Professional Documents
Culture Documents
Gastrointestinal Bleeding
Gastrointestinal Bleeding
Uploaded by
Mike GCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Gastrointestinal Bleeding
Gastrointestinal Bleeding
Uploaded by
Mike GCopyright:
Available Formats
Gastrointestinal Bleeding
1- Immediate management of life
life-threatening Bleeding
Recognize Risk Factors for Severe Initial Stabilization Procedures
Gastrointestinal Bleeding :
As with any emergency ABCs first.
Signs, symptoms, or history that may indicate
ongoing hemorrhage are as follows: AIRWAY MANAGEMENT
1- If the patient is having ongoing hematemesis Endotracheal
ndotracheal intubation.
1- Profuse hematemesis or hematochezia 2- If immediat
immediate airway control is not needed oxygen to maintain saturation > 93%
2- Hypotension,
otension, tachycardia, or signs of
BREATHING :
shock . 1- Assess breathing ( See Ahmados papers )
3- Postural
ostural hypotension, tachycardia, or 2- Pulse oxymetery,
lightheadedness CIRCULATION :
4- Possible aortoenteric fistula 1-Assess circulation ( See Ahmados papers )
(history of abdominal aortic aneurysm repair 2-Apply monitor.
or palpable pulsating abdominal mass) 3-Obtain IV access : Insert two large-bore IV (18 gauge or larger)
• BEGIN FLUID RESUSCITATION:
RESUSCIT
5- Previous history of GI bleeding
- Either
Either lactated Ringer's or normal saline to restore intravascular volume.
6- Known or suspected varices • ASSESS THE NEED FOR IMMEDIATE BLOOD TRANSFUSION
1- For persistent hypotension despite the infusion of 2 L of crystalloid
crystalloid :
7- History of diverticulosis - Immediate
I transfusion of cross-matched
matched blood if available.
- If not, then transfuse O-negative
O blood until cross-matched
matched blood is available.
Continue transfusion to maintain systolic blood pressure at > 90 mm Hg.
2- If a patient's hematocrit < 30% + history of ischemic heart disease, consider
early transfusion.
3- Obtain an electrocardiogram (ECG) for any patient :
- Older
O than 50 years;
- With
W a history of ischemic heart disease
- With Significant
S anemia;
- any patient with chest pain, shortness of breath,
breath, or severe hypotension.
If the initial ECG shows ongoing ischemia in the face of ongoing GI bleeding,
then consider immediate transfusion of packed red blood cells.
PERFORM LABORATORY STUDIES,
S Send blood for :
1- Complete Blood Count.
C
2- Determine site of bleeding 2- Type and crossmatch blood.
Once the patient is stabilized, attempt to determine the bleeding site if it is not already obvious. 3- Measure prothrombin & partial thromboplastin time to assess for any coagulopathy.
• In 90% of pa-ents presen-ng with GI hemorrhage, the bleeding has an upper GI source (i.e., proximal to the ligament of Treitz);
Trei 4- Measure serum electrolytes
• n only about 10% of pa-ents is the source of bleeding distal to this proximal por-on of the duodenum
In 5- Renal & Liver
L functions. Blood urea nitrogen is elevated in many with upper GI bleeding.
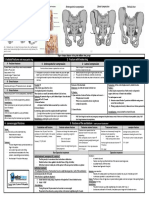
Diagnostic Characteristics of Upper Gastrointestinal Bleeding (Figure 14-2) Diagnostic Characteristics of Lower Gastrointestinal Bleeding (Figure 14-3) 6- Venous blood gas & lactate may be helpful in assessing tissue perfusion status.
PHYSICAL EXAMINATION
1- General examination : general appearance & mental status;
2- Cardiac examination
3- Pulmonary examination
4- Abdominal
bdominal examination (including noting surgical scars, distention, auscultation
auscultatio
for bruits that may indicate an aneurysm, palpating organ size); skin changes such
as pallor, moisture, telangiectasia, ecchymoses, and petechiae.
5- Rectal examination for hemorrhoids or fissures
6- Stool
tool examination for occult blood are essential.
PERFORM BLADDER CATHETERIZATION
1- If a patient is in shock insert a Foley catheter to monitor urinary output.
2- Order a urine analysis to assess for hematuria, indicate an abdominal aneurysm.
After resuscitation
NASOGASTRIC TUBE LAVAGE
LAV :
If hematemesis
emesis has not been documented :
N
Nasogastric tube lavage with normal saline until aspirate is clear.
• Persistent bleeding during lavage indicates life-threatening
life threatening upper GI bleeding,
and immediate consultation with a gastroenterologist or surgeon for :
HEMATEMESIS HEMATOCHEZIA Emergent Endoscopy
Hematemesis (excluding hemoptysis or swallowed blood from epistaxis
epistaxis) is observed during • An upper GI source is found for suspected lower GI bleeding in up to 15% of pa-ents
upper gastrointestinal bleeding. Lavage prior to endoscopy may improve visualization during endoscopic procedure
presenting with hematochezia.
• Blood or material in the nasogastric lavage tests positive for blood.
• The aspirate will be negative in about 10% of pa-ents with duodenal source of GI hemorr.
In these instances, consider : CORRECT COAGULOPATHY
1- Aortoenteric
ortoenteric fistula (in patients with abdominal aortic aneurysm repair) or - Patients taking Coumadin or those who show signs of hepatic failure (e.g.,
A duodenal source cannot be excluded unless gastric lavage contents reveal bile.
2- Duodenal ulcer. jaundice) may require :
Even if bile is returned, the bleeding may have resolved spontaneously prior to arrival.
• If a patient reports unwitnessed hematemesis and gastric lavage is inconclusive • Otherwise, Bleeding
leeding distal to the ligament of Treitz is associated with hematochezia. 1- Vitamin K
MELENA 2- Fresh frozen plasma
consultation
nsultation with a gastroenterologist for early endoscopy is warranted.
to correct coagulopathy before bleeding can be controlled.
• Melena is rarely associated with lower GI bleeding EXCEPT when motility in the intestinal
MELENA AND HEMATOCHEZIA
tract is decreased. Admission in ICU or Disposition
• Melena is usually due to bleeding from an upper GI source.
BRIGHT RED BLOOD
• Hematochezia from an upper source usually indicates severe hemorrhage and Intensive care unit admission should be reserved for patients with :
• Bright red blood usually indicates : 1- Continued bleeding
corresponds with significant increases in mortality, need for :
1- Hemorrhoidal or 2- Abnormal vital signs
1- Transfusion 2- Complications 33- Need for surgery.
2- Anal fissure source of bleeding. 3- Significant comorbid disease
ABSENCE OF BLEEDING ABSENCE OF BLEEDING 4- Need for transfusion therapy
• If nasogastric lavage reveals bile and no blood
blood, then active bleeding from an upper GI • Spontaneous cessa-on of bleeding occurs in about 80
80–85% of cases without intervention 5- Those at increased risk for re-bleeding
bleeding (i.e., esophageal varices).
source is less likely. although cessation can be intermittent, and bleeding can restart at any time.
3-
3 Further evaluation of gastrointestinal bleeding
Once the patient's hemodynamic status has stabilized, a more thorough examination should be done.
History
Inquire about history of GI bleeding :
• Esophageal varices,, alcohol or nonsteroidal anti inflammatory drug (NSAID) use, oral anticoagulation, recent weight loss, change in caliber of stools, abdominal pain suggesti
anti-inflammatory ve of ulcer or gastritis, liver disease, or abdominal surgery.
suggestive
• Inquire about history of hemorrhoids
hemorrhoids,, anal fissures, or rectal trauma (e.g., rectal intercourse, placement of foreign objects in rectum)
Physical Examination
VITAL SIGNS CARDIOPULMONARY EXAM EXAMINATION ABDOMINAL EXAMINATIO
EXAMINATION RECTAL EXAMINATION
Evaluate the patient for : • Epigastric tenderness : common with gastritis or peptic ulcer disease. • Obtain a stool sample for hemoccult testing,
Reassess vitals signs every 15 min. • Evidence of cardiac dysfunction • A patient whose complaints of abdominal pain are out of proportion to the examination and who also has • Check for evidence of :
(i.e., murmurs, rubs, gallops, melena should be considered at risk for mesenteric ischemia
ischemia. - hemorrhoids or
arrhythmias). • Significant tenderness or peritoneal signs
sig may indicate perforation - anal fissures.
• Lungs for abnormal sounds • Examine the patient for signs of chronic liver disease : indicate esophageal varices.
suggestive of - heart failure or (hepatosplenomegaly, ascites, enlarged
ed abdominal vessels, jaundice
jaundice,, asterixis, palmar erythema).
- infectious process. • Inspect the patient for surgical scars indicate previous abdominal surgery or vascular repair.
Special Examinations
UPPER GASTROINTESTIN
GASTROINTESTINAL BLEEDING LOWER GASTROINTESTINAL
AL BLEEDING
Endoscopy: ( Diagnostic & Therapeutic ) Colonoscopy: ( Diagnostic & Therapeutic )
• If the patient is actively bleeding, endoscopy should be performed as soon as • Modality
odality of choice for diagnos
diagnosis + therapeutic intervention.
possible.
Anoscopy/Proctosigmoidoscopy
• If the patient is stable and has no active bleeding, can performed within 24
• Examination of the rectum & distal sigmoid colon should be undertaken as soon as the patient has been stabilized.
hours.
Barium Enema
Angiography • This radiographic study is not commonly used as a diagnostic study for lower GI bleeding BECAUSE: It interferes
interfere not with
• Angiography is used in only about 1% of pa-ents with upper GI bleeding. endoscopic visualization & visceral angiography.
• It may be useful if endoscopy cannot identify a bleeding source even when Mesenteric Angiography
active bleeding is suspected. • If the bleeding rate is es-mated to be greater than 0.5
0.5–1
1 mL/min, angiography allows for selec-ve emboliza-on or
vasopressin infusion.
Technetium Red Cell Scintigraphy
• Techne-um bleeding scans may be indicated if the bleeding rate is greater than 0.1 mL/min.
• A portion of the patient's red blood cells are labeled with technetium
technetium-99m
99m and reinfused, followed by scanning.
Monitoring for Rebleeding
GASTRIC LAVAGE
• After placement of a nasogastric tube, continue reassessment for rebleeding by using intermittent low continuous suction.
• Continued bleeding or rebleeding is an indication for emergent endoscopy.
STOOL
• Record frequency, color, and approximate amount of stool passed by the patient.
• Continued passage of bright red, maroon, or melenic stools may indicate need for further studies or transfusion.
HEMOGLOBIN AND HEMATOCRIT
• Frequent checking of hemoglobin
oglobin and hematocrit (every 4 hours) iss essen-al
essen- in pa-ents with ac-ve bleeding a?er th
they are hemodynamically stabilized.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5819)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Lesson Plan On DVTDocument18 pagesLesson Plan On DVTAlma Susan100% (1)
- SYCDW 2011 Coag Made EasyDocument17 pagesSYCDW 2011 Coag Made EasyRose KasidiNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Hem Lab Microhematocrit F15Document10 pagesHem Lab Microhematocrit F15Joan Christie WijayaNo ratings yet
- Capillary Puncture Equipment and ProcedureDocument3 pagesCapillary Puncture Equipment and ProcedureSieg100% (1)
- Fractures of FemurDocument1 pageFractures of FemurYogi drNo ratings yet
- Fractures of FemurDocument1 pageFractures of FemurYogi drNo ratings yet
- Maternal and Neonatal Outcomes of Pregnant Women With COVID-19 Pneumonia: A Case-Control StudyDocument20 pagesMaternal and Neonatal Outcomes of Pregnant Women With COVID-19 Pneumonia: A Case-Control StudyYogi drNo ratings yet
- Pathology of Fructure & OsteoprosisDocument3 pagesPathology of Fructure & OsteoprosisYogi drNo ratings yet
- Pathology of OsteoarthritisDocument2 pagesPathology of OsteoarthritisYogi drNo ratings yet
- Nonsteroidal Anti-Inflamatory DrugsDocument4 pagesNonsteroidal Anti-Inflamatory DrugsYogi drNo ratings yet
- Neuromuscular Blocking DrugsDocument3 pagesNeuromuscular Blocking DrugsYogi drNo ratings yet
- Muscles of The Gluteal RegionDocument2 pagesMuscles of The Gluteal RegionYogi drNo ratings yet
- Comments, Opinions, and Reviews: Vascular Syndromes of The ThalamusDocument15 pagesComments, Opinions, and Reviews: Vascular Syndromes of The ThalamusYogi drNo ratings yet
- Abdominal Wall Defects: Omphalocele and Gastroschisis: DR - Enono Yhoshu Department of Pediatric SurgeryDocument42 pagesAbdominal Wall Defects: Omphalocele and Gastroschisis: DR - Enono Yhoshu Department of Pediatric SurgeryYogi drNo ratings yet
- Fracturte of Pelvis PDFDocument2 pagesFracturte of Pelvis PDFYogi drNo ratings yet
- Cardiac Arrest PDFDocument4 pagesCardiac Arrest PDFYogi drNo ratings yet
- Surgical Anatomy-Anal Canal: Dr. Belal MansoorDocument79 pagesSurgical Anatomy-Anal Canal: Dr. Belal MansoorYogi drNo ratings yet
- Abdominal Wall Defects: Omphalocele GastroschisisDocument20 pagesAbdominal Wall Defects: Omphalocele GastroschisisYogi drNo ratings yet
- Human Kidney Is A Target For Novel Severe Acute Respiratory Syndrome Coronavirus 2 (Sars-Cov-2) InfectionDocument16 pagesHuman Kidney Is A Target For Novel Severe Acute Respiratory Syndrome Coronavirus 2 (Sars-Cov-2) InfectionYogi drNo ratings yet
- Sexually Transmitted Diseases 1Document3 pagesSexually Transmitted Diseases 1Yogi drNo ratings yet
- Axonal Degeneration: Nerve RegenerationDocument1 pageAxonal Degeneration: Nerve RegenerationYogi drNo ratings yet
- Gender Differences in Patients With COVID-19: Focus On Severity and MortalityDocument18 pagesGender Differences in Patients With COVID-19: Focus On Severity and MortalityYogi drNo ratings yet
- Medial Longitudinal BundleDocument14 pagesMedial Longitudinal BundleYogi drNo ratings yet
- Imaging in Acute Abdomen: Dr. Wan Najwa Zaini Wan Mohamed Radiologist, Hospital Queen Elizabeth IiDocument70 pagesImaging in Acute Abdomen: Dr. Wan Najwa Zaini Wan Mohamed Radiologist, Hospital Queen Elizabeth IiYogi drNo ratings yet
- Skull CommunicationDocument56 pagesSkull CommunicationYogi drNo ratings yet
- Vitamin B12 Deficiency and Anemia in 140 Taiwanese Female Lacto-VegetariansDocument13 pagesVitamin B12 Deficiency and Anemia in 140 Taiwanese Female Lacto-VegetariansLunaNo ratings yet
- Blood Bank List HariyanaDocument22 pagesBlood Bank List HariyanadaniNo ratings yet
- CASE REPORT COMPETITION With Identifying FeaturesDocument12 pagesCASE REPORT COMPETITION With Identifying FeaturesJoel Cesar AtinadoNo ratings yet
- Histology Laboratory Manual: Olgga A. Hara MSDocument77 pagesHistology Laboratory Manual: Olgga A. Hara MSMark LopezNo ratings yet
- Muscular SystemDocument3 pagesMuscular SystemJanica Pauline DaydayNo ratings yet
- Campbell Biology 12e (1) - 921-946Document26 pagesCampbell Biology 12e (1) - 921-946Lâm PhạmNo ratings yet
- Transfusion and Apheresis Science: Ravneet Kaur Bedi, Kshitija Mittal, Tanvi Sood, Rakesh Kumar, Ajay S. PraveenDocument3 pagesTransfusion and Apheresis Science: Ravneet Kaur Bedi, Kshitija Mittal, Tanvi Sood, Rakesh Kumar, Ajay S. PraveenLuis Enrique Tinoco JuradoNo ratings yet
- Epithelial TissueDocument26 pagesEpithelial Tissueaimi BatrisyiaNo ratings yet
- Tissue Level Lab Exercise ModuleDocument14 pagesTissue Level Lab Exercise Modulecasseyareola100% (1)
- MUST To KNOW in Blood Banking 1Document19 pagesMUST To KNOW in Blood Banking 1Aya Virtucio100% (1)
- Haematopathology 3:: Leucocytosis/LeucopeniaDocument113 pagesHaematopathology 3:: Leucocytosis/LeucopeniaarwaNo ratings yet
- Lab Report Ayham FaisalDocument7 pagesLab Report Ayham Faisalayham omariNo ratings yet
- Human Blood GroupsDocument12 pagesHuman Blood GroupsAme Roxan AwidNo ratings yet
- Blood Case 6Document12 pagesBlood Case 6إنعام الحفيانNo ratings yet
- Patient Medical Transcript C++ Mini ProjectDocument9 pagesPatient Medical Transcript C++ Mini ProjectAzmi Bin A MataliNo ratings yet
- Blood DonationDocument19 pagesBlood Donationsundesh4100% (1)
- 3-Differential WBC CountDocument11 pages3-Differential WBC CountdlerNo ratings yet
- Guidelines On The Management of Massive Blood Loss: GuidelineDocument8 pagesGuidelines On The Management of Massive Blood Loss: GuidelineRatna AgustinaNo ratings yet
- XS 1000i English PDFDocument8 pagesXS 1000i English PDFTanveerNo ratings yet
- TissuesDocument9 pagesTissuesAtharv AggarwalNo ratings yet
- Notes: Heparin-Induced Thrombocytopenia (Hit)Document6 pagesNotes: Heparin-Induced Thrombocytopenia (Hit)MOHIT SHARMANo ratings yet
- Physiology of Muscle Tissue: A Marvel of Movement!Document119 pagesPhysiology of Muscle Tissue: A Marvel of Movement!romiNo ratings yet
- Notes - Structural Organisation in AnimalsDocument41 pagesNotes - Structural Organisation in AnimalsAnubhab SilNo ratings yet
- EpitheliumDocument48 pagesEpitheliumdrpankaj28100% (1)
- Chapter8-Transport in HumansDocument15 pagesChapter8-Transport in HumansミーチェルNo ratings yet
- Leunase and TrombolismDocument12 pagesLeunase and TrombolismSanta UlinaNo ratings yet