Professional Documents
Culture Documents
MS-SL Prelims Firstsem
Uploaded by
mcdonald 1234Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
MS-SL Prelims Firstsem
Uploaded by
mcdonald 1234Copyright:
Available Formats
MEDICAL SURGICAL NURSING SKILLS LAB
University of Santo Tomas - College of Nursing Batch 2024
PRELIMS | 1ST SEMESTER
Clarificatory + all lecture videos ○ Best to do it immediately after waking up before breakfast and at
least an hour before client goes to sleep
RESPIRATORY MODALITIES 1 ○ Should not be done after feeding (vomiting)
○ Should be taught preoperatively
○ Indications:
● Provide patent airways ■ Patients on bed rest
● Provide supplemental oxygen ■ Patients had undergone any surgical procedure
■ Patients who are prone to pulmonary problems
ANATOMY AND PHYSIOLOGY OF THE RESPIRATORY SYSTEM ■ Px susceptible to accumulating respiratory secretions.
○ Contraindications:
■ Px with increased ICP (intracranial pressure)
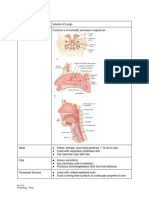
● Respiration ■ Unstable head or neck injury
○ The process of gaseous exchange ■ Spinal injury
■ Breathing is the process that brings oxygen into the lungs ■ Rib or vertebral fractures
and move oxygen to the body. ■ Px who have experienced heart attack
■ The lungs take the carbon dioxide from the blood and is ■ Px with skin grafts or spinal fusions it can induce stress on
released through exhalation. the areas of repair.
○ The left lung is divided into 2 lobes, the right lung is divided into 3 ■ Medical conditions like bronchial hemorrhage and brittle
lobes. bones
○ For the airway it is divided into upper and lower airways ■ Px who had their recent meals and underwent tube
■ Upper Airways feeding. Di siya ginagawa dapat after kumain. You have to
● Nasal cavity coordinate with the respiratory therapist for the timing of
● Pharynx the DBE and CE.
● Larynx or voicebox ■ Px with chest tubes
■ Lower Airways (Tracheobronchial tree) ■ Px who are post eye surgery
● Trachea or windpipe
● Right and left main stem bronchi
● Segmental bronchi
● Terminal bronchi
● The Thorax and the Diaphragm
○ Serves as protector
○ 12 pairs of ribs, bounded anteriorly by the sternum and posteriorly
by the thoracic vertebrae
○ Diaphragm
■ Seperates the chest and abdominal cavity
■ Main muscle for inspiration
■ Supplied by the phrenic nerve
● Includes:
○ Acessory muscles for inspiration:
1. Deep breathing exercises
■ Sternocleidomastoid
○ Helps expand the lungs and forces better distribution of air
■ Parasternal
into all sections of the lungs.
■ Trapezius
○ The patient either sits on the chair or sits uprise and
■ Pectoralis muscle
inhales pushes the abdomen out to force maximum air into
the lungs
OXYGEN MONITORING ○ Done several times each day for short periods.
2. Coughing exercises
● Pulse Oximeter ● Moves mucous out of the large airways
○ Measures Sp02 -oxygen saturation of hemoglobin ● Moving mucous out of the small airways would require the
○ Non-invasive airway clearance techniques (ACTs). Coughing should be
○ Uses light signals done in combination with other airway clearance
○ Normal SpO2 - 95-100% techniques
○ Can be attached to the fingers, forehead, bridge of the nose, the 3. Incentive Spirometry
foot, sole of the foot, earlobe, and toes. 4. Peak flow meter
○ Nursing Considerations: 5. Blow bottle
■ Sites: adequate circulation and free of moisture 6. Chest physiotherapy
■ Monitor skin integrity under sensor ● Postural drainage
■ Usually if the patient is wearing dark colored nail polish, ● Vibration
pinapatangal natin yon because it can interfere with the ● Percussion
accuracy of the SpO2 levels. 7. Pulse oximetry
8. Artificial airway
DEEP BREATHING AND COUGHING EXERCISES
● If post surgery, give client first analgesics, pillows just to splint, binders sa
incision site if meron
● Should be taught preoperatively para after operation, client will be able to
comply
INCENTIVE SPIROMETRY
Page 597
● Incentive spirometry will just be providing you parang visual feedback of the
pulmonary function of the client; if he/she is able to inspire air that much that
will expand the lungs.
● INcentive - INspiration - INhalation
● Helps a patient deep breathe
○ A method of deep breathing that provides visual feedback to
encourage px to inhale slowly and deeply to maximize lung inflation
and prevent / reduce atelectasis
○ Uses incentive spirometer (aka SMIDs, or sustained maximal
PULMONARY HYGIENE inspiration devices), which measures the flow of air inhaled through
the mouthpiece
● To loosen secretions and we want the client to drain these secretions ○ Works by inhalation
● Could do one procedure only but it is more effective if you will be doing the ● Used post-operatively (post abdominal and thoracic surgery)
procedure together with other procedure ● Purposes of IS
● Purpose: ○ Improve pulmonary ventilation
○ Facilitate the exchange of gases ○ Counteract effects of anesthesia
○ Maximize the amount of oxygen available to the cells ○ Help loosen respiratory secretion
○ To promote maximum lung expansion ○ Facilitatie respiratory gas exchange
○ Prevent pulmonary complications like orthostatic pneumonia ○ Helps expand collapsed alveoli
○ Reduce pain ○ indicated for thick, tenacious mucous secretions, usually thoracic
○ Reduce chances of chest complications after surgery and abdominal surgery, to treat atelectasis
● General considerations ● Use of IS, in combination with DBCE and CPT, lowers the rates of post-op
pneumonia
DIAZ, PASCUAL, QUILBAN, TANGO | 1NUR-4 1
SUBJECT | 1ST SEMESTER
● 2 types: ■ Ie. increase dosage of bronchodilators or anti-inflammatory
○ (1) Flow oriented - to provide maximum expansion of the lungs medications
■ May mga bola na magssuspend if you inhale it as long as
you can
■ With one or more plastic chambers with colored balls
■ Balls elevates to a premarked area
■ Same purpose with volume oriented but the volume is not
preset, instead it has a number of movable balls that is
pushed up and held suspended in the air as the patient
inhales. (patagalan na nakaraise yung balls) ● Standard range: 60-900 lpm
■ Measured depending on how long or how high the balls ● Low range: 30-400 lpm
are suspended
○ Usually there is gauge (starts from 0) in L/min
○ The blowing off should be sa green area (80-100%) - if client is on
maintenance doses of medications, continue lng ung gamot
○ Yellow - 50-80%
Triflo IS ■ There will be a need for the client to have an additional medication
○ Red - less than 50%
■ Critical
■ Client should be referred to doctors
■ There could be medications that should be stopped or added
○ (2) Volume oriented
■ May piston (yellow) that will be adjusted by doctors for you
to be able to breathe in a specified amount of air
■ Use a bellows that a patient must raise to a predetermined
volume by inhaling slowly BLOW BOTTLE
■ Tidal voume of IS is set accdg to manufacturer’s
instructions ● Aim is for the client to blow off carbon dioxide
■ Purpose is to ensure that the volume of air inhaled is ● If bata, if walang blow bottle pwedeng bubbles or trumpet para mablow off
increased gradually as the px takes deeper and deeper lang excess CO2
breaths, taking several normal breaths before attempting to
another attempt to avoid fatigue CHEST PHYSIOTHERAPY
● I-time niyo sya; wag sunod-sunod kasi
nakakahingal
● Goal : to improve respiratory gas exchange
● Let the patient catch his/her breath before
○ CPT used to mobilize secretions and involves physical chest wall
another attempt
maneuvers such as percussion, vibration, shaking, and postural
drainage followed by coughing or suctioning.
● Purposes
○ Designed to improve respiratory efficiency and promote expansion
of the lungs.
○ Strengthen respiratory muscle
○ Eliminate respiratory secretions
○ Helps the patient breathe more freely and get more oxygen
○ Prevent bronchial obstructions because of secretions accumulation
○ It can help move secretions from the smaller airways to the main
bronchi and trachea which can be easily removed by suctioning or
coughing.
● Indications and contraindications
○ Indicated for patients whose cough is insufficient to clear thick,
■ Piston: the one that will elevate when the patient inhales tenacious, or localized secretions
■ Ex. patient needs to practice everyday until he/she reach ○ Mga pasyente na hirap mag-expel ng secretions
the goal (yellow indicator) ○ Examples: cystic fibrosis, atelectasis, lung abscess, neuromuscular
■ diseases and pneumonias in dependent lung regions
○ Contraindicated for patients with rib fracture, fracture of other rib
cage structures like clavicle, severe pain, dyspnea, osteoporosis,
thin frail patients with osteoporosis (they are susceptible to chest
injury)
● Nursing considerations
○ Before you perform chest physiotherapy, make sure you ghave
performed respiratory assessment first
○ Review patient chart
○ Determine patient stability
○ Determine affected areas of the lungs
○ What positions can the patient assume so they can position the
PEAK FLOW METER (EXHALATION) patient well so that he/she can breathe freely
○ Monitor patient’s tolerance to the procedure
● Pp. 604 in the book ○ Check vital signs
○ Forceful exhalation ○ Be familiarized with any patient precautions related to his/her
○ Incentive spirometry: measures inhalation disease and treatment. Is chest phjysio indicated or contraindicated
○ Peak flow meter: measures exhalation/expiration for the patient
● Is a portable, easy-to-use device that measures how well your lungs are able ● Methods
to expel air ○ Position
● Gives objective data about severity of airway obstruction ○ Vibration
● Done 3x following bronchodilators
○ Best used after taking bronchodilators
● PEFR: Peak Expiratory Flow Rate
○ Maximum flow that a patient force4s out during 1 quick force
expiration and is measured in liters
○ An objective indicator of a patient's current status in the
effectiveness of a treatment
○ If PEFR is low, there’s a need for further intervention
DIAZ, DIWA, FLANDEZ, FRANCISCO, GARCIA | 2NUR-3 2
SUBJECT | 1ST SEMESTER
○ In cases of patients with increased intracranial pressure
○ Patients with head and neck injury, with active hemorrhage
○ Underwent recent spinal injury
○ Active hemoptysis
○ Pulmonary edema, pulmonary embolism
○ Aged, confused, or anxious patients
○ Rib fracture
○ With surgical wound
● Each position will be assumed for 10-15 minutes
○ During the 10 to 15 minutes of drainage in selected postures, u can
perform chest percussion, vibration, and shaking over the affected
lung region
○ After 10 to 15 minutes in the fist posture, you can have the patient sit
■ Done in sets of three
up and cough
■ The sustained co-contraction of the upper extremities by
● The entire treatment should last for 30 minutes
the caregiver/nurse to produce a cvuibratory force that is
● Gradual change of position, assess for changes in O2 sat or VS
transmitted to the thorax over the involved lung region
● BEFORE: bronchodilator; nebulization is given, as ordered
■ This pressure change is transmitted through to the lung
○ Prior to positioning, give bronchodilator and nebulizer if ordered
tissues and assessed in the secretions
● The best time: before meals in morning upon awakening and at bedtime
■ Usually 5 to 15 minutes following a session of percussion
○ Habang natutulog siya, naiipon ung secretions, so the best way to
and then secretions are cleared by coughing
mobilize it is early in the morning, upon awakening, and at bedtime
○ Percussion
● Do not perform immediately after meals
○ Baka magsuka
● Provide good oral hygiene after procedure
○ This will involve coughing out of secretions
○ Ask to gargle or toothbrush after the procedure
\
■ Involves clapping a patient’s chest wall
■ If done correctly with cupped hands, it is painless
■ The application of force to the chest wall alters the
intrapleural pressure
● Different position depending on the specific area of the lungs you want to
clear of secretions
● You want to remove secretions in Right upper lobe / interior apical bronchi, sit
px on chair on high fowlers or leaning back
● Left upper lobe / posterior apical – edge of bed leaning forward with pillow or
table
● Anterior upper lobe – lie on bed flat on back with small pillows under knees
○ Cough
(1) POSTURAL DRAINAGE
● Technique for loosening mucus in the airway so it may be coughed out
Place client wherein the phlegm is on the top to facilitate drainage of
secretions
● Position client based on location of the phlegm
● Use of positioning techniques to drain secretions from specific segments of
the lungs and bronchi into the trachea
● Each position drains a specific corresponding section of the tracheobronchial
tree either the upper, middle, or lower lung field into the trachea
● Coughing and suctioning helps remove secretion from the trachea
● Purposes:
○ Helps maintain a patent airway by mobilizing secretions into larger
area where they can be coughed out or suctioned
○ Increases respiratory gas exchange by increasing the available
surface area at the alveolar level
○ Decreases incidence of respiratory infections
● Indications
○ When there is evidence of difficulty of secretion clearance
○ Presence of atelectasis caused by mucus plugging
○ Diagnosis of diseases such as cystic fibrosis and bronchiectasis
● Contraindications:
DIAZ, DIWA, FLANDEZ, FRANCISCO, GARCIA | 2NUR-3 3
SUBJECT | 1ST SEMESTER
How Vest Airway Clearance System works (VIDEO played in this part)
● Inflatable vest attached by air hoses to an air pulse generator tht rapidly
inflates and deflates the vest
● During tx, the chest wall is gently compressed and released, which creates
● In pedia patients, use postural drainage cradle airway oscillations and increased airflow in lungs
● Extra airflow allows air to move beyond retained secretions, increased
expiratory airflows, combined with airway oscillations, thin and sheer(?)
secretions from the walls of the airways
● The secretions are then moved towards the large airways, where they can be
cleared by coughing or suctioning
● This type of therapy can be referred to as high frequency chest wall
oscillation
● Nursing considerations:
● Assess the client: kaya niya ba mag postural drainage?
○ What if the client has increased intracranial pressure? If
ittrendelenburg, it will increase lalo ung pressure sa ulo
○ If fractured rib, di pwede ipaprone position
● Check on ABG levels, O2 sat.
○ If client will be able to tolerate this pulmonary hygiene
● If you have to position the client, place the client wherein the
● Page 622 phlegm is on the topmost position
● When px has excessive pulmonary secretions like in cystitis fibrosis, ○ Ex: Phlegm is in right lower lobe - position: left side
mechanical vibrator (instead of manual) is more effective in removing
secretions
● Pano malalaman san plema? Auscultate (baka may crackles, ronchi, etc
indicating may phlegm)
● Ask client to be on upright position then expectorate secretions
○ If unable to expectorate, suction
(2) PERCUSSION
● With a cupped hand, due to pressure, causing dislodgement of secretions
● Cupped hand - para may air onti (dull sound ung expected)
● For pedia, you can use percussion cup ● This air will cause dislodgement of the secretions attached to the lobe of the
client
● Percussion cup may also be used
Percussion cup
(3) VIBRATION
● With 2 hands, apply pressure to cause dislodgement of secretions
● See to it client can tolerate the procedure
○ Baka may spinal cord injury, fractured rib
Pediatric positioning, cupped hands
PULSE OXIMETRY
● Page 619
● Most indicated for cystic fibrosis patients; they benefit best from this type of
system
DIAZ, DIWA, FLANDEZ, FRANCISCO, GARCIA | 2NUR-3 4
SUBJECT | 1ST SEMESTER
(4) TRACHEOSTOMY TUBE
● Opening in the trachea - mismong obstruction is upper airway
● Long-term use
● Portable pulse oximetry or it could be machine oximetry ● Nasal cancer, pharyngeal cancer
● Check first temperature ● Parts:
● Hypothermic - low O2 saturation (due to vasoconstriction → ○ Faceplate
compromising O2 delivery system) ○ Outer cannula
● Hyperthermic - increase in O2 saturation because of vasodilation ○ Shaft
● Assess the factors that can affect the O2 stat: ○ Cuff - usually to prevent client from aspirating if being fed
○ Nail polish - alter the reading ■ Prevent escape of gas from mech ven
■ In the OR, anes or circu nurse will be making use of ○ Pilot balloon - will be inflated; air will be injected to allow air to open
acetone up
○ Placement of the pulse oximeter ○ Inner cannula - yan ung nililinis. Di tinatanggal outer cannula
○ For pedia: foot part dapat or sometimes, ang ginagamit is parang ■ May instances na walang inner cannula
bandage or tape ■ Could be made of plastic or metal. Ifmetal, walang cuff.
■ Di pwede finger probe kasi this will compromise the Mismong shaft or cannula itself lng
circulation of the client ○ Obturator (red circle) - used during insertion of tracheostomy. If
inserted na, tinatanggal na siya
ARTIFICIAL AIRWAY
(1) NASAL TRUMPET
○ Can be nasopharyngeal or nasotracheal
○ If nasopharyngeal, measure the length of the nasal trumpet from tip
of the nose to the mandible
○ Water-soluble lubricant is used. illubricate di basta basta pinapasok
○ Intended if the client has difficulty breathing and you have to provide
a patent nasal airway
○ If there’s a need for suctioning this client, make use of this also
○ Artificial airways can be tubes made of plastic or metal, that will
provide patent airways
(2) ORAL AIRWAY
OXYGEN THERAPY
● The administration of supplemental oxygen to prevent or to treat hypoxia and
hypoxemia
○ Hypoxia - decrease in the oxygen content in tissues and cells
○ Hypoxia - more of oxygen concentration in the blood
● Indications
○ For clients who may not be able to really provide adequate
oxygenation to tissues and cells.
○ Hypoxemic clients - decrease in the oxygenation in the blood.
● Can be 180 or 90 degrees insertion Hemoglobin is responsible for the transport of respiratory gasses
○ 90 degrees - pag pasok sa bibig, nakaside muna (toward the cheek) which may include O2, CO2.
then iikot pabbaa ■ If the client is acidotic, an increase for hemoglobin to
○ 180 degree - nakataas ung tip muna pagpasok (toward the soft release oxygen to the system.
palate) then iikot pababa ■ If the client is alkalotic, the chgb will have a delay in the
● Also known as bite black release of oxygen
● Supplied in hospitals in 2 ways:
(3) ENDOTRACHEAL TUBE ○ Liquid portable system
■ Naka-tanke
○ Wall outlet
● Humidifying device
○ Oxygen should be humidified
○ In the book, up to 4 liters. If below 4 liters, don't humidify it - only 4
liters and above that's the time you can humidify it
○ But in reality, in the hospital setting, whether 1 or 2 liters, basta
naka-oxygen it has to be humidified
○ Why humidify? To prevent irritation of the mucosa. Kasi ung oxygen
is being delivered in high pressure that will eventually cause
mucosal irritation
● General considerations
○ If the client is on oxygen, this is actually a treatment, a medication. Di
sya basta basta binibigyan- it has to be ordered by the doctor
○ The administration/regulation of the oxygen will be dependent on
● IF CLIENT CAN'T breathe on his own doctor’s order
● Dapat nasa gitna lang so there will be equal distribution of air in right and left ○ Oxygen also supports combustion. Di sya nageexplode. As much as
lung. If masyado malalim, if makapunta sya sa example right bronchus, possible, if you have to offer something to the client in terms of
compromised ung oxygen delivery sa left side. (absent breath sounds, gadgets, toys, preferably it should not spark. If the client has to be
inflated lung) using one, there should be a sign that will tell you that oxygen is in
● Measured in cm use
● Client has to be assisted by mech ventilator. ● Providing patient with oxygen at a concentration of pressure greater than in
● Inserted using laryngoscope to visualize epiglottis (entry point of ET tube) the atmosphere to maintain the body’s physiologic need for oxygen
● Not for long term use (7-10 days ; max: 21 days) ● Indications: patient who may not be able to provide adequate oxygen to
tissues and cells
DIAZ, DIWA, FLANDEZ, FRANCISCO, GARCIA | 2NUR-3 5
SUBJECT | 1ST SEMESTER
○ Hemoglobin is responsible to transport oxygen, if client is acidotic, ■ Do not attempt to open it without oxygen regulator
○ Alkalotic, client will have a delay in release of oxygen because of the increased pressure na baka matangay ka
● Supplied in hospitals in 2 ways: ■ Usually nilalagay muna regulator tapos kailangan ng
○ Liquid portable system wrench (sa may kanan) just to tighten the screw
○ Wall outlet ○ Pressure gauge / oxygen gauge - tell you the amount of oxygen
● Humidifying device (<4L liters dont humidify it) but it has to be humidified inside the tank.
whether its 4 L or not ■ Make sure na di sya nageempty - (should not go below
○ To prevent irritation in mucous 500 Lts) because it will be difficult for you to replace it kasi
● General considerations di basta basta pinapalitan. Hangga’t maaari it should not
○ A treatment/medication. Has to be ordered be below 500.
○ Supports combustion so it does not sabog ○ Flow meter
● Purposes of oxygen therapy: ■ Meron nagffloat na ball.
○ Provide oxygen according to target saturation rate and maintaining ■ Kung saan tatapat ung ball as you increase or adjust the
within the target range regulator, iikot ung ball or parang may magssuspend na
○ Restore and maintain blood oxygen levels piston
○ Maintain adequate oxygenation of vital tissues and organs ○ Humidifier - eventually magbbubble which means there is air
○ Reduce workload of breathing coming out from the tank
○ Improve quality of life ■ May para siyang mga level. Ung water that has to be
● Indicated for patients with hypoxia, hypoxemia, cardiac failure. coronary placed inside the humidifier should not be tap water
occlusion, anesthesia, certain types of headache because it can be contaminated. It should be cooled boiled
● When does a patient need oxygen? water or minsan ung mga distilled water.
○ Hypoxemia ■ It should also be at the level of the line or above it pero
■ Low oxygen in the blood hindi sobra otherwise this will compromise the exit of the
■ Can cause mild problems such as headache, sweating, and oxygen inside the humidifier.
shortness of breath
■ SPF required
■ Severe hypoxemia is life-threatening. It can ultimately lead
to confusion, coma and death
○ Hypoxia
■ Low oxygen in tissues
○ Clinical decision point: ■ Should not be below the line kasi di mahhumidify ung air
■ Patients with sudden changes in their vital signs, LOC, or ○ Oxygen stand - there should be a stand or bakal sa floor to prevent
behavior may be experiencing profound hypoxia. Patients the oxygen tank from being mobilized and prevent it to follow.
who demonstrate subtle changes over time may have ■ Ung gilid kasi ng tank medo cylindrical or rounded ung
worsening of a chronic or existing condition or a new edges kasi this will facilitate moving from one area to
medical condition (Kaul et al., 2009) another kaya medyo rounded ung edge and hindi flat.
● Why must oxygen be humidified?
○ O2 therapy is combined with a dehumification device to prevent ● Compressed air tank - black tank
mucosal dryness ○ The room air compressed inside the tank
● When/how often can oxygen be administered ○ Used if client is in mechanical ventilation
○ Can be given for a shorter or longer period of time in a ○ The mixture of the oxygen and compressed air will be directed
hospital/home setting toward the mechanical ventilator. This mechanical ventilator will be
○ Prescribed when the blood oxygen level is low providing the required oxygen to the patient.
● How is oxygen level measured
○ Through pulse oximetry
■ Though there are other tests but the fastest way to
determine it is through this
● How is oxygen provided?
○ Wall outlet
■ Commonly seen in the hospitals (medical setting)
1. Flow meter/regulator valve - nurse is the one who sets it depending on the
doctor’s order. 1 L/Min or 10 L/Min. 1-10 L
2. O2 gauge - if it is a tank, it is the visual indication if the tank still has oxygen.
○ Oxygen Cylinder May laman pa bang oxygen yung tank? If it's close to 0 or red, it is almost
■ Mga tanks empty → inform for changing or have a standby o2 tank for immediate
■ Portable o2 tanks – if the patient needs to be in a certain replacement
area in a hospital or transferred from one area to another. 3. Cylinder valve
The delivery of oxygen is not stopped even in transit.
4. Bubbling bottle - for humidification purposes. It is filled up with sterile water.
If the water is almost finished, you can refill with sterile water.
PARTS OF OXYGEN DELIVERY SYSTEM
5. Aquapack - disposable type
● Oxygen - green tank
○ Has a valve to release the oxygen from the tank
DIAZ, DIWA, FLANDEZ, FRANCISCO, GARCIA | 2NUR-3 6
SUBJECT | 1ST SEMESTER
(3) SIMPLE FACE MASK (40%-60%) at 5-10 LPM
● 4 types of O2 masks:
○ (1) Simple face mask
○ (2) Nonrebreather
○ (3) Partial rebreather
○ (4) Venturi mask
NURSING CONSIDERATIONS
● Note: O2 is colorless, odorless, and tasteless, and dry gas that supports
combustions
● Nursing implication
○ It can irritate mucous membrane of the airways
○ It supports combustion – fire
■ Make sure to keep it from heat sources and flammable
materials. Don't forget to put up a sign that oxygen is in use
and strictly no smoking
DIFFERENT OXYGEN DELIVERY SYSTEMS
● Can be low flow or high flow system
● Simple face masks have no rebreather bag. It’s a simple mask
LOW FLOW SYSTEM / LOW FLOW ADMINISTRATION DEVICES ● Delivers oxygen concentrations from 40% to 60%
● A flexible cone shaped device with a metal strap to mold the mask
● This will provide onl around 21-40% of fraction of inspired oxygen that is into the nose, with an adjustable head strap and multiple exhalation
needed for the client ports.
● Contraindicated to clients who retain carbon dioxide
(1) NASAL CANNULA (21-45%) at 1-6 LPM ● Use for short-term oxygen therapy
● O2 concentration: 21-45% at a flow rate of 1 to 6 L/Min
● May be used in clients with COPD at 2-3 LPM if venturi mask is not
available
(4) PARTIAL REBREATHING MASK (60%-90%) at 6-10 LPM
● Tubing placed behind ears ● Mask with a rebreather
● Check on integrity of skin behind ears and nose ● Partial rebreather - bag should ALL THE TIME be inflated. For what
● There’s this tube with 2 prongs. These 2 prongs should be placed purpose? Kasi sa mask, may exhalation ports (may butas), ung butas
inside the nostrils of the client na yan bilog sya pero may maliliit na butas. Pag partial rebreather
● Naka curve sya downwards. And dapat pag nilagay sya sa loob, mask, it is open WITHOUT ONE WAY VALVE.
dapat pababa din. Why? This is curved based on the anatomical ● Naka-open sya so everytime client will inhale and exhale, there will
structure of the nostril be some amount of room air that could be breathe in through the
● Before you apply this, see to it that the nostrils are clean and that it rebreather mask kasi may butas
has the right size for the client since iba iba ang size niya. ● 6-10 L/min; FIO2 60-90% = low-flow
● If you will be administering this, dapat bukas na ung oxygen source. ● Mask with rebreather bag
If nagbbubbles na, meron na un. ● The bag should all the time be inflated because if not, it will be more
○ And if you have already connected this to the oxygen of CO2 that client will be inhaling and not the mixture of CO2 and
source, ifeel mo kung meron nang parang bumubuga na air O2
sa may nasal cannula before administering it to the patient. ● It has no one way valve
● Simple , effective, comfortable device ● Every time client is inhaling and exhaling, there is some amount of
○ Remember to remove the cannula and clean the nares room air that will be breathe in kasi may butas
every 8 hours ● The mask differs from non rebreathing mask for there is no one way
○ Provide oral care flap valve between bag and exhalation port.
○ Use gauze pads Behind the ears to decrease irritation (lalo ● Indicated for clients with severe hypoxia
na if pang matagalan na gamit, it can cause irritation at the ● The air mixes with room air through the ports
back of the ears)
● 1-6 L/min
● Provides oxygen concentration of 21-45%
● Does not hinder eating, drinking, and speaking
(5) NON-REBREATHING MASK (95%-100%)
● WITH ONE WAY VALVE, naka cover siya
● May one way valve na nagoopen and close. Every time that the
client will exhale, there will be CO2 that will be removed from the
mask, some will be trapped inside the rebreather bag. If the client
will inhale, since there is one way valve, di makakapasok room air.
(2) OXYGEN-CONSERVING CANNULA Ang maiinhale lng is oxygen frm O2 source and oxygen trapped
○ A type of nasal cannula pero it has an oxymizer (parang equipment inside the rebreather bag.
just below) to serve as a filter for the oxygen and will provide client ● The rebreather bag is combined with CO2 and O2. as much as
more precise oxygen delivery through nasal cannula possible, this should be inflated all the time. If not, it will be more of
○ Usually kasi ang nagbibigay talaga ng precise amount of fiO2 is the CO2 that the client will inhale and not the mixture.
venturi mask. Pero eto, per cannula naman. Ang venturi is more of ● 10-15 L/min = 80%-95% FIO2
the mask ● A flexible cone shaped device with a thermobag attached with a one
○ FIO2 = fraction of inspired oxygen delivered way valve between the bag and the mask to allow for inhalation of
oxygen and prevention of accumulation of carbon dioxide
● Used for hypoxia patients
● Reservoir bag should not collapse during inhalation. It offers highest
concentration among low flow devices
● The valves open during exhalation/expiration and opens during
inhalation
● There is a one way valve.
● Every time a client breathes out, CO2 will be removed from the
mask and some will also be trapped.
DIAZ, DIWA, FLANDEZ, FRANCISCO, GARCIA | 2NUR-3 7
SUBJECT | 1ST SEMESTER
● If the client breathes in, di makakapasok room air. It will be the
oxygen from O2 source and oxygen trapped inside the mask (2) FACE TENT
● Is a shield like device that fits under a patient’s chin and sweeps
around the face
● Open mask not unlike oxygen mask that should cover nose and
mouth
● Sometimes used in derma
● 25%-50% FIO2; 4-8 LPM
(3) OXYGEN TENT/CROUPETTE
● The client is placed inside a tent
● The child is inside it na parang kulambo. It’s made of plastic, is
transparent
● Often used for children to allow freedom of movement in the bed or
crib
● Problem is that it creates moisture that leaves damp clothing and
linens, so you must frequently change them.
● Oxygen source, humidified
● Since oxygen is being provided, there’s a possibility for it to
condense. Dry up the tent all the time to see the client inside. Check
on the linens and check gamit ng client
● Based on the pic above, the nasal cannula is on the upper left. ● Ex: the baby is holding on to a stuffed toy made of fur/cloth, the
○ Tubing is placed behind the ears and will be tightened para tendency is it will moisten. If something is wet, it’s a good medium
di mahatak for growth of microorganism
○ Check on the intergrity of the skin behind the ears and the ● If friction toys, di rin pwede ksai pwede mag promote ng combustion
nose ung oxygen since nasa loob nga ung laruan
○ Apply gauze sa may likod ng tenga ra di maimpair skin ● Ung tent din, the hemline should be tucked in to prevent oxygen
integrity from escaping. Parang sa kulambo, pinapasok ung dulo ng kulambo
● Oxymizer - sa upper right to prevent mosquito from coming in. eto baliktad, we’re trying to
● Simple mask - lower left - no rebreather bag; the mask itself should prevent the oxygen to escape.
cover both the nose and the mouth; dapat medyo tight to prevent
escape of air
● Nonrebreather mask - lower right ; with rebreather bag ; the white
on the mask is the one way valve to prevent client from inhaling
room air, but client will be able to exhale CO2
○ Remember: The bag should always be inflated
(6) Croupette
(7) Oxygen tent
HIGH FLOW SYSTEM / HIGH FLOW OXYGEN
● Around 60-100% (in the book, be familiar with the concentration of (4) OXYGEN HOOD
O2) ● Can be used for high and low flow oxygen
(1) VENTURI MASK ● Specific for pediatric clients but there are some adults who may be
● Low concentration venturi-type mask is preferred for clients with using this.
COPD because it provides an accurate amount of oxygen. They ○ Fiberglass dome placed over the head of client
require 2-3 L/min or 28% oxygen. ● Generally used to deliver O2 for infants at rate of 100%
● Providing a precise delivery of oxygen based on the venturi barrel ● It is placed over the infant's head and shoulders
○ Meron parang adaptor na pwede ilagay tas color-coded. ● Make sure to cluster activities when giving medications or doing
Nakasulat kung how many percent is to be administered to procedures to make sure that the hood is in placed and oxygen
the client would not escape
● Cone-shaped high-flow device with entrainment ports of various Oxygen hood and oxygen tent is commonly used in pediatric settings because they
sizes at the base of the mask are able to provide high concentration of humidified oxygen
● Can deliver a more precise concentration of oxygen to the patients
(color coded)
● Can identify the number of liters per minute through the color of the
venturi mask valve
(5) TRACHEOSTOMY COLLAR
● A miniature oxygen mask only intended to cover tracheostomy
○ Tracheostomy - an opening made to the trachea to provide
patency in the lower airway
● can deliver high humidity and O2 to client with tracheostomy
DIAZ, DIWA, FLANDEZ, FRANCISCO, GARCIA | 2NUR-3 8
SUBJECT | 1ST SEMESTER
(6) T-PIECE/BRIGG’S ADAPTOR
● Useful for weaning patients from mechanical ventilation
● Onti-onting tinatanggal na siya sa mechanical ventilator
● T-tube / T-Piece or Briggs Adaptor
● Transtracheal catheter - use at home
● Tracheostomy Button - also an artificial airway used for weaning patients
from mechanical ventilation
HYPERBARIC OXYGEN THERAPY
● Exhalation port
● Involves breathing in pure oxygen in a pressurized environment inside the
chamber
● Air pressure is around 2-3x greater or higher than the normal air pressure
● Used to treat decompression sickness (ex. Scuba divers, carbon monoxide
poisoning, infections, and radiation injuries)
● Connected to O2 port
● The one attached to endotracheal tube
(7) AMBU BAG (ARTIFICIAL MANUAL BREATHING UNIT)
● Pinipindot siya to provide the client with positive pressure to inflate
the lungs
● Positive pressure ventilation INHALATION THERAPY
● Stands for Artificial Manual Breathing Unit
● Or bag valve mask ● Provide clients with soothing sensation, bronchodilation, or it depends on
● Self inflating and sometimes called resuscitator what has been the reason why client was ordered for such
● Can provide 100% oxygen, provided at least 10L/min O2 is used
● The cord is connected to the auto-gauge of the tank/outlet, and MOIST INHALATION
then set the flow meter at 10L/min so the bag will inflate then you
can now use the ambu bag Steam inhalation
● Available in different sizes, for adults and for pediatric clients ● Steam itself will be inhaled by client
● To moisturize airway or liquefy secretions
● Usually walang gamot. Parang air lang
● Vicks vaporub - minsan hinahalo kasi may mint scent na pwede maka soothe
ng difficulty of breathing
Medimist inhalation
● Are for adults to administer bronchodilators
● May gamot na nilalagay sa machine
● Almost the same as aerosol inhalation kasi parehas na may nebulizer set
wherein there will be medications which need to be converted into small
particles.
Aerosol inhalation/ Small Volume nebulizer
○ Commonly used among pediatric clients to administer bronchodilators or
expectorants
○ Connected to a nebulizer machine that will cause pressure that will cause
medication to vaporize
○ Pag nagvvaporize, it will be inhaled by the client and themedications will be
directed toward the lower airways causing bronchodilation (depende sa
reason)
(8) INCUBATOR/ISOLETTE
(9) FACE MASK Examples of moist inhalation:
(1) STEAM VAPORIZER
TRANSTRACHEAL/TRACHEOSTOMY
● Tracheostomy collar/mask
DIAZ, DIWA, FLANDEZ, FRANCISCO, GARCIA | 2NUR-3 9
SUBJECT | 1ST SEMESTER
○ Purposes:
■ To liquefy mucus secretions
■ To warm and humidify inspired air ○ Older adults with weak grasp, hand tremors, or coordination
■ To relieve edema of the airways problems may not be able to manipulate or hold a nebulizer, so
instead they may make use of a mouthpiece
■ To soothe irritated airways
○ For home care, make sure to rinse your nebulizer parts after each
■ To administer medications
use with clean water and air dry it.
○ For it to be effective, you need to render it for 15-20 mins
○ Small Volume Nebulizers
○ Perform deep breathing and coughing techniques after the
procedure
○ Make sure to provide good oral hygiene
○ Perform aftercare of your materials/equipments uses
○ Document the findings and reactions of the patient to the treatment
○ A dependent nursing function
■ Requires a doctor’s order before it is done to the patient
○ Inform client about procedure
○ Check electrical device before use
■ Baka mamaya mag malfunction/ sira na pala ● Converts a drug solution into a mist that is inhaled by the
○ Place steam inhalator in a flat, stable surface patient into their tracheobronchial tree
■ Make sure it is safely placed ● The droplets in the mist are much finer than those created
○ Semi-fowler’s position by metered dose inhalers or dry powder inhalers
○ Cover client’s eye with wash cloths ● A face mask or mouthpiece held between the teeth
■ May cause eye irritation/burning sensation due to hot delivers a nebulized mist
steam ● A nebulized medication is designed to create a local effect
○ Place 12-18 inches away from the client’s nose or adjust the distance but it can also be absorbed in the bloodstream through the
as necessary alveoli, and as a result it may create a systemic effect.
○ CAUTION: Avoid burns. Cover the chest with towel. Assess for
redness. (3) AEROSOL MASK
■ You cover the chest since maddampen siya and may cause
the gown to be moist
(2) NEBULIZATION
● Is a process of adding medications or moisture to inspired air by
mixing particles of various sizes with air
● Useful for client who requires high humidity after extubation or after
upper airway surgery or with thick secretions
● Assess that the aerosol mist escapes from the vents of the delivery
system
● Empty condensation from the tubing after use
● Remove and clean the tubing at least every 4 hours
● Adding moisture to the respiratory system through nebulization ● May also deliver medication to the lungs
improves clearance of pulmonary secretions ● Pediatric variation:
● Medications like bronchodilators, mucolytics, and corticosteroids are
often administered by nebulization
● Ask client to place the mouthpiece tightly inside the mouth then
normal inhalation and exhalation.
● Medicine cup - where you put your medicine (ex. salbutamol)
● Hose - connects the medicine cup and the mouthpiece to the
nebulizer
DRY INHALATION
● Metered dose inhaler (MDI)
○ Push the canister to supply the medication to the client
● Spirit of Ammonia
○ Pag may nahihilo, pag inamoy to magigising ka talga
○ Ung iba diretso na, from the small bottle ng anommia. Ung iba
nilalagay sa cotton ball tapos ipapaamoy
● Puff/ Turbohaler
● Rotadisk
Examples of Dry Inhalation:
(1) METERED DOSE INHALERS
DIAZ, DIWA, FLANDEZ, FRANCISCO, GARCIA | 2NUR-3 10
SUBJECT | 1ST SEMESTER
● 3 parts: canister, plastic holder, and cap
■ Canister - the one you have to press if you’re going to
administer the medication to the client
○ Initial teaching is done by the doctor not the nurse.
○ Some MDI have actuations/counters (mas mahal).
(3) TURBOHALER
●
● Is a device that sprays a pre-set amount of medicine through the
mouth to the airways.
● 5 minutes apart for each puff
● Spacer - ensures that the lower airways receive the medication
■ Used especially for pediatric clients
■ “Aerospace” “babyhaler”
■ Ideally, dapat pagpuff, inhale then control breathing pero
since baby, you dont expect the baby to comply. Pag may
spacer, magfflow lng ung gamot so habang humihinga
naiinhale nya ung gamot with a mask
■ Okay lang umiiyak ung baby kasi mas naiinhale nya ung (4) HANDIHALER
mismong gamot ●
○ Wash the spacer, nebulizer set kasi may narretain na gamot.
Nebulizer dapat soap and water kasi pwede magcrystallize ung
medications sa tubing
● Uses powdered medication or tablets
How to use a metered dose inhaler
● Baka may asthma ka kaya u use metered dose inhaler
1. Shake the medicine.
2. Hold the metered dose inhaler so the mouthpiece is at the bottom. Open your
mouth and hold the mouthpiece 1 ½ to 2 inches (about 2-3 finger widths) in
front of your mouth. Breathe out normally.
3. Press the metered dose inhaler down once so it releases a spray of medicine
into your mouth while you breathe in slowly. Continue breathing in as slowly
and deeply as possible.
4. Hold your breath for 10 seconds or as long as it is comfortable. Breathe out
slowly.
How to use a metered dose inhaler with an aerochamber (Spacer)
CLOSED THORACOSTOMY TUBE
1. Shake the medicine.
2. Insert the mouthpiece of the inhaler into the rubber-sealed end of the
aerochamber PAGE 656 OF THE BOOK
3. Breathe all the air out of your lungs then put the aerochamber into your ● Inserted inside the pleural cavity to drain whatever it is that has been present
mouth between your teeth. Make a tight seal around the mouthpiece with (accident, inflammation, bacterial invasion)
your lips ○ Chest wall has 3 layer: visceral pleura, pleural cavity, parietal
4. Press the metered dose inhaler down once to release a spray of medicine. ● Treatment for most types of effusions, pneumothorax, hemothorax, and
The medicine will be trapped in the spacer. Breathe in slowly and deeply post-op chest surgery or trauma
5. Hold your breath for at least 5-10 seconds. Breath out slowly ● TUBE INSERTED INSIDE THE PLEURAL CAVITY to drain whatever it is that
has been present
○ If air - pneumothorax
■
○ Fluid - hydrothorax
○ Blood - hemothorax
○ Pus - pyothorax or empyema
● Purposes:
○ To drain out fluids or blood
● Insert a tube on the anterior/posterior aspect
● Prepare a gauze with petroleum jelly para if mahatak, matakpan agad to
prevent dair
THE MECHANICS OF BREATHING
(2) ROTADISK/DISKUS ● In normal situations, the pressure between the pleura of the lungs is below
● May tablet tapos ilalagay sa loob atmospheric pressure
● Pag press, mappuncture ung gamot (may parang needles sa loob) ● When air or fluid enters the intrapleural space, the pressure is altered, and
then ask the client to inhale this can cause collapse of a portion of the lungs
DIAZ, DIWA, FLANDEZ, FRANCISCO, GARCIA | 2NUR-3 11
SUBJECT | 1ST SEMESTER
● Even with adequate oxygenation and an open airway, a patient with a
collapsed portion of the lung will not have adequate oxygen - carbon dioxide
exchange
● The only treatment for this altered condition is to restore the negative
pressure to the intrapleural space. This is accomplished through the use of a
chest tube.
CHEST TUBE
● A large catheter inserted through the thorax to remove fluid (effusions), blood
(hemothorax, and/or air (pneumothorax)
● PURPOSES:
○ To remove air or fluids in the pleural space
○ To reestablish the negative pressure and re expand the lungs
● CHEST TUBE SIZE:
○ Diameter depends on:
■ Size of the patient
■ Type of drainage (air/fluid)
■ Durations of drainage
○ Size
■ Infants and young children Fr. 8-12
■ Children and young adults Fr. 16-20 ● (1) One Bottle System/ Single chamber
■ Most adults FR. 24-32 ○ Serves as a collector and water seal and drainage
● SITE OF CHEST TUBE INSERTION ○ Used for removing small amount of drainage
● 2nd to 3rd intercostal space if air is removed (air is lighter kaya
higher)
○ Tube coming from the patient is immersed in 3-5 cm water → the air
● 5th to 6th intercostal space (Posterior or lateral - used to drain escapes out of the other tube
fluid/blood/pus and suction is applied
○ You have to make sure to mark the level of the water so that you can
determine the drainage output so that you can separate
○ Ex. Initial water amount is 250 ml, after 2 hrs, naging 300 ml,
meaning may drainage na 50 mL
○ Make sure you have a spare bottle to replace the bottle with a
sterilized one
○ Expect fluctuations sa water seal
○ If nagbubble, baka may leak sa tubing
○ If nagstop bubble, it could mean the lung has reexpanded
○ Ensure there is a spare bottle to replace the bottle with a sterilized
one kasi need na idrain ung asa bottle eventually if puno na.
○ Quantify how much of the secretion has been drained by the client
○
● Mediastinal Chest tube
● (2) Two Bottle System
● Connected to a drainage system to drain blood/fluid and to prevent
○ Magkahiwalay na yung drainage chamber and water seal
its accumulation in the heart
○ Drainage for fluid
● Commonly used after heart surgery
○ Air flowing into the water seal
○ Right bottle: drainage bottle
○ Left bottle: water seal bottle
● Comparison of a patient with pneumothorax and a patient with a re-expanded ○ The tube from the patient goes to the drainage bottle (You can
lung because of the chest tube accurately measure the drainage from the px) → The air escapes and
○ The air is removed through the chest tube to allow the lungs to go through the water seal → The tube again is immersed around 2cm
re-expand in 5 cm water → There is a tube open to atmosphere and vents the
● If there is dislodgement, ensure there is: gauze with petroleum jelly air
(vaselinized gauze). Since may butas, aim is takpan agad to prevent entry of ○ Sometimes known as collection bottle
air then put tape on all sides since may negative pressure dapat sa loob ng
chest wall. ● (3) Three Bottle System
○ Paghihiwahiwalayin ang drainage, water seal, and suction
TYPES OF CLOSED CHEST DRAINAGE/CLOSED THORACOSTOMY TUBE
● regardless of the system used, the principles of patient management are the
same. Lung re-expansion occurs as the fluid or air is removed from the space
● Serves as both drainage and water seal
○ One bottle system or single chamber system
○ Two bottle system
○ Three bottle system
■ Reusable types^^^
○ Disposable CT drainage system
r
Reusable types
DIAZ, DIWA, FLANDEZ, FRANCISCO, GARCIA | 2NUR-3 12
SUBJECT | 1ST SEMESTER
■ Leaks may develop a positive pressure in the pleural space
and collapse the lung
○ Suction
■ A pull force of less than atmospheric pressure
■ The water level in the suction system/bottle regulates the
suction pool/pressure
COMMON PROBLEMS EXPERIENCED AND HOW TO TROUBLESHOOT
1. Water seal is accidentally elevated above chest level/ inangat ng relative
yung water seal bottle
○ Immediately lower the bottle and refer to physician
2. Water bottle is accidentally broken (nasipa, nabasag)
○ Clamp or immerse the tubes in a container with water, this is why
you should have an extra bottle/ stand-by bottle bed side
○ Refer right away
3. Chest tube is accidentally pulled out
○ Make sure to cover the site with petrolatum gauze
○ Refer the px
○ Observe for distress
○ Bottle #1: Drainage bottle 3 Things to prepare if you have a px with chest tube
○ Bottle #2: Water seal bottle 1. Clamp
○ Bottle #3: Suction bottle (connected to suction) 2. Extra bottle
○ Drainage → drainage bottle → air from the client → water seal → 3. Petrolatum gauze
suction bottle (with suction machine)
○ Make sure that the middle tube in bottle #3 is immersed in water RESPIRATORY MODALITIES 2
level determined by the physician
○ Immersion of the tube depends on the pressure needed CLICK ME: Respiratory Modalities 2 Lecture Video
○ Can be regulated through the suction machine ● Sometimes, the condition of the patient may be so severe that noninvasive
procedures previously discussed (such as use of oxygen masks and nasal
cannula) no longer work and they resort to invasive procedures.
AIRWAY MAINTENANCE
● Nasopharyngeal/Nasal Airway
○ Nasal Trumpets
■ A flexible tube is inserted
■ Indications
Disposable CT drainage system ● Clenched teeth, enlarged tongue, need for
● Water-sealed drainage system frequent nasal suctioning
■ Measurement
● Hold the airway on the side of the patient’s face,
measure from the tragus of the ear to the nostril
plus one inch
■ Position
● Conscious; semi-fowler’s
● Unconscious - side-lying
■ Use water soluble lubricant to coat the distal 6-8cm for
easy insertion
● Oropharyngeal/Oral Airway
○ Ang kinaganda nito ay yung 3 bottle system ay ito na mismo
○ Disposable
○ Ex. Pleur-evac, atrium
NURSING CONSIDERATIONS
● Assess for signs of respiratory distress (chest pain, breath sounds, vs)
● Assess the drained fluids in the drainage bottle (amount and characteristics)
● Assess the water seal bottle if there are intermittent fluctuations/tidaling. If
you don't see any fluctuations, the system may not be patent or is not
working properly, or the lung has already re expanded
○ Measurement: hold the airway on the side of the patient’s face,
● Assess your suction apparatus. It should be working and can be set in
measure from the opening of the mouth to the ear (back angle of the
different suction pressure
jaw)
● Promote safety of the system, make sure that it is placed 2-3 feet lower than
○ Check for loose teeth, food, and dentures
the client’s chest to drain by gravity. System must be placed in a rack or box.
Pwedeng matumba or masipa pag nasa ibaba ng patient
● Check for patency SUCTIONING
● Observe asepsis
● Never clamp tubings without order from the physician ● Oropharyngeal
● Avoid milking → could increase intrathoracic pressure ● nasopharyngeal/nasotracheal
● Endotracheal
● PRINCIPLES USED IN CHEST TUBE ● Tracheal
○ Gravity
■ Air and fluid flow must be from a higher pressure to a lower PURPOSES
pressure ● To remove secretions that obstructs airway
■ Make sure to keep the chest drainage apparatus below the ● To facilitate ventilation
level of the patient’s chest ● To obtain secretions for diagnostic purposes
○ Water seal ● To prevent infection that may result from accumulated secretions
■ It seals off pleural space from atmospheric pressure ● To maintain a patent airway
■ It should be airtight
DIAZ, DIWA, FLANDEZ, FRANCISCO, GARCIA | 2NUR-3 13
SUBJECT | 1ST SEMESTER
INDICATIONS FOR SUCTIONING
● Thick tenacious mucous/secretions
○ Makapal mahirap isuction
● Decreased or absence of ability to cough
○ Cough reflex is a protective mechanism to dislodge the secretions.
○ This is to prevent aspiration.
● Semi-comatose or comatose patients - patients with alterd level of
consciousness
○ Pwede silang maaspirate sa kanilang mga secretions.
● Ineffective CPT and other non-invasive management.
SUCTIONING ○ When you suction, sa figure B yung level ???
● Hyperventilate with 100% O2 saturation before and after suctioning ○ Pic A – nasopharyngeal yung level
○ When you suction the secretion, you also suction the air. It is ○ Pic C – target is at the trachea / nasotrachea. Medyo malalim
important to hyperoxygenate the patient in order to replace the ○ Both nasophrayngeal and and nasotracheal is mahirap i-delegate sa
oxygen of the patient. You don’t want the patient to experience nurse aide bc of the risk, so follow institutional policies
hypoxia or hypoxemia. ● Mucus Trap
○ Indicators of hypoxia: irritable, apprehensive, anxious, pulse ox
indicates low oxygen saturation.
● Suction not more than 10-15 seconds
○ Because suctioning can suction air and can cause hypoxia.
● Apply intermittent suctioning upon withdrawal using rotating motion
○ As you introduce the catheter in the patient’s mouth or in the
artificial airway like tracheostomy or ET, do not apply suction
pressure yet. You apply it when you remove it, through intermittent ○
matter. In a rotating motion para matanggal talaga yung mga ○ Sometimes in suctioning we collect specimen with doctor’s order, so
secretions. have the mucus trap
● Allow 1-2 minutes between suction
○ Allow rest periods especially in patients with ET and tracheostomy.
○ You will see the rise in the chest of the patient or the eyes open and
umiiyak (?) pa which is signs na nahihirapan yung patient sa pag
suctioning.
SUCTION PRESSURE
● Infants
○ 60-80 mmHg ○
○ If you apply the pressure of adults, the risk of trauma in tha patients ○ As you suction, some secretions will go in the container and we
mouth is high. send it to the lab / ancillary department once we collect enough
● Small children amount
○ 80-100 mmHg ○ Why do we collect?
● Older children ■ Depending on the case of the px, ex. nilalagnat for days na,
○ 100-120 mmHg ubo ng ubo and marami phlegm (greenish), probably
● Adults bacterial infection – so the doctor orders sputum collection
○ 100-150 mmHg for analysis (CS)
○ If you apply the suction pressure of infants/small children, the
pressure is not enough to remove the secretions.
TYPES OF SUCTIONINGS
● Oropharyngeal (Yankauer)
○
○ Also known as tonsilar tip ○ Usually when we suction mouth of adult px, we have to block?? the
○ Rigid, minimally flexible plastic catheter / french
○ Used for thick secretions ○ As we suction the artificial airways (ex. ET and tracheostomy), we
○ Removes secretions up ot back of the throat usually use the green tip catheter or french port
○ Can we delegate suctioning? Answer: depending on agency policy
■ You can delegate oral suctioning to the nursing assitive
personal/nurse aid/nursing assitant.
■ You have to understand the concept of delegation, you just
transfer the task but the accountable is the nurse.
■ Make it a point that when you delegate, may alam yung
gagawa nung procedure.
■ Also check on your patient every now and then, since they
are still under your care
■ Bottomline: follow the institution’s policies about it
○ Where do you find px with ET tube or ??? tube?
■ ICU, highly skilled nurses
● Nasopharyngeal / Nasotracheal Suctioning
○ Removes secretions from pharynx / throat and trachea
○ Deep breath upon insertion
■ Kung wala artificial airways, a form of hyperoxygenating
the patient is to instruct the px to do deep breathing ○
exercises ○ Everytime we suction a patient, assess the oxygenation status of the
● but if your px is ET / endotracheostomy, the px is px
connected to a ventilator, so there is need to ■ Can be assessed thru behavioral (ex. px is lethargic,
hyperoxygenate with ambu bag apprehensive, anxious, etc.), but what is advised is the
○ Length of insertion (tip of nose / mouth to angle of the mandible) pulse oximeter to have an objective accurate indicator of
■ Adult – 16 cm the oxygenation status in the px.
■ Older children – 8-12 cm ■ In between, before, and after – check the O2 saturation of
■ Younger children – 4-8 cm the px bc if it reaches below 90%, ask the px to deep
breathe, or hyperoxygenate first, para tumaas muna yung
O2
● Bc if mababa O2 saturation then mag susuction
ka, it does not make sense at all
ET AND TRACH CARE
DIAZ, DIWA, FLANDEZ, FRANCISCO, GARCIA | 2NUR-3 14
SUBJECT | 1ST SEMESTER
doctors result in a tracheostomy tube which is usually long-term or
permanent.
● It can also be used for a short-term basis. For example,a patient undergoes
thyroidectomy. The thyroid has a role in calcium regulation. Then tinanggal
na, the risk for hypocalcemia is high, and if there is hypocalcemia, tetanus is
possible. We induce tetanic contractions including the airway. The risk of
respiratory paralysis/difficulty in this case is high. Kaya inuunahan na, so they
use a tracheostomy tube for a temporary purpose. Once the condition
improves, they remove it. However, it still depends on the case of the patient.
● Usually the use of tracheostomy tube is long term. There are patients who go
home with a tracheostomy tube.
● Patient with respiratory problem (di na makahinga), resort with an invasive
procedure, 02 facemask, O2 cannula
● Endotracheal intubation
○ A short term way of relieving airway problems
● Nursing responsibility:
○ Prepare the materials and check its functionality:
■ Intubation set (usually in the ER)
● Laryngoscope
● Blade Tracheostomy
○ Straight ● Inserted by a doctor
○ Curved ○ It is done at the OR (operating room)
○ Shorter one (for pediatric clients) ● To provide artificial airway
○ When you connect the handle and the ○ Main purpose is to provide artificial airway
blade, iilaw yan since there’s a battery ● To maintain patent airway
inside ○ Also serves as a route for suctioning the secretions of your patient
and by doing so prevents the infection of the respiratory tract
● Prevent infection of respiratory tract
● Usually needs frequent suctioning
○ Especially if it is immediate post OP, so medyo madugo pa pero
habang tumatagal, nawawala naman.
● Advance suction catheter about 10-12.5 cm or until patient coughs
○ If masyado malalim ang pagsuction, baka nagagasgas na yung
airway. Compared to an ET, short ang mga tracheostomy tube.
○ Assess the patient every time you suction
○ We do not want to suction because of severe irritation and trauma to
the patient's airway, may blood na yung nasusuction, increasing the
risk of infection.
● The target is above the carina ● Do not occlude y-port upon insertion
○ Auscultate ● Limit suctioning to 3 times, multiple suctioning may result to irritation and
● Di pwedeng masyadong malalim → absence of perfusion eventually increased amount of secretions
○ To determine this, auscultate the right side of lungs, may air but sa ○ If kaya ng 3 times
left side biglang may absence or diminished of air flow → inform ○ For example emphysema patients, every time you suction, may have
doctor phlegm ulit. So, sometimes we need to suction as needed.
● When intubating a patient, provide privacy for patient ○ Yung limit 3 times is for those na naka tracheostomy. For example, a
patient who has a brain tumor and underwent craniotomy.
ENDOTRACHEAL (ET) Remember the medulla and the pons as the respiratory center, and
● Indication: because of the operation, hirap na sila makahinga. Because of the
○ route for mechanical ventilation condition, the tracheostomy is permanent. You can suction them 3
○ easy access for secretion removal times, compared to COPD patients.
○ artificial airway inserted to relieve mechanical airway obstruction. ● Position: supine or high fowler’s
● Cuffed – adult ○ Preferable: high fowler’s position especially when you suction the
● Uncuffed – pedia (sizes 5 below) patient, to minimize aspiration.
● Sterile technique - acute phase following tracheostomy insertion
Care of the patient with ET ○ To prevent and minimize infection
● Position: supine or side-lying ● Clean technique - once it became a client procedure or home care
○ Some doctors prefer naka low fowler's position
● Repositioned on the opposite side of the mouth at least every 24-48 hours ● Tie: One-man: Place the new tie first then remove the old one
● Depth and length during insertion should be maintained ○ Trache care requires time kasi after mo mag suction, magttrache
○ Notice that in the endotracheal tube, there are levels (22,24,26) so care ka naman
you should know when successful intubation has been achieved ○ Done if mag-isa ka
and at what level, because this would signify that the perfusion is ● Two-man: first person; hold the tube, second person- remove old and replace
okay for both lung fields. with a new tie
○ When you do your care, you have to maintain the level. For example, ○ If may kasama ka
the level is at 22, then napansin mo napailalim or napaibabaw, there ● Clean by necessity not be definite schedule
could be a problem for your patient. ○ You do it for your patient para gumaling siya
● Level of the tube: gumline or “bite” of the patient ○ Will still depend on the needs of the patient
● Remove all previous tapes. Check the lips for cracks and irritation ● Usually on the first 24-48 hours. Trache care is done every 4 hours
● Do not uncuff ○ Or depending on the doctor’s order
○ Do not attempt because pwede matanggal and it can be a big ● Provide adequate humidification and hydration
problem in the unit. ● Prevent aspiration - inflate tube cuff before giving gavage or oral feedings,
ET HOLDER deflate the cuff after 30 minutes-1 hour after feeding as ordered
● They secure the endotracheal tube, especially among pediatric patients since
sometimes they are very anxious about it (gusto nila tanggalin). Parts of Tracheostomy Tube
● Secure the ET in place
● If the patient is anxious, explain the purpose. The more they get anxious, the
more na mahihirapan sila huminga
Plastic Tracheostomy Tube
TRACHEOSTOMY TUBE
● The use of endotracheal tube is usually term, depending on the guidelines
the doctor follows. So kunwari if 6 months na, then hindi pa din natatanggal,
DIAZ, DIWA, FLANDEZ, FRANCISCO, GARCIA | 2NUR-3 15
SUBJECT | 1ST SEMESTER
● ABNORMALITIES OF THE PLEURAL SPACE
Tracheostomy with cuff
○ Fluids tend to settle down
● SITE OF CHEST TUBE INSERTION
● This is a __?? of a type of cannula
● You gradually wean?? the patient
Tracheostomy without cuff
○ 2nd or 3rd intercostal space - air is removed
○ 5th or 6th intercostal space (Posterior or lateral - used to drain
Placement of Tracheostomy Tube fluid/blood and suction is applied
● TYPES OF CHEST TUBES
● Depending on the case of your patient
Tracheostomy Collar
○ One way bottle system
■ Sometimes tub is in 2 cm water
■ Usually for patients with pneumothorax
■ No drainage expected because only air is removed from
● To secure the tracheostomy
the patient
Tracheostomy Mask
● Expect that it will moisten because oxygen will enter the mask
● Nursing responsibility: assess the mask/patient in totality because moisture is
a good medium of bacterial growth ○ Two way bottle system
■ Additional bottle connected to a suction machine
39:00 - 45:30 gwy ■ Used for patients with blood traumas
● DEFINITION
○ Also known as the chest tube or closed chest drainage
○ A device inserted by a physician when air or fluid enters the
intrapleural space compromising oxygenation or ventilation, and is
connected to sterile bottles or disposable commercial products
which acts as a drain or water sealed
● PURPOSES
○ To remove air or fluids in the pleural space
■ Pleural cavity is between the visceral and parietal pleura
which is a potential site for entry of air or fluid which
increases the risk of compromised breathing by the patient
○ Three way bottle system
■ Pleural space normally has 100-150 ml of fluid which acts as
■ Drainage, water seal, and suction bottles are now
a lubricant and prevents friction rubs during cycles of
separated into 3 bottles
breathing
● RESPONSIBILITIES
○ To reestablish the negative pressure and agree expand lungs
○ Assess the drainage, especially kung may blood. The bottles have
● INDICATIONS
calibrations beside them
○ Pneumothorax - air in the pleural space
○ Ex. Px has hemothorax trauma, nurse endorsed that the px level is at
○ Hydrothorax - water or fluid in the pleural space 400 mL. After your shift, it became 500 ml. Output is 100 mL.
○ Hemothorax - blood in the pleural space Document and write in the IO sheet CTT output under “Others”
○ Pyothorax - pus in the pleural space category
■ Cheesy like substance or milky
DIAZ, DIWA, FLANDEZ, FRANCISCO, GARCIA | 2NUR-3 16
SUBJECT | 1ST SEMESTER
○ Pano pag malapit na mapuno? Magready ka na ng bote. Punta ka sa
CUR (?)/ Central Supply Unit. Do not panic dahil readily available at
sterile na ang mga ito
○ Ingatan na hindi matisod ng kung sino man. Usually merong bottle
guard. We seldom encounter this because the bottle systems are
commercially prepared now, pero mas mahal. Wala ka nang iisipin,
order ka na lang
○ Check for fluctuations along the tube. Fluctuations are normal.
Usually medyo nag increase siya when the px is inhaling. Sometimes
intermittent bubbling is also normal.
○ If the bottle system is used, you should prepare at bedside forceps,
clamp, tape, and petrolatum (vasilinized) gauze. In case nabasag
yung bottle, i clamp then palitan. Para di ma dislodge yung tube
kung san naka insert, maglagay ng petrolatum gauze and tape, call
for help to call the doctor
○ In case na may continuous bubbling sa bottle, that signifies air leak,
which has to be assessed and investigated
○ Pag walang bubbling or fluctuations, this also has to be assessed
because this signifies that the lung has re expanded. This is
confirmed through xray. Pag nakitang wala nang hemothorax, the
doctor will now remove it. It can be removed at bedside. The nurse
has to assess, prepare gauze and what the doctor would need
Water-sealed drainage
● Eto na yung usually nakikita ngayon compare sa bottles
● Medyo ginagamit pa yung bottles in some government institutions because it
is cheaper
SUCTIONING AND TRACHEOSTOMY CARE DEMONSTRATION VIDEO
LINK: https://drive.google.com/file/d/1yyp-ZoFkCaFvtnh4rxdjaGhQ37bpKNka/view
DIAZ, DIWA, FLANDEZ, FRANCISCO, GARCIA | 2NUR-3 17
You might also like
- 11 Lung PathologyDocument7 pages11 Lung PathologycarlgangcaNo ratings yet
- Chapter 21 RespiratoryDocument5 pagesChapter 21 RespiratoryJanet KayeNo ratings yet
- Critical CareDocument21 pagesCritical Carepaulzilicous.artNo ratings yet
- Trauma Module FinalDocument34 pagesTrauma Module FinalMarian YuqueNo ratings yet
- Schwartz's Hour Notes On TraumaDocument19 pagesSchwartz's Hour Notes On TraumaEver Seneca EscaLera100% (2)
- The Respiratory SystemDocument40 pagesThe Respiratory SystemAdriana ChasiguanoNo ratings yet
- (BCA 3) Respiratory Physiology (Dr. Mendoza)Document9 pages(BCA 3) Respiratory Physiology (Dr. Mendoza)Carla P100% (1)
- Tourocom Oms2: Omm (Section Done)Document56 pagesTourocom Oms2: Omm (Section Done)Ritesh PatelNo ratings yet
- Week 10 - Assessment of The Thorax and LungsDocument8 pagesWeek 10 - Assessment of The Thorax and LungsJuan Miguel TevesNo ratings yet
- M4 - Didactic - NCM 118Document4 pagesM4 - Didactic - NCM 118KARL FESARITNo ratings yet
- Oto.s1.l04.nasal Discharge (Rhinitides) (CD)Document9 pagesOto.s1.l04.nasal Discharge (Rhinitides) (CD)VICTOR AMORESNo ratings yet
- Pulmo Case Simulation-TEAM Yellow-Blue - 01-04-21Document35 pagesPulmo Case Simulation-TEAM Yellow-Blue - 01-04-21Jolaine ValloNo ratings yet
- Line and TubesDocument18 pagesLine and Tubespaulzilicous.artNo ratings yet
- Review - Spinal Cord Injury - 2Document1 pageReview - Spinal Cord Injury - 2Sarah MendozaNo ratings yet
- Pulmonary Ventilation ModuleDocument5 pagesPulmonary Ventilation ModulejunquelalaNo ratings yet
- Analec DigestiveDocument8 pagesAnalec DigestiveDalgom's WifeNo ratings yet
- Feb 24 2024 Gastrointestinal System ReviewDocument6 pagesFeb 24 2024 Gastrointestinal System ReviewJezzabel Kyra BadayosNo ratings yet
- Zoology Mammals (Rabbit)Document3 pagesZoology Mammals (Rabbit)PerrieNo ratings yet
- EMERGENCY NURSING TRIAGE AND BASIC LIFE SUPPORTDocument5 pagesEMERGENCY NURSING TRIAGE AND BASIC LIFE SUPPORTMarvin Heramis RyanNo ratings yet
- Health Assessment (EMA)Document17 pagesHealth Assessment (EMA)ericamaeabellanosa22No ratings yet
- Orotracheal Intubation Techniques and ComplicationsDocument5 pagesOrotracheal Intubation Techniques and ComplicationsDianne GalangNo ratings yet
- PHARMADocument20 pagesPHARMAGummy BearsNo ratings yet
- Week 6Document3 pagesWeek 6api-530814583No ratings yet
- 2P4 Group 5 Chapter 13Document7 pages2P4 Group 5 Chapter 13Chantelle SiyNo ratings yet
- Mods 1-2Document42 pagesMods 1-2Gin CruzNo ratings yet
- The Nervous System342024Document44 pagesThe Nervous System342024anum Asad AliNo ratings yet
- Respiratory System 3 - 6Document6 pagesRespiratory System 3 - 6sapphirelangsapatnaNo ratings yet
- Dean - Diagnostic 1 PDFDocument3 pagesDean - Diagnostic 1 PDFSophia GoNo ratings yet
- AnaPhy - Digestive SystemDocument11 pagesAnaPhy - Digestive SystemGia P. de VeyraNo ratings yet
- Prelims Course Outline Oro-Nasal SuctioningDocument8 pagesPrelims Course Outline Oro-Nasal SuctioningNicole Faith L. NacarioNo ratings yet
- Oxygenation: An Essential Process for LifeDocument14 pagesOxygenation: An Essential Process for LifeVinzii DrtNo ratings yet
- Upper Airway Lower Airway: Respiratory ComplicationsDocument6 pagesUpper Airway Lower Airway: Respiratory ComplicationsKhadijah KhanNo ratings yet
- Our Lady of Fatima University: San Fernando, Pampanga NCMB 314: Case StudyDocument17 pagesOur Lady of Fatima University: San Fernando, Pampanga NCMB 314: Case StudyriverabeanicoNo ratings yet
- 3 AbdomenDocument7 pages3 Abdomenapi-3757921100% (1)
- Chapter 45 - Thoracic Trauma: Episode OverviewDocument17 pagesChapter 45 - Thoracic Trauma: Episode OverviewmalathiNo ratings yet
- Airway Management TechniquesDocument48 pagesAirway Management TechniquesRea Dominique CabanillaNo ratings yet
- Chest PhysiotherapyDocument29 pagesChest PhysiotherapyHari25885No ratings yet
- Thorax Breast and Lymphatic System AssesmentDocument106 pagesThorax Breast and Lymphatic System AssesmentJanelle LasalaNo ratings yet
- Chest PhysiotherapyDocument29 pagesChest PhysiotherapyPaul GeorgeNo ratings yet
- Cptposturaldrainage 150627150049 Lva1 App6892 PDFDocument29 pagesCptposturaldrainage 150627150049 Lva1 App6892 PDFBruce LeeNo ratings yet
- Care of The Patient After ThoracotomyDocument12 pagesCare of The Patient After ThoracotomyRaymond EdgeNo ratings yet
- Ped - Pcc.s1.l04.clinico-Radiologic Correlation (D)Document6 pagesPed - Pcc.s1.l04.clinico-Radiologic Correlation (D)VICTOR AMORESNo ratings yet
- Prone Position Ventilation in Critical Care: IndicationsDocument3 pagesProne Position Ventilation in Critical Care: Indicationsolam batorNo ratings yet
- Week 3 Lung AssessmentDocument16 pagesWeek 3 Lung AssessmentIris FrancheNo ratings yet
- Physiology Reviewer - FinalsDocument7 pagesPhysiology Reviewer - FinalsRYABELLE JESUSA SANCHEZNo ratings yet
- HA Lec Overall 16 23Document8 pagesHA Lec Overall 16 23Sofia Denise JoseNo ratings yet
- Assessment of The Thorax and LungsDocument30 pagesAssessment of The Thorax and LungsMarc Andreo MalalaNo ratings yet
- Anesthesia CasesDocument19 pagesAnesthesia Casesالدعوه الحسنهNo ratings yet
- Anatomi Sistem RespirasiDocument80 pagesAnatomi Sistem RespirasialiaNo ratings yet
- 2) Mechanics of Pulmonary VentilationDocument20 pages2) Mechanics of Pulmonary Ventilationsuresh1malaysia28No ratings yet
- Komplikasi IntubasiDocument11 pagesKomplikasi Intubasijeremy ludwigNo ratings yet
- SEHH2234 2021 S2 Ch14 RespirationDocument56 pagesSEHH2234 2021 S2 Ch14 Respirationmiki leeNo ratings yet
- Histology of The Endocrine System SPC Mls 2f Histo LecDocument19 pagesHistology of The Endocrine System SPC Mls 2f Histo LecnhcsmlmolNo ratings yet
- Reviewer in HaaaDocument15 pagesReviewer in HaaaabiogkristelannNo ratings yet
- Postural DrainageDocument7 pagesPostural DrainageBiway RegalaNo ratings yet
- SuctioningDocument2 pagesSuctioningKyla DauagNo ratings yet
- 3I 3J AUBF LEC L3 Renal FunctionDocument7 pages3I 3J AUBF LEC L3 Renal Functionniquemendoza12No ratings yet
- Neck: Fascial SpacesDocument3 pagesNeck: Fascial SpacesCygrusNo ratings yet
- AirwayDocument66 pagesAirwayMolina NaputriNo ratings yet
- Geria PrelimsDocument44 pagesGeria Prelimsmcdonald 1234No ratings yet
- 1 s2.0 S1089947218303526 MainDocument15 pages1 s2.0 S1089947218303526 Mainmcdonald 1234No ratings yet
- Updated BIblio Guidelines Level 3 2021Document2 pagesUpdated BIblio Guidelines Level 3 2021mcdonald 1234No ratings yet
- DRRDocument8 pagesDRRmcdonald 1234No ratings yet
- Reserts WanDocument4 pagesReserts Wanmcdonald 1234No ratings yet
- A Textbook of Clinical Pharmacology and TherapeuticsDocument476 pagesA Textbook of Clinical Pharmacology and TherapeuticsAli Hassan100% (1)
- EndometriosisDocument2 pagesEndometriosisIrham KasyfulNo ratings yet
- Taking A History of DEPRESSIONDocument3 pagesTaking A History of DEPRESSIONPrarthana Thiagarajan100% (13)
- HAUNG - 2021 - Economic and Environmental Estimated Assessment of PowerDocument10 pagesHAUNG - 2021 - Economic and Environmental Estimated Assessment of PowerThobiasNo ratings yet
- 30.plDocument54 pages30.plRobert GarciaNo ratings yet
- ESSAY 9 (When Grandiosity Speaks, Medical Students Are Supposed To Listen..)Document5 pagesESSAY 9 (When Grandiosity Speaks, Medical Students Are Supposed To Listen..)Kay BorzsonyNo ratings yet
- SikaGrout Aid SDS 1683389Document10 pagesSikaGrout Aid SDS 1683389om prakashNo ratings yet
- Manalo-John, EssayDocument11 pagesManalo-John, EssayJohn ManaloNo ratings yet
- Residency Scheme PDFDocument15 pagesResidency Scheme PDFPriyank Gupta100% (2)
- 404 - Ielts - AcademicDocument140 pages404 - Ielts - AcademicNihar Shah71% (7)
- Dr. Nirali Patel Pediatric Emergency MedicineDocument31 pagesDr. Nirali Patel Pediatric Emergency Medicinemarsan12No ratings yet
- Accutorr V Service ManualDocument125 pagesAccutorr V Service ManualMiguel IralaNo ratings yet
- Fmea FinalDocument30 pagesFmea FinalRakesh SrivastavaNo ratings yet
- Bundy Et. Al, 2017Document265 pagesBundy Et. Al, 2017MathiasNo ratings yet
- Ivf Center PDFDocument15 pagesIvf Center PDFKinjalNo ratings yet
- MDR 040501991289Document1 pageMDR 040501991289REZEL JOHN MAYRENANo ratings yet
- Blood Transfusion GuideDocument7 pagesBlood Transfusion GuideBELIGANIO JOHANNANo ratings yet
- DLL - Mapeh 4 - Q2 - W8Document6 pagesDLL - Mapeh 4 - Q2 - W8Amy Santillan PanisalNo ratings yet
- 36Document8 pages36Andra IrinaNo ratings yet
- The Narcissist On Instagram: Epigrams and Observations - Vol IIIDocument267 pagesThe Narcissist On Instagram: Epigrams and Observations - Vol IIISam VakninNo ratings yet
- Imago Couples Therapy: Instructor's ManualDocument72 pagesImago Couples Therapy: Instructor's ManualSam EmekaNo ratings yet
- Derma Sciences Product GuideDocument36 pagesDerma Sciences Product GuideBrian NiuNo ratings yet
- The Dog Encyclopedia (VetBooks - Ir)Document362 pagesThe Dog Encyclopedia (VetBooks - Ir)miki122295% (22)
- Gabriel's Rage: The Horrors of Ward 13Document59 pagesGabriel's Rage: The Horrors of Ward 13Branislav IvanovicNo ratings yet
- Jurnal MFSDocument11 pagesJurnal MFSAfni YusnitaNo ratings yet
- Import cosmetics Philippines FDA rulesDocument6 pagesImport cosmetics Philippines FDA rulesClaire Anne BernardoNo ratings yet
- Subclavian Steal SyndromeDocument14 pagesSubclavian Steal SyndromeCelineNo ratings yet
- Forecast Reguler TGL 18 Juni Yg Di Kirim Ke PemasokDocument669 pagesForecast Reguler TGL 18 Juni Yg Di Kirim Ke PemasokKFA SENGKANGNo ratings yet
- The Impact of DHIS 2 in Kenya - A User PerspectiveDocument12 pagesThe Impact of DHIS 2 in Kenya - A User PerspectiveJames GathogoNo ratings yet
- Types, Symptoms, Causes and Treatments of Anxiety DisordersDocument2 pagesTypes, Symptoms, Causes and Treatments of Anxiety Disordersbeep777No ratings yet