Professional Documents
Culture Documents
Tailor Pci
Uploaded by
Mathew McCarthyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Tailor Pci
Uploaded by
Mathew McCarthyCopyright:
Available Formats
Research
JAMA | Original Investigation
Effect of Genotype-Guided Oral P2Y12 Inhibitor Selection
vs Conventional Clopidogrel Therapy on Ischemic Outcomes
After Percutaneous Coronary Intervention
The TAILOR-PCI Randomized Clinical Trial
Naveen L. Pereira, MD; Michael E. Farkouh, MD, MSc; Derek So, MD; Ryan Lennon, MS; Nancy Geller, PhD; Verghese Mathew, MD;
Malcolm Bell, MD; Jang-Ho Bae, MD; Myung Ho Jeong, MD; Ivan Chavez, MD; Paul Gordon, MD; J. Dawn Abbott, MD; Charles Cagin, DO;
Linnea Baudhuin, PhD; Yi-Ping Fu, PhD; Shaun G. Goodman, MD, MSc; Ahmed Hasan, MD, PhD; Erin Iturriaga, PhD; Amir Lerman, MD;
Mandeep Sidhu, MD; Jean-Francois Tanguay, MD; Liewei Wang, MD, PhD; Richard Weinshilboum, MD; Robert Welsh, MD;
Yves Rosenberg, MD, MPH; Kent Bailey, PhD; Charanjit Rihal, MD
Editorial page 747
IMPORTANCE After percutaneous coronary intervention (PCI), patients with CYP2C19*2 or *3 Supplemental content
loss-of-function (LOF) variants treated with clopidogrel have increased risk of ischemic
events. Whether genotype-guided selection of oral P2Y12 inhibitor therapy improves CME Quiz at
jamacmelookup.com and CME
ischemic outcomes is unknown.
Questions page 798
OBJECTIVE To determine the effect of a genotype-guided oral P2Y12 inhibitor strategy on
ischemic outcomes in CYP2C19 LOF carriers after PCI.
DESIGN, SETTING, AND PARTICIPANTS Open-label randomized clinical trial of 5302 patients
undergoing PCI for acute coronary syndromes (ACS) or stable coronary artery disease (CAD).
Patients were enrolled at 40 centers in the US, Canada, South Korea, and Mexico from May
2013 through October 2018; final date of follow-up was October 2019.
INTERVENTIONS Patients randomized to the genotype-guided group (n = 2652) underwent
point-of-care genotyping. CYP2C19 LOF carriers were prescribed ticagrelor and noncarriers
clopidogrel. Patients randomized to the conventional group (n = 2650) were prescribed
clopidogrel and underwent genotyping after 12 months.
MAIN OUTCOMES AND MEASURES The primary end point was a composite of cardiovascular
death, myocardial infarction, stroke, stent thrombosis, and severe recurrent ischemia at 12
months. A secondary end point was major or minor bleeding at 12 months. The primary
analysis was in patients with CYP2C19 LOF variants, and secondary analysis included all
randomized patients. The trial had 85% power to detect a minimum hazard ratio of 0.50.
RESULTS Among 5302 patients randomized (median age, 62 years; 25% women), 82% had
ACS and 18% had stable CAD; 94% completed the trial. Of 1849 with CYP2C19 LOF variants,
764 of 903 (85%) assigned to genotype-guided therapy received ticagrelor, and 932 of 946
(99%) assigned to conventional therapy received clopidogrel. The primary end point
occurred in 35 of 903 CYP2C19 LOF carriers (4.0%) in the genotype-guided therapy group
and 54 of 946 (5.9%) in the conventional therapy group at 12 months (hazard ratio [HR],
0.66 [95% CI, 0.43-1.02]; P = .06). None of the 11 prespecified secondary end points showed
significant differences, including major or minor bleeding in CYP2C19 LOF carriers in the
genotype-guided group (1.9%) vs the conventional therapy group (1.6%) at 12 months (HR,
1.22 [95% CI, 0.60-2.51]; P = .58). Among all randomized patients, the primary end point
occurred in 113 of 2641 (4.4%) in the genotype-guided group and 135 of 2635 (5.3%) in the
conventional group (HR, 0.84 [95% CI, 0.65-1.07]; P = .16).
CONCLUSIONS AND RELEVANCE Among CYP2C19 LOF carriers with ACS and stable CAD
undergoing PCI, genotype-guided selection of an oral P2Y12 inhibitor, compared with
conventional clopidogrel therapy without point-of-care genotyping, resulted in no statistically
Author Affiliations: Author
significant difference in a composite end point of cardiovascular death, myocardial infarction, affiliations are listed at the end of this
stroke, stent thrombosis, and severe recurrent ischemia based on the prespecified analysis article.
plan and the treatment effect that the study was powered to detect at 12 months. Corresponding Author: Naveen L.
Pereira, MD, Department of
TRIAL REGISTRATION ClinicalTrials.gov Identifier: NCT01742117 Cardiovascular Medicine, Mayo Clinic,
200 First Street SW, Rochester, MN
JAMA. 2020;324(8):761-771. doi:10.1001/jama.2020.12443 55905 (pereira.naveen@mayo.edu).
(Reprinted) 761
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Rochester User on 08/26/2020
Research Original Investigation Effect of Genotype-Guided Oral P2Y12 Inhibitor Selection vs Clopidogrel on Ischemic Outcomes After PCI
C
lopidogrel is the most widely prescribed oral inhibi-
tors of the platelet adenosine diphosphate P2Y12 Key Points
receptor (P2Y12).1 A drug label “black box warning”
Question Does CYP2C19 genotype–guided prescription of oral
cautions against its use in poor metabolizers of hepatic cyto- P2Y12 inhibitor therapy after percutaneous coronary intervention
chrome P450 enzyme CYP2C19 because it is a prodrug and (PCI) improve ischemic outcomes in patients with acute coronary
needs to be biotransformed to an active metabolite by syndromes and stable coronary artery disease?
CYP2C19.2 The most common loss-of-function (LOF) alleles,
Findings In this randomized clinical trial that included 5302
which account for most patients with reduced metabolizer patients undergoing PCI and included 1849 patients with CYP2C19
status, are CYP2C19*2 and CYP2C19*3.3 Clopidogrel-treated loss-of-function alleles in the primary analysis, genotype-guided
carriers of CYP2C19 LOF alleles as compared with noncarriers selection of oral P2Y12 inhibitor therapy, compared with
have a higher incidence of ischemic events.4 Despite this conventional therapy using clopidogrel, resulted in no significant
association, patients are prescribed clopidogrel without difference in a composite end point of cardiovascular death,
myocardial infarction, stroke, stent thrombosis, or severe
knowledge of CYP2C19 genotype because of lack of prospec-
recurrent ischemia at 12 months (4.0% vs 5.9%, respectively;
tive evidence demonstrating the clinical utility of genetic hazard ratio, 0.66).
testing, ie, whether changing clopidogrel to an alternative
oral P2Y12 inhibitor based on CYP2C19 LOF genotype Meaning Among patients with CYP2C19 loss-of-function alleles
who underwent PCI, genotype-guided selection of an oral P2Y12
improves clinical outcomes.2 Therefore, current guidelines
inhibitor, compared with conventional clopidogrel therapy, did not
do not recommend genetic testing when prescribing significantly reduce ischemic events based on the treatment effect
clopidogrel.2 TAILOR PCI was designed and conducted as a that the study was powered to detect at 12 months.
pragmatic, open-label, international, multicenter, random-
ized clinical trial testing the hypothesis that CYP2C19
genotype–guided use of oral P2Y12 inhibitors as compared patients. The choice of stent, loading dose of oral P2Y12
with non–genotype-guided conventional clopidogrel therapy inhibitors, access site, and choice of lesions to treat were at
significantly reduces ischemic events in CYP2C19 LOF variant the discretion of the treating physician. Patients were ran-
carriers after percutaneous coronary intervention (PCI). domized to either a genotype-guided therapy group using
point-of-care genotyping or conventional therapy group
without prospective genotyping. Point-of-care genotyping
was performed using Spartan Rx (Spartan Bioscience). In the
Methods genotype-guided group, those identified as hav ing
Trial Design CYP2C19*2 or *3 LOF alleles (CYP2C19 LOF carriers) were pre-
The trial design has been published.1,5 The trial protocol scribed ticagrelor for maintenance therapy, and noncarriers
(Supplement 1) and trial protocol amendments (Supple- or those with inconclusive results were prescribed clopido-
ment 2) were approved by the ethics boards of participating grel; patients randomized to the conventional therapy group
sites. An independent National Heart, Lung, and Blood Insti- were all prescribed clopidogrel according to drug label
tute–appointed data and safety monitoring board was respon- instructions. Prasugrel was recommended as an alternative
sible for overseeing the conduct and safety of the trial. All par- for patients who did not tolerate ticagrelor. All patients
ticipants provided written informed consent. received aspirin (81 mg).
All patients provided blood samples at enrollment that
Patients were analyzed after 12 months post-PCI by laboratory-based
Patients 18 years and older with acute coronary syndromes genotyping using TaqMan (Applied Biosystems), to enable
(ACS) or stable coronary artery disease (CAD) who under- uniform comparison of CYP2C19 LOF carriers in both groups.
went PCI with planned 12 months of dual antiplatelet therapy A difference in ischemic outcomes in patients who were
were eligible. A complete list of exclusion criteria is provided CYP2C19 LOF noncarriers receiving clopidogrel in the
in eTable 1 in Supplement 3. Race/ethnicity was collected be- genotype-guided or conventional therapy groups was not
cause of the genetic nature of the study, its international en- expected. Therefore, the primary analysis was undertaken in
rollment, and as required by the National Institutes of Health. only those patients who had CYP2C19 LOF variants identified
Race/ethnicity categories were fixed prior to study initiation by laboratory-based genotyping who were randomized to the
and were collected from the patient’s medical record. Pa- genotype-guided or conventional therapy group. Patients in
tients were enrolled at 40 centers in the US, Canada, South the conventional group could not undergo point-of-care
Korea, and Mexico from May 29, 2013, to October 31, 2018, with genotyping to identify CYP2C19 LOF carriers, as they would
follow-up completed on October 31, 2019. not be able to continue clopidogrel and would have to be pre-
scribed alternative P2Y12 therapy because of the black box
Randomization and Interventions warning in the drug labeling information, therefore not
Patients were randomized on a 1:1 ratio stratified by age allowing a randomized comparison.
group, sex, site, and CAD presentation using real-time
dynamic allocation through Medidata Balance versions End Points
2013.3.0-2018.4.1 (Medidata). Randomization took place Study-related events were assessed at hospital discharge
within 72 hours after PCI and less than 24 hours in 87% of by the study coordinator and at 1 month, 6 months, and 12
762 JAMA August 25, 2020 Volume 324, Number 8 (Reprinted) jama.com
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Rochester User on 08/26/2020
Effect of Genotype-Guided Oral P2Y12 Inhibitor Selection vs Clopidogrel on Ischemic Outcomes After PCI Original Investigation Research
months after PCI by telephone. If patients could not be ing results were not used to determine inclusion in the pri-
reached by telephone after multiple attempts, the site coor- mary analysis, to maintain uniformity in comparison of
dinator conducted a medical record review to assess follow- results between the 2 randomized groups. The “all random-
up. All cardiovascular-related end points and hospitaliza- ized” cohort included randomized patients regardless of
tions were reviewed and adjudicated by an independent laboratory-based genotyping results. The per-protocol
committee blinded to study groups and P2Y12 inhibitor cohort included patients from the primary analysis cohort
received by the patient. Only study-related events con- meeting all inclusion and exclusion criteria whose first dose
firmed by the adjudication committee to be end points were of maintenance therapy was concordant with protocol direc-
included in the analysis. tion. If the null hypothesis of the primary analysis was
The primary outcome was the composite of cardiovascu- rejected, a complementary analysis of the primary end point
lar death, myocardial infarction, stroke, definite or probable in noncarriers was prespecified to estimate the effect of
stent thrombosis, and severe recurrent ischemia at 12 knowledge of genotype among noncarriers receiving clopi-
months after index PCI based on standard definitions out- dogrel. Patients were analyzed according to their random-
lined in the eMethods in Supplement 3. Secondary end ized treatment assignment, regardless of medication
points were major or minor bleeding as defined by the received, unless otherwise noted.
Thrombolysis in Myocardial Infarction (TIMI) criteria6; the Event rates at 12 months after PCI were calculated using
individual components of the primary end point; all-cause Kaplan-Meier estimates. Patients who withdrew or who were
mortality; major bleeding; and bleeding end points of lost to follow-up were treated as censored at the date of last
increasing severity defined by Bleeding Academic Research contact. Patients completing follow-up through the sched-
Consortium (BARC) criteria7 (class 2,3 or 5; class 3 or 5; and uled 12-month follow-up visit were censored at 365 days after
class 5).6 All time-to-event end points were defined with index PCI. A Cox proportional hazards model was used to
time of randomization as time zero. estimate the HR for time to first occurrence of the primary
end point, adjusted for sex, age group, and CAD presentation
Statistical Analysis and with site included as a random effect. A 2-sided likeli-
Initial sample size calculations were conducted based on hood ratio test was used to calculate the P value. Hazard
assumed 12-month event rates of the primary end point of ratios are reported with 95% CIs. The same model was used
12% in the CYP2C19 LOF carriers receiving clopidogrel and to analyze time to major or minor bleeding in the primary
8% in LOF carriers receiving ticagrelor8 (minimum detectable analysis cohort as the primary adverse event analysis. The
hazard ratio [HR], 0.65 at 80% power). These assumptions proportional hazards assumption was investigated by plot-
resulted in a required sample size of 1694 LOF carriers. To ting scaled Schoenfeld residuals vs follow-up time and by
account for a potential dropout rate of 5%, enrollment of testing the interaction between treatment groups and the
1784 LOF carriers was planned. Assuming a prevalence of logarithm of follow-up time. When the assumption was vio-
30% of LOF carriers, a total trial enrollment of 5945 was lated, a post hoc analysis was undertaken to estimate the
planned. When enrollment from Korean sites was subse- treatment effect over different segments of the follow-up
quently added, the total trial enrollment was reduced to period. The time segments were not prespecified and were
5270, assuming 1015 patients would be enrolled from Korea chosen based on clinical importance of these periods. A Cox
with a 50% prevalence of LOF carriers. When the trial had proportional hazards model was used to estimate the time-
enrolled approximately 3800 patients, the Operations and specific treatment effects adjusting for the same covariates as
Executive committees approved a reassessment of power the primary analysis, with time-dependent indicators for
because of the overall low event rates observed in the study. genotype-guided treatment. Four prespecified sensitivity
The committees approved a revision that retained the a priori analyses were conducted, including per-protocol, recurrent
sample size (5270), under the assumption of event rates of events, time-dependent medication, and multiple imputa-
6% and 3%, respectively (minimum detectable HR, 0.50), tion for missing laboratory-based genotyping results analyses
with 85% power. An HR of 0.50 was selected to demonstrate (see eMethods in Supplement 3 for details). Subgroup analy-
a clinically important absolute risk reduction in the context ses were conducted by adding a main effect for the subgroup
of the interim observed overall event rate being 4.5% and of interest in the primary analysis model and an interaction
based on the effect size observed in clopidogrel-treated term between the subgroup indicator and the treatment
CYP2C19 LOF carriers in prior observational studies with low group. The P value for the interaction term estimate was used
event rates.9-11 The proposal was additionally reviewed and to test for the presence of a treatment interaction between
approved by the data and safety monitoring board and the the subgroups. All hypotheses tests were 2-sided with a .05
National Heart, Lung, and Blood Institute. The overall type I type I error rate. Because of the potential for type 1 error due
error rate was set at .05, with a plan for 3 interim analyses to lack of adjustment for multiple comparisons, findings
using stopping boundaries by Peto and Haybittle12; thus, the from the analyses of secondary end points and the subgroup
final significance test of the null hypothesis uses P < .0495 as analyses should be interpreted as exploratory.
its rejection region. All analyses were conducted with SAS software, version
The primary analysis cohort included randomized 9.4 (SAS Institute Inc). Additional details of the statistical analy-
patients from both groups identified as CYP2C19 LOF carri- ses, including definition of the noncarrier analysis cohort, are
ers by the laboratory-based platform. Point-of-care genotyp- reported in the eMethods in Supplement 3.
jama.com (Reprinted) JAMA August 25, 2020 Volume 324, Number 8 763
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Rochester User on 08/26/2020
Research Original Investigation Effect of Genotype-Guided Oral P2Y12 Inhibitor Selection vs Clopidogrel on Ischemic Outcomes After PCI
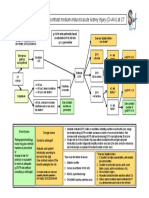
Figure 1. Study Flow for the TAILOR-PCI Randomized Clinical Trial
5302 Patients randomizeda
2652 Randomized to receive 2650 Randomized to receive
genotype-guided therapy conventional therapy
2641 Received guided therapy 2635 Received conventional
as randomized therapy as randomized
11 Did not receive guided therapy 15 Did not receive conventional
as randomized therapy as randomized
8 Informed consent issue 11 Informed consent issue
2 No PCI/failed PCI 3 No PCI/failed PCI
1 Duplicate randomization 1 Duplicate randomization
Patients randomized in spite of the
presence of exclusion criteria were
2641 Eligible for analysis 2635 Eligible for analysis still eligible for analysis. In the 5276
patients eligible for analysis, 5007
(94.9%) either completed follow-up
1738 Excluded 1689 Excluded or died during follow-up, including
1632 Identified as CYP2C19 LOF 1600 Identified as CYP2C19 LOF
1760 (95.1%) in the primary analysis
noncarriers by TaqMan noncarriers by TaqMan
1561 Completed follow up 1519 Completed follow up cohort. The 269 who withdrew or
71 Did not complete follow-up 81 Did not complete follow-up were lost to follow-up had a mean
17 Died 17 Died follow-up time of 3.4 months. Of the
39 Lost to follow-up 50 Lost to follow-up 195 with laboratory-based
15 Withdrew 14 Withdrew genotyping results not available, the
106 No TaqMan results available 89 No TaqMan results available reasons were sample not received at
68 Completed follow-up 62 Completed follow-up biospecimen processing facility
38 Did not complete follow-up 27 Did not complete follow-up (n = 66), low-quality sample not
3 Died 0 Died
suitable for analysis (n = 60), no
6 Lost to follow-up 5 Lost to follow-up
29 Withdrew 22 Withdrew index sample taken (n = 59),
withdrew consent for use of DNA
(n = 10). LOF indicates loss of
903 Identified as CYP2C19 LOF 946 Identified as CYP2C19 LOF function; PCI, percutaneous coronary
carriers by TaqMan carriers by TaqMan intervention.
847 Completed follow-up 897 Completed follow-up a
Patients screened for approach but
56 Did not complete follow-up 49 Did not complete follow-up
6 Died 10 Died who did not provide consent were
29 Lost to follow-up 25 Lost to follow-up not recorded.
21 Withdrew 14 Withdrew b
eTable 2 in the Supplement details
the point-of-care genotyping results
and the initial antiplatelet therapy
903 CYP2C19 LOF carriers included 946 CYP2C19 LOF carriers included according to treatment group and
in primary analysisb in primary analysisb
laboratory-based genotyping
results.
Supplement 3). Point-of-care genotyping results were avail-
Results able within 24 hours of randomization for 99% of patients.
Among the CYP2C19 LOF carriers, 85% in the genotype-
Trial Patients guided therapy group received ticagrelor and 15% received
A total of 5302 patients were enrolled (Figure 1; eTable 2 in clopidogrel as initial oral P2Y12 inhibitor therapy after ran-
Supplement 3); of these, 26 patients were excluded from all domization; 99% in the conventional therapy group received
analyses (19 improperly consented, 5 did not have PCI or failed clopidogrel. The primary reasons that LOF carriers in the
PCI, 2 were duplicate randomizations). This resulted in inclu- genotype-guided group received clopidogrel are inconclusive
sion of 5276 patients, with 2641 patients in the genotype- or unavailable point-of-care genotyping results and physician
guided therapy group and 2635 in the conventional therapy or patient preference (eTable 4 in Supplement 3). During the
group. Laboratory-based genotyping results could not be ob- 12-month follow-up period, among the CYP2C19 LOF carriers
tained for 195 patients (inadequate or unavailable DNA sample); the percentage of days receiving protocol oral P2Y12 therapy
hence, these patients were not included in the primary analy- was 85% in the genotype-guided group and 97% in the con-
sis, resulting in 903 and 946 CYP2C19 LOF carriers in the geno- ventional group. Reasons for switching or discontinuing
type-guided and conventional groups, respectively. assigned oral P2Y12 therapy after randomization are reported
Baseline patient characteristics were balanced between in eTable 5 in Supplement 3. Five thousand seven patients
the 2 overall randomized groups and between the subgroups (95%) had complete follow-up or died during the study, with
of CYP2C19 LOF carriers (Table 1) included in the primary the remaining 269 either withdrawing before 12 months or
analysis. The concordance between the point-of-care geno- being lost to follow-up (Figure 1). The median follow-up time
typing and laboratory-based genotyping was 99% (eTable 3 in was 364 days.
764 JAMA August 25, 2020 Volume 324, Number 8 (Reprinted) jama.com
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Rochester User on 08/26/2020
Effect of Genotype-Guided Oral P2Y12 Inhibitor Selection vs Clopidogrel on Ischemic Outcomes After PCI Original Investigation Research
Table 1. Baseline Patient and Procedural Characteristics
No. (%)
LOF allele (CYP2C19 *2/*3) carriers All randomized patients
Genotype-guided Conventional Genotype-guided Conventional
therapy therapy therapy therapy
(n = 903) (n = 946) (n = 2641) (n = 2635)
Patient characteristics
Age, y
Median (range) 62 (26-95) 62 (21-93) 62 (26-95) 62 (21-93)
<50 120 (13) 123 (13) 327 (12) 328 (12)
50-59 260 (29) 280 (30) 737 (28) 730 (28)
60-69 276 (31) 310 (33) 867 (33) 863 (33)
70-74 115 (13) 104 (11) 333 (13) 334 (13)
75-79 73 (8) 80 (8) 216 (8) 218 (8)
≥80 59 (7) 49 (5) 161 (6) 162 (6)
Sex
Men 676 (75) 728 (77) 1993 (75) 1990 (76)
Women 227 (25) 218 (23) 648 (25) 645 (24)
Race n = 884 n = 927 n = 2578 n = 2588
White 442 (50) 462 (50) 1750 (68) 1754 (68)
East Asian 345 (39) 363 (39) 595 (23) 592 (23)
South Asian 62 (7) 66 (7) 116 (4) 120 (5)
African American 17 (2) 20 (2) 57 (2) 67 (3)
Othera 18 (2) 16 (2) 60 (2) 55 (2)
Hispanic or Latinx ethnicity 14/884 (2) 15/927 (2) 78/2578 (3) 70/2588 (3)
Country of enrollment
US 345 (38) 380 (40) 1359 (51) 1358 (52)
South Korea 381 (42) 397 (42) 654 (25) 650 (25)
Canada 168 (19) 161 (17) 577 (22) 580 (22)
Mexico 9 (1) 8 (1) 51 (2) 47 (2)
BMI, median (IQR)b 26.9 (24.3-30.9) 27.0 (24.0-30.6) 27.9 (24.9-31.8) 28.1 (24.8-31.9)
Comorbidities
Hypertension 531 (59) 575 (61) 1636 (62) 1667 (63)
Dyslipidemia 414 (46) 416 (44) 1363 (52) 1384 (53)
Diabetes 253 (28) 257 (27) 733 (28) 695 (26)
Heart failure 107 (12) 105 (11) 225 (9) 219 (8)
Peripheral artery disease 20 (2) 18 (2) 75 (3) 61 (2)
Risk factors
Family history of CAD 279 (31) 303 (32) 995 (38) 1005 (38)
Cigarette use 228 (25) 239 (25) 648 (25) 637 (24)
History of PCI 174 (19) 188 (20) 612 (23) 612 (23)
History of MI (excluding 112 (12) 111 (12) 387 (15) 371 (14)
index event)
History of CABG surgery 53 (6) 53 (6) 196 (7) 188 (7)
Stroke/TIA 28 (3) 27 (3) 72 (3) 76 (3)
CAD presentation
Stable CAD 127 (14) 148 (16) 488 (18) 484 (18)
ACS: unstable angina 336 (37) 335 (35) 830 (31) 792 (30)
ACS: non-STEMI 250 (28) 263 (28) 749 (28) 785 (30)
ACS: STEMI 190 (21) 200 (21) 574 (22) 574 (22)
Pre-PCI LVEF, 60 (53-66) 60 (53-67) 60 (51-65) 59 (52-65)
median (IQR), %
Kidney function, eGFR,
mL/minc
<60 100 (12) 94 (11) 243 (10) 296 (12)
≥60 738 (88) 773 (89) 2171 (90) 2105 (88)
(continued)
jama.com (Reprinted) JAMA August 25, 2020 Volume 324, Number 8 765
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Rochester User on 08/26/2020
Research Original Investigation Effect of Genotype-Guided Oral P2Y12 Inhibitor Selection vs Clopidogrel on Ischemic Outcomes After PCI
Table 1. Baseline Patient and Procedural Characteristics (continued)
No. (%)
LOF allele (CYP2C19 *2/*3) carriers All randomized patients
Genotype-guided Conventional Genotype-guided Conventional
therapy therapy therapy therapy
(n = 903) (n = 946) (n = 2641) (n = 2635)
Multivessel disease 379 (42) 343 (36) 1120 (43) 1099 (42)
Procedural characteristics
PCI to randomization, 4.5 (1.1-19.7) 4.8 (1.1-20.1) 7.0 (1.9-20.7) 8.3 (1.9-20.6)
median (IQR), h
Antithrombin use
Unfractionated heparin 775 (86) 828 (88) 2255 (86) 2262 (86)
Bivalirudin 91 (10) 96 (10) 340 (13) 329 (13)
Low-molecular-weight 38 (4) 47 (5) 130 (5) 148 (6)
heparin
GpIIb-IIIa inhibitor use 55 (6) 88 (9) 264 (10) 270 (10)
Loading medication
Clopidogrel 606 (67) 622 (66) 1786 (68) 1792 (68)
Ticagrelor 219 (24) 238 (25) 587 (22) 620 (24) Abbreviations: ACS, acute coronary
syndrome; BMI, body mass index;
Prasugrel 19 (2) 23 (2) 74 (3) 53 (2)
CABG, coronary artery bypass graft;
Ticlopidine 1 (<1) 1 (<1) 1 (<1) 1 (<1) CAD, coronary artery disease;
Other 4 (<1) 2 (<1) 8 (<1) 5 (<1) eGFR, estimated glomerular filtration
rate; GpIIb-IIIa, glycoprotein IIb/IIIa
None 52 (6) 60 (6) 168 (6) 160 (6)
complex; IQR, interquartile range;
No. of stents placed, 1.0 (1.0-2.0) 1.0 (1.0-2.0) 1.0 (1.0-2.0) 1.0 (1.0-2.0) LOF, loss of function; LVEF, left
median (IQR) ventricular ejection fraction;
Artery treated MI, myocardial infarction;
Left anterior descending 456 (51) 500 (53) 1356 (52) 1355 (52) PCI, percutaneous coronary
intervention; STEMI, ST-segment
Right coronary 312 (35) 329 (35) 935 (36) 931 (35)
elevation myocardial infarction;
Left circumflex 239 (26) 253 (27) 683 (26) 727 (28) TIA, transient ischemic attack.
a
Left main coronary 32 (4) 21 (2) 71 (3) 56 (2) Other race consists of 130 patients
First antiplatelet after who indicated “other” and 19 who
randomization indicated “Native American Indian
Clopidogrel 132 (15) 932 (99) 1790 (68) 2586 (99) or Native Alaskan.”
b
Calculated as weight in kilograms
Ticagrelor 764 (85) 9 (1) 822 (31) 35 (1)
divided by height in meters
Prasugrel 4 (<1) 2 (<1) 9 (<1) 3 (<1) squared.
Cilostazol 1 (<1) 0 1 (<1) 0 c
eGFR calculated by Modification of
Time from PCI to first 21.7 (10.1-26.1) 21.9 (17.7-25.0) 21.9 (17.2-28.5) 21.9 (17.8-27.9) Diet in Renal Disease equation.
postrandomization Equation = 186*([serum creatinine]^
antiplatelet therapy, (–1.154))*([age, y]^(–0.203))*
median (IQR), h
(0.742^[female])*(1.21^[black]).
Primary End Point 2 treatment groups, including the other bleeding-related end
The primary end point occurred in 35 (4.0%) of the genotype- points (Table 2).
guided therapy group CYP2C19 LOF carriers vs 54 (5.9%) of the
conventional therapy group CYP2C19 LOF carriers at 12 months Prespecified Sensitivity Analyses of the Primary Outcome
(Table 2 and Figure 2A). The absolute difference of 1.8% (5.85% The robustness of the primary analysis was investigated by sev-
vs 4.03%) in primary outcomes between the 2 groups in the eral prespecified sensitivity analyses. An analysis allowing for
CYP2C19 LOF carriers did not meet the predetermined level multiple events per patient favored the use of genotype-
of statistical significance for superiority (HR, 0.66 [95% CI, guided as compared with conventional therapy in CYP2C19 LOF
0.43-1.02]; P = .06). carriers (HR, 0.60 [95% CI, 0.41-0.89]; P = .01). Using mul-
tiple imputation analysis for patients excluded from the pri-
Secondary End Points mary analysis because of missing laboratory-based genotyp-
The adverse event end point (TIMI major or minor bleeding) ing results, the estimated HR was similar to the primary analysis
was observed in 30 patients in the primary analysis cohort with results (HR, 0.68 [95% CI, 0.45-1.04]). To address the 15% lack
no significant difference between the genotype-guided therapy of adherence to ticagrelor in the genotype-guided CYP2C19 LOF
group (16 [1.9%]) and the conventional therapy group carriers, time-dependent variables were used to model ac-
(14 [1.6%]) CYP2C19 LOF carriers at 12 months (HR, 1.22 [95% tual medication usage over time in the CYP2C19 LOF carriers
CI, 0.60-2.51]) (Table 2 and Figure 2B). None of the other sec- rather than treatment groups; the HR for ticagrelor vs clopi-
ondary end points were significantly different between the dogrel was 0.69 (95% CI, 0.44-1.10).
766 JAMA August 25, 2020 Volume 324, Number 8 (Reprinted) jama.com
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Rochester User on 08/26/2020
Effect of Genotype-Guided Oral P2Y12 Inhibitor Selection vs Clopidogrel on Ischemic Outcomes After PCI Original Investigation Research
Table 2. Primary and Secondary End Points in CYP2C19 Loss-of-Function Allele Carriers
No. (%)
Genotype-guided Conventional Difference in 12-mo HR for genotype-guided
therapy therapy event rates, therapy
(N = 903) (N = 946) % (95% CI)a (95% CI)b P valueb
Primary end point
CV death, MI, stroke, severe recurrent 35 (4.0) 54 (5.9) −1.8 (−3.9 to 0.1) 0.66 (0.43 to 1.02) .06
ischemia, stent thrombosis
Secondary end points
Severe recurrent ischemia 19 (2.2) 29 (3.2) −1.0 (−2.6 to 0.5) 0.68 (0.38 to 1.22) .19
BARC bleeding
2,3,5c,d 26 (3.0) 16 (1.8) 1.3 (−0.1 to 2.7) 1.72 (0.92 to 3.20) .08
3,5c,d 17 (2.0) 14 (1.5) 0.5 (−0.8 to 1.8) 1.27 (0.63 to 2.59) .50
TIMI major or minor bleeding (primary 16 (1.9) 14 (1.6) 0.3 (−0.9 to 1.6) 1.22 (0.60 to 2.51) .58
adverse events end point)
Myocardial infarction 11 (1.3) 14 (1.5) −0.3 (−1.3 to 0.8) 0.82 (0.37 to 1.81) .62
Major bleeding 11 (1.3) 11 (1.2) 0.1 (−1.0 to 1.1) 1.05 (0.45 to 2.44) .90
Death from any cause 6 (0.7) 10 (1.1) −0.4 (−1.2 to 0.5) 0.56 (0.20 to 1.54) .25
CV death 4 (0.5) 8 (0.9) −0.4 (−1.2 to 0.4) 0.49 (0.15 to 1.64) .24
Stent thrombosis 2 (0.2) 8 (0.9) −0.6 (−1.4 to 0.0) 0.25 (0.05 to 1.18) .05
Minor bleeding 5 (0.6) 3 (0.3) 0.2 (−0.3 to 0.9) 2.27 (0.57 to 9.08) .23
Stroke 2 (0.2) 4 (0.4) −0.2 (−0.8 to 0.3) 0.51 (0.09 to 2.79) .42
c
Abbreviations: BARC, Bleeding Academic Research Consortium; BARC 5 results not shown, as there are were no fatal bleeds.
CV, cardiovascular; HR, hazard ratio; MI, myocardial infarction; d
BARC is a classification system for bleeding events categorizing bleeds into
TIMI, Thrombolysis in Myocardial Infarction. levels of severity, with higher numbers indicating greater severity. Class 2 are
a
Confidence intervals for differences in Kaplan-Meier rates were estimated by generally overt bleeds requiring medical intervention or evaluation but with
bootstrapping. minimal blood loss (<3-g/dL decrease in hemoglobin level); class 3 is generally
b
Hazard ratios, confidence intervals, and P values are from Cox proportional more serious (either in amount of bleeding or location of bleed); class 4 is
hazards regression models adjusting for age, sex, coronary artery disease bleeding related to coronary artery bypass graft surgery; class 5 is fatal
presentation, and site (factors used for stratified randomization). bleeding. More precise descriptions can be found in Mehran et al.7
Subgroup and Additional Analyses ondary end point analyses in the noncarrier cohort are de-
The primary outcome was also evaluated in 11 prespecified sub- scribed in eTable 8 and eFigures 5 and 6 in Supplement 3.
groups in CYP2C19 LOF carriers, with no significant sub-
group interactions detected (Figure 3). Post Hoc Analysis of the Primary Outcome
When patients in the per-protocol cohort in the genotype- The test of the proportional hazards assumption was signifi-
guided therapy (n = 815) and conventional therapy (n = 930) cant (P = .03), suggesting that the assumption may not hold;
groups were analyzed, results similar to those from the pri- this was further supported by graphical displays (eFigure 7 in
mary analysis cohort were observed (HR, 0.68 [95% CI, 0.44- Supplement 3). Therefore, a post hoc analysis was performed
1.05]) (eTable 6 and eFigure 1 in Supplement 3). Results of that demonstrated an estimated HR for the CYP2C19 LOF geno-
analysis for TIMI bleeding in the per-protocol cohort were con- type-guided therapy group as compared with the conven-
sistent with those in the primary analysis (HR, 1.29 [95% CI, tional therapy group of 0.21 (95% CI, 0.08-0.54; P = .001) at
0.63-1.84]) (eTable 6 and eFigure 2 in Supplement 3). How- 0 to 3 months’ follow-up, 0.78 (95% CI, 0.38-1.61; P = .50) at 3
ever, BARC 2,3,5 bleeding in the per-protocol genotype- to 6 months’ follow-up, and 1.44 (95% CI, 0.69-3.03; P = .33)
guided group (3.3%) in this study was increased compared with at 6 to 12 months’ follow-up.
that in the per-protocol conventional therapy group (1.7%) (HR,
1.96 [95% CI, 1.04-3.71]; P = .03) (eTable 6 in Supplement 3).
When examined in the 2 overall randomized groups
(genotype-guided vs conventional therapy), the primary end
Discussion
point was not significantly different. There were 113 (4.4%) pri- Among CYP2C19 LOF carriers with ACS and stable CAD who
mary events in the 2641 genotype-guided group and 135 (5.3%) underwent PCI, genotype-guided oral P2Y12 inhibitor therapy,
primary events in the 2635 conventional group (HR, 0.84 [95% compared with conventional clopidogrel therapy without
CI, 0.65-1.07]; P = .16) (eTable 7 and eFigure 3 in Supple- point-of-care genotyping, resulted in no significant differ-
ment 3). Similarly, in the all randomized cohort there was no ence in a composite end point of cardiovascular death, myo-
significant difference in TIMI major/minor bleeding episodes cardial infarction, stroke, stent thrombosis, and severe recur-
in the overall genotype-guided group (1.4%) as compared with rent ischemia at 12 months. These results should be interpreted
the conventional group (1.2%) (HR, 1.13 [95% CI, 0.70-1.84]) in the context of the treatment effect (50% reduction in ische-
(eTable 7 and eFigure 4 in Supplement 3). The primary and sec- mic events) that the study was powered to detect based on the
jama.com (Reprinted) JAMA August 25, 2020 Volume 324, Number 8 767
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Rochester User on 08/26/2020
Research Original Investigation Effect of Genotype-Guided Oral P2Y12 Inhibitor Selection vs Clopidogrel on Ischemic Outcomes After PCI
Figure 2. Event Rates in the Primary Analysis Cohort
A CV death, MI, stroke, stent thrombosis, or SRI
8
Adjusted HR, 0.66 (95% CI, 0.43-1.02)
Conventional therapy
stent thrombosis, or SRI, %
6
CV death, MI, stroke,
Genotype-guided therapy
2
0
0 45 90 135 180 225 270 315 360
Days from randomization
No. at risk
Genotype-guided therapy 903 875 870 863 854 838 833 824 556
Conventional therapy 946 906 898 894 878 867 864 859 604
B TIMI major or minor bleeding A, Kaplan-Meier estimated event
rates in the 2 treatment groups in the
4 primary analysis cohort of CYP2C19
Adjusted HR, 1.22 (95% CI, 0.60-2.51) loss-of-function carriers for the
TIMI major or minor bleeding, %
primary end point of time to
3 cardiovascular (CV)–related death,
myocardial infarction (MI), stroke,
stent thrombosis, or severe recurrent
Genotype-guided therapy
2 ischemia (SRI). B, Kaplan-Meier
estimated event rates for the primary
adverse event end point of
Conventional therapy Thrombolysis in Myocardial Infarction
1
(TIMI) major or minor bleeding in the
primary analysis cohort. The median
observation time for the
0 genotype-guided therapy group was
0 45 90 135 180 225 270 315 360
Days from randomization 364 days (interquartile range,
No. at risk 360-365) and for the conventional
Genotype-guided therapy 903 876 867 866 864 847 844 836 560 therapy group was 364 days
Conventional therapy 946 916 911 910 901 890 888 887 622 (interquartile range, 353-365).
HR indicates hazard ratio.
prespecified analysis plan. This study is the first clinical trial event rate that ranged from 9.8% to 11.7%.15 In the current study
to our knowledge to prospectively address the potential util- a lower HR of 0.5 was selected that was greater than that when
ity of genotype-guided oral P2Y12 inhibitor therapy as com- using ticagrelor for all patients, irrespective of genotype sta-
pared with conventional therapy. tus and based on the large effect size of the CYP2C19 geno-
The advent of point-of-care genotyping technology to per- type noted in other observational studies with low event
sonalize P2Y12 therapy, as shown in the RAPID GENE study, rates.9-11 The trial’s primary results did not meet the predeter-
provides proof of concept to apply the technology early after mined level of statistical significance. The potential effect of
PCI.13 Time-to-first-event analysis, which was the analysis of a precision medicine approach may be more important early
the primary end point of this trial, does not account for recur- after PCI, as suggested in the post hoc analysis that demon-
rent events that can occur during the follow-up period. Mea- strated the potential benefit of genotype-guided oral P2Y12 in-
suring the total burden of recurrent events in a study popula- hibitor therapy in the first 3 months after PCI, and may ques-
tion is reflective of overall morbidity, and studying the effect tion the 12-month duration of follow-up in this trial to
of an intervention such as genotype-guided antiplatelet demonstrate the efficacy of such an approach.
therapy, as was done in a prespecified analyses in this trial, on All patients in the conventional therapy group in this trial
cumulative ischemic end points is important.14 were assigned clopidogrel, specifically to provide guidance to
As in other post-PCI trials using newer-generation drug- the medical practitioner regarding the utility of genetic test-
eluting stents, the primary event rate in this trial was much ing when prescribing clopidogrel. The relevance and impor-
lower than the event rate assumed when the trial was ini- tance of this approach is demonstrated by the use of clopido-
tially designed, necessitating a recalculation of power. The use grel in 44% to 72%16 of patients after PCI and in up to 51% to
of ticagrelor as compared with clopidogrel without a genotyp- 70%17 of patients with ACS.18,19 Prescription data from the
ing strategy in the PLATO trial decreased ischemic events (HR, OptumLabs Data Warehouse, a large national administrative
0.84) in 18 624 patients with ACS, with an overall ischemic claims database that includes longitudinal health data of more
768 JAMA August 25, 2020 Volume 324, Number 8 (Reprinted) jama.com
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Rochester User on 08/26/2020
Effect of Genotype-Guided Oral P2Y12 Inhibitor Selection vs Clopidogrel on Ischemic Outcomes After PCI Original Investigation Research
Figure 3. Subgroup Analyses of the Primary Outcome
No. of events/total (%)
Genotype-guided Conventional Absolute HR Favors Favors P value for
Source therapy therapy difference, % (95% CI) genotype-guided conventional interaction
Hospital presentation .62
Stable CAD 4/127 (3.3) 10/148 (6.8) –3.5 0.47 (0.15-1.49)
Unstable angina/non-STEMI 24/586 (4.2) 31/598 (5.3) –1.0 0.78 (0.46-1.33)
STEMI 7/190 (3.8) 13/200 (6.8) –3.0 0.53 (0.21-1.32)
Age, y .78
<75 27/771 (3.6) 41/817 (5.2) –1.5 0.69 (0.43-1.13)
≥75 8/132 (6.5) 13/129 (10.3) –3.8 0.60 (0.25-1.45)
Sex .61
Men 27/676 (4.1) 40/728 (5.6) –1.5 0.71 (0.43-1.15)
Women 8/227 (3.7) 14/218 (6.6) –2.9 0.54 (0.23-1.30)
Current smoker .31
No 27/675 (4.2) 46/707 (6.7) –2.5 0.60 (0.37-0.96)
Yes 8/228 (3.6) 8/239 (3.4) –0.2 1.05 (0.39-2.80)
Diabetes .82
No 20/649 (3.2) 32/689 (4.8) –1.6 0.64 (0.36-1.12)
Yes 15/253 (6.2) 22/257 (8.8) –2.6 0.70 (0.36-1.36)
Race .40
White 20/442 (4.7) 33/462 (7.3) –2.6 0.60 (0.35-1.06)
Asian 10/407 (2.5) 17/429 (4.0) –1.5 0.61 (0.28-1.32)
Black 3/17 (19.6) 1/20 (5.0) 14.6 3.83 (0.39-37.20)
Other/unknown 2/37 (5.8) 3/35 (8.9) –3.1 0.72 (0.12-4.33)
Country of enrollmenta .61
US 18/345 (5.5) 30/380 (8.2) –2.7 0.66 (0.37-1.18)
South Korea 10/381 (2.7) 16/397 (4.1) –1.4 0.63 (0.29-1.40)
Cannada 7/168 (4.3) 7/161 (4.5) –0.2 0.89 (0.31-2.55)
Body mass indexb .54
<25 12/287 (4.4) 14/329 (4.3) 0.0 0.94 (0.43-2.04)
25-30 11/347 (3.3) 20/342 (6.0) –2.8 0.54 (0.26-1.14)
≥30 12/264 (4.7) 20/268 (7.6) –2.9 0.57 (0.28-1.16)
History of heart failure .82
No 28/794 (3.7) 43/841 (5.2) –1.6 0.67 (0.42-1.09)
Yes 7/107 (6.8) 11/105 (10.7) –4.0 0.60 (0.23-1.54)
Kidney function, eGFR, mL/minc .20
<60 8/100 (8.5) 6/94 (6.5) 2.0 1.28 (0.44-3.69)
≥60 26/738 (3.7) 44/773 (5.8) –2.2 0.60 (0.37-0.97)
Proton pump inhibitor at discharge .97
No 26/634 (4.2) 37/636 (6.0) –1.8 0.69 (0.41-1.13)
Yes 9/258 (3.6) 15/303 (5.0) –1.5 0.70 (0.31-1.61)
0.1 1 10
HR (95% CI)
a
Hazard ratios and 95% CIs for the effect of genotype-guided therapy within CYP2C19 The hazard ratio for the Mexico subgroup is not shown, as there were no
loss-of-function carriers were estimated within clinically relevant prespecified events in the genotype-guided therapy group and only 1 event in the
subgroups. The number of events and the sample size of each subgroup as well as conventional therapy group.
the Kaplan-Meier estimated event rates at 12 months are provided according to b
Calculated as weight in kilograms divided by height in meters squared.
the 2 treatment groups. P values for tests of interaction have not been adjusted for c
eGFR calculated by Modification of Diet in Renal Disease equation.
multiplicity. CAD indicates coronary artery disease; eGFR, estimated glomerular
filtration rate; STEMI, ST-segment elevation myocardial infarction.
than 120 million individuals enrolled in private and Medicare months.20 In clinical practice the question arises whether a
Advantage health plans, were analyzed to evaluate which an- genotype-guided choice of P2Y12 inhibitors vs clopidogrel for
tiplatelet agent was initiated after PCI in 2018. Clopidogrel was all or ticagrelor for all without point-of-care genotyping is an
prescribed in 61% of patients after PCI, ticagrelor in 31%, and appropriate strategy. This trial was not powered to demon-
prasugrel in 8%. strate superiority in outcomes of the overall genotype-
In contrast to this trial, patients with MI in the conven- guided therapy group as compared with the overall group re-
tional therapy group in the POPular Genetics trial received ti- ceiving clopidogrel. However, in this study, the ischemic event
cagrelor after PCI and were compared with patients receiving rate of 4.4% in the genotype-guided group was similar to the
genotype-guided P2Y12 inhibitors, demonstrating noninferi- rate for ticagrelor for all groups in the POPular Genetics trial,
ority with event rates of 4.6% and 4.7%, respectively, at 12 highlighting the efficacy of a genotype-guided strategy. The
jama.com (Reprinted) JAMA August 25, 2020 Volume 324, Number 8 769
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Rochester User on 08/26/2020
Research Original Investigation Effect of Genotype-Guided Oral P2Y12 Inhibitor Selection vs Clopidogrel on Ischemic Outcomes After PCI
TIMI bleeding rates in both groups in the current study were strated findings similar to those from the primary analysis.
similar and relatively low (≤2% at 12 months after PCI). In con- Third, the trial was open-label; however, the conventional
trast, POPular Genetics and other clinical trials have consis- therapy group was blinded for the primary analysis, since geno-
tently reported higher bleeding rates with ticagrelor for all use typing was performed 12 months after PCI in that group and
compared with a CYP2C19 genotype-guided oral P2Y12 inhibi- adjudication of all events was blinded.
tor strategy or clopidogrel for all, respectively.15,20 Consis-
tent with these and other studies, BARC 2,3,5 bleeding in the
per-protocol genotype-guided group in this study was in-
creased compared with the conventional therapy group.
Conclusions
Among CYP2C19 LOF carriers with ACS and stable CAD under-
Limitations going PCI, genotype-guided selection of an oral P2Y12 inhibi-
This study has several limitations. First, the trial was under- tor, compared with conventional clopidogrel therapy with-
powered to detect an effect size less than the 50% relative risk out point-of-care genotyping, resulted in no statistically
reduction used in the revised sample size calculation. Sec- significant difference in a composite end point of cardiovas-
ond, the pragmatic nature of the trial, which relied on provi- cular death, myocardial infarction, stroke, stent thrombosis,
sion of P2Y12 inhibitors by an individual’s health plan, may and severe recurrent ischemia based on the prespecified analy-
have led to some patients not receiving designated antiplate- sis plan and the treatment effect that the study was powered
let therapy. However, the per-protocol analysis demon- to detect at 12 months.
ARTICLE INFORMATION Concept and design: Pereira, Farkouh, So, Lennon, from Amgen, AstraZeneca, Bayer, Boehringer
Accepted for Publication: June 25, 2020. Mathew, Jeong, Baudhuin, Fu, Goodman, Hasan, Ingelheim, Bristol Myers Squibb, CSL Behring, Eli
Iturriaga, Lerman, Wang, Weinshilboum, Bailey, Lilly Merck, Novartis, Pfizer, and York University
Author Affiliations: Department of Cardiovascular Rihal. Clinical Coordinating Centre; and receiving personal
Medicine, Mayo Clinic, Rochester, Minnesota Acquisition, analysis, or interpretation of data: fees from Daiichi-Sankyo/American Regent,
(Pereira, Bell, Lerman, Rihal); Peter Munk Cardiac Pereira, Farkouh, So, Lennon, Geller, Mathew, Bell, Esperion, Ferring Pharmaceuticals,
Centre and Heart and Stroke Richard Lewar Centre, Bae, Chavez, Gordon, Abbott, Cagin, Hasan, GlaxoSmithKline, HLS Therapeutics, Janssen/
University of Toronto, Toronto, Ontario, Canada Lerman, Sidhu, Tanguay, Weinshilboum, Welsh, Johnson & Johnson, Novo Nordisk A/C, Regeneron,
(Farkouh); University of Ottawa Heart Institute, Rosenberg, Bailey, Rihal. Servier, the Heart and Stroke Foundation of
Ottawa, Ontario, Canada (So); Department of Drafting of the manuscript: Pereira, Farkouh, So, Ontario/University of Toronto (Polo) chair, the
Health Sciences Research, Mayo Clinic, Rochester, Lennon, Bae, Jeong, Fu, Hasan, Weinshilboum, Canadian Heart Research Centre and MD Primer,
Minnesota (Lennon, Bailey); National Heart, Lung, Rihal. Canadian VIGOUR Centre, Duke Clinical Research
and Blood Institute, National Institutes of Health, Critical revision of the manuscript for important Institute, and PERFUSE Research Institute.
Bethesda, Maryland (Geller, Fu, Hasan, Iturriaga, intellectual content: Pereira, Farkouh, So, Lennon, Dr Lerman reported receiving personal fees from
Rosenberg); Department of Medicine, Loyola Geller, Mathew, Bell, Chavez, Gordon, Abbott, Itamar Medical, Phillips/Volcano, Shahal, and Wei
University, Maywood, Illinois (Mathew); Cagin, Baudhuin, Goodman, Hasan, Iturriaga, Jian RC Inc. Dr Sidhu reported serving on scientific
Department of Internal Medicine, Division of Lerman, Sidhu, Tanguay, Wang, Weinshilboum, advisory boards for Sanofi Regeneron and
Cardiology, Konyang University, Seo-gu, Taejon, Welsh, Rosenberg, Bailey, Rihal. AstraZeneca. Dr Tanguay reported receiving
South Korea (Bae); Heart Research Center, Statistical analysis: Lennon, Geller, Hasan, Bailey, personal fees from Mayo Clinic, AstraZeneca, Bayer,
Chonnam National University, Gwangju, South Rihal. Daiichi-Sankyo, Servier, Novartis, and BMS-Pfizer
Korea (Jeong); Department of Cardiology, Obtained funding: Pereira, Farkouh, Lennon, Alliance. Dr Wang reported receiving grants from
Minneapolis Heart Institute Foundation, Goodman, Lerman, Wang, Weinshilboum. NIH and NHLBI. Dr Weinshilboum reported
Minneapolis, Minnesota (Chavez); Division of Administrative, technical, or material support: receiving grants from NIH and NHLBI and that he is
Cardiology, The Miriam Hospital, Providence, Pereira, Mathew, Bae, Jeong, Gordon, Baudhuin, cofounder of, and stockholder in, OneOme LLC.
Rhode Island (Gordon); Division of Cardiology, Fu, Goodman, Iturriaga, Weinshilboum, Welsh, Dr Welsh reported receiving personal fees from
Rhode Island Hospital, Providence, Rhode Island Rosenberg, Bailey, Rihal. Mayo Clinic; receiving grants from AstraZeneca and
(Abbott); Mayo Clinic Health System—La Crosse, Supervision: Pereira, Farkouh, Lennon, Bae, Chavez, Pfizer; and receiving grants and personal fees from
La Crosse, Wisconsin (Cagin); Department of Goodman, Tanguay, Weinshilboum, Rosenberg, Bayer and Boerhinger Ingelheim. Dr Bailey reported
Laboratory Medicine and Pathology, Mayo Clinic, Bailey, Rihal. receiving grants from NIH. No other disclosures
Rochester, Minnesota (Baudhuin); St Michael’s were reported.
Hospital, University of Toronto, Toronto, Ontario, Conflict of Interest Disclosures: Dr Pereira
Canada (Goodman); Canadian VIGOUR Centre, reported receiving grants from the National Heart, Funding/Support: Funding for this research was
University of Alberta, Edmonton, Alberta Lung, and Blood Institute (NHLBI). Dr Farkouh provided by the NIH (grants U01HL128606 and
(Goodman); Division of Cardiology, Department of reported receiving grants from NHLBI, Amgen, U01HL128626).
Medicine, Albany Medical Center and Albany Novartis, and Novo Nordisk. Dr So reported Role of the Funder/Sponsor: The NIH established
Medical College, Albany, New York (Sidhu); receiving grants from Eli Lilly Canada, Spartan an independent data and safety monitoring board
Montreal Heart Institute and Université de Biosciences, Roche Diagnostics, and Aggredyne Inc to monitor adverse events but had no role in the
Montréal, Montreal, Quebec, Canada (Tanguay); and receiving personal fees from AstraZeneca design of the study; collection, management, and
Department of Molecular Pharmacology and Canada, Bayer Canada, and Servier Canada. interpretation of the data; preparation of the
Experimental Therapeutics, Mayo Clinic, Rochester, Dr Lennon reported receiving grants from the manuscript; or decision to submit the manuscript
Minnesota (Wang, Weinshilboum); Department of National Institutes of Health (NIH)/NHLBI and for publication.
Medicine, Mazankowski Alberta Heart Institute and receiving nonfinancial support from Spartan
Biosciences. Dr Abbott reported receiving grants Disclaimer: The views expressed in this manuscript
University of Alberta, Edmonton, Alberta, Canada are those of the authors and do not necessarily
(Welsh). from AstraZeneca, Bristol Myers Squibb, Sino
Medical, Biosensors Research USA, Abbott represent the views of the NHLBI, the NIH, or the
Author Contributions: Drs Pereira and Bailey had Vascular, and CSL Behring. Dr Goodman reported US Department of Health and Human Services.
full access to all of the data in the study and take receiving grants from the Mayo Clinic and NIH; Data Sharing Statement: See Supplement 4.
responsibility for the integrity of the data and the receiving nonfinancial support from Spartan
accuracy of the data analysis. Drs Pereira and Additional Contributions: We are grateful for the
Biosciences; receiving grants and personal fees effort and assistance from Daniel Crusan, BS,
Farkouh were coprimary first authors.
770 JAMA August 25, 2020 Volume 324, Number 8 (Reprinted) jama.com
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Rochester User on 08/26/2020
Effect of Genotype-Guided Oral P2Y12 Inhibitor Selection vs Clopidogrel on Ischemic Outcomes After PCI Original Investigation Research
Monica Olson, MBA, and Julia Byrne, BS, Mayo clopidogrel clinical alert: approaches to the FDA clopidogrel-treated Chinese patients undergoing
Clinic; Spartan, Applied Health Research Centre “boxed warning”: a report of the American College percutaneous coronary intervention. Eur J Clin
(AHRC), DREAM CIS, Biospecimens Accessioning of Cardiology Foundation Task Force on Clinical Pharmacol. 2013;69(4):771-777. doi:10.1007/s00228-
and Processing (BAP) at Mayo Clinic, and the Expert Consensus Documents and the American 012-1392-5
TAILOR-PCI clinical trial site principal investigators Heart Association. Circulation. 2010;122(5):537-557. 12. Haybittle JL. Repeated assessment of results in
and their study coordinators. The TAILOR-PCI doi:10.1161/CIR.0b013e3181ee08ed clinical trials of cancer treatment. Br J Radiol. 1971;
clinical trial site principal investigators include 3. Pereira NL, Weinshilboum RM. Cardiovascular 44(526):793-797. doi:10.1259/0007-1285-44-526-
Khaled Abdul-Nour, MD, Henry Ford Health System; pharmacogenomics and individualized drug 793
Amir Darki, MD, Loyola University Medical Center; therapy. Nat Rev Cardiol. 2009;6(10):632-638. doi:
Payam Dehghani, MD, Regina General Hospital; 13. Roberts JD, Wells GA, Le May MR, et al.
10.1038/nrcardio.2009.154 Point-of-care genetic testing for personalisation of
Josh Doll, MD, Greenville Health System;
Mohammed El-Hajjar, MD, Albany Medical Center; 4. Mega JL, Simon T, Collet J-P, et al. antiplatelet treatment (RAPID GENE):
Jorge Escobedo, MD, Mexico-La Raza, Centro Reduced-function CYP2C19 genotype and risk of a prospective, randomised, proof-of-concept trial.
Medico; Adam Frank, MD, NCH Healthcare System; adverse clinical outcomes among patients treated Lancet. 2012;379(9827):1705-1711. doi:10.1016/
Wilson Ginete, MD, and Alok Bachuwar, MD, with clopidogrel predominantly for PCI: S0140-6736(12)60161-5
Essentia Institute of Rural Health; Ronald Goldberg, a meta-analysis. JAMA. 2010;304(16):1821-1830. 14. Dong H, Robison LL, Leisenring WM, Martin LJ,
MD, Sharp Healthcare Center for Research; John doi:10.1001/jama.2010.1543 Armstrong GT, Yasui Y. Estimating the burden of
Graham, MD, St. Michael’s Hospital; Cameron Guild, 5. Pereira NL, Sargent DJ, Farkouh ME, Rihal CS. recurrent events in the presence of competing
MD, and William Campbell, MD, University of Genotype-based clinical trials in cardiovascular risks: the method of mean cumulative count. Am J
Mississippi Medical Center; Sang Wook Kim, MD, disease. Nat Rev Cardiol. 2015;12(8):475-487. doi: Epidemiol. 2015;181(7):532-540. doi:10.1093/aje/
Chung-Ang University Hospital; Louie Kostopoulis, 10.1038/nrcardio.2015.64 kwu289
MD, Aurora Research Institute; Gary Lane, MD, 6. Chesebro JH, Knatterud G, Roberts R, et al. 15. Wallentin L, Becker RC, Budaj A, et al; PLATO
Mayo Clinic in Florida; Hong-seok Lim, MD, Ajou Thrombolysis in Myocardial Infarction (TIMI) trial, Investigators. Ticagrelor versus clopidogrel in
University Hospital; Andrea MacDougall, MD, phase I: a comparison between intravenous tissue patients with acute coronary syndromes. N Engl J
Thunder Bay Regional Research Institute; Mina plasminogen activator and intravenous Med. 2009;361(11):1045-1057. doi:10.1056/
Madan, MD, Sunnybrook Research Institute; Kevin streptokinase: clinical findings through hospital NEJMoa0904327
Marzo, MD, Winthrop University Hospital; Tamim discharge. Circulation. 1987;76(1):142-154. doi:10.
Nazif, MD, Columbia University Medical Center; 16. Dayoub EJ, Seigerman M, Tuteja S, et al. Trends
1161/01.CIR.76.1.142 in platelet adenosine diphosphate P2Y12 receptor
Fearghas O’Cochlain, MD, Mayo Clinic Health
System—Eau Claire Hospital Inc; Christopher 7. Mehran R, Rao SV, Bhatt DL, et al. Standardized inhibitor use and adherence among
Overgaard, MD, and Vlad Dzavik, MD, Toronto bleeding definitions for cardiovascular clinical trials: antiplatelet-naive patients after percutaneous
General Hospital; Ganesh Raveendran, MD, a consensus report from the Bleeding Academic coronary intervention, 2008-2016. JAMA Intern Med.
University of Minnesota; Louai Razzouk, MD, NYU Research Consortium. Circulation. 2011;123(23): 2018;178(7):943-950. doi:10.1001/jamainternmed.
Langone Medical Center; Carl Reimers, MD, and Kirk 2736-2747. doi:10.1161/CIRCULATIONAHA.110. 2018.0783
Garratt, MD, The Feinstein Institute for Medical 009449 17. Basra SS, Wang TY, Simon DN, et al. Ticagrelor
Research-Lenox Hill; Jorge Saucedo, MD, and Justin 8. Mega JL, Close SL, Wiviott SD, et al. Cytochrome use in acute myocardial infarction: insights from the
Levisay, MD, NorthShore University Health System; p-450 polymorphisms and response to clopidogrel. National Cardiovascular Data Registry. J Am Heart
Jacqueline Saw, MD, Vancouver General Hospital; N Engl J Med. 2009;360(4):354-362. doi:10.1056/ Assoc. 2018;7(12):e008125. doi:10.1161/JAHA.117.
D.P. Suresh, MD, St. Elizabeth Healthcare; John NEJMoa0809171 008125
Sweeney, MD, Mayo Clinic in Arizona; Irving Tiong, 9. Oh I-Y, Park KW, Kang S-H, et al. Association of 18. Karve AM, Seth M, Sharma M, et al.
MD, Humber River Hospital; Steven Weitz, MD, cytochrome P450 2C19*2 polymorphism with Contemporary use of ticagrelor in interventional
Cardiology Associates of Schenectady; and Alan clopidogrel response variability and cardiovascular practice (from Blue Cross Blue Shield of Michigan
Wu, PhD, Zuckerberg San Francisco General events in Koreans treated with drug-eluting stents. Cardiovascular Consortium). Am J Cardiol. 2015;115
Hospital. None of these individuals received any Heart. 2012;98(2):139-144. doi:10.1136/hrt.2011. (11):1502-1506. doi:10.1016/j.amjcard.2015.02.049
compensation for their role in the study. 227272 19. Gandhi S, Zile B, Tan MK, et al; Canadian ACS
REFERENCES 10. Ono T, Kaikita K, Hokimoto S, et al. Reflective Group. Increased uptake of
Determination of cut-off levels for on-clopidogrel guideline-recommended oral antiplatelet therapy:
1. Pereira NL, Rihal CS, So DYF, et al. Clopidogrel platelet aggregation based on functional CYP2C19 insights from the Canadian Acute Coronary
pharmacogenetics. Circ Cardiovasc Interv. 2019;12 gene variants in patients undergoing elective Syndrome Reflective. Can J Cardiol. 2014;30(12):
(4):e007811. doi:10.1161/CIRCINTERVENTIONS.119. percutaneous coronary intervention. Thromb Res. 1725-1731. doi:10.1016/j.cjca.2014.09.011
007811 2011;128(6):e130-e136. doi:10.1016/j.thromres.2011. 20. Claassens DMF, Vos GJA, Bergmeijer TO, et al.
2. Holmes DR Jr, Dehmer GJ, Kaul S, Leifer D, 07.028 A genotype-guided strategy for oral P2Y12 inhibitors
O’Gara PT, Stein CM; Society for Cardiovascular 11. Zou J-J, Xie H-G, Chen S-L, et al. Influence of in primary PCI. N Engl J Med. 2019;381(17):1621-1631.
Angiography and Interventions; Society of Thoracic CYP2C19 loss-of-function variants on the doi:10.1056/NEJMoa1907096
Surgeons; Writing Committee Members. ACCF/AHA antiplatelet effects and cardiovascular events in
jama.com (Reprinted) JAMA August 25, 2020 Volume 324, Number 8 771
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University of Rochester User on 08/26/2020
You might also like
- New Insights into Glioblastoma: Diagnosis, Therapeutics and TheranosticsFrom EverandNew Insights into Glioblastoma: Diagnosis, Therapeutics and TheranosticsCarla VitorinoNo ratings yet
- Clopidogrel PharmacogeneticsDocument11 pagesClopidogrel PharmacogeneticsYaxkin NikNo ratings yet
- Clopidogrel PharmacogeneticsDocument11 pagesClopidogrel PharmacogeneticsGisela GloryNo ratings yet
- Cardiovascular Risk in Clopidogrel-Treated Patients According To Cytochrome P450 2C19 2 Loss-of-Function Allele or Proton Pump Inhibitor CoadministrationDocument10 pagesCardiovascular Risk in Clopidogrel-Treated Patients According To Cytochrome P450 2C19 2 Loss-of-Function Allele or Proton Pump Inhibitor CoadministrationVenansius ReinaldiNo ratings yet
- Project Presentation-Sydney StratfordDocument17 pagesProject Presentation-Sydney Stratfordapi-611918048No ratings yet
- White 2012 Champion PooledDocument13 pagesWhite 2012 Champion PooledRadu CiprianNo ratings yet
- The Role of CYP2C19 Genotyping To Guide Antiplatelet Therapy Following IschemicDocument15 pagesThe Role of CYP2C19 Genotyping To Guide Antiplatelet Therapy Following IschemicmedgusNo ratings yet
- Article 9Document10 pagesArticle 9vzwsvt7hgkNo ratings yet
- Dapa-Ckd 2020 NejmDocument11 pagesDapa-Ckd 2020 NejmInês MendonçaNo ratings yet
- Nejmoa 2024816Document11 pagesNejmoa 2024816Cessar OrnlsNo ratings yet
- The Dapagliflozin and Prevention of Adverse Outcomes in Chronic Kidney Disease (DAPA-CKD) Trial: Baseline CharacteristicsDocument12 pagesThe Dapagliflozin and Prevention of Adverse Outcomes in Chronic Kidney Disease (DAPA-CKD) Trial: Baseline CharacteristicsSorina ElenaNo ratings yet
- Chi 2019Document9 pagesChi 2019docadax848No ratings yet
- 1 s2.0 S0019483213000382 MainDocument10 pages1 s2.0 S0019483213000382 Mainsiddhi divekarNo ratings yet
- 1 s2.0 S0735109708008656 MainDocument10 pages1 s2.0 S0735109708008656 MainraniahNo ratings yet
- AHA 2022 Key InsightsDocument15 pagesAHA 2022 Key InsightsBinod KumarNo ratings yet
- CYP2C19 Protocol 20111122 PDFDocument24 pagesCYP2C19 Protocol 20111122 PDFGordon FagrasNo ratings yet
- Nej Mo A 1912388Document9 pagesNej Mo A 1912388dralourdesreyespediatraNo ratings yet
- Cocot TrialDocument9 pagesCocot TrialAngelEduardoVillarrealGiraldoNo ratings yet
- Eur Heart J 2008 Angiolillo 2202 11Document10 pagesEur Heart J 2008 Angiolillo 2202 11Muhammad Akbar 'AnifaNo ratings yet
- Cardiovascular PharmacogenomicsDocument51 pagesCardiovascular PharmacogenomicsNemer EzzeddineNo ratings yet
- 【DAPA-CKD FSGS】Safety and efficacy of dapagliflozin in patients with focal segmental glomerulosclerosis a prespecified analysis of the DAPA-CKDDocument10 pages【DAPA-CKD FSGS】Safety and efficacy of dapagliflozin in patients with focal segmental glomerulosclerosis a prespecified analysis of the DAPA-CKD陈诗哲No ratings yet
- Joc120067 882 889Document8 pagesJoc120067 882 889www.manvith8No ratings yet
- 256 FullDocument5 pages256 FullanindythaNo ratings yet
- 2719-Article Text Orig-23698-1-10-20210712Document2 pages2719-Article Text Orig-23698-1-10-20210712Oeij Henri WijayaNo ratings yet
- Manejo y Tratamiento de Enfermedades Glomerulares (Parte 2) : Conclusiones KDIGODocument25 pagesManejo y Tratamiento de Enfermedades Glomerulares (Parte 2) : Conclusiones KDIGORodrigo Avellaneda CamposNo ratings yet
- DAPA HF TrialDocument14 pagesDAPA HF TrialB ShahNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument7 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- Copia de Parcial 4 - TP 1. Riesgo IBP y ClopidogrelDocument8 pagesCopia de Parcial 4 - TP 1. Riesgo IBP y ClopidogrelVictoria ChristieNo ratings yet
- Heart Failure ArticleDocument7 pagesHeart Failure Articlefaraz.mirza1No ratings yet
- FDA Approval of Dapagliflozin For Chronic Kidney Disease A Rem - 2021 - The LanDocument2 pagesFDA Approval of Dapagliflozin For Chronic Kidney Disease A Rem - 2021 - The LanAvril JatariuNo ratings yet
- LeaderDocument12 pagesLeaderMoeez AkramNo ratings yet
- Cardiovascular and Renal Outcomes With Efpeglenatide in Type 2 DiabetesDocument12 pagesCardiovascular and Renal Outcomes With Efpeglenatide in Type 2 DiabetesMoeez AkramNo ratings yet
- Sta Final PPT Team A Done (1) - 1Document26 pagesSta Final PPT Team A Done (1) - 1Sumi FaNo ratings yet
- 1 s2.0 S2213177917305358 MainDocument10 pages1 s2.0 S2213177917305358 MainMayar HassanNo ratings yet
- Broniscer 2013Document9 pagesBroniscer 2013docadax848No ratings yet
- COMMIT ClopidogrelDocument15 pagesCOMMIT ClopidogrelCristina PazmiñoNo ratings yet
- Pi Is 1933287417302908Document11 pagesPi Is 1933287417302908Anonymous yptjlwJNo ratings yet
- DECAL LNH Refrac JCO 2001Document7 pagesDECAL LNH Refrac JCO 2001sunrasta23No ratings yet
- Effect of Oral Nimodipine After Subarachnoid Haemorrhage: Nimodipine TrialDocument7 pagesEffect of Oral Nimodipine After Subarachnoid Haemorrhage: Nimodipine TrialRian KurniaNo ratings yet
- NEJMoa NEJM Bundle The Articles and Place in EverandDocument12 pagesNEJMoa NEJM Bundle The Articles and Place in Everandlakshminivas PingaliNo ratings yet
- Evolocumab To Reduce Cardiovascular Events: Results of The (FOURIER) Multinational TrialDocument2 pagesEvolocumab To Reduce Cardiovascular Events: Results of The (FOURIER) Multinational TrialWaqas ShahnawazNo ratings yet
- Dapaglifozina y Anemia en Enfermedad Renal Crónica NEJMDocument10 pagesDapaglifozina y Anemia en Enfermedad Renal Crónica NEJMDolores AlemánNo ratings yet
- Emailing Expression of KGF-1 and KGF-2 in Skin Wounds ADocument12 pagesEmailing Expression of KGF-1 and KGF-2 in Skin Wounds ARimaWulansariNo ratings yet
- Dapagliflozin and Cardiovascular Outcomes in Type 2 DiabetesDocument12 pagesDapagliflozin and Cardiovascular Outcomes in Type 2 DiabetesAlina PopaNo ratings yet
- DAPA-HF Full PublicationDocument13 pagesDAPA-HF Full PublicationPutra AchmadNo ratings yet
- Treatment of Giant Cell Arteritis (GCA)Document13 pagesTreatment of Giant Cell Arteritis (GCA)Kori Karina Cueva TovarNo ratings yet
- Sample Journal Club 1Document2 pagesSample Journal Club 1aguocha1No ratings yet
- Vascilar CKDDocument7 pagesVascilar CKDanggi abNo ratings yet
- Diabetes Obesity Metabolism - 2023 - McGuire - Effects of Oral Semaglutide On Cardiovascular Outcomes in Individuals WithDocument10 pagesDiabetes Obesity Metabolism - 2023 - McGuire - Effects of Oral Semaglutide On Cardiovascular Outcomes in Individuals Withivan dario hernandez erazoNo ratings yet
- Empagliflozin in Heart Failure With A Preserved Ejection FractionDocument11 pagesEmpagliflozin in Heart Failure With A Preserved Ejection FractionVinh Quy VoNo ratings yet
- Review ArticleDocument9 pagesReview ArticleJeronim H'gharNo ratings yet
- HHF 9 E002560Document12 pagesHHF 9 E002560Putri Atthariq IlmiNo ratings yet
- Healthcare 10 02356Document18 pagesHealthcare 10 02356Rakhmat RamadhaniNo ratings yet
- Noz 124Document10 pagesNoz 124albertoNo ratings yet
- Journal 1 Nejmoa1506930Document11 pagesJournal 1 Nejmoa1506930Dyo O RNo ratings yet
- Empaglifozina Posterior A IMADocument12 pagesEmpaglifozina Posterior A IMAstoledoqNo ratings yet
- Clopidogrel Resistance and Clopidogrel Treatment Failure - UpToDateDocument39 pagesClopidogrel Resistance and Clopidogrel Treatment Failure - UpToDateRenato RamonNo ratings yet
- AHA 2022 - Efficacy and Safety of Dapagliflozin in Type 2 Diabetes According To Baseline Blood PressureDocument11 pagesAHA 2022 - Efficacy and Safety of Dapagliflozin in Type 2 Diabetes According To Baseline Blood PressureBigPharma HealtcareNo ratings yet
- 1304 FullDocument8 pages1304 FullNurul AmaliaNo ratings yet
- CABANADocument14 pagesCABANAIsmael Rivera DiazNo ratings yet
- MamaGioMeny Host 22 ENGDocument2 pagesMamaGioMeny Host 22 ENGMathew McCarthyNo ratings yet
- Risk Assessment of Contrast Medium-Induced Acute Kidney Injury (CI-AKI) at CTDocument1 pageRisk Assessment of Contrast Medium-Induced Acute Kidney Injury (CI-AKI) at CTMathew McCarthyNo ratings yet
- Newest Definition of Heart FailureDocument27 pagesNewest Definition of Heart FailurecrsscribdNo ratings yet
- Asymptomatic ST-Segment - Elevation ECG in Patient With Kidney Failure - 2022Document3 pagesAsymptomatic ST-Segment - Elevation ECG in Patient With Kidney Failure - 2022Mathew McCarthyNo ratings yet
- Ehv 727Document9 pagesEhv 727Matias HerreraNo ratings yet
- Rest and Inf CMPs P1Document19 pagesRest and Inf CMPs P1Mathew McCarthyNo ratings yet
- DOI - ReviewedDoiSummary EHRA NOAC 2021 ReviewersDocument4 pagesDOI - ReviewedDoiSummary EHRA NOAC 2021 ReviewersMathew McCarthyNo ratings yet
- Practical Guidance in Echocardiographic Assessment of Global Longitudinal StrainDocument4 pagesPractical Guidance in Echocardiographic Assessment of Global Longitudinal StrainMathew McCarthyNo ratings yet
- Nejmra 2000348Document16 pagesNejmra 2000348Mathew McCarthyNo ratings yet
- Left Atrial Expansion Index Predicts All-Cause Mortality and Heart Failure Admissions in DyspnoeaDocument8 pagesLeft Atrial Expansion Index Predicts All-Cause Mortality and Heart Failure Admissions in DyspnoeaMathew McCarthyNo ratings yet
- Jeaa 243Document10 pagesJeaa 243Mathew McCarthyNo ratings yet
- Quadruple Therapy Is The New Standard of Care For Hfref: Editorial CommentDocument3 pagesQuadruple Therapy Is The New Standard of Care For Hfref: Editorial CommentMathew McCarthyNo ratings yet
- Victims of Success in Failure: CirculationDocument3 pagesVictims of Success in Failure: CirculationMathew McCarthyNo ratings yet
- Schmidt Int J Cardiovasc ImagDocument8 pagesSchmidt Int J Cardiovasc ImagMathew McCarthyNo ratings yet
- Prognostic Significance of Left Ventricular Noncompaction: Original ArticleDocument14 pagesPrognostic Significance of Left Ventricular Noncompaction: Original ArticleMathew McCarthyNo ratings yet
- Circulationaha 122 059598Document10 pagesCirculationaha 122 059598Mathew McCarthyNo ratings yet
- TVP 2021Document16 pagesTVP 2021Madalina BadeaNo ratings yet
- Extensive Dermatitis (Coumadin) : Due Warfarin SodiumDocument2 pagesExtensive Dermatitis (Coumadin) : Due Warfarin SodiumMathew McCarthyNo ratings yet
- Acs 2022 Bav 18Document10 pagesAcs 2022 Bav 18Mathew McCarthyNo ratings yet
- Position PaperDocument16 pagesPosition PaperMathew McCarthyNo ratings yet
- 2019 Esc PPCMDocument17 pages2019 Esc PPCMJayden WaveNo ratings yet
- Swedish: An Elementary Grammar-Reader PDF, Epub, EbookDocument5 pagesSwedish: An Elementary Grammar-Reader PDF, Epub, EbookMathew McCarthyNo ratings yet
- 2021 NOAC Guide Online Supplement - Ver21-Apr-21JSDocument21 pages2021 NOAC Guide Online Supplement - Ver21-Apr-21JSMathew McCarthyNo ratings yet
- Ehra Consensus Paper: Europace (2020) 22, 515-516 Doi:10.1093/europace/euz246Document35 pagesEhra Consensus Paper: Europace (2020) 22, 515-516 Doi:10.1093/europace/euz246Mathew McCarthyNo ratings yet
- GaibazziDocument7 pagesGaibazziMathew McCarthyNo ratings yet
- DOI - ReviewedDoiSummary EHRA NOAC 2021 Reviewers - CHAIRSDocument2 pagesDOI - ReviewedDoiSummary EHRA NOAC 2021 Reviewers - CHAIRSMathew McCarthyNo ratings yet
- Bar MenuDocument13 pagesBar MenuMathew McCarthyNo ratings yet
- AShortandEasyModernGreekGrammar 10457586Document161 pagesAShortandEasyModernGreekGrammar 10457586RaymondNo ratings yet
- Esc CurriculumDocument88 pagesEsc CurriculumMathew McCarthyNo ratings yet
- Fiitjee All India Test Series: Concept Recapitulation Test - Iv JEE (Advanced) - 2019Document13 pagesFiitjee All India Test Series: Concept Recapitulation Test - Iv JEE (Advanced) - 2019Raj KumarNo ratings yet
- ENGLISH TOEFL Structure (3rd Exercise)Document5 pagesENGLISH TOEFL Structure (3rd Exercise)susannnnnnNo ratings yet
- Of Personality Traits of Only and Sibling School Children in BeijingDocument14 pagesOf Personality Traits of Only and Sibling School Children in BeijingMuhammad Hamza AsgharNo ratings yet
- Anger Management: Gaurav Sharma 138Document21 pagesAnger Management: Gaurav Sharma 138gaurav_sharma_19900No ratings yet
- 2021 3 AbstractsDocument168 pages2021 3 AbstractsLong An ĐỗNo ratings yet
- MLAB 3 - BoilerDocument3 pagesMLAB 3 - BoilerReden LopezNo ratings yet
- NIELIT Recruitment For Scientist and Technical Assistants 2017 Official NotificationDocument6 pagesNIELIT Recruitment For Scientist and Technical Assistants 2017 Official NotificationKshitija100% (1)
- Chilere - Unitatile de Racire - Technical - Brochures - NX - 0152P - 0812P - EN PDFDocument72 pagesChilere - Unitatile de Racire - Technical - Brochures - NX - 0152P - 0812P - EN PDFDaniel MilosevskiNo ratings yet
- Wearable BiosensorsDocument16 pagesWearable BiosensorsShreehari Haridasan100% (1)
- Chapter4 RetainingwallDocument55 pagesChapter4 RetainingwallNur HazwaniNo ratings yet
- Literature Review On Parking SpaceDocument6 pagesLiterature Review On Parking Spacefvgy6fn3100% (1)
- Is There Any Way To Download The Whole Package of Asphalt 8 Airborne So That I Can Install It On Any Android Device Without An Internet Connection - QuoraDocument4 pagesIs There Any Way To Download The Whole Package of Asphalt 8 Airborne So That I Can Install It On Any Android Device Without An Internet Connection - QuoraMounir2105No ratings yet
- Pitch Analysis PaperDocument7 pagesPitch Analysis PaperMunib MunirNo ratings yet
- Automatic Control ExercisesDocument183 pagesAutomatic Control ExercisesFrancesco Vasturzo100% (1)
- UnitPlan (P.E) Grade 6Document13 pagesUnitPlan (P.E) Grade 6Lou At CamellaNo ratings yet
- HVS Hotel Cost Estimating Guide 2021Document124 pagesHVS Hotel Cost Estimating Guide 2021pascal rosasNo ratings yet
- Solved Consider Again The Demand Function For Corn in Formula 1Document1 pageSolved Consider Again The Demand Function For Corn in Formula 1M Bilal SaleemNo ratings yet
- (Prestressed Concrete) Lecture 05 Dr. ZubairDocument62 pages(Prestressed Concrete) Lecture 05 Dr. ZubairAhmed RiadNo ratings yet
- Introduction To Rhetorical Analysis: Week 1Document16 pagesIntroduction To Rhetorical Analysis: Week 1Will KurlinkusNo ratings yet
- COCCIMORPHDocument13 pagesCOCCIMORPHmiminNo ratings yet
- Re 150821Document2 pagesRe 150821francis puthuserilNo ratings yet
- Beamforming For 4.9G/5G Networks: Exploiting Massive MIMO and Active Antenna TechnologiesDocument12 pagesBeamforming For 4.9G/5G Networks: Exploiting Massive MIMO and Active Antenna TechnologiesAymen Ben zinebNo ratings yet
- ASME Geometric Dimension Ing and Tolerance Professional CertificationDocument20 pagesASME Geometric Dimension Ing and Tolerance Professional CertificationPaul Anthony Red60% (5)
- Enterpreneurship Assignment 2Document8 pagesEnterpreneurship Assignment 2Khusbu JaiswalNo ratings yet
- KV Class 3 Half Yearly Previous Year Question Paper 2019 ComputerDocument2 pagesKV Class 3 Half Yearly Previous Year Question Paper 2019 Computer02 Aanya Gupta VII CNo ratings yet
- IPE SakibBhaiMagicChothaDocument55 pagesIPE SakibBhaiMagicChothaTousif SadmanNo ratings yet
- Effect of Liquidity Risk On Performance of Deposit Money Banks in NigeriaDocument6 pagesEffect of Liquidity Risk On Performance of Deposit Money Banks in NigeriaEditor IJTSRDNo ratings yet
- Law of DemandDocument16 pagesLaw of DemandARUN KUMARNo ratings yet
- The Aerodynamics of ParachutesDocument78 pagesThe Aerodynamics of Parachutesstevehuppert50% (2)
- Century Vemap PDFDocument5 pagesCentury Vemap PDFMaster MirrorNo ratings yet