Professional Documents
Culture Documents
Optic Nerve Hyperintensity Correlates with Visual Impairment in Pituitary Macroadenoma
Uploaded by
Malekseuofi مالك السيوفيOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Optic Nerve Hyperintensity Correlates with Visual Impairment in Pituitary Macroadenoma
Uploaded by
Malekseuofi مالك السيوفيCopyright:
Available Formats
Optic Nerve Hyperintensity on T2-Weighted
Images among Patients with Pituitary
ORIGINAL
Macroadenoma: Correlation with Visual
RESEARCH Impairment
A.M. Tokumaru PURPOSE: Visual acuity (VA) disturbance other than field defect is important in evaluating patients with
I. Sakata pituitary macroadenoma. The purpose of this study was to evaluate MR imaging appearances of optic
nerves in patients with pituitary macroadenoma and to ascertain whether visual impairment was
H. Terada
correlated with abnormality in optic nerve signal intensity.
S. Kosuda
PATIENTS AND METHODS: Twenty-seven patients with pituitary macroadenoma were examined. Optic
H. Nawashiro
nerves were evaluated on T2-weighted images and correlations of signal intensity abnormality with VA
M. Yoshii disturbance, visual field disturbance, degree of optic chiasm compression, pathologic findings of
surgical specimen, and disease duration were statistically analyzed. Correlations between recovery of
VA after treatment and the above-mentioned factors were also determined.
RESULTS: Coronal T2-weighted images demonstrated unilateral optic nerve hyperintensity lesions in 9
patients. Bilateral signal intensity abnormality of the optic nerve was seen in 5 patients. Signal intensity
abnormality of the optic nerve was seen at the site of compression and in the ventral side of the tumor.
These patients did not demonstrate signal intensity abnormality posterior to the tumor. Presence of
such signal intensity abnormalities was correlated with the degree of optic chiasmal compression and
with VA disturbance. Recovery of VA after treatment was correlated with disease duration.
CONCLUSION: Hyperintensity of the optic nerves ventral to the pituitary macroadenoma was associated
with VA impairment. Recovery of VA after treatment was correlated with disease duration. MR imaging of
the optic nerves can provide valuable information for management of pituitary macroadenoma.
I n some patients with pituitary macroadenoma, visual acuity
(VA) diminishes despite the existence of no field defect
other than bitemporal hemianopia. This clinical information
treated surgically at the National Defense Medical College between
April 1999 and November 2003. All MR examinations were per-
formed by using a 1.5T system. We used fast spin-echo sequences
is very important in patient management; however, no pub- for T2-weighted (3500/110/2) and T1-weighted (500/15/1) im-
lished reports have analyzed the relationship between VA dis- ages. Three-millimeter-thick sections were obtained in the coronal
turbance and MR imaging findings of the optic nerves of the and sagittal planes with a 256 ⫻ 512 acquisition matrix. All images
patients with the pituitary macroadenoma. In this study, the were blindly reviewed by 2 radiologists, focusing on the presence
authors used T2-weighted MR imaging to investigate signal of abnormal signal intensity in the optic nerves ventral to the
intensity abnormality of the optic nerves and statistically ana- tumor, at the site of compression, and dorsal to the tumor. We also
lyzed the relationship between this and factors including the classified degree of optic chiasm compression into 3 grades as
degree of optic chiasm compression, disease duration, degree follows: (⫺) no compression; (⫹) compression of less than half of
of VA disturbance, and tumor histopathology. the optic chiasm; and (⫹⫹) compression with severe thinning.
Hyperintensity of the optic nerves was frequently detected Signal intensity abnormality of the optic nerve was defined as ab-
among patients with diminished VA. Among those with long normality involving not only the area around the optic nerve, but
disease duration and prolonged signal intensity abnormality, also the septum (⫹). In patients with (⫹) or (⫹⫹) compression,
improvements in VA disturbance tended to be poor, which we also evaluated the location of the tumor in relation to the optic
suggests the possibility of degeneration of optic nerves caused nerve and optic chiasm. Cephalocaudal diameter of each tumor
not only by compression-induced edema, but also by com- was also measured
pression of the arteries, veins, and capillary networks in the Visual signs (visual field defect and VA) were evaluated by an
optic chiasm. ophthalmologist. Twenty-four patients underwent surgical proce-
dures, and histologic confirmation of the diagnosis was obtained in
Patients and Methods each case.
We reviewed pre- and postoperative MR images from 27 con-
A Mann-Whitney U test was used for statistical analysis of the
secutive patients with pituitary macroadenoma, 24 of whom were
relationships between signal intensity abnormality and tumor size,
Received August 1, 2004; accepted after revision July 23, 2005.
degree of chiasm compression, histology, VA disturbance, and disease
duration. Correlations between recovery of VA after treatment and
From the Department of Radiology (A.M.T.), Tokyo Metropolitan Geriatric Hospital, Tokyo
Japan; Departments of Radiology (I.S., S.K.) and Neurosurgery (H.N.), National Defense the above-mentioned factors were also ascertained.
Medical College, Saitama Japan; Department of Ophthalmology (M.Y.), National Rehabil-
itation Center for Persons with Disabilities, Saitama Japan; and The 2nd Department of
Radiology (H.T.), Toho University School of Medicine, Tokyo Japan. Results
Address correspondence to Aya M.Tokumaru, Department of Radiology, Tokyo Metropolitan Patient clinical data are summarized in Table 1. The results
Geriatric Hospital, 35-2 Sakae-Cho, Itabashi-Ku, Tokyo, Japan 173-0015. are shown in Figs 1– 4.
250 Tokumaru 兩 AJNR 27 兩 Feb 2006 兩 www.ajnr.org
Optic tract hyperintensity on T2-weighted images among patients with pituitary macroadenoma: correlation with visual impairment
Patient No./
Age (y)/Sex Duration Size (mm) OC AS VAD VFD Pathology IAT
1/36/M 2 mo 18 ⫺ ⫺ ⫺ ⫹
2/61/M 9y 23.7 ⫹ ⫺ ⫹ (rt 0.7, lt blind) ⫹ PA ⫺
3/42/F 16 mo 26.5 ⫹⫹ ⫹ ⫹ (rt 0.02, lt 1.5) ⫹ PA (corticotro) ⫺
4/38/F 10 mo 14 ⫺ ⫺ ⫺ ⫹
5/40/M 6 mo 35 ⫹⫹ ⫹ ⫹ (rt 0.07, lt 0.05) ⫹ PA (null) ⫺
6/55/F 4y 46 ⫹⫹ ⫹ ⫹ (rt 0.06, lt 0.06) ⫹ PA (chromophobe) ⫺
7/65/F 2 mo 13 ⫺ ⫺ ⫺ ⫹ PA (null)
8/74/M 18 mo 16.4 ⫹ ⫹ ⫹ (rt 0.7, lt 0.4) ⫹ PA (null) ⫺
9/54/F 3 mo 27 ⫹ ⫹ ⫹ (rt 0.06, lt 0.1) ⫹ PA (nonfunctioning) ⫹ (rt 1.2, lt 0.8)
10/65/M 2 mo 13 ⫺ ⫹ ⫹ (rt light sense) ⫹ Pituitary carcinoma ⫺
11/59/F 14 mo 35 ⫹⫹ ⫹ ⫹ (rt 0.3, lt 0.9) ⫹ PA (null) ⫺
12/55/M 3 mo 22 ⫹⫹ ⫹ ⫹ (rt 0.5, lt 0.1) ⫹ PA ⫹ (rt 1.0, lt 1.0)
13/41/F 19 mo 25 ⫹⫹ ⫹ ⫹ (hand sense) ⫹ PA (null) ⫺
14/37/F 3 mo 16 ⫺ ⫺ ⫺ ⫹
15/70/F 6 mo 18 ⫹ ⫹ ⫹ (rt 0.1, lt blind) ⫺
16/27/M 6 mo 15 ⫺ ⫹ ⫹ (finger sense) ⫹ PA (chromophobe) ⫹ (rt 0.7, lt 0.9)
17/58/M 26 mo 24 ⫹⫹ ⫹ ⫹ (rt 1.5, lt 0.4) ⫺ PA (null) ⫺
18/21/F 8 mo 30 ⫹ ⫺ ⫺ ⫹ PA (GH) ⫺
19/50/F 10 y 51 ⫹⫹ ⫹ ⫹ (rt 0.03, lt 0.1) ⫹ PA(FSH-LH) ⫺
20/74/F 1.5 mo 18 ⫺ ⫹ ⫹ (lt light sense) ⫺ PA (prolactinoma) ⫹ (rt 0.8, lt 0.4)
21/66/F 2 mo 15 ⫺ ⫺ ⫺ ⫺ PA (null)
22/63/M 2 mo 23.7 ⫹⫹ ⫹ ⫹ (rt 0.1, lt 0.7) ⫹ PA (chromophobe) ⫹ (rt 0.7, lt 0.8)
23/54/F 3 mo 13 ⫺ ⫺ ⫺ ⫺ PA
24/56/F 3 mo 20 ⫺ ⫺ ⫺ ⫺ PA
25/45/M 2 mo 16 ⫺ ⫺ ⫺ ⫹ PA (chromophobe)
26/36/M 2 mo 12.2 ⫺ ⫺ ⫺ ⫺
27/50/M 3 mo 16 ⫹⫹ ⫹ ⫹ (rt 0.9, lt 0.3) ⫹ PA (GH) ⫹ (rt 0.9, lt 0.7)
Note.—OC indicates optic chiasm compression; AS, abnormal signal in optic nerve; VAD, visual acuity disturbance; VFD, visual field disturbance; IAT, improvement of visual acuity after
HEAD & NECK
treatment; PA, pituitary adenoma; FSH-LH, follicle stimulating hormone-luteinizing hormone; GH, growth hormone.
Coronal T2-weighted images demonstrated unilateral op- roids were administered from an early stage as a result of signal
tic nerve hyperintensity lesions in 9 patients. Bilateral signal intensity abnormality in optic nerves on MR imaging and pap-
intensity abnormality of the optic nerve was seen in 5 patients. illary edema, leading to an improvement in VA. Degree of
Signal intensity abnormality of optic nerve was seen at the improvement in VA was significantly correlated with disease
ORIGINAL RESEARCH
compression site and at the ventral side of the tumor. No pa- duration but not with any other factors in this study.
tients demonstrated signal intensity abnormality posterior to
the tumor. Discussion
Signal intensity normalized in 9 of 21 patients after surgery The literature contains several reports concerning edema-
or other treatment. like change along the optic pathway in association with supra-
Presence of optic nerve hyperintensity lesions was corre- sellar tumors such as craniopharyngioma, pituitary adenoma,
lated to the degree of optic chiasm compression and to the and meningioma.1-2 Hyperintensity in the optic nerve ventral
presence of diminished VA (P ⬍ .01). In all patients with to pituitary macroadenoma, however, has not been reported.
(⫹⫹) optic chiasm compression, the optic nerve was com- As far as the management of pituitary macroadenoma is con-
pressed beyond 1 cm anterior and posterior to the optic chi- cerned, VA disturbance is an important factor, and, as a result,
asm, and tumor location exhibited no significant correlation related diagnostic imaging findings are also of consequence.7
to the presence or absence of optic nerve signal intensity ab- In the present study, the relationship between optic nerve sig-
normality; however, no correlation between hyperintensity nal intensity abnormality, degree of optic chiasm compres-
and tumor size was demonstrated in this study. Other than in sion, and the presence of VA disturbance were statistically an-
patients with a tumor size ⬍2 cm, the results suggested the alyzed. The results suggested that prolonged compression
need to consider type II error. Hence, the relationship to tu- caused signal intensity abnormality of the optic nerve and VA
mor size might be clarified by studying greater numbers of disturbance. Consequently, decompression should be per-
patients. formed promptly in patients demonstrating compression of
After surgery and other forms of treatment, size of the tu- the optic chiasm or signal intensity abnormality of the optic
mor diminished and compression of the optic chiasm re- nerve.
solved. Of patients with improved VA, signal intensity abnor- Signal intensity abnormality persists after decompression,
mality improved in 4 patients but persisted in 5 cases (Fig. 5). can lead to atrophy, and is associated with a high frequency of
Atrophy of optic nerves was seen on MR imaging in 3 patients VA disturbance and thus appears to represent changes that
in whom VA abnormalities persisted on ophthalmologic ex- extend beyond edema. The mechanism by which pituitary
amination (Fig. 6). In one case with improved VA, although macroadenoma appears to damage the optic nerve and impair
the degree of compression to the optic chiasm was mild, ste- VA is unclear. VA disturbance, however, cannot be explained
AJNR Am J Neuroradiol 27:250 –254 兩 Feb 2006 兩 www.ajnr.org 251
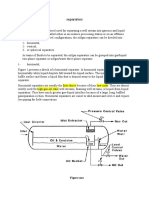
Fig 1. Degree of optic chiasmal compression. A, No compression to optic chiasma (⫺).
B, Compression of less than half of the optic chiasm (⫹). C, Compression with marked
thinning (⫹⫹).
fects, however, are extremely rare.3 As reported by Hoyt, how-
ever, compression disrupts the arterial supply, and long-term
compression of the arteries, veins, and capillary networks in
the optic chiasm leads to stagnant anoxia, thus resulting in a
characteristic bitemporal visual field defect.4 Signal intensity
abnormality in the optic nerves was considered to represent
damage by compression and stagnant anoxia at the optic chi-
solely in terms of mechanical damage due to compression.
Because the axons for the entire superior visual field course
through the inferior aspect of the optic nerves and chiasm,
compression of these structures from below would be ex-
pected to produce a defect in the entire upper field. Such de- Fig 3. Correlation between abnormal signal intensity of optic nerve and optic chiasm
compression.
Fig 4. Correlation between abnormal signal intensity of optic nerve and improvement after
Fig 2. Correlation between abnormal signal intensity of optic nerve and tumor size. treatment of VA.
252 Tokumaru 兩 AJNR 27 兩 Feb 2006 兩 www.ajnr.org
Fig 5. Case 3, a 42-year-old woman whose disease duration was 6 months. Right VA disturbance was recognized (right VA ⫽ 0.02; left VA ⫽ 1.5). A, Pituitary macroadenoma markedly
compressed the optic chiasm especially the right side (white arrows ). B–E, Hyperintensity was recognized in the right optic nerve on T2-weighted image (arrows ). F–H, Hyperintensiy in
the right optic nerve lasted for 2 years after the tumor reduction (arrows ).
asm and Wallerian degeneration in the ventral side of the optic disease duration and improvement in VA. We also showed
chiasm. that it is meaningful to be able to visually assess compression
With regard to VA disturbance caused by compression of the optic chiasm and optic nerves and accurately examine
near the optic chiasm, several studies have reported that this the optic nerves.
was caused by optic chiasm compression from the internal In the present study, signal intensity abnormality did not
carotid artery,5,6 but few studies have compared imaging find- advance to the optic pathway posterior to the tumor, even in
ings.5-7 The present study on tumor-induced compression patients in whom compression advanced posterior to the optic
demonstrated a statistically significant correlation between chiasm. Moreover, tumor location in relation to the optic chi-
AJNR Am J Neuroradiol 27:250 –254 兩 Feb 2006 兩 www.ajnr.org 253
Fig 6. Case 17, a 58-year-old man, whose disease duration from the initial examination to the operation
was 26 months. VA was not stable, though fixed VA disturbance was not recognized on the initial
examination. A, Pituitary adenoma compressed the optic chiasm. B, Hyperintensiy of the optic nerve
was not shown (arrows) on the initial examination. C, Right-side perioptic subarachnoid space dilated
slightly on the initial examination (arrow). D and E, Tumor reduction was performed 26 months after the
initial examination. Hyperintensity was shown in the bilateral optic nerve ventral to the optic chiasm (D,
white arrows) and bilateral perioptic subarachnoid space dilated markedly (E, white arrows), probably
representing atrophic change of the optic nerves.
20), signal intensity abnormality was localized to the left pre-
chiasmatic region and the perioptic subarachnoid space was
enlarged, resulting in symptoms resembling acute optic neu-
ritis. In this patient, pituitary apoplexy was suspected, and
microhemorrhage could have caused chemical inflammation.
Hence, optic nerve degeneration due to long-term compres-
sion was not the sole factor in VA impairment. In other words,
it is necessary to assess etiology in each patient. Furthermore,
in this patient, as a result of imaging findings and papillary
edema, steroids were administered from an early stage, leading
asm and optic nerves exhibited no correlation to signal inten- to an improvement in VA. This case emphasized the impor-
sity abnormality. In craniopharyngioma arising in the supra- tance of carefully analyzing imaging findings.
chiasmal region, though, edema has been known to occur in
the optic pathway posterior to a tumor, and, as a result, we References
believe that it will be necessary to further investigate the rela- 1. Nagahata M, Hosoya T, Kayama T, et al. Edema along the optic tract: useful MR
findings for the diagnosis of craniopharyngiomas. AJNR Am J Neuroradiol
tionship of signal intensity abnormality to tumor location. 1998;19:1753–57
In case 17 (Fig. 6), only signal intensity abnormality of the 2. Saeki N, Uchino Y, Murai H, et al. MR imaging study of edema-like change
perioptic subarachnoid space was initially observed, and, though along the optic tract in patients with pituitary region tumors. AJNR Am J
Neuroradiol 2003;24:336 – 42
VA was not stable, surgery was delayed for various reasons and 3. Miller NR. Tumors of the pituitary gland. In: Walsh and Hoyt’s clinical neuro-
optic atrophy eventually developed. In other words, signal inten- opthalmology. 4th ed. Philadelphia: Willliams and Wilkins; 1424 – 86
sity abnormality can lead to severe atrophy, which suggests the 4. Hoyt WF. Correlative function anatomy of the optic chiasm. Clin Neurosurg
1970;17:189 –208
importance of performing surgery at an appropriate stage. Be- 5. Ogata N, Imaizumi M, Kurokawa H, et al. Optic nerve compression by normal
cause VA improvement is closely correlated to disease stage, it is carotid artery in patients with normal tension glaucoma. Br J Ophthalmol
important to recommend expedient decompression. 2005;89:174 –79
6. Kawasaki A, Puruvin VA. Photophobia as a the presenting visual symptom of
VA disturbance was marked from the beginning in some chiasmal compression. J Neuroophthalmol 2002;22:3– 8
patients despite mild compression. In one such patient (case 7. Forooan R. Chiasmal syndrome. Curr Opin Ophthalmol 2003;14:325–31
254 Tokumaru 兩 AJNR 27 兩 Feb 2006 兩 www.ajnr.org
You might also like
- Presentation on Chancroid: Bacterial STI Causes Painful Genital UlcersDocument12 pagesPresentation on Chancroid: Bacterial STI Causes Painful Genital UlcersBikash Sah0% (1)
- Work Permit Renewal Application FormDocument2 pagesWork Permit Renewal Application FormyamojodnabNo ratings yet
- Spec MRI Distinguish Acue TM of NMOSD N Infarction. Kister Et Al 2015Document21 pagesSpec MRI Distinguish Acue TM of NMOSD N Infarction. Kister Et Al 2015Ido BramantyaNo ratings yet
- Seguridad Social en AlemaniaDocument8 pagesSeguridad Social en AlemaniaMichael RojasNo ratings yet
- Cervical Facet OedemaDocument6 pagesCervical Facet OedemaMarco PeroliNo ratings yet
- Bone Marrow Edema Syndrome 1Document8 pagesBone Marrow Edema Syndrome 1drbane123No ratings yet
- 264 2007 Article 320Document5 pages264 2007 Article 320Sibu KashyapNo ratings yet
- J Wneu 2010 08 021Document9 pagesJ Wneu 2010 08 021Boukhenoufa Mouhammed ElamineNo ratings yet
- Kudo 2022 Clinical Relevance of UltrasonograpDocument9 pagesKudo 2022 Clinical Relevance of UltrasonograpMayra Nuria Rojas RojasNo ratings yet
- Utility of Mri in The Early and Accurate Diagnosis of Avascular Necrosis of Hip JointDocument9 pagesUtility of Mri in The Early and Accurate Diagnosis of Avascular Necrosis of Hip JointDenis AlexandruNo ratings yet
- Hipertensão IntracranianaDocument6 pagesHipertensão IntracranianaFelipe Stoquetti de AbreuNo ratings yet
- Uso de Ultrasonografia para Medial EpycondilitisDocument5 pagesUso de Ultrasonografia para Medial EpycondilitisSantiago BianchiNo ratings yet
- Cortical Laminar Necrosis Findings on SWI in Pediatric PatientsDocument4 pagesCortical Laminar Necrosis Findings on SWI in Pediatric PatientsSulaiman Al SheikhNo ratings yet
- MRI, DWI, and MRS features of an adult intracranial yolk sac tumorDocument4 pagesMRI, DWI, and MRS features of an adult intracranial yolk sac tumortiaraNo ratings yet
- Magnetic Resonance Imaging - 2013 - Ignjatovi - Brain Iron MRI A Biomarker For Amyotrophic Lateral SclerosisDocument8 pagesMagnetic Resonance Imaging - 2013 - Ignjatovi - Brain Iron MRI A Biomarker For Amyotrophic Lateral SclerosisMahima vermaNo ratings yet
- Hemimegalencephaly: A Study of Abnormalities Occurring Outside The Involved HemisphereDocument5 pagesHemimegalencephaly: A Study of Abnormalities Occurring Outside The Involved Hemisphereapi-148100258No ratings yet
- Meta-Analysis On Continuous Nerve Monitoring in ThyroidectomiesDocument13 pagesMeta-Analysis On Continuous Nerve Monitoring in ThyroidectomiesazharbattooNo ratings yet
- Neurosciences 26-4-392Document4 pagesNeurosciences 26-4-392esinsubozatliNo ratings yet
- TMP 61 BFDocument9 pagesTMP 61 BFFrontiersNo ratings yet
- Fnhum 16 778347Document5 pagesFnhum 16 778347Josue GarciaNo ratings yet
- Sca IiDocument8 pagesSca IiAlfredo Enrique Marin AliagaNo ratings yet
- A Child With Acute Eyelid Edema and Proptosis: JAMA Ophthalmology Clinical ChallengeDocument2 pagesA Child With Acute Eyelid Edema and Proptosis: JAMA Ophthalmology Clinical ChallengePatriciaNo ratings yet
- Ajnr A5528 FullDocument9 pagesAjnr A5528 FullMehranNasrallaNo ratings yet
- MR Imaging of Traumatic Lesions of TheDocument4 pagesMR Imaging of Traumatic Lesions of ThelazacaixNo ratings yet
- Neuroimage: Clinical: A B A A C C A C A C A DDocument9 pagesNeuroimage: Clinical: A B A A C C A C A C A Dro111111No ratings yet
- MRI in Evaluating AdenocarsinomaDocument5 pagesMRI in Evaluating AdenocarsinomaAnggit Adhi PrasetyaNo ratings yet
- 1369 Full PDFDocument9 pages1369 Full PDFIqbal AbdillahNo ratings yet
- Madhusudhan2008 Article ClinicalExaminationMRIAndArthrDocument6 pagesMadhusudhan2008 Article ClinicalExaminationMRIAndArthrMaddy WolsmenNo ratings yet
- MRI Findings of 26 Patients With Parsonage-Turner SyndromeDocument6 pagesMRI Findings of 26 Patients With Parsonage-Turner SyndromeTopciu Mihaela FeliciaNo ratings yet
- Stroke-2002-Gerraty-2019-24Document7 pagesStroke-2002-Gerraty-2019-24Fauzan IndraNo ratings yet
- Thoracic Anterior Spinal Cord Adhesion Syndrome Imaging FindingsDocument7 pagesThoracic Anterior Spinal Cord Adhesion Syndrome Imaging Findingspaulina_810100% (1)
- Distinguishing Benign Notochordal Cell Tumors From Vertebral ChordomaDocument9 pagesDistinguishing Benign Notochordal Cell Tumors From Vertebral ChordomaOM JHANo ratings yet
- Neuroimage: Clinical: ArticleinfoDocument8 pagesNeuroimage: Clinical: ArticleinfoROHITNo ratings yet
- 027 Optokinetic Nystagmus and Sensorial Tests in Different Types of StrabismusDocument1 page027 Optokinetic Nystagmus and Sensorial Tests in Different Types of StrabismusExo L1485No ratings yet
- 2017 - Morris Et Al-AnnotatedDocument7 pages2017 - Morris Et Al-AnnotatedCemal GürselNo ratings yet
- Osteoradionecrosis of The Upper Cervical Spine - MR Imaging Following Radiotherapy For Nasopharyngeal CarcinomaDocument7 pagesOsteoradionecrosis of The Upper Cervical Spine - MR Imaging Following Radiotherapy For Nasopharyngeal CarcinomaakreditasiNo ratings yet
- Sipola. Detection and Quantification of Rotator Cuff Tears With Ultrasonography and Magnetic Resonance Imaging - A ProsDocument9 pagesSipola. Detection and Quantification of Rotator Cuff Tears With Ultrasonography and Magnetic Resonance Imaging - A Prossteven saputraNo ratings yet
- NuropathologyDocument1 pageNuropathologykib240309No ratings yet
- 0068KJR - KJR 10 121Document8 pages0068KJR - KJR 10 121Astrid GayatriNo ratings yet
- Imaging in RadiculopathyDocument17 pagesImaging in RadiculopathyFerdy DamaraNo ratings yet
- kiuru2002Document6 pageskiuru2002Laraib KanwalNo ratings yet
- Imaging and Surgical Treatment of Invasive MeningiomaDocument6 pagesImaging and Surgical Treatment of Invasive Meningiomaniluhputu asrinidewiNo ratings yet
- Vestibular Neuritis Affects Both Superior and Inferior Vestibular NervesDocument10 pagesVestibular Neuritis Affects Both Superior and Inferior Vestibular NervesSabina BădilăNo ratings yet
- Pi Is 0007122605001840Document7 pagesPi Is 0007122605001840Annisa Fitri AnggrainiNo ratings yet
- Diagnostic Utility of Ultrasonography Versus Nerve Conduction Studies in Mild Carpal Tunnel SyndromeDocument10 pagesDiagnostic Utility of Ultrasonography Versus Nerve Conduction Studies in Mild Carpal Tunnel SyndromeJP ChenNo ratings yet
- Chemicalshift MRIDocument4 pagesChemicalshift MRIshreyahospital.motinagarNo ratings yet
- The Diagnostic Relationship With Clinical and Neuroimaging Studies of Patients With Back PainDocument5 pagesThe Diagnostic Relationship With Clinical and Neuroimaging Studies of Patients With Back PainCentral Asian StudiesNo ratings yet
- Spinal Cord Injury Without Radiographic Abnormality in AdultsDocument4 pagesSpinal Cord Injury Without Radiographic Abnormality in AdultsAle ParraNo ratings yet
- Veterinary Internal Medicne - 2021 - Vezzosi - The Mitral INsufficiency Echocardiographic Score A Severity ClassificationDocument7 pagesVeterinary Internal Medicne - 2021 - Vezzosi - The Mitral INsufficiency Echocardiographic Score A Severity Classificationmv.sanchez.irvingNo ratings yet
- Visual Acuity After Gamma-Knife Radiosurgery of Choroidal MelanomasDocument7 pagesVisual Acuity After Gamma-Knife Radiosurgery of Choroidal Melanomasmaria alejandra garcia moncadaNo ratings yet
- Management of Atypical Cranial Meningiomas Part 2Document8 pagesManagement of Atypical Cranial Meningiomas Part 2Edie DelgadoNo ratings yet
- Research Article: Prognostic Factors For Visual Outcome in Traumatic Cataract PatientsDocument7 pagesResearch Article: Prognostic Factors For Visual Outcome in Traumatic Cataract PatientsMarcella PolittonNo ratings yet
- Basal Gangila CahngesDocument12 pagesBasal Gangila CahngesJakkani RavikanthNo ratings yet
- Clinical Outcomes of Neonatal Hypoxic Ischemic Encephalopathy Evaluated With Diffusion-Weighted Magnetic Resonance ImagingDocument6 pagesClinical Outcomes of Neonatal Hypoxic Ischemic Encephalopathy Evaluated With Diffusion-Weighted Magnetic Resonance ImagingDrsandy SandyNo ratings yet
- MRI SeizuresDocument7 pagesMRI SeizuresMarco MalagaNo ratings yet
- Cervical MyelpathyDocument12 pagesCervical MyelpathyannamarianeuroNo ratings yet
- Zhang Et Al-2016-Journal of Magnetic Resonance ImagingDocument8 pagesZhang Et Al-2016-Journal of Magnetic Resonance ImagingMarisol AcostaNo ratings yet
- Atypical Teratoid:Rhabdoid Tumors in Adult Patients: CT and MR Imaging FeaturesDocument7 pagesAtypical Teratoid:Rhabdoid Tumors in Adult Patients: CT and MR Imaging FeaturesMauro CampelloNo ratings yet
- FFFFDocument4 pagesFFFFAby SuryaNo ratings yet
- Sensitivity and Specificity of Ultrasonography in Early Diagnosis of Metatarsal Bone Stress Fractures A Pilot Study of 37 PatientsDocument5 pagesSensitivity and Specificity of Ultrasonography in Early Diagnosis of Metatarsal Bone Stress Fractures A Pilot Study of 37 PatientsJUAN DIEGONo ratings yet
- Jurnal r4Document9 pagesJurnal r4Rezkina Azizah PutriNo ratings yet
- Mascard2015 ABCs Vs UBCsDocument9 pagesMascard2015 ABCs Vs UBCsWemdi Priya PrasetyaNo ratings yet
- The Clinical Outcomes of Endovenous Microwave and Laser Ablation For Varicose VeinsDocument6 pagesThe Clinical Outcomes of Endovenous Microwave and Laser Ablation For Varicose VeinsMalekseuofi مالك السيوفيNo ratings yet
- CryothyrapyDocument10 pagesCryothyrapyMalekseuofi مالك السيوفيNo ratings yet
- One-Year Duplex Ultrasound-Assessed Closure Outcomes of Percutaneous Endovenous Microwave Ablation For The Treatment of VV of The Lower LimbsDocument6 pagesOne-Year Duplex Ultrasound-Assessed Closure Outcomes of Percutaneous Endovenous Microwave Ablation For The Treatment of VV of The Lower LimbsMalekseuofi مالك السيوفيNo ratings yet
- Endovenous Microwave Ablation of Great Saphenous VeinDocument3 pagesEndovenous Microwave Ablation of Great Saphenous VeinMalekseuofi مالك السيوفيNo ratings yet
- NICE - Percutaneous Ultrasound-Guided Microwave AblationDocument5 pagesNICE - Percutaneous Ultrasound-Guided Microwave AblationMalekseuofi مالك السيوفيNo ratings yet
- On Demand Pediatric SkullDocument20 pagesOn Demand Pediatric SkullMalekseuofi مالك السيوفيNo ratings yet
- Endometrial CarcinomaDocument73 pagesEndometrial CarcinomaMalekseuofi مالك السيوفيNo ratings yet
- Evaluation of Microwave Ablation of Liver Malignancy With Enabled Constant Spatial Energy Control To Achieve A Predictable Spherical Ablation ZoneDocument10 pagesEvaluation of Microwave Ablation of Liver Malignancy With Enabled Constant Spatial Energy Control To Achieve A Predictable Spherical Ablation ZoneMalekseuofi مالك السيوفيNo ratings yet
- Targeted Percutaneous Microwave Ablation at The Pulmonary Lesion Combined With Mediastinal Radiotherapy With or Without Concurrent Chemotherapy inDocument8 pagesTargeted Percutaneous Microwave Ablation at The Pulmonary Lesion Combined With Mediastinal Radiotherapy With or Without Concurrent Chemotherapy inMalekseuofi مالك السيوفيNo ratings yet
- Imp Repeated Percutaneous MicrowaveDocument6 pagesImp Repeated Percutaneous MicrowaveMalekseuofi مالك السيوفيNo ratings yet
- Image and Pathological Changes After Microwave Ablation of Breast CancerDocument7 pagesImage and Pathological Changes After Microwave Ablation of Breast CancerMalekseuofi مالك السيوفيNo ratings yet
- Safety and Efficiency of Microwave Ablation For Recurrent and Persistent Secondary HyperparathyroidismDocument7 pagesSafety and Efficiency of Microwave Ablation For Recurrent and Persistent Secondary HyperparathyroidismMalekseuofi مالك السيوفيNo ratings yet
- Ultrasound-Guided Microwave Ablation A Promising Tool in Management of Benign Breast TumoursDocument9 pagesUltrasound-Guided Microwave Ablation A Promising Tool in Management of Benign Breast TumoursMalekseuofi مالك السيوفيNo ratings yet
- US-guided Microwave Ablation Shown Safe and Effective for Treating Hyperparathyroidism in Patients with Kidney FailureDocument9 pagesUS-guided Microwave Ablation Shown Safe and Effective for Treating Hyperparathyroidism in Patients with Kidney FailureMalekseuofi مالك السيوفيNo ratings yet
- Microwave Ablation in Primary and Secondary Liver Tumours Technical and Clinical ApproachesDocument11 pagesMicrowave Ablation in Primary and Secondary Liver Tumours Technical and Clinical ApproachesMalekseuofi مالك السيوفيNo ratings yet
- Inferior Concha Bullosa Connected With Maxilary SinusDocument3 pagesInferior Concha Bullosa Connected With Maxilary SinusMalekseuofi مالك السيوفيNo ratings yet
- Comparison of Microwave Ablation and Hepatic Resection For Hepatocellular CarcinomaDocument11 pagesComparison of Microwave Ablation and Hepatic Resection For Hepatocellular CarcinomaMalekseuofi مالك السيوفيNo ratings yet
- 2020 Thermal Ablation in The Management of Colorectal LiverDocument10 pages2020 Thermal Ablation in The Management of Colorectal LiverMalekseuofi مالك السيوفيNo ratings yet
- IS - Safe T Centesis Catheter Drainage - BR - ENDocument6 pagesIS - Safe T Centesis Catheter Drainage - BR - ENMalekseuofi مالك السيوفيNo ratings yet
- Microwave Ablation For Palliation of Bone MetastasesDocument4 pagesMicrowave Ablation For Palliation of Bone MetastasesMalekseuofi مالك السيوفيNo ratings yet
- MWV VS Radio VS CryoDocument7 pagesMWV VS Radio VS CryoMalekseuofi مالك السيوفيNo ratings yet
- CA A Cancer J Clinicians - 2022 - Miller - Cancer Treatment and Survivorship Statistics 2022Document28 pagesCA A Cancer J Clinicians - 2022 - Miller - Cancer Treatment and Survivorship Statistics 2022Malekseuofi مالك السيوفيNo ratings yet
- Septic Abortion PDFDocument4 pagesSeptic Abortion PDFmariachrismayaniNo ratings yet
- Mitsubishi Galant 4g63 Engine Repair ManualDocument29 pagesMitsubishi Galant 4g63 Engine Repair ManualMoaed Kanbar100% (1)
- 02 - Purulent Inflammatory DiseaseDocument60 pages02 - Purulent Inflammatory Diseaseshekhawatyuvraj051No ratings yet
- Aire Acondicionado Mazda 3 2006Document2 pagesAire Acondicionado Mazda 3 2006Jhon ConnorNo ratings yet
- Chemistry Units 8 12Document29 pagesChemistry Units 8 12reg speckNo ratings yet
- Shandong Lingong Wheel Loader LG956l Operation & Maintenance Manual Final 10.3.23Document130 pagesShandong Lingong Wheel Loader LG956l Operation & Maintenance Manual Final 10.3.23mliugong94% (16)
- Filipino Nurses United OrientationDocument30 pagesFilipino Nurses United OrientationErlinda PosadasNo ratings yet
- Agriculture Class-8Document67 pagesAgriculture Class-8Sahej100% (2)
- Scope Management Plan TemplateDocument10 pagesScope Management Plan TemplateAlessandro Rota100% (1)
- Preparation of Starch Nanoparticles in A New Ionic Liquid-in-Oil MicroemulsionDocument12 pagesPreparation of Starch Nanoparticles in A New Ionic Liquid-in-Oil MicroemulsionPaula NancyNo ratings yet
- Gaggia Cadorna Milk Full Instruction ManualDocument76 pagesGaggia Cadorna Milk Full Instruction ManualKanen Coffee, LLC.No ratings yet
- What Do You Already Know?: True TrueDocument3 pagesWhat Do You Already Know?: True TrueJeffrey MangaoangNo ratings yet
- Miller Toyota-Conversion-Kit Letter ENG WEBDocument4 pagesMiller Toyota-Conversion-Kit Letter ENG WEBskyduckNo ratings yet
- EXU EN 2017-12 Manual Web PDFDocument126 pagesEXU EN 2017-12 Manual Web PDFИльнур ТагировNo ratings yet
- MINDFULNESS CALENDARDocument1 pageMINDFULNESS CALENDARNiccy McOrrieNo ratings yet
- Text StructureDocument25 pagesText Structureapi-245317957No ratings yet
- Data Sheet Dump ValveDocument2 pagesData Sheet Dump ValveVlade NaumovskiNo ratings yet
- 85 HP John Deere 4045DFM50 Marine Diesel EngineDocument2 pages85 HP John Deere 4045DFM50 Marine Diesel EngineDAVIDNo ratings yet
- Plumbing-Water-System-Review (3B) PDFDocument22 pagesPlumbing-Water-System-Review (3B) PDFJhyneJazarenoAtutuboNo ratings yet
- Conveying Water Distribution SEODocument90 pagesConveying Water Distribution SEOmichelghanemNo ratings yet
- Separators: Figure OneDocument8 pagesSeparators: Figure OneMohamed Moder100% (1)
- DILEM 10 G (24VDC) MoellerDocument7 pagesDILEM 10 G (24VDC) MoellerElizabeth RamirezNo ratings yet
- Food Industry JTM2Document35 pagesFood Industry JTM2Jofin TMNo ratings yet
- E 242 - 95 R00 - Rti0mi1sruq - PDFDocument5 pagesE 242 - 95 R00 - Rti0mi1sruq - PDFLeón SuárezNo ratings yet
- FarkolDocument7 pagesFarkolHasiadin LaodeNo ratings yet
- PCOS Diet Cookbook For Newly Diagnosed IndividualsDocument67 pagesPCOS Diet Cookbook For Newly Diagnosed Individualsmavendave4lifeNo ratings yet
- Major Emergencies in Power PlantDocument29 pagesMajor Emergencies in Power Plantsourav mahapatraNo ratings yet
- 2.factory Price - Alarm Accessories-Complete 20150325Document15 pages2.factory Price - Alarm Accessories-Complete 20150325FREE BUSINESS INTELLIGENCENo ratings yet