Professional Documents
Culture Documents
EMCrit Lae Pulmonary Flow
Uploaded by
hmsptrOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
EMCrit Lae Pulmonary Flow
Uploaded by
hmsptrCopyright:
Available Formats
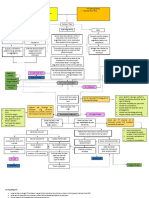
EMCrit RACC Pulmonary Embolism Pathway
Vascular Consult if Notes:
Order Bilateral Dopplers of Legs
HIGH BLEEDING RISK: POSITIVE CTPA OR HIGH PROBABILTY V/Q SCAN Contraindication to
(if suspicion, consider UE as well) pos
Anticoagulation with Proximal LE ▪ Proximal clot=Filling defect in
1. Any Prior ICH DVT lobar or more proximal artery
2. Known structural intracranial ▪ RV dysfunction on echo findings
cerebrovascular disease (e.g., avm) Risk stratify based on vital signs, CTPA include: dilated and/ or
3. Known malignant intracranial findings, BNP, troponin and hypokinetic RV, septal flattening
neoplasm bedside echo or bowing
4. Ischemic stroke within the past 3 ▪ If IV thrombolysis or catheter-
months directed treatment anticipated,
5. Suspected Aortic Dissection NON-MASSIVE [ LOW RISK ] PE: SUBMASSIVE WITH RV STRAIN MASSIVE [HIGH RISK ] PE: prefer UFH administration and if
6. Active, non-compressible [ INTERMEDIATE RISK ] you know you will be
bleeding Normotensive contemplating thrombolysis,
Proximal clot and:
7. Known inherited or acquired without RV strain
SBP < 90 mmHg/MAP <65 for > 15 consider holding initial heparin
bleeding disorder, e.g., hemophilia, Normotensive, proximal clot Min or 40 mmHg drop from ▪ Stop heparin drip during
platelet count <50,000/uL, or liver and: baseline; or profound bradycardia administration of tPA. Recheck
failure with prothrombin time RV>LV on CTPA or RV dysfunction (<40 bpm) PTT immediately after tPA infusion
abnormal (INR > 1.7) on echo
HEPARIN is complete. When PTT < 2 x ULN,
8. Surgery that required opening of ANTICOAGULATION restart heparin drip WITHOUT
the chest cavity, peritoneum, skull, or (LMWH Preferred) bolus at same rate as before tPA
spinal canal within the previous 14 was started. Consider waiting until
days UNFRAC HEPARIN UNFRAC HEPARIN fibrinogen returns to normal
9. Recent significant closed-head or ANTICOAGULATION (see notes) ANTICOAGULATION (see notes) levels as well before restarting
facial trauma with radiographic heparin.
evidence of bony fracture or brain
injury
ADMIT TO INTERNAL
MEDICINE EVIDENCE OF SHOCK OR
(consider Discharge) RESPIRATORY FAILURE:
consider
MODERATE BLEEDING RISK:
Episodic hypotension
SBP (<90mmHg or MAP<65)
1. Age >70 years (AHA uses >75) OR ASSESS BLEEDING RISK
ACTIVATE
2. Current use of anticoagulation HR/SBP consistently > 1.0 Code PE
3. Pregnancy (Consult OB) OR
4. Noncompressible vascular Respiratory Distress or SpO2 <
punctures 90% on ≥ 6 L NC
5. Traumatic or prolonged MICU Consult
**Monitor for Note: Also consider further HIGH Moderate LOW
cardiopulmonary resuscitation (>10 PERT TEAM
worsening therapies in patients with elevated
minutes) CONSULT lactate or troponin depending on
respiratory and
6. Recent internal bleeding (within 2 (Pulm Fellow) bleeding risk
hemodynamic
to 4 weeks) status**
7. Remote (>3 months) ischemic
stroke
Depending on Severity:
8. Major surgery within 3 weeks. Depending on Severity and ▪ Alteplase 50 mg over 1
9. Uncontrollable hypertension: Bleeding Risk: hour
SBP>180 or DBP > 100, despite anti- ASSESS BLEEDING RISK ▪ Alteplase 25 mg over 6 hours ▪ Alteplase 100 mg over
hypertensive treatment ▪ Alteplase 50 mg over 1 hour 2 hours
10. Metastatic cancer (consider Head ▪ Alteplase 100 mg over 2 ▪ Weight-Based
CT in any cancer patient) Alteplase 50 mg over 1 hours Tenecteplase (Peri-
11. Head trauma causing loss of hour ACTIVATE ▪ Weight-Based Tenecteplase Code or Coding)
or CODE PE (Peri-Code or Coding)
consciousness within previous 7 days LOW MODERATE HIGH
(Get a Head CT) Alteplase 25 Mg over 6
12. Large Pericardial Effusion Hours
Persistent
Consider: Hypotension or
Alteplase 25 mg over 6 Consider advanced therapy Hypoxemia
Hours options [open embolectomy,
If CDT Needed
or endovascular embolectomy,
Catheter Directed CDT, ECMO]
Therapies
Version 0.9 2021-09-22
Inspired by North Carolina Medical Center Protocol
You might also like
- VSIM Clinical Worksheet 07.10.2020Document6 pagesVSIM Clinical Worksheet 07.10.2020Jackie Griffis100% (1)
- Palliative and Hospice CareDocument61 pagesPalliative and Hospice Careeinjjereu xxiNo ratings yet
- ST Elevation MI, STEMIDocument3 pagesST Elevation MI, STEMInmyza89No ratings yet
- M) IV Anticoagulation M) Arterial Thrombolytic (Document1 pageM) IV Anticoagulation M) Arterial Thrombolytic (christine louise bernardoNo ratings yet
- Stroke Summary Document For Medical StudentsDocument3 pagesStroke Summary Document For Medical StudentsDeclan O'KaneNo ratings yet
- Poster SpecCircs Traumatic Cardiac Arrest Algorithm SERB V20160714 HRESDocument1 pagePoster SpecCircs Traumatic Cardiac Arrest Algorithm SERB V20160714 HRESJelena TadićNo ratings yet
- 6 Head and Neck Trauma - Thoracic and Cardiovascular TraumaDocument7 pages6 Head and Neck Trauma - Thoracic and Cardiovascular TraumaMyrtle Yvonne RagubNo ratings yet
- Physiology: StrokeDocument7 pagesPhysiology: StrokeJunYuuuNo ratings yet
- Damage - Control - Resus - Quick - Reference - Guide - Medics - Corpsmen - 2023-Quick Reference Guide For Combat Medics and CorpsmenDocument1 pageDamage - Control - Resus - Quick - Reference - Guide - Medics - Corpsmen - 2023-Quick Reference Guide For Combat Medics and Corpsmenchou youNo ratings yet
- Acute Ischaemic Stroke: Recent Advances in Reperfusion TreatmentDocument11 pagesAcute Ischaemic Stroke: Recent Advances in Reperfusion TreatmentJose MartinezNo ratings yet
- Hematology: CoagulationDocument40 pagesHematology: CoagulationMuhammad SaeedNo ratings yet
- Week 13 Disorders of Secondary Hemostasis LecDocument8 pagesWeek 13 Disorders of Secondary Hemostasis LecCzarina Mae IlaganNo ratings yet
- Eau Guidelines On Urological Trauma: (Limited Text Update March 2017)Document18 pagesEau Guidelines On Urological Trauma: (Limited Text Update March 2017)Peri HidayatNo ratings yet
- AneurysmDocument11 pagesAneurysmNashrah HusnaNo ratings yet
- Nursing Cardiology: Rebound HypertensionDocument8 pagesNursing Cardiology: Rebound HypertensionVon R SemillaNo ratings yet
- Acute Medicine: Shock: Inadequate Tissue and Organ PerfusionDocument3 pagesAcute Medicine: Shock: Inadequate Tissue and Organ Perfusionmyat252No ratings yet
- SF1-Lecture-03 - Body Fluids and Circulation - NotesDocument7 pagesSF1-Lecture-03 - Body Fluids and Circulation - Notesdisha shuklaNo ratings yet
- Anatomy 2Document2 pagesAnatomy 2Ahmed AdelNo ratings yet
- Pa Tho Physiology of Congestive Heart FailureDocument3 pagesPa Tho Physiology of Congestive Heart FailureErin MarieNo ratings yet
- Anti Thrombotic Drugs and Transfusion MedicineDocument5 pagesAnti Thrombotic Drugs and Transfusion MedicineIS99057No ratings yet
- Acute Ischemia of The Lower Limb (LL) : Sudden Occlusion of A Previously Patent Artery Supplying A LimbDocument4 pagesAcute Ischemia of The Lower Limb (LL) : Sudden Occlusion of A Previously Patent Artery Supplying A LimbOmar MohammedNo ratings yet
- 1 RhythmDocument10 pages1 Rhythmcatcat669111No ratings yet
- College of Nursing and Allied Medical Sciences: WesleyanDocument3 pagesCollege of Nursing and Allied Medical Sciences: WesleyanMay Anne ManuzonNo ratings yet
- Aortic Dissection (Schwartz's 11 Ed.) Pathology and Classification Causes and Clinical HX Clinical Manifestations Diagnostic Evaluation TreatmentDocument3 pagesAortic Dissection (Schwartz's 11 Ed.) Pathology and Classification Causes and Clinical HX Clinical Manifestations Diagnostic Evaluation TreatmentSean Dominique Cruz MaghinayNo ratings yet
- Poster SpecCircs Traumatic Cardiac Arrest Algorithm ENG V20151005 HRES SiteDocument1 pagePoster SpecCircs Traumatic Cardiac Arrest Algorithm ENG V20151005 HRES SiteangelologrilloNo ratings yet
- Atrial Arrhythmias Definition and Pathology Significance Etiology Clinical Manifestations InterventionDocument5 pagesAtrial Arrhythmias Definition and Pathology Significance Etiology Clinical Manifestations Interventionmakyofrancis20No ratings yet
- CARDIAC TUMORS TransDocument12 pagesCARDIAC TUMORS TransjeccomNo ratings yet
- 9 - Internal Medicine Buzzwords Handout Oct 2023 John Michael RuizDocument8 pages9 - Internal Medicine Buzzwords Handout Oct 2023 John Michael RuizJohn Michael RuizNo ratings yet
- Cyanotic Congenital Heart Diseases, Etc.Document12 pagesCyanotic Congenital Heart Diseases, Etc.sarguss14100% (2)
- Cardiac DisordersDocument4 pagesCardiac DisordersEUNICE CORILLONo ratings yet
- Brain Arteriovenous Malforamtion: Dr. Suresh Bishokarma MS, MCH (Neurosurgery)Document95 pagesBrain Arteriovenous Malforamtion: Dr. Suresh Bishokarma MS, MCH (Neurosurgery)rr_eeyNo ratings yet
- TRP Surgery Study GuideDocument27 pagesTRP Surgery Study GuidekatNo ratings yet
- ICU One Pager Massive Hemoptysis v11Document1 pageICU One Pager Massive Hemoptysis v11Nicholas HelmstetterNo ratings yet
- What Is It? Risk Factors/ Causes My Columns For My Cardiac Spreadsheet 2 Unique Symptoms Heart Failure (General)Document3 pagesWhat Is It? Risk Factors/ Causes My Columns For My Cardiac Spreadsheet 2 Unique Symptoms Heart Failure (General)Aji PicanteNo ratings yet
- 2.3 Cập nhật chẩn đoán và điều trị suy tim-14-11-2021 - .pptx 2Document1 page2.3 Cập nhật chẩn đoán và điều trị suy tim-14-11-2021 - .pptx 2tranlekieutrinh166No ratings yet
- Materi - Gagal Jantung NeonatusDocument36 pagesMateri - Gagal Jantung NeonatusPutra AchmadNo ratings yet
- Vascular Surgery TNDocument4 pagesVascular Surgery TNVictor Matias BarriosNo ratings yet
- Surgery Update PDFDocument1 pageSurgery Update PDFskNo ratings yet
- IM Part 1 and 2 CombinedDocument100 pagesIM Part 1 and 2 CombinedsasghfdgNo ratings yet
- IM Part 1Document48 pagesIM Part 1sasghfdgNo ratings yet
- AbstrakDocument1 pageAbstraktriana_nimanNo ratings yet
- DR Anna Mira Lubis - Diagnostic Approach of ThrombocytopeniaDocument36 pagesDR Anna Mira Lubis - Diagnostic Approach of Thrombocytopeniayosua simarmataNo ratings yet
- 6.6 CardiovascularDocument9 pages6.6 CardiovascularGhianx Carlox PioquintoxNo ratings yet
- Concept MapDocument4 pagesConcept MapDud AccNo ratings yet
- Case Chest Pain and DyspneaDocument1 pageCase Chest Pain and DyspneaVineeNo ratings yet
- Lung CaDocument1 pageLung CaAqila MumtazNo ratings yet
- Inadequate Reperfusion Therapy: Myocardial InfarctionDocument4 pagesInadequate Reperfusion Therapy: Myocardial InfarctionPäw YusophNo ratings yet
- This Study Resource WasDocument2 pagesThis Study Resource WasKimberly WhitesideNo ratings yet
- Clinical Medicine CVS Tabulated 2019Document5 pagesClinical Medicine CVS Tabulated 2019Justin TayabanNo ratings yet
- 3 에크모는 오크모 요약Document1 page3 에크모는 오크모 요약breaking nurseNo ratings yet
- Anesthesia Pocket Guide 2020 PDFDocument2 pagesAnesthesia Pocket Guide 2020 PDFMaksym DemianchukNo ratings yet
- Acute Limb Ischemia SiteDocument23 pagesAcute Limb Ischemia Sitebenypermadi100% (1)
- Right + Increased Vascularity + Fixed S2 / Widely Split Austin-Flint (Chronic) Graham Steele MurmurDocument14 pagesRight + Increased Vascularity + Fixed S2 / Widely Split Austin-Flint (Chronic) Graham Steele MurmurRojales FrancisNo ratings yet
- Ischemic Heart DiseaseDocument3 pagesIschemic Heart DiseaseNurul Aqilah MazlanNo ratings yet
- Concept Map 11 15 2023 RachelDocument1 pageConcept Map 11 15 2023 Rachelapi-726698459No ratings yet
- Acute Limb Ischemia (Ali) : Tributed To: Ismoyo Sunu, MDDocument54 pagesAcute Limb Ischemia (Ali) : Tributed To: Ismoyo Sunu, MDMhd Ridho FahreziNo ratings yet
- Pathophysiology - AKI (Bana) 3Document1 pagePathophysiology - AKI (Bana) 3Elizalde HusbandNo ratings yet
- Drug Moa PK Use Se Ci Blood Coagulation: AnticoagulantsDocument4 pagesDrug Moa PK Use Se Ci Blood Coagulation: AnticoagulantsYusoff RamdzanNo ratings yet
- RAAS InhibitorsDocument57 pagesRAAS InhibitorsMelissa DelgadoNo ratings yet
- NM - Cerebrovascular AccidentDocument26 pagesNM - Cerebrovascular AccidentRj PolvorosaNo ratings yet
- CARDIAC TUMORS Approach To ManagementDocument12 pagesCARDIAC TUMORS Approach To ManagementAnkit GulatiNo ratings yet
- General Prescribing Guidelines For Geriatric PatientsDocument41 pagesGeneral Prescribing Guidelines For Geriatric PatientsBharath Gowda100% (1)
- SYLLABUS of Ayurveda Medical OfficerDocument61 pagesSYLLABUS of Ayurveda Medical OfficerLipun PurohitNo ratings yet
- Feline Non-Regenerative Immune-Mediated Anaemia: Features and Outcome in 15 CasesDocument7 pagesFeline Non-Regenerative Immune-Mediated Anaemia: Features and Outcome in 15 CasesTORRES GUTIERREZ JOYNY RAQUEL catedraticoNo ratings yet
- Barangay Sinabaan: Republic of The Philippines Province of PangasinanDocument2 pagesBarangay Sinabaan: Republic of The Philippines Province of PangasinanOmar DizonNo ratings yet
- College of Nursing & Allied Health Sciences Tunga-Tunga, Maasin City, Southern Leyte, PhilippinesDocument68 pagesCollege of Nursing & Allied Health Sciences Tunga-Tunga, Maasin City, Southern Leyte, PhilippinesAgent PimpNo ratings yet
- BPH and HematuriaDocument40 pagesBPH and HematuriaJohn LeeNo ratings yet
- 2021 Overdose Fatality Report (Final)Document26 pages2021 Overdose Fatality Report (Final)Sierra NewtonNo ratings yet
- Septemper 2014: Answer: L1Document22 pagesSeptemper 2014: Answer: L1kyahuaNo ratings yet
- The Pandemic Effect A Social Isolation Report AARP FoundationDocument60 pagesThe Pandemic Effect A Social Isolation Report AARP FoundationAilynne Joy Rojas Lim100% (1)
- General Surgery&plastic Surgery Board-Part One Exam Blueprint (v.1)Document4 pagesGeneral Surgery&plastic Surgery Board-Part One Exam Blueprint (v.1)Mohammed S. Al Ghamdi100% (1)
- Textbook DiabetesDocument4 pagesTextbook Diabetessadiq alaliNo ratings yet
- Clinic Guidance Case History Form UCO Sep2017 FINALDocument4 pagesClinic Guidance Case History Form UCO Sep2017 FINALShaun TylerNo ratings yet
- OREM'SDocument32 pagesOREM'SJoji JohnNo ratings yet
- Fulminant Myocarditis (Springer, 2022)Document375 pagesFulminant Myocarditis (Springer, 2022)Phuoc NguyenNo ratings yet
- Health and Well-Being in Older AgeDocument7 pagesHealth and Well-Being in Older AgeImran ShaNo ratings yet
- Edwards' SyndromeDocument2 pagesEdwards' Syndromeمحمود محمد0% (1)
- Identifying The Determinants of Childhood Immunization in The PhilippinesDocument7 pagesIdentifying The Determinants of Childhood Immunization in The PhilippinesCarlo Joseph Intal LlacerNo ratings yet
- MIKROSEFALIDocument14 pagesMIKROSEFALIfikasilvia_ciyank5771No ratings yet
- Gall StonesDocument26 pagesGall StonesNia SinghNo ratings yet
- Pulmonary Edema II: Noncardiogenic Pulmonary EdemaDocument31 pagesPulmonary Edema II: Noncardiogenic Pulmonary EdemaGita Helvia SariNo ratings yet
- Horizontal Transmission P. Salmonis Wild Sub Antarctic Rainbow Trout Under Experimental ConditionsDocument12 pagesHorizontal Transmission P. Salmonis Wild Sub Antarctic Rainbow Trout Under Experimental Conditionsandres riofrioNo ratings yet
- Psychiatric Nursing Mastery Test Part 1Document12 pagesPsychiatric Nursing Mastery Test Part 1Rika MaeNo ratings yet
- 1ST Drug StudyDocument10 pages1ST Drug Study황춘히No ratings yet
- Adrenocortical DisordersDocument73 pagesAdrenocortical DisordersReunita ConstantiaNo ratings yet
- Incident Report Form: RPSG-IMS-F-24 Accident and Investigation Form 5ADocument2 pagesIncident Report Form: RPSG-IMS-F-24 Accident and Investigation Form 5ARocky BisNo ratings yet
- Osteonecrosis: Avascular NecrosisDocument8 pagesOsteonecrosis: Avascular NecrosisJezreel BonaNo ratings yet
- دوائيات ن- lec22-ReducedDocument24 pagesدوائيات ن- lec22-Reducedma22mdmmNo ratings yet
- Intermittent Fasting Facts and Myths: Metabolic Benefits of Intermittent FastingDocument4 pagesIntermittent Fasting Facts and Myths: Metabolic Benefits of Intermittent FastingIJAR JOURNALNo ratings yet