Professional Documents
Culture Documents
Aspirin For Primary Prevention of Atherosclerotic Cardiovascular Disease 2016
Uploaded by
Luis Alberto Alvarez AnkassOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Aspirin For Primary Prevention of Atherosclerotic Cardiovascular Disease 2016
Uploaded by
Luis Alberto Alvarez AnkassCopyright:
Available Formats
Clinical Review & Education
Review
Aspirin for Primary Prevention of Atherosclerotic
Cardiovascular Disease
Advances in Diagnosis and Treatment
Samia Mora, MD, MHS; JoAnn E. Manson, MD, DrPH
IMPORTANCE Clinical decision making regarding the appropriate use of aspirin for the primary
prevention of atherosclerotic cardiovascular disease (ASCVD) events is complex, and requires
an individualized benefit to risk assessment.
OBJECTIVE To review advances in the individualized assessment for ASCVD and bleeding risk,
and to provide an update of the randomized clinical trial evidence that examined the use of
aspirin for primary prevention (primarily for ASCVD, and secondarily for colorectal cancer).
The recently released 2016 US Preventive Services Task Force recommendations are
discussed, as well as the role of ASCVD risk, age, sex, and aspirin dose/formulation in clinical
decision making.
EVIDENCE REVIEW We performed a detailed review of peer-reviewed publications that were
identified through searches of MEDLINE and the Cochrane Database through 2016 using the
literature search terms “aspirin,” “primary prevention,” “cardiovascular disease,” “mortality,”
“cancer.” Bibliographies from these references as well as meta-analyses of these randomized
clinical trials were also reviewed.
FINDINGS Evidence from a total of 11 trials involving more than 118 000 patients is available
to guide clinical decision making for aspirin use in the primary prevention of ASCVD. Clinicians
should balance the benefit to risk ratio and the individual’s preferences, calculating the
10-year ASCVD risk and evaluating risk factors for gastrointestinal bleeding, to facilitate a
safer and more personalized approach to appropriate selection of candidates for low-dose
aspirin (75 to 81 mg/d) for the primary prevention of ASCVD, with secondary considerations
for reducing colorectal cancer risk when taken for longer periods (>10 years). Both the net
ASCVD benefit and the bleeding risk of aspirin therapy increased as the absolute ASCVD risk
increased, but the net benefits generally exceeded the risks at higher baseline ASCVD risk
(!10% ASCVD 10-year risk). The Aspirin-Guide is a clinical decision making support tool (app
for mobile devices) with internal risk calculators to help clinicians with this dual assessment
by calculating the ASCVD risk and the bleeding risk in the individual patient, and
incorporating age- and sex-specific guidance based on randomized trial results.
Author Affiliations: Division of
CONCLUSIONS AND RELEVANCE Balancing the benefit of ASCVD reduction with the risk of Preventive Medicine, Department of
bleeding from low-dose aspirin is difficult but essential for informed decision making and Medicine, Brigham and Women’s
Hospital and Harvard Medical School,
achieving a net clinical benefit from aspirin for primary prevention. This is facilitated by a free
Boston, Massachusetts (Mora,
and readily-available evidence-based clinical decision support tool. Manson); Cardiovascular Division,
Department of Medicine, Brigham
and Women’s Hospital and Harvard
Medical School, Boston,
Massachusetts (Mora); Department
of Epidemiology, Harvard T. H. Chan
School of Public Health, Boston,
Massachusetts (Manson).
Corresponding Author: Samia Mora,
MD, MHS, Center for Lipid
Metabolomics, Brigham and
Women’s Hospital,
Harvard Medical School,
900 Commonwealth Ave E,
JAMA Intern Med. doi:10.1001/jamainternmed.2016.2648 Boston, MA 02215
Published online June 20, 2016. (smora@partners.org).
(Reprinted) E1
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://archinte.jamanetwork.com/ by a La Trobe University User on 06/20/2016
Clinical Review & Education Review Aspirin for Primary Prevention of Atherosclerotic Cardiovascular Disease
C
ardiovascular death remains the leading cause of death in
the United States, for both women and men.1 Over the past Key Points
decades, death rates from cardiovascular disease (which in- Question Which patients should be prescribed aspirin for the
clude coronary heart disease and stroke) have declined in US men, primary prevention of atherosclerotic cardiovascular disease?
and more recently over the past decade in US women.1,2 Approxi-
Findings In this review of advances in cardiovascular and bleeding
mately half of the decline in cardiovascular death rates may be ac-
risk assessment and the randomized clinical trial results for aspirin
counted for by improvements in cardiovascular risk factors, includ- in primary prevention, the net cardiovascular benefit and the
ing smoking cessation and lower rates of untreated cholesterol and bleeding events increased as the absolute cardiovascular risk
blood pressure, while the other half may be accounted for by evi- increased, but the benefits exceeded the risks among individuals
dence-based therapies including aspirin, other antiplatelet medica- with higher cardiovascular risk (approximate 10-year risk !10%).
tions, statins, and antihypertensives, among other advances.3 The Aspirin-Guide is a clinical decision making support tool (app
for mobile devices ) with internal risk calculators to help clinicians
The use of aspirin in medicine dates as far back as 3500 years
with this dual assessment, and incorporates age- and sex-specific
ago, when Assyrian and Egyptian physicians reported (on stone and
guidance based on randomized clinical trial results and secondary
papyrus, respectively) on the analgesic and antiinflammatory ef- considerations for colorectal cancer prevention.
fects of the extract (salicin) of willow leaves.4-6 Aspirin remains one
Meaning For the primary prevention of cardiovascular disease,
of the most widely used medications. Currently, approximately 40%
decisions regarding aspirin use should be individualized, balancing
of US adults older than 50 years use aspirin for the prevention of car-
the benefit to risk ratio. This can be facilitated by a free and
diovascular diseases.7-9 Aspirin irreversibly and nonselectively in- readily-available evidence-based clinical decision support tool.
activates cyclooxygenase (COX), inhibiting both COX-1 and COX-2
enzymes.10 At the doses used for prevention of cardiovascular dis-
eases, aspirin’s effect on COX-1 predominates,11 preventing plate- “mortality,” “cancer,” “clinical trials.” Bibliographies from these
lets from synthesizing thromboxane A2, a potent vasoconstrictor and references as well as meta-analyses of these randomized clinical
promoter of platelet aggregation. But inhibiting COX-1 also de- trials, were also reviewed. We also reviewed the studies in the
pletes prostaglandin production, resulting in gut injury and contrib- relevant systematic reviews on aspirin from the 2009 and 2016
uting to the main adverse effects of aspirin including gastrointesti- USPSTF recommendations.
nal (GI) bleeding and ulceration. 11,12 Aspirin also has other
antiinflammatory and vasodilatory effects that may be important.12,13
Randomized clinical trials14,15 confirm that, in the high-risk
Advances in Treatment
setting of prevalent atherosclerotic cardiovascular disease (ASCVD)
or acute myocardial infarction (MI), aspirin decreases ASCVD events Randomized Clinical Trials and Meta-analyses
(approximately 20% reduction in coronary events and total stroke) in Primary Prevention
and, to a lesser extent, total and cardiovascular mortality, with simi- In individuals without clinical ASCVD, the benefit to risk ratio for as-
lar results in men and women. On an absolute scale, aspirin use for pirin should be carefully weighed because the absolute ASCVD risk
secondary prevention reduced ASCVD events by about 1% to 2% is lower than that associated with patients who have been diag-
per year (greater reduction for nonfatal than fatal events), at a cost nosed with ASCVD and the increased risk of aspirin-related bleed-
of bleeding that was generally an order of magnitude less than the ing (GI bleeding and, rarely, hemorrhagic stroke) is more closely
ASCVD benefit.14,16 However, the picture is less clear for patients matched with the potential for benefit.25 In the 2016 USPSTF sys-
without established ASCVD (primary prevention), which has re- tematic evidence review of the major aspirin primary prevention clini-
sulted in inconsistent guideline recommendations from various na- cal trials (11 trials, total N = 118 445) (Table 1),17 aspirin significantly
tional and international organizations (Box). In 2014, the US Food reduced nonfatal MI (22%), cardiovascular mortality (6%), and all-
and Drug Administration advised against aspirin use by patients to cause mortality (6%), with a nonsignificant reduction in nonfatal
lower their risk of first heart attack or stroke unless it was pre- stroke (5%).9 In the 8 trials (N = 87 524) (Table 1) that examined
scribed by a health care professional and after a careful evaluation doses of 100 mg or less daily, aspirin significantly reduced nonfatal
of the risks and benefits.24 This review focuses on advances in treat- MI (17%), nonfatal stroke (14%), with a nonsignificant reduction in
ment and diagnosis that relate to the use of aspirin for primary pre- all-cause mortality (5%).9 These results are consistent with the ear-
vention of cardiovascular disease, with discussion of additional ben- lier 2009 Antithrombotic Trialists’ (ATT) individual-level meta-
efits that relate to colorectal cancer, and evaluates the evidence base analysis (N = 6 trials, 95 456 individuals),14 that found a 12% rela-
for recent clinical recommendations, including those of the 2016 US tive risk reduction of total ASCVD events (absolute risk reduction
Preventive Services Task Force (USPSTF) (Box).17 0.51% vs 0.57%) in primary prevention trials (compared with 20%
in secondary prevention trials), as well as results from several more
recent meta-analyses. Since the ATT meta-analysis, 4 additional re-
cent randomized trials37-41 have evaluated aspirin in primary pre-
Methods vention on a background of contemporary statin and other preven-
We identified English-language, peer-reviewed publications through tative therapies (included in the USPSTF analysis) (Table 1).33-36 In
searches of the electronic databases of MEDLINE and the Cochrane each of these trials individually, aspirin did not significantly reduce
Database through April 2016 using the literature search terms the primary endpoints of total ASCVD (nonfatal and fatal events),
“aspirin,” in combination with one of the following: “primary raising questions about the use of aspirin for primary prevention.
prevention,” “heart disease,” “stroke,” “cardiovascular disease,” However, reductions in nonfatal ASCVD events were seen in some
E2 JAMA Internal Medicine Published online June 20, 2016 (Reprinted) jamainternalmedicine.com
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://archinte.jamanetwork.com/ by a La Trobe University User on 06/20/2016
Aspirin for Primary Prevention of Atherosclerotic Cardiovascular Disease Review Clinical Review & Education
of these recent trials, although they may have been underpowered
to detect significant differences in these events and had lower than Box. Summary of Guideline Recommendations on the Use
expected incidence rates. of Low-Dose Aspirin for Primary Prevention
of Atherosclerotic Cardiovascular Disease
Cardiovascular Mortality US Preventive Services Task Force
In individuals without ASCVD, there has been little or no benefit from 201617
aspirin in reducing cardiovascular mortality (Table 1). However, the Use aspirin for adults aged 50-59 y with 10-y ASCVD risk
smaller reduction in cardiovascular mortality in primary prevention !10%, not at increased risk of bleeding, life expectancy of
!10 y, and willing to take aspirin for !10 y
trials has to be viewed in the context of several important points:
(1) recent advances in contemporary treatments (including anti- Individualize the decision for adults aged 60-69 y with 10-y
ASCVD risk 10%, not at increased risk of bleeding, life
platelet and other regimens) and interventions (eg, revasculariza-
expectancy of !10 y, and willing to take aspirin for !10 y
tion and thrombolysis) for both MI and stroke, which have resulted
No recommendation for adults aged <50 y or !70 y
in lower ASCVD death rates; (2) cross-contamination by crossover
to active aspirin among individuals in the control arms once a non- 200918
Use aspirin when potential benefit outweighs the risk
fatal ASCVD event occurs, resulting in attenuation of the relative risk
of GI bleeding:
reduction of aspirin vs control for fatal ASCVD events; (3) lower
Men
absolute mortality rates in primary vs secondary prevention popu-
lations, which would necessitate much longer follow-up periods than Aged 45-59 y with 10-y CHD risk !4%
the mean follow-up in these trials (5 to 10 years); and (4) significant Aged 60-69 y with 10-y CHD risk !9%
reductions in nonfatal ASCVD events (MI and stroke) with aspirin in Aged 70-79 y with 10-y CHD risk !12%
primary prevention populations would be expected to result in Women
lower cardiovascular mortality if the duration of follow-up were Aged 55-59 y with 10-y stroke risk !3%
adequate, because individuals with prior MI or stroke are at the Aged 60-69 y with 10-y stroke risk !8%
highest risk for cardiovascular mortality.
Aged 70-79 y with 10-y stroke risk !11%
Not recommended for men aged <45 y, women aged < 55 y,
Baseline ASCVD Risk
men and women !80 y
There is a continuum of risk from primary to secondary prevention,
American Diabetes Association,19 2016
and it is uncertain where along this continuum lies the threshold level
Use aspirin 75 to 162 mg/d for individuals with diabetes who are
of risk that warrants aspirin use in patients without clinical ASCVD not at increased bleeding risk and who have 10-y ASCVD risk
(ie, when benefit exceeds risk). Importantly, the primary preven- >10% (includes most men and women !50 y with diabetes and
tion trials reported so far have mostly enrolled subjects with low or with !1 other ASCVD risk factors)
very low estimated baseline ASCVD risk, with more than 90% of par- Individualize for adults with diabetes, <50 y, and multiple
ticipants having an estimated risk of less than 1% per year (10-year ASCVD risk factors (10-y ASCVD risk 5%-10%)
risk <10%).14 Both the net ASCVD benefit and the bleeding events Not recommended for adults with diabetes who are at low
increased as the absolute ASCVD risk increased, but the net ben- ASCVD risk (10-y risk <5%)
efits exceeded the risks at higher baseline ASCVD risk (above 1% per American College of Chest Physicians,20 2012
year, or 10% ASCVD risk over 10 years).14,37 Hence, the absolute ben- Suggest aspirin use for adults !50 y
efit vs risk of aspirin depends on baseline ASCVD risk. Specifically, European Society of Cardiology,21 2012
among individuals with a baseline calculated 10-year ASCVD risk of Not recommended
at least 10%, the estimated absolute benefit of aspirin was about 1% American Heart Association,22 2011
to 2% for reducing ASCVD events over 5 years (ie, 2% to 4% over Can be useful in women !65 y if blood pressure is controlled
10 years), with a corresponding absolute GI bleeding rate of 0.5% and benefit outweighs risk
to 1% over the same period (ie, 1% to 2% over 10 years).14 The re- May be reasonable in women <65 y for prevention
sults of ongoing trials are eagerly awaited, as these have enrolled a of ischemic stroke
large proportion of individuals with 10-year risk of 10% or more on Not recommended for women <65 y for prevention
a background of modern-day therapies including statins. of myocardial infarction
Canadian Cardiovascular Society,23 2011
Age Consider only in special circumstances (CHD risk is high and
Age is the strongest predictor of ASCVD risk.14 Although the 2009 ATT bleeding risk is low)
meta-analysis of primary prevention trials found similar relative risk Not recommended for routine use
reduction with aspirin for individuals younger or older than 65 years,14 Abbreviations: ASCVD, atherosclerotic cardiovascular disease;
several individual trials found differences by age (Table 2). Age was a CHD, coronary heart disease; GI, gastrointestinal
key determinant of a woman’s cardiovascular response to aspirin and
her benefit to risk ratio with treatment.32 In the 4097 participants 65 aspirin by age interaction, P = .05 for major ASCVD and P= .03 for
years and older in the Women’s Health Study (WHS), the only large MI).32 On the other hand, women aged 45 to 64 years had no reduc-
primary prevention trial of aspirin in women (total N = 39 876), aspi- tion in ASCVD events, but experienced a similar increase in GI bleed-
rin was clearly beneficial for the primary endpoint of the trial (major ing, which resulted in an unfavorable benefit to risk ratio. In unpub-
ASCVD, 26% reduction), including for both MI and ischemic stroke (for lished data, the relative risk reduction for WHS women aged 70 to 79
jamainternalmedicine.com (Reprinted) JAMA Internal Medicine Published online June 20, 2016 E3
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://archinte.jamanetwork.com/ by a La Trobe University User on 06/20/2016
Downloaded From: http://archinte.jamanetwork.com/ by a La Trobe University User on 06/20/2016
E4
JAMA Internal Medicine Published online June 20, 2016 (Reprinted)
Clinical Review & Education Review
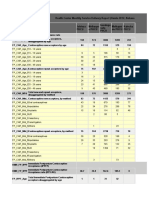
Table 1. Summary of the Major Aspirin Primary Prevention Trials
Aspirin Dose No. of Subjects Relative Risk (95% CI), Aspirin/Control Number of Events
(Daily, Unless Control (Aspirin/Control), Nonfatal Nonfatal Cardiovascular All-Cause
Trial (Acronym) Noted) Group Sex, Mean Age, y MI Stroke Mortality Mortality
British Doctors’ Study (BDS)26 300-500 mg No aspirin 3429/1710, M, 61 0.97 (0.67-1.41), 80/41 1.13 (0.72-1.77), 61/27 1.01 (0.74-1.37), 119/59 0.89 (0.74-1.08), 270/151
Physicians’ Health Study (PHS)27 325 mg every Placebo 11 037/11 034, M, 53 0.59 (0.47-0.74), 129/213 1.20 (0.91-1.59), 110/92 0.92 (0.66-1.28), 66/72 0.96 (0.80-1.14), 217/227
other day
Early Treatment Diabetic 650 mg Placebo 1856/1855, M/F, ~50 0.83 (P ≤ .05), 524 (combined) 1.26 (0.89-1.80), 67/53 0.89 (0.76-1.04), 244/275 0.93 (0.79-1.09), 284/305
Retinopathy Study (ETDRS)28
Thrombosis Prevention Trial 75 mg Placebo 1268/1272, M, 57 0.65 (0.45-0.92), 47/73 0.64 (0.34-1.20), 16/25 1.05 (0.69-1.61), 42/40 1.03 (0.80-1.32), 113/110
(TPT)29
Hypertension Optimal Treatment 75 mg Placebo 9399/9391, M/F, 61 0.60 (0.45-0.81), 68/113 0.99 (0.78-1.24),a 146/148 0.95 (0.75-1.20), 133/140 0.93 (0.79-1.09), 284/305
(HOT)30
Copyright 2016 American Medical Association. All rights reserved.
Primary Prevention Project 100 mg No aspirin 2226/2269, M/F, 64 0.69 (0.36-1.33), 15/22 0.84 (0.42-1.67), 15/18 0.56 (0.31-1.01), 17/31 0.81 (0.58-1.13), 62/78
(PPP)31
Women’s Health Study (WHS)32 100 mg every Placebo 19 934/19 942, F, 54 1.01 (0.83-1.24), 184/181 0.81 (0.67-0.97), 198/244 0.95 (0.74-1.22), 120/126 0.95 (0.85-1.06), 609/642
other day
Prevention of Progression 100 mg Placebo 638/638, M/F, 60 0.98 (0.69-1.40), 55/56 0.71 (0.45-1.12), 29/41 1.23 (0.80-1.89), 43/35 0.93 (0.72-1.21), 94/101
of Arterial Disease and Diabetes
(POPADAD)33
Japanese Primary Prevention 81-100 mg No aspirin 1262/1277, M/F, 65 1.35 (0.57-3.19), 12/9 1.01 (0.60-1.72), 27/27 0.10 (0.01-0.79), 1/10 0.91 (0.57-1.43), 33/38
of Atherosclerosis with Aspirin
for Diabetes (JPAD)34
Aspirin for Asymptomatic 100 mg Placebo 1675/1675, M/F, 62 0.91 (0.65-1.28), 62/68 0.97 (0.62-1.52), 37/38 1.17 (0.72-1.89), 43/35 0.95 (0.85-1.06), 609/642
Atherosclerosis (AAA)35
Japanese Primary Prevention 100 mg No aspirin 7220/7244, M/F, 70 0.53 (0.31-0.91), 20/38 1.00 (0.77-1.31), 109/109 1.02 (0.71-1.47), 58/57 0.98 (0.84-1.15), 297/303
Project (JPPP)36
b
Total All doses 118 445 0.78 (0.71-0.87) 0.95 (0.85-1.06) 0.94 (0.86-1.03) 0.94 (0.89-0.99)
Aspirin for Primary Prevention of Atherosclerotic Cardiovascular Disease
Low-dose aspirin trialsb ≤100 mg 87 524 0.83 (0.74-0.94) 0.86 (0.76-0.98) 0.97 (0.85-1.10) 0.95 (0.89-1.01)
Abbreviation: MI, myocardial infarction.
a
Total stroke.
b
From Guirguis-Blake et al, US Preventive Services Task Force 2016 Systematic Evidence Review.9
jamainternalmedicine.com
Aspirin for Primary Prevention of Atherosclerotic Cardiovascular Disease Review Clinical Review & Education
Table 2. Relative Risk of Aspirin vs Control in Primary Prevention Trials by Age and Study
Relative Risk, P Value
Age, Aspirin for Interaction
Source Endpoint Range, y vs Control by Age
Physicians’ Health Study (PHS)27 MI 40-49 1.12
50-59 0.58
.02
60-69 0.46
70-84 0.49
Thrombosis Prevention Trial (TPT)29 CHD 45-49 0.48
50-54 0.77
55-59 0.73 .055
60-64 0.61
65-69 1.29
Hypertension Optimal Treatment (HOT)30 CVD (MI) <65 0.79 (0.66)
NR (NR)
≥65 0.92 (0.62)
Women’s Health Study (WHS)32 CVD (MI) 45-54 1.01 (1.23)
55-64 0.98 (1.17) .05 (.03)
≥65 0.74 (0.66)
Prevention of Progression of Arterial CVD/limb <60 1.11
Disease and Diabetes (POPADAD)33 ischemia .44
≥60 0.89
Japanese Primary Prevention CVD <65 1.0
of Atherosclerosis with Aspirin .27
for Diabetes (JPAD)34 ≥65 0.68
Aspirin for Asymptomatic Atherosclerosis CVD <62 0.85
(AAA)35 NR
≥62 1.13 Abbreviations: CHD, coronary heart
Japanese Primary Prevention Project CVD <65 1.00 disease; CVD, cardiovascular disease;
(JPPP)36 NR MI, myocardial infarction; NR, not
≥65 0.92
reported.
Figure. Risk Reductions in Major Coronary Events and Ischemic Stroke by Randomized Aspirin Use and Sex
in Primary Prevention Trials Adapted From the 2009 ATT Meta-analysis14
Events (%/y)
RR Favors Favors
Subgroup Allocated Aspirin Allocated Control (95% CI) protection harm
Major coronary events
Men 635 (0.57%/y) 801 (0.72%/y) 0.77 (0.67-0.89)
Women 299 (0.14%/y) 314 (0.14%/y) 0.95 (0.77-1.17)
P for interaction = .03
Ischemic stroke
Men 312 (0.28%/y) 292 (0.26%/y) 1.06 (0.85-1.32)
Women 227 (0.10%/y) 301 (0.14%/y) 0.75 (0.60-0.94)
P for interaction = .05
0.50 0.75 1.0 1.25 1.50
RR (95% CI)
years was similar to women aged 60 to 69 years, with a similar rela- Differences by Sex
tive risk of GI bleeding. Age also modified (P for interaction, .02) the Trials14 in patients with established ASCVD have found similar
aspirin benefit in reducing MI in the Physicians’ Health Study,27 where aspirin efficacy in men and women. However, trials in primary pre-
aspirin did not reduce MI or ASCVD in men younger than 50 years, in vention populations have reported sex differences (Figure). In
contrast with relative risk reductions in men age 50 to 59 years (42%), men, aspirin reduces the risk of MI but not ischemic stroke; in
60 to 69 years (54%), and 70 to 84 years (51%). In the more recent women, aspirin reduces the risk of ischemic stroke but not MI.32,42
Japanese Primary Prevention of Atherosclerosis with Aspirin for Dia- It is unclear if this reflects biologic sex differences in aspirin phar-
betes trial,34 aspirin significantly reduced ASCVD (by a third) only in macokinetics and/or pharmacodynamics or different incidence
participants 65 years and older. Prior guidelines18 concluded that the rates in MI and stroke by sex and age (as the occurrence of stroke
evidence was insufficient to assess the balance of benefits and harms relative to MI is greater in younger than older women, and MI
of aspirin therapy for primary prevention in individuals 80 years and occurs on average a decade later in women than men). The former
older, while the 2016 USPSTF recommendations considered the evi- explanation of biological differences is less likely, as no substantial
denceinsufficientforindividuals70yearsorolder,orforthoseyounger differences have been noted in aspirin effects on platelet
than 50 years.17 reactivity43 and no sex differences were observed in secondary
jamainternalmedicine.com (Reprinted) JAMA Internal Medicine Published online June 20, 2016 E5
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://archinte.jamanetwork.com/ by a La Trobe University User on 06/20/2016
Clinical Review & Education Review Aspirin for Primary Prevention of Atherosclerotic Cardiovascular Disease
prevention trials. The WHS suggested a different pattern of 162 mg daily.19 For cardiovascular primary prevention, we recom-
ASCVD benefit with aspirin in women whereby aspirin significantly mend using regular (noncoated, nonbuffered) aspirin at a daily dose
lowered the risk of total and ischemic stroke, but did not lower the of 75 to 81 mg.
risk of MI except in women 65 years or older.32 This contrasted
with the significant reduction in MI in men 50 years and older and Genetic Profiling
neutral effect on stroke observed for men in the Physicians’ Health There are currently no clinical indications for targeting aspirin use
Study27 and other primary prevention trials.42 based on genetic testing. In the WHS study, 2 genetic variations
Nonetheless, the 2009 ATT meta-analysis and the 2016 USP- influenced aspirin efficacy, 1 in the LPA gene encoding
STF concluded that there is no strong evidence supporting effect lipoprotein(a) 50,51 and another in the COMT gene encoding
modification of aspirin benefit by sex, citing that the P values for in- catecho-O-methyltransferase.49 These promising findings await rep-
teraction by sex was no longer significant after accounting for mul- lication in other populations. Genetic variation in the genes encod-
tiple testing, despite clear sex differences in effect estimates for both ing the COX enzymes has been associated with platelet function, but
MI and stroke (Figure).9,14 The 2016 USPSTF recommendations for there is no strong evidence of association with clinical outcomes.50,51
aspirin use in primary prevention do not differ by sex (Box). 17
Indeed, the strongest recommendation (Grade B, the net benefit is Colorectal Cancer Incidence and Mortality
moderate to substantial) is given for men and women aged 50 to The 2016 USPSTF recommendations now incorporate the advice to
59 years with a 10% or greater ASCVD risk, in contrast with a Grade take low-dose aspirin daily for at least 10 years among individuals
I (insufficient evidence) recommendation for men and women 70 with a life expectancy of at least 10 years (predominantly for colo-
years and older.17 In our opinion, the results of the 2009 ATT meta- rectal cancer benefit), on top of the ASCVD risk cutpoints (predomi-
analysis, which included trials of diverse study populations with re- nantly for cardiovascular benefit).
spect to sex, age, and risk factor profiles, as well as a wide array of An association between daily aspirin allocation and reduction
aspirin doses, are less relevant than the results of the WHS—the only of long-term cancer mortality has been recently reported, with a 2011
large-scale primary prevention trial in initially healthy women—for meta-analysis52 of pooled cardiovascular randomized trials of daily
developing primary prevention guidelines for this population. We aspirin vs no aspirin (25 570 participants, 674 cancer deaths) find-
favor the approach taken by the 2011 American Heart Association ing a net reduction in cancer mortality of about 20%, which was
(AHA) Guidelines for Cardiovascular Prevention in Women,22 which greater with longer duration of follow-up and consistent in both
used the age cutpoint of 65 years (evidence-based from WHS) to sexes. In addition to the observed effect of aspirin in reducing can-
recommend aspirin for older women with a favorable benefit to risk cer mortality, the data for aspirin’s delayed benefit for reducing GI
ratio, and only recommended consideration of aspirin in younger cancer incidence, in particular colorectal cancer, are also plausible
women if the benefit for ischemic stroke outweighed the risk. and consistent,39,53 with aspirin reducing the long-term risk of
colorectal cancer incidence by approximately 20%. The 2016
Aspirin Dose and Formulation USPSTF systematic review54 estimated a relative risk reduction of
Current guidelines offer mixed recommendations regarding the as- 40% for aspirin use of at least 10 years on colorectal cancer inci-
pirin dose, ranging from not mentioning the dose to considering dence. Although most of the data come from a follow-up of more
doses up to 325 mg /d, reflecting uncertainty in the optimal dose for than 10 years in randomized clinical trials of cardiovascular preven-
cardiovascular prevention. Currently available data support the use tion, these results are remarkably consistent with a recent ex-
of doses between 75 and 162 mg /d, since these are as effective as tended follow-up report55 from 1 large trial done in women (WHS),
higher doses for ASCVD prevention, and may have lower bleeding which had cancer as a prespecified primary endpoint, as well as with
rates.44 Most primary prevention trials tested doses of 100 mg/d a trial done among individuals with a genetic predisposition for co-
or less (Table 1).14 We agree with the pragmatic 2016 USPSTF rec- lorectal cancer.56 Aspirin may be particularly beneficial for reduc-
ommendation to use a dose of 81 mg/d (or 75 to 100 mg/d outside ing cancer incidence and cancer mortality,39,52 especially for colo-
the United States),17 because higher doses do not prevent more rectal and other GI cancers,57 with longer durations of aspirin use
ASCVD events while possibly increasing the risk of bleeding. The 2016 (>5 to 10 years) and among individuals with risk factors for colorec-
recommendations also appropriately point out that enteric-coated tal cancer, including a family history of colorectal cancer, familial syn-
or buffered formulations do not improve the safety of aspirin, be- dromes (familial adenomatous polyposis or Lynch syndrome), or a
cause GI bleeding and ulceration is a systemic adverse effect of pros- personal history of colorectal adenomas. Aspirin for cancer preven-
taglandin depletion by aspirin inhibiting COX-1.45 Aspirin resis- tion may be considered for individuals in whom the risks for ASCVD
tance based on platelet function testing can occur in up to 28% of and bleeding are closely balanced; those at higher risk for colorec-
individuals treated with aspirin, and this has been associated with tal cancer may have net benefit even if the net cardiovascular
worse ASCVD outcomes in small observational studies.46 A recent benefit for aspirin in these individuals is less clear.
study in healthy volunteers compared a dose of 325 mg immediate-
release with enteric-coated aspirin and found no aspirin resistance
(by platelet function testing) in subjects given immediate-release
Advances in Diagnosis
aspirin, compared with a substantial proportion of aspirin resis-
tance (49% at 4 hours and 17% at 8 hours) with the enteric-coated Advances in Cardiovascular Risk Assessment
aspirin.47 Aspirin dosing of 100 mg twice daily may be more effec- Estimating cardiovascular risk is central to clinical decision making
tive in inhibiting platelets than 200 mg or 100 mg once daily,48 but to initiate and maintain preventative therapies when risks and
the data are insufficient for recommending doses higher than benefits of interventions are in question, as in the case of aspirin
E6 JAMA Internal Medicine Published online June 20, 2016 (Reprinted) jamainternalmedicine.com
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://archinte.jamanetwork.com/ by a La Trobe University User on 06/20/2016
Aspirin for Primary Prevention of Atherosclerotic Cardiovascular Disease Review Clinical Review & Education
use for primary prevention. Cardiovascular risk assessment is usu- Table 3. Major Risk Factors for Gastrointestinal Bleeding
ally obtained from a global risk score.58,59 Until recently, separate and Related Complications
risk scores were used to estimate the risk of coronary heart dis-
Risk Factor Adjusted Relative Risk Increase
ease (CHD: MI and coronary death) and stroke. In 2013, the Ameri-
History of upper GI disorder
can College of Cardiology (ACC) and the AHA recommended using
Dyspepsia/pain 2
a risk score that estimates 10-year risk of ASCVD, which includes
Prior GI hospitalization 3
MI, ischemic stroke, and ASCVD death, providing separate equa-
Peptic ulcer (uncomplicated) 3 to 6
tions for women, men, blacks, and whites. These sex- and race-
Peptic ulcer with GI 10
specific risk equations quantify the 10-year risk of ASCVD events in bleeding/perforation
asymptomatic women and men age 40 to 79 years, taking into Age >60 y Exponential
account their age, systolic blood pressure, antihypertensive Male sex 2
therapy, diabe te s, smoking status, and total and HDL Medications Variable
cholesterol.58,59 Moreover, these risk equations can also be used
NSAID use (current or recent) 1.1 to 2
among individuals treated with statins. While the calibration accu-
Aspirin (≤325 mg/d) 1.5 to 2
racy of these equations in contemporary populations has been
Other antiplatelets/anticoagulants 1.3 to 2
debated (ie, whether the estimated ASCVD risks accurately corre-
Other Variable (generally <2)
spond to the observed 10-year ASCVD risks), the high-risk thresh-
Smoking
old for considering aspirin use in the 2016 USPSTF recommenda-
Excess alcohol
tions is a 10-year ASCVD risk of 10%, which is more conservative
Hypertension
than the 10-year risk of 5% to 7.5% recommended for initiating a
Diabetes
statin discussion,58 and also similar to or higher than thresholds
recommended in other recent aspirin guidelines.18,60-62 Increased BMI
Renal or liver disease
Advances in Bleeding Risk Assessment Abbreviations: BMI, body mass index calculated as weight in kilograms divided
Individuals who are at highest risk for ASCVD events tend to also be by height in meters squared; GI, gastrointestinal.
at highest risk for bleeding complications.63,64 The 2016 USPSTF as-
pirin recommendations apply to individuals without increased risk
of bleeding (eg, history of GI ulcers, recent bleeding, or use of medi-
cations that increase bleeding risk). In the 2009 ATT meta-analysis,14 to greater than 0.5% per year at age 85 years, with approximately
extracranial and/or GI bleeding rates were low (0.7 per 1000 person- doubling of risk per decade. Men have a 2-fold increased risk com-
years) and hemorrhagic stroke was even lower (0.3 per 1000 person- pared with women. The ues of NSAIDs, which is common among the
years). Risk factors for hemorrhagic stroke include increasing age, elderly population,70 has been associated with a variable increased
current smoking, and hypertension.65 Older age is a strong risk fac- risk from 1.1 in a recent Italian study71 to an increased risk of 2- to
tor for intracranial hemorrhage, and the risk of bleeding in elderly 4-fold in other populations.68,69 This risk is not mitigated by using
individuals on aspirin is comparable to the risk of bleeding on oral a selective NSAID (COX-2 inhibitor) as the GI ulcer and bleeding risk
anticoagulation.1,66,67 Individuals with a history of atrial fibrillation of a COX-2 inhibitor combined with aspirin is similar to the risk of a
are often older and have comorbidities and concomitant medica- nonselective NSAID.11 In randomized clinical trials, the risk of GI
tions that put them at increased risk of bleeding.66,67 bleeding is approximately 50% higher with aspirin than placebo,14,37
but risks may be higher in real-world situations.72
GI Bleeding
Gastrointestinal bleeding is a significant predictor of death, even af- GI Prophylaxis
ter adjusting for comorbidities.63,64 The 2009 meta-analysis14 found A 2015 meta-analysis73 of randomized clinical trials and observa-
no increase in the risk of fatal GI bleeding with aspirin use in the pri- tional studies reported that the use of a proton pump inhibitor (PPI)
mary prevention trials. In general populations, the estimated inci- may reduce the aspirin-related risk of upper GI bleeding by half, be-
dence rate of upper GI complications is approximately 1 to 2 per 1000 cause it suppresses gastric acid production and promotes healing
person-years,65 with a case fatality rate of 5% to 10% of these of ulcers and erosions.74,75 Routine use of PPI is not recommended
complications.68,69 The incidence rate of upper GI complications is for patients at lower bleeding risk.76 Limited data suggest that PPIs
often more than 2% per year in high-risk individuals. The risk of GI may be more effective than H2 receptor antagonists.76 Proton pump
bleeding increases with the number of risk factors. Major risk fac- inhibitor use is recommended for reducing risk of GI bleeding in in-
tors (Table 3) include a history of an upper GI disorder (dyspepsia, dividuals with multiple bleeding risk factors who require aspirin.11,76
peptic ulcer, Helicobacter pylori infection, upper GI bleeding and/or A recent expert consensus statement recommended PPI use for in-
perforation), age more than 60 years (doubling in risk with each de- dividuals with 2 or more GI risk factors (! 60 years, current use of
cade), male sex, and concomitant or recent use of NSAIDs and other corticosteroids, NSAIDs, anticoagulant therapy [each counts as 1 risk
medications, ASCVD risk factors, excess alcohol, and renal or liver factor], and dyspepsia and/or gastroesophageal reflux disease
disease. The strongest risk factor for GI bleeding is a prior history of symptoms), similar to recent recommendations from the Euro-
peptic ulcer disease, in particular if complicated by bleeding or per- pean Society of Cardiology.77 Furthermore, limited evidence sug-
foration. Gastrointestinal bleeding risk increases exponentially with gests that patients with a history of a peptic ulcer may derive
age, going from less than 0.1% per year in those older than 60 years additional benefit from Helicobacter pylori eradication.78
jamainternalmedicine.com (Reprinted) JAMA Internal Medicine Published online June 20, 2016 E7
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://archinte.jamanetwork.com/ by a La Trobe University User on 06/20/2016
Clinical Review & Education Review Aspirin for Primary Prevention of Atherosclerotic Cardiovascular Disease
Aspirin-Guide: A Clinical Decision Support Tool
Guidelines have relegated the individualized ASCVD and bleeding Conclusions
risk assessments to health care providers in discussion with pa-
tients, although there are limited support tools for these complex In the absence of contraindications, decisions regarding
comparative calculations in the busy clinic setting. The Aspirin- aspirin use for the primary prevention of ASCVD should be
Guide decision support tool (available for mobile devices) aids cli- highly individualized, balancing the benefit to risk ratio and
nicians with this dual assessment for individual patients by incor- patient preferences regarding anticipated long-term treatment.
porating evidence-based decision making for the use of aspirin in Clinicians should consider GI bleeding risk factors and personalize
primary prevention. Formal assessment of the ASCVD and GI bleed- the ASCVD risk assessment with 10-year ASCVD risk calculations
ing risks is provided through internal risk calculators for these dual as well as age- and sex-specific guidance based on randomized
risk scores, along with the estimated numbers needed to treat and clinical trial results, with secondary considerations regarding
harm. As further refinements to the 10-year ASCVD risk estimates, the potential benefit of aspirin use for colorectal cancer
the decision support tool additionally uses age and sex categories prevention. The Aspirin-Guide is a clinical decision making
(<50 or !50 years for men, and <65 or !65 years for women, based support tool and mobile app with internal risk calculators
on age- and sex-specific results from the randomized trials) to fur- to help busy clinicians make more personalized and evidence-
ther enhance ASCVD risk stratification, and also incorporates con- based decisions. Aspirin should be used consistently in both
siderations for reducing colorectal cancer risk among individuals in s exe s f o r t h e s e c o n d a r y p r e ve n t i o n o f A S C V D u n l e s s
whom the ASCVD and bleeding risks are closely balanced. contraindicated.
ARTICLE INFORMATION 5. Fuster V, Sweeny JM. Aspirin: a historical and individual participant data from randomised trials.
Published Online: June 20, 2016. contemporary therapeutic overview. Circulation. Lancet. 2009;373(9678):1849-1860.
doi:10.1001/jamainternmed.2016.2648. 2011;123(7):768-778. 15. Collaborative overview of randomised trials of
Conflict of Interest Disclosures: Dr Mora has 6. Manson JE, Burning JE, Ridker PM, Gaziano JM, antiplatelet therapy, I: prevention of death,
received research support from Atherotech eds. Clinical Trials in Cardiovascular Disease: myocardial infarction, and stroke by prolonged
Diagnostics and NHLBI, served as a consultant to A Companion to Braunwald's Heart Disease. 2nd ed. antiplatelet therapy in various categories of
Quest Diagnostics, Lilly, Amgen, Pfizer, and Cerenis Philadelphia, PA: WB Saunders; 2004:333-348. patients. Antiplatelet Trialists’ Collaboration. BMJ.
Therapeutics. No other disclosures are reported. 7. Pignone M, Anderson GK, Binns K, Tilson HH, 1994;308(6921):81-106.
Funding/Support: Drs Manson and Mora receive Weisman SM. Aspirin use among adults aged 40 16. Antithrombotic Trialists’ Collaboration.
support from the National Institutes of Health and older in the United States: results of a national Collaborative meta-analysis of randomised trials of
(HL034594, HL117861, CA138962, and survey. Am J Prev Med. 2007;32(5):403-407. antiplatelet therapy for prevention of death,
HHSN268201100001C). 8. Mainous AG, Tanner RJ, Shorr RI, Limacher MC. myocardial infarction, and stroke in high risk
Use of aspirin for primary and secondary patients. BMJ. 2002;324(7329):71-86.
Role of the Funder/Sponsor: The funders/
sponsors had no role in the design and conduct of cardiovascular disease prevention in the United 17. Siu AL; US Preventive Services Task Force.
the study; collection, management, analysis, and States, 2011-2012. J Am Heart Assoc. 2014;3(4): Aspirin use for the primary prevention of
interpretation of the data; preparation, review, or e000989. cardiovascular disease and colorectal cancer: US
approval of the manuscript; and decision to submit 9. Whitlock EP, Williams SB, Burda BU, Feightner A, Preventive Services Task Force recommendation
the manuscript for publication. Beil T. Aspirin Use in Adults: Cancer, All-Cause statement. Ann Intern Med. 2016;164: Epub ahead
Mortality, and Harms: A Systematic Evidence Review of print. doi:10.7326/M7316-0577.
Additional Contributions: We thank Jeffrey M.
Ames, BS, MEng, computer scientist, for expert for the US Preventive Services Task Force. Rockville, 18. US Preventive Services Task Force. Aspirin for
assistance in the development of Aspirin-Guide, a MD: Agency for Healthcare Research and Quality; the prevention of cardiovascular disease: U.S.
mobile application and clinical decision support tool 2015. Report No. 13-05193-EF-1. Preventive Services Task Force recommendation
that facilitates assessment of the comparative 10. Vane JR. Inhibition of prostaglandin synthesis statement. Ann Intern Med. 2009;150(6):396-404.
benefits and risks of aspirin for the individual as a mechanism of action for aspirin-like drugs. Nat 19. American Diabetes Association. 8.
patient. He was not compensated for his New Biol. 1971;231(25):232-235. Cardiovascular disease and risk management.
contribution. 11. Bhatt DL, Scheiman J, Abraham NS, et al; Diabetes Care. 2016;39(suppl 1):S60-S71.
American College of Cardiology Foundation Task 20. Vandvik PO, Lincoff AM, Gore JM, et al.
REFERENCES Force on Clinical Expert Consensus Documents. Primary and secondary prevention of
1. Mozaffarian D, Benjamin EJ, Go AS, et al; ACCF/ACG/AHA 2008 expert consensus document cardiovascular disease: Antithrombotic therapy and
American Heart Association Statistics Committee on reducing the gastrointestinal risks of antiplatelet prevention of thrombosis, 9th ed: American College
and Stroke Statistics Subcommittee. Heart disease therapy and NSAID use: a report of the American of Chest Physicians evidence-based clinical practice
and stroke statistics—2015 update: a report from College of Cardiology Foundation Task Force on guidelines. Chest. 2012;141(suppl 2):e637S-668S.
the American Heart Association. Circulation. 2015; Clinical Expert Consensus Documents. J Am Coll 21. Perk J, De Backer G, Gohlke H, et al; European
131(4):e29-e322. Cardiol. 2008;52(18):1502-1517. Association for Cardiovascular Prevention &
2. Murray CJ, Atkinson C, Bhalla K, et al; U.S. 12. Wallace JL. Prostaglandins, NSAIDs, and gastric Rehabilitation (EACPR); ESC Committee for Practice
Burden of Disease Collaborators. The state of US mucosal protection: why doesn’t the stomach Guidelines (CPG). European Guidelines on
health, 1990-2010: burden of diseases, injuries, and digest itself? Physiol Rev. 2008;88(4):1547-1565. cardiovascular disease prevention in clinical
risk factors. JAMA. 2013;310(6):591-608. 13. Yin MJ, Yamamoto Y, Gaynor RB. The practice (version 2012): the Fifth Joint Task Force of
3. Ford ES, Ajani UA, Croft JB, et al. Explaining the anti-inflammatory agents aspirin and salicylate the European Society of Cardiology and Other
decrease in U.S. deaths from coronary disease, inhibit the activity of I(kappa)B kinase-beta. Nature. Societies on Cardiovascular Disease Prevention in
1980-2000. N Engl J Med. 2007;356(23):2388-2398. 1998;396(6706):77-80. Clinical Practice (constituted by representatives of
nine societies and by invited experts). Eur Heart J.
4. Jack DB. One hundred years of aspirin. Lancet. 14. Baigent C, Blackwell L, Collins R, et al; 2012;33(13):1635-1701.
1997;350(9075):437-439. Antithrombotic Trialists’ (ATT) Collaboration.
Aspirin in the primary and secondary prevention of 22. Mosca L, Benjamin EJ, Berra K, et al.
vascular disease: collaborative meta-analysis of Effectiveness-based guidelines for the prevention
of cardiovascular disease in women—2011 update:
E8 JAMA Internal Medicine Published online June 20, 2016 (Reprinted) jamainternalmedicine.com
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://archinte.jamanetwork.com/ by a La Trobe University User on 06/20/2016
Aspirin for Primary Prevention of Atherosclerotic Cardiovascular Disease Review Clinical Review & Education
a guideline from the american heart association. population screened for a low ankle brachial index: 50. Roden DM. Cardiovascular
Circulation. 2011;123(11):1243-1262. a randomized controlled trial. JAMA. 2010;303(9): pharmacogenomics: current status and future
23. Bell AD, Roussin A, Cartier R, et al. The use of 841-848. directions. J Hum Genet. 2016;61(1):79-85.
antiplatelet therapy in the outpatient setting: 36. Ikeda Y, Shimada K, Teramoto T, et al. Low-dose 51. Paynter NP, Ridker PM, Chasman DI. Are genetic
Canadian Cardiovascular Society Guidelines aspirin for primary prevention of cardiovascular tests for atherosclerosis ready for routine clinical
Executive Summary. Can J Cardiol. 2011;27(2):208- events in Japanese patients 60 years or older with use? Circ Res. 2016;118(4):607-619.
221. atherosclerotic risk factors: a randomized clinical 52. Rothwell PM, Fowkes FG, Belch JF, Ogawa H,
24. US Department of Health and Human Services. trial. JAMA. 2014;312(23):2510-2520. Warlow CP, Meade TW. Effect of daily aspirin on
FDA. Can an aspirin a day help prevent a heart 37. Seshasai SR, Wijesuriya S, Sivakumaran R, et al. long-term risk of death due to cancer: analysis of
attack? http://www.fda.gov/forconsumers Effect of aspirin on vascular and nonvascular individual patient data from randomised trials. Lancet.
/consumerupdates/ucm390539.Htm. 2014. outcomes: meta-analysis of randomized controlled 2011;377(9759):31-41.
Accessed October 11, 2015. trials. Arch Intern Med. 2012;172(3):209-216. 53. Bosetti C, Rosato V, Gallus S, Cuzick J,
25. Mora S. Aspirin therapy in primary prevention: 38. Sutcliffe P, Connock M, Gurung T, et al. Aspirin La Vecchia C. Aspirin and cancer risk: a quantitative
comment on “effect of aspirin on vascular and in primary prevention of cardiovascular disease and review to 2011. Ann Oncol. 2012;23(6):1403-1415.
nonvascular outcomes.” Arch Intern Med. 2012;172 cancer: a systematic review of the balance of 54. Chubak J, Whitlock EP, Williams SB, et al.
(3):217-218. evidence from reviews of randomized trials. PLoS Aspirin for the prevention of cancer incidence and
26. Peto R, Gray R, Collins R, et al. Randomised trial One. 2013;8(12):e81970. mortality: Systematic evidence reviews for the US
of prophylactic daily aspirin in British male doctors. 39. Cuzick J, Thorat MA, Bosetti C, et al. Estimates Preventive Services Task Force. Ann Intern Med. 2016;
Br Med J (Clin Res Ed). 1988;296(6618):313-316. of benefits and harms of prophylactic use of aspirin Epub ahead of print. doi:10.7326/M15-2117.
27. Steering committee of the Physicians' Health in the general population. Ann Oncol. 2015;26(1): 55. Cook NR, Lee IM, Zhang SM, Moorthy MV,
Study research group. Final report on the aspirin 47-57. Buring JE. Alternate-day, low-dose aspirin and
component of the ongoing Physicians’ Health 40. Raju N, Sobieraj-Teague M, Hirsh J, O’Donnell cancer risk: long-term observational follow-up of a
Study. N Engl J Med. 1989;321(3):129-135. M, Eikelboom J. Effect of aspirin on mortality in the randomized trial. Ann Intern Med. 2013;159(2):77-85.
28. ETDRS Investigators. Aspirin effects on primary prevention of cardiovascular disease. Am J 56. Burn J, Gerdes AM, Macrae F, et al; CAPP2
mortality and morbidity in patients with diabetes Med. 2011;124(7):621-629. Investigators. Long-term effect of aspirin on cancer
mellitus. Early Treatment Diabetic Retinopathy 41. Bartolucci AA, Tendera M, Howard G. risk in carriers of hereditary colorectal cancer: an
Study report 14. JAMA. 1992;268(10):1292-1300. Meta-analysis of multiple primary prevention trials analysis from the CAPP2 randomised controlled
29. Thrombosis prevention trial. Thrombosis of cardiovascular events using aspirin. Am J Cardiol. trial. Lancet. 2011;378(9809):2081-2087.
prevention trial: randomised trial of low-intensity 2011;107(12):1796-1801. 57. Chan AT, Arber N, Burn J, et al. Aspirin in the
oral anticoagulation with warfarin and low-dose 42. Berger JS, Roncaglioni MC, Avanzini F, chemoprevention of colorectal neoplasia: an
aspirin in the primary prevention of ischaemic heart Pangrazzi I, Tognoni G, Brown DL. Aspirin for the overview. Cancer Prev Res (Phila). 2012;5(2):164-178.
disease in men at increased risk. The Medical primary prevention of cardiovascular events in 58. Stone NJ, Robinson JG, Lichtenstein AH, et al;
Research Council’s General Practice Research women and men: a sex-specific meta-analysis of American College of Cardiology/American Heart
Framework. Lancet. 1998;351(9098):233-241. randomized controlled trials. JAMA. 2006;295(3): Association Task Force on Practice Guidelines. 2013
30. Hansson L, Zanchetti A, Carruthers SG, et al; 306-313. ACC/AHA guideline on the treatment of blood
HOT Study Group. Effects of intensive 43. Becker DM, Segal J, Vaidya D, et al. Sex cholesterol to reduce atherosclerotic cardiovascular
blood-pressure lowering and low-dose aspirin in differences in platelet reactivity and response to risk in adults: a report of the American College of
patients with hypertension: principal results of the low-dose aspirin therapy. JAMA. 2006;295(12): Cardiology/American Heart Association Task Force
Hypertension Optimal Treatment (HOT) 1420-1427. on Practice Guidelines. Circulation. 2014;129(25)
randomised trial. Lancet. 1998;351(9118):1755-1762. 44. Campbell CL, Smyth S, Montalescot G, (suppl 2):S1-S45.
31. de Gaetano G; Collaborative Group of the Steinhubl SR. Aspirin dose for the prevention of 59. Goff DC Jr, Lloyd-Jones DM, Bennett G, et al;
Primary Prevention Project. Low-dose aspirin and cardiovascular disease: a systematic review. JAMA. American College of Cardiology/American Heart
vitamin E in people at cardiovascular risk: 2007;297(18):2018-2024. Association Task Force on Practice Guidelines. 2013
a randomised trial in general practice. Lancet. 2001; 45. Wallace JL, Vong L. NSAID-induced ACC/AHA guideline on the assessment of
357(9250):89-95. gastrointestinal damage and the design of cardiovascular risk: a report of the American
32. Ridker PM, Cook NR, Lee IM, et al. GI-sparing NSAIDs. Curr Opin Investig Drugs. 2008; College of Cardiology/American Heart Association
A randomized trial of low-dose aspirin in the 9(11):1151-1156. task force on practice guidelines. Circulation. 2014;
primary prevention of cardiovascular disease in 129(25)(suppl 2):S49-S73.
46. Krasopoulos G, Brister SJ, Beattie WS,
women. N Engl J Med. 2005;352(13):1293-1304. Buchanan MR. Aspirin “resistance” and risk of 60. Pearson TA, Blair SN, Daniels SR, et al;
33. Belch J, MacCuish A, Campbell I, et al; cardiovascular morbidity: systematic review and American Heart Association Science Advisory and
Prevention of Progression of Arterial Disease and meta-analysis. BMJ. 2008;336(7637):195-198. Coordinating Committee. AHA guidelines for
Diabetes Study Group; Diabetes Registry Group; primary prevention of cardiovascular disease and
47. Grosser T, Fries S, Lawson JA, Kapoor SC, Grant stroke: 2002 update: Consensus panel guide to
Royal College of Physicians Edinburgh. The GR, FitzGerald GA. Drug resistance and
prevention of progression of arterial disease and comprehensive risk reduction for adult patients
pseudoresistance: an unintended consequence of without coronary or other atherosclerotic vascular
diabetes (POPADAD) trial: factorial randomised enteric coating aspirin. Circulation. 2013;127(3):377-
placebo controlled trial of aspirin and antioxidants diseases. Circulation. 2002;106(3):388-391.
385.
in patients with diabetes and asymptomatic 61. Redberg RF, Benjamin EJ, Bittner V, et al;
peripheral arterial disease. BMJ. 2008;337:a1840. 48. Bethel MA, Harrison P, Sourij H, et al. American Academy of Family Physicians; American
Randomized controlled trial comparing impact on Association of Cardiovascular and Pulmonary
34. Ogawa H, Nakayama M, Morimoto T, et al; platelet reactivity of twice-daily with once-daily
Japanese Primary Prevention of Atherosclerosis Rehabilitation; Preventive Cardiovascular Nurses
aspirin in people with type 2 diabetes. Diabet Med. Association. AHA/ACCF [corrected] 2009
With Aspirin for Diabetes (JPAD) Trial Investigators. 2016;33(2):224-230.
Low-dose aspirin for primary prevention of performance measures for primary prevention of
atherosclerotic events in patients with type 2 49. Chasman DI, Shiffman D, Zee RY, et al. cardiovascular disease in adults: a report of the
diabetes: a randomized controlled trial. JAMA. Polymorphism in the apolipoprotein(a) gene, American College of Cardiology Foundation/
2008;300(18):2134-2141. plasma lipoprotein(a), cardiovascular disease, and American Heart Association task force on
low-dose aspirin therapy. Atherosclerosis. 2009; performance measures (writing committee to
35. Fowkes FG, Price JF, Stewart MC, et al; Aspirin 203(2):371-376. develop performance measures for primary
for Asymptomatic Atherosclerosis Trialists. Aspirin prevention of cardiovascular disease): developed in
for prevention of cardiovascular events in a general collaboration with the American Academy of Family
Physicians; American Association of Cardiovascular
jamainternalmedicine.com (Reprinted) JAMA Internal Medicine Published online June 20, 2016 E9
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://archinte.jamanetwork.com/ by a La Trobe University User on 06/20/2016
Clinical Review & Education Review Aspirin for Primary Prevention of Atherosclerotic Cardiovascular Disease
and Pulmonary Rehabilitation; and Preventive prevention in an elderly community population 74. Lanas A, Wu P, Medin J, Mills EJ. Low doses of
Cardiovascular Nurses Association: endorsed by the with atrial fibrillation (the Birmingham Atrial acetylsalicylic acid increase risk of gastrointestinal
American College of Preventive Medicine, American Fibrillation Treatment of the Aged Study, BAFTA): bleeding in a meta-analysis. Clin Gastroenterol
College of Sports Medicine, and Society for a randomised controlled trial. Lancet. 2007;370 Hepatol. 2011;9(9):762-768.e6..
Women’s Health Research. Circulation. 2009;120 (9586):493-503. 75. Laine L, Hennekens C. Proton pump inhibitor
(13):1296-1336. 67. Lip GY. Implications of the CHA(2)DS(2)-VASc and clopidogrel interaction: fact or fiction? Am J
62. Goldstein LB, Bushnell CD, Adams RJ, et al; and HAS-BLED Scores for thromboprophylaxis in Gastroenterol. 2010;105(1):34-41.
American Heart Association Stroke Council; Council atrial fibrillation. Am J Med. 2011;124(2):111-114. 76. Abraham NS, Hlatky MA, Antman EM, et al;
on Cardiovascular Nursing; Council on 68. Hernández-Díaz S, Rodríguez LA. Incidence of ACCF/ACG/AHA. ACCF/ACG/AHA 2010 Expert
Epidemiology and Prevention; Council for High serious upper gastrointestinal bleeding/perforation Consensus Document on the concomitant use of
Blood Pressure Research; Council on Peripheral in the general population: review of epidemiologic proton pump inhibitors and thienopyridines:
Vascular Disease, and Interdisciplinary Council on studies. J Clin Epidemiol. 2002;55(2):157-163. a focused update of the ACCF/ACG/AHA 2008
Quality of Care and Outcomes Research. Guidelines expert consensus document on reducing the
for the primary prevention of stroke: a guideline for 69. Hernández-Díaz S, García Rodríguez LA.
Cardioprotective aspirin users and their excess risk gastrointestinal risks of antiplatelet therapy and
healthcare professionals from the American Heart NSAID use: a report of the American College of
Association/American Stroke Association. Stroke. of upper gastrointestinal complications. BMC Med.
2006;4:22. Cardiology Foundation Task Force on Expert
2011;42(2):517-584. Consensus Documents. Circulation. 2010;122(24):
63. Abbas AE, Brodie B, Dixon S, et al. Incidence 70. Talley NJ, Evans JM, Fleming KC, Harmsen WS, 2619-2633.
and prognostic impact of gastrointestinal bleeding Zinsmeister AR, Melton LJ III. Nonsteroidal
antiinflammatory drugs and dyspepsia in the 77. Hamm CW, Bassand JP, Agewall S, et al; ESC
after percutaneous coronary intervention for acute Committee for Practice Guidelines. ESC Guidelines
myocardial infarction. Am J Cardiol. 2005;96(2): elderly. Dig Dis Sci. 1995;40(6):1345-1350.
for the management of acute coronary syndromes
173-176. 71. De Berardis G, Lucisano G, D’Ettorre A, et al. in patients presenting without persistent
64. Moukarbel GV, Signorovitch JE, Pfeffer MA, Association of aspirin use with major bleeding in ST-segment elevation: The Task Force for the
et al. Gastrointestinal bleeding in high risk survivors patients with and without diabetes. JAMA. 2012; management of acute coronary syndromes (ACS) in
of myocardial infarction: the VALIANT Trial. Eur 307(21):2286-2294. patients presenting without persistent ST-segment
Heart J. 2009;30(18):2226-2232. 72. García Rodríguez LA, Hernández-Díaz S, elevation of the European Society of Cardiology
65. Whitlock EP, Burda BU, Williams SB, de Abajo FJ. Association between aspirin and upper (ESC). Eur Heart J. 2011;32(23):2999-3054.
Guirguis-Blake JM, Evans CV. Bleeding risks with gastrointestinal complications: systematic review of 78. Gisbert JP, Calvet X, Cosme A, et al; H. pylori
aspirin use for primary prevention in adults: epidemiologic studies. Br J Clin Pharmacol. 2001;52 Study Group of the Asociación Española de
A systematic evidence review for the US Preventive (5):563-571. Gastroenterología (Spanish Gastroenterology
Services Task Force. Ann Intern Med. 2016; Epub 73. Tran-Duy A, Vanmolkot FH, Joore MA, Hoes Association). Long-term follow-up of 1,000
ahead of print. doi:10.7326/M15-2112. AW, Stehouwer CD. Should patients prescribed patients cured of Helicobacter pylori infection
66. Mant J, Hobbs FD, Fletcher K, et al; BAFTA long-term low-dose aspirin receive proton pump following an episode of peptic ulcer bleeding. Am J
investigators; Midland Research Practices Network inhibitors? a systematic review and meta-analysis. Gastroenterol. 2012;107(8):1197-1204.
(MidReC). Warfarin versus aspirin for stroke Int J Clin Pract. 2015;69(10):1088-1111.
E10 JAMA Internal Medicine Published online June 20, 2016 (Reprinted) jamainternalmedicine.com
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://archinte.jamanetwork.com/ by a La Trobe University User on 06/20/2016
You might also like
- Screening For Prostate Cancer With The Prostate-Specific Antigen Test A Review of Current EvidenceDocument7 pagesScreening For Prostate Cancer With The Prostate-Specific Antigen Test A Review of Current EvidenceSebastián MooreNo ratings yet
- Cost-Effectiveness of 10-Year Risk ThresholdsDocument9 pagesCost-Effectiveness of 10-Year Risk Thresholds62qg962xpbNo ratings yet
- 10 1001@jamainternmed 2019 0392Document8 pages10 1001@jamainternmed 2019 0392Tantri SyahtiraNo ratings yet
- JVP 160080Document2 pagesJVP 160080JavierstpNo ratings yet
- CMHDocument14 pagesCMHPaulaNo ratings yet
- Original PDF Pathophysiology of Heart Disease A Collaborative 6th Edition PDFDocument41 pagesOriginal PDF Pathophysiology of Heart Disease A Collaborative 6th Edition PDFwilliams.allen717100% (37)
- Artículo Síndrome Compartimental PDFDocument11 pagesArtículo Síndrome Compartimental PDFMoises OnofreNo ratings yet
- SICA en EMGDocument30 pagesSICA en EMGCarolinaDeLaCruzDavilaNo ratings yet
- 2016 ASCO - ONS Chemo Standards PDFDocument13 pages2016 ASCO - ONS Chemo Standards PDFSindu SaiNo ratings yet
- Download ebook Diagnostic Pathology Familial Cancer Syndromes 2 full chapter pdfDocument67 pagesDownload ebook Diagnostic Pathology Familial Cancer Syndromes 2 full chapter pdfmildred.maldonado199100% (20)
- Effect of Vitamin D and ω-3 Fatty Acid Supplementation on Risk of Age-Related Macular Degeneration An Ancillary Study of the VITAL Randomized Clinical TrialDocument10 pagesEffect of Vitamin D and ω-3 Fatty Acid Supplementation on Risk of Age-Related Macular Degeneration An Ancillary Study of the VITAL Randomized Clinical TrialAnis RanisNo ratings yet
- Patient Characteristics and Differences in Hospital Readmission RatesDocument10 pagesPatient Characteristics and Differences in Hospital Readmission RatesblahgzNo ratings yet
- Sex Differences in High-Intensity StatinUse Following Myocardial InfarctionDocument9 pagesSex Differences in High-Intensity StatinUse Following Myocardial InfarctionjoNo ratings yet
- 10 2147@VHRM S132556Document12 pages10 2147@VHRM S132556Irma SihotangNo ratings yet
- Samia PDFDocument2 pagesSamia PDFSafiulNo ratings yet
- Professional Dissonance and Burnout in Primary Care A Qualitative StudyDocument7 pagesProfessional Dissonance and Burnout in Primary Care A Qualitative StudyPriyanka MalikNo ratings yet
- jamainternal_anderson_2023_oi_230029_1687982028.79016 (1)Document9 pagesjamainternal_anderson_2023_oi_230029_1687982028.79016 (1)lakshminivas PingaliNo ratings yet
- Download Diagnostic Pathology Familial Cancer Syndromes 2Nd Edition Uk full chapterDocument67 pagesDownload Diagnostic Pathology Familial Cancer Syndromes 2Nd Edition Uk full chapterina.mccrea979100% (8)
- Cancer-And Chemotherapy - Induced Anemia: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Document54 pagesCancer-And Chemotherapy - Induced Anemia: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Hataitap ChonchepNo ratings yet
- Therapeutic Monitoring of Vancomycin IDSADocument29 pagesTherapeutic Monitoring of Vancomycin IDSAArturo ArturoNo ratings yet
- The ASAM Principles of Addiction Medicine - Shannon Miller, Danny Peary-Wolters Kluwer LWW (2018)Document4,444 pagesThe ASAM Principles of Addiction Medicine - Shannon Miller, Danny Peary-Wolters Kluwer LWW (2018)Austin Hall100% (4)
- ProstateDocument204 pagesProstatevonicaNo ratings yet
- Letters To The Editor: Association Between Recreational Cannabis Use and Cardiac Structure and FunctionDocument3 pagesLetters To The Editor: Association Between Recreational Cannabis Use and Cardiac Structure and Functionzionluis007No ratings yet
- Therapeutic Guidelines Monitoring Vancomycin ASHP IDSA PIDSDocument31 pagesTherapeutic Guidelines Monitoring Vancomycin ASHP IDSA PIDSJorge AlvarezNo ratings yet
- Cancer de Prostata NCCNDocument204 pagesCancer de Prostata NCCNGerman FigueroaNo ratings yet
- Vascular Anomalies: A Guide for the Hematologist/OncologistFrom EverandVascular Anomalies: A Guide for the Hematologist/OncologistCameron C. Trenor IIINo ratings yet
- NCCN Guideline Prostate Cancer 2020Document167 pagesNCCN Guideline Prostate Cancer 2020akbarbudhi antonoNo ratings yet
- 2894 FullDocument12 pages2894 FullDesyHandayaniNo ratings yet
- Guía de Diagnóstico y Tratamiento de Las Complicaciones Del Pie Diabético ADA (2018)Document24 pagesGuía de Diagnóstico y Tratamiento de Las Complicaciones Del Pie Diabético ADA (2018)David SilvaNo ratings yet
- Evaluation of Point-of-Care Decision Support For Adult Acne Treatment by Primary Care CliniciansDocument7 pagesEvaluation of Point-of-Care Decision Support For Adult Acne Treatment by Primary Care CliniciansbellaNo ratings yet
- Cancer Rehabilitation: A Concise and Portable Pocket GuideFrom EverandCancer Rehabilitation: A Concise and Portable Pocket GuideJennifer BaimaNo ratings yet
- Jurnal Dr. BobbinDocument11 pagesJurnal Dr. BobbinNhiyar Indah HasniarNo ratings yet
- Pediatric Radiology The Requisites 4Document414 pagesPediatric Radiology The Requisites 4Beng DinNo ratings yet
- OrbidadesDocument6 pagesOrbidadesJose Rodrigues JuniorNo ratings yet
- Grossman Baims Cardiac Catheterization Angiography and Intervention 8th Edition Ebook PDFDocument62 pagesGrossman Baims Cardiac Catheterization Angiography and Intervention 8th Edition Ebook PDFjeffrey.nevarez629100% (37)
- Baugh Et Al-2017-Academic Emergency MedicineDocument9 pagesBaugh Et Al-2017-Academic Emergency MedicineRovanNo ratings yet
- Aspirin + StatinDocument12 pagesAspirin + StatinRenato Schuck SaraivaNo ratings yet
- Cdem 17march WebDocument24 pagesCdem 17march WebRicardo Jonathan Ayala GarciaNo ratings yet
- Tracheotomy On Obese Patient PDFDocument5 pagesTracheotomy On Obese Patient PDFListya ParamitaNo ratings yet
- XlskdsladDocument9 pagesXlskdsladJoãoNo ratings yet
- 10.1016@S1470 20451830909 4Document11 pages10.1016@S1470 20451830909 4Robert ChristevenNo ratings yet
- PIONEERstudy 2016Document12 pagesPIONEERstudy 2016Jose Enrique Valecillos MorenoNo ratings yet
- Guias 2013 CCM PDFDocument44 pagesGuias 2013 CCM PDFDaria ColaliaNo ratings yet
- Nephsap Article Pi i (7)Document94 pagesNephsap Article Pi i (7)doc keddyNo ratings yet
- Breast RiskDocument58 pagesBreast RiskLendyll MangabaNo ratings yet
- Highlights RiskFactors WebPost PDFDocument32 pagesHighlights RiskFactors WebPost PDFteju patneediNo ratings yet
- Nihms866890 UPLOAD 3Document21 pagesNihms866890 UPLOAD 3Peter GardinerNo ratings yet
- C.A.-2Document7 pagesC.A.-2Kasturi SriramNo ratings yet
- Vulvar Cancer: (Squamous Cell Carcinoma)Document60 pagesVulvar Cancer: (Squamous Cell Carcinoma)nuvitaNo ratings yet
- filedate_6091Document67 pagesfiledate_6091melinda.warren862No ratings yet
- Anemia NCCN 2018Document53 pagesAnemia NCCN 2018WassCANNo ratings yet
- Full download book Braunwalds Heart Disease Part 2 A Textbook Of Cardiovascular Medicine Pdf pdfDocument41 pagesFull download book Braunwalds Heart Disease Part 2 A Textbook Of Cardiovascular Medicine Pdf pdfedith.mays178100% (13)
- B-Cell-Spanish HASTA 310Document318 pagesB-Cell-Spanish HASTA 310Ely SalazarNo ratings yet
- First Aid For The Usmle Step 1 2020 Thirtieth EditionDocument61 pagesFirst Aid For The Usmle Step 1 2020 Thirtieth Editionmyrtle.leverenz833100% (39)
- American College of Physicians - MKSAP 19 - Medical Knowledge Self-Assessment Program. Rheumatology-American College of Physicians (2021)Document194 pagesAmerican College of Physicians - MKSAP 19 - Medical Knowledge Self-Assessment Program. Rheumatology-American College of Physicians (2021)Paulo VizcardoNo ratings yet
- Clinical Cancer Research Report 2016Document1 pageClinical Cancer Research Report 2016WeiLinNo ratings yet
- Preface ReprintDocument19 pagesPreface Reprintabaidurrehman0546No ratings yet
- Toxicities of Radiation Treatment for Breast Cancer: Risks and Management StrategiesFrom EverandToxicities of Radiation Treatment for Breast Cancer: Risks and Management StrategiesJean L. WrightNo ratings yet
- Articles: BackgroundDocument11 pagesArticles: BackgroundMr. LNo ratings yet
- Genetic Risk, Adherence To A Healthy Lifestyle, and Coronary DiseaseDocument10 pagesGenetic Risk, Adherence To A Healthy Lifestyle, and Coronary DiseaseNurul Falah KalokoNo ratings yet
- 3020 FullDocument17 pages3020 FullReyhan IsmNo ratings yet
- Diabetes Algorithm Executive SummaryDocument30 pagesDiabetes Algorithm Executive SummaryLuis Alberto Alvarez AnkassNo ratings yet
- Coagulacion Intravascular Diseminada PDFDocument12 pagesCoagulacion Intravascular Diseminada PDFLuis Alberto Alvarez AnkassNo ratings yet
- Evaluation and Management of Chronic Kidney Disease - Synopsis of The Kidney Disease 2012Document7 pagesEvaluation and Management of Chronic Kidney Disease - Synopsis of The Kidney Disease 2012Luis Alberto Alvarez AnkassNo ratings yet
- Acute Diare DiaseseDocument9 pagesAcute Diare DiaseseAnonymous l3X3jf0NPNo ratings yet
- 2013 AHA/ACC Cholesterol Guidelines Flowchart SummaryDocument2 pages2013 AHA/ACC Cholesterol Guidelines Flowchart SummaryLuis Alberto Alvarez AnkassNo ratings yet
- Cholesterol-Lowering Agents Statins-For Everyone? 2019Document10 pagesCholesterol-Lowering Agents Statins-For Everyone? 2019Luis Alberto Alvarez AnkassNo ratings yet
- Ecv Aha Recovery 2016Document73 pagesEcv Aha Recovery 2016Luis Alberto Alvarez AnkassNo ratings yet
- Management of Blood Cholesterol 2019Document2 pagesManagement of Blood Cholesterol 2019Luis Alberto Alvarez AnkassNo ratings yet
- TIA Management-Should TIA Patients Be Admitted? Should TIA Patients Get Combination Antiplatelet Therapy? 2015Document10 pagesTIA Management-Should TIA Patients Be Admitted? Should TIA Patients Get Combination Antiplatelet Therapy? 2015Luis Alberto Alvarez AnkassNo ratings yet
- Guia Aha Asa Stroke PDFDocument77 pagesGuia Aha Asa Stroke PDFAndrea Cayufilo CarmonaNo ratings yet
- Animal Testing Multimodal EssayDocument6 pagesAnimal Testing Multimodal Essayapi-535566007No ratings yet
- NMDs OrientationDocument31 pagesNMDs OrientationRasheedAladdinNGuiomalaNo ratings yet
- COPING MECHANISMS OF STEM STUDENTS AMIDST THE PANDEMICDocument2 pagesCOPING MECHANISMS OF STEM STUDENTS AMIDST THE PANDEMICJeph ReyesNo ratings yet
- 6month Report NewDocument123 pages6month Report NewEmag YonisNo ratings yet
- Jane Dunlap - Exploring Inner Space - Personal Experiences Under LSD-25 PDFDocument224 pagesJane Dunlap - Exploring Inner Space - Personal Experiences Under LSD-25 PDFJimy Robayo100% (1)
- USP Public Health Final Letter Shutdowns V2Document22 pagesUSP Public Health Final Letter Shutdowns V2National Content DeskNo ratings yet
- Collaborative Working RelationshipsDocument15 pagesCollaborative Working RelationshipsMadhabi MondalNo ratings yet
- Karnataka Milk Federation Deepak MB 1 Report 1Document40 pagesKarnataka Milk Federation Deepak MB 1 Report 1udaya kumarNo ratings yet
- Daily House Keeping ChecklistDocument290 pagesDaily House Keeping ChecklistJafar AliNo ratings yet
- 1 - Woodbine DRF BetsDocument19 pages1 - Woodbine DRF BetsCristian HernandezNo ratings yet
- Theories of Juris - American JurisprudenceDocument5 pagesTheories of Juris - American JurisprudenceERICKSKIE23No ratings yet
- Here's What To Know About Cardiovascular-Kidney-Metabolic Syndrome, Newly Defined by The AHADocument2 pagesHere's What To Know About Cardiovascular-Kidney-Metabolic Syndrome, Newly Defined by The AHAluis sanchezNo ratings yet
- B. Choose The Word That Has Different Stress From Others.: Test 6 Part I: Phonetics: (2Pt)Document3 pagesB. Choose The Word That Has Different Stress From Others.: Test 6 Part I: Phonetics: (2Pt)Ngọc VươngNo ratings yet
- IS1.14 Humidification Brochure INT Issue3 WebDocument24 pagesIS1.14 Humidification Brochure INT Issue3 WebHundalHarmanNo ratings yet
- Seminar ReportDocument31 pagesSeminar ReportBitNo ratings yet
- Chapter 1Document15 pagesChapter 1ErikaNo ratings yet
- Open Chest WoundDocument17 pagesOpen Chest WoundDael GerongNo ratings yet
- Evidence Based PracticeDocument3 pagesEvidence Based PracticeTyler HemsworthNo ratings yet
- Attitudes and Behaviour of School Students Towards Global Warming - A Cross Sectional Observational StudyDocument5 pagesAttitudes and Behaviour of School Students Towards Global Warming - A Cross Sectional Observational StudyIOSRjournalNo ratings yet
- The Hierarchical Taxonomy of Psychopathology (Hitop) : A Quantitative Nosology Based On Consensus of EvidenceDocument29 pagesThe Hierarchical Taxonomy of Psychopathology (Hitop) : A Quantitative Nosology Based On Consensus of EvidenceJose A RodasNo ratings yet
- Saudi License Exam - SLE (DENTAL Test Papers) Set-1Document108 pagesSaudi License Exam - SLE (DENTAL Test Papers) Set-1Adeel Ahmad86% (22)
- Electronic Cigarettes A Primer For CliniciansDocument10 pagesElectronic Cigarettes A Primer For CliniciansGina Marcela Chaves HenriquezNo ratings yet
- Patient Satisfaction With Hospital Care and Nurses in England: An Observational StudyDocument10 pagesPatient Satisfaction With Hospital Care and Nurses in England: An Observational StudySelfa YunitaNo ratings yet
- Diverifikasi DPJP AgustusDocument6 pagesDiverifikasi DPJP AgustusKadek candraNo ratings yet
- E4 SubtypesDocument26 pagesE4 SubtypesJuliaNo ratings yet
- Certification Study GuideDocument482 pagesCertification Study GuideHosam Gomaa100% (8)
- CBC HILOT WELLNESS 21stDocument64 pagesCBC HILOT WELLNESS 21stjazzy mallari100% (3)
- A03 - Mr. Wasim Akhter - PSC Karamat Chowki CC - 9, Labour Chouraha, Kareli, AllahabadDocument3 pagesA03 - Mr. Wasim Akhter - PSC Karamat Chowki CC - 9, Labour Chouraha, Kareli, AllahabadMohd Asad AbbasNo ratings yet
- Edukasi Program Keluarga Berencana (KB) Pada Wanita Usia Subur Selama Masa Pandemi Covid 19Document5 pagesEdukasi Program Keluarga Berencana (KB) Pada Wanita Usia Subur Selama Masa Pandemi Covid 19Puja Ayesha HasibuanNo ratings yet
- Diabetics PrescriptionDocument1 pageDiabetics PrescriptionSunil HNo ratings yet