Professional Documents
Culture Documents
Hsci Lesson 7
Uploaded by
Eyvette GoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hsci Lesson 7
Uploaded by
Eyvette GoCopyright:
Available Formats
HEALTH SCIENCE (HSCI) 1ST SEMESTER
LECTURE LESSON 7
HEMATOPOIESIS ➢ myeloid-to-erythroid ratio gradually approaches 3:1 to
4:1 (normal adult levels)
➢ The continuous, regulated process of renewal, ➢ By the end of 24 weeks gestation, the bone marrow
proliferation, differentiation, and maturation of all becomes the primary site of hematopoiesis
blood cell lines.
HEMATOPOIESIS
SITES OF HEMATOPOIESIS BY AGE
➢ In adults, hematopoietic tissue is located in the bone
marrow, lymph nodes, spleen, liver and thymus
➢ The bone marrow contains developing erythroid,
myeloid, megakaryocytic, and lymphoid cells.
➢ Lymphoid development occurs in both primary and
secondary lymphoid tissue
STEM CELL THEORY
➢ Originally there were two theories describing the
origin of the hematopoietic progenitor cells
▪ Monophyletic Theory – suggests that all blood
cells are derived from a single progenitor stem
cell called pluripotent hematopoietic stem cell
▪ Polyphyletic Theory – suggests that each of the
blood cell lineages is derived from its own unique
stem cell.
➢ The monophyletic theory is the most widely accepted
3 PHASES OF HEMATOPOIESIS theory among experimental hematologists
1) Mesoblastic Phase DIAGRAM OF HEMOTOPOIESIS
➢ Hematopoiesis is considered to begin around the
nineteenth day of embryonic development after
fertilization
➢ Early in embryonic development, cells from the
mesoderm migrate to the yolk sac
➢ These primitive but transient yolk sac erythroblasts
are important in early embryogenesis to produce
hemoglobin (Gower-1, Gower-2, and Portland)
needed for delivery of oxygen to rapidly developing
embryonic tissues
➢ Yolk sac hematopoiesis differs from hematopoiesis
that occurs later in the fetus and adult in that it occurs
intravascularly (within developing blood vessels)
2) Hepatic Phase
➢ Begin at 5 to 7 gestational weeks and is characterized
by recognizable clusters of developing erythroblasts,
granulocytes, and monocytes colonizing the fetal liver,
thymus, spleen, placenta, and ultimately the bone
marrow space in the final medullary phase
➢ Hematopoiesis during this phase occurs extra
vascularly, with the liver remaining the major site of
hematopoiesis during the second trimester of fetal life
➢ The thymus, the first fully developed organ in the
fetus, becomes the major site of T cell production, ERYTHROPOIESIS
whereas the kidney and spleen produce B cells
➢ Occurs in the bone marrow and is complex, regulated
3) Medullary (Myeloid) Phase process for maintaining adequate numbers of
erythrocytes in the peripheral blood
➢ Begin between the fourth and fifth month of fetal ➢ Erythroid Progenitors
development ▪ Burst forming unit – Erythroid (BFU-E)
➢ Hematopoietic activity, especially myeloid activity, is ▪ Colony forming unit – Erythroid (CFU-E)
apparent during this stage of development, and the
➢ Erythroid Precursors
▪ The earliest morphologically recognizable
erythrocyte precursor, the pronormoblast
➢ Criteria used in identification of Erythroid Precursors
▪ Overall diameter of the cell decreases
▪ Diameter of the nucleus decreases more rapidly
than does the diameter of the cell
▪ Nuclear chromatin pattern becomes coarser,
clumped, and condensed
▪ Nucleoli disappear
▪ Cytoplasm changes from the gray-blue to salmon
pink
PRONORMOBLAST (Proerythroblast)
➢ First microscopically recognizable precursor cell in
erythropoiesis
➢ NUCLEUS: is round and oval, containing one or 2
nucleoli. The purples red chromatin is open and
contains few, if any fine clumps
➢ CYTOPLASM: Basophilic
➢ NC Ratio: High (8:1)
➢ Forms two basophilic normoblast after mitosis
➢ The pronormoblast is present only in the bone marrow
in healthy states
BASOPHILIC NORMOBLAST (Basophilic Erythroblast)
A. Diameter decreases and cytoplasm changes from ➢ NUCLEUS: the chromatin begins to condense,
blue to salmon pink revealing clumps along the periphery of the nuclear
B. Nuclear diameter decreases and color changes from membrane and a few in the interior
purplish-red to a very dark purple-blue ➢ CYTOPLASM: deeply basophilic. The cytoplasm is
C. Nuclear chromatin becomes coarser, clumped, and dark blue because of the concentration of ribosomes
condensed and RNA
D. Composite of changes during the developmental ➢ NC Ratio: Moderate (6:1)
process ➢ Undergoes mitosis, giving rise to two daughter cells
➢ Is present only in the bone marrow in healthy states
RED BLOOD CELL ➢ Detectable hemoglobin synthesis occurs
➢ Major Function: Carry Oxygen from the lung to the POLYCHROMATIC (Polychromatophilic) NORMOBLAST
tissues (Polychromatic Erythroblast)
▪ Attachment of oxygen to hemoglobin, the major
cytoplasmic component of mature RBCs ➢ NUCLEUS: The condensation of chromatin reduces
➢ Acid base buffer the diameter of the nucleus considerably
➢ Biconcave in shape ➢ CYTOPLASM: This is the first stage in which the pink
➢ Distensible color associated with stained hemoglobin can be seen
➢ NC RATIO: Moderate
Three Erythroid Precursor Nomenclature Systems ➢ Last stage which contains a nucleus
➢ Last stage capable of mitosis
Normoblastic Rubriblastic Erythroblastic
Pronormoblast Rubriblast Proerythroblast ORTHOCHROMATIC NORMOBLAST (Metarubricyte)
Basophilic Prorubricyte Basophilic
Normoblast erythroblast ➢ NUCLEUS: is completely condensed (i.e., pyknotic) or
Polychromatic Rubricyte Polychromatic nearly so
(polychromatophili (polychromatophili ➢ CYTOPLASM: pink gray (more pinkish)
c) Normoblast c) Erythroblast ▪ The increase in the salmon pink color of the
Orthochromic Metarubricyte Orthochromic cytoplasm reflects nearly complete hemoglobin
Normoblast Erythroblast production
Polychromatic Polychromatic Polychromatic ➢ NC Ratio: Low
(polychromatophili (polychromatophili (polychromatophili ➢ No longer capable of division
c) Erythrocyte c) Erythrocyte c) Erythrocyte
Erythrocyte Erythrocyte Erythrocyte POLYCHROMATIC ERYTHROCYTE (Reticulocyte)
➢ First anucleated precursor
➢ RNA synthesis stops while heme synthesis continues
➢ Loses its RNA and mitochondria
➢ NUCLEUS: none MARROW. There are two significant pathways to
➢ CYTOPLASM: Pink gray generate various types of leukocytes:
▪ By the end of the polychromatic erythrocyte ➢ MYELOPOIESIS, in which leukocytes in the blood are
stage, the cell is the same color as a mature derived from MYELOID STEM CELLS, and
RBC, salmon pink. It remains larger than a ➢ LYMPHOPOIESIS, in which leukocytes of the
mature cell, however. lymphatic system (LYMPHOCYTES) are generated
➢ Resides in the bone marrow for about 1 to 2 days and from lymphoid stem cells.
then moves into the peripheral blood for about 1 day ➢ Factors that promote differentiation of the CFU-GEM
before reaching maturity. into neutrophils, monocytes, eosinophils, and
basophils include GM-CSF, G- CSF, macrophage
ERYTHROCYTES colony-stimulating factor (M-CSF), IL3, IL5, IL11, and
KIT ligand.
➢ Life span: 120 days
➢ No nucleus, mitochondria, or endoplasmic reticulum NEUTROPHIL DEVELOPMENT
➢ The mature circulating erythrocyte is a biconcave disc
measuring 7 to 8 "m in diameter, with thickness of ➢ Neutrophil development occurs in the bone marrow,
about 1.5 to 2.5 "m. neutrophils share a common progenitor with
➢ On a Wright-stained blood film, it appears as a monocytes and distinct from eosinophils and
salmon-pink stained cell with a central pale area that basophils, known as the granulocyte monocyte
corresponds to the concavity. The central pallor is progenitor (GMP). The major cytokine responsible for
about one-third the diameter of the cell. the stimulation of neutrophil production is granulocyte
➢ Contains Cytoplasmic enzymes capable of colony stimulating factor, or G-CSF.
metabolizing glucose ➢ There are three pools of developing neutrophils in the
bone marrow:
ERYTHROKINETICS ▪ The stem cell pool:
o Consists of HSCs that are capable of self-
➢ Is the term describing the dynamics of RBC
renewal and differentiation
production and destruction
▪ The proliferation pool
➢ If tissue oxygen is inadequate, RBC production and
o Consists of cells that are dividing and
the functional efficiency of existing cells must be
includes common myeloid progenitors
enhanced
(CMPs), CFUGEMMs, and Granulocyte-
➢ The primary oxygen-sensing system of the body is
monocyte progenitors
located in peritubular and fibroblasts of the kidney
▪ The maturation pool
➢ Hypoxia, too little tissue oxygen is detected by the
o Consisting of cells undergoing nuclear
peritubular fibroblasts, which then produce
maturation that form the marrow reserve and
erythropoietin (EPO), the major stimulatory cytokine
available for release: metamyelocytes, band
for RBC
neutrophils, and segmented neutrophils.
➢ It is well documented that testosterone directly
stimulates erythropoiesis, which partially explains the MYELOBLAST
higher hemoglobin concentration in men than in
women ➢ Myeloblasts make up 0% to 3% of the nucleated cells
and the bone marrow and measure 14 to 20 " m in
ERYTHROPOIETIN diameter. They are often subdivided into type I, type
II, and type III myeloblasts
➢ EPO is a thermostable, nondialyzable, glycoprotein
➢ First recognizable cell that begin the process of
hormone with a molecular weight of 34 kD.
granulopoiesis
➢ EPO is a true hormone, being produced at one
➢ Earliest microscopically recognizable neutrophil
location (kidney) and acting at a distant location (bone
precursor cell in the bone marrow
marrow).
➢ Large euchromatic spherical nucleus with three to five
➢ It is a growth factor (or cytokine) that initiates an
nucleoli
intracellular message to the developing erythroid
➢ Large nuclear to cytoplasmic volume
cells; this process is called signal transduction
➢ The small amount of agranular cytoplasm stains
➢ EPO had three major effects:
intensely basophilic
▪ Allowing early release of reticulocytes from the
bone marrow PROMYELOCYTE
▪ Preventing apoptotic cell death
▪ Reducing the time needed for cells to mature in ➢ Comprise of 1% to 5% of the nucleated cells in the
the bone marrow bone marrow.
➢ They are relatively larger than the myeloblast cells
WBC PRODUCTION and measure 16 to 25" m in diameter.
➢ The nucleus is round to oval and is often eccentric
LEUKOPOIESIS
➢ Only cells to produce azurophilic granules
➢ The process of generating white blood cells ➢ Azurophilic (primary) granules in the cytoplasm
(LEUKOCYTES) from the pluripotent
HEMATOPOIESIS STEM CELLS of the BONE
MYELOCYTES oxidants and
release cationic
➢ First that exhibit specific granules proteins
➢ Last stage capable of Mitosis Move in a zigzag Granules contain
➢ Recognition of the neutrophil, eosinophil, and basophil pattern in the major basic
lines is possible presence of protein
▪ NEUTROPHIL: patches of grainy pale pink chemoattractant
cytoplasm representing secondary granules Phagocytose a
begin to be evident in the area of the Golgi foreign particle
Apparatus. This has been referred to as the dawn Bactericidal
of neutrophilia activity mediated
▪ EOSINOPHIL: characterized by the presence of by H2O2
superoxide anion,
large, pale, reddish orange, secondary granules,
myeloperoxidase,
along with azure granules in blue cytoplasm. The
and free halogen
nucleus is similar to that described for neutrophil Important in the
myelocytes defense against
infectious agents
METAMYELOCYTE
Can cause tissue
➢ constitute 3% to 20% of nucleated marrow cells necrosis, tissue
➢ From this stage forward, the cells are no longer injury, and
inflammation
capable of division and the major morphologic change
is in the shape of the nucleus
➢ The nucleus is intended (kidney bean shaped or MONOCYTES
peanut shaped), and the chromatin is increasingly
➢ Appear to be larger than neutrophils (diameter of 15
clumped. Nucleoli are absent
to 20" m) because they tend to stick to and spread out
➢ Synthesis of tertiary granules (also known as
on glass or plastic
gelatinase granules) may begin during this stage
➢ Are slightly immature cells whole ultimate goal is to
➢ The size of the metamyelocyte is slightly smaller than
enter the tissues and mature into macrophages,
that of the myelocyte (14 to 16" m)
osteoclasts, or dendritic cells
➢ The cytoplasm contains very little residual ribonucleic
➢ The nucleus may be round, oval, or kidney shaped
acid (RNA) and therefore little to no basophilia
but more often is deeply indented (horseshoe shaped)
BAND (STAB) CELL or folded on itself
➢ The chromatin pattern is looser than in the other
➢ bands make up 9% to 32% of nucleated marrow cells leukocytes and has sometimes been described as
and 0% to 5% of the nucleated peripheral blood cells lace-like or stringy
➢ All evidence of RNA (cytoplasmic basophilia) is ➢ Their cytoplasm is blue-grey, with fine azure granules
absent, and tertiary granules continue to be formed often referred to as azure dust or a ground-glass
during this stage appearance
➢ Secretory granules (Secretory Vesicles) may begin to ➢ Monocytes remain in the circulation approximately 3
be formed during this stage days. Monocytes with different patterns of chemokine
➢ The nucleus is highly clumped, and the nuclear receptors have different target tissues and different
indentation that began in the metamyelocyte stage functions
now exceeds one half of the diameter of the nucleus, ➢ Mononuclear phagocyte system (reticuloendothelial
but actual segmentation has not yet occurred system)
➢ Defense against microorganism including
MATURE GRANULOCYTE mycobacteria, fungi, bacteria, protozoa, and viruses
➢ Called histocytes or macrophage when migrates to
➢ Segmented Neutrophils - make up 7% to 30% of
the tissue
nucleated cells in the bone marrow. Secretory
granules continue to be formed during this stage. The DIFFERENTIATION INTO MACROPHAGES
only morphologic difference between segmented In areas of inflammation or infection (inflammatory
neutrophils and bands is the presence of between two macrophages)
and five nuclear lobes connected by thread-like As "resident" macrophages in:
filaments ➢ Liver (Kupffer Cells)
➢ Mature Eosinophils - usually display a bilobed ➢ Lungs (Alveolar Macrophages)
nucleus. Their cytoplasm contains characteristic ➢ Brain (Microglia)
refractile, orange-red secondary granules ➢ Skin (Langerhans Cells)
➢ Spleen (Splenic Macrophages)
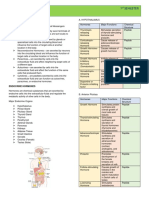
NEUTROPHILS EOSINOPHILS BASOPHILS ➢ Intestines (Intestinal Macrophages)
Phagocytosis Modulate Immediate ➢ Peritoneum (Peritoneal Macrophages)
Inflammatory Hypersensitivity ➢ Bone (Osteoclasts)
Response Reactions ➢ Synovial Macrophages (Type A Cells)
Bacterial Activity Anthelmintic ➢ Kidneys (Renal Macrophages)
activity - ➢ Reproductive Organ Macrophages
generating ➢ Lymph Nodes (Dendritic Cells)
LYMPHOCYTES ➢ Megakaryocyte progenitors arise from the common
myeloid progenitor under the influence of the
➢ Lymphocytes are divided into three major groups: T transcription gene product, GATA-1, regulated by
Cells, B Cells, and Natural Killer (NK) Cells cofactor FOG1
▪ T and B Cells are major players in adaptive ➢ Megakaryocyte differentiation is suppressed by
immunity another transcription gene product, MYB, so GATA-1
▪ NK Cells make up small percentage of act in opposition to balance megacaryocytopoiesis
lymphocytes and are part of innate immunity ➢ Three megakaryocyte lineage-committed progenitor
➢ Lymphocytes can be subdivided into two major stages, defined by their in vitro culture colony
categories: Those that participate in humoral immunity characteristics, arise from the common myeloid
by producing antibodies and those that participate in progenitor
cellular immunity by attacking foreign organisms or ➢ In order of differentiation these are:
cells directly ▪ The least mature burst-forming unit (BFU-Meg)
➢ Antibody producing lymphocytes are called B ▪ The intermediate colony forming unit (CFU-Meg)
lymphocytes or simply B cells because they develop ▪ The more mature progenitor, the light-density
in the bone marrow CFU (LD-CFU-Meg)
➢ Cellular immunity is accomplished by two types of ▪ All three progenitor stages resemble lymphocytes
lymphocytes: T cells, so named because they develop and cannot be distinguished by Writghtstained
in the thymus, and NK cells, which develop in both the light microscopy
bone marrow and the thymus
➢ NK lymphocytes function as part of innate immunity
and are capable of killing certain tumor cells and
virus-infected cells without prior sensitization
➢ In addition, NK cells modulate the functions of other
cells, including macrophages and T cells
➢ Lymphocytes are different from the other leukocytes
in several ways, including the following:
▪ Lymphocytes are not end cells. They are resting
cells, and when stimulated, they undergo mitosis
to produce both memory and effector cells
▪ Unlike other leukocytes, lymphocytes recirculate
from the blood to the tissues and back to the
blood
▪ B and T lymphocytes are capable of rearranging
antigen receptor gene segments to produce a
wide variety of antibodies and surface receptors
▪ Although early lymphocyte progenitors such as
the common lymphoid progenitor originate in the
bone marrow, T and NK lymphocytes develop THROMBOCYTOPOIESIS (Platelet Shedding)
and mature outside the bone marrow
➢ Illustrate the process of platelet Shedding, termed
T CELLS B CELLS thrombocytopoiesis. During thrombocytopoiesis a
➢ Cells mediated ➢ Humoral Immunity single megakaryocyte may shed 2000 to 4000
immunity ➢ Plasma cells and platelets
➢ Delayed Produce antibodies ➢ The total platelet population turns over in 8 to 9 days
hypersensitivity ➢ Minor populations (the so-called platelet life span)
➢ Graft rejection (10-20% of
➢ Graft vs Host lymphocytes)
Disease ➢ Short life span
➢ Defense against
intracellular
organisms (tubercle
bacilli & brucella)
➢ Life Span: Months
to Years
MEGAKARYOPOIESIS
➢ is the process by which megakaryocytes and
ultimately platelets develop
➢ Earlier influences include GM-CSF, IL-6, IL-11, KIT
ligand, and TPO. The stimulating hormonal factor
TPO (also known as MPL ligand), along with IL-11,
controls the production and release of platelets. The
liver is the main site of production of TPO.
You might also like
- Salads: 300 Salad Recipes For Rapid Weight Loss & Clean Eating (PDFDrive) PDFDocument1,092 pagesSalads: 300 Salad Recipes For Rapid Weight Loss & Clean Eating (PDFDrive) PDFDebora PanzarellaNo ratings yet
- !perdev Notes!Document33 pages!perdev Notes!Eyvette GoNo ratings yet
- Types:: Precursor CellsDocument4 pagesTypes:: Precursor CellsGrace UrbanoNo ratings yet
- ErythropoiesisDocument51 pagesErythropoiesisKevin Leo100% (1)
- Oracle - Prep4sure.1z0 068.v2016!07!12.by - Lana.60qDocument49 pagesOracle - Prep4sure.1z0 068.v2016!07!12.by - Lana.60qLuis AlfredoNo ratings yet
- Hematopoiesis PDFDocument10 pagesHematopoiesis PDFJezzah Mae CañeteNo ratings yet
- H E M A T O P O I E S I S (Rodaks, Turgeon, and PPT) 11Document4 pagesH E M A T O P O I E S I S (Rodaks, Turgeon, and PPT) 11Kristin SoquilloNo ratings yet
- Human Chromosomes: An Illustrated Introduction to Human CytogeneticsFrom EverandHuman Chromosomes: An Illustrated Introduction to Human CytogeneticsRating: 5 out of 5 stars5/5 (1)
- !literature Notes!Document16 pages!literature Notes!Eyvette Go100% (1)
- Project ManagementDocument11 pagesProject ManagementBonaventure NzeyimanaNo ratings yet
- Hematopoiesis Reading NotesDocument7 pagesHematopoiesis Reading NotesMemeowwNo ratings yet
- WebLMT HelpDocument12 pagesWebLMT HelpJoão LopesNo ratings yet
- Shostack ModSec08 Experiences Threat Modeling at MicrosoftDocument11 pagesShostack ModSec08 Experiences Threat Modeling at MicrosoftwolfenicNo ratings yet
- Erythropoiesis 150731072608 Lva1 App6891Document51 pagesErythropoiesis 150731072608 Lva1 App6891shinigami07700254100% (1)
- Jesus Prayer-JoinerDocument13 pagesJesus Prayer-Joinersleepknot_maggotNo ratings yet
- HematologyDocument23 pagesHematologyWynlor AbarcaNo ratings yet
- CHAPTER 2 HematopoiesisDocument7 pagesCHAPTER 2 HematopoiesisAMELIA DALE MARQUEZNo ratings yet
- German Atv-Dvwk Rules and StandardsDocument25 pagesGerman Atv-Dvwk Rules and StandardsMehmet Emre Bastopcu100% (1)
- Hematology Trans - Module 3 & 4 - Hematopoiesis and Lineage Specific HematopoiesisDocument6 pagesHematology Trans - Module 3 & 4 - Hematopoiesis and Lineage Specific HematopoiesisFaye Kyla Heart ResuelloNo ratings yet
- Human Histology Midterms: Blood and HemopoesisDocument3 pagesHuman Histology Midterms: Blood and Hemopoesisabi dimatulacNo ratings yet
- MT1 HSCI LEC L7 HematopoiesisDocument10 pagesMT1 HSCI LEC L7 HematopoiesisSEBASTIEN ANDREI BUENAFENo ratings yet
- Hema 1A Lec 1 Shift Reviewer Hematopoiesis Prepared By: C Hematopoiesis DefinedDocument7 pagesHema 1A Lec 1 Shift Reviewer Hematopoiesis Prepared By: C Hematopoiesis DefinedMarc ViduyaNo ratings yet
- Module 2 CANVAS NOTES HematopoiesisDocument6 pagesModule 2 CANVAS NOTES HematopoiesisMohammad MasacalNo ratings yet
- 3 HEMA HematopoiesisDocument9 pages3 HEMA HematopoiesisJohanna Rose Cobacha SalvediaNo ratings yet
- Module 2 PPT NOTES HematopoiesisDocument8 pagesModule 2 PPT NOTES HematopoiesisMohammad MasacalNo ratings yet
- Molbog Villangca Hema 1A Compre Reviewer 2Document53 pagesMolbog Villangca Hema 1A Compre Reviewer 2Camella Beatrice Lujan ValleNo ratings yet
- Hematology 1 L2 Hematopoiesis LectureDocument4 pagesHematology 1 L2 Hematopoiesis LectureChelze Faith DizonNo ratings yet
- HEMATOPOESISDocument71 pagesHEMATOPOESISHussenNo ratings yet
- Hematology & Blood Bank TechniqueDocument125 pagesHematology & Blood Bank Techniquemandawa786No ratings yet
- Week 1 - HEMATOPOIESISDocument8 pagesWeek 1 - HEMATOPOIESISAcel Jone CayotNo ratings yet
- Hema Report PDFDocument25 pagesHema Report PDFdaliaNo ratings yet
- Hematopoiesis Part 1 Hema LecDocument4 pagesHematopoiesis Part 1 Hema LecAngela ReyesNo ratings yet
- Hematopoiesis ErythropoiesisDocument8 pagesHematopoiesis ErythropoiesisASHLEY ALEXIS GUEVARRANo ratings yet
- Hematopoiesis (HEMA)Document12 pagesHematopoiesis (HEMA)April Lady Faith P. PaundogNo ratings yet
- Hematology Module 2 and 3Document11 pagesHematology Module 2 and 3SEAN MELNOR LOSBAÑESNo ratings yet
- Micro - Male Repro (Sec A) PDFDocument5 pagesMicro - Male Repro (Sec A) PDFKaren ValdezNo ratings yet
- Dr. Waluyo Rudiyanto, M.KesDocument50 pagesDr. Waluyo Rudiyanto, M.KesAsiatiNo ratings yet
- Topic 1Document21 pagesTopic 1Ria AccadNo ratings yet
- Ha Ema To PoiesisDocument38 pagesHa Ema To PoiesisEmma Joel OtaiNo ratings yet
- Module 01 HematopeisisDocument15 pagesModule 01 HematopeisisKoarie Frae ZuleNo ratings yet
- MCN Lec M1L3B ReviewerDocument6 pagesMCN Lec M1L3B ReviewerEmily BernatNo ratings yet
- ANAT0001 Introduction To Developmental BiologyDocument6 pagesANAT0001 Introduction To Developmental BiologyOmed ZarifiNo ratings yet
- Heamtopoises ReviewerDocument17 pagesHeamtopoises ReviewerClyde BaltazarNo ratings yet
- EMBRYOLOGY Part1Document90 pagesEMBRYOLOGY Part1Daly DaliaNo ratings yet
- Primary and Secondary Lymphoid Organs - Aditi SinghDocument50 pagesPrimary and Secondary Lymphoid Organs - Aditi SinghEunice PalloganNo ratings yet
- Erythropoiesis and ErythropoietinDocument29 pagesErythropoiesis and ErythropoietinmaduksjaycryptoNo ratings yet
- Human Development TransesDocument5 pagesHuman Development TransesReign SaplacoNo ratings yet
- CLINPATH-01.Hematopoiesis & Morphology of Blood CellsDocument10 pagesCLINPATH-01.Hematopoiesis & Morphology of Blood CellsCharisse Angelica MacedaNo ratings yet
- Haematology: Red Blood Cells DisordersDocument47 pagesHaematology: Red Blood Cells Disordersbv2328002No ratings yet
- Hematopoeitic System: Alya Amila Fitrie Lokot Donna LubisDocument80 pagesHematopoeitic System: Alya Amila Fitrie Lokot Donna LubisrubyniNo ratings yet
- Hematopoeitic System& Blood, KBK 2015 LDLDocument80 pagesHematopoeitic System& Blood, KBK 2015 LDLgita dwi ananda100% (1)
- Ch13 Hematopoiesis: Prepared and Presented byDocument47 pagesCh13 Hematopoiesis: Prepared and Presented bymmmmmmmmmmNo ratings yet
- Conceptos Clave en HematologíaDocument15 pagesConceptos Clave en HematologíaChristian GarciaNo ratings yet
- Lec 5 Hematology ErythropoiesisDocument16 pagesLec 5 Hematology ErythropoiesisROOA OmarNo ratings yet
- Erythropoiesis: Presented by DR Etu-Efeotor T. PDocument88 pagesErythropoiesis: Presented by DR Etu-Efeotor T. PPrincewill SeiyefaNo ratings yet
- He Ma To PoiesisDocument64 pagesHe Ma To Poiesismatthew deguzman100% (1)
- CL1 HaemopoiesisDocument41 pagesCL1 HaemopoiesisSamuel George100% (1)
- Leukocyte's Classification, Structure, Function, and AssessmentDocument32 pagesLeukocyte's Classification, Structure, Function, and Assessmenthayamitib11No ratings yet
- Cell DivisionDocument10 pagesCell DivisionGale SatsatinNo ratings yet
- Parasitology (Lect #5) TransDocument3 pagesParasitology (Lect #5) TransSherlyn Giban InditaNo ratings yet
- LECTURE 2 - HEMATOPOIESIS and ERYTHROPOIESIS - 10 - 17 - 2020Document49 pagesLECTURE 2 - HEMATOPOIESIS and ERYTHROPOIESIS - 10 - 17 - 2020apoorva krishnagiriNo ratings yet
- CYTODocument21 pagesCYTOANGELICA ROMAWAKNo ratings yet
- Composition of Blood and Normal Erythropoiesis: NotesDocument8 pagesComposition of Blood and Normal Erythropoiesis: NotesSelmaNo ratings yet
- TRANS PPT TOPIC MegakaryopoeisisDocument5 pagesTRANS PPT TOPIC MegakaryopoeisisPaul LesterNo ratings yet
- ZON HematopoyesisDocument16 pagesZON HematopoyesisMariana CabagnaNo ratings yet
- Hema TransesDocument25 pagesHema TransesNikoh Anthony EwayanNo ratings yet
- BSC Lecture Notes Semester 1Document7 pagesBSC Lecture Notes Semester 1satasha28No ratings yet
- HEMATOPOIESISDocument24 pagesHEMATOPOIESISJustin Louie EstradaNo ratings yet
- Chem Lab NotesDocument5 pagesChem Lab NotesEyvette GoNo ratings yet
- Expt 2Document26 pagesExpt 2Eyvette GoNo ratings yet
- Expt 1 To 4 Lab ReportDocument4 pagesExpt 1 To 4 Lab ReportEyvette GoNo ratings yet
- !research Notes!Document7 pages!research Notes!Eyvette GoNo ratings yet
- BIOLAB Exp 1 To 15 MergedDocument62 pagesBIOLAB Exp 1 To 15 MergedEyvette Go0% (1)
- !gen Physics Notes!Document11 pages!gen Physics Notes!Eyvette GoNo ratings yet
- !DR3 Notes!Document13 pages!DR3 Notes!Eyvette GoNo ratings yet
- !gen Bio Notes!Document14 pages!gen Bio Notes!Eyvette GoNo ratings yet
- !peh Notes!Document5 pages!peh Notes!Eyvette GoNo ratings yet
- PC NotesDocument4 pagesPC NotesEyvette GoNo ratings yet
- Hsci Lesson 2Document10 pagesHsci Lesson 2Eyvette GoNo ratings yet
- Hsci Lesson 4Document8 pagesHsci Lesson 4Eyvette GoNo ratings yet
- Hsci Lesson 8 (Print 2)Document11 pagesHsci Lesson 8 (Print 2)Eyvette GoNo ratings yet
- Hsci Lesson 5Document9 pagesHsci Lesson 5Eyvette GoNo ratings yet
- Hsci Lesson 3Document4 pagesHsci Lesson 3Eyvette GoNo ratings yet
- Report Card Grade 1 2Document3 pagesReport Card Grade 1 2Mely DelacruzNo ratings yet
- PR KehumasanDocument14 pagesPR KehumasanImamNo ratings yet
- Science7 - q1 - Mod3 - Distinguishing Mixtures From Substances - v5Document25 pagesScience7 - q1 - Mod3 - Distinguishing Mixtures From Substances - v5Bella BalendresNo ratings yet
- DP 2 Human IngenuityDocument8 pagesDP 2 Human Ingenuityamacodoudiouf02No ratings yet
- RSA - Brand - Guidelines - 2019 2Document79 pagesRSA - Brand - Guidelines - 2019 2Gigi's DelightNo ratings yet
- Read While Being Blind.. Braille's Alphabet: Be Aware and Active !Document3 pagesRead While Being Blind.. Braille's Alphabet: Be Aware and Active !bitermanNo ratings yet
- 18 June 2020 12:03: New Section 1 Page 1Document4 pages18 June 2020 12:03: New Section 1 Page 1KarthikNayakaNo ratings yet
- The Indonesia National Clean Development Mechanism Strategy StudyDocument223 pagesThe Indonesia National Clean Development Mechanism Strategy StudyGedeBudiSuprayogaNo ratings yet
- Impact of Advertising On Consumers' Buying Behavior Through Persuasiveness, Brand Image, and Celebrity EndorsementDocument10 pagesImpact of Advertising On Consumers' Buying Behavior Through Persuasiveness, Brand Image, and Celebrity Endorsementvikram singhNo ratings yet
- Monkey Says, Monkey Does Security andDocument11 pagesMonkey Says, Monkey Does Security andNudeNo ratings yet
- Chapter 1 To 5 For Printing.2Document86 pagesChapter 1 To 5 For Printing.2Senku ishigamiNo ratings yet
- Deal Report Feb 14 - Apr 14Document26 pagesDeal Report Feb 14 - Apr 14BonviNo ratings yet
- PyhookDocument23 pagesPyhooktuan tuanNo ratings yet
- Working Capital in YamahaDocument64 pagesWorking Capital in YamahaRenu Jindal50% (2)
- .Urp 203 Note 2022 - 1642405559000Document6 pages.Urp 203 Note 2022 - 1642405559000Farouk SalehNo ratings yet
- Gods Omnipresence in The World On Possible MeaninDocument20 pagesGods Omnipresence in The World On Possible MeaninJoan Amanci Casas MuñozNo ratings yet
- ME Eng 8 Q1 0101 - SG - African History and LiteratureDocument13 pagesME Eng 8 Q1 0101 - SG - African History and Literaturerosary bersanoNo ratings yet
- Test ScienceDocument2 pagesTest Sciencejam syNo ratings yet
- Spesifikasi PM710Document73 pagesSpesifikasi PM710Phan'iphan'No ratings yet
- De Thi Hoc Ki 1 Mon Tieng Anh Lop 5 Co File NgheDocument10 pagesDe Thi Hoc Ki 1 Mon Tieng Anh Lop 5 Co File Nghetuyen truongNo ratings yet
- 2SB817 - 2SD1047 PDFDocument4 pages2SB817 - 2SD1047 PDFisaiasvaNo ratings yet
- Appendix - Pcmc2Document8 pagesAppendix - Pcmc2Siva PNo ratings yet
- 5c3f1a8b262ec7a Ek PDFDocument5 pages5c3f1a8b262ec7a Ek PDFIsmet HizyoluNo ratings yet