Professional Documents
Culture Documents
Mirror Neuron Stimulation Improves Motor Skills in Kids with Cerebral Palsy
Uploaded by
Ana Barneto CortésOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Mirror Neuron Stimulation Improves Motor Skills in Kids with Cerebral Palsy
Uploaded by
Ana Barneto CortésCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/256075042
Effects of mirror neurons stimulation on motor skill rehabilitation in children
with cerebral palsy: a clinical trial
Article in Journal of the Medical Association of Thailand = Chotmaihet thangphaet · January 2012
Source: PubMed
CITATIONS READS
9 916
4 authors, including:
Prinnapak Mahasup Paskorn Sritipsukho
Thammasat University Thammasat University
5 PUBLICATIONS 28 CITATIONS 34 PUBLICATIONS 409 CITATIONS
SEE PROFILE SEE PROFILE
All content following this page was uploaded by Prinnapak Mahasup on 16 February 2017.
The user has requested enhancement of the downloaded file.
Effects of Mirror Neurons Stimulation on Motor Skill
Rehabilitation in Children with Cerebral Palsy:
A Clinical Trial
Namfon Mahasup MSc*, Paskorn Sritipsukho MD**,
Raweewan Lekskulchai PhD***, Tippawan Hansakunachai MD**
* Postgraduate Studies Program, Faculty of Medicine, Thammasat University, Pathumthani, Thailand
** Department of Pediatrics, Faculty of Medicine, Thammasat University, Pathumthani, Thailand
*** Faculty of Physical Therapy, Mahidol University, Bangkok, Thailand
Objective: The authors aimed to compare the motor function measured by Gross Motor Function Measure (GMFM-66)
between mirror neurons stimulation based VCD program at home and conventional physical therapy in children with
cerebral palsy for two months.
Material and Method: A randomized controlled trial was performed with thirty children with spastic diplegia aged 2-10
years in Thammasat university hospital and Rajanukul institue. They were randomly assigned to receive either the mirror
neurons stimulation based VCD program practice at home (experimental group) or the conventional physical therapy
(control group) for two months. Both groups were measured the motor function by GMFM-66 at entry, the first month and the
end of the second month. Analysis of covariance was used to compare mean changes of GMFM-66 scores between both
groups at the second month after adjusted for the baseline level.
Results: A total of 30 children with cerebral palsy, aged 2.2 - 9.5 years (mean age 5.9 + 2.2 years). The mean changes of the
GMFM scores in experimental group were slightly higher than those in the control group of 2.1 (95% CI: -2.3, 6.5) at the
second month after adjusted for the baseline level. The mean GMFM scores were significantly improved in all dimensions
except lying and rolling dimension, at the first and second month when compared to the baseline level in both groups.
Conclusion: This pilot study demonstrated the mirror neurons stimulation based VCD program can improve motor
function, at least, as much as the conventional physical therapy.
Keywords: Cerebral palsy, Mirror neuron, Action observation, Gross motor function measure
J Med Assoc Thai 2012; 95 (Suppl. 1): S166-S172
Full text. e-Journal: http://jmat.mat.or.th
Children with cerebral palsies often lack of activities or environments by stimulating sensorimotor
opportunity to learn or practice motor skills because of experience(2). Recently, human mirror neuron system
static pathology of their brains in development of has been discovered. It is involved in action
movement and posture(1). The central nervous system understanding, imitation, learning of novel complex
dysfunction is a major problem of those children actions, and internal rehearsal of actions(3). Implication
causing loss of communication between the brain and of using action observation and imitation may be
body. This results in uncontrolled movements and beneficial in motor rehabilitation of children with cerebral
posturing. Motor learning is one of strategies to palsy (4,5). Action observation and imitation were
maximize motor function in children with cerebral palsy. reported in recovery of motor function in stroke
Motor learning, the acquisition of new skills with patients(4,6,7). Steenbergen B et al(8) reported that motor
practice, is based on practice of goal-oriented motor imagery training may be a valuable additional tool for
function tasks that matched to the children’s abilities, rehabilitation in children with hemiparetic cerebral palsy.
for successful retention and transfer to other motor Practicing and learning at home is the most successful
way to motivate and facilitate children with cerebral
Correspondence to: palsy(9-11).
Sritipsukho P, Department of Pediatrics, Faculty of Medicine,
Thammasat University, Pathumthani 12120, Thailand.
The author hypothesized that motor learning
Phone: 0-2926-9759 by imitation could help children with cerebral palsy to
E-mail: paskorn100@yahoo.com improve their motor ability. Repetitive watching daily
S166 J Med Assoc Thai Vol. 95 Suppl. 1 2012
activities movement via video compact disc (VCD), assigned according to the randomization list to receive
containing mirror neurons stimulation based VCD either the mirror neurons stimulation based VCD
program on motor skill rehabilitation, at home may program and practice at home or conventional physical
facilitate children with cerebral palsy to imitate therapy for two months. A sample size of 30 children,
movements. A VCD program was designed to improve 15 for each group, was needed to obtain 80% power at
both upper and lower extremities function in children 0.05 level of significance (two-sided) to test that the
with cerebral palsy. Finally, the authors have developed successful event rate (increasing GMFM scores at least
VCD program that applying concept of the mirror 30% from baseline at the end of 2 months) in experimental
neurons stimulation on standard rehabilitation group and control group of 0.8 and 0.3 respectively.
technique. The process to develop the VCD included The present study was approved by the ethics
reviewing the literature, small group discussion with committee of Thammasat University and Rajanukul
pediatric specialists in behavioral and development, institute. The participants in the experiment group
pediatric physical therapists and caregivers. The VCD received the mirror neurons stimulation based VCD
contained stretching exercises and daily activities program and practice at home three times a day for two
including wearing sock, putting on shirt, shorts and months. The mirror neurons stimulation based VCD
walking sideways(12-14). Then, the VCD master has been program contained four volumes. The first volume
produced by the television producers. Piloting the VCD includes activities for improving balance in sitting
program has been performed from experts and 3 children position. The second volume includes activities of
with cerebral palsy to ensure accurate contents and sitting to standing. The third volume includes activities
good performance of VCD presentation. This pilot for improving balance in standing position. The last
study aimed to determine the effect of the mirror neurons one includes activities of sideway walking. Activities
stimulation based VCD program on motor skill in the VCD program are demonstrated by a child actress.
rehabilitation of children with cerebral palsy by The activities consist of fundamental daily activities
comparing motor function measured by the gross motor and stretching exercises. The running time of each
function measure (GMFM) between conventional volume is about 30 minutes. The subjects were informed
physical therapy and the mirror neurons stimulation for to regularly practice for two weeks per volume. Their
based VCD program for 2 months. parents were informed and trained for practicing their
children by VCD program at home and were asked to
Material and Method complete daily record of participant’s activities. The
A randomized controlled trial was performed participants were scheduled to meet a pediatric physical
with thirty children with cerebral palsy recruited from therapist once a week to monitor possible side effects.
Thammasat university hospital and Rajanukul institute. Concerning the control group, the participants received
The clinicaltrials.gov identifier is NCT01267929. The conventional physical therapy regularly at the hospital
inclusion criteria were children diagnosed of spastic once a week for two months. The conventional physical
diplegia aged 2-10 years with Gross Motor Function therapy technique in the present study derived from
Classification System (GMFCS) level of 1-3 who can the manual technique including the Bobath concept,
comply verbal instruction and can ambulate stretching exercise and functional training for 30-45
independently. The GMFCS, a five level classification minutes at a time. Both experimental and control groups
system is used to describe the gross motor function of were measured their motor functions with GMFM-66(16)
children with cerebral palsy on the basis of their self- by an independent pediatric physical therapist who
initiated movement especially sitting, walking and was blinded for treatment allocation at entry, the first
wheeled mobility (15). The exclusion criteria were month and the second month.
participants who had orthopedic intervention or All data were coded and entered into Epidata
botulinum toxin injection within 6 months, seizure, software. Statistical analysis was conducted using
cardiopulmonary compromise conditions, or severe STATA (version 9.0). Frequency and percentage was
visual and hearing deficits. Informed consent was used to describe qualitative variables. Mean and
obtained from the participants’ parents before standard deviation was used to describe quantitative
participation in the present study. The randomization variables. The Chi-square test was used to compare
lists with sealed envelopes, using stratified the characteristics between both groups. The Wilcoxon
randomization by centers with permuted blocks of two, matched-pairs signed-rank test was used to compare
were prepared. The participants were randomly mean score within group. Analysis of Covariance
J Med Assoc Thai Vol. 95 Suppl. 1 2012 S167
(ANCOVA) was used to compare mean scores of difference of 2.1 (95% CI: -2.3, 6.5) after adjusted for the
GMFM at the second month between two groups after baseline level. Also, the mean GMFM scores of sitting,
adjusted for the baseline scores at entry. All tests were crawling and kneeling and walking running and jumping
tested the significance level at 0.05. The compliance in the experimental group were higher than those of the
was measured by daily records containing the number control group with the mean difference of 4.9 (95% CI:
of watching days, the number of watching times, watch -0.6, 10.5), 3.9 (95% CI: -3.0, 10.8) and 2.8 (95% CI: -7.1,
attention and practice intention. The percentage of 12.8) respectively after adjusted for the baseline level.
compliance was calculated by number of days that However, the mean scores of the participants were
participants complied provided activities divided by significantly improved in all dimensions except lying
the total days of 56 for each category. The level of the and rolling dimension, at the first and second month
compliance of each item was categorized by the when compared to the baseline level in both groups.
percentage of compliance into three levels as good According to the experimental group, most
compliance (> 70%), moderate compliance (50%-70%) participants had good compliance in watching but
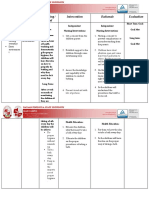
and low compliance (< 50%). had moderate compliance in practicing as shown in the
Fig. 1.
Results
A total of 30 children with cerebral palsy, aged Discussion
2.2-9.5 years (mean age 5.9 + 2.2 years), was followed This was the first study in Thailand to
and completed the study. The baseline characteristics determine the effect of action observation and imitation
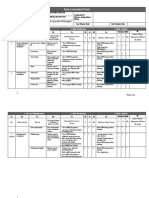
were shown in Table 1. As shown in Table 2, the total by stimulating mirror neurons in children with cerebral
score of GMFM in the experimental group (receiving palsy. The authors believe that the mirror neurons
VCD program) was higher than the control group stimulation based VCD program on motor skill
(receiving conventional physical therapy) with the mean rehabilitation in the present study would be benefit to
Table 1. Characteristics of children with cerebral palsy in both groups
Characteristics Experimental group* Control group**
(n = 15) (n = 15)
Frequency (%) Frequency (%)
Sex
Boy 9 (60.0) 10 (67.0)
Girl 6 (40.0) 5 (34.0)
GMFCS (Gross Motor Function Classification System)
II 1 (7.0) 1 (7.0)
III 14 (93.0) 14 (93.0)
Weight for height age
Normal weight 13 (87.0) 9 (60.0)
Under weight 2 (13.0) 3 (20.0)
Over weight 0 (0) 3 (20.0)
On anti-spasticity medications
Yes 4 (27.0) 6 (40.0)
No 11 (73.0) 9 (60.0)
Caregiver
Mother 11 (74.0) 10 (67.0)
Father 2 (13.0) 3 (20.0)
Other 2 (13.0) 2 (13.0)
Mean age (SD) in years 6.2 (2.2) 5.5 (2.2)
(Range) (2.6-9.5) (2.2-8.3)
Baseline GMFM-66, mean (SD) 44.8 (14.0) 49.4 (13.1)
* The experimental group, the group having mirror neurons stimulation based VCD program
** The control group, the group having conventional physical therapy
S168 J Med Assoc Thai Vol. 95 Suppl. 1 2012
Table 2. GMFM-66 of children with cerebral palsy in both groups at entry, the first and the second month
GMFM-66 Experimental group (n = 15) Control group (n = 15) Adjusted mean changes at 2nd
Mean (SD) Mean (SD) month between experimental
and control groups
Baseline 1st 2 nd Baseline 1st 2 nd Mean difference# p-value##
month month month month (95%CI)
Total score 44.8 50.0 * 54.7 ** 49.4 53.8* 57.5** 2.1 0.341
(14.0) (13.8) (14.5) (13.1) (15.2) (16.2) (-2.3, 6.5)
Lying and rolling 70.8 75.9 75.9 78.4 78.4 78.4 -0.3 0.815
dimension score (14.0) (6.5) (6.5) (0) (0) (0) (-3.4, 2.7)
Sitting dimension 57.3 62.5* 68.0** 61.3 64.3* 67.2** 4.9 0.080
score (20.0) (19.0) (21.3) (17.0) (17.2) (19.1) (-0.6, 10.5)
Crawling and kneeling 81.9 90.6* 92.1** 92.3 95.2* 96.0** 3.9 0.260
dimension score (24.1) (22.8) (21.2) (18.3) (16.9) (14.8) (-3.0, 10.8)
Standing dimension 26.2 34.9* 43.9** 26.6 37.1* 44.6** -0.3 0.946
score (16.7) (17.1) (18.2) (21.1) (26.2) (24.1) (-10.1, 9.4)
Walking, running and 7.06 13.4* 19.6** 21.5 25.0* 31.6** 2.8 0.561
jumping dimension (21.3) (21.7) (22.8) (26.4) (28.4) (31.7) (-7.1, 12.8)
score
# The mean scores difference of the end of the 2nd month between experimental and control groups after adjusted for the
baseline level
## The p-value was based on the analysis of covariance between experimental and control groups at the end of 2nd month
after adjusted for the baseline level
* Significant change (p < 0.05) within group between baseline and 1st month measures using wilcoxon matched-pairs signed-
rank test
** Significant change (p < 0.05) within group between baseline and 2nd months measures using wilcoxon matched-pairs
signed-rank test
piloted by both the experts and children with cerebral
palsy before performing this trial to test the
effectiveness of the program. This result showed a
trend of the larger mean changes of GMFM scores in
the experimental group at the second month compared
to those in the control group in many dimensions after
adjusted for the baseline level although the mean
changes did not reach the statistical significance level.
Larger sample size will be required to determine more
precise result. However, significant improvement of the
mean GMFM scores was found in both groups after
the first and the second month periods. In addition,
- Percentage more than 70 percents that mean good level the good compliance in watching reflected good
- Percentage between 50 and 70 percents that mean moderate performance of VCD presentation. The authors suggest
level
that the mirror neurons stimulation based VCD program
- Percentage below 50 percents that mean low level
is an alternative treatment for children with cerebral
Fig. 1 The compliance level of participants in palsy who lack the opportunities to access
experimental group conventional physical therapy in medical center. The
present study confirmed that the mirror neurons
children with cerebral palsy since it was developed by stimulation based VCD program could improve motor
multidisciplinary team and produced by the television function, at least, as much as the conventional physical
producers. The contents and its performance were also therapy. However, the children with cerebral palsy
J Med Assoc Thai Vol. 95 Suppl. 1 2012 S169
should not use this VCD program for practicing at home neurons stimulation based VCD program can improve
only, contacting physical therapist for assessing motor motor function, at least, as much as the conventional
function and receiving individual treatment program physical therapy. It may be an alternative treatment for
together periodically is also essential. Apart from this, children with cerebral palsy who lack the opportunities
meeting physicians and other healthcare personnel for to access conventional physical therapy in medical
holistic approach management is recommended to center. Good compliance by practice repeatedly and
achieve the best result. regularly with the VCD program at home is suggested
The authors also recommend that the children to achieve the best clinical outcome.
have to practice via the VCD program repeatedly and
regularly since development of such skill in children Acknowledgement
depends on imitation. There were also several The authors wish to thank Physical Therapy
researches studying on children’s imitation. Katherine and Hydrotherapy Center, Department of Physical
et al(17) measured imitative learning of a novel action Therapy, Faculty of Allied Health Sciences, Thammasat
seen only in a third-party interaction in a group of 48 University and Rajanukul institute for kindly supports.
18-to 20-month-olds. Their study found that 50% of We gratefully acknowledge all children and their
children passed the imitative task; therefore, the parents who participated in the present study. The
children could imitate novel actions of adults who were present study was supported by a research grant from
not interacting with them. The mechanism could be the National Research Council of Thailand.
explained by the study of Lepage JF et al(18) who used
EEG to probe mu rhythm modulation in 15 children Potential conflicts of interest
during observation and execution of hand movements. None.
The observation of objected-oriented movement could
produce modulation of the mu rhythm. The mu rhythm References
attenuation occurred in children under 11 years old 1. Papavasiliou AS. Management of motor problems
during observation of hand movements which similar in cerebral palsy: a critical update for the clinician.
to what had been reported in adults. Steenbergen B et Eur J Paediatr Neurol 2009; 13: 387-96.
al(8) presented motor imagery training may be a valuable 2. Bar-Haim S, Harries N, Nammourah I, Oraibi S,
additional tool for rehabilitation in children with Malhees W, Loeppky J, et al. Effectiveness of motor
hemiparetic cerebral palsy. Finally, Chaiyawat P et al(7) learning coaching in children with cerebral palsy:
developed and examined the effectiveness of individual a randomized controlled trial. Clin Rehabil 2010;
home rehabilitation program on the mirror neuron 24: 1009-20.
concept for Thai ischemic stroke patients. They found 3. Rizzolatti G, Craighero L. The mirror-neuron system.
that early home rehabilitation program for Thai ischemic Annu Rev Neurosci 2004; 27: 169-92.
stroke patients provided significantly better outcomes 4. Buccino G, Solodkin A, Small SL. Functions of the
in improving motor function than usual care. mirror neuron system: implications for
Since the VCD program including the contents neurorehabilitation. Cogn Behav Neurol 2006; 19:
has been developed solely for the present study and 55-63.
has not been used for children with cerebral palsy in 5. de Vries S, Mulder T. Motor imagery and stroke
real practice. Further feedback and amendment of the rehabilitation: a critical discussion. J Rehabil Med
contents and VCD presentation has to be done after 2007; 39: 5-13.
launching this VCD program in real practice. There are 6. Ertelt D, Small S, Solodkin A, Dettmers C,
some limitations of this study. This VCD program was McNamara A, Binkofski F, et al. Action observation
applicable for children with cerebral palsy with spastic has a positive impact on rehabilitation of motor
diplegia who had high GMFCS level (1-3). Generalized deficits after stroke. Neuroimage 2007; 36 (Suppl
the results to children with other types of cerebral palsy 2): T164-73.
with different severity are limited. Further studies of 7. Chaiyawat P, Sritipsukho P, Kulkantrakorn K.
larger sample size and longer duration are required to Effectiveness of home rehabilitation program for
determine the effectiveness of the VCD program. ischemic stroke. Thammasat Med J 2009; 9: 111-9.
8. Steenbergen B, Craje C, Nilsen DM, Gordon AM.
Conclusion Motor imagery training in hemiplegic cerebral
This pilot study demonstrated the mirror palsy: a potentially useful therapeutic tool for
S170 J Med Assoc Thai Vol. 95 Suppl. 1 2012
rehabilitation. Dev Med Child Neurol 2009; 51: 690- cerebral palsy and similar movement disorders. A
6. guide for parents and professionals. Bethesda,
9. Palisano RJ. A collaborative model of service MD: Woodbine House; 2006.
delivery for children with movement disorders: a 14. Wiart L, Darrah J, Kembhavi G. Stretching with
framework for evidence-based decision making. children with cerebral palsy: what do we know and
Phys Ther 2006; 86: 1295-305. where are we going? Pediatr Phys Ther 2008; 20:
10. Weightman A, Preston N, Levesley M, Holt R, 173-8.
Mon-Williams M, Clarke M, et al. Home based 15. Palisano RJ, Rosenbaum P, Bartlett D, Livingston
computer-assisted upper limb exercise for young MH. Content validity of the expanded and revised
children with cerebral palsy: a feasibility study Gross Motor Function Classification System. Dev
investigating impact on motor control and Med Child Neurol 2008; 50: 744-50.
functional outcome. J Rehabil Med 2011; 43: 359- 16. Bjornson K, Graubert C, McLaughlin J. Test-retest
63. reliability of the gross motor function measure in
11. Katz-Leurer M, Rotem H, Keren O, Meyer S. The children with cerebral palsy. Pediatr Phys Ther
effects of a ‘home-based’ task-oriented exercise 2000; 12: 200-2.
programme on motor and balance performance in 17. Herold KH, Akhtar N. Imitative learning from a third-
children with spastic cerebral palsy and severe party interaction: relations with self-recognition
traumatic brain injury. Clin Rehabil 2009; 23: 714- and perspective taking. J Exp Child Psychol 2008;
24. 101: 114-23.
12. O’Connor J, Yu E, Guohui L. Moving ahead: a 18. Lepage JF, Theoret H. EEG evidence for the
training manual for children with motor disorders. presence of an action observation-execution
New York: Springer-Verlag Publisher; 1998. matching system in children. Eur J Neurosci 2006;
13. Martin S. Teaching motor skills to children with 23: 2505-10.
J Med Assoc Thai Vol. 95 Suppl. 1 2012 S171
ผลของการฟืน้ ฟูทกั ษะการเคลือ่ นไหวโดยกระตุน้ การทำงานของเซลล์กระจกเงาในเด็กภาวะสมองพิการ
น้ำฝน มหาทรัพย์, ภาสกร ศรีทพ
ิ ย์สโุ ข, ระวีวรรณ เล็กสกุลไชย, ทิพวรรณ หรรษคุณาชัย
วัตถุประสงค์: เพือ่ เปรียบเทียบผลลัพธ์การรักษาด้านการเคลือ่ นไหวประเมินโดย Gross Motor Function Measure
(GMFM-66) ระหว่ า งการรั ก ษาทางกายภาพบำบั ด แบบมาตรฐานกั บ การรั ก ษาด้ ว ยโปรแกรมกายภาพบำบั ด
สำหรับพัฒนาทักษะการเคลื่อนไหวโดยกระตุ้นการทำงานของเซลล์กระจกเงาในรูปแบบวีดิทัศน์ เป็นเวลา 2 เดือน
ในเด็กภาวะสมองพิการ
วัสดุและวิธกี าร: เป็นการวิจยั เชิงทดลองทางคลินกิ โดยคัดเลือกอาสาสมัครเด็กภาวะสมองพิการชนิด spastic diple-
gia จำนวน 30 คน อายุระหว่าง 2-10 ปี จากโรงพยาบาลธรรมศาสตร์เฉลิมพระเกียรติและสถาบันราชานุกลู จากนัน้ สุม่
อาสาสมัครเพื่อแบ่งเข้ากลุ่ม ระหว่างกลุ่มที่ได้รับโปรแกรมกายภาพบำบัดสำหรับพัฒนาทักษะการเคลื่อนไหวโดย
กระตุ้นการทำงานของเซลล์กระจกเงาในรูปแบบวีดิทัศน์โดยให้นำไปฝึกปฏิบัติที่บ้าน (กลุ่มทดลอง) หรือกลุ่มที่ได้รับ
การรั ก ษาทางกายภาพบำบั ด แบบมาตรฐาน (กลุ ่ ม ควบคุ ม ) ทั ้ ง สองกลุ ่ ม จะได้ ร ั บ การประเมิ น ความสามารถ
ด้านการเคลือ่ นไหวด้วยแบบประเมิน GMFM-66 เมือ่ เข้าร่วมการศึกษาทีร่ ะยะเวลา 1 เดือน และทีร่ ะยะเวลา 2 เดือน
วิเคราะห์ข้อมูลด้วยสถิติ analysis of covariance เพื่อเปรียบเทียบความแตกต่างค่าคะแนนเฉลี่ยของ GMFM-66
ที่เปลี่ยนแปลงหลังการรักษา 2 เดือน ระหว่างทั้งสองกลุ่ม
ผลการศึกษา: เด็กภาวะสมองพิการจำนวน 30 คน มีอายุเฉลีย่ 5.9 + 2.2 ปี (2.2-9.5 ปี) ค่าคะแนนเฉลีย่ ของ GMFM-
66 ทีเ่ ปลีย่ นแปลงหลังการรักษาในกลุม่ ทดลองมากกว่าในกลุม่ ควบคุม 2.1 คะแนน (ช่วงแห่งความเชือ่ มัน่ ที่ 95% เป็น
-2.3 ถึ ง 6.5) เมื ่ อ ได้ ป รั บ ค่ า คะแนนเมื ่ อ เริ ่ ม เข้ า โครงการแล้ ว คะแนนเฉลี ่ ย ของอาสาสมั ค รทั ้ ง สองกลุ ่ ม
มีคา่ เพิม่ ขึน้ อย่างมีนยั สำคัญทางสถิตทิ กุ หัวข้อการประเมิน ยกเว้นหัวข้อท่านอน ท่ากลิง้ ทีร่ ะยะเวลา 1 เดือน และ 2
เดือน เมื่อเปรียบเทียบกับคะแนนก่อนเข้าร่วมวิจัย
สรุป: การศึกษานำร่องนี้พบว่าโปรแกรมกายภาพบำบัดสำหรับพัฒนาทักษะการเคลื่อนไหวโดยกระตุ้นการทำงาน
ของเซลล์ ก ระจกเงาในรู ป แบบวี ด ิ ท ั ศ น์ ท ำให้ ค วามสามารถ ด้ า นการเคลื ่ อ นไหวดี ข ึ ้ น เช่ น เดี ย วกั บ การรั ก ษา
ทางกายภาพบำบัดแบบมาตรฐาน
S172 J Med Assoc Thai Vol. 95 Suppl. 1 2012
View publication stats
You might also like
- Effectiveness of Sensory Integration Therapy (Vestibular & Proprioception Input) On Gross Motor Functioning in Developmental Delayed and Spastic Diplegic CP ChildrenDocument6 pagesEffectiveness of Sensory Integration Therapy (Vestibular & Proprioception Input) On Gross Motor Functioning in Developmental Delayed and Spastic Diplegic CP ChildrenYanuar Adi SanjayaNo ratings yet
- Upw WorkbookDocument109 pagesUpw WorkbookAdriana SuruNo ratings yet
- Lim Meng Heck (SR - Operation Manager) : ISK Ssessment ORMDocument2 pagesLim Meng Heck (SR - Operation Manager) : ISK Ssessment ORMVaradaraju ThirunavukkarasanNo ratings yet
- Steps To Prevent Drug AddictionDocument9 pagesSteps To Prevent Drug AddictionLuna DizonNo ratings yet
- Neuro Developmental Treatment (NDT) For Cerebral Palsy: - A Clinical StudyDocument2 pagesNeuro Developmental Treatment (NDT) For Cerebral Palsy: - A Clinical StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Mental Health Action PlanDocument2 pagesMental Health Action PlanKenny Ann Grace Batiancila100% (9)
- Scientific Research Journal of India SRJI Vol 3, Issue 2, Year 2014 Full IssueDocument120 pagesScientific Research Journal of India SRJI Vol 3, Issue 2, Year 2014 Full IssueDr. Krishna N. SharmaNo ratings yet
- With Answers No RationaleDocument41 pagesWith Answers No RationaleronnaxNo ratings yet
- Mirror Therapy Feedback For Selective Motor Control of The Upper Extremities in Spastic Hemiplegic Cerebral Palsy: A Randomized Controlled TrialDocument4 pagesMirror Therapy Feedback For Selective Motor Control of The Upper Extremities in Spastic Hemiplegic Cerebral Palsy: A Randomized Controlled TrialPaula Tirado GuallarNo ratings yet
- N.Vago ApprendimentoDocument30 pagesN.Vago ApprendimentoLuca PellaNo ratings yet
- Original Article: Effects of Neurodevelopmental Therapy On Gross Motor Function in Children With Cerebral PalsyDocument6 pagesOriginal Article: Effects of Neurodevelopmental Therapy On Gross Motor Function in Children With Cerebral PalsyIkhwatul FitriNo ratings yet
- Tugas Bahasa Inggris Temu 9Document12 pagesTugas Bahasa Inggris Temu 9Ari PutraNo ratings yet
- Effects of Modified Adeli Suit Therapy On Improvement of Gross Motor Function in Children With Cerebral Palsy (2011)Document6 pagesEffects of Modified Adeli Suit Therapy On Improvement of Gross Motor Function in Children With Cerebral Palsy (2011)caterina1990No ratings yet
- Two Year Motor Outcomes Associated With The Dose of NICU - 2022 - Early Human DDocument7 pagesTwo Year Motor Outcomes Associated With The Dose of NICU - 2022 - Early Human DJUAN HIMMEL ESPINOZA ANDIANo ratings yet
- Interventions To Improve Gross Motor Performance in Children With Neurodevelopmental Disorders A Meta AnalysisDocument16 pagesInterventions To Improve Gross Motor Performance in Children With Neurodevelopmental Disorders A Meta AnalysissilNo ratings yet
- Evidencias VojtaDocument9 pagesEvidencias VojtaRommel AndresNo ratings yet
- Yabunaka 2011Document9 pagesYabunaka 2011Carolina BorchesNo ratings yet
- Comparison Between The Effect of NeurodevelopmentaDocument9 pagesComparison Between The Effect of NeurodevelopmentaDellNo ratings yet
- Int. Therapy Research DatoreDocument25 pagesInt. Therapy Research DatoreAll About Kids100% (1)
- Ymj 55 1736Document7 pagesYmj 55 1736Cristian HanganNo ratings yet
- Dementia, Physical Fitness and Cognitive Function Research PDFDocument9 pagesDementia, Physical Fitness and Cognitive Function Research PDFdevdsantoshNo ratings yet
- CP Research News 2020 May 4Document10 pagesCP Research News 2020 May 4Ana paula CamargoNo ratings yet
- 7608-Article Text-13581-1-10-20210613Document20 pages7608-Article Text-13581-1-10-20210613SuniNo ratings yet
- Studyprotocol Open Access: Grecco Et Al. BMC Pediatrics 2013, 13:168Document11 pagesStudyprotocol Open Access: Grecco Et Al. BMC Pediatrics 2013, 13:168Ana paula CamargoNo ratings yet
- Comparison Between Kinesitherapy, Magnetic Field and Their Combination For Cerebral Motor Disorders in Early ChildhoodDocument8 pagesComparison Between Kinesitherapy, Magnetic Field and Their Combination For Cerebral Motor Disorders in Early ChildhoodIJAR JOURNALNo ratings yet
- NeuroOncolPract 2016 Carlson Green Nop npw015Document11 pagesNeuroOncolPract 2016 Carlson Green Nop npw015Elías Coreas SotoNo ratings yet
- Yonsei Med J2014 ParkDocument8 pagesYonsei Med J2014 ParkCristian HanganNo ratings yet
- Tdcs Inglês 1Document8 pagesTdcs Inglês 1Augusto ManoelNo ratings yet
- Ijpbs 124236Document7 pagesIjpbs 124236erfan.izadpanahNo ratings yet
- Cia 14 347Document14 pagesCia 14 347Josefina PalmesNo ratings yet
- PJMS 32 181Document4 pagesPJMS 32 181RobertoVargasPérezNo ratings yet
- Pzaa 232Document11 pagesPzaa 232Aroa BermudezNo ratings yet
- Papn MS Id 000156Document7 pagesPapn MS Id 000156niekoNo ratings yet
- cpDocument11 pagescp409530315fjuNo ratings yet
- Effectiveness of Early Intervention of Coma ArousaDocument7 pagesEffectiveness of Early Intervention of Coma ArousaZoroNo ratings yet
- Durairaj Satheeskumar, Ku Dhaneshkumar, K Rajasenthil: KeywordsDocument5 pagesDurairaj Satheeskumar, Ku Dhaneshkumar, K Rajasenthil: KeywordsEmad Eldin Mohamed AbdelatiefNo ratings yet
- MineDocument13 pagesMineZahra Faras SukmaNo ratings yet
- Motor Development Research PaperDocument8 pagesMotor Development Research Paperepfdnzznd100% (1)
- 1 s2.0 S1013702515000615 MainDocument9 pages1 s2.0 S1013702515000615 MainLalala Safitri2000No ratings yet
- Plyometric Training Effectiveness and Optimal.3Document11 pagesPlyometric Training Effectiveness and Optimal.3LeonardoValenzuelaNo ratings yet
- Effects of A Neurodevelopmental Treatment Based.3Document13 pagesEffects of A Neurodevelopmental Treatment Based.3ivairmatiasNo ratings yet
- Jpts 27 673Document4 pagesJpts 27 673Lazlo SecretNo ratings yet
- 1840 8465 1 PBDocument7 pages1840 8465 1 PBsarah fitriaNo ratings yet
- Potential Effects of Traditional Massage On SpastiDocument6 pagesPotential Effects of Traditional Massage On SpastievinovianiNo ratings yet
- Single Blind Randomised Controlled Trial of GAME Goals Activity Motor Enrichment in Infants at High Risk of Cerebral Palsy 2016 Research in DevelopmenDocument12 pagesSingle Blind Randomised Controlled Trial of GAME Goals Activity Motor Enrichment in Infants at High Risk of Cerebral Palsy 2016 Research in DevelopmenFarin MauliaNo ratings yet
- PNF 6 Proprioceptive Neuromuscular Facilitation (PNF) vs. Task Specific TrainingDocument6 pagesPNF 6 Proprioceptive Neuromuscular Facilitation (PNF) vs. Task Specific TrainingAnonymous j0xAgHs3No ratings yet
- Kwon 2015Document7 pagesKwon 2015Waqar HassanNo ratings yet
- Holistic Brain Injury Program for ChildrenDocument12 pagesHolistic Brain Injury Program for ChildrenCatherineNo ratings yet
- J Head Trauma Rehabil 2014 29 E49Document16 pagesJ Head Trauma Rehabil 2014 29 E49Alejandra VitiNo ratings yet
- Disabilities 02 00026 v2Document14 pagesDisabilities 02 00026 v2Kaka Satria PratamaNo ratings yet
- Cerebral Palsy Update - Focusing On The Treatments and InterventionsDocument6 pagesCerebral Palsy Update - Focusing On The Treatments and InterventionsDianNo ratings yet
- Journal Presentation by 18PT3015 PEDDocument20 pagesJournal Presentation by 18PT3015 PEDAbdul KhadeerNo ratings yet
- TAMO Terapija PDFDocument9 pagesTAMO Terapija PDFIkre19No ratings yet
- Morgan 2013Document14 pagesMorgan 2013NéstorNo ratings yet
- Articulo en Ingles 1Document9 pagesArticulo en Ingles 1Leidy GarciaNo ratings yet
- 2022 Article 16332Document11 pages2022 Article 16332ClaudiaNo ratings yet
- 14Document9 pages14yeremias setyawanNo ratings yet
- Archive of SID: Research ArticleDocument8 pagesArchive of SID: Research ArticleAnushka RaipureNo ratings yet
- Alternative Seating Devices For Children With.23Document38 pagesAlternative Seating Devices For Children With.23Alex LyrNo ratings yet
- Effectiveness of Modified Constraint-Induced Movement Therapy in Children With Unilateral Spastic Cerebral Palsy: A Randomized Controlled TrialDocument10 pagesEffectiveness of Modified Constraint-Induced Movement Therapy in Children With Unilateral Spastic Cerebral Palsy: A Randomized Controlled TrialMunni KNo ratings yet
- Effects of Neuro-Linguistic Programming (NLP) Imagery Model On Enhancing Kickboxers' PerformanceDocument11 pagesEffects of Neuro-Linguistic Programming (NLP) Imagery Model On Enhancing Kickboxers' PerformanceIveta NikolovaNo ratings yet
- FulltextDocument9 pagesFulltextVivek Edamuriyil RamesanNo ratings yet
- Running Head: Brain and CognitionDocument10 pagesRunning Head: Brain and CognitionHassan SiddiquiNo ratings yet
- Randomized Trial of Observation and ExecutionDocument9 pagesRandomized Trial of Observation and ExecutionAna Barneto CortésNo ratings yet
- Pri 1674Document9 pagesPri 1674Ana Barneto CortésNo ratings yet
- Mirror Neuron SystemDocument13 pagesMirror Neuron SystemAna Barneto CortésNo ratings yet
- Effects of Live and VideoDocument7 pagesEffects of Live and VideoAna Barneto CortésNo ratings yet
- PSYCH 7 Course OutlineDocument4 pagesPSYCH 7 Course OutlineJM FranciscoNo ratings yet
- Atos CFSDocument22 pagesAtos CFSPaul SmithNo ratings yet
- Efficacy of Facet Block in Lumbar Facet Joint Syndrome PatientsDocument6 pagesEfficacy of Facet Block in Lumbar Facet Joint Syndrome PatientsthiagoNo ratings yet
- Canadian Diabetes Clinical Guidelines 2008Document215 pagesCanadian Diabetes Clinical Guidelines 2008FelipeOrtiz100% (4)
- Simplified Version of Kisumu County CIDPDocument29 pagesSimplified Version of Kisumu County CIDPGolden AshNo ratings yet
- Reading Unit 3Document2 pagesReading Unit 3estefania aranda jimenezNo ratings yet
- Safety Data Sheet Conbextra Gp2: Revision Date: 01/01/2020 Revision: 0ADocument8 pagesSafety Data Sheet Conbextra Gp2: Revision Date: 01/01/2020 Revision: 0AAnonymous kRIjqBLkNo ratings yet
- UW Water Resources and Innovation Conference 2015Document61 pagesUW Water Resources and Innovation Conference 2015LungisaniNo ratings yet
- Food Security - Definition and Measurement PDFDocument3 pagesFood Security - Definition and Measurement PDFFristhaPratiwi100% (1)
- Breech BirthDocument10 pagesBreech Birthcirlce:twoworldsconnectedNo ratings yet
- My Courses: Home UGRD-PHYED6101-2113T Week 2: Health-Related Fitness Components Prelim Quiz 1Document4 pagesMy Courses: Home UGRD-PHYED6101-2113T Week 2: Health-Related Fitness Components Prelim Quiz 1Miguel Angelo GarciaNo ratings yet
- NBME Form 1 Step 2 ReviewDocument77 pagesNBME Form 1 Step 2 Reviewalex karevNo ratings yet
- B3223Document45 pagesB3223Irwan Meidi LubisNo ratings yet
- Medical Treatment of Aortic Stenosis: in DepthDocument19 pagesMedical Treatment of Aortic Stenosis: in DepthAlexandra NalgomNo ratings yet
- Research Made EasyDocument74 pagesResearch Made EasygloriacunananNo ratings yet
- FULL Download Ebook PDF Introduction To One Health An Interdisciplinary Approach To Planetary Health PDF EbookDocument41 pagesFULL Download Ebook PDF Introduction To One Health An Interdisciplinary Approach To Planetary Health PDF Ebookvalerie.iribarren889100% (35)
- Metformin Use in Polycystic Ovary Syndrome (PCOS)Document2 pagesMetformin Use in Polycystic Ovary Syndrome (PCOS)matasatuNo ratings yet
- OET Nursing Case Notes: Introducing Maeve GreersonDocument2 pagesOET Nursing Case Notes: Introducing Maeve GreersonLigy GeorgeNo ratings yet
- 22 CR Protean NeurologicalDocument2 pages22 CR Protean NeurologicalCamii CvNo ratings yet
- Peme Invitation 2021Document18 pagesPeme Invitation 2021hernie w. vergel de dios jrNo ratings yet
- 9966 Cons enDocument225 pages9966 Cons enOmz DonNo ratings yet
- NCP BathingDocument3 pagesNCP BathingNICOLE TOLENTINONo ratings yet
- NIC Claim FormDocument4 pagesNIC Claim FormImtiazNo ratings yet
- Midterm Surgery PYQsDocument77 pagesMidterm Surgery PYQs6vqk4z8wnhNo ratings yet
- Two Brain Business Ultimate Biz Plan FInal 4Document35 pagesTwo Brain Business Ultimate Biz Plan FInal 4Adrian TorresNo ratings yet