Professional Documents
Culture Documents
Original Investigation: Importance
Uploaded by
sarahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Original Investigation: Importance
Uploaded by
sarahCopyright:
Available Formats
Research
Original Investigation
Percutaneous Coronary Intervention Outcomes in Patients
With Stable Obstructive Coronary Artery Disease
and Myocardial Ischemia
A Collaborative Meta-analysis of Contemporary
Randomized Clinical Trials
Kathleen Stergiopoulos, MD, PhD; William E. Boden, MD; Pamela Hartigan, PhD; Sven Möbius-Winkler, MD;
Rainer Hambrecht, MD; Whady Hueb, MD, PhD; Regina M. Hardison, MS; J. Dawn Abbott, MD;
David L. Brown, MD
Editor's Note page 231
IMPORTANCE Myocardial ischemia in patients with stable coronary artery disease (CAD) has Related article page 223
been repeatedly associated with impaired survival. However, it is unclear if revascularization
with percutaneous coronary intervention (PCI) to relieve ischemia improves outcomes
compared with medical therapy (MT).
OBJECTIVE The objective of this study was to compare the effect of PCI and MT with MT
alone exclusively in patients with stable CAD and objectively documented myocardial
ischemia on clinical outcomes.
DATA SOURCES MEDLINE, Cochrane, and PubMed databases from 1970 to November 2012.
Unpublished data were obtained from investigators.
STUDY SELECTION Randomized clinical trials of PCI and MT vs MT alone for stable coronary
artery disease in which stents and statins were used in more than 50% of patients.
DATA EXTRACTION For studies in which myocardial ischemia diagnosed by stress testing or
fractional flow reserve was required for enrollment, descriptive and quantitative data were
extracted from the published report. For studies in which myocardial ischemia was not a
requirement for enrollment, authors provided data for only those patients with ischemia
determined by stress testing prior to randomization. The outcomes analyzed included death
from any cause, nonfatal myocardial infarction (MI), unplanned revascularization, and angina.
Summary odds ratios (ORs) were obtained using a random-effects model. Heterogeneity was
assessed using the Q statistic and I2.
RESULTS In 5 trials enrolling 5286 patients, myocardial ischemia was diagnosed in 4064
patients by exercise stress testing, nuclear or echocardiographic stress imaging, or fractional
flow reserve. Follow-up ranged from 231 days to 5 years (median, 5 years). The respective
event rates for PCI with MT vs MT alone for death were 6.5% and 7.3% (OR, 0.90 [95% CI,
0.71-1.16); for nonfatal MI, 9.2% and 7.6% (OR, 1.24 [95% CI, 0.99-1.56]); for unplanned
revascularization, 18.3% and 28.4% (OR, 0.64 [95% CI, 0.35-1.17); and for angina, 20.3% and
23.3% (OR, 0.91 [95% CI, 0.57-1.44]).
CONCLUSIONS AND RELEVANCE In patients with stable CAD and objectively documented
Author Affiliations: Author
myocardial ischemia, PCI with MT was not associated with a reduction in death, nonfatal MI, affiliations are listed at the end of this
unplanned revascularization, or angina compared with MT alone. article.
Corresponding Author: David L.
Brown, MD, Division of
Cardiovascular Medicine, Department
of Medicine, State University of New
York–Stony Brook School of Medicine,
Health Sciences Center T16-080,
JAMA Intern Med. 2014;174(2):232-240. doi:10.1001/jamainternmed.2013.12855 Stony Brook, NY 11794 (david.brown
Published online December 2, 2013. @stonybrookmedicine.edu).
232 jamainternalmedicine.com
Copyright 2014 American Medical Association. All rights reserved.
Downloaded From: http://archinte.jamanetwork.com/ by a Florida Atlantic University User on 05/22/2015
Percutaneous Coronary Intervention Meta-analysis Original Investigation Research
W
orldwide, coronary artery disease (CAD) is the lead- filter for randomized clinical trials was used. Additionally, bib-
ing cause of death and will continue to be at least liographies of retrieved articles and prior reviews on the sub-
through the year 2030.1 Approximately 1 in 30 pa- ject were searched for other relevant studies.
tients with stable CAD experiences cardiovascular death or
myocardial infarction (MI) each year.2 The increasing global Inclusion Criteria
prevalence of CAD3 coupled with these high event rates un- For inclusion, studies were required to be prospective, ran-
derscores the need to identify and intervene in patients at high- domized trials of PCI plus MT vs MT alone in patients with
est risk for these adverse clinical outcomes. Because an ische- stable CAD with the individual outcomes of death and nonfa-
mic response on stress testing identifies an increased risk of tal MI reported. Additionally, to reflect contemporary inter-
death or MI in patients with CAD, the presence of myocardial ventional and medical practice, inclusion required stent im-
ischemia is commonly used to select patients with stable CAD plantation in at least 50% of PCI procedures and statin
for elective coronary revascularization even in the absence of medications in at least 50% of patients in both PCI and MT arms.
limiting symptoms under the assumption that since ische- Finally, myocardial ischemia or abnormal FFR had to be docu-
mia confers adverse risk,4-7 reducing ischemia by revascular- mented in some or all patients prior to randomization. For stud-
ization will reduce risk.8,9 ies in which MT was compared with separate arms of PCI or
More recently, fractional flow reserve (FFR) has emerged coronary artery bypass graft (CABG) surgery,13,14 only the com-
as an invasive technique performed at the time of coronary an- parisons of MT vs PCI were extracted. Studies of stable pa-
giography to detect coronary stenoses of sufficient hemody- tients following a completed MI were excluded as were trials
namic severity to induce myocardial ischemia.8 Fractional flow in which MT was compared with any form of revasculariza-
reserve is defined as the maximal blood flow to the myocar- tion (PCI or CABG).
dium in the presence of a stenosis in the supplying coronary
artery divided by the theoretical normal maximal flow in the Data Extraction
same distribution. This index represents the fraction of the nor- For studies in which all patients had either myocardial ische-
mal maximal myocardial flow that can be achieved despite the mia on stress testing or an abnormal FFR,15,16 patient charac-
coronary stenosis. The normal value of the index is 1.0, re- teristics, study design, and outcomes were systematically
gardless of the patient or the specific vessel studied. The posi- reviewed and recorded independently by 2 of us (K.S. and
tive predictive value of an FFR of less than approximately 0.75 D.L.B.). For studies in which not all patients were required to
for identifying coronary stenoses associated with reversible have ischemia on stress testing,13,14,17 the primary authors
myocardial ischemia is 100%10 and is therefore used to select were contacted and provided data on the subset of patients
lesions for percutaneous coronary intervention (PCI) with the with ischemia at the time of randomization. For a study in
goal of reducing ischemia and improving outcomes.9 which some end points of interest (all-cause mortality,
In support of the strategy of ischemia-guided revascu- angina) were not reported,15 the primary authors were con-
larization, a large observational study of patients in the tacted and provided the data. Study quality was evaluated
1990s suggested that revascularization in patients with evi- according to the criteria of Jadad et al,18 which included
dence of at least moderate ischemia (>10% of the myocar- ascertainment of randomization, blinding of the patient and
dium) was associated with fewer cardiac deaths than treat- investigator to treatment allocation, and an account of the
ment with medical therapy (MT) alone.4 Conversely, 2 post patients who withdrew.
hoc studies of patients enrolled in the Clinical Outcomes
Using Revascularization and Aggressive Drug Evaluation Outcomes
(COURAGE) trial with either mild or moderate to severe The following clinical outcomes were analyzed: death from any
ischemia at baseline failed to demonstrate a reduction in cause, nonfatal MI, unplanned revascularization (PCI or CABG),
death or MI in patients treated with PCI compared with and angina. For each outcome, we used data from the longest
those who received MT.11,12 follow-up available for that particular outcome to a maxi-
Given the equipoise surrounding this issue, we per- mum follow-up of 5 years. End point definitions were those
formed a systematic review and collaborative meta-analysis used in the individual trials. The definition of nonfatal MI var-
of contemporary randomized clinical trials that compared PCI ied and became more precise in the more recent studies. In gen-
and MT with initial MT alone in patients with stable obstruc- eral, the diagnosis of nonfatal MI required appropriate symp-
tive CAD and objectively documented ischemia. toms, biomarker elevation, and/or electrocardiographic
changes. Nonfatal postprocedural MI, when identified, was in-
cluded as a nonfatal MI event. Troponin screening for post-
procedure MI was used in 2 studies.14,17 Unplanned revascu-
Methods larization included any PCI or CABG excluding the PCI
Search Strategy mandated by initial randomization and could occur in partici-
A systematic search of published studies in any language in pants initially assigned to either PCI or MT arms. In each study,
MEDLINE, Cochrane, and PubMed from 1970 to November 2012 revascularization decisions were made by the treating physi-
was performed independently by 2 of us (K.S. and D.L.B.). cian and not mandated by the study protocols. The definition
Search terms included stent, medical therapy, stable angina, of angina was that used in the individual trials and included
coronary artery disease, and combinations of these terms. A recurrent or persistent angina during follow-up.
jamainternalmedicine.com JAMA Internal Medicine February 2014 Volume 174, Number 2 233
Copyright 2014 American Medical Association. All rights reserved.
Downloaded From: http://archinte.jamanetwork.com/ by a Florida Atlantic University User on 05/22/2015
Research Original Investigation Percutaneous Coronary Intervention Meta-analysis
Figure 1. Study Selection
2180 PubMed articles 37 MEDLINE articles 18 Cochrane Library articles
2235 Total articles
108 Articles screened for 2137 Did not meet inclusion criteria based on
more detailed evaluation title and abstract review or were duplicates
45 Full-text articles 40 Full-text articles excluded
assessed for eligibility 17 Studies or substudies including patients
within 1 week of myocardial infarction
13 Studies were substudies or late follow-up
of included studies
5 Studies included in
4 Studies had <50% stent use
qualitative synthesis
1 Study had <50% statin use at baseline
5 Articles were not original research,
defined as editorials and review articles
Flow diagram depicts study selection
for inclusion in the meta-analysis
according to the PRISMA statement
5 Studies included in quantitative synthesis (meta-analysis)
for reporting systematic reviews and
meta-analyses.19
Statistical Analysis erated. The Egger weighted linear regression test was used to
Because individual patient-level data from each trial were not examine the quantitative association between mean effect es-
available, a meta-analysis of summary statistics from indi- timate and its variance.
vidual trials was performed using Comprehensive Meta Analy-
sis software, version 2 (Biostat Inc). Data were analyzed ac-
cording to the intention-to-treat principle. For trials with no
events in either treatment group,15 a nominal amount (0.5
Results
cases) was added to the results for both groups. The presence Literature Search
of statistically significant heterogeneity was assessed by the The electronic search yielded 2235 citations, which were
Q statistic (significant at P < .10), and the extent of any ob- screened by reviewing the title or abstract of each. Of these,
served heterogeneity was determined by I2 (ranging from 0% 108 publications were reviewed in full, and 5 trials were in-
to 100%). The Q statistic failed to indicate statistical hetero- cluded in the meta-analysis according to the PRISMA
geneity for the outcomes of death and nonfatal MI, whereas statement 19 for reporting systematic reviews and meta-
statistical heterogeneity was present for the end points of un- analyses (Figure 1). These were the Medicine, Angioplasty, or
planned revascularization and angina. Since the absence of sta- Surgery Study II (MASS II),13 the trial by Hambrecht et al,15 Clini-
tistical heterogeneity does not guarantee clinical homogene- cal Outcomes Using Revascularization and Aggressive Drug
ity, summary odds ratios (ORs) for all end points were Evaluation (COURAGE),17 Bypass Angioplasty Revasculariza-
calculated with the inverse variance method using a random- tion 2 Diabetes (BARI 2D),14 and the Fractional Flow Reserve
effects model from the ORs and 95% CIs for each end point in vs Angiography for Multivessel Evaluation 2 (FAME 2) 16
each study. The random-effects model provides a more con- (Table 1). The 5 trials enrolled patients between 1997 and 2012
servative summary estimate because it incorporates both from Brazil, North America, and Europe. Funding was de-
within-trial and between-trial variance. P < .05 was consid- rived from government, university, and industry sources. The
ered statistically significant, and all tests were 2-sided unless stress testing techniques used to diagnose ischemia are listed
otherwise indicated. in Table 1. The stress tests were interpreted at the individual
We further assessed potential associations of the treat- clinical sites. From the total enrollment of 5286 patients in these
ment effect with study-level variables in subgroup analyses. studies, 4064 were identified with myocardial ischemia at the
A prespecified subgroup analysis was performed based on the time of randomization on the basis of stress testing or the pres-
requirement of ischemia for study entry vs no requirement for ence of at least 1 hemodynamically significant coronary ste-
ischemia at study entry and for studies that enrolled patients nosis by FFR. Of these, 2016 patients were randomized to PCI
prior to the year 2000 vs enrollment after 2000. Sensitivity and MT, and 2048 were randomized to MT alone. Baseline char-
analyses were performed for each outcome to determine acteristics of the study populations are provided in Table 2. Pa-
whether any single study disproportionately influenced the tients enrolled in the studies were predominantly men. Pa-
pooled estimate by excluding individual trials one at a time and tients with diabetes made up 22% to 100% of the study
recalculating the combined OR for the remaining studies. To populations, and 25% to 40% of all patients had experienced
qualitatively assess publication bias, a funnel plot of the loga- a prior MI. Mean ejection fractions ranged from 57% to 69%.
rithm of effect size vs the standard error for each trial was gen- The extent of CAD ranged from single-vessel to 3-vessel dis-
234 JAMA Internal Medicine February 2014 Volume 174, Number 2 jamainternalmedicine.com
Copyright 2014 American Medical Association. All rights reserved.
Downloaded From: http://archinte.jamanetwork.com/ by a Florida Atlantic University User on 05/22/2015
Percutaneous Coronary Intervention Meta-analysis Original Investigation Research
Table 1. Characteristics of Included Trials
Total
Techniques Participants/
Source, for Detection With
Country Years of of Myocardial Criteria for Diagnosis Ischemia, Follow-up, Funding
or Region Enrollment Inclusion Criteria Exclusion Criteria Ischemia of Ischemia No. y Source
13
MASS II, 1997-2001 Angiographically Refractory angina or Treadmill ECG Clinical (angina) and/or 408/165 5 University
Brazil documented proximal acute MI, ventricular testing ECG (magnitude of and national
multivessel coronary aneurysm, LVEF horizontal or downsloping
stenosis of >70% by <40%, a history of ST-segment depression)
visual assessment and PCI or CABG, and/or scintigraphic
documented ischemia single-vessel disease (severity and extent of
(stress testing or CCS and normal or the perfusion defects)
class) minimal CAD
Left main disease
≥50%
Hambrecht 1997-2001 Stable CAD and 1 Acute coronary syn- Stress ECG Presence of angina 101/101 5 University
et al,15 native coronary artery drome (<2 mo), left and/or 99mTc ST-segment changes and national
Germany stenosis of ≥75% by main >25% or high- scintigraphy ≥1 mm horizontal or
visual assessment by grade proximal LAD, downsloping ST
PCI LVEF <40%, prior PCI depression
CCS Class I-III with or CABG Presence of any perfusion
documented ischemia defect
during stress ECG
and/or SPECT imaging
COURAGE,17 1999-2004 Stable CAD and CCS Persistent CCS class Treadmill Any of >1-mm ST 2287/1938 4.6 Department
North class IV angina IV angina testing, exercise deviation on standard of Veterans
America (medically stabilized) Markedly positive or pharmaco- treadmill exercise ECG; Affairs
At least 70% stenosis stress test logic stress ≥1 scintigraphic perfusion Cooperative
in at least 1 epicardial (substantial imaging (nuclear defect during exercise Studies
coronary artery and ST-segment or echocardio- technetium, 99mTc Program,
objective evidence of depression or graphic imaging) sestamibi, or thallium Canadian
ischemia or at least 1 hypotensive imaging; ≥1 perfusion Institutes of
coronary stenosis of response during defect (reversible or Health
at least 80% and stage 1 of Bruce partial reversible) with Research,
classic angina on protocol) pharmacologic supplemental
provocative testing Refractory heart (dipyridamole, support from
failure or adenosine) stress during industry
99m
cardiogenic shock Tc sestamibi or
LVEF <30%, thallium imaging; ≥1 wall
revascularization in motion abnormality
the prior 6 mo, during exercise
coronary anatomy radionuclide
not suitable for ventriculography or
revascularization 2-dimensional
echocardiography
(exercise or dobutamine)
BARI 2D,14 2001-2005 Type 2 diabetes and Required immediate Treadmill ≥1-mm horizontal ST 1605/972 5 National
North and CAD documented on revascularization, testing, exercise depression or Institutes of
South angiography (≥50% left main disease, or pharmaco- downsloping ST-segment Health,
America, stenosis of a major creatinine >2.0 logic stress depression or elevation additional
Europe epicardial vessel mg/dL, Hgb A1c imaging (nuclear for ≥60-80 milliseconds support from
associated with a >13.0%, class III or or echocardio- after the end of the QRS industry
positive stress test IV heart failure, prior graphic imaging) complex; myocardial
and classic angina) PCI or CABG perfusion defect;
myocardial wall motion
abnormality; decline in
ejection fraction with
stress; Doppler or
pressure wire showing
coronary flow reserve
<2.0 or fractional flow
reserve <0.75
FAME 216 2010-2012 Stable CAD Patients in whom the FFR Pressure wire showing 888/888 0.59 Industry
Europe and considered for PCI preferred treatment fractional flow reserve
North with at least 1 is CABG ≤0.80 during
America functionally Left main coronary adenosine-induced
significant stenosis artery disease hyperemia in at least 1
(FFR≤0.80) Recent (<1 week) MI major coronary artery
Prior CABG
LVEF <30%
Abbreviations: CABG, coronary artery bypass grafting; CAD, coronary artery infarction; PCI, percutaneous coronary intervention; SPECT, single-photon
disease; CCS, Canadian Cardiovascular Society; ECG, electrocardiography; emission computed tomography; 99mTc, technetium 99m.
FFR, fractional flow reserve; Hgb, hemoglobin; LAD, left anterior descending SI conversion: To convert creatinine to micromoles per liter, multiply by 76.25.
coronary artery; LVEF, left ventricular ejection fraction; MI, myocardial
ease. Stents were implanted in 66% to 100% of patients. Drug- hibitors, and statins (Table 2). All studies allowed crossover
eluting stents were used in 37% and 95% of patients in the BARI from MT to PCI for intolerable symptoms at the discretion of
2D14 and FAME 216 studies, respectively. Medical therapy in- the treating physician. The median follow-up duration was 5
cluded aspirin, β-blockers, angiotensin-converting enzyme in- years.
jamainternalmedicine.com JAMA Internal Medicine February 2014 Volume 174, Number 2 235
Copyright 2014 American Medical Association. All rights reserved.
Downloaded From: http://archinte.jamanetwork.com/ by a Florida Atlantic University User on 05/22/2015
Research Original Investigation Percutaneous Coronary Intervention Meta-analysis
Table 2. Characteristics of Patients With Documented Ischemiaa
MASS II13 Hambrecht15 COURAGE17 BARI 2D14 FAME 216
Characteristic MT+PCI MT MT+PCI MT MT+PCI MT MT+PCI MT MT+PCI MT
Participants, No. 68 97 50 51 968 970 483 489 447 441
Age, mean, y 59 59 61 62 62 62 62 62 64 64
Male 62 79 100 100 86 85 73 73 80 77
Diabetes 22 31 22 24 33 35 100 100 28 27
Prior MI 38 33 40 51 35 40 26 25 37 37
Ejection fraction, 69 68 62 64 61 61 57 57 NR NR
mean
Vessels with stenosis 2.35 3.37 1.52 1.6 1.98 2.0 1.55 1.63 1.87 1.73
>50%, mean No.
Stent placed 66 NA 100 NA 94 NA 90 NA 97 NA
Drug-eluting stent 0 NA 0 NA 3 NA 37 NA 95 NA
Medications
Aspirin 100 97 98 98 93 93 97 95 87 90
β-Blocker 85 85 86 88 83 83 92 91 76 78
ACEI or ARB 28 28 88 75 74 73 94 94 69 70
Statin 74 59 80 71 89 90 96 96 83 82
Abbreviations: ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; MI, myocardial infarction; MT, medical therapy; NA, not
applicable; NR, not reported; PCI, percutaneous coronary intervention.
a
Unless otherwise indicated, data are reported as percentage of participants.
Table 3. Quality Metrics of Included Studies
Source Study Blinding Blinding Technique Random Assignment Withdrawal Descriptions
MASS II13 No No Yes Yes
Hambrecht et al15 No No Yes Yes
COURAGE17 No No Yes Yes
BARI-2D14 No No Yes Yes
FAME 216 No No Yes Yes
Table 4. Summary Odds Ratios for Major Outcomes of Percutaneous Coronary Intervention vs Medical Therapy
Heterogeneity
Outcome Odds Ratio (95% CI) P Value Q (I2) P Value
Death 0.90 (0.71-1.16) .42 1.6 (0) .80
Nonfatal MI 1.24 (0.99-1.56) .06 0.52 (0) .97
Unplanned revascularization 0.64 (0.35-1.17) .14 39.2 (90) <.001
Abbreviation: MI, myocardial
Angina 0.91 (0.57-1.44) .67 14.2 (72) .007
infarction.
Study quality as assessed by the Jadad et al18 criteria is sum- PCI compared with initial MT was 1.24 (95% CI, 0.99-1.56; P = .06;
marized in Table 3. None of the trials was blinded. All of the I2 = 0%) (Figure 2B). Unplanned revascularization was per-
studies were randomized and reported on study withdrawals formed in 369 of 2016 PCI patients (18.3%) compared to 583 of
and described the completeness of follow-up. All studies used 2048 medical therapy patients (28.4%). The OR for unplanned
an independent committee to adjudicate end points. revascularization in the PCI vs MT patients was 0.64 (95% CI,
0.35-1.17; P = .14; I2 = 90%) (Figure 2C). Among the patients ran-
Quantitative Outcomes domized to PCI, 410 of 2016 (20.3%) had recurrent or persis-
Table 4 summarizes the effect sizes for the main outcomes of tent angina compared with 478 of 2048 (23.3%) randomized to
the meta-analysis. Of the 281 deaths in the 4064 randomized MT (OR, 0.91; 95% CI, 0.57-1.44; P = .67; I2 = 72%) (Figure 2D).
patients with ischemia, 132 deaths occurred in the 2016 pa-
tients (6.5%) randomized to PCI, whereas 149 deaths occurred Subgroup Analyses
in the 2048 patients (7.3%) randomized to MT. The OR for PCI Subgroup analysis showed that the requirement for ischemia
vs MT for mortality was 0.90 (95% CI, 0.71-1.16; P = .42; I2 = 0%) at study entry15,16 did not make a significant difference for any
(Figure 2A). Nonfatal MI was reported in 187 of 2016 patients of the 4 end points considered. Trials that enrolled patients
(9.2%) in the PCI arms compared with 156 of 2048 patients (7.6%) prior to 200013,15,17 had OR for each end point similar to those
in the MT arms of randomized trials. The OR for nonfatal MI for of trials that enrolled all patients after 2000.14,16
236 JAMA Internal Medicine February 2014 Volume 174, Number 2 jamainternalmedicine.com
Copyright 2014 American Medical Association. All rights reserved.
Downloaded From: http://archinte.jamanetwork.com/ by a Florida Atlantic University User on 05/22/2015
Percutaneous Coronary Intervention Meta-analysis Original Investigation Research
Figure 2. Comparison of Percutaneous Coronary Intervention (PCI) and Medical Therapy (MT) vs Medical Therapy Alone in Patients With
Documented Myocardial Ischemia
A B
Source OR (95% CI) P Value OR (95% CI) Source OR (95% CI) P Value OR (95% CI)
Hambrecht15 1.02 (0.02-52.43) .99 Hambrecht15 3.12 (0.12-78.45) .49
MASS II13 0.76 (0.27-2.16) .60 MASS II13 1.24 (0.40-3.88) .71
COURAGE17 0.84 (0.61-1.18) .32 COURAGE17 1.24 (0.94-1.65) .13
BARI 2D14 1.06 (0.71-1.58) .78 BARI 2D14 1.29 (0.82-2.04) .27
FAME 216 0.33 (0.03-3.16) .33 FAME 216 1.06 (0.51-2.22) .88
Overall 0.90 (0.71-1.16) .42 Overall 1.24 (0.99-1.55) .06
0.01 0.1 1 10 100 0.01 0.1 1 10 100
Favors PCI Favors MT Favors PCI Favors MT
C D
Source OR (95% CI) P Value OR (95% CI) Source OR (95% CI) P Value OR (95% CI)
Hambrecht15 2.60 (0.63-10.71) .18 Hambrecht15 6.82 (0.79-58.85) .08
MASS II13 1.84 (0.91-3.73) .09 MASS II13 3.06 (0.83-11.29) .09
COURAGE17 0.60 (0.48-0.74) <.001 COURAGE17 0.91 (0.74-1.10) .33
BARI 2D14 0.61 (0.46-0.80) <.001 BARI 2D14 0.87 (0.59-1.28) .47
FAME 216 0.13 (0.07-0.24) <.001 FAME 216 0.42 (0.25-0.72) <.001
Overall 0.64 (0.35-1.17) .14 Overall 0.90 (0.57-1.44) .67
0.01 0.1 1 10 100 0.01 0.1 1 10 100
Favors PCI Favors MT Favors PCI Favors MT
Each graph illustrates an outcome. A, Death; B, nonfatal myocardial infarction; and respective 95% CIs. The sizes of the squares denoting the point estimate in
C, unplanned revascularization; and D, angina during follow-up. All included each study are proportional to the weight of the study. The diamonds represent
studies are listed by name along with point estimates of the odds ratios (ORs) the overall findings in each plot.
Sensitivity Analyses and Publication Bias Figure 3. Assessment of Publication Bias
Sensitivity analyses to assess the potential impact of qualita-
tive differences in study design and patient selection showed 0
that exclusion of any single trial from the analysis for mortal-
ity, nonfatal MI, and angina did not alter the overall findings
of the analysis (data not shown). However, removal of MASS
1
II13 data from the unplanned revascularization meta-analysis
Standard Error
resulted in a statistically significant reduction in the OR for re-
vascularization in favor of the PCI group compared with the
MT group (OR, 0.49 [95% CI, 0.26-0.91] (P = .02). The exclu- 2
sion of data from FAME 2,16 which was the only study to ex-
clusively use FFR rather than conventional stress testing, the
only study funded entirely by industry, the study with the
3
shortest follow-up, and the only study that predominantly used
drug-eluting stents, did not change the overall results for any –2.0 –1.5 –1.0 –0.5 0.0 0.5 1.0 1.5 2.0
end point. Log Odds Ratio
The funnel plot was symmetric, suggestive of a lack of pub-
lication bias (Figure 3). The Egger test further supported the This funnel plot is a plot of a measure of study size on the vertical axis as a
function of effect size on the horizontal axis for mortality. Large studies appear
absence of publication bias with a 1-tailed P value of .22.
toward the top of the graph and tend to cluster near the mean effect size.
Smaller studies appear toward the bottom of the graph and (since there is more
sampling variation in effect size estimates in the smaller studies) will be
dispersed across a range of values. In the absence of publication bias, as
Discussion demonstrated in this funnel plot, the studies, represented by pale dotted
circles, are distributed symmetrically about the combined effect size. The
The principal finding of this meta-analysis of randomized clini- dashed diamond appearing below the x-axis represents the summary effect.
cal trials of patients with stable obstructive CAD and myocar-
dial ischemia documented by stress testing or FFR is that a
strategy of initial PCI in combination with MT results in no sig- went treatment with intracoronary stents and disease-
nificant reduction in mortality, nonfatal MI, unplanned revas- modifying secondary prevention therapy. The implications of
cularization, or angina compared with MT alone. These find- these findings are 3-fold. First, the results strongly suggest that
ings are unique in that this is the first meta-analysis to our the relationship between ischemia and mortality is not al-
knowledge limited to patients with documented, objective tered or ameliorated by catheter-based revascularization of ob-
findings of myocardial ischemia, almost all of whom under- structive, flow-limiting coronary stenoses. Second, the lack of
jamainternalmedicine.com JAMA Internal Medicine February 2014 Volume 174, Number 2 237
Copyright 2014 American Medical Association. All rights reserved.
Downloaded From: http://archinte.jamanetwork.com/ by a Florida Atlantic University User on 05/22/2015
Research Original Investigation Percutaneous Coronary Intervention Meta-analysis
clinical benefit from PCI in patients with inducible ischemia The second and more recent study12 enrolled 1381 of the
suggests that the genesis of late clinical events is not neces- 2287 COURAGE patients (60%) who had a baseline stress myo-
sarily a consequence of the ischemic vascular territory sub- cardial perfusion single-photon emission computed tomo-
tending a stenotic coronary segment but rather due to the de- graphic imaging study. Patients were divided into 2 groups—
velopment of new plaque ruptures in distant coronary those with no or mild ischemia and those with moderate to
segments without flow-limiting stenoses. Finally, these find- severe ischemia. Percutaneous coronary intervention was not
ings call into question the common practice of ischemia- associated with a reduction in death or MI compared with MT
guided revascularization (either using noninvasive testing tech- alone in either group, findings that were discordant from the
niques or FFR) where the presence of myocardial ischemia earlier COURAGE substudy.11
routinely determines patient selection for coronary angiogra- Although it remains unclear how myocardial ischemia con-
phy and revascularization. fers increased mortality risk, our results in combination with
The seminal studies of Brown et al20 and Ladenheim et al21 those of prior research suggest that myocardial ischemia may
introduced the concept of stress testing for the assessment of be more of a marker for atherosclerotic burden, with the in-
prognosis in patients with CAD. Since that time, several hun- creased propensity of future events being mediated by the vol-
dred papers have reported on the prognostic value of exercise ume of atherosclerotic plaques at risk of becoming unstable,
treadmill testing,22 stress echocardiography,5-7 myocardial per- rupturing, and inciting thrombosis and MI rather than by pro-
fusion imaging,23-26 and most recently, stress myocardial per- gressive fibroatherosclerotic coronary disease. In support of
fusion with positron emission tomography.27 These studies have this concept, patients with myocardial ischemia have a greater
consistently demonstrated that patients with more extensive atherosclerotic plaque burden as measured by calcium score
and severe ischemia experience increased long-term mortal- than those without ischemia.36 This concept is also consis-
ity or reduced event-free survival compared with patients with- tent with the 25-year-old observation that the vast majority of
out ischemia. The assumption that this ischemia-mortality plaques responsible for acute MI emanate from stenoses of less
association is mediated by an obstructive coronary stenosis has than 70% by angiography prior to the acute event.37 Thus, the
been used to justify coronary angiography and revascular- lesions that are responsible for most cases of MI and subse-
ization26,28-30 in patients with ischemia. quent death are not severe enough to induce ischemia on stress
However, while this ischemia-driven approach to PCI is a cor- testing, and the lesions responsible for causing ischemia do not
nerstone of daily practice in the evaluation of patients with chest tend to rupture. Since intervening on a marker of an outcome
pain or known CAD—endorsed by the American College of Car- that is not in the causal pathway of the subsequent adverse
diology Foundation/American Heart Association and European clinical events would not be expected to reduce those events,
Society of Cardiology guidelines28-30 and reiterated in recent it should not be surprising that prior clinical trials14,17 and
reviews8,31,32—there are scant data supporting it. A single retro- meta-analyses33,38-40 consistently demonstrate that PCI fails
spective observational study of over 10 000 patients who un- to reduce death or MI in patients with stable CAD who are con-
derwent exercise or adenosine myocardial perfusion scintigra- comitantly aggressively treated with contemporary medical
phy from 1991 to 1997 found that revascularization in patients therapy for secondary prevention.
with moderate to large amounts of myocardial ischemia was as- The persistence of angina in over 20% of patients in both
sociated with a reduction in the risk of cardiac death on Cox arms of the present study suggests that, similar to death and
analysis compared with MT alone.4 While the specific compo- MI, this important symptom is not exclusively mediated by
nents of MT were not described in this propensity-matched flow-limiting stenoses. Rather, other pathogenetic mecha-
analysis, MT in the 1990s did not reflect contemporary concepts nisms appear to be involved, including inflammation, endo-
of guideline-directed MT that includes disease-modifying thera- thelial dysfunction, microvascular disease, coronary vaso-
pies such as statins, inhibitors of the renin angiotensin system, spasm, thrombosis, and angiogenesis.41 In most patients,
β-blockers, and thienopyridines.33 Furthermore, observational because MT is systemic treatment, it is better able to address
studies are intrinsically biased by unidentifiable confounders these components than PCI, which is targeted only focally to
that are not completely adjusted for by propensity methods.34 treat a specific stenotic coronary segment.
In contrast, 2 more recent substudies of the COURAGE trial As pointed out by Califf,42 although the ischemia-guided
failed to demonstrate that PCI conferred a reduction in mor- approach to revascularization is conceptually appealing, it has
tality or MI compared with MT in patients with myocardial notable inconsistencies, including the inability to make an
ischemia.11,12 The first study11 analyzed a subset of 314 of the asymptomatic patient feel better, the inability of PCI to pre-
2287 COURAGE patients (13.7%) who had non–protocol- vent MI, and the inevitable complications of PCI, including
mandated serial gated stress perfusion imaging with sesta- death, stroke, MI, and hemorrhage at the access site. The pre-
mibi before and 6 to 18 months after randomization. Percuta- sent study confirms and extends these inconsistencies by dem-
neous coronary intervention was found to be more effective onstrating that not only does PCI not reduce the likelihood of
than MT at reducing moderate to severe ischemia, but while MI, it also offers no durable benefit in terms of reduced mor-
it appeared to reduce death and MI on unadjusted analysis, that tality, need for revascularization, or occurrence of angina in
benefit did not persist after risk adjustment. Despite the lack patients with stable obstructive CAD and myocardial ische-
of clinical benefit associated with PCI in this small substudy, mia. Furthermore, since ischemia does not identify patients
these results have been repeatedly used to justify a strategy who clinically benefit from revascularization, this study calls
of ischemia-based revascularization.8,32,35 into question the use of nuclear stress testing or measure-
238 JAMA Internal Medicine February 2014 Volume 174, Number 2 jamainternalmedicine.com
Copyright 2014 American Medical Association. All rights reserved.
Downloaded From: http://archinte.jamanetwork.com/ by a Florida Atlantic University User on 05/22/2015
Percutaneous Coronary Intervention Meta-analysis Original Investigation Research
ment of FFR in patients with documented CAD but without lim- Third, only the FAME 2 study16 used a predominance of
iting symptoms, as is currently considered appropriate and drug-eluting stents. It is likely that some of the unplanned re-
widely practiced.43 vascularizations in the PCI arms of the other studies were ne-
Our analysis should be interpreted within the context of sev- cessitated by restenosis of a bare metal stent, which might have
eral limitations. First, complete information on the extent and been avoided had a drug-eluting stent been placed originally.
severity of myocardial ischemia was not available for all stud- Fourth, the trials included in this meta-analysis enrolled only
ies, limiting this analysis to patients with any degree of objec- those patients with CAD considered appropriate for revascu-
tively documented ischemia. Although recent data suggest no larization with PCI. Thus, these results do not apply to pa-
benefit of PCI in reducing death or MI in patients with both mild tients with CAD for whom CABG would be the preferred mode
and moderate to severe ischemia,12 this issue will be defini- of revascularization. Finally, data were extracted from only ran-
tively addressed by the International Study of Comparative domized controlled trials and, therefore, may not be repre-
Health Effectiveness with Medical and Invasive Approaches sentative of patients seen in daily practice.
(ISCHEMIA) Trial (www.clinicaltrials.gov Identifier NCT01471522),
funded by the National Heart, Lung, and Blood Institute. This
study of 8000 patients with at least moderate myocardial ische-
mia will compare the effect of MT combined with revasculariza-
Conclusions
tion with that of MT alone on cardiovascular death and MI. For patients with stable obstructive CAD and objective evi-
Second, in COURAGE17 and BARI 2D,14 patients were not dence of myocardial ischemia, a strategy of initial PCI and MT
mandated to undergo stress testing. Thus, it is possible that does not confer benefit in terms of reduction of death, MI, re-
patients who underwent stress testing in those studies are not peat revascularization, or angina compared with MT alone.
representative of the entire study population. However, this These findings underscore existing clinical practice guide-
is unlikely in light of a recent meta-analysis33 that included the lines that recommend an initial approach of contemporary MT
entire COURAGE and BARI 2D cohorts and found results iden- for patients with stable CAD and ischemia rather than pro-
tical to those of the present study. ceeding directly to ischemia-guided PCI.30
ARTICLE INFORMATION Study supervision: Möbius-Winkler, Hambrecht, the duke treadmill score. Circulation.
Accepted for Publication: July 8, 2013. Brown. 2001;103(21):2566-2571.
Published Online: December 2, 2013. Conflict of Interest Disclosures: Dr Möbius-Winkler 8. Pijls NH, Sels JW. Functional measurement of
doi:10.1001/jamainternmed.2013.12855. reports receiving lecture fees from Boston Scientific coronary stenosis. J Am Coll Cardiol.
Germany. Dr Hambrecht reports receiving lecture 2012;59(12):1045-1057.
Author Affiliations: Division of Cardiovascular fees from Berlin Chemie, Merck Sharp and Dohme,
Medicine, Department of Medicine, State 9. Tonino PA, De Bruyne B, Pijls NH, et al; FAME
PohlBoskamp, and Lilly. No other conflicts have been Study Investigators. Fractional flow reserve versus
University of New York–Stony Brook School of reported.
Medicine, Stony Brook (Stergiopoulos, Brown); angiography for guiding percutaneous coronary
Samuel S Stratton VA Medical Center, Albany intervention. N Engl J Med. 2009;360(3):213-224.
REFERENCES
Medical Center, Albany, New York (Boden); VA 10. Pijls NH, De Bruyne B, Peels K, et al.
Cooperative Studies Program Coordinating Center, 1. Mathers CD, Loncar D. Projections of global Measurement of fractional flow reserve to assess
VA Connecticut Healthcare System, West Haven mortality and burden of disease from 2002 to the functional severity of coronary-artery stenoses.
(Hartigan); Universität Leipzig, Leipzig, Germany 2030. PLoS Med. 2006;3(11):e442. N Engl J Med. 1996;334(26):1703-1708.
(Möbius-Winkler); Klinikum, Links der Weser 2. Steg PG, Bhatt DL, Wilson PW, et al; REACH 11. Shaw LJ, Berman DS, Maron DJ, et al; COURAGE
GmbH, Chefarzt Klinik für Kardiologie und Registry Investigators. One-year cardiovascular Investigators. Optimal medical therapy with or
Angiologie, Bremen, Germany (Hambrecht); Heart event rates in outpatients with atherothrombosis. without percutaneous coronary intervention to
Institute of the University of Săo Paolo, Săo Paolo, JAMA. 2007;297(11):1197-1206. reduce ischemic burden: results from the Clinical
Brazil (Hueb); Department of Epidemiology, 3. Tardif J-C. Coronary artery disease in 2010. Eur Outcomes Utilizing Revascularization and
University of Pittsburgh Graduate School of Public Heart J Suppl. 2010;12(suppl C):C2-C10. Aggressive Drug Evaluation (COURAGE) trial
Health, Pittsburgh, Pennsylvania (Hardison); nuclear substudy. Circulation. 2008;117(10):1283-
Warren Alpert Brown University School of 4. Hachamovitch R, Hayes SW, Friedman JD, Cohen
I, Berman DS. Comparison of the short-term 1291.
Medicine, Providence, Rhode Island (Abbott).
survival benefit associated with revascularization 12. Shaw LJ, Weintraub WS, Maron DJ, et al.
Author Contributions: Dr Brown had full access to compared with medical therapy in patients with no Baseline stress myocardial perfusion imaging
all the data in the study and takes responsibility for prior coronary artery disease undergoing stress results and outcomes in patients with stable
the integrity of the data and the accuracy of the myocardial perfusion single photon emission ischemic heart disease randomized to optimal
data analysis. computed tomography. Circulation. medical therapy with or without percutaneous
Study concept and design: Stergiopoulos, Hueb, 2003;107(23):2900-2907. coronary intervention. Am Heart J.
Brown. 2012;164(2):243-250.
Acquisition of data: Stergiopoulos, Boden, Hartigan, 5. Marwick TH, Case C, Poldermans D, et al. A
Möbius-Winkler, Hueb, Hardison, Abbott, Brown. clinical and echocardiographic score for assigning 13. Hueb W, Lopes NH, Gersh BJ, et al. Five-year
Analysis and interpretation of data: Stergiopoulos, risk of major events after dobutamine follow-up of the Medicine, Angioplasty, or Surgery
Boden, Hambrecht, Abbott, Brown. echocardiograms. J Am Coll Cardiol. Study (MASS II): a randomized controlled clinical
Drafting of the manuscript: Stergiopoulos, Brown. 2004;43(11):2102-2107. trial of 3 therapeutic strategies for multivessel
Critical revision of the manuscript for important 6. Marwick TH, Case C, Sawada S, et al. Prediction coronary artery disease. Circulation.
intellectual content: Stergiopoulos, Boden, of mortality using dobutamine echocardiography. 2007;115(9):1082-1089.
Hartigan, Möbius-Winkler, Hambrecht, Hueb, J Am Coll Cardiol. 2001;37(3):754-760. 14. Frye RL, August P, Brooks MM, et al; BARI 2D
Hardison, Abbott, Brown. 7. Marwick TH, Case C, Vasey C, Allen S, Short L, Study Group. A randomized trial of therapies for
Statistical analysis: Stergiopoulos, Boden, Brown. Thomas JD. Prediction of mortality by exercise type 2 diabetes and coronary artery disease. N Engl
Administrative, technical, or material support: Hueb, echocardiography: a strategy for combination with J Med. 2009;360(24):2503-2515.
Hardison, Brown.
jamainternalmedicine.com JAMA Internal Medicine February 2014 Volume 174, Number 2 239
Copyright 2014 American Medical Association. All rights reserved.
Downloaded From: http://archinte.jamanetwork.com/ by a Florida Atlantic University User on 05/22/2015
Research Original Investigation Percutaneous Coronary Intervention Meta-analysis
15. Hambrecht R, Walther C, Möbius-Winkler S, 26. Hachamovitch R, Berman DS, Kiat H, et al. therapy alone for stable coronary artery disease:
et al. Percutaneous coronary angioplasty compared Exercise myocardial perfusion SPECT in patients meta-analysis of randomized controlled trials. Arch
with exercise training in patients with stable without known coronary artery disease: Intern Med. 2012;172(4):312-319.
coronary artery disease: a randomized trial. incremental prognostic value and use in risk 34. Stukel TA, Fisher ES, Wennberg DE. Using
Circulation. 2004;109(11):1371-1378. stratification. Circulation. 1996;93(5):905-914. observational data to estimate treatment effects.
16. De Bruyne B, Pijls NH, Kalesan B, et al; FAME 2 27. Dorbala S, Di Carli MF, Beanlands RS, et al. JAMA. 2007;297(19):2078-2079.
Trial Investigators. Fractional flow reserve-guided Prognostic value of stress myocardial perfusion 35. Fearon WF. Is a myocardial infarction more
PCI versus medical therapy in stable coronary positron emission tomography: results from a likely to result from a mild coronary lesion or an
disease. N Engl J Med. 2012;367(11):991-1001. multicenter observational registry. J Am Coll Cardiol. ischemia-producing one? Circ Cardiovasc Interv.
17. Boden WE, O’Rourke RA, Teo KK, et al; 2013;61(2):176-184. 2011;4(6):539-541.
COURAGE Trial Research Group. Optimal medical 28. Wijns W, Kolh P, Danchin N, et al; Task Force on 36. Schenker MP, Dorbala S, Hong EC, et al.
therapy with or without PCI for stable coronary Myocardial Revascularization of the European Interrelation of coronary calcification, myocardial
disease. N Engl J Med. 2007;356(15):1503-1516. Society of Cardiology (ESC) and the European ischemia, and outcomes in patients with
18. Jadad AR, Moore RA, Carroll D, et al. Assessing Association for Cardio-Thoracic Surgery (EACTS); intermediate likelihood of coronary artery disease:
the quality of reports of randomized clinical trials: European Association for Percutaneous a combined positron emission tomography/
is blinding necessary? Control Clin Trials. Cardiovascular Interventions (EAPCI). Guidelines on computed tomography study. Circulation.
1996;17(1):1-12. myocardial revascularization. Eur Heart J. 2008;117(13):1693-1700.
2010;31(20):2501-2555.
19. Liberati A, Altman DG, Tetzlaff J, et al. The 37. Little WC, Constantinescu M, Applegate RJ,
PRISMA statement for reporting systematic reviews 29. Levine GN, Bates ER, Blankenship JC, et al; et al. Can coronary angiography predict the site of
and meta-analyses of studies that evaluate health American College of Cardiology Foundation; a subsequent myocardial infarction in patients with
care interventions: explanation and elaboration. American Heart Association Task Force on Practice mild-to-moderate coronary artery disease?
Ann Intern Med. 2009;151(4):W65-W94. Guidelines; Society for Cardiovascular Angiography Circulation. 1988;78(5 Pt 1):1157-1166.
and Interventions. 2011 ACCF/AHA/SCAI Guideline
20. Brown KA, Boucher CA, Okada RD, et al. for Percutaneous Coronary Intervention: a report of 38. Pursnani S, Korley F, Gopaul R, et al.
Prognostic value of exercise thallium-201 imaging in the American College of Cardiology Foundation/ Percutaneous coronary intervention versus optimal
patients presenting for evaluation of chest pain. American Heart Association Task Force on Practice medical therapy in stable coronary artery disease: a
J Am Coll Cardiol. 1983;1(4):994-1001. Guidelines and the Society for Cardiovascular systematic review and meta-analysis of randomized
21. Ladenheim ML, Pollock BH, Rozanski A, et al. Angiography and Interventions. J Am Coll Cardiol. clinical trials. Circ Cardiovasc Interv.
Extent and severity of myocardial hypoperfusion as 2011;58(24):e44-e122. 2012;5(4):476-490.
predictors of prognosis in patients with suspected 30. Fihn SD, Gardin JM, Abrams J, et al; American 39. Thomas S, Gokhale R, Boden WE, Devereaux
coronary artery disease. J Am Coll Cardiol. College of Cardiology Foundation; American Heart PJ. A meta-analysis of randomized controlled trials
1986;7(3):464-471. Association Task Force on Practice Guidelines; comparing percutaneous coronary intervention
22. Shaw LJ, Peterson ED, Shaw LK, et al. Use of a American College of Physicians; American with medical therapy in stable angina pectoris. Can
prognostic treadmill score in identifying diagnostic Association for Thoracic Surgery; Preventive J Cardiol. 2012;29(4):472-482.
coronary disease subgroups. Circulation. Cardiovascular Nurses Association; Society for 40. Katritsis DG, Ioannidis JP. Percutaneous
1998;98(16):1622-1630. Cardiovascular Angiography and Interventions; coronary intervention versus conservative therapy in
23. Staniloff HM, Forrester JS, Berman DS, Swan Society of Thoracic Surgeons. 2012 nonacute coronary artery disease: a meta-analysis.
HJ. Prediction of death, myocardial infarction, and ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for Circulation. 2005;111(22):2906-2912.
worsening chest pain using thallium scintigraphy the diagnosis and management of patients with 41. Marzilli M, Merz CN, Boden WE, et al.
and exercise electrocardiography. J Nucl Med. stable ischemic heart disease: a report of the Obstructive coronary atherosclerosis and ischemic
1986;27(12):1842-1848. American College of Cardiology Foundation/ heart disease: an elusive link! J Am Coll Cardiol.
American Heart Association Task Force on Practice 2012;60(11):951-956.
24. Hachamovitch R, Berman DS, Shaw LJ, et al. Guidelines, and the American College of Physicians,
Incremental prognostic value of myocardial American Association for Thoracic Surgery, 42. Califf RM. The trouble with ischemia. Am Heart
perfusion single photon emission computed Preventive Cardiovascular Nurses Association, J. 2012;164(2):133-134.
tomography for the prediction of cardiac death: Society for Cardiovascular Angiography and 43. Hendel RC, Budoff MJ, Cardella JF, et al.
differential stratification for risk of cardiac death Interventions, and Society of Thoracic Surgeons. ACC/AHA/ACR/ASE/ASNC/HRS/NASCI/RSNA/SAIP/
and myocardial infarction. Circulation. J Am Coll Cardiol. 2012;60(24):e44-e164. SCAI/SCCT/SCMR/SIR 2008 key data elements and
1998;97(6):535-543. definitions for cardiac imaging: a report of the
31. Zellweger MJ, Pfisterer ME. Therapeutic
25. Berman DS, Hachamovitch R, Kiat H, et al. strategies in patients with chronic stable coronary American College of Cardiology/American Heart
Incremental value of prognostic testing in patients artery disease. Cardiovasc Ther. 2011;29(6):e23-e30. Association Task Force on Clinical Data Standards
with known or suspected ischemic heart disease: (Writing Committee to Develop Clinical Data
a basis for optimal utilization of exercise 32. Pfisterer ME, Zellweger MJ, Gersh BJ. Standards for Cardiac Imaging). Circulation.
technetium-99m sestamibi myocardial perfusion Management of stable coronary artery disease.
2009;119(1):154-186.
single-photon emission computed tomography. Lancet. 2010;375(9716):763-772.
J Am Coll Cardiol. 1995;26(3):639-647. 33. Stergiopoulos K, Brown DL. Initial coronary
stent implantation with medical therapy vs medical
240 JAMA Internal Medicine February 2014 Volume 174, Number 2 jamainternalmedicine.com
Copyright 2014 American Medical Association. All rights reserved.
Downloaded From: http://archinte.jamanetwork.com/ by a Florida Atlantic University User on 05/22/2015
You might also like
- CourageDocument14 pagesCourageSuryaNo ratings yet
- Initial Invasive or Conservative Strategy For Stable Coronary DiseaseDocument12 pagesInitial Invasive or Conservative Strategy For Stable Coronary DiseaseDrMarcus KeyboardNo ratings yet
- Blush Grade STEMI Meta-Analysis 2022Document6 pagesBlush Grade STEMI Meta-Analysis 2022Ionașcu SimonaNo ratings yet
- New England Journal Medicine: The ofDocument14 pagesNew England Journal Medicine: The ofIMNo ratings yet
- Ischemia CKD Trial - NEJM 2020Document11 pagesIschemia CKD Trial - NEJM 2020Vicken ZeitjianNo ratings yet
- Madit CRTNEJMseot 09Document10 pagesMadit CRTNEJMseot 09binh doNo ratings yet
- 2022 JAMA Diagnosis and Treatment of ACSDocument14 pages2022 JAMA Diagnosis and Treatment of ACSPeter Albeiro Falla Cortes100% (1)
- Castle AfDocument11 pagesCastle AfgustavoNo ratings yet
- Iam 2022Document14 pagesIam 2022Mateo Daniel Gutierrez CastañedaNo ratings yet
- J Jacadv 2022 100120Document14 pagesJ Jacadv 2022 100120Axel Hiram Hernandez PinedaNo ratings yet
- Optimal Medical Therapy vs. Percutaneous Coronary Intervention For Patients With Coronary Chronic Total OcclusionDocument7 pagesOptimal Medical Therapy vs. Percutaneous Coronary Intervention For Patients With Coronary Chronic Total OcclusionsarahNo ratings yet
- Jaha 120 019114Document28 pagesJaha 120 019114Andi Tiara S. AdamNo ratings yet
- PCI or CABG, That Is The Question!: Jong Shin Woo, MD, and Weon Kim, MDDocument2 pagesPCI or CABG, That Is The Question!: Jong Shin Woo, MD, and Weon Kim, MDHeńřÿ ŁøĵæńNo ratings yet
- Manual Aspiration Thrombectomy in Acute Myocardial Infarction: A Clinical ExperienceDocument9 pagesManual Aspiration Thrombectomy in Acute Myocardial Infarction: A Clinical ExperienceArdiana FirdausNo ratings yet
- Ehac 811Document3 pagesEhac 811Rositaka1991No ratings yet
- Catheter Ablationin in AF With CHFDocument11 pagesCatheter Ablationin in AF With CHFKristian Sudana HartantoNo ratings yet
- Nikolsky2007 PDFDocument7 pagesNikolsky2007 PDFPicha PichiNo ratings yet
- Ischemic 19Document8 pagesIschemic 19Adina Alexandra CNo ratings yet
- (19330693 - Journal of Neurosurgery) Decompressive Hemicraniectomy - Predictors of Functional Outcome in Patients With Ischemic StrokeDocument7 pages(19330693 - Journal of Neurosurgery) Decompressive Hemicraniectomy - Predictors of Functional Outcome in Patients With Ischemic StrokeRandy Reina RiveroNo ratings yet
- Stone Et Al 2023 Impact of Complete Revascularization in The Ischemia TrialDocument14 pagesStone Et Al 2023 Impact of Complete Revascularization in The Ischemia TrialKardiologi ManadoNo ratings yet
- Randomized Trial of Primary PCI With or Without Routine Manual ThrombectomyDocument15 pagesRandomized Trial of Primary PCI With or Without Routine Manual ThrombectomyTony Santos'sNo ratings yet
- 1-s2.0-S1071916423003068-mainDocument13 pages1-s2.0-S1071916423003068-mainevelyn.minichNo ratings yet
- Complete Revascularization With Multivessel PCI For Myocardial InfarctionDocument11 pagesComplete Revascularization With Multivessel PCI For Myocardial InfarctionRicardo BarreraNo ratings yet
- Angina/Non-ST-elevation Myocardial Infarction: B-Type Natriuretic Peptide Evaluation of B-Type Natriuretic Peptide For Risk Assessment in UnstableDocument12 pagesAngina/Non-ST-elevation Myocardial Infarction: B-Type Natriuretic Peptide Evaluation of B-Type Natriuretic Peptide For Risk Assessment in Unstablesyaiful rinantoNo ratings yet
- Features of Branch Occlusive Disease-Type Intracranial Atherosclerotic Stroke in Young PatientsDocument7 pagesFeatures of Branch Occlusive Disease-Type Intracranial Atherosclerotic Stroke in Young PatientsrajaririnNo ratings yet
- DudjDocument4 pagesDudjsyaiful rinantoNo ratings yet
- 708 FullDocument8 pages708 FullHidayadNo ratings yet
- 1 Running Head: Preventing Recurrent Myocardial InfarctionsDocument10 pages1 Running Head: Preventing Recurrent Myocardial InfarctionsIsaacNo ratings yet
- Jamacardiology Perera 2023 Oi 230054 1696866153.86277Document8 pagesJamacardiology Perera 2023 Oi 230054 1696866153.86277Omar MedinaNo ratings yet
- Evaluating Stable Chest Pain - An Evolving Approach: EditorialDocument2 pagesEvaluating Stable Chest Pain - An Evolving Approach: EditorialMahmoud AbouelsoudNo ratings yet
- 397 671 1 SMDocument7 pages397 671 1 SMbobirfansyahputraNo ratings yet
- Nej Me 2210183Document2 pagesNej Me 2210183lakshminivas PingaliNo ratings yet
- Original Research Abstract AFCC ASMIHA 2019Document82 pagesOriginal Research Abstract AFCC ASMIHA 2019Program Studi Kardiologi100% (1)
- Acs 33 241Document9 pagesAcs 33 241Ratna AyieNo ratings yet
- Research Article Baseline Serum Uric Acid Levels Are Associated With All-Cause Mortality in Acute Coronary Syndrome Patients After Percutaneous Coronary InterventionDocument9 pagesResearch Article Baseline Serum Uric Acid Levels Are Associated With All-Cause Mortality in Acute Coronary Syndrome Patients After Percutaneous Coronary InterventionmikeNo ratings yet
- Outcomes of Percutaneous Coronary Interventions in Patients With Anemia Presenting With Acute Coronary SyndromeDocument14 pagesOutcomes of Percutaneous Coronary Interventions in Patients With Anemia Presenting With Acute Coronary SyndromesarahNo ratings yet
- Heartfailure FixDocument10 pagesHeartfailure FixdhikaNo ratings yet
- 1 s2.0 S0914508719301765 MainDocument8 pages1 s2.0 S0914508719301765 MainAdriani HartantoNo ratings yet
- A Comparative Study of Platelet Indices in Acute Coronary SyndromeDocument4 pagesA Comparative Study of Platelet Indices in Acute Coronary SyndromeMarcellia AngelinaNo ratings yet
- Identificacion Choque Cardiogenico ERDocument9 pagesIdentificacion Choque Cardiogenico ERZai RojasNo ratings yet
- Ehu 090Document9 pagesEhu 090Tatiana CumbicosNo ratings yet
- Arang Samim - Treatment of Angina and Microvascular Coronary DysfunctionDocument11 pagesArang Samim - Treatment of Angina and Microvascular Coronary DysfunctionM. PurnomoNo ratings yet
- Packer 2019Document14 pagesPacker 2019Renata D GNo ratings yet
- Nejmoa1608029 PDFDocument10 pagesNejmoa1608029 PDFFhirastika AnnishaNo ratings yet
- Bleeding and Ischemic Risks of Ticagrelor Monotherapy After Coronary InterventionsDocument14 pagesBleeding and Ischemic Risks of Ticagrelor Monotherapy After Coronary InterventionsKardiologi ManadoNo ratings yet
- Brain-X - 2023 - Li - Heart Brain Team Approach of Acute Myocardial Infarction Complicating Acute Stroke Evidencing TheDocument2 pagesBrain-X - 2023 - Li - Heart Brain Team Approach of Acute Myocardial Infarction Complicating Acute Stroke Evidencing TheBlackswannnNo ratings yet
- Milri Vs DobutaDocument10 pagesMilri Vs DobutaEliana Lopez BaronNo ratings yet
- Low Diagnostic AngiographyDocument10 pagesLow Diagnostic AngiographyMei Lisa PutriNo ratings yet
- Defibrilator in CardioDocument10 pagesDefibrilator in CardioNabila CpNo ratings yet
- Coronary InterventionDocument27 pagesCoronary InterventionOnon EssayedNo ratings yet
- Acute Coronary Syndromes: Unstable Angina and Non-ST Elevation Myocardial InfarctionDocument18 pagesAcute Coronary Syndromes: Unstable Angina and Non-ST Elevation Myocardial InfarctionLOZANO GARCIA PAOLA ALEJADRANo ratings yet
- Cardiac Mortality in Patients Randomised To Elective Coronary Revascularization Plus Medical Therapy or Medical Therapy Alone - A Systematic Review and Meta-AnalysisDocument14 pagesCardiac Mortality in Patients Randomised To Elective Coronary Revascularization Plus Medical Therapy or Medical Therapy Alone - A Systematic Review and Meta-AnalysisThales FernandesNo ratings yet
- Cartlidge Timothy Role of Percutaneous CoronaryDocument7 pagesCartlidge Timothy Role of Percutaneous Coronarybruno baileyNo ratings yet
- Colchicine in Coronary Artery Disease (NEJM, 2020) PDFDocument10 pagesColchicine in Coronary Artery Disease (NEJM, 2020) PDFthe_leoNo ratings yet
- Chronic Stable Coronary Artery Disease: Drugs vs. RevascularizationDocument16 pagesChronic Stable Coronary Artery Disease: Drugs vs. RevascularizationAndrea OrtizNo ratings yet
- Ijmsv 14 P 1241Document10 pagesIjmsv 14 P 1241Milan PetrikNo ratings yet
- Ing 5Document11 pagesIng 5Farida MufidatiNo ratings yet
- Troponina Guided Coronary ComputedDocument11 pagesTroponina Guided Coronary ComputedafFNo ratings yet
- Clinical Relevance of Acute Cerebral Microinfarcts in Vascular Cognitive ImpairmentDocument10 pagesClinical Relevance of Acute Cerebral Microinfarcts in Vascular Cognitive Impairmentzefri suhendarNo ratings yet
- Imaging in Peripheral Arterial Disease: Clinical and Research ApplicationsFrom EverandImaging in Peripheral Arterial Disease: Clinical and Research ApplicationsNo ratings yet
- Patient Instructions - Clean Catch UrineDocument1 pagePatient Instructions - Clean Catch UrinesarahNo ratings yet
- Yasmin Mogahed - Healing The Emptiness - A Guide To Emotional & Spiritual Well Being (2022)Document244 pagesYasmin Mogahed - Healing The Emptiness - A Guide To Emotional & Spiritual Well Being (2022)sarah100% (3)
- RG 2018180056Document13 pagesRG 2018180056sarahNo ratings yet
- Special Senses: Elaine N. MariebDocument55 pagesSpecial Senses: Elaine N. Mariebadelina.jianu9991No ratings yet
- Chapter 01Document30 pagesChapter 01sarahNo ratings yet
- Cervical Cancer StagingDocument35 pagesCervical Cancer StagingOttofianus Hewick KalangiNo ratings yet
- Morghan Edisi 6 - 1Document34 pagesMorghan Edisi 6 - 1sarahNo ratings yet
- 326-Article Text-1472-1-10-20211018Document8 pages326-Article Text-1472-1-10-20211018sarahNo ratings yet
- Selection Set Menu Ballroom 2021Document6 pagesSelection Set Menu Ballroom 2021sarahNo ratings yet
- Lancet-Gate in The COVID-19 Pandemic Era - Is It Alright For Science To Be WrongDocument4 pagesLancet-Gate in The COVID-19 Pandemic Era - Is It Alright For Science To Be WrongsarahNo ratings yet
- 242 FullDocument5 pages242 FullsarahNo ratings yet
- We Are Intechopen, The World'S Leading Publisher of Open Access Books Built by Scientists, For ScientistsDocument20 pagesWe Are Intechopen, The World'S Leading Publisher of Open Access Books Built by Scientists, For ScientistssarahNo ratings yet
- Guias ESC para Insuficiencia Cardiaca CronicaDocument128 pagesGuias ESC para Insuficiencia Cardiaca CronicaKarla HernandezNo ratings yet
- jpg20000 628 628Document1 pagejpg20000 628 628Galuh M ArtamtiNo ratings yet
- Contrast-Induced Acute Kidney Injury After Primary Percutaneous Coronary Intervention: Results From The HORIZONS-AMI SubstudyDocument9 pagesContrast-Induced Acute Kidney Injury After Primary Percutaneous Coronary Intervention: Results From The HORIZONS-AMI SubstudysarahNo ratings yet
- s12933 020 01087 4Document12 pagess12933 020 01087 4sarahNo ratings yet
- Introducing Serenia Hills, your private sanctuary in South JakartaDocument30 pagesIntroducing Serenia Hills, your private sanctuary in South JakartasarahNo ratings yet
- 1071 4385 1 PBDocument8 pages1071 4385 1 PBsarahNo ratings yet
- Optimal Medical Therapy vs. Percutaneous Coronary Intervention For Patients With Coronary Chronic Total OcclusionDocument7 pagesOptimal Medical Therapy vs. Percutaneous Coronary Intervention For Patients With Coronary Chronic Total OcclusionsarahNo ratings yet
- Impact of Optimal Medical Therapy On 10-Year Mortality After Coronary RevascularizationDocument12 pagesImpact of Optimal Medical Therapy On 10-Year Mortality After Coronary RevascularizationsarahNo ratings yet
- Relationship Between Operator Volume and Long-Term Outcomes After Percutaneous Coronary InterventionDocument15 pagesRelationship Between Operator Volume and Long-Term Outcomes After Percutaneous Coronary InterventionsarahNo ratings yet
- Early Rhythm-Control Therapy in Patients With Atrial FibrillationDocument11 pagesEarly Rhythm-Control Therapy in Patients With Atrial FibrillationMohammad AlmuhaiminNo ratings yet
- Supplement GuidelinesDocument2 pagesSupplement GuidelinessarahNo ratings yet
- BLS Acls Aha 2020Document103 pagesBLS Acls Aha 2020Nicholas PetrovskiNo ratings yet
- PIIS2212267215013829Document6 pagesPIIS2212267215013829sarahNo ratings yet
- Role of Echocardiography in Assessing Atrial Structure & Guiding AF AblationDocument14 pagesRole of Echocardiography in Assessing Atrial Structure & Guiding AF AblationsarahNo ratings yet
- Original Article Triple Negative Breast Cancer Characteristics Based On Basal-Like and Non-Basal-like SubtypesDocument8 pagesOriginal Article Triple Negative Breast Cancer Characteristics Based On Basal-Like and Non-Basal-like SubtypessarahNo ratings yet
- Medical Nutrition Therapy in Chronic Renal Disease: A Case StudyDocument6 pagesMedical Nutrition Therapy in Chronic Renal Disease: A Case StudysarahNo ratings yet
- Ahmed AlsheweredDocument9 pagesAhmed AlsheweredsarahNo ratings yet
- Medication Error Who PDFDocument32 pagesMedication Error Who PDFMica HernandezNo ratings yet
- Computer Engineering SyllabusDocument47 pagesComputer Engineering SyllabusLily ChanNo ratings yet
- Cs Project Book ManagementDocument22 pagesCs Project Book ManagementabNo ratings yet
- GROHE Specification Sheet 19443000-1Document2 pagesGROHE Specification Sheet 19443000-1Fred PrzNo ratings yet
- Lista Arancelaria EUADocument547 pagesLista Arancelaria EUAvilisbeth18No ratings yet
- 4jj1tybw01 Spec Sheet PDFDocument10 pages4jj1tybw01 Spec Sheet PDFcpaolinodNo ratings yet
- 5 Variable K-MapDocument15 pages5 Variable K-MapBen SewellNo ratings yet
- Memories of HomeDocument14 pagesMemories of HomeMary Francis Edmer SayconNo ratings yet
- Meralco Bill 330370940102 04142023Document2 pagesMeralco Bill 330370940102 04142023Jha CruzNo ratings yet
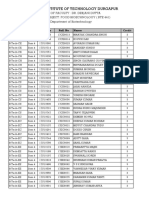
- List of Students Allotted in Open Elective Subjects (B. Tech and M. Tech (Dual Degree) Integrated MSc. - 4th Semester - Regular - 2018 - 19) - 2 PDFDocument26 pagesList of Students Allotted in Open Elective Subjects (B. Tech and M. Tech (Dual Degree) Integrated MSc. - 4th Semester - Regular - 2018 - 19) - 2 PDFArpan JaiswalNo ratings yet
- Differences in Left Ventricular and Left Atrial FuDocument10 pagesDifferences in Left Ventricular and Left Atrial FueugeniaNo ratings yet
- G5 C11 TestDocument6 pagesG5 C11 TestvictoriaNo ratings yet
- Osha Top 25 Physical HazardsDocument100 pagesOsha Top 25 Physical HazardsHasan Shakeel100% (2)
- Image Forgery DetectionDocument17 pagesImage Forgery DetectionanlemacoNo ratings yet
- Wda 201Document72 pagesWda 201MoussaNo ratings yet
- Pharmaceutical Ingredients and Excipient - LastpptDocument72 pagesPharmaceutical Ingredients and Excipient - LastpptFANTANo ratings yet
- Cattlemans Steakhouse MenuDocument1 pageCattlemans Steakhouse Menuapi-300741654No ratings yet
- Reles, Fuentes, Etc. Catalogo - ABBDocument452 pagesReles, Fuentes, Etc. Catalogo - ABBmpica100% (1)
- SK716 Pengintegrasian Mekanisme Nilai Karbon (English)Document13 pagesSK716 Pengintegrasian Mekanisme Nilai Karbon (English)Isti HanifahNo ratings yet
- Recycle ProgramDocument2 pagesRecycle ProgramKaps BlazeNo ratings yet
- Rules For The CertificationDocument84 pagesRules For The CertificationhdelriovNo ratings yet
- Deks Olje ArticleDocument5 pagesDeks Olje ArticleTomMacNaughtonNo ratings yet
- Practice Quiz M1 (Ungraded) - MergedDocument22 pagesPractice Quiz M1 (Ungraded) - MergedAbdullah Abdullah100% (1)
- Chemistry of Food Changes During Storage: Group 7Document22 pagesChemistry of Food Changes During Storage: Group 7Sonny MichaelNo ratings yet
- Sabp X 002Document18 pagesSabp X 002Hassan MokhtarNo ratings yet
- IQ 250/260 Transducer Quick Start GuideDocument2 pagesIQ 250/260 Transducer Quick Start GuideJoséEmmanuelCasasMunguíaNo ratings yet
- Pantheon-Katalog Eng WebDocument16 pagesPantheon-Katalog Eng WebJoe DoeNo ratings yet
- Circuits Review P2Document44 pagesCircuits Review P2José CastilloNo ratings yet
- Computations on a waiters bill pad and conversations in the mistDocument3 pagesComputations on a waiters bill pad and conversations in the mistRavishu NagarwalNo ratings yet
- Demonstration POSTNATAL EXAMINATION Easy WayDocument9 pagesDemonstration POSTNATAL EXAMINATION Easy Wayjyoti singhNo ratings yet
- Pasture FatteningDocument15 pagesPasture FatteningKartika PurnamasariNo ratings yet