Professional Documents
Culture Documents
Outline: (Trans) Lesson 4: Imci Summary
Uploaded by
Abish Julienne Pecundo0 ratings0% found this document useful (0 votes)
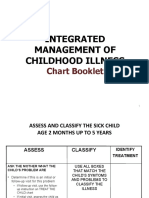
12 views2 pagesThe document outlines the IMCI (Integrated Management of Childhood Illness) case management process for assessing, classifying, and treating children under 5 for common illnesses like diarrhea, fever, and malnutrition. It describes assessing children for danger signs and main symptoms, classifying their condition as severe, moderate, or mild based on strategic assessment words, and treating conditions like dehydration either at home or as an outpatient. The process is similar to the nursing process of assessing, diagnosing, planning treatment, implementing it, and evaluating the patient.
Original Description:
IMCI MANILA TYTANA COLLEGES TRANS
Original Title
IMCI SUMMARY
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe document outlines the IMCI (Integrated Management of Childhood Illness) case management process for assessing, classifying, and treating children under 5 for common illnesses like diarrhea, fever, and malnutrition. It describes assessing children for danger signs and main symptoms, classifying their condition as severe, moderate, or mild based on strategic assessment words, and treating conditions like dehydration either at home or as an outpatient. The process is similar to the nursing process of assessing, diagnosing, planning treatment, implementing it, and evaluating the patient.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
12 views2 pagesOutline: (Trans) Lesson 4: Imci Summary
Uploaded by
Abish Julienne PecundoThe document outlines the IMCI (Integrated Management of Childhood Illness) case management process for assessing, classifying, and treating children under 5 for common illnesses like diarrhea, fever, and malnutrition. It describes assessing children for danger signs and main symptoms, classifying their condition as severe, moderate, or mild based on strategic assessment words, and treating conditions like dehydration either at home or as an outpatient. The process is similar to the nursing process of assessing, diagnosing, planning treatment, implementing it, and evaluating the patient.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 2
RLE\POWERPOINT
[TRANS] LESSON 4: IMCI SUMMARY
DIARRHEA 2 or More 2 or More
OUTLINE • Pinched goes • Pinched
I IMCI Case Management Process back very goes
A Assess slowly (>2 back
B Classify secs) slowly
C Treat • Unable to • Drinking
D Follow up
drink or eagerly/
breastfeed thirsty
IMCI CASE MANAGEMENT PROCESS • Sunken Eyes • Sunken
• The following steps can be observed when caring for children • Abnormally eyes
less than 5 years old who visits RHU or out-patient department sleepy or • Irritable
of a hospital for consultation. lethargic or
• You should always ACT (Assess, Classify and Treat). restless
• They are similar with the phase of nursing process
Diarrhea
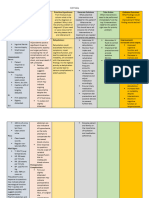
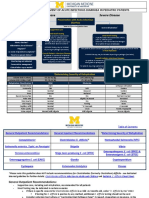
Table No.1 IMCI vs Nursing Process Diarrhea greater greater than
IMCI CASE MANAGEMENT PROCESS NURSING PROCESS than 14 days with 14 days
Assess Assess signs of without signs
Classify Diagnose dehydration of
Treat Plan dehydration
• Identify the treatment
• Treat the child Implement
• Counsel the mother Evaluate • Blood in
• Follow-up care the stool
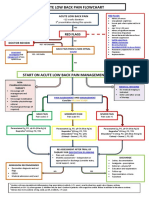
ASSESS FEVER Malaria Malaria
• Interview: ASK Stiff Neck (+) blood
o What’s the child’s problem? smear
o Initial or follow-up visit?
• Observe: LOOK, LISTEN AND FEEL Measles Measles
o DANGER SIGNS (VUCA) • Clouding of • Pus
Vomiting the cornea drainage in
Unable to drink or breastfeed • Extensive the eyes
Convulsions Mouth Ulcers • Mouth
Abnormally sleepy or lethargic Ulcers
o MAIN SYMPTOMS (CDFE) Dengue
Cough Hemorrhagic Fever
Diarrhea
Fever (4Ps)
Ear problem • Persistent
o OTHER PROBLEMS vomiting
Malnutrition • Persistent
Anemia abdominal
Immunization Status pain
Deworming Status • Positive
Feeding Problem tourniquets
• Petechiae
CLASSIFY
• Based on the group of signs and symptoms (2Cs)
• Color Coding Triage (PINK, YELLOW, GREEN) • Cold clammy
• To facilitate our classification, ASSESS for the following extremities
STRATEGIC WORDS • Capillary refill
• Note: one sign in pink row and one sign in yellow row is >3 secs
classified as SEVERE (PINK)
(S&S of Bleeding)
Table No.2 Classification: A Summary • Epistaxis
DANGER PINK YELLOW GREEN • Bleeding gum
SIGNS (SEVERE) (MODERATE; (MILD; • Hematemesis
DHN: SOME) DHN:NO) • Melena
COUGH • Stridor Fast No or
• Chest Breathing Inadequate
indrawing • 2-11 Signs and EAR Tender swelling • Pus
mos: 50 symptoms PROBLEM drainage on
bpm or the ear less
more than 14 days
• 12-59
mos 40 • or
bpm or greater
more than 14
days
ALCALA. IBARRA. MARIANO. ONG. PECUNDO. PERALTA. RICO. 1
[TRANS] LESSON 4: IMCI SUMMARY
MALNUTRI • Severe Muscle Very low TREATMENT FOR DEHYDRATION
-TION Wasting weight for
• Edema on age • PLAN A (HOME MANAGEMENT)
both feet RULE OF HOME MANAGEMENT
• If 6 mos and o Continue feeding the child
above MUAC o Give extra fluid
<115 cm <2 y/o: 50-100 ml ORS/LBM
ANEMIA Severe Palmar Some Palmar >2 y/o: 100-200 ml ORS/LBM
Pallor Pallor o Zinc supplement for 14 days
o Advise mother when to return
• PLAN B (OUT-PATIENT)
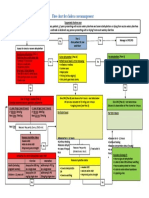
TREAT o Solution: ORS (Oral Rehydration Salts)
• Based on classification o Amount: 75 ml/kg in 4 hours
If <6 mos : give 100-200 ml of clean water to
Table No.3 General Treatment Plan prevent hypernatremia
URGENT/REFERAL OUT-PATIENT HOME If the child vomits, wait 10 minutes before
MANAGEMENT giving again fluids
• 1st dose of • 1st dose of • DHN: Plan A • PLAN C (SEVERE)
appropriate appropriate • Vitamin A o Solution: LRS (Lactated Ringer Solution) or PNSS
(infection) (infection) (measles) (Plain Normal Saline Solution)
• Treat low • DHN: Plan B • Advise the o Amount: 100ml/kg
blood sugar • Vitamin A mother when
• DHN: Plan C • Advise the to return
30 ml/kg 70 ml/kg
• Vitamin A mother when immediately
<1 /0 1 hour 5 hours
• Counsel the to return • Follow up
>1 y/o 30 minutes 2.5 hours
mother immediately
• Follow up
VITAMIN A
• Supplementation: THE 6-6-6 RULE
SPECIFIC TREATMENTS o Starts at 6 months, end at 6 years old and at least 6
• PRE-REFERRAL ANTIBIOTCS months of minimum interval
o 1st line: Gentamicin (7.5 mg/kg) • Treatment: 2day, 2morrow, 2weeks After Rule
o 2nd line: Benzyl Penicillin (50,000 units/kg) o Same dosage as below
o Sever Malaria: Quinine
AGE DOSE INTERVAL
Table No.4 Oral Antibiotics 6 mos – 11 mos 100,000 IU
DISEASE 1ST LINE 2ND LINE 12 mos – 6 y/o 200,000 IU Every 6 mos
PNEUMONIA Amoxicillin bid x 3 days Co-trimoxazole bid ADVISE THE MOTHER WHEN TO RETURN
x 3 days • If the child is not able to drink or breastfeed
ACUTE EAR Amoxicillin bid x 5 days Co-trimoxazole bid • If child becomes sicker
INFECTION x 5 days • If child develops fever
CHOLERA Tetracycline qid x 3 days Erythromycin qid x FOLLOW UP
3 days
*(given 2 y/o Table No.5 Follow-Up Plan
and above) DISEASE FOLLOW UP AFTER
if there is MALNUTRITION 30 days
cholera in ANEMIA 14 days
the area PENS 2 days – conditions other
DYSENTERY Ciprofloxacin bid x 3 • Persistent Diarrhea than mentioned above
days • Ear Infection
• No Pneumonia
MALARIA Artemeter-Lumefantrine Chloroquine, • Some/No Dehydration
Primaquine,
Sulfadoxine, and
Pyrimethamine
REFERENCES
OTIC ANTIBIOTICS
Notes from the discussion by Prof. Albert Jerom Y. Jopida RN
• Chronic Ear infection: Quinolone Drops
Manila Doctors Colleges of Nursing PowerPoint Presentation
TREAT LOW BLOOD SUGAR
• Continue breastfeeding
• Give expressed milk
• Sugar Water – Oresol (200ml clean water + 4 tsp of sugar)
ALCALA. IBARRA. MARIANO. ONG. PECUNDO. PERALTA. RICO. 2
You might also like
- Newborn Nursing Care Plan With ReferncesDocument6 pagesNewborn Nursing Care Plan With Referncesneuronurse92% (63)
- CJSS 11Document3 pagesCJSS 11j5khdwgywwNo ratings yet
- Management of The Sick Young Infant Age 1 Week Up To 2 MonthsüüüDocument3 pagesManagement of The Sick Young Infant Age 1 Week Up To 2 MonthsüüüJonah MaasinNo ratings yet
- Summary of IMCI Case ManagementDocument2 pagesSummary of IMCI Case Managementjanesky09100% (1)
- PEDIADocument16 pagesPEDIAMELANIE GALEDONo ratings yet
- CEM7213 Bronchiolitis Pathway Acute Care West Sussex Oct 2011Document2 pagesCEM7213 Bronchiolitis Pathway Acute Care West Sussex Oct 2011drgrizahNo ratings yet
- Acute Low Back Pain Flowchart January 2017Document1 pageAcute Low Back Pain Flowchart January 20171234chocoNo ratings yet
- Integrated Management of Childhood Illness: Chart BookletDocument81 pagesIntegrated Management of Childhood Illness: Chart BookletReadcast EFNo ratings yet
- Acute Abdominal Pain Pathway: Management - Primary Care and Community SettingsDocument2 pagesAcute Abdominal Pain Pathway: Management - Primary Care and Community Settingsshella1selinaNo ratings yet
- IMCIDocument6 pagesIMCIsnow.parconNo ratings yet
- Unit 2 Imnci BSCDocument67 pagesUnit 2 Imnci BSCNdina ElaoNo ratings yet
- IM JobAids 2005 06engDocument1 pageIM JobAids 2005 06engKeziah Marie Chua Santa-AnaNo ratings yet
- POPGUNS Benchmarque JTebomiDocument1 pagePOPGUNS Benchmarque JTebomistarwarsgladyNo ratings yet
- Appendix 11. Flow Chart For Cholera Case ManagementDocument1 pageAppendix 11. Flow Chart For Cholera Case ManagementGerard Pio Wee100% (1)
- IMCIDocument17 pagesIMCIapi-3707883No ratings yet
- Application of Nursing Process To Different Respiratory MedicationsDocument13 pagesApplication of Nursing Process To Different Respiratory MedicationssharedNo ratings yet
- F-IMNCI Chart BookletDocument45 pagesF-IMNCI Chart BookletGunda SrinivasNo ratings yet
- Recognition of Critically Ill ChildDocument58 pagesRecognition of Critically Ill ChildEmpat patimahNo ratings yet
- Fever in Children Dr. Red Dr. BantasanDocument2 pagesFever in Children Dr. Red Dr. Bantasanmaki RemularNo ratings yet
- ParkinsonsDocument2 pagesParkinsonspsyNo ratings yet
- ParkinsonsDocument2 pagesParkinsonspsyNo ratings yet
- Imci Booklet 69 70Document2 pagesImci Booklet 69 70Ivan MaximusNo ratings yet
- ETATModule 1 Lecture - TriageDocument59 pagesETATModule 1 Lecture - TriageDishani DeyNo ratings yet
- Evolve. Adapt. Overcome. Is Now ReadyDocument8 pagesEvolve. Adapt. Overcome. Is Now ReadyKarl Symon AmperNo ratings yet
- Health Problems Common in PRESCHOOLDocument15 pagesHealth Problems Common in PRESCHOOLJanelle Lois EscolanoNo ratings yet
- PALS Systematic Approach Summary: Initial ImpressionDocument2 pagesPALS Systematic Approach Summary: Initial ImpressionMark Vergel II100% (3)
- Tatalaksana Balita Sakit Umur 2 Bulan Sampai 5 Tahun: Jika YaDocument3 pagesTatalaksana Balita Sakit Umur 2 Bulan Sampai 5 Tahun: Jika YaMuhamad FandiNo ratings yet
- IMCIDocument7 pagesIMCImarlou agananNo ratings yet
- Paula George: Management of The Sick Child Aged 2 Months Up To 5 YearsDocument1 pagePaula George: Management of The Sick Child Aged 2 Months Up To 5 Yearsallkhusairy6tuansiNo ratings yet
- Imci Forms GuideDocument2 pagesImci Forms GuideFhey Bernadette BeltranNo ratings yet
- 2nd Preceptorials FinalDocument14 pages2nd Preceptorials FinalGabriel MillaNo ratings yet
- UAS Mtbs Tita Setiawati Rishqi 09180000043Document7 pagesUAS Mtbs Tita Setiawati Rishqi 09180000043Kezia MuskittaNo ratings yet
- Activity (Fever)Document8 pagesActivity (Fever)April NojaraNo ratings yet
- Integrated Management ofDocument39 pagesIntegrated Management ofABEGAIL BALLORANNo ratings yet
- Fever Measles Ear ProblemsDocument10 pagesFever Measles Ear ProblemsEBNo ratings yet
- Diarrhea PediaDocument10 pagesDiarrhea PediaSuneeth Kumar MohantyNo ratings yet
- Integratedhealt 150201183122 Conversion Gate02 PDFDocument145 pagesIntegratedhealt 150201183122 Conversion Gate02 PDFVhince PiscoNo ratings yet
- Imci Recording FormDocument4 pagesImci Recording Formxalwoqaali2018No ratings yet
- Integrated Management of Childhood IllnessesDocument7 pagesIntegrated Management of Childhood IllnessesMae Alexes TamañoNo ratings yet
- PMVPH 4 - Intro 2022Document14 pagesPMVPH 4 - Intro 2022DB “ByulHa” KimNo ratings yet
- Imci2007 Part 3Document57 pagesImci2007 Part 3api-3709260No ratings yet
- Immediate Care of The NewbornDocument19 pagesImmediate Care of The Newbornelijah aquinoNo ratings yet
- NicuDocument4 pagesNicuGiel Margareth LindoNo ratings yet
- Imci Recording Form 2Document3 pagesImci Recording Form 2Dea Sabelle Castro100% (1)
- Management of The Sick Child Aged 2 Months Up To 5 Years: ASSESS (Circle All Signs Present) ClassifyDocument1 pageManagement of The Sick Child Aged 2 Months Up To 5 Years: ASSESS (Circle All Signs Present) ClassifyCooky JeonNo ratings yet
- Operational Obstetrics & Gynecology Bureau of Medicine and Surgery 2000 Slide 1Document16 pagesOperational Obstetrics & Gynecology Bureau of Medicine and Surgery 2000 Slide 1Jhoana Rose Joaquin SantosNo ratings yet
- Management of The Sick Child Aged 2 Months Up To 5 Years: Severe DehydrationDocument2 pagesManagement of The Sick Child Aged 2 Months Up To 5 Years: Severe DehydrationMonique LeonardoNo ratings yet
- Pews Charts 4 11 MonthsDocument2 pagesPews Charts 4 11 MonthsKiara RevalinaNo ratings yet
- Integrated Management of Childhood IllnessesDocument65 pagesIntegrated Management of Childhood IllnessesJocel LañasNo ratings yet
- Diarrhea PEDSDocument10 pagesDiarrhea PEDSOasis LimitedNo ratings yet
- Examination: Short History Positioning of The PatientDocument1 pageExamination: Short History Positioning of The PatientAshan BopitiyaNo ratings yet
- SeizuresDocument1 pageSeizurestiraray30No ratings yet
- Imci Rec Form FinalDocument1 pageImci Rec Form FinalHecia Gaga-aNo ratings yet
- Checklist - IMCI-Sick Young ChildDocument3 pagesChecklist - IMCI-Sick Young ChildAriel Delos ReyesNo ratings yet
- Unit-Plan: Submitted By: Ms - Prerna SharmaDocument4 pagesUnit-Plan: Submitted By: Ms - Prerna SharmaPrernaSharma50% (2)
- Integrated Management of Childhood Illness 1Document4 pagesIntegrated Management of Childhood Illness 1Joseph Adrian Theodore TuyNo ratings yet
- Pews Charts 0 3 MonthsDocument2 pagesPews Charts 0 3 MonthsThiaNo ratings yet
- PediatricDocument10 pagesPediatrictalarashad2002No ratings yet
- The Complete Dysphagia Diet Cookbook:The Ultimate Nutrition Guide For People With Swallowing And Chewing Difficulties With Foodlist, Meal Plan And Nourishing RecipesFrom EverandThe Complete Dysphagia Diet Cookbook:The Ultimate Nutrition Guide For People With Swallowing And Chewing Difficulties With Foodlist, Meal Plan And Nourishing RecipesNo ratings yet
- Original PDF Dosage Calculations A Multi Method Approach 2nd PDFDocument41 pagesOriginal PDF Dosage Calculations A Multi Method Approach 2nd PDFwilbur.hensley96397% (38)
- Fluid Disturbance and Therapy 2021Document49 pagesFluid Disturbance and Therapy 2021Alfathri Yunedi100% (1)
- Acute Pancreatitis Treatment & ManagementDocument7 pagesAcute Pancreatitis Treatment & ManagementDicky SangadjiNo ratings yet
- Coconut Handbook PDFDocument187 pagesCoconut Handbook PDFDewika S.100% (1)
- Acute PancreatitisDocument58 pagesAcute PancreatitissujithNo ratings yet
- Dengue1234 PDFDocument20 pagesDengue1234 PDFdanielacorreia1919No ratings yet
- Maintenance Intravenous Fluid Therapy in Children - UpToDateDocument19 pagesMaintenance Intravenous Fluid Therapy in Children - UpToDaterolland_arrizaNo ratings yet
- Cholera: Presenter: Dr. Sohani Bajracharya Date: 26 February 2018Document32 pagesCholera: Presenter: Dr. Sohani Bajracharya Date: 26 February 2018Bajracharya SohaniNo ratings yet
- Introduction To Public Health Module # 6: Dr. Shaikh Abdus Salam Dept. of Public Health North South UniversityDocument142 pagesIntroduction To Public Health Module # 6: Dr. Shaikh Abdus Salam Dept. of Public Health North South UniversityUsama RahmanNo ratings yet
- Burns: Hadi Munib Oral and Maxillofacial SurgeryDocument79 pagesBurns: Hadi Munib Oral and Maxillofacial SurgeryAli ahmedNo ratings yet
- 9-12 BurnsDocument32 pages9-12 BurnsralukNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale: EvaluationDocument2 pagesAssessment Diagnosis Planning Intervention Rationale: EvaluationPotato BananaNo ratings yet
- Optimizing Fluid Therapy in Shock.10Document6 pagesOptimizing Fluid Therapy in Shock.10Paulo Victor100% (1)
- Shift Assessment of Nursing DocumentationDocument18 pagesShift Assessment of Nursing DocumentationQwequ Gong Ananse100% (3)
- SWBCN011-Guideline - Initial Assessment and Management Burn Injury v2Document8 pagesSWBCN011-Guideline - Initial Assessment and Management Burn Injury v2Thanujaa UvarajNo ratings yet
- Explanation: MRCS Part A - Sep 2019 ExamDocument46 pagesExplanation: MRCS Part A - Sep 2019 ExamHasan ManghiNo ratings yet
- Elia Jennifer Perioperative Fluid Management andDocument19 pagesElia Jennifer Perioperative Fluid Management andSiddhartha PalaciosNo ratings yet
- Sepsis 2021 A ReviewDocument9 pagesSepsis 2021 A ReviewvictorNo ratings yet
- 003 - DM - Acute ComplicationsDocument17 pages003 - DM - Acute ComplicationsLucas Victor AlmeidaNo ratings yet
- Resusitasi Cairan Dan DarahDocument33 pagesResusitasi Cairan Dan DarahWahyu HidayatiNo ratings yet
- Septic Shock in Children - Rapid Recognition and Initial Resuscitation (First Hour) PDFDocument18 pagesSeptic Shock in Children - Rapid Recognition and Initial Resuscitation (First Hour) PDFLilik NatasubrataNo ratings yet
- DiabetekDocument15 pagesDiabetekMaira GonzálezNo ratings yet
- First Aid Management For Common Life Threatening ConditionsDocument38 pagesFirst Aid Management For Common Life Threatening ConditionsBSN 2 - Sasis, Rusmaryte C.No ratings yet
- Fluid Volume DeficitDocument2 pagesFluid Volume DeficitpeternohibiNo ratings yet
- The Origin of IV FluidsDocument15 pagesThe Origin of IV Fluidsashley nicholeNo ratings yet
- Severe Hyperglycemia: Effects of Rehydration On Endocrine Derangements and Blood Glucose ConcentrationDocument8 pagesSevere Hyperglycemia: Effects of Rehydration On Endocrine Derangements and Blood Glucose Concentrationmohamadafif_drNo ratings yet
- Self-Assessment Colour Review OF Avian MedicineDocument193 pagesSelf-Assessment Colour Review OF Avian MedicineXimenaPantiPrieto100% (1)
- 15 - Supportive Care and Emergency TherapyDocument35 pages15 - Supportive Care and Emergency TherapyPeterNo ratings yet
- Contrast-Induced Nephropathy (CIN)Document42 pagesContrast-Induced Nephropathy (CIN)kkyyyhNo ratings yet
- Fluid Resuscitation in Acoute Pancreatitis - PrefinalDocument35 pagesFluid Resuscitation in Acoute Pancreatitis - PrefinalSahir BNo ratings yet