Professional Documents
Culture Documents
Ncp3 Romeo
Ncp3 Romeo
Uploaded by
Jane Melody Reyes0 ratings0% found this document useful (0 votes)
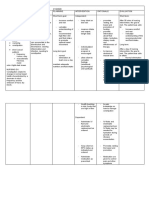
18 views4 pagesThe document outlines an assessment, diagnosis, plan, intervention, rationale, and evaluation for a patient presenting with dry, scaly skin; brittle nails and hair; bruising; fatigue; and constipation. The plan is to establish a bowel program involving increased fluids and fiber, daily monitoring of bowel movements, and developing personal behaviors to support normal elimination. Massage and exercise may help stimulate bowel function. The goals are for the patient to participate in their care, develop a regular pattern of bowel movements, and show physiological improvements. Progress will be evaluated against goals of regular elimination, examination skills, and established habits supporting normal function.
Original Description:
nursing care plan
Original Title
(Ncp3 Romeo)
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe document outlines an assessment, diagnosis, plan, intervention, rationale, and evaluation for a patient presenting with dry, scaly skin; brittle nails and hair; bruising; fatigue; and constipation. The plan is to establish a bowel program involving increased fluids and fiber, daily monitoring of bowel movements, and developing personal behaviors to support normal elimination. Massage and exercise may help stimulate bowel function. The goals are for the patient to participate in their care, develop a regular pattern of bowel movements, and show physiological improvements. Progress will be evaluated against goals of regular elimination, examination skills, and established habits supporting normal function.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
18 views4 pagesNcp3 Romeo
Ncp3 Romeo
Uploaded by
Jane Melody ReyesThe document outlines an assessment, diagnosis, plan, intervention, rationale, and evaluation for a patient presenting with dry, scaly skin; brittle nails and hair; bruising; fatigue; and constipation. The plan is to establish a bowel program involving increased fluids and fiber, daily monitoring of bowel movements, and developing personal behaviors to support normal elimination. Massage and exercise may help stimulate bowel function. The goals are for the patient to participate in their care, develop a regular pattern of bowel movements, and show physiological improvements. Progress will be evaluated against goals of regular elimination, examination skills, and established habits supporting normal function.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 4
ASSESSMENT DIAGNOSIS PLANNING INTERVENTION RATIONALE EVALUATION
Subjective: STG: Dependent: A successful treatment plan is STG:
Her skin has been dry and Mr. Romeo will be involved in the Observe the frequency and built on careful monitoring. Mr. Romeo was involved in the
scaly and her fingernails was making of the bowel program. features of the patient's feces establishment of the bowel
easily broken. on a daily basis. To improve physiological program.
Exercise is out, because she As needed, the patient will report function
lacks energy. a need to defecate. Provide privacy for As appropriate, the patient stated a
Her scalp hair is dry and euthanasia To achieve a regular need to defecate.
breaks easily. Her scalp is The patient's hydration and fiber elimination pattern; and an
scaling. consumption will be increased. Create and carry out a bowel exercise regimen to increase Mr. Romeo increased his intake of
She walks slowly. routine that is unique to you. abdominal and pelvic muscle fluids and fiber.
The patient will report smooth and tone.
She has poor appetite and she full stool evacuation. The patient claimed that the stools
lacks of sleep. were easily and completely
Independent: It can encourage relaxation and
Her skin is cold to touch. LTG: evacuated.
Contribute to general hygiene a sense of well-being.
She has multiple bruises on
and comfort measures.
both forearms and anterior The patient's elimination pattern LTG:
It can reduce pain.
lower legs, which are in will be within normal ranges. The patient's elimination pattern
Make use of a foam mattress,
various stages of healing and was within normal ranges.
a bed cradle, or other similar To sustain normal
tender when touched. The patient will show the process items. physiological functioning, a
Objective: of skin examination. The patient exhibited a technique
prompt reaction to the need to
Lethargic Stress the significance of for skin examination.
defecate is required.
Hypothermia The patient will develop personal
reacting to the need to
Sleep deprivation behaviors that will allow him or The patient established personal
defecate. To encourage proper bowel
Anorexia her to eliminate normally. practices that ensured proper
function
Fatigue Teach the patient how to find elimination.
Brittle public facilities and how to Massage may aid in the
Xerosis wear readily detachable stimulation of peristalsis and
Alopecia clothing when going on trips. the need to defecate.
Teach the patient how to to avoid reliance on laxatives.
massage the abdomen once a Overuse of laxatives and
day, as well as how to find enemas can result in fluid and
and gently massage the electrolyte loss, as well as
transverse and descending injury to the intestinal mucosa.
colons.
To encourage a natural
Teach the patient how to use evacuation stance.
laxatives and enemas
properly. To provide mass for proper
excretion as well as to increase
Encourage the patient to use a muscle tone Encourage fluid
bedside commode or to walk consumption of 6–8 glasses
to the restroom. (1,420–1,900 ml) per day,
unless contraindicated, to
Encourage the consumption maintain normal metabolic
of high-fiber meals. activities.
To encourage compliance with
Collaboration: endorsed count calories.
Assist the patient in
understanding the food
modification plan, working
with a dietician if necessary.
ASSESSMENT DIAGNOSIS PLANNING INTERVENTION RATIONALE EVALUATION
STG: Dependent:
Subjective: Constipation would be a symptom of The patient will Identify On a scale of 1–10, rate the Descriptions of the specifics STG:
"Masakit at nahihirapan akong chronic discomfort. characteristics of pain and pain descriptive qualities of pain, of pain will aid in The patient recognized pain features
dumumi parang may nakalawit na behaviors. such as location, quality, determining what the patient's and pain behaviors.
balat dito sa pwet ko" (I've been severity, and temporal objectives are reasonable.
having trouble / pain pooping, it The patient will develop pain elements and sources of The patient devised pain
seems that there's a skin protruding at management that includes activity relief; pain tolerance; This permits the patient to management strategies that include
my anus) as verbalized by the and rest, exercise, and medication ethnicity; attitude, and values. take an active role in his or activity and rest, exercise, and a non-
patient. regimen that isn’t pain contingent. her therapy. pain-related pharmaceutical regimen.
Change the surroundings to
Objective: The patient will state and carry out encourage sleep at the To lessen or eliminate The patient expressed and carried out
Guarding behavior appropriate interventions for relief of patient's recommendation. discomfort suitable pain-relieving
Restlessness pain.
Facial mask of pain LTG: Apply heat or cold as To alleviate muscle spasms LTG:
V/S taken as follows: directed. and relieve pressure on The patient reported a link between
The patient will state relationship of various bodily regions growing discomfort and stress,
Temp - 37.2OC
increasing pain to stress, activity, and Reposition the patient and, if exercise, and weariness.
PR - 95
fatigue. necessary, use cushions to Behavioral–cognitive
RR - 20 The patient engaged in
BP - 130/80 splint or support sore regions. interventions can assist
The patient will carry out patients in changing learned resocialization activities and
resocialization behaviors and Create a behavior-oriented pain behaviors. behaviors.
activities strategy, such as one for
A contract is an agreement The patient emphasized the
adhering to an activity
that can always be referred to significance of self-care behavior or
schedule.
The patient will state importance of if the patient attempts to activities.
self-care behavior or activities. make decisions that are not in
Contract with the patient to
enhance the likelihood that accordance with the terms of
they will follow the pain the plan.
treatment strategy devised
with him. When a patient wants more
than the plan permits, repeat
Administer analgesic pain the plan's provisions to avoid
medicine in accordance with overmedicating.
the strategy.
Purposeful relaxing attempts
typically aid in the promotion
Independent of sleep.
Teach guided visualization, Caffeine-containing foods
deep breathing, meditation, and beverages ingested less
aromatherapy, and gradual than 4 hours before night may
muscle relaxation to patients. disrupt sleep. Alcohol
Practice with the patient on a interferes with regular sleep,
regular basis, especially especially when consumed
before night. just before bed.
Instruct the patient to avoid Listening carefully conveys
meals that interfere with sleep to the patient that the nurse is
and to avoid coffee and interested. It also aids in
alcohol. determining improvement in
Pay attention to the patient's pain relief.
account of his or her
suffering. Allow time for the Pain-related discomfort may
patient to express his or her hinder the patient from
dissatisfaction. sleeping soundly.
Every day, ask the patient to Achieving pain management
report the quality of his or her objectives while maximizing
sleep. patient cooperation
Collaboration with To advocate for
Employees and families is nonpharmacologic pain
essential. treatment.
Allow the patient to employ To alleviate pain and sadness
alternative pain therapies
typical in his or her culture Maintaining care that is goal-
(such as acupuncture) as a oriented
substitute or supplement to
western therapy wherever
possible.
Please refer the patient to a
support group.
Set up regular
multidisciplinary/family care
conferences.
You might also like
- W2 - MEDSURG Guidelines For Nursing Interventions On Coma PatientsDocument6 pagesW2 - MEDSURG Guidelines For Nursing Interventions On Coma PatientsKyla L. Madjad100% (1)
- NCP DiverticulitisDocument6 pagesNCP DiverticulitisLovely Cacapit100% (1)
- NCP Impaired Skin IntegrityDocument2 pagesNCP Impaired Skin IntegrityEden Marie Francisco100% (2)
- CS5 (AGE) Acute Gastroenteritis NCPDocument2 pagesCS5 (AGE) Acute Gastroenteritis NCPAudrie Allyson GabalesNo ratings yet
- Nursing Care Plan (ImpairedphyssicalDocument5 pagesNursing Care Plan (ImpairedphyssicalkuroroexileNo ratings yet
- Top 3 NCP For CASE-PRES PDFDocument9 pagesTop 3 NCP For CASE-PRES PDFSmartieNo ratings yet
- Nursing Care Plan AppendicitisDocument2 pagesNursing Care Plan Appendicitisderic95% (57)
- Electrolyte ImbalanceDocument76 pagesElectrolyte ImbalanceSarah Racheal Akello100% (2)
- Regaining Bladder Control: For Incontinence on Exertion or Following Pelvic SurgeryFrom EverandRegaining Bladder Control: For Incontinence on Exertion or Following Pelvic SurgeryNo ratings yet
- Chapter 6 - Dimension of Development - Health AwarenessDocument12 pagesChapter 6 - Dimension of Development - Health AwarenessAsh MooreNo ratings yet
- NCPDocument2 pagesNCPWyethBeltranDeLeonNo ratings yet
- NCP-post-op 2Document2 pagesNCP-post-op 2Eyanah Delos ReyesNo ratings yet
- 3CNCPDocument7 pages3CNCPHelen MontesNo ratings yet
- Nursing Care PlanDocument6 pagesNursing Care PlanperezNo ratings yet
- Case Scenario: Hot Spells, Porous BonesDocument10 pagesCase Scenario: Hot Spells, Porous Bonesjaira magbanua100% (1)
- NCP - Hygiene and ComfortDocument3 pagesNCP - Hygiene and ComfortJaella EpeNo ratings yet
- NCP - ConstipationDocument2 pagesNCP - Constipationgringo1388No ratings yet
- Nursing Care Plan Cues Nursing Diagnosis Analysis Goal Intervention Rationale Evaluatio NDocument3 pagesNursing Care Plan Cues Nursing Diagnosis Analysis Goal Intervention Rationale Evaluatio NAishleen OrmandoNo ratings yet
- Spina Bifida NCPDocument3 pagesSpina Bifida NCPShahzad GulfamNo ratings yet
- Nursing Care PlanDocument5 pagesNursing Care PlankingpinNo ratings yet
- Geria NCP, Dela CruzDocument7 pagesGeria NCP, Dela CruzStephany Dela CruzNo ratings yet
- Cues Nursing Diagnosis Planning Intervention Rationale EvaluationDocument2 pagesCues Nursing Diagnosis Planning Intervention Rationale EvaluationBiancaGabatinoAbarcaNo ratings yet
- NCP casepresVBDocument5 pagesNCP casepresVBDaisy Jane TabonNo ratings yet
- Cues/Needs Nursing Diagnosis Scientific Explanation Goals and Objectives Nursing Intervention Rationale Evaluation Short Term Independent Short TermDocument3 pagesCues/Needs Nursing Diagnosis Scientific Explanation Goals and Objectives Nursing Intervention Rationale Evaluation Short Term Independent Short TermLatrell GelacioNo ratings yet
- NCP 2Document2 pagesNCP 2Momshie SyNo ratings yet
- NCP Constipation NauseatedDocument3 pagesNCP Constipation NauseatedEzekiel Seth UmangayNo ratings yet
- Acute Pain Related To Body Response To An Infective AgentDocument2 pagesAcute Pain Related To Body Response To An Infective AgentSheril Sularte CasanesNo ratings yet
- Nursing Care Plan: Assessment Diagnosis Goals Intervention Rationale EvaluationDocument2 pagesNursing Care Plan: Assessment Diagnosis Goals Intervention Rationale EvaluationLeizel ApolonioNo ratings yet
- Disturbed SleepDocument3 pagesDisturbed SleepNicole MapiliNo ratings yet
- NCP Impaired Skin IntegrityDocument3 pagesNCP Impaired Skin IntegrityMiar QuestNo ratings yet
- Nursing Care Plan - NCP-PIHDocument4 pagesNursing Care Plan - NCP-PIHAally ChandraNo ratings yet
- Nursing Diagnosis: Impaired Physical Mobility Assessment Planning Intervention Rationale EvaluationDocument3 pagesNursing Diagnosis: Impaired Physical Mobility Assessment Planning Intervention Rationale EvaluationSheril Sularte CasanesNo ratings yet
- Ncma 2Document6 pagesNcma 2Hilario AndreaNo ratings yet
- NCP VergelDocument3 pagesNCP VergelKelly Vergel de DiosNo ratings yet
- NCP FormDocument3 pagesNCP FormJasmine diokNo ratings yet
- Activity On Care PlanningDocument14 pagesActivity On Care PlanningClaire Maurice JuaneroNo ratings yet
- Actual Nursing Care PlanDocument3 pagesActual Nursing Care PlanJinky Nacar DomingoNo ratings yet
- Nursing Care PlanDocument4 pagesNursing Care PlanKatrene Lequigan100% (1)
- NCPDocument5 pagesNCPMark John Dela CruzNo ratings yet
- Icu NCPDocument8 pagesIcu NCPClaire Nicole ApostolNo ratings yet
- Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDocument1 pageAssessment Diagnosis Inference Planning Intervention Rationale EvaluationLoverMind CabaronNo ratings yet
- Volume 1Document2 pagesVolume 1roxybiscanteNo ratings yet
- Assessment Explanation of The Problem Objective Intervention Rationale Evaluation Subjective: Objective: Sto: DX StoDocument2 pagesAssessment Explanation of The Problem Objective Intervention Rationale Evaluation Subjective: Objective: Sto: DX StoBasema HashhashNo ratings yet
- Assessment Explanation of The Problem Objective Intervention Rationale Evaluation Subjective: Sto: DX StoDocument2 pagesAssessment Explanation of The Problem Objective Intervention Rationale Evaluation Subjective: Sto: DX StoBasema HashhashNo ratings yet
- A N D A P N I R E: Ssessment Ursing Iagnosis Nalysis Lanning Ursing Ntervention Ationale ValuationDocument10 pagesA N D A P N I R E: Ssessment Ursing Iagnosis Nalysis Lanning Ursing Ntervention Ationale ValuationAngYap Lyn Oloan Saipen100% (1)
- Nursing Care PlanDocument5 pagesNursing Care PlanLaceth Joyce T. LASATNo ratings yet
- IndependentDocument4 pagesIndependentMAe Bag-aoNo ratings yet
- Beronio, Gracel Caye M. CMC Module 6 GI Pedia (Nursing Care Plans)Document5 pagesBeronio, Gracel Caye M. CMC Module 6 GI Pedia (Nursing Care Plans)Gracel Caye Maon BeronioNo ratings yet
- Assessment Diagnosis Planning Implementation Rationale Evaluation Subjective Data: Objective Data: Short Term: Independent: Short Term: Goal Partially MetDocument3 pagesAssessment Diagnosis Planning Implementation Rationale Evaluation Subjective Data: Objective Data: Short Term: Independent: Short Term: Goal Partially MetCess YNo ratings yet
- NCP CVA ImmoblityDocument3 pagesNCP CVA ImmoblityAnalyn FloresNo ratings yet
- Nursing Care Plan Assesment Nursing Diagnosis Nursing Goal Nursing Intervention Rationale Actual EvaluationDocument4 pagesNursing Care Plan Assesment Nursing Diagnosis Nursing Goal Nursing Intervention Rationale Actual EvaluationFebee GeeNo ratings yet
- Assessment Explanation of The Problem Objectives Nursing Interventions Rationale EvaluationDocument5 pagesAssessment Explanation of The Problem Objectives Nursing Interventions Rationale EvaluationAlyssa NicoleNo ratings yet
- NURSING CARE PLAN (For Case Study)Document2 pagesNURSING CARE PLAN (For Case Study)Kathleen Martinez100% (1)
- NCP Ruth DeveraDocument8 pagesNCP Ruth DeveraBESA JERIC FLORESNo ratings yet
- Ate Gabs Nyo Pagod NaDocument3 pagesAte Gabs Nyo Pagod NaGabrielle EvangelistaNo ratings yet
- Collaborative Plan of Care For Urinary Tract InfectionsDocument2 pagesCollaborative Plan of Care For Urinary Tract InfectionsmysterioushumaneNo ratings yet
- Breaking the Itch-Scratch Cycle of Eczema by Behavior ModificationFrom EverandBreaking the Itch-Scratch Cycle of Eczema by Behavior ModificationNo ratings yet
- Digit BrochureDocument24 pagesDigit Brochureinsurance advisorNo ratings yet
- Inglés II - Examen Final Regular - Junio 2022pdfDocument6 pagesInglés II - Examen Final Regular - Junio 2022pdfIvan GregoriniNo ratings yet
- NCM118 TransesDocument11 pagesNCM118 TransesAlejandro Saclolo, IIINo ratings yet
- CASEDocument4 pagesCASEkateNo ratings yet
- Dandy WalkerDocument5 pagesDandy WalkerDiana Hazel Delos ReyesNo ratings yet
- Understanding Pathophysiology Canadian Edition Sue E Huether Ebook Full ChapterDocument34 pagesUnderstanding Pathophysiology Canadian Edition Sue E Huether Ebook Full Chapterirene.hart908100% (5)
- Colorectal CancerDocument3 pagesColorectal CancerFarah FarahNo ratings yet
- Nursing-Care-Plan 4Document4 pagesNursing-Care-Plan 4Christine CornagoNo ratings yet
- Hypertension Health ChallengeDocument19 pagesHypertension Health ChallengeElijah Tochukwu DavidNo ratings yet
- Endometrial BiopsyDocument9 pagesEndometrial BiopsyAnna BartolomeNo ratings yet
- 1women Behaving BadlyDocument5 pages1women Behaving BadlySimbarashe MarisaNo ratings yet
- Instructional DesignDocument4 pagesInstructional DesignSACHIDANANDA PRADHANNo ratings yet
- Carbidopa and Levodopa - Drug Information - UpToDateDocument29 pagesCarbidopa and Levodopa - Drug Information - UpToDatehochanh199xNo ratings yet
- Health FormDocument1 pageHealth Formnoera angel montemayorNo ratings yet
- Group 10Document12 pagesGroup 10Esdras DountioNo ratings yet
- Vulnus IctumDocument18 pagesVulnus IctumHardyanti DahlanNo ratings yet
- Incidence of Gallstone Disease and Complications (DANIEL MONSTED)Document9 pagesIncidence of Gallstone Disease and Complications (DANIEL MONSTED)abraham suarezNo ratings yet
- Diagnostic Dyspraxia and Apraxia in Nmda EncephalitisDocument2 pagesDiagnostic Dyspraxia and Apraxia in Nmda EncephalitisPriyanka SamalNo ratings yet
- Bone Marrow Edema: A Case of Regional Migratory OsteoporosisDocument13 pagesBone Marrow Edema: A Case of Regional Migratory OsteoporosisRobert Partarrieu StegmeierNo ratings yet
- DiphtheriaDocument15 pagesDiphtheriaelka.kgmaNo ratings yet
- School Form 8 SF8 Grade 6 2022-2023Document3 pagesSchool Form 8 SF8 Grade 6 2022-2023DORINA RODRIGUEZNo ratings yet
- Lecture 1 The Background of HIVDocument32 pagesLecture 1 The Background of HIVAPONDI SIMON ODONGONo ratings yet
- Preterm Labour (Prematurity) : DR - Abdulkarim Ahmed Mohamud MBCHB (Ust), Mmed (Uon)Document17 pagesPreterm Labour (Prematurity) : DR - Abdulkarim Ahmed Mohamud MBCHB (Ust), Mmed (Uon)PeterNo ratings yet
- Ebook Criminal Investigation 11Th Edition Hess Solutions Manual Full Chapter PDFDocument44 pagesEbook Criminal Investigation 11Th Edition Hess Solutions Manual Full Chapter PDFkhuongdiamond6h5100% (11)
- Mood Disorder and SuicideDocument58 pagesMood Disorder and SuicideMichael AsetreNo ratings yet
- EPI and HIV 1Document5 pagesEPI and HIV 1April Ivonne Claire BatoNo ratings yet
- Health Education ss2 3rd TermDocument4 pagesHealth Education ss2 3rd TermoloyedefisayoNo ratings yet
- Nurses A GuideTo Dermatology in Primary Care NHSDocument44 pagesNurses A GuideTo Dermatology in Primary Care NHSgaspe1999No ratings yet