Professional Documents
Culture Documents
MANAGEMENT OF ACUTE ASTHMA ATTACKS IN ADULTS
Uploaded by
Massimo Di BenedettoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
MANAGEMENT OF ACUTE ASTHMA ATTACKS IN ADULTS
Uploaded by
Massimo Di BenedettoCopyright:
Available Formats
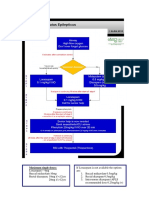
MANAGEMENING ACUTE ASTHMA IN ADULTS IN HOSPITAL
Features of acute severe asthma Immediate treatment
• Peak expiratory flow (PEF) 33–50% • Oxygen to maintain SpO2 94–98%
of best (use % predicted if recent best • β2 Bronchodilator (Salbutamol 5 mg) via an oxygen-driven nebuliser
unknown) • Ipratropium Bromide 0.5 mg via an oxygen-driven nebuliser
• Can’t complete sentences in one breath • Prednisolone tablets 40–50 mg or IV Hydrocortisone 100 mg
• Respiration ≥25 breaths/min • No sedatives of any kind
• Pulse ≥110 beats/min • Chest X-ray if pneumothorax or consolidation are suspected or patient requires
Life-threatening features mechanical ventilation
• PEF <33% of best or predicted If life-threatening features are present:
• SpO2 <92% • Discuss with senior clinician and ICU team
• Silent chest, cyanosis, or poor • Consider IV magnesium sulphate 1.2–2 g infusion over 20 minutes (unless already
respiratory effort given)
• Arrhythmia or hypotension • Give nebulised β2 bronchodilator more frequently eg. Salbutamol 5 mg up to every
15-30 minutes or 10 mg per hour via continuous nebulisation (requires special
• Exhaustion, altered consciousness nebuliser)
If a patient has any life-threatening Subsequent management
feature, measure arterial blood gases.
if patient is improving continue:
No other investigations are needed for
immediate management. • Oxygen to maintain SpO2 94–98%
Blood gas markers of a life-threatening • Prednisolone 40–50mg daily or IV hydrocortisone 100 mg 6 hourly
attack: • Nebulised β2 bronchodilator with ipratropium 4–6 hourly
• ‘Normal’ (4.6–6 kPa, 35–45 mmHg) If patient not improving after 15–30 minutes:
PaCO2
• Continue oxygen and steroids
• Severe hypoxia: PaCO2 <8 kPa
• Use continuous nebulisation of salbutamol at 5–10 mg/hour if an appropriate
(60 mmHg) irrespective of treatment
nebuliser is available. Otherwise give nebulised salbutamol 5 mg every 15–30
with oxygen
minutes
• A low pH (or high H+)
• Continue ipratropium 0.5 mg 4–6 hourly until patient is improving
Caution: Patients with severe or
If patient is still not improving:
life-threatening attacks may not be
distressed and may not have all these • Discuss patient with senior clinician and ICU team
abnormalities. The presence of any • Consider IV magnesium sulphate 1.2–2 g over 20 minutes (unless already given)
should alert the doctor. • Senior clinician may consider use of IV β2 bronchodilator or IV aminophylline or
progression to mechanical ventilation
Near-fatal asthma
• Raised PaCO2
Monitoring
• Requiring mechanical ventilation with • Repeat measurement of PEF 15–30 minutes after starting treatment
raised inflation pressures
• Oximetry: maintain SpO2 94–98%
• Repeat blood gas measurements within 1 hour of starting treatment if:
Peak Expiratory Flow Rate - Normal Values - initial PaO2 <8 kPa (60 mmHg) unless subsequent SpO2 >92% or
- PaCO2 normal or raised or
- patient deteriorates
• Chart PEF before and after giving β2 bronchodilator and at least 4 times daily throughout
hospital stay
Transfer to ICU accompanied by a doctor prepared to intubate if:
• Deteriorating PEF, worsening or persisting hypoxia, or hypercapnia
• Exhaustion, altered consciousness
• Poor respiratory effort or respiratory arrest
Discharge
When discharged from hospital, patients should have:
• Been on discharge medication for 12–24 hours and have had inhaler technique checked and
recorded
• PEF >75% of best or predicted and PEF diurnal variability <25% unless discharge is agreed
with respiratory physician
• Treatment with oral steroids (prednisolone 40–50 mg until recovery - minimum 5 days) and
inhaled steroids in addition to bronchodilators
• Own PEF meter and written asthma action plan
• GP follow up arranged within 2 working days
• Follow-up appointment in respiratory clinic within 4 weeks
Patients with severe asthma (indicated by need for admission) and adverse behavioural or
psychosocial features are at risk of further severe or fatal attacks.
• Determine reason(s) for exacerbation and admission
• Send details of admission, discharge and potential best PEF to GP
BTS/SIGN Guideline for the management of asthma 2019. Reproduced with permission
You might also like
- Asthma Clinical Care GuidelinesDocument17 pagesAsthma Clinical Care GuidelinesWalaa MoustafaNo ratings yet
- Guidelines For First-Line Empirical Antibiotic Therapy in AdultsDocument1 pageGuidelines For First-Line Empirical Antibiotic Therapy in AdultsAnonymous s4yarxNo ratings yet
- Medical Encyclopedia XXL: Prof. J.P. Schadé, M.D., Ph.D. D.Sc.hcFrom EverandMedical Encyclopedia XXL: Prof. J.P. Schadé, M.D., Ph.D. D.Sc.hcNo ratings yet
- Occupational Therapy Practice Framework: Domain and Process Fourth Edition (2020)Document87 pagesOccupational Therapy Practice Framework: Domain and Process Fourth Edition (2020)Susana Ahumada100% (1)
- HUMAN REPRODUCTION-1 Madhu - QuestionDocument69 pagesHUMAN REPRODUCTION-1 Madhu - QuestionAyan Sarkar100% (1)
- COPD Exacerbation Management Primary CareDocument1 pageCOPD Exacerbation Management Primary Caremufidah mawaddahNo ratings yet
- 4 Weaning Ventilator-NIADocument31 pages4 Weaning Ventilator-NIAResyana Widyayani100% (1)
- Status AsthmaticusDocument18 pagesStatus AsthmaticusUmar Azlan0% (1)
- Critical Care Management of Acute Severe AsthmaDocument53 pagesCritical Care Management of Acute Severe AsthmaYohana SepthiyaNo ratings yet
- The Kübler-Ross Change Curve: Emotional Response To ChangeDocument9 pagesThe Kübler-Ross Change Curve: Emotional Response To ChangeChanel PostelNo ratings yet
- Natural Ways To Treat Hydrosalpinx (Blocked Fallopian Tube)Document11 pagesNatural Ways To Treat Hydrosalpinx (Blocked Fallopian Tube)drleetcmclinicNo ratings yet
- Recovery Room Care: BY Rajeev KumarDocument50 pagesRecovery Room Care: BY Rajeev Kumarramanrajesh83No ratings yet
- Poisoning II FinalDocument45 pagesPoisoning II FinalBi PinNo ratings yet
- Laporan Pendahuluan Polycystic Ovarian Syndrome (PCOS)Document14 pagesLaporan Pendahuluan Polycystic Ovarian Syndrome (PCOS)Jali24No ratings yet
- Emergency Neurological Life Support Status Epilepticus ProtocolDocument12 pagesEmergency Neurological Life Support Status Epilepticus ProtocolFransiskus MikaelNo ratings yet
- Special 13 BTS SIGN AsthmaDocument1 pageSpecial 13 BTS SIGN AsthmacositaamorNo ratings yet
- Prescriptions On Asthma & APDDocument9 pagesPrescriptions On Asthma & APDeesha shahNo ratings yet
- Acute Asthma ExacerbationDocument28 pagesAcute Asthma ExacerbationMike singhNo ratings yet
- 01 - Bronchial AsthmaDocument6 pages01 - Bronchial AsthmaFrank VaronaNo ratings yet
- Patient Management Flow Chart: Appt W/ Bronchoscopist PFT/ P&H/StabilityDocument7 pagesPatient Management Flow Chart: Appt W/ Bronchoscopist PFT/ P&H/StabilityKinnari PatelNo ratings yet
- Ventilator Management ProtocolDocument15 pagesVentilator Management Protocolihtisham1No ratings yet
- Acute Severe Asthma Hospital ManagementDocument1 pageAcute Severe Asthma Hospital ManagementItharshan IndreswaranNo ratings yet
- NIV ProformaDocument10 pagesNIV ProformaWael N Sh GadallaNo ratings yet
- Acute Asthma Bts 2011 QRCDocument2 pagesAcute Asthma Bts 2011 QRCJustin AuchwitzNo ratings yet
- FINAL COVID19 1 April 2021Document14 pagesFINAL COVID19 1 April 2021Wleed KhledNo ratings yet
- Asthma EmergencyDocument20 pagesAsthma EmergencyJanice Shaileen KrishnaNo ratings yet
- Pediatric Asthma Pathway GuideDocument2 pagesPediatric Asthma Pathway GuideIswa AsyharNo ratings yet
- Status Epilepticus: Kenya Medical Training CollegeDocument21 pagesStatus Epilepticus: Kenya Medical Training CollegeSalman KhanNo ratings yet
- COPDDocument20 pagesCOPDعزالدين الزوقريNo ratings yet
- Management of Convulsions After The Neonatal Period: DR NgugiDocument22 pagesManagement of Convulsions After The Neonatal Period: DR NgugitheintrovNo ratings yet
- Propofol 2Document22 pagesPropofol 2Bhaskar PendyalaNo ratings yet
- Peak Expiratory Flow RateDocument35 pagesPeak Expiratory Flow RateLiya RafeekhNo ratings yet
- RBCH - PHT Aminophylline Loading Dose GuidelinesDocument2 pagesRBCH - PHT Aminophylline Loading Dose GuidelinesAdrian PrasetioNo ratings yet
- COVID-19 Management ProtocolDocument13 pagesCOVID-19 Management ProtocolajiNo ratings yet
- Acute Exacerbation of Copd & Status AsthmaticusDocument59 pagesAcute Exacerbation of Copd & Status AsthmaticusSaras SinghNo ratings yet
- Management of Asthma Exacerbations: Key Points: Early Treatment Is Best. Important Elements IncludeDocument47 pagesManagement of Asthma Exacerbations: Key Points: Early Treatment Is Best. Important Elements IncludeEmilio Fernandez CenturiónNo ratings yet
- Managing Respiratory InfectionsDocument13 pagesManaging Respiratory InfectionsPangestu DhikaNo ratings yet
- AIIMS/ ICMR-COVID-19 National Task Force/ Joint Monitoring Group (Dte - GHS) Ministry of Health & Family Welfare, Government of IndiaDocument1 pageAIIMS/ ICMR-COVID-19 National Task Force/ Joint Monitoring Group (Dte - GHS) Ministry of Health & Family Welfare, Government of IndiaSomnath Das GuptaNo ratings yet
- Sepsis and Septic Shock Management Guidelines 2019: Insp. Dr. Sunder Chapagain Nepal APF Hospital KathmanduDocument33 pagesSepsis and Septic Shock Management Guidelines 2019: Insp. Dr. Sunder Chapagain Nepal APF Hospital KathmanduKHAIRUL REDZUANNo ratings yet
- Guideline for managing eclampsia and severe pre-eclampsiaDocument15 pagesGuideline for managing eclampsia and severe pre-eclampsiaCitra KristiNo ratings yet
- Acute Pyelonephritis Treatment GuidelinesDocument4 pagesAcute Pyelonephritis Treatment GuidelinesPeter InocandoNo ratings yet
- Management Guidelines For COVID 19 in Resource Limited Settings - MOH - NUG July 2021Document11 pagesManagement Guidelines For COVID 19 in Resource Limited Settings - MOH - NUG July 2021MYo OoNo ratings yet
- AIIMS Issues New Guidelines For Treatment of CovidDocument7 pagesAIIMS Issues New Guidelines For Treatment of Covidsenthil kumarNo ratings yet
- Farmakoterapi Pada SepsisDocument36 pagesFarmakoterapi Pada SepsisNathaniaNo ratings yet
- Common Medical Emergencies 3 (Autosaved)Document55 pagesCommon Medical Emergencies 3 (Autosaved)Alex XanderNo ratings yet
- Should Be Available at All Sites If Feasible, Include at Sites (Not Required)Document5 pagesShould Be Available at All Sites If Feasible, Include at Sites (Not Required)Ahmed QlhamdNo ratings yet
- CovidDocument31 pagesCovidShaheen SultanNo ratings yet
- Medicine RotatationbookletDocument20 pagesMedicine RotatationbookletJanelle JosephsNo ratings yet
- UNC ED Pediatric Asthma ProtocolDocument2 pagesUNC ED Pediatric Asthma ProtocolAhmed BekhetNo ratings yet
- Status Epilepticus - APLSDocument3 pagesStatus Epilepticus - APLSMuhammadafif SholehuddinNo ratings yet
- Assessment and Management OF Acute Severe AsthmaDocument43 pagesAssessment and Management OF Acute Severe Asthmadentist40No ratings yet
- Sedation and Analgesia in PicuDocument37 pagesSedation and Analgesia in PicubhoopendraNo ratings yet
- Bronchial Asthma Diagnosis and Treatment PlanDocument35 pagesBronchial Asthma Diagnosis and Treatment PlanMichael BusiaNo ratings yet
- Organophosphate Poisoning 2Document12 pagesOrganophosphate Poisoning 2Diana MurguiaNo ratings yet
- OpioidsDocument35 pagesOpioidsDr-Mohammad Ali-Fayiz Al TamimiNo ratings yet
- Protocol For in Patient Status Epilepticus in Adults (Includes Convulsive and Non-Convulsive Status Epilepticus)Document3 pagesProtocol For in Patient Status Epilepticus in Adults (Includes Convulsive and Non-Convulsive Status Epilepticus)BarneyNo ratings yet
- AIIMS issues new guidelines for treatment of Covid-19 casesDocument7 pagesAIIMS issues new guidelines for treatment of Covid-19 casessenthil kumarNo ratings yet
- Acute Severe Asthma in AdultsDocument3 pagesAcute Severe Asthma in AdultssobanNo ratings yet
- Management of acute asthma in children in Emergency DepartmentDocument1 pageManagement of acute asthma in children in Emergency Departmentdr.spartaNo ratings yet
- Salbutamol for Asthma and COPD ReliefDocument5 pagesSalbutamol for Asthma and COPD ReliefFildehl Janice Bomediano CatipayNo ratings yet
- ACUTE ASTHMA ATTACK EMERGENCY TREATMENTDocument31 pagesACUTE ASTHMA ATTACK EMERGENCY TREATMENTMuneeb YounisNo ratings yet
- COVID-19 Treatment GuidelinesDocument26 pagesCOVID-19 Treatment GuidelinesStonefalconNo ratings yet
- Based On The Case, Assess The Patient's Asthma Control According To The Two Domains: 1. Symptom Control 2. Future Risk of Adverse OutcomesDocument7 pagesBased On The Case, Assess The Patient's Asthma Control According To The Two Domains: 1. Symptom Control 2. Future Risk of Adverse OutcomesNicole BaysaNo ratings yet
- Guideline For Management Protocol of Children With Fever and Respiratory SymptomsDocument44 pagesGuideline For Management Protocol of Children With Fever and Respiratory SymptomsKushagr GautamNo ratings yet
- Ephedrine & Phenylephrine 2Document27 pagesEphedrine & Phenylephrine 2Sabrina ShalhoutNo ratings yet
- Traumatic Cardiac Arrest Resuscitation AlgorithmDocument1 pageTraumatic Cardiac Arrest Resuscitation AlgorithmMassimo Di BenedettoNo ratings yet
- 7.5 Post Resus Algorithms 2Document1 page7.5 Post Resus Algorithms 2Massimo Di BenedettoNo ratings yet
- Education 4Document1 pageEducation 4Massimo Di BenedettoNo ratings yet
- Education 2Document1 pageEducation 2Massimo Di BenedettoNo ratings yet
- 7.2post Resus Algorithms 1Document1 page7.2post Resus Algorithms 1Massimo Di BenedettoNo ratings yet
- 7.6 Post Resus Algorithms 3Document1 page7.6 Post Resus Algorithms 3Massimo Di BenedettoNo ratings yet
- Cardiac Surgery: 1. Prevent and Be PreparedDocument1 pageCardiac Surgery: 1. Prevent and Be PreparedMassimo Di BenedettoNo ratings yet
- 6.10 CPR Spec Circs Algorithms 6Document1 page6.10 CPR Spec Circs Algorithms 6Massimo Di BenedettoNo ratings yet
- Paediatric Basic Life Support: Nresponsive?Document1 pagePaediatric Basic Life Support: Nresponsive?Massimo Di BenedettoNo ratings yet
- 5.ALS Algorithms TachycardiaDocument1 page5.ALS Algorithms TachycardiaMassimo Di BenedettoNo ratings yet
- Suspect Foreign Body Airway ObstructionDocument1 pageSuspect Foreign Body Airway ObstructionMassimo Di BenedettoNo ratings yet
- Rare Case of Sirenomelia Congenital AnomalyDocument3 pagesRare Case of Sirenomelia Congenital Anomalymahesh shindeNo ratings yet
- IBH 6111 Final PresentationDocument13 pagesIBH 6111 Final PresentationSidney OxboroughNo ratings yet
- Physiologic Function and Appearance of The NewbornDocument5 pagesPhysiologic Function and Appearance of The NewbornJanelle Cabida SupnadNo ratings yet
- Nursing Standard PrinciplesDocument2 pagesNursing Standard PrinciplesRoscelie KhoNo ratings yet
- Cure Disease: Charred Skeever Hide Felsaad Tern Feathers Hawk Feathers Mudcrab Chitin Vampire DustDocument5 pagesCure Disease: Charred Skeever Hide Felsaad Tern Feathers Hawk Feathers Mudcrab Chitin Vampire DustFarsiko Risma YandiNo ratings yet
- Ocean Quest SSD Trainer Manual 2020Document109 pagesOcean Quest SSD Trainer Manual 2020Carmen LuckNo ratings yet
- CIL Recruitment for 66 Medical Executive PostsDocument12 pagesCIL Recruitment for 66 Medical Executive PostsTaseemNo ratings yet
- Prof Prac 2 EssayDocument3 pagesProf Prac 2 EssayEryka DyenghongNo ratings yet
- German Healthcare Exam Prep CourseDocument1 pageGerman Healthcare Exam Prep CourseANJIMA JOYNo ratings yet
- Problem and Its BackgroundDocument7 pagesProblem and Its BackgroundErika Chloe H. YabutNo ratings yet
- Neurotoxicity of Local Anesthetics in DentistryDocument7 pagesNeurotoxicity of Local Anesthetics in DentistryVinicíus PavaniNo ratings yet
- Carestation 600 SeriesDocument3 pagesCarestation 600 SeriesABHINANDAN SHARMANo ratings yet
- f3 Home-Sci Simplified Notes SPDocument20 pagesf3 Home-Sci Simplified Notes SPmicah isabokeNo ratings yet
- Importance of Sustainable Development GoalsDocument2 pagesImportance of Sustainable Development GoalsDyas FerNo ratings yet
- Accomplishment Report: Municipality of NarvacanDocument3 pagesAccomplishment Report: Municipality of Narvacanuser computerNo ratings yet
- BA Euroflyer Direct Entry Pilot - Captain A320 at British AirwaysDocument1 pageBA Euroflyer Direct Entry Pilot - Captain A320 at British AirwaysdifjdjdjNo ratings yet
- Debate US Initial Release Single Use PlasticsDocument226 pagesDebate US Initial Release Single Use Plasticsnamtran1066No ratings yet
- 12 SM 2017 Biology EngDocument206 pages12 SM 2017 Biology EngJaiminGajjar100% (1)
- Oral Surgery Maxill - Anesthesia TechniquesDocument4 pagesOral Surgery Maxill - Anesthesia TechniquesSaif AyedNo ratings yet
- Effect of Ethanol Leaf Extract of Chromolaena Odorata On Lipid Profile of Streptozotocin Induced Diabetic Wistar Albino RatsDocument9 pagesEffect of Ethanol Leaf Extract of Chromolaena Odorata On Lipid Profile of Streptozotocin Induced Diabetic Wistar Albino RatsPUBLISHER JOURNALNo ratings yet
- Graded RecitationDocument22 pagesGraded RecitationClara MaeNo ratings yet
- An Analysis of The Mercury Content of The Water and Life Forms in Manila Bay (Cavite Area)Document24 pagesAn Analysis of The Mercury Content of The Water and Life Forms in Manila Bay (Cavite Area)Jesse Nicole SantosNo ratings yet
- Reflective Practice JournalDocument5 pagesReflective Practice JournalReuben RussellNo ratings yet
- Growing Uganda's mushroom farming industryDocument2 pagesGrowing Uganda's mushroom farming industrymaboni ismaelNo ratings yet
- Cardiology Dr. Payawal UltimateDocument9 pagesCardiology Dr. Payawal UltimateSven OrdanzaNo ratings yet