Professional Documents
Culture Documents
Synonyms/ Origin of Name: Tuberculosis - Leprae - Acid - Fast
Uploaded by
Angeli Marie Padilla0 ratings0% found this document useful (0 votes)
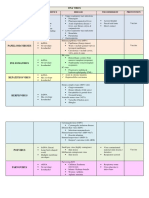
25 views15 pagesThis document summarizes and compares key details of several infectious respiratory diseases: pulmonary tuberculosis, leprosy, measles/mumps/chickenpox, SARS, and pneumonia. It outlines their synonyms, origins of names, causative agents, incubation periods, and modes of transmission. The diseases are caused by a variety of bacteria, viruses and other pathogens. They are generally transmitted through airborne droplets or close personal contact, with incubation periods varying from days to years depending on the specific disease.
Original Description:
piblic health
Original Title
Pubhealth Diseases
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document summarizes and compares key details of several infectious respiratory diseases: pulmonary tuberculosis, leprosy, measles/mumps/chickenpox, SARS, and pneumonia. It outlines their synonyms, origins of names, causative agents, incubation periods, and modes of transmission. The diseases are caused by a variety of bacteria, viruses and other pathogens. They are generally transmitted through airborne droplets or close personal contact, with incubation periods varying from days to years depending on the specific disease.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
25 views15 pagesSynonyms/ Origin of Name: Tuberculosis - Leprae - Acid - Fast
Uploaded by
Angeli Marie PadillaThis document summarizes and compares key details of several infectious respiratory diseases: pulmonary tuberculosis, leprosy, measles/mumps/chickenpox, SARS, and pneumonia. It outlines their synonyms, origins of names, causative agents, incubation periods, and modes of transmission. The diseases are caused by a variety of bacteria, viruses and other pathogens. They are generally transmitted through airborne droplets or close personal contact, with incubation periods varying from days to years depending on the specific disease.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 15
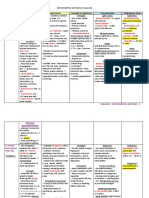
DISEASE
PULMONARY TB LEPROSY MEASLES, MUMPS, CHICKENPOX SARS PNEUMONIA
(Airborne) (Airborne) (Airborne) (Airborne) (Airborne)
SYNONYMS/ • TB (Tubercle bacilli) • Hansen’s disease • Me: Rubeola, morbilli, hard • severe acute • Respiratory
ORIGIN OF • Consumption • Leprosy -‐ leprae (L.) measles, 14-‐day measles, respiratory illness/disease/disor
NAME • Phthisis = “scaly” English measles, contagious syndrome der
• Phthisis pulmonalis disease, contagion
• Wasting disease • Mu: Epidemic parotitis
• White plague • CP: Varicella, pox
• King’s evil
CAUSATIVE 1. Mycobacterium • Mycobacterium • Me: paramyxovirus, genus • SARS Coronavirus Bacteria -‐
AGENT tuberculosis -‐ leprae -‐ acid-‐fast, Morbilivirus, ssRNA -‐ inact by (SARS CoV) -‐ ssRNA, pneumococcal;
aerobe, neither G+/-‐ alcohol-‐fast, G+, heat, pH, trypsin, ether, survival enveloped • Strep. pneumoniae
, nonmotile, acid-‐ resemble M. tb, has time in objects = n.m.t. 2hrs • S. aureus
fast, cell wall longest doubling • Mu: mumps virus, genus • Klebsiella pneumoniae
w/mycolic acid) time of 13 days Rubulavirus, ssRNA -‐ inact by • H. influenza
2. M. Africanus -‐ lower • M. lepromatosis formalin, ether, chloroform, • Legionella
pathogenicity, heat, UV pneumophila
subsp. of M. tb) • CP: Varicella zoster virus (VZV), • Chlamydiophilapneum
3. M. bovis -‐ frm cow family Herpesviridae, dsDNA oniae
thru unpasteurized • Mycoplasma
milk, or other pneumoniae
animals) Virus
• Influenza virus type
A/B (most common)
• RSV
• Rhinovirus, HSV,
SARS, etc
Fungi
• Histoplasmosis
• Coccidioidomycosis
• Blastomycosis
Parasites
• Toxoplasma gondii
• Strongyloides
stercoralis
• Ascaris lumbricoides
• Plasmodium
malariae
**It is an inflammation
in 1/both of longs
INCUBATION PD • 2-‐12 weeks Me: 7-‐21 (to onset of fever), ave.
• Up to 5 yrs (may be • 2-‐7 days • Varied for caus.
symptomatic for up 14 (appearance of rash) Agents
to 20 yrs) Mu: ave 16-‐18 days • 2-‐10 days
CP: ave 14-‐16 days
MODE OF • Airborne droplet • Uncertain but usually **MMC: • Airborne • Airborne
TRANSMISSION method (Cough, through nasal • Airborne, inhalation of resp • Close person-‐to-‐ • Bloodstream
sneeze, talk, sing) droplets (cough, droplets person contact infection
sneeze, inhale) • Direct contact w/skin, fluids, • Fomite
• Armadillo mucus • Fecal-‐oral*
• Fomite transmission possible
SIGNS AND • Productive, • Granulomas of the Me: (course usally last 7-‐10 days) • Similar to pneumonia • Chest pain
SYMPTOMS prolonged cough nerves, respiratory • systemic inf, esp in resp. • Flu-‐like symptoms, • Shaking chills
3/more wks tract, skin, eyes epithelium in nasopharynx nonspecific: fever, • Dry cough
• Blood-‐tinged mucus • Hypopigmented skin • 4-‐day fevers myalgia, lethargy • Muscle ache
• Chest pain patches • 3 Cs -‐ cough, coryza (head symptoms, cough, • N/V
• Hemoptysis • Lack ability to feel cold), and conjunctivitis (red sore throat • Rapid breathing &
• Fever, night sweats pain eyes) • Common to all inf: heartbeat
• Weight loss (hence • Loss of extremities • Fever -‐ up to 40 °C (104 °F) fever above 38 °C • DOB
consumption) • Poor • Koplik spots (exanthem rash) -‐ (100 °F) • Bluish skin
eyesight/blindess pathognomic, blue-‐white spots • Shortness of breath • Blood in sputum
on buccal mucosa (“currant jelly” from
• Rash (last up to 8 days) -‐ STAGES: Klebsiella)
maculopapular erythematosus 1) Prodromal -‐ fever, • decreased thirst,
lesion, start on back of ears, to chills, malaise, etc; convulsions,
head & neck to hands & feet; incub 2-‐7 days extremes of temp
“Stain” -‐ turn brown before 2) Respiratory -‐ • decreased level of
disappears deadly; dry consciousness
• Others: anorexia, diarrhea, nonproductive cough,
lymphadenopathy hypoxia, etc
Mu:
• Inflamm of parotid glands
(parotitis)
• Low-‐grade fever
• Orchitis -‐ inflamm of testicular
gland-‐>infertile
• May be asymptomatic
CP:
• Characteristic rash (itchy, raw
pockmarks, small red spots,
become raised and form
blisters)
• Malaise
• Low-‐grade fever
• No prodrome (nausea,
headache etc) in children
• Ave child with 250-‐500 blisters
DIAGNOSIS 1. Chest x-‐ray • Skin Biopsy -‐ most Me: • 38C fever • Physical exam -‐
2. TB (Mantoux) skin accurate • history of fever (at least 3 • Contact w/inf pt w/in crackling, bubbling,
test -‐ often for • Commonly based on days), at least 1 of 3 Cs, last 10 days rumbling sounds in
latent TB, inj signs & symptoms Koplik’s spots • Travel to inf regions lungs
tuberculin in arm • NO blood tests • Lab test -‐ IgM, IgA in saliva, • Chest x-‐ray: (+) • Chest x-‐ray -‐ best
3. Interferon Gamma isolate virus frm resp specimen atypical pneumonia diagnosis, not specific
Release Assays • Contact with infected pt or resp distress for agent;
(IGRAs) -‐ blood test Mu: syndrome consolidation in
on immune • Clincal manifestations (esp • Lab tests: ELISA, 1/more lobes; patchy
response parotitis) immunofluorescence consolidation in bases
4. Serological Tests for • Phys exam, saliva/blood test, or PCR of lungs
Ab serology & EIA (for IgM & IgG) • Blood Tests -‐ sample
5. Direct Sputum Spear • PCR from vein; CBC
Microscopy (DSSM) • Elevated serum amylase measures WBCs (to
+ Fluorescent CP: know bacterial inf), to
microscope* • Clinical diagnosis (prodromal know if spread to
symp, rash) bloodstream
• Vesicular fluid tests -‐ Tzanck • Chest computed
smear, Direct Fluorescent Ab tomography (CT) scan
(DFA) more detail than X-‐ray
• blood test -‐ IgM (acute inf), • Pleural fluid culture -‐
IgG (resolved inf/ developed sample frm pleural
immunity) space
• Ultrasound -‐ fetal inf • Sputum test -‐ after
deep cough
• Pulse oximetry
• Arterial blood gas test
• Bronchoscopy
DRUG OF • First line treatment: • MDT (Multi-‐drug Me: no specific treatment, rest, • Only supportive with Bacteria (7-‐10 days)
CHOICE/ Rifampicin, Isoniazid therapy) only for symptoms antipyretics, • CAP: Amoxicillin, with
TREATMENT (INH), Pyrazinamide • Paucibacillary (mild): Mu: treat symptoms, apply supplemental Doxycycline &
(PZA), Ethambutol, dapsone and ice/heat to affected area, saltwater oxygen, mechanical Clarithromycin as
Streptomycin; 6 mos rifampicin for 6 mos gargle, soft food, extra fluids, ventilation alternative; Atypical:
• Intensive phase (2 • Multibacillary *avoid acidic food/beverages Macrolides
mos): RIPE (severe): rifampicin, **ASA-‐ CI for <16yrs,cause Reye’s • HAP: 3rd-‐4th gen ceph,
• Continuation phase dapsone, clofazimine syndrome carbapenems,
(4 mos): RI for 12 mos CP: treat rash blister scab (topical fluoroquinolones
treatment), antihistamine for itch, Virus
antivirals (e.g. acyclovir, • Neuraminidase
valacyclovir) for adults, calamine, inhibitors (-‐ivir) for
oatmeal bath, don’t use inf A&B
ASA,*Sorivudine • Rimantadine,
Amantadine
Aspiration pneumonia
• Clindamycin, B-‐
lactam + Metronida,
Aminoglycoside
RISK FACTORS • HIV, low immune • Polluted water Me: may complicate into • Occasionally lead to • Weak immune
system • Poor diet bronchitis, pneumonia or pneumonia system, HIV,Measles
• Infected with TB in • People suffering encephalitis • Post-‐SARS pts have • Environmental
last 2 yrs from diseases that • HIV, travel, Vit. A def major depressive factors
• Past TB not correctly compromise immune disorder • Children, elderly
treated function (e.g. DM, **MMC: Children have high • Smoking
• Children, elderly AIDS, heart disease) incidence in temperate climate, • Other lung cond’n
• Silicosis usual in winter/spring; Adults high • Heart, kidney, liver
• DM incidence in tropical climates cond’n
• Smoking • Use of PPI/H2 blocker
PREVENTION & • BCG (Bacillus • 95% of people Me: MMR (Measles, Mumps, • Isolation & • Influenza vaccine
VACCINE Calmette-‐Guérin) naturally immune Rubella) vaccine quarantine (1yr), Pneumococcal
vaccine -‐ live • Sufferers no longer • Measles vaccine -‐ from chick • Disinfect surface, Pneumonia vaccine
attenuated M. bovis infectious after 2 wks embryo; first dose after 1yr wash personal (5yrs), Hib (H.
• DOTS of Tx old items influenza type b)
• Improve social Mu: MMR vaccine • Influenza & vaccine
cond’n CP: MMRV, Varicella vaccine (live pneumococcal • Amantadine &
(overcrowding) attenuated) cut nails and wear vaccine may reduce Rimantadine
• Cover mouth/nose gloves if infected severity • Vaccines for
when cough/sneeze **MMRV -‐ 12mos-‐12yrs, not 13 or pertussis, varicella,
older measles
• Wash hands with
soap
• Don’t smoke
• Zn supplements
PROGRAMS • NTP (Nat’l TB • National Leprosy • House Bill 5937 -‐ • Expanded Programs
Control Program) Control Program Me: Quarantine of inf on Immunization
• DOTS (Directly (DOH) -‐ elim. Leprosy • Expanded Programs on pts (DPT, TB, Measles,
Observed by 2020 Immunization (DPT, TB, • EO 201 -‐ resp of pneumococcal
Therapy/Treatment, • Partners in Leprosy Measles) govt to respond to conjugate
Short-‐ Action (Phil. Leprosy • Iligtas sa Tigdas ang Pinas (for SARS vaccine/PCV)
course/Strategy) -‐ Mission, Inc.) -‐ Measles & Rubella) • Program for Control
control strategy by detect skin diseases of Acute Resp.
DOH Infections (CARI)
EPIDEMIOLOGY • 1/3 of world has • Also occur in Me: • Zoonotic origin, • Phil one of 15
been inf animals/primates • no animal reservoir, no resp disease countries for 75%
• Most are latent (chimpanzee, asymptomatic childhood pneumonia
• Second most armadillo, squirrel, • extremely infectious cases
common COD from etc) Mu: • Major cause of death
inf. disease (after • Tropical & • common cause of aseptic • 450M affected/yr
HIV/AIDS) subtropical climate meningitis & deafness in • Rates highest in
• 1/10 latent progress • India has most cases children children<5, adults>75
to active CP:
• Active kills abt 50% • May be asymptomatic
• most cases in children <10 (4-‐
10); adults & older children get
more sick
• Occur in primates
HISTORY • Robert Koch • Egypt, India, Greece, Me: • Started in • Hippocrates -‐
(German) -‐ disc M. Rome • Antonine/Galen Plaque -‐ by Guangdong, China “disease named by
tuberculosis • Gerhard Hansen smallpox or measles (2002) from masked ancients”
• White Plague in 18th (Norway) -‐ disc M. • Rhazes first described palm civets or from • Maimonides -‐ desc
cent leprae Mu: bats symptoms
• Spinal TB/Pott’s • documented in the • Hilleman (Am.) invented • WHO alerted on • Klebs -‐ saw bacteria
disease in Egyptian Synoptic Gospels vaccine (1967) epidemic flu in airways
mummies CP: Takahashi disc live attenuated • William Osler -‐
vaccine frm Oka strain “captain of men of
death”
NOTES • Types of TB: • Types: Me: endemic • More serious • TYPES: Community-‐
pulmonary & 1. Paucibacillary -‐ CP: dormant virus frm prev damage due to acquired (CAP) &
extrapulmonary; 5 or less poorly infection can be later reactivated immune sys Hospital-‐acquired
latent & active pigmented skin into shingles (Herpes zoster) (cytokine storm) (HAP)
• May infect animals patch, (-‐) • Aspiration
(M. bovis) smears at all **MMC: self-‐limiting pneumonia -‐ inhale
• Famous people: sites food, drink, vomit, or
Henry VII, Graciano 2. Multibacillary -‐ saliva frm mouth to
Lopez-‐Jaena, Louis >5, (+) smears lungs; if disturbed
Braille • World Leprosy Day: normal gag reflex
Jan. 26 (commem. • Atypical pneumonia
Gandhi’s death) -‐ person-‐to-‐person,
• PWL -‐ person with caused by types of
leprosy bacteria (L.
pneumophila, M.
pneumonia,
Chlamydophila
pneumoniae)
• World Pneumonia
Day: Nov. 12
QUESTIONS 1) why do children give 1. Examples ng what are the common tagalog When did it start? 1. what are the types of
a false positive test leprosariums sa name of measles, mumps -‐November 2002, but pneumonia?
when tested for TB? -‐ Philippines-‐ Culion chickenpox : bulutong, beke, tigdas first confirmed case 2. which is hardest to
because of the BCG Sanitarium (Palawan), why you should not take aspirin as was on February 2003 treat? why?
vaccine (contains Tala Leprosarium treatment of the disease: it can Where did it 3. Most common under
attenuated (Caloocan), Eversley develop Reye's syndrome, a fatal originate? hospital acquired-‐
Mycobacterium bovis) Childs Sanitarium complexion -‐Guangdong Province PSEUDOMONAS
2) other name for TB -‐ (Cebu City), Cotabato why do people develop vertigo of China 4. What are the
"consumption"(Wt Sanitarium (Cotabato) from mumps: because mumps is How was it treated? different causative
loss) cause by the swelling of the parotid -‐Same drugs as agents?
3) best drug of choice 2. Mode of glands located under the ears treating pneumonia. 5. Vaccination effective?
for TB-‐ first line of Transmission-‐ which can affect the vestibular Steroids to decrease 6. Strains of bacteria in
drugs, RIPES Airborne disease yung nerves located at the ears lung inflammation, vaccine
4) can TB only infect leprosy. Tapos yung what are the difference between Antipyretics to 7. 100% immunity if
the lungs?-‐ no, it can frequent skin contact measles, mumps, chickenpox: suppress high fever. given with vaccine? NO
also infect other parts sa may leprosy. measles is formation of red rashes Were there vaccines 8. how long is the
of the body, this is while chickenpox are formation of proven effective to immunization if given
called extrapulmonary 3. Incubation period-‐ liquid filled blisters while mumps is combat SARS? with vaccine?
TB, spine TB, pleural Up to 5 years the swelling of parotid glands -‐No. It takes 3-‐6 years 9. How many
TB,TB of the lymph why use ice pack/ warm compress to develop a vaccine microorganisms inside
nodes 4. Aside pa dun sa at swelling of mumps: to relieve for a new disease. By vaccine?
5) What do you call armadillo, ano pa yung swelling the time scientists 10. Why can it cause
children with tb? parang nagiging is there a cure: there are no cure from WHO came up death?
primary complex reservoir na ginagamit (antibiotic or antibacterial) because with vaccines, there 11. What's responsible
6) kailan nagiging sa lab for research sa the disease are self limiting, the were no more cases of for death?
infectious ang isang leprosy-‐ foot pad ng treatment are application of SARS. Thus, none of 12. Best treatment sa
bata? kapag natuto mouse ointments to relieve itching and them were proven bacteria, virus, fungi,
magdura ng sputum using paracetamol to relieve fever effective. parasite
What is the 13. World Pneumonia
pathogen's origin? Day-‐ November 12
-‐Zoonotic Origin (from 14. Specific Govt
bats) Program wala
Is it possible for SARS
to recur?
-‐Yes. Since it is a virus
from a zoonotic
origin, the human
body has no innate
immunity to fight
against it. In fact, a
disease similar with
SARS' strains already
occured, that which is
MERS-‐CoV in 2012.
The only difference is
that SARS came from
bats in China, while
MERS-‐CoV(Middle
East Corona Virus)
originated from
Egyptian bats.
DISEASE SWINE FLU DENGUE MALARIA RABIES BIRD FLU
(Airborne) (Vector-‐borne) (Vector-‐borne) (Zoonotic) (Zoonotic)
SYNONYMS/ • A(H1N1) flu • From Ka-‐dinga pepo • Ague or Marsh fever • Rabhas (Sanskrit) = “to • Avian influenza/flu
ORIGIN OF • Pig flu/ (Swahili phrase) = • Tertian fever do violence” • Fowl Plague
NAME influenza “cramp-‐like seizure • Quartan fever • Rabere (L.) = “to
• Swine influenza caused by evil spirit” • Intermittent fever rage/rave”
• Hog flu • Breakbone fever • Roman fever • Lyssa/lytta (Gk.) =
(myalgia & arthralgia) • Mala aria (Italian) = “bad “frenzy or madness”
• Dandy fever air” • Hydrophobia
• Dengue hemorrhagic
fever
• Dengue shock
syndrome
• Duengero
• Seven Day Fever
CAUSATIVE • Swine influenza • Dengue virus -‐ ssRNA Plasmodium -‐ single-‐celled • Lyssavirus, family • Influenza A viruses,
AGENT virus (SIV) or (+) strand, mosquito-‐ 1. falciparum Rhabdoviridae -‐ (-‐) Orthomyxoviridae
swine-‐origin borne, family • Malignant tertian ssRNA, non-‐segmented, family -‐ (-‐) ssRNAm
influenza virus Flaviviridae, genus • Blackwater fever rod/bullet-‐shaped, segmented
(S-‐OIV) Flavivirus • Africa neurotropic virus • Many subtypes but the ff
• A(H1N1) virus • Four serotypes: DEN-‐ • Deadly, severe (humans and mammals) are highly pathogenic to
subtype (comb 1, DEN-‐2, DEN-‐3, DEN-‐ 2. vivax • Virus is in saliva & humans: H5N1, H7N3,
of human 4, DEN-‐5 • Benign tertian malaria nerves H7N7, H7N9, and H9N2.
influenza, • Mild yet aggravating • H5N1 -‐ most common
swine, avian: 3. ovale cause, highly virulent
triple • Benign tertian/ovale • H7N9 -‐ new
reassortant flu), malariae • Wild aquatic birds -‐
genus Influenza • Rare, usual in West natural hosts
A, family Africa • Antigenic shift -‐ genetic
Orthomyxovirid 4. malariae reassortment
ae • Benign quartan malaria
• Also: H1N2, • Rare, usual in Africa
H2N1, H3N1, • Freq not observed,
H3N2, H2N3 parasites dormant in
**Influenza A,B blood
(not in pigs), C 5. knowlesi
(possible, rare) • recentrly emerged
• among monkeys, forests
in SE Asia
INCUBATION PD • 1-‐4 days • 4-‐7 days • 7-‐18 days: Humans: 1-‐3 mos/30-‐90 2-‐4 days
1. falciparum days
⎯ 7-‐14 days Animals: 10-‐80 days
2. vivax after exposure
⎯ 12-‐17 days ⎯ Virus excretion: 2-‐7
3. ovale days before/after
⎯ 15-‐18 days appearance of
4. malariae symptoms
⎯ 18-‐40 days
5. knowlesi
MODE OF • Person-‐to-‐ • Transmission vectors: • Female mosquitos of genus • Most by dog bites, Bird-‐to-‐bird
TRANSMISSION person 1) Aedes aegypti -‐ Anopheles (Culicidae); male infect warm-‐blooded Human-‐to-‐bird
• Similar to flu invasive, feed on nectar, not blood mammals Human-‐to-‐human
• Airborne tropical/subtropical, frm • Anopheles gambiae -‐ one 1. Human-‐human -‐
• Also zoonotic Africa of best known, for corneal or organ
(Pigs) 2) Aedes albopictus -‐ falciparum transplants
invasice, from Asia • “night-‐biting” 2. Animal-‐animal or
• Blood products/organ • Blood transfusion animal-‐human -‐
donation • Congenital through bite; penetrate
• Not person-‐to-‐person infected saliva into
**Life cycle of mosquito: egg, broken skin/mucosa
larva, pupa, adult 3. Aerosol -‐ enter
**intermediate host (MAN), nasal epithelium
definitive host (MOSQUITO) Rabid dogs -‐ no
hydrophobia, only
sensitive to
external stimuli
Rabid mother to
baby -‐ exposed to
saliva
Not oral/thru
eating infected
meat
SIGNS AND • Lethargy • Fever (above 40C), • Fever • Hydrophobia -‐ morbid • Muscle ache
SYMPTOMS • Lack of appetite headache, muscle & • Fatigue fear of water • Cough
• Coughing, joint pains • Vomiting • Painful muscle spasms • Fever
runny nose • Rash similar to • Headaches when swallowing • Sore throat
• Sore throat, measles • Initial: flu-‐like • Sore eyes
N/V, diarrhea • • paralysis, anxiety, • DOB (severe)
• Commonly • • Severe: jaundice/yellow insomnia, confusion,
mistaken for ("islands of white in a sea skin, seizures, coma, death, agitation, abnormal Complications:
common cold of red") kidney failure, hemoglobin behavior, paranoia, Pneumonia
• Low platelet, low BP in urine, pulmo edema, terror, and Respi failure & other
• Black tarry stools acidosis hallucinations, organs
• Similar to common • Paroxysm -‐ classical progressing to delirium Seizure, shock
cold and symptom; cyclical coldness • Stages: (1) Prodromal, Death
gastroenteritis by shivering then fever & (2) Acute neurologic
• Neuro disorders: sweating (Furious in 80%,
transverse myelitis, • Cerebral malaria -‐ Paralytic/dumb type in
Guillain-‐Barré abnormal posture, 20%), (3) Coma/death
syndrome nystagmus, palsy, etc • Death usually 2-‐10 days
• Dengue Hemorrhagic • Liver dysfunction -‐ in those after appearance of
Fever (DHV) -‐ rare, w/liver cond’n; malarial symptoms; respiratory
damaged lymph & hepatitis paralysis
blood vessels, failure
of circ system
• *Dengue Shock
Syndrome (DSS)
DIAGNOSIS • Rapid influenza • Clinical: symptoms, • Microscopy -‐ of blood • Symptom hydrophobia • PCR -‐ differentiate bet
diagnostic test physical exam specimen; gold standard; and/or aerophobia is a H5, H7, and N1 subtypes
(RIDT) -‐ dist. • Difficult to diagnose determine species and % of straightforward dx • Virus isolation
bet. Inf A&B (symptoms similar to blood cell infected • Fluorescent Antibody • H/N subtyping
• PCR typhoid, scarlet fever • Antigen Detection-‐Rapid Test (FAT) -‐ ref method, • Genetic sequencing
• Viral culture -‐ leptrospirosis etc) Diagnostic Test -‐ specific use skin biopsy • Pathogenicity tests
confirm (+) • Torniquet test -‐ antigen in blood, followed • RT-‐PCR
rapid test capillary-‐fragility test, by microscopy to confirm • RFFIT (Serum Rapid
know hemorrhagic • Serology -‐ Indirect Fluorescent Focus
tendency,apply BP cuff Fluorescent Ab test -‐ Inhibition Test) -‐ know
• CBC -‐ general test, falciparum, vivax, malariae potency of rabies erum
most impt only; for blood donor & Ig’s used
-‐classical dengue triad: • Molecular Diagnosis -‐ PCR -‐ • Seller’s Test or Negri
1) increase hematocrit most useful for confirming Body Detection in Direct
2) atypical species Microscopic Exam
lymphocytosis • Mouse Inoculation Test
3) thrombocytopenia
• MAC-‐ELISA assay -‐
IgM antibodies +
DENV1-‐4
• PCR test
• Plaque reduction &
neutralization test -‐
most specific
serological tool for
dengue Ab’s
• Coagulation studies,
blood/urine culture
DRUG OF • Oseltamivir • No specific Tx • Recomm 1st line (WHO): • Post-‐exposure Amantadine
CHOICE/ (Tamiflu) -‐ • Supportive: ACTs/Artemisinin-‐based prophylaxis: Rimantadine
TREATMENT emergency use rehydration therapy, comb therapies for ⎯ local wound care Oseltamivir
for >1y/o, oral pain control, bedrest falciparum; (a) Arthemether (povidone iodine Zanamivir
susp • Antipyretics, pain & Lumefantrine, (b) or alcohol)
• Zanamivir relievers (Paracetamol, Dihydroartemisin-‐ ⎯ admin of rabies **H5N1 resistant to A & R
(Relenza) -‐ Codeine) piperaquine vaccine (active
children > 7, • Avoid ASA, Ibuprofen, • Quinine -‐ 1 of most immunization)
10mg/day, corticosteroids effective • Check Prevention**
inhaled powder • Chloroquine -‐ for P. vivax (vaccines and Ig)
• Amodiaquine • Supportive mgt:
• Pyrimethamine -‐ for ⎯ Antitetanus
uncomplicated malaria, for immunization -‐ to
chloroquine-‐resistant when all bite victims
comb w/sulfadoxine ⎯ Antimicrobials -‐ for
• Mefloquine (Lariam) -‐ used category III bites;
solely against falciparum Amoxicillin,
• Clindamycin -‐ w/quinine to Cloxacillin,
treat acute cases of Cefuroxime,
falciparum Doxycycline or
• Artemisinin -‐ rapid action, Erythromycin for
improve w/in 1-‐3 days, pen-‐allergic
fastest clearance, act on
trophozoite phase Milwaukee/Wisconsin
Protocol -‐ chem induced
coma + admin of
antiviral drugs
RISK FACTORS • Medical • Tropical climate • Climate change Cold climate where they
cond’ns e.g. • Stagnant water in • Behavioral factors survive longer
heart/lung domestic environmtn • Geographical location Poultry farmer
disease (breed mosquitos) • Environmental cond’n Travel to place
• Weak immune • Travelling, cheap
system, accommodation
obesity,etc • Outdoors at nighttime
• <2yrs old, • Elderly, pregnant
pregnant
• Higher risk may
lead to
pneumonia/blo
odstream
infection
• Swine
farmers/vets
PREVENTION & • Properly-‐ • Recovery from 1 type • ABCD: Awareness of risk, • Domesticated animals H5N1 inactivated
VACCINE cooked (71C) provides immunity Bite prevention, Check if subjected to rabies vaccine, or live
pork ONLY to that serotype need to take malaria vaccine, away frm attenuated
• Wash hands, • No vaccine prevention tablets, wildlife; repeat vaccine Protecting eyes, nose,
contain • Environmental mgt Diagnosis when needed mouth and hands from
cough/sneeze • Chemical methods for • no licensed vaccine • Avoid contact with virus particles
• H1N1 vaccines: vector control (e.g. • RTS,S/AS01 -‐ most adv wild/undomesticated Avoid contact w/poultry
1) Flu shot -‐ N,N-‐diethyl-‐meta-‐ research against falciparum animals Rapid
inactivated; for 6 toluamide/DEET) • Reduce breeding site • Human Diploid Cell destruction/stamping
mos and older • Waste mgt Rabies vaccine: out of all infected
2) Nasal spray -‐ • Vector control (insecticidal ⎯ Inactivated vaccine Wash hands at least
live, attenuated; 2-‐ nets, residual spraying) ⎯ ID when IM is CI for 20sec before & after
49yrs, not hematologic handling poultry
pregnant; 2-‐9y/o cond’n, inj on Cook poultry at temp at
receive 2 doses deltoid least 165F
⎯ IM for
immunocompromis
ed pts or those
taking
steroids/chloroqui
ne, not inj in
gluteal region but
anterolateral of
thigh
Recombinant Rabies
Vaccine (V-‐RG)
Immunity: 2-‐3yrs, 10yrs
if w/booster
Passive immunization
w/Human Rabies Ig
(HRIG) -‐ for category III
exposure
PROGRAMS • Interim • National Dengue • Roll Back Malaria • National Rabies • Preparedness and
Guidelines No. Prevention & Control • Malaria Control Program Prevention & Control Response Plan for Avian
15 on Program • Malaria Program Medium-‐ Program and Pandemic Influenza
Quarantine • ABaKaDa -‐ Aksyon Term Dev’t Plan
Procedures in Barangay Kontra
Relation to Dengue (DILG)
Influenza A • DOST Mosquito
• RA 9271: Ovicidal/Larvicidal
Quarantine Law Trap System
of 2004 • Nat’l Tepok Lamok,
• AO 2009-‐0009 Dengue Sapok
(application of Program and 4’O Clock
DOH guidelines) Habit -‐ alim all
mosquito breeding
grounds every 4pm
EPIDEMIOLOGY • Pandemic • Phil has highest cases • 1-‐2.5M deaths/yr • In all continents except • Not yet in the Phil/rare
(2009) started in Western Pacific • Most highly endemic in Phil: Antarctica • H5N1 said to be world’s
in US & Mexico • Endemic in >110 Apayao, Quirino, Sulu, Tawi-‐ • Philippines: 4th in largest pandemic threat
-‐ killed 203k countries tawi incidence, most <15y/o
worldwide • 80% asymptomatic • India -‐ highest rates
HISTORY • first proposed • Aedes mosquito • Genus Plasmodium -‐ by • First written in Codex of • Fowl Plague -‐ 1878, Italy
to be a disease identified (1906) Marchiafava & Celli Eshnunna
related to • Vivax & malariae -‐ by Grassi • Cardanus -‐ saliva from
human flu & Filetti (Italian) rabid dog as a virus
during the 1918 • Ronald Ross -‐ parasite trans • Celcus -‐ saliva only
flu pandemic frm inf. pt to mosquito contains virus
• Welch -‐ falciparum • Pasteur & Roux -‐ disc
vaccine
NOTES • Probable case -‐ • an acute febrile illness • Classified as severe malaria • World Rabies Day -‐ • H -‐ hemagglutinin
(+) inf A, not (low blood) or September 28 • N -‐ neuraminidase
known subtype uncomplicated malaria • Rabies Awareness • H & N -‐ proteins on
• Confirmed case • RECURRENCE: Month (EO 84) -‐ March surface of virus
-‐ confirmed Recrudescence (return after • There are 144 subtypes
A(H1N1) symptom-‐free pd), Relapse of influenza A: H1N1 to
(reappear after H9N16
elimination), or Reinfection • Origin of Angry Birds
(new parasite)
QUESTIONS *prevention-‐ Normal platelet count: 1. Difference between 1. Ano yung ginagamit pag 1. Bakit walang case sa
wash hands, 150-‐350 dengue and malaria? nag conduct ng euthanasia Philippines? The virus
cough and sneeze Blood donor: atleast 50 Vector: Dengue -‐ Aedes, sa dogs? Carbon monoxide survives longer in colder
into elbows kg, no current disease, no Malaria -‐ Plasmodium gas or by overdose ng weathers. Philippines has
*treatment-‐ tattoo pero kung more Dengue -‐ day, Malaria -‐ night anesthesia (by injection) strict regulations in terms
antivirals -‐ than 5 yrs na yung tattoo Symptoms: Dengue -‐ may 2. World Rabies Day -‐ of poultry imports from
oseltamivir and pwede na, rashes, Malaria -‐ chills, september 28 countries that are reported
zanamivir ratio ng blood na ibabalik recurrent fever, sweating 3. Nattransfer daw ba to be affected.
*nakakamatay mo kapag nagpablood 2. Commonly found in yung virus sa pagkain ng 2. Alin mas mahirap i-‐
ba? pag transfusion (1:2 packs) what province? kinatay na aso na may treat-‐-‐Swine flu o bird flu?
nagkaroon ng enzyme na bumababa: Palawan, tawi-‐tawi, other rabies -‐ walang evidence Bird flu, dahil ang virus na
complication cyclooxygenase provinces in mindanao na magpapakita na may ito mas madaling
*ano 5 serotypes/strain: denv 3. Bakit endemic pa rin ganun ng case magmutate.
complications? 1, 2, 3,4,5 malaria sa kanila? 4. Nattransfer ba siya 3. May vaccine na ba? Yes.
Pneumonia & transmission: vector logistics problem, security through casual contact-‐ Currently, 2 vaccines have
bloodstream components ng blood: problem, politically unstable No. Kailangan ng broken been released. However,
infection rbc, wbc, plasma, 4. Kung pupunta sa skin or directly sa mucous they are not available in
*H1N1 lang ba? platelets provinces na endemic membrane the Philippines since the
Yes malaria, what would Philippines remains to be
*Gov't program-‐ Kapag kelangan ang you do? Add’l: one of the countries in Asia
orders lng nung patient ay platelet lang, take antimalarial prophylaxis 1-‐ 1. Bakit meron dog collar not yet to have been
pandemic; no sa blood transfusion 2 weeks before sa ibang countrines? for affected by the influenza.
specific program ibabalik daw yung ibang 5. Commonly used identification 4. Effective ba ang
components ng blood sa prophylaxis? Nasa 2. Bakit dito sa Pilipinas vaccine? Not necessarily.
donor, platelets lang powerpoint walang mga dog collar-‐ Since ung virus nga ay
daw yung itatransfer sa 6. Is it deadly? What can walang budget? Haha capable of mutation, it is
patient sabi ni the great cause death? 3. Is there a seminar for possible that the vaccine
maam ngo Yes. Yung complications like animal welfare? -‐Yes can work on a mutated
cerebral malaria, severe 4. Is there a government strain of the subtype but
anemia, etc. & if left untreated program for rabies? -‐Yes not on a new and different
7. Common species yung Rabies Free by 2020.. mutation of the subtype.
found in the Philippines. bale lahat na program na 5. Cause of death in some
falciparum -‐ deadliest, vivax, about rabies cases? Complications may
ovale nakaincorporate na dito arise. The most common
complication is pneumonia.
LEGEND: LEPROSY
• Ab -‐ antibodies
• Ag -‐ antigen
• MDR -‐ multiple drug resistance
• Inf -‐ infected/infection/infectious
• COD -‐ cause of death
• Disc -‐ discovered
• Tx -‐ treatment
• Dx -‐ diagnosis
• G+/-‐ -‐ gram positive/negative
• DM -‐ Diabetes mellitus
• N/V -‐ nausea & vomiting
• ID -‐ intradermal
• IM -‐ intramuscular
• CI -‐ contraindicated
ADD’L TABLES:
PULMONARY TB
RABIES
You might also like
- Im Dude HandoutDocument1 pageIm Dude Handoutapi-535001113No ratings yet
- Microbiology MnemonicsDocument5 pagesMicrobiology MnemonicsFritzel SusbillaNo ratings yet
- Module 6: Dna Viruses: History of Viral Classification and NomenclatureDocument10 pagesModule 6: Dna Viruses: History of Viral Classification and NomenclatureCiara PamonagNo ratings yet
- Virus ClassificationDocument5 pagesVirus ClassificationNUR AIN NADHIRAH SHAMSUL BADRINo ratings yet
- Measles - German Measles - ChickenpoxDocument3 pagesMeasles - German Measles - Chickenpoxd3mooz13No ratings yet
- Lexicon of Parasites and Diseases in Livestock: Including Parasites and Diseases of All Farm and Domestic Animals, Free-Living Wild Fauna, Fishes, Honeybee and Silkworm, and Parasites of Products of Animal OriginFrom EverandLexicon of Parasites and Diseases in Livestock: Including Parasites and Diseases of All Farm and Domestic Animals, Free-Living Wild Fauna, Fishes, Honeybee and Silkworm, and Parasites of Products of Animal OriginNo ratings yet
- VirologyDocument24 pagesVirologyRohama Qubra 279No ratings yet
- Breathless: The Scientific Race to Defeat a Deadly VirusFrom EverandBreathless: The Scientific Race to Defeat a Deadly VirusRating: 4 out of 5 stars4/5 (17)
- 4.paramyxoviridae Henipa (K)Document10 pages4.paramyxoviridae Henipa (K)NatAsyaNo ratings yet
- 3.paramyxoviridae ND (K)Document7 pages3.paramyxoviridae ND (K)NatAsyaNo ratings yet
- RNA and DNA VirusesDocument62 pagesRNA and DNA Viruseseren16jaegerNo ratings yet
- Goku Notes: Viral Hemorrhagic Fevers (Bunyaviruses, Arenaviruses, Filoviruses) - Dra. Ma. Ellery MendezDocument5 pagesGoku Notes: Viral Hemorrhagic Fevers (Bunyaviruses, Arenaviruses, Filoviruses) - Dra. Ma. Ellery MendezRonald BeasleyNo ratings yet
- Paramyxoviridae EditedDocument30 pagesParamyxoviridae EditedstudymedicNo ratings yet
- تجميعة فارماDocument1 pageتجميعة فارماAhmed SobhNo ratings yet
- Reoviruses Picornaviruses: RNA VirusesDocument11 pagesReoviruses Picornaviruses: RNA VirusesHanunNo ratings yet
- Microbial Aspect of Respiratory TrackDocument23 pagesMicrobial Aspect of Respiratory TrackNovi AdriNo ratings yet
- Ssrna Ssrna Dimer Dsrna Ssdna Dsdna: Genome GenomeDocument28 pagesSsrna Ssrna Dimer Dsrna Ssdna Dsdna: Genome GenomeVirgil CendanaNo ratings yet
- Arbo Robo Viruses KMCDocument16 pagesArbo Robo Viruses KMCmaregnrodiNo ratings yet
- Activity 2 Critical ThinkingDocument10 pagesActivity 2 Critical ThinkingBryant Riego IIINo ratings yet
- 3 Kasus, Etiologi, DKKDocument2 pages3 Kasus, Etiologi, DKKmellyNo ratings yet
- Table Virology 1Document28 pagesTable Virology 1Virgil CendanaNo ratings yet
- Viral InfectionDocument35 pagesViral Infectionanushka guptaNo ratings yet
- Pneumonia - Knowledge at AMBOSSDocument3 pagesPneumonia - Knowledge at AMBOSSKC Dela RosaNo ratings yet
- 8 InfectiousDocument113 pages8 InfectiousLeng IlyNo ratings yet
- Tugas Mikrobiologiku Mendekati SeleseDocument5 pagesTugas Mikrobiologiku Mendekati SelesealdaNo ratings yet
- Pneumonia II MicrobesDocument15 pagesPneumonia II MicrobespuniariNo ratings yet
- ViroDocument4 pagesVirolctorres7462antNo ratings yet
- Chemical Composition of VirusesDocument24 pagesChemical Composition of VirusesMohammed Yousif mzori100% (1)
- Addtl Info ViroDocument6 pagesAddtl Info ViroAlondra SagarioNo ratings yet
- PneumoniaDocument41 pagesPneumoniaAli Aborges Jr.No ratings yet
- Familia Subfamilia Género EspecieDocument4 pagesFamilia Subfamilia Género EspecieAdamary MerinoNo ratings yet
- 39 Viral Haemorrhagic Diseases (Edited)Document42 pages39 Viral Haemorrhagic Diseases (Edited)qianyuNo ratings yet
- Microbiology - 17Document5 pagesMicrobiology - 17karmylle andradeNo ratings yet
- Disease Causative Agent Diagnosis Classification/ S&S TreatmentDocument4 pagesDisease Causative Agent Diagnosis Classification/ S&S Treatmentfreya_28No ratings yet
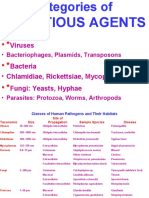
- Infectious Agents: - PrionsDocument45 pagesInfectious Agents: - PrionshilmaNo ratings yet
- All Details About Pneumocystis Carinii Pneumonia (PCP)Document7 pagesAll Details About Pneumocystis Carinii Pneumonia (PCP)NHZANo ratings yet
- IntegumentaryDocument10 pagesIntegumentarysteffiNo ratings yet
- Pneumonia 2018Document63 pagesPneumonia 2018Abraham AnaelyNo ratings yet
- Activity 2 CriticalDocument11 pagesActivity 2 CriticalWILJOHN DE LA CRUZNo ratings yet
- Im Rotation ReviewerDocument2 pagesIm Rotation ReviewerVictoria Eliza InguilloNo ratings yet
- Pneumonia - Spread SheetDocument1 pagePneumonia - Spread SheetRobin KeaneNo ratings yet
- Oncogenic VirusesDocument25 pagesOncogenic VirusesMedicina 19No ratings yet
- Astro, Arena, Bunya, Cali, FiloDocument6 pagesAstro, Arena, Bunya, Cali, FilomyeducationalfilesonlyNo ratings yet
- VirologyDocument40 pagesVirologyKutub SikderNo ratings yet
- Human Virus Families and Their DiseasesDocument1 pageHuman Virus Families and Their DiseasesKate EvangelistaNo ratings yet
- Paramyxovirus LecDocument25 pagesParamyxovirus Lecapi-19969058No ratings yet
- Basic 2021 TanvirDocument11 pagesBasic 2021 TanvirRA TanvirNo ratings yet
- CHNDocument28 pagesCHNVed TiwariNo ratings yet
- ArbovirusesDocument70 pagesArbovirusesRandy BerryNo ratings yet
- DNA Viruses SS Linear Mumps Measles RSV (2) Heparna (HAV Entero 72)Document1 pageDNA Viruses SS Linear Mumps Measles RSV (2) Heparna (HAV Entero 72)Famela Anne GOmez MadambaNo ratings yet
- 1 Methods of Virol ResearchesDocument26 pages1 Methods of Virol ResearchesMann SarwanNo ratings yet
- Community Health NursingDocument4 pagesCommunity Health NursingOnurNo ratings yet
- Mumps VirusDocument13 pagesMumps VirusLara MasriNo ratings yet
- Thesun 2009-04-28 Page09 Swine Flu Spreads To Europe Death Toll RisesDocument1 pageThesun 2009-04-28 Page09 Swine Flu Spreads To Europe Death Toll RisesImpulsive collectorNo ratings yet
- نسخة Virology Pictures for SpotsDocument25 pagesنسخة Virology Pictures for Spotsعبدالله العثمانNo ratings yet
- Virus-Pms - Sistim-2007Document39 pagesVirus-Pms - Sistim-2007ibhrahimNo ratings yet
- Viruses IIDocument55 pagesViruses IIk10 Lớp Dinh DưỡngNo ratings yet
- 4 - PnevmoniiDocument49 pages4 - PnevmoniiPetreNo ratings yet
- Vector Borne DiseasesDocument104 pagesVector Borne Diseasesnugraha a cNo ratings yet
- UV - Vis Spectroscopy: Mjla2015 - Spectrometric Methods 1Document15 pagesUV - Vis Spectroscopy: Mjla2015 - Spectrometric Methods 1Angeli Marie PadillaNo ratings yet
- Elements: Mjlabraham2014 - Nutrition 1Document8 pagesElements: Mjlabraham2014 - Nutrition 1Angeli Marie PadillaNo ratings yet
- Physical Pharmacy: Different Types of SolutionsDocument10 pagesPhysical Pharmacy: Different Types of SolutionsAngeli Marie PadillaNo ratings yet
- BiopharmaceuticsDocument13 pagesBiopharmaceuticsAngeli Marie PadillaNo ratings yet
- Angeli Marie PadillaDocument1 pageAngeli Marie PadillaAngeli Marie PadillaNo ratings yet
- TEAM-a Number of People Who Act Together As A Group, Either in A Sport or in Order To AchieveDocument3 pagesTEAM-a Number of People Who Act Together As A Group, Either in A Sport or in Order To AchieveAngeli Marie PadillaNo ratings yet
- Drugs For Hematologic DisordersDocument35 pagesDrugs For Hematologic DisordersAngeli Marie PadillaNo ratings yet