoid therapy because these drugs increase the
normal secretion, with highest levels between 4 a.m. appetite. Dizziness is not specific to the effects of
and 6 a.m. and lowest levels in the evening. glucocorticoid therapy. Poor skin turgor is a late sign
of fluid volume deficit.
CN: Pharmacological and parenteral
therapies; CL: Evaluate CN: Pharmacological and parenteral
therapies; CL: Evaluate
75. 3. Fludrocortisone acetate (Florinef Acetate)
can be administered once a day, but cortisone 79. 1. Medication compliance is an essential part
acetate (Cortone) administration should follow the of the self-care required to manage Addison’s dis-
body’s natural diurnal pattern of secretion. Greater ease. The client must learn to adjust the glucocorti-
amounts of cortisol are secreted during the day to coid dose in response to the normal and unexpected
meet increased demand of the body. Typically, base- stresses of daily living. The nurse should instruct
line administration of cortisone acetate is 25 mg in the client never to stop taking the drug without con-
the morning and 12.5 mg in the afternoon. Taking it sulting the health care provider to avoid an addiso-
three times a day would result in an excessive dose. nian crisis. Regularity in daily habits makes adjust-
Taking the drug only in the morning would not meet ment easier, but the client should not be encouraged
the needs of the body later in the day and evening. to withdraw from normal activities to avoid stress.
The client does not need to restrict sodium. The
CN: Pharmacological and parenteral client is at risk for hyponatremia. Hypotension, not
therapies; CL: Apply hypertension, is more common with Addison’s
76. 4. Oral steroids can cause gastric irritation disease.
and ulcers and should be administered with meals, CN: Reduction of risk potential;
if possible, or otherwise with an antacid. Only CL: Evaluate
Billings_Part 2_Chap 3_Test 08.indd 496 8/7/2010 10:17:13 AM
The Client with Endocrine Health Problems 497
80. 3. Illness or surgery places tremendous stress by a tumor, overstimulation from the pituitary, or the
on the body, necessitating increased glucocorticoid use of prescription steroid drugs. Androgens are also
dosage. Extreme emotional or psychological stress secreted in excess. ACTH is only one hormone that
also necessitates dosage adjustment. Increased dos- is abnormal in Cushing’s disease. Excessive secretion
ages are needed in times of stress to prevent drug- of catecholamines accompanies pheochromocytoma,
induced adrenal insufficiency. Returning to work a disease of the adrenal medulla.
after the weekend, going on a vacation, or having a CN: Physiological adaptation; CL: Apply
routine checkup usually will not alter glucocorti-
coid dosage needs. 85. 2. Sodium retention is typically accompanied
by potassium depletion. Hypertension, hypokalemia,
CN: Reduction of risk potential; edema, and heart failure may result from the hyper-
CL: Synthesize secretion of aldosterone. The client with Cushing’s
81. 4. Bronzing, or general deepening of skin pig- disease exhibits postprandial or persistent hyperg-
mentation, is a classic sign of Addison’s disease and lycemia. Clients with Cushing’s disease have hyper-
is caused by melanocyte-stimulating hormone pro- natremia, not hyponatremia. Bone resorption of
duced in response to increased ACTH secretion. The calcium increases the urine calcium level.
hyperpigmentation is typically found in the distal CN: Reduction of risk potential;
portion of extremities and in areas exposed to sun. CL: Analyze
Additionally, areas that may not be exposed to sun,
such as the nipples, genitalia, tongue, and knuck- 86. 3. Cushing’s disease is commonly caused by
les, become bronze-colored. Treatment of Addison’s loss of the diurnal cortisol secretion pattern. The cli-
disease usually reverses the hyperpigmentation. ent’s random morning cortisol level may be within
Bilirubin level is not related to the pathophysiol- normal limits, but secretion continues at that level
ogy of Addison’s disease. Hyperpigmentation is not throughout the entire day. Cortisol levels should
related to the effects of the glucocorticoid therapy. normally decrease after the morning peak. Analysis
of a 24-hour urine specimen is often useful in iden-
CN: Physiological adaptation; CL: Apply tifying the cumulative excess. Clients will not have
symptoms with normal cortisol levels. Hormones
are present in the blood.
The Client with Cushing’s Disease
CN: Reduction of risk potential;
CL: Apply
82. 3. Skin bruising from increased skin and
blood vessel fragility is a classic sign of Cushing’s 87. 2. A primary dietary intervention is to restrict
disease. Hyperpigmentation and bruising are caused sodium, thereby reducing fluid retention. Increased
by the hypersecretion of glucocorticoids. Fluid protein catabolism results in loss of muscle mass
retention causes hypertension, not hypotension. and necessitates supplemental protein intake. The
Muscle wasting occurs in the extremities. Hair on client may be asked to restrict total calories to
the head thins, while body hair increases. reduce weight. The client should be encouraged to
eat potassium-rich foods because serum levels are
CN: Physiological adaptation;
typically depleted. Although reducing fat intake as
CL: Analyze
part of an overall plan to restrict calories is appro-
83. 2. In Cushing’s disease, excessive cortisol priate, fat intake of less than 20% of total calories is
secretion causes rapid protein catabolism, depleting not recommended.
the collagen support of the skin. The skin becomes
CN: Basic care and comfort;
thin and fragile and susceptible to easy bruising.
CL: Synthesize
The typical “cushingoid” appearance of the cli-
ent includes a moon face, buffalo hump, central 88. 2. Osteoporosis is a serious outcome of pro-
obesity, and thin musculature. Weight gain, mood longed cortisol excess because calcium is resorbed
swings, and slow wound healing are other signs and out of the bone. Regular daily weight-bearing
symptoms of Cushing’s disease. Hypertension, not exercise (e.g., brisk walking) is an effective way to
hypotension, is a sign of Cushing’s disease. Abdomi- drive calcium back into the bones. The client should
nal pain is not a symptom of Cushing’s disease. also be instructed to have a dietary or supplemen-
tal intake of calcium of 1,500 mg daily. Potassium
CN: Physiological adaptation;
levels are not relevant to prevention of bone resorp-
CL: Analyze
tion. Vitamin D is needed to aid in the absorption of
84. 3. Excessive levels of glucocorticoids, aldos- calcium. Isometric exercises condition muscle tone
terone, and androgens secreted from the adrenal cor- but do not build bones.
tex result in the constellation of symptoms known as
CN: Reduction of risk potential;
Cushing’s disease. Cushing’s disease can be caused
CL: Synthesize
Billings_Part 2_Chap 3_Test 08.indd 497 8/7/2010 10:17:14 AM
498 The Nursing Care of Adults with Medical and Surgical Health Problems
89. 2. Effective splinting for a high incision includes turning the client and having the client
reduces stress on the incision line, decreases pain, cough and deep-breathe every 1 to 2 hours, or more
and increases the client’s ability to deep-breathe frequently as ordered. The client will have post-
effectively. Deep breathing should be done hourly operative I.V. fluid replacement ordered to prevent
by the client after surgery. Sitting upright ignores dehydration. Wound infections typically appear 4 to
the need to splint the incision to prevent pain. 7 days after surgery. Urinary tract infections would
Tightening the stomach muscles is not an effective not be typical with this surgery.
strategy for promoting deep breathing. Raising CN: Physiological adaptation;
the shoulders is not a feature of deep-breathing CL: Analyze
exercises.
94. 3. Pain control should be evaluated at least
CN: Physiological adaptation; CL: Apply every 2 hours for the client with a PCA system.
90. 3. The priority in the first 24 hours after Addiction is not a common problem for the postop-
adrenalectomy is to identify and prevent adrenal erative client. A client should not be encouraged to
crisis. Monitoring of vital signs is the most impor- tolerate pain; in fact, other nursing actions besides
tant evaluation measure. Hypotension, tachycardia, PCA should be implemented to enhance the action
orthostatic hypotension, and arrhythmias can be of opioids. One of the purposes of PCA is for the
indicators of pending vascular collapse and hypo- client to determine frequency of administering the
volemic shock that can occur with adrenal crisis. medication; the nurse should not interfere unless
Beginning oral nutrition is important, but not the client is not obtaining pain relief. The nurse
necessarily in the first 24 hours after surgery, and should ensure that the client is instructed on the
it is not more important than preventing adrenal use of the PCA control button and that the button is
crisis. Promoting self-care activities is not as impor- always within reach.
tant as preventing adrenal crisis. Ambulating in the CN: Pharmacological and parenteral
hallway is not a priority in the first 24 hours after therapies; CL: Synthesize
adrenalectomy.
95. 4. Alternately flexing and relaxing the
CN: Physiological adaptation; quadriceps femoris muscles helps prepare the cli-
CL: Synthesize ent for ambulation. This exercise helps maintain
91. 3. Hydromorphone hydrochloride (Dilau- the strength in the quadriceps, which is the major
did) is about five times more potent than morphine muscle group used when walking. The other exer-
sulfate, from which it is prepared. Therefore, it is cises listed do not increase a client’s readiness for
administered only in small doses. Hydromorphone walking.
hydrochloride can cause dependency in any dose; CN: Basic care and comfort;
however, fear of dependency developing in the CL: Synthesize
postoperative period is unwarranted. The dose
is determined by the client’s need for pain relief. 96. 1. Decreased mobility is one of the most
Hydromorphone hydrochloride is not irritating to common causes of abdominal distention related to
subcutaneous tissues. As with opioid analgesics, retained gas in the intestines. Peristalsis has been
excretion depends on normal liver function. inhibited by the general anesthesia, analgesics,
and inactivity during the immediate postoperative
CN: Pharmacological and parenteral period. Ambulation increases peristaltic activity and
therapies; CL: Apply helps move gas. Walking can prevent the need for
92. 1. Ketoconazole (Nizoral) suppresses adrenal a rectal tube, which is a more invasive procedure.
steroid secretion and may cause acute hypoadren- An NG tube is also a more invasive procedure and
alism. The adverse effect should reverse when the requires a physician’s order. It is not a preferred
drug is discontinued. Ketoconazole does not destroy treatment for gas postoperatively. Walking should
adrenal cells; mitotane (Lysodren) destroys the cells prevent the need for further interventions. Carbon-
and may be used to obtain a medical adrenalectomy. ated liquids can increase gas formation.
Ketoconazole decreases, not increases, ACTH- CN: Reduction of risk potential;
induced serum corticosteroid levels. It increases the CL: Synthesize
duration of adrenal suppression when given with
steroids. 97. 2. Persistent cortisol excess undermines
the collagen matrix of the skin, impairing wound
CN: Pharmacological and parenteral healing. It also carries an increased risk of infection
therapies; CL: Apply and of bleeding. The wound should be observed
93. 2. Poor lung expansion from bed rest, pain, and documentation performed regarding the status
and retained anesthesia is a common cause of slight of healing. Confusion and emboli are not expected
postoperative temperature elevation. Nursing care complications after adrenalectomy. Malnutrition
Billings_Part 2_Chap 3_Test 08.indd 498 8/7/2010 10:17:15 AM
The Client with Endocrine Health Problems 499
also is not an expected complication after adrenalec- 102. 1. As the ovarian follicle ceases to produce
tomy. Nutritional status should be regained postop- estrogen, menopause occurs. The endocrine changes
eratively. that occur in menopause due to cessation of the
CN: Reduction of risk potential; ovarian follicle include hot flashes, headaches, and
CL: Analyze mood changes with irritability and anxiety.
98. 2. As the body readjusts to normal cortisol CN: Physiological adaptation;
levels, mood and physical changes will gradually CL: Apply
return to a normal state. The body changes are not 103. 2. Unopposed estrogen in a woman with an
permanent, and the mood swings should level off. intact uterus can cause overgrowth of the endome-
CN: Physiological adaptation; trium, or endometrial hyperplasia. This hyperplasia
CL: Synthesize can be a precursor to endometrial cancer. Estrogen
is effective in the control of hot flashes. If libido is
99. 3. Testosterone is an androgen hormone that is a major problem, testosterone is usually deficient.
responsible for protein metabolism as well as mainte- Hormone replacement therapy (HRT) is not known
nance of secondary sexual characteristics; therefore, to be related to the incidence of ovarian cancer but
it is needed by both males and females. Removal it is considered a risk factor for breast cancer. HRT
of both adrenal glands necessitates replacement of should be used at the lowest dosage for the shortest
glucocorticoids and androgens. Testosterone does period of time to control hot flashes.
not balance the reproductive cycle, stabilize mood
swings, or restore sodium and potassium balance. CN: Pharmacological and parenteral
therapies; CL: Apply
CN: Physiological adaptation; CL: Apply
104. 3. A woman with severe hot flashes is a can-
100. 1. Bilateral adrenalectomy requires lifelong didate for HRT for a short time in the lowest dos-
adrenal hormone replacement therapy. If unilateral age possible. A family or personal history of breast
surgery is performed, most clients gradually rees- cancer or a history of estrogen-dependent dysplasia
tablish a normal secretion pattern. The client and is an absolute contraindication for HRT.
family will require extensive teaching and support
to maintain self-care management at home. Informa- CN: Pharmacological and parenteral
tion on dosing, adverse effects, what to do if a dose therapies; CL: Apply
is missed, and follow-up examinations is needed 105. 2. Endometrial or uterine cancer is a potential
in the teaching plan. Although steroids are tapered complication for postmenopausal women on HRT.
when given for an intermittent or one-time problem, Unfortunately, no signs or symptoms except irregu-
they are not discontinued when given to clients who lar vaginal bleeding are evident in endometrial or
have undergone bilateral adrenalectomy because uterine cancer. A menopausal or postmenopausal
the clients will not regain the ability to manufacture woman with irregular bleeding requires a biopsy to
steroids. Steroids must be taken on a daily basis, not rule out endometrial or uterine cancer. Hot flashes
just during periods of physical or emotional stress. may occur but are not a danger sign. Vaginal dry-
CN: Physiological adaptation; ness, a common complaint during menopause, can
CL: Synthesize be treated with vaginal lubricants. However, this
condition is not life-threatening. Changes in vaginal
pH may occur but need not be reported.
The Female Client with CN: Reduction of risk potential;
Perimenopausal or CL: Analyze
Menopausal Syndrome
101. 2. Deficiency of estrogen causes the major The Client with Pheochromocytoma
characteristics of perimenopause and menopause.
As estrogen decreases, many physiologic changes 106. 3. Pheochromocytomas release cate-
occur with perimenopause. Although many of the cholamines, both epinephrine and norepinephrine.
changes occur in the female reproductive system, The excessive hormone secretion can be constant
other organs and systems are affected as well. or episodic, producing constant or episodic severe
Progesterone is the hormone responsible for main- hypertension. The pheochromocytoma does not
taining pregnancy. Prolactin is one of the hormones cause release of renin, aldosterone, or glucocorti-
responsible for lactation. Oxytocin is secreted by the coids.
posterior pituitary and is responsible for labor. CN: Physiological adaptation;
CN: Physiological adaptation; CL: Apply CL: Apply
Billings_Part 2_Chap 3_Test 08.indd 499 8/7/2010 10:17:16 AM
500 The Nursing Care of Adults with Medical and Surgical Health Problems
107. 3. The release of catecholamines, epinephrine Managing Care Quality and Safety
and norepinephrine, causes hypertension that is
resistant to treatment. Although pheochromocytoma 111. 2. Insulin is on the list of error-prone medi-
accounts for fewer than 1% of the cases of hyperten- cations and the nurse should ask the physician to
sion, it is important to diagnose so the client may be rewrite the order to spell out the word “units” and
correctly treated. The hypertension occurs with both to indicate the route the drug is to be administered.
systolic and diastolic pressures, and the pressures The nurse should contact the physician immedi-
may be very labile. Widening pulse pressure is not ately as the nurse is to administer the insulin now.
related to pheochromocytoma. The nurse can then also report the most current
glucose level. While waiting for the insulin order
CN: Reduction of risk potential;
to be rewritten, the nurse can administer the pain
CL: Apply
medication if needed, start the oxygen, and check
108. 4. Postoperative management is directed at the client’s vital signs.
maintaining a normal blood pressure because the
CN: Safety and infection control;
client may be hypertensive immediately after sur-
CL: Synthesize
gery. The nurse must monitor blood pressure fre-
quently and report abnormalities. Clients in hyper- 112. 3. The client needs fluid volume replacement
tensive crisis should be in an intensive care unit for due to the dehydration. However, the nurse should
cardiac, blood pressure, and neurologic monitor- verify the order for I.V. dextrose with the physi-
ing. Orthostatic hypotension may be a concern for cian due to the risk of hyperglycemia that dextrose
clients on prolonged bed rest or with fluid deficits. would present when administered to a client with
Although hemorrhage may accompany surgery, it is diabetes. The potassium level is within normal
unlikely with this surgery. Elevated blood glucose limits. The client does not have restrictions on oral
concentrations, not hypoglycemia, occur with pheo- fluids and the nurse can encourage the client to
chromocytoma. drink fluids. The client does not need to be placed
in isolation at this time.
CN: Reduction of risk potential;
CL: Analyze CN: Management of care; CL: Synthesize
109. 2. Bending, lifting, and the Valsalva maneu- 113. 3. Glulisine (Apidra) is a rapid-acting insulin
ver can precipitate hypertensive crises or parox- with an action onset of 15 minutes. The client could
ysms. These activities increase transabdominal experience hypoglycemia with the insulin in the
pressure and may cause cardiac-stimulating bloodstream and no breakfast. It is not necessary to
effects. The blood pressure is very labile with these call the client’s physician; the nurse should determine
activities, and paroxysms may be accompanied by what test was scheduled and then locate the client and
tachycardia, palpitations, angina, or electrocardio- provide either breakfast or 4 oz of fruit juice. To bring
graphic changes. Jogging, anxiety, and hypogly- the client back to the room would be wasting valuable
cemia are not triggers for hypertensive crises or time needed to prevent or correct hypoglycemia.
paroxysms.
CN: Management of care; CL: Synthesize
CN: Management of care; CL: Synthesize
114. 3. Because subcutaneous administration of
110. 3. A beta blocker such as propranolol insulin has a slower rate of absorption than I.V.
(Inderal) is administered to block the cardiac-stim- insulin, there must be an adequate level of insulin
ulating effects of epinephrine. ACE inhibitors and in the bloodstream before discontinuing the insulin
calcium channel blockers do not block sympathetic drip; otherwise, the glucose level will rise. Adding
activity as beta blockers do. Diuretics decrease fluid an I.V. antibiotic has no influence on the insulin drip;
volume and peripheral resistance, but they do not it should not be piggy-backed into the insulin drip.
block sympathetic activity. Glargine (Lantus) cannot be administered I.V., and
should not be mixed with other insulins or solutions.
CN: Pharmacological and parenteral
therapies; CL: Apply CN: Management of care; CL: Synthesize
Billings_Part 2_Chap 3_Test 08.indd 500 8/7/2010 10:17:17 AM
You might also like
- Set 1 PDFDocument62 pagesSet 1 PDFAlyssa MontimorNo ratings yet
- Set 1Document62 pagesSet 1Alyssa MontimorNo ratings yet
- Endocrine System - AnswersDocument6 pagesEndocrine System - AnswersF6imNo ratings yet
- Intravenous Therapy in Clinical PracticeDocument8 pagesIntravenous Therapy in Clinical PracticeTyron Rigor Silos100% (1)
- Cardio QuizDocument100 pagesCardio QuizEvidence ChaibvaNo ratings yet
- 2 PDFDocument25 pages2 PDFDianne NuñalNo ratings yet
- FnE MCQsDocument11 pagesFnE MCQsGladys YaresNo ratings yet
- SCENARIO: at 8:30am, Mrs. Cercan Come in at The Unit With Her Husband. They Are Bringing The ReferralDocument3 pagesSCENARIO: at 8:30am, Mrs. Cercan Come in at The Unit With Her Husband. They Are Bringing The ReferralDinarkram Rabreca EculNo ratings yet
- ATI Comprehensive PredictorDocument34 pagesATI Comprehensive Predictorsimo.oukoNo ratings yet
- Diabetes, DKA, HHNS NCLEX REVIEWDocument10 pagesDiabetes, DKA, HHNS NCLEX REVIEWMonica JubaneNo ratings yet
- Answers, Rationales, and Test Taking Strategies: The Nursing Care of Adults With Medical and Surgical Health ProblemsDocument18 pagesAnswers, Rationales, and Test Taking Strategies: The Nursing Care of Adults With Medical and Surgical Health ProblemsNursyNurseNo ratings yet
- Ms DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesDocument9 pagesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesLariza LopegaNo ratings yet
- Neuro Senses Onco OrthoDocument11 pagesNeuro Senses Onco OrthoNom NomNo ratings yet
- Preboard 5Document11 pagesPreboard 5Jona BartzNo ratings yet
- Multiple Clients With Adrenal Gland Disorders 1Document3 pagesMultiple Clients With Adrenal Gland Disorders 1Chermona DanielNo ratings yet
- Endocrine Nclex QuestionsDocument9 pagesEndocrine Nclex QuestionsTiffany Fain Noles100% (1)
- CompositionDocument12 pagesCompositionMustafa KhudhairNo ratings yet
- Should Be Available at All Sites If Feasible, Include at Sites (Not Required)Document5 pagesShould Be Available at All Sites If Feasible, Include at Sites (Not Required)Ahmed QlhamdNo ratings yet
- Pharmacology Test 1: Questions and RationalesDocument52 pagesPharmacology Test 1: Questions and RationalesElla ReyesNo ratings yet
- Diabetes Exam With AnswersDocument12 pagesDiabetes Exam With AnswersJed TumaliwanNo ratings yet
- Pharm Exam1Document17 pagesPharm Exam1Jill Putman Beistline75% (4)
- Nclex Sata 1 Coagulation: Activity Intolerance Increased Impaired Gas Exchange DecreasedDocument14 pagesNclex Sata 1 Coagulation: Activity Intolerance Increased Impaired Gas Exchange DecreasedElizabella Henrietta Tanaquil100% (1)
- PharmDocument16 pagesPharmEi SetteNo ratings yet
- Nclex Sata 1 5Document14 pagesNclex Sata 1 5Elizabella Henrietta TanaquilNo ratings yet
- Compilation P2 MS2 PDFDocument31 pagesCompilation P2 MS2 PDFGwenn SalazarNo ratings yet
- Pharma RenalDocument8 pagesPharma Renalmarlou agananNo ratings yet
- Cardio QuizDocument7 pagesCardio Quizemac186983% (6)
- 1 PDFDocument8 pages1 PDFDianne NuñalNo ratings yet
- NCLEX Final CoachingDocument11 pagesNCLEX Final CoachingmonmonNo ratings yet
- Pharm Quiz 1Document59 pagesPharm Quiz 1Anonymous vXOM1Wxt100% (1)
- NCLEX Question C AnswersDocument14 pagesNCLEX Question C AnswersDavis WhiteNo ratings yet
- Do All of The AboveDocument16 pagesDo All of The AboveMeazaNo ratings yet
- Peptic UlcerDocument53 pagesPeptic UlcerHoney Lyn AlebioNo ratings yet
- Exam Cardio 1Document12 pagesExam Cardio 1Anonymous iG0DCOfNo ratings yet
- Hesi Exit Exam RN 2017 2018 Most Recent UpdatedDocument38 pagesHesi Exit Exam RN 2017 2018 Most Recent Updatedbhangglassilyihpok100% (12)
- Page - 1Document21 pagesPage - 1AnnizaNo ratings yet
- 5 TH Key PointDocument12 pages5 TH Key PointDr-Sanjay SinghaniaNo ratings yet
- Nursing Care Plan 2Document6 pagesNursing Care Plan 2ayanori_boyNo ratings yet
- Reviewer in 2nd Sem NursingDocument17 pagesReviewer in 2nd Sem NursingAnne Joyce Lara AlbiosNo ratings yet
- MS QuestionsDocument53 pagesMS QuestionsHoney Lyn AlebioNo ratings yet
- NCLEX Review Cardiovascular QuizDocument17 pagesNCLEX Review Cardiovascular Quizdany tesemaNo ratings yet
- 4) CORRECT - Primary Goal Is To Protect Spine From Strain and Further Damage While InjuryDocument41 pages4) CORRECT - Primary Goal Is To Protect Spine From Strain and Further Damage While InjuryJujuNo ratings yet
- Nclex Practice Exam Part1Document20 pagesNclex Practice Exam Part1stuffednurse40% (5)
- PN Comprehensive Practice A Anad B Questions and Answers VerifiedDocument8 pagesPN Comprehensive Practice A Anad B Questions and Answers Verifiedianshirow834No ratings yet
- 4Document4 pages4Abdul Hamid NoorNo ratings yet
- Dialysis ReviewerDocument16 pagesDialysis ReviewerlarraNo ratings yet
- Lippincott's PEDIATRIC7 ANSWERSDocument11 pagesLippincott's PEDIATRIC7 ANSWERSNursyNurseNo ratings yet
- MS5-107 27Document59 pagesMS5-107 27Gil Raphael GanibanNo ratings yet
- Answers, Rationales, and Test Taking Strategies: Managing Care Quality and SafetyDocument16 pagesAnswers, Rationales, and Test Taking Strategies: Managing Care Quality and SafetyNursyNurseNo ratings yet
- Beq 6TH RotationDocument6 pagesBeq 6TH RotationMariezen FernandoNo ratings yet
- NCLEX Review Cardiovascular QuizDocument17 pagesNCLEX Review Cardiovascular QuizApple Mesina100% (2)
- 200 MS33 RbeDocument9 pages200 MS33 RbeJade HemmingsNo ratings yet
- CardiovascularDocument46 pagesCardiovascularHamza NejibNo ratings yet
- Nursing Care Plan 2Document6 pagesNursing Care Plan 2KM TopacioNo ratings yet
- Finals ReviewerDocument3 pagesFinals ReviewerMary Ann SacramentoNo ratings yet
- Mosbys Comprehensive Review of Nursing For The NCLEX RN ExaminationDocument46 pagesMosbys Comprehensive Review of Nursing For The NCLEX RN ExaminationDarren VargasNo ratings yet
- Chapter 9 (Margot-Desevo)Document11 pagesChapter 9 (Margot-Desevo)Jesse ParkNo ratings yet
- CH 32Document8 pagesCH 32Elizabeth PetersenNo ratings yet
- FabsDocument7 pagesFabsRJ CarmzNo ratings yet
- Nursing Care Plan #1 Mental HealthDocument13 pagesNursing Care Plan #1 Mental HealthNursyNurseNo ratings yet
- Mental Status Assessment#2Document5 pagesMental Status Assessment#2NursyNurseNo ratings yet
- Online Connect Verbatim Report (Sample)Document5 pagesOnline Connect Verbatim Report (Sample)NursyNurseNo ratings yet
- 3 Communicable Diseases NotesDocument3 pages3 Communicable Diseases NotesNursyNurseNo ratings yet
- Verbatim 1Document10 pagesVerbatim 1NursyNurseNo ratings yet
- Dosage Titration PresentationDocument17 pagesDosage Titration PresentationNursyNurseNo ratings yet
- 3 Chapter 29 Practice Questions CardioDocument17 pages3 Chapter 29 Practice Questions CardioNursyNurseNo ratings yet
- Dosage Calculation Review Part 3 - Flow Rate CalculationsDocument3 pagesDosage Calculation Review Part 3 - Flow Rate CalculationsNursyNurseNo ratings yet
- Dosage Calculation Review Part 1 - ConversionsDocument4 pagesDosage Calculation Review Part 1 - ConversionsNursyNurseNo ratings yet
- Skin Pediatric NotesDocument8 pagesSkin Pediatric NotesNursyNurseNo ratings yet
- Dosage Calculation Review Part 2 - Medication DosagesDocument2 pagesDosage Calculation Review Part 2 - Medication DosagesNursyNurseNo ratings yet
- Pedi Math Packet 2016-2017-1Document26 pagesPedi Math Packet 2016-2017-1NursyNurseNo ratings yet
- BNS Exam 4 CH 31 Book Review Questions, Questions Taken From Key Points, and Within Book - Details - Kahoot!Document32 pagesBNS Exam 4 CH 31 Book Review Questions, Questions Taken From Key Points, and Within Book - Details - Kahoot!NursyNurseNo ratings yet
- Procedure Checklist Chapter 38, Skill 38-01: Administering IV Medication Via PRN Lock or IV LineDocument2 pagesProcedure Checklist Chapter 38, Skill 38-01: Administering IV Medication Via PRN Lock or IV LineNursyNurseNo ratings yet
- Antidiuretic Hormone: Manifestations of Dehydration-ElderlyDocument15 pagesAntidiuretic Hormone: Manifestations of Dehydration-ElderlyNursyNurseNo ratings yet
- Dosage by Weight Exercises and AnswersDocument3 pagesDosage by Weight Exercises and AnswersNursyNurseNo ratings yet
- Procedure Checklist Chapter 26, Skill 26-04: Obtaining A Wound CultureDocument1 pageProcedure Checklist Chapter 26, Skill 26-04: Obtaining A Wound CultureNursyNurseNo ratings yet
- Procedure Checklist Chapter 37, Skill 37-01: Reconstituting and Withdrawing Medication From A VialDocument2 pagesProcedure Checklist Chapter 37, Skill 37-01: Reconstituting and Withdrawing Medication From A VialNursyNurseNo ratings yet
- Procedure Checklist Chapter 34, Skill 34-02: Performing VenipunctureDocument3 pagesProcedure Checklist Chapter 34, Skill 34-02: Performing VenipunctureNursyNurseNo ratings yet
- Exam 1 Slides APDocument13 pagesExam 1 Slides APNursyNurseNo ratings yet
- BNS Exam 4 2021 - Details - Kahoot!Document6 pagesBNS Exam 4 2021 - Details - Kahoot!NursyNurseNo ratings yet
- Common Subcutaneous Medications Check Off - Details - Kahoot!Document9 pagesCommon Subcutaneous Medications Check Off - Details - Kahoot!NursyNurseNo ratings yet
- BNS Insulins & Other Meds We Covered - Details - Kahoot!Document22 pagesBNS Insulins & Other Meds We Covered - Details - Kahoot!NursyNurseNo ratings yet
- Important Slides Nutrition ch5Document18 pagesImportant Slides Nutrition ch5NursyNurseNo ratings yet
- DONOR SELECTION (Deferral) - BBDocument5 pagesDONOR SELECTION (Deferral) - BBMaikka IlaganNo ratings yet
- Urinary Incontinence in Elderly: DefinitionDocument13 pagesUrinary Incontinence in Elderly: DefinitionTarek AhmedNo ratings yet
- Nimhans Previous QuestionDocument51 pagesNimhans Previous QuestionravasoNo ratings yet
- Clinodactyly: Christian Dumontier MD, PHD Centre de La Main-Guadeloupe - FwiDocument34 pagesClinodactyly: Christian Dumontier MD, PHD Centre de La Main-Guadeloupe - FwiProfesseur Christian Dumontier0% (1)
- Case PresentationDocument11 pagesCase PresentationHira Rafique100% (1)
- Mike McKendrickDocument61 pagesMike McKendrickVikas AgrawalNo ratings yet
- Differentiatingfamilial Neuropathiesfrom Guillain-Barre SyndromeDocument22 pagesDifferentiatingfamilial Neuropathiesfrom Guillain-Barre SyndromeKartika IwangNo ratings yet
- List of Diseases & Afflictions: Intestinal Parasites (Stalker & Interloper)Document2 pagesList of Diseases & Afflictions: Intestinal Parasites (Stalker & Interloper)Alex Vikingoviejo SchmidtNo ratings yet
- Test Bank For Clinical Laboratory Hematology 2nd Edition MckenzieDocument12 pagesTest Bank For Clinical Laboratory Hematology 2nd Edition Mckenzienoumenalskall0wewNo ratings yet
- Eward SKDRDocument87 pagesEward SKDRBasroni FaizalNo ratings yet
- Basic First Aid NotesDocument9 pagesBasic First Aid NotesPaul SealyNo ratings yet
- Emergency Nursing IntroDocument111 pagesEmergency Nursing IntroteuuuuNo ratings yet
- Neuro Trauma: Nathan Mcsorley Speciality Trainee Neurosurgery 23B Ninewells HospitalDocument35 pagesNeuro Trauma: Nathan Mcsorley Speciality Trainee Neurosurgery 23B Ninewells HospitalnathanNo ratings yet
- Principles of Clinical CytogeneticsDocument34 pagesPrinciples of Clinical CytogeneticsZainab Jamal SiddiquiNo ratings yet
- Fistula Ani Japanese GuidelineDocument7 pagesFistula Ani Japanese GuidelinevivianmtNo ratings yet
- Week 8 Hepato Biliary 2Document94 pagesWeek 8 Hepato Biliary 2طفوف محمد.No ratings yet
- Gambaran Klinis Dan Patologis Pada Ayam Yang Terserang Flu Burung Sangat Patogenik (HPAI) Di Beberapa Peternakan Di Jawa Timur Dan Jawa BaratDocument9 pagesGambaran Klinis Dan Patologis Pada Ayam Yang Terserang Flu Burung Sangat Patogenik (HPAI) Di Beberapa Peternakan Di Jawa Timur Dan Jawa BaratILHAM BAGUS DARMA .NNo ratings yet
- Cardiogenic SyokDocument51 pagesCardiogenic SyokRamadhyanNo ratings yet
- Dengue Fever (Nepal) An Emerging Public Health Problem.Document13 pagesDengue Fever (Nepal) An Emerging Public Health Problem.Bzay DhitalNo ratings yet
- Public Health COC ExamDocument19 pagesPublic Health COC ExamTut Kong RuachNo ratings yet
- Capgras' Delusion: A Systematic Review of 255 Published CasesDocument13 pagesCapgras' Delusion: A Systematic Review of 255 Published CasesKaren RosasNo ratings yet
- Review: Arthritis in LeprosyDocument6 pagesReview: Arthritis in LeprosyadlestariNo ratings yet
- FNCP - Inadequate Exercise & Breeding Site For MosquitoesDocument2 pagesFNCP - Inadequate Exercise & Breeding Site For MosquitoesGwyneth Fisher100% (1)
- Female Genital Tract Cytopathology: PracticalDocument26 pagesFemale Genital Tract Cytopathology: PracticalNgotelo FunwiNo ratings yet
- Removing Gallstones From Your Body: Recommended PracticeDocument1 pageRemoving Gallstones From Your Body: Recommended PracticeRyok DaysNo ratings yet
- Aortic Regurgitation PathophysiologyDocument1 pageAortic Regurgitation Pathophysiologydana100% (1)
- Pandemic vs. NeurodivergenceDocument5 pagesPandemic vs. NeurodivergenceEuan PasamonteNo ratings yet
- 4 - Clinical Patterns in Crohn's Disease - A Statistical Study of 615 CasesDocument9 pages4 - Clinical Patterns in Crohn's Disease - A Statistical Study of 615 CasesVân NguyễnNo ratings yet
- Notes by Dr. Khurram PDFDocument22 pagesNotes by Dr. Khurram PDFAdnan AsgharNo ratings yet
- DR - Thompsons CBC-RBC Indices Guide - A Guide To Red Blood Cell IndicesDocument54 pagesDR - Thompsons CBC-RBC Indices Guide - A Guide To Red Blood Cell IndicesYohana SetiawanNo ratings yet
- Peak: The New Science of Athletic Performance That is Revolutionizing SportsFrom EverandPeak: The New Science of Athletic Performance That is Revolutionizing SportsRating: 5 out of 5 stars5/5 (97)
- Relentless: From Good to Great to UnstoppableFrom EverandRelentless: From Good to Great to UnstoppableRating: 5 out of 5 stars5/5 (788)
- Chair Yoga: Sit, Stretch, and Strengthen Your Way to a Happier, Healthier YouFrom EverandChair Yoga: Sit, Stretch, and Strengthen Your Way to a Happier, Healthier YouRating: 3.5 out of 5 stars3.5/5 (5)
- Strong Is the New Beautiful: Embrace Your Natural Beauty, Eat Clean, and Harness Your PowerFrom EverandStrong Is the New Beautiful: Embrace Your Natural Beauty, Eat Clean, and Harness Your PowerRating: 4 out of 5 stars4/5 (5)
- Aging Backwards: Reverse the Aging Process and Look 10 Years Younger in 30 Minutes a DayFrom EverandAging Backwards: Reverse the Aging Process and Look 10 Years Younger in 30 Minutes a DayNo ratings yet
- Pranayama: The Yoga Science of BreathingFrom EverandPranayama: The Yoga Science of BreathingRating: 4.5 out of 5 stars4.5/5 (8)
- Functional Training and Beyond: Building the Ultimate Superfunctional Body and MindFrom EverandFunctional Training and Beyond: Building the Ultimate Superfunctional Body and MindRating: 4.5 out of 5 stars4.5/5 (1)
- Endure: Mind, Body, and the Curiously Elastic Limits of Human PerformanceFrom EverandEndure: Mind, Body, and the Curiously Elastic Limits of Human PerformanceRating: 4.5 out of 5 stars4.5/5 (237)
- The Total Kettlebell Workout: Trade Secrets of a Personal TrainerFrom EverandThe Total Kettlebell Workout: Trade Secrets of a Personal TrainerRating: 5 out of 5 stars5/5 (1)
- Power of 10: The Once-A-Week Slow Motion Fitness RevolutionFrom EverandPower of 10: The Once-A-Week Slow Motion Fitness RevolutionRating: 3.5 out of 5 stars3.5/5 (11)
- The Yogi Code: Seven Universal Laws of Infinite SuccessFrom EverandThe Yogi Code: Seven Universal Laws of Infinite SuccessRating: 4.5 out of 5 stars4.5/5 (104)
- True Yoga: Practicing With the Yoga Sutras for Happiness & Spiritual FulfillmentFrom EverandTrue Yoga: Practicing With the Yoga Sutras for Happiness & Spiritual FulfillmentRating: 4.5 out of 5 stars4.5/5 (22)
- The Power of Fastercise: Using the New Science of Signaling Exercise to Get Surprisingly Fit in Just a Few Minutes a DayFrom EverandThe Power of Fastercise: Using the New Science of Signaling Exercise to Get Surprisingly Fit in Just a Few Minutes a DayRating: 4 out of 5 stars4/5 (4)
- Muscle for Life: Get Lean, Strong, and Healthy at Any Age!From EverandMuscle for Life: Get Lean, Strong, and Healthy at Any Age!Rating: 4.5 out of 5 stars4.5/5 (22)
- Boundless: Upgrade Your Brain, Optimize Your Body & Defy AgingFrom EverandBoundless: Upgrade Your Brain, Optimize Your Body & Defy AgingRating: 4.5 out of 5 stars4.5/5 (67)
- Strength Training Over 40: The Only Weight Training Workout Book You Will Need to Maintain or Build Your Strength, Muscle Mass, Energy, Overall Fitness and Stay Healthy Without Living in the GymFrom EverandStrength Training Over 40: The Only Weight Training Workout Book You Will Need to Maintain or Build Your Strength, Muscle Mass, Energy, Overall Fitness and Stay Healthy Without Living in the GymRating: 4 out of 5 stars4/5 (6)
- Mind Your Body: 4 Weeks to a Leaner, Healthier LifeFrom EverandMind Your Body: 4 Weeks to a Leaner, Healthier LifeRating: 4.5 out of 5 stars4.5/5 (5)
- Enter The Kettlebell!: Strength Secret of the Soviet SupermenFrom EverandEnter The Kettlebell!: Strength Secret of the Soviet SupermenRating: 4 out of 5 stars4/5 (29)
- Easy Strength: How to Get a Lot Stronger Than Your Competition-And Dominate in Your SportFrom EverandEasy Strength: How to Get a Lot Stronger Than Your Competition-And Dominate in Your SportRating: 4.5 out of 5 stars4.5/5 (17)
- Tibetan Yoga: Magical Movements of Body, Breath, and MindFrom EverandTibetan Yoga: Magical Movements of Body, Breath, and MindRating: 5 out of 5 stars5/5 (1)
- Not a Diet Book: Take Control. Gain Confidence. Change Your Life.From EverandNot a Diet Book: Take Control. Gain Confidence. Change Your Life.Rating: 4.5 out of 5 stars4.5/5 (124)
- Fascia: A Comprehensive Guide to Fascia Stretch Training (Explain the Effects on the Body Due to the Connection)From EverandFascia: A Comprehensive Guide to Fascia Stretch Training (Explain the Effects on the Body Due to the Connection)No ratings yet
- Roxane Gay & Everand Originals: Built for This: The Quiet Strength of PowerliftingFrom EverandRoxane Gay & Everand Originals: Built for This: The Quiet Strength of PowerliftingRating: 4.5 out of 5 stars4.5/5 (133)
- Calisthenics: Guide for Bodyweight Exercise, Build your Dream Body in 30 MinutesFrom EverandCalisthenics: Guide for Bodyweight Exercise, Build your Dream Body in 30 MinutesRating: 3 out of 5 stars3/5 (5)
- Wheels of Life: A User's Guide to the Chakra SystemFrom EverandWheels of Life: A User's Guide to the Chakra SystemRating: 4.5 out of 5 stars4.5/5 (34)
- Yamas & Niyamas: Exploring Yoga's Ethical PracticeFrom EverandYamas & Niyamas: Exploring Yoga's Ethical PracticeRating: 4.5 out of 5 stars4.5/5 (111)
- The Science of Getting Ripped: Proven Diet Hacks and Workout Tricks to Burn Fat and Build Muscle in Half the TimeFrom EverandThe Science of Getting Ripped: Proven Diet Hacks and Workout Tricks to Burn Fat and Build Muscle in Half the TimeRating: 4 out of 5 stars4/5 (8)